Abstract
Inotuzumab ozogamicin (InO) is a CD22-directed antibody conjugated with calicheamicin. The phase IB of the ITCC-059 trial tested InO combined with chemotherapy in pediatric B-cell precursor acute lymphoblastic leukemia (BCP-ALL). Relapsed /refractory CD22+ BCP-ALL pediatric patients were enrolled. The primary objective was to establish the recommended phase II dose (RP2D). Secondary objectives included preliminary efficacy and tolerability. InO was combined with 1.5 mg/m2 of vincristine (days 3, 10, 17, 24), 20 mg/m2 of dexamethasone (2 5-day blocks, then amended), and intrathecal therapy. A rolling-6 design was used testing InO from 0.8 to 1.8 mg/m2/cycle. Between May 2020 and April 2022, 30 patients were treated, and 29 were evaluable for dose limiting toxicities (DLT). At 1.1 mg/m2/cycle, two of four patients had DLT (liver toxicity). InO was de-escalated to 0.8 mg/m2/cycle (N=6) without DLT while awaiting a protocol amendment to reduce dexamethasone dose to 10 mg/m2. Post amendment, InO was re-escalated to 1.1 mg/m2/cycle (N=6, 1 DLT), then to 1.4 mg/m2/cycle (N=3, no DLT), and finally to 1.8 mg/m2/cycle (N=7, 1 DLT). Three additional patients were treated in an expansion cohort. The pooled response rate was 80% (24/30; 95% confidence interval [CI]: 61.4-92.3) and, among responders, 66.7% achieved minimal residual disease negativity. The RP2D of InO combined with vincristine, dexamethasone and intrathecal therapy was declared at 1.8 mg/m2/cycle (1.5 mg/m2/cycle after remission) in a fractioned schedule. This combination showed a response rate similar to the single agent cohorts of this trial, with liver toxicity issues at the initial higher dexamethasone dose (clinicaltrials gov. Identifier: NTR5736).
Introduction
Approximately 10-15% of pediatric patients with acute lymphoblastic leukemia (ALL) experience disease relapse.1 Following relapse, the estimated 10-year overall survival (OS) probability is around 50%, depending on the risk group.2,3 The traditional treatment for relapsed patients is based on intensive chemotherapy.4 A randomized trial in relapsed and refractory (R/R) pediatric patients comparing the two most used treatment strategies in Europe, the ALL-REZ BFM 2002 and the UKALL-R3, showed no significant differences in the 5-year probability of event-free survival (EFS) or OS.5 Nevertheless, a subgroup analysis showed that patients with isolated bone marrow (BM) relapse had a significantly lower relapse rate (RR) if treated within the R3 arm (5-year cumulative incidence 6.5%, N=153) compared to the BFM arm (5-year cumulative incidence 12.5%, N=146); while the BFM approach resulted in superior outcome in patients experiencing isolated central nervous system (CNS) relapse (5-year EFS 81.6%, N=40 vs. 43.3%, N=45).5
Increasing the intensity of chemotherapy to treat R/R patients is constrained by toxicity. For example, the UKALL-R3 re-induction block 1 (vincristine, mitoxantrone, dexamethasone, and asparaginase) results in non-negligible adverse events (AE), especially in terms of severe infections (23.7%) and induction death (3%).5 In B-cell precursors (BCP) ALL, toxicity can be reduced by using the CD19-directed T-cell engager blinatumomab, which proved efficacious in high-risk first relapse patients, while the re-induction remission rate in overt relapse ranged between 34% and 60%.6-8 Moreover, CD19-specific chimeric antigen receptor (CAR) T-cell therapies showed high complete remission rates in multiple relapsed BCP-ALL patients, and may be considered definitive therapy without allogeneic hematopoietic stem cell transplantation (HSCT) in some cases. Indeed, a 3-year EFS of 44% was reported for patients enrolled in the ELIANA trial.9 ,10
Despite improvements, new options for effective salvage of pediatric R/R ALL patients and for increasing the overall cure rates in this cancer are still needed. In the context of targeted chemotherapy, inotuzumab ozogamicin (InO) is a CD22-directed antibody-drug conjugate loaded with the cytotoxic agent calicheamicin which is already approved for adults with CD22+ R/R BCP-ALL, based on the results from the INO-VATE ALL trial.11,12 The safety and preliminary efficacy of InO as a single agent in pediatric R/R BCP-ALL have been tested in phase I and phase II trials conducted by the Innovative Therapies for Children with Cancer (ITCC) consortium in Europe and by the Children’s Oncology Group (COG) in the USA.13-15 Namely, the estimated overall response rate (ORR) in the phase II trials from COG and ITCC groups ranged from 58.3% (90% confidence interval [CI]: 46.5-69.3) to 81.5% (95% CI: 61.9-93.7), respectively, with approximately 70% minimal residual disease (MRD) negativity rate in responding patients.14,16 Overall, InO appeared well-tolerated in children with R/R BCP-ALL and was associated with high response rates, potentially higher than with blinatumomab, despite no trial compared the two treatments in this population.
Studies in adults have investigated InO combined with chemotherapy, for examples with mini-hyper-CVD (cyclophosphamide, vincristine and dexamethasone in cycles 1, 3, 5, 7, and methotrexate plus cytarabine in cycles 2, 4, 6 and 8) or CVP (cyclophosphamide, vincristine and prednisone), and showed it is safe to combine these agents.17,18 By contrast, in pediatrics, the safety of InO in combination with chemotherapy has not been assessed yet. Herein, we report the results from the phase IB of the trial ITCC-059 in the R/R setting, in which InO was combined with a modified UKALL-R3 regimen containing vincristine, dexamethasone and intrathecal (IT) therapy. This combination was developed with the aim to replace mitoxantrone with InO in the UKALL-R3 re-induction regimen, aiming at increasing efficacy while reducing toxicity.
Trial ITCC-059 is a phase I-II, multicenter, international, open-label clinical trial conducted in accordance with the International Council for Harmonization Guidelines for Good Clinical Practice, and the Declaration of Helsinki. Patients were treated under protocol version 3 and 4 following an amendment, after the single-agent recommended phase II dose (RP2D) was established in the single agent phase I part. Informed consent was obtained from all patients or their parents (as applicable) before enrollment. The study was sponsored by the Erasmus MC and funded by Pfizer Inc. in the context of a Pediatric Investigational Plan (Netherlands Trial Registry number: NL5629; EudraCT: 2016-000227-71).
Methods
Patients and treatment
Patients aged ≥1 to <18 years, with CD22+ BCP-ALL, M2/M3 bone marrow status, and either refractory disease, ≥2nd relapse, or any relapse post-HSCT were enrolled. Patients with isolated extramedullary disease were excluded (Online Supplementary Table S1). The protocol received Institutional Review Board and/or Ethics Committee review and approval at all participating centers.
Four dose levels (DL) of InO (fractionated on days 1, 8, and 15 of each cycle) with loading dose on day 1 (omitted once in remission) were tested (Online Supplementary Table S2).19 Namely, 0.8 mg/m2/cycle (0.4 + 0.2 + 0.2 mg/m2), 1.1 mg/m2/cycle (0.5 + 0.3 + 0.3 mg/m2), 1.4 mg/m2/cycle (0.6 + 0.4 + 0.4 mg/m2) and 1.8 mg/m2/cycle (0.8 + 0.5 + 0.5 mg/m2). InO was combined with vincristine 1.5 mg/m2 (days 3, 10, 17 and 24), two 5-days blocks (days 1-5 and 15-20) of dexamethasone 20 mg/m2 (later amended), and, depending on CNS status, IT therapy (days 1 and 8) with methotrexate alone or combined with cytarabine and steroids as per the UKALL-R3 regimen (Online Supplementary Figure S1).20 From cycle 2, and per investigator’s discretion, patients could receive either combination therapy or InO single agent at 1.8 mg/m2/cycle, or 1.5 mg/m2/cycle if already in remission.13 A maximum of six cycles were allowed (of which maximum 2 combination cycles), except for those cases planned to proceed to HSCT, for which two cycles, or three in case the patient was not yet MRD-negative after cycle 2 two, were recommended. Criteria to proceed with the next cycle are reported in the Online Supplementary Methods S1.
Study design
The primary objective was to determine the RP2D. A rolling-6 design was used, assessing dose limiting toxicities (DLT) during cycle 1 (28 days) and capping the maximum escalation dose at 1.8 mg/m2/cycle, based on the RP2D of InO single agent.13,21 The primary endpoint was the occurrence of DLT, defined as any of the following toxicities related to InO: any grade 5 toxicity; absolute neutrophil count (ANC) <0.5x109/L and/or a platelet count <50x109/L lasting >42 days in the absence of persisting leukemia; grade 3-4 non-hematologic toxicities persisting for >48 hours (>7 days for hepatic transaminases or bilirubin abnormalities). Secondary endpoints included frequency and severity of AE based on the Common Terminology Criteria for Adverse Events version 4.03, and occurrence of toxic death. Preliminary efficacy endpoints included ORR and MRD negativity status (as best response after InO treatment and after cycle 1), OS, EFS, duration of response (DOR). All patients who received at least one dose of InO were considered for safety analysis. Those who also completed at least one baseline and one post-baseline disease assessment were considered for efficacy analysis (Online Supplementary Methods S2). ORR was defined as the combined complete remission (CR; <5% BM blast, CNS1 without extramedullar leukemia), CR with insufficient platelet recovery (CRp; ANC >0.5x109/L but platelets ≤50x109/L), and CR without recovery of counts (CRi; ANC ≤0.5x109with or without platelets ≤50x109/L). MRD negativity was centrally determined and defined as either a quantitative polymerase chain reaction (QT-PCR) result below 10-4, or a flow cytometry result below 0.01% when was negative, but the quantitative range was >10-4 (Online Supplementary Methods S3).22,23 EFS and OS probabilities (Online Supplementary Methods S4) were estimated using the Kaplan-Meier method. sinusoidal obstruction syndrome (SOS) definition is provided in the Online Supplementary Methods S5.
Results
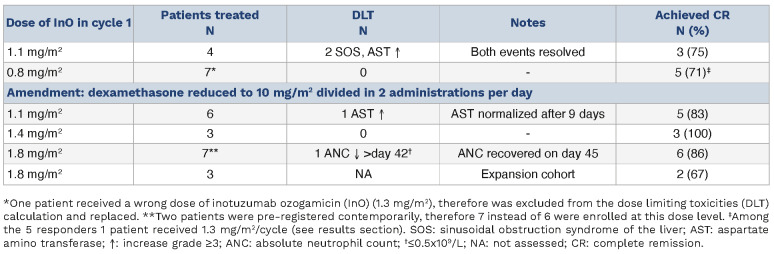
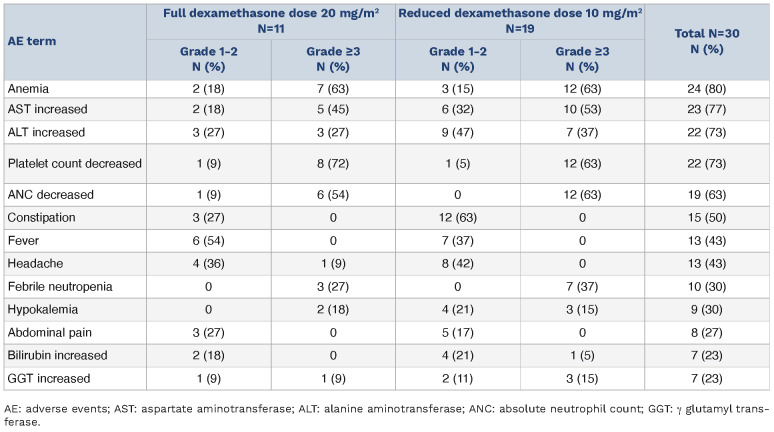
Between May 14, 2020 and April 11, 2022, 37 patients were screened, 30 were treated, 29 were evaluable for the assessment of DLT, and 30 were evaluable for response (1 patient received the wrong dose of InO on day 1 of cycle 1; the patient was excluded from the DLT assessment, but counted for response and overall safety as per protocol). Dataset cut-off date was February 28, 2023. Patient characteristics are reported in Table 1. Initially, four patients were enrolled at 1.1 mg/m2/cycle of InO. Two DLT occurred; namely grade 3 hepatic transaminases elevation lasting more than 7 days, and one case of grade 3 SOS. InO was then de-escalated to 0.8 mg/m2/cycle, and seven patients completed cycle 1, of which one received in error 0.8 mg/m2 on day 1, 0.5 mg/m2 on day 8, and skipped the day 15 dose (instead of receiving 0.4 + 0.2 + 0.2 mg/m2 on days 1, 8 and 15) and therefore was not evaluable for DLT (but included in the safety and efficacy dataset). No DLT were recorded at 0.8 mg/m2/cycle of InO. Nevertheless, the Steering Committee decided to amend the protocol to reduce the dexamethasone dose from 20 mg/m2/day to 10 mg/m2/day (divided in 2 daily administrations). The intent was 2-fold. First, mitigating liver toxicity which consisted of transient hepatic transaminase elevation probably caused by steroids and, secondly, allowing the use of higher doses of InO, closer to the RP2D already established for the single agent regimen (1.8 mg/m2/cycle) also given the lower response rate observed at lower doses in phase IA (DL1: ORR 75% and MRD negativity: 66%; DL2: ORR 85%, and MRD negativity 100%).13,16
Table 1.
Patient characteristics.
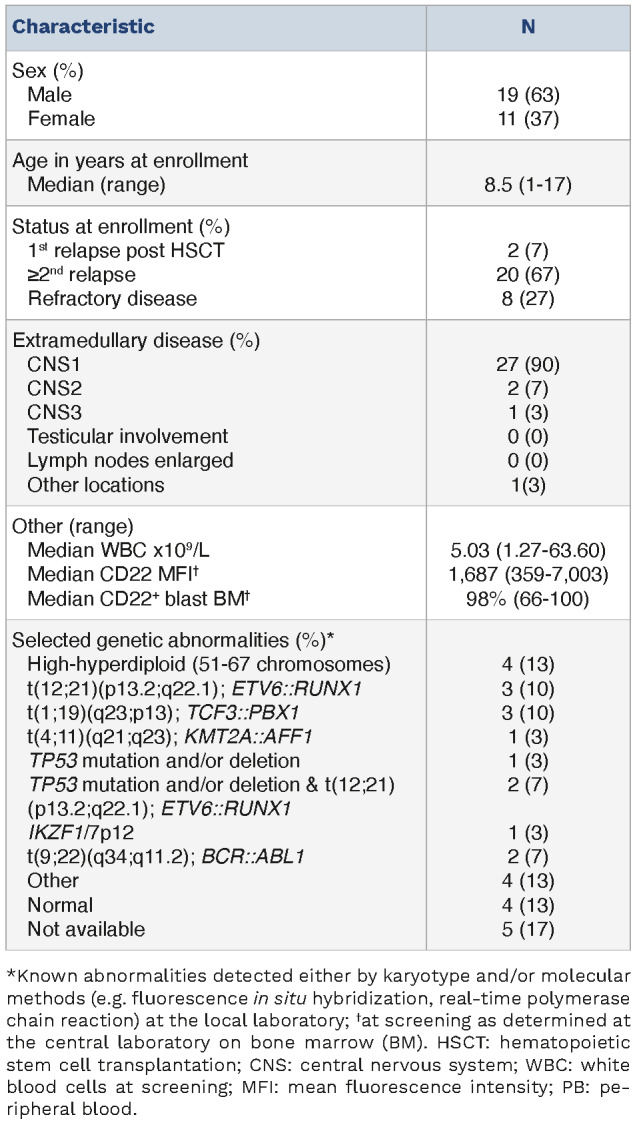
Upon approval of the amendment the dose of InO was re-escalated. InO was first tested at 1.1 mg/m2/cycle (N=6, one DLT: grade 3 hepatic transaminases elevation >7 days); subsequently at 1.4 mg/m2/cycle (N=3, no DLT), and then at 1.8 mg/m2/cycle (N=7 as 2 patients registered contemporary; 1 DLT occurred: ANC below 0.5x109/L >day 42). At the same dose level, three additional patients were enrolled in an expansion cohort (not assessed for DLT), increasing the total number of patients treated at 1.8 mg/m2 of InO combined with chemotherapy to ten (Table 2). The RP2D of InO in combination with 1.5 mg/m2 of vincristine (days 3, 10, 17, 24) and 10 mg/m2 of dexamethasone (2 5-day blocks) was declared at 1.8 mg/m2/cycle (1.5 mg/m2/cycle once in complete remission).
Table 2.
Dose escalation history.
Table 3.
Most frequent treatment emergent adverse events (>20%) divided by grade and before and after dexamethasone amended dose.
Safety
Sixteen patients received only one cycle of combination therapy, ten patients one combination cycle plus one single agent cycle, three patients two combination cycles, and one patient received one combination cycle plus two single agent cycles.
All patients experienced at least one AE (Online Supplementary Table S3). Alanine aminotransferase increase (ALT) occurred in 23 patients (76.%) of which 15 (50%) were grade ≥3. Aspartate aminotransferase (AST) increase occurred in 22 patients (73.3%) of which ten (33.3%) were grade ≥3. Overall, 24 (80%) patients had either AST and/or ALT elevation. Seven patients (23.3%) had bilirubin increase; of which six (20%) at grade 1-2, and one (3%) at grade 3. None met Hy’s law criteria.24 Toxicities recorded before and after amending the dexamethasone dose are provided in Table 3.
Overall, 63% of patients reported infections. Four (13%) patients had sepsis, one (3%) had grade 3 skin infection, one (3%) grade 3 urinary infection, and two (7%) other grade 3 infections. Other eleven (36.7%) patients had grade 1-2 infections. Ten patients (33.3%) had grade 3 febrile neutropenia.
Platelet count decrease was experienced by 22 patients (73%) of which 20 (67%) at grade ≥3. Overall, ANC decrease was observed in 19 patients (63.3%) of which 18 (60%) at grade ≥3. Anemia was experienced by 24 patients (80%) of which 19 (63.3%) at grade ≥3. The full lists of AE, treatment-relatedness, and laboratory abnormalities are provided in Online Supplementary Tables S3-5. In total, five (17%) patients developed SOS. Four following HSCT (1 grade 4 and 3 grade 3), after receiving a cumulative dose of 2.2, 2.9, 3.2 and 3.6 mg/m2 of InO, and being transplanted 68, 38, 30 and 29 days since the last InO dose, respectively. The fifth case of SOS (grade 3) occurred on treatment after the administration of 0.8 mg/m2 (0.5 + 0.3) of InO. Among those developing SOS post InO, one subject had a prior transplant. Four patients with SOS recovered completely, while in one case SOS was ongoing when the patient died due to sepsis after HSTC. Overall, SOS occurred in 21% (4/19) of the patients that received a HSCT any time after InO (including patients receiving additional treatment after InO and before HSCT). The median time to onset of SOS since the last InO dose was 47.5 days (range, 36-119). Among the transplanted patients, six received prophylaxis with defibrotide per investigators’ discretion, none of which developed SOS. An 11-year-old female subject who had received chemotherapy and two prior HSCT developed posterior reversable encephalopathy syndrome while on treatment with InO at 1.8 mg/m2/cycle and dexamethasone at 10 mg/m2 at day 19 of the first cycle. The patient also received IT methotrexate on day 1 and 8 (15 mg) and vincristine on days 3, 10, 17. The subject recovered completely. The event was not considered related to InO but rather attributed to the background chemotherapy.25 Four patients died while in CR after receiving HSCT. Two of them died due to infection (respiratory infection and post SOS septic shock), one had a multiorgan failure, and the fourth death was due to thrombotic microangiopathy (without prior SOS). The cumulative incidence of non-relapse death was 6.7% (95% CI: 1.1-19.5) at 6 months, and 10.2% (95% CI: 2.5-24.3) at 12 months, including post HSCT follow-up.
Figure 1.
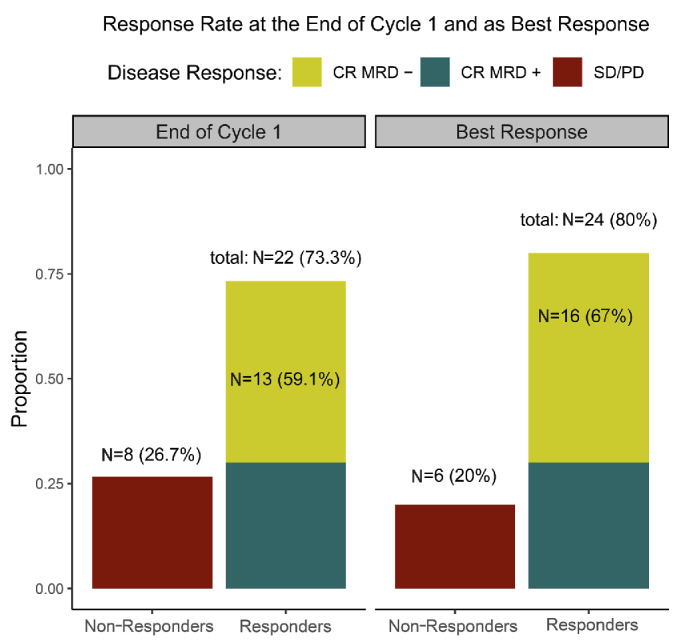
Proportions of non-responders, responders and minimal residual disease negativity. Responders are defined as those with <5% of bone marrow blasts regardless the recovery of the neutrophil count and platelets. Minimal residual disease (MRD) negativity is defined as <10-4. CR: complete remission; SD/PD: stable disease/progressive disease.
Efficacy
Combining all dose levels (N=30), 24 patients achieved complete response (ORR 80%; 95% CI: 61.4-92.3) of which 22 (73%) after cycle 1; 20 were in CR, three in CRp and one in CRi. Response by dose level is provided in Table 2. Among responders, MRD negativity as best response was achieved by 16 (66.7%) subjects of which 13 after cycle 1 (Figure 1). Among those treated at 1.8 mg/m2 in cycle 1 (N=10), eight (80.0%) achieved response, and six (75.0%) also achieved MRD negativity after cycle 1.
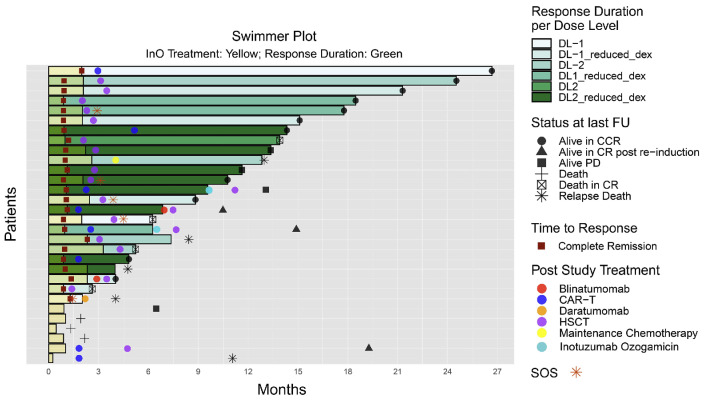
A total of 21 patients (70%) proceeded to consolidation therapy, 15 (50%) with HSCT (of which 1 after bridging with blinatumomab in presence of MRD positivity) and six (20%) with CAR T-cell therapy. Additionally, at the time of cut-off date, one responding patient received maintenance chemotherapy (then died due to relapse 10 months after last dose of InO) and other two responding patients had not yet received consolidation treatment and relapsed a few months later (Figure 2). Other four patients received HSCT following additional therapy, of which three after relapse post InO, and one among the non-responders. Notably two of them received InO a second time and were able to proceed to HSCT (after relapse post CAR T).
The median follow-up was 15.9 months (interquartile range [IQR], 12.4-18.4). At 6 months, the EFS probability was 66.5% (95% CI: 51.5-85.8) and the OS probability was 76.6% (95% CI: 62.9-93.4). At 12 months, the EFS probability was 41.7% (95% CI: 27.1-64.3) and the OS probability was 62.3% (95% CI: 46.9-82.8) (Figure 3). Median DOR was 8.38 months (IQR, 2.3-11.9). In a post hoc analysis, we did not observe statistically significant differences in EFS and OS between responders consolidated with HSCT or CAR T-cell therapy (Online Supplementary Figures S2, S3). The cumulative incidence of relapse was 8.3% (95% CI: 1.0-27.0) at 6 months and 13.6% (95% CI: 2.9-34.0) at 12 months. Overall, ten patients relapsed of which five died (Figure 4), and three deaths occurred among the five non-responding subjects. Additionally, four patients died while in remission, for a total of 12 deaths.
Discussion
This trial showed that in pediatric R/R CD22+ BCP-ALL patients InO can be safely combined with 1.5 mg/m2 of vincristine (days 3, 10, 17, 24), 10 mg/m2 of dexamethasone (2 5-day blocks, BID) and IT therapy, at 1.8 mg/m2/cycle, the same RP2D as per InO single agent.13,19
Figure 2.
Swimmer plot of patients’ treatment and response. Each bar starts at day 1 of cycle 1. Yellow shaded areas represent the study treatment period. Green shaded areas represent the duration of response. Inotuzumab ozogamicin (InO) dose levels (DL): DL-1: 1.1 mg/m2/cycle; DL-2: 0.8 mg/m2/cycle; DL2: 1.8 mg/m2/cycle; DL-1_amd: 1.1 mg/m2/cycle (reduced dexamethasone); DL1_amd: 1.8 mg/m2/cycle (reduced dexamethasone); DL2_amd: 1.8 mg/m2/cycle (reduced dexamethasone); 16 patients received only 1 cycle (combination), 10 patients 1 combination cycle + 1 single agent cycle, 3 patients 2 combination cycles, 1 patient received 3 cycles (1 combination cycle + 2 single agent cycles). CR: complete remission; CCR: continuous complete remission achieved on InO therapy; PD: progressive disease/relapse; CAR T: chimeric antigen receptor T-cell therapy; HSCT: hematopoietic stem cell transplantation; SOS: sinusoidal obstruction syndrome; NA: not applicable; FU: follow-up.
Despite this promising safety profile, our data suggest that the combination of InO with chemotherapy might increase the risk of transaminases elevation compared to the single-agent treatment. Indeed, we observed 14.3% AST elevation grade ≥3 and 17.9% ALT elevation grade ≥3 in the single agent arm of this trial, compared to 33.3% grade ≥3 AST elevation and 50% grade ≥3 ALT elevation in the combination arm reported here. It is well known that transaminases are frequently increased by chemotherapy and by dexamethasone.26 The clinical relevance of this data remains unclear as ALT/AST increase does not necessarily reflect or predict severe hepatotoxicity and, in our study, it was neither associated with severe or long-lasting liver impairment, nor with clinically significant bilirubin increase, which only in one case was reported at grade 3 and none at grade 4.26,27 By contrast, we confirm that one of the major risks associated with InO is SOS, and particularly in patients proceeding to HSCT as consolidation after InO treatment. Nevertheless, the addition of vincristine and dexamethasone to InO did not seem to further increase the incidence of SOS when compared to the single agent arms of the same trial (overall SOS incidence was 16.6% in phase IB vs. 17.3% in phase IA and II combined; while among patients consolidating with HSCT after InO treatment it was 21% vs. 26.1%, respectively), despite a rigorous comparison was not possible due to the non-randomized approach, the heterogeneity of the InO dose administered, SOS prophylaxis which was not uniformly performed, and the small sample size.13,16 Beside, no significant differences in the incidence of AE were observed before and after the amendment of the protocol (Table 3) in this limited sample size. Nevertheless, reducing dexamethasone dose prevented the occurrence of DLT and allowed a higher escalation of InO under the rolling-6 rules.
The data reported above are in line with other trials in older R/R patients with CD22+ BCP-ALL. In trial SWOG 1312 (NSC-772518), InO at 1.8 mg/m2 was safely combined with cyclophosphamide 750 mg/m2, vincristine 1.4 mg/m2 and maximum 2 mg, prednisone 100 mg orally days 1-5 for R/R CD22+ BCP-ALL, resulting in approximately 60% response.18 Similarly, in the EWALL-INO study (clinicaltrials gov. Identifier: NCT03249870), InO was safely combined at 1.8 mg/m²/cycle with one triple IT injection, vincristine (1-2 mg, weekly) on day 1, 8, 15 and 22, and four 2-day blocks of dexamethasone (20 mg/day) and resulted in 87.7% response.28
In terms of efficacy, the ORR of InO combined with chemotherapy was comparable to the single agent arm of the trial (ORR 80% vs. 81.5%).16 In this phase IB, though, it should be noticed that in cycle 1 we tested a much larger spectrum of dose levels, from 0.8 mg/m2/cycle to 1.8 mg/m2/cycle. In addition, the estimated ORR for the single agent cohort of this trial is already very high and it might be unnecessary to combine InO with toxic chemotherapy in heavily pretreated patients to obtain a relatively small marginal improvement. Due to these considerations, it was decided not to proceed with the additional cohort 1B-ASP as originally planned, in which PEG-asparaginase on day 3 and 17 (1,000 IU/m2) would have been simultaneously added to the combination of InO and chemotherapy.
Figure 3.
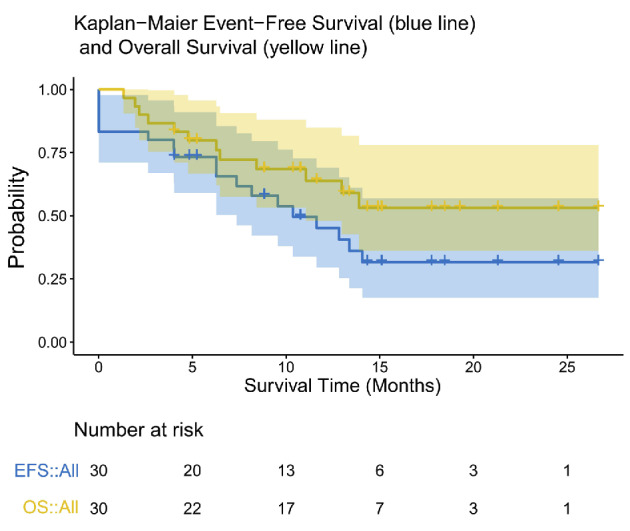
Overall survival and event-free survival. Probabilities were estimated using the Kaplan-Meier method. Events were defined as non-response (not achieving complete remission [CR], CR with insufficient platelet recovery [CRi] or CR without recovery of counts [CRp], considered as event at day 0), relapse after remission achieved as a result of inotuzumab ozogamicin (InO) treatment, death from any cause, or secondary malignancies. Crosses represent censored subjects. Shaded areas represent the 95% confidence interval. OS: overall survival; EFS: event-free survival.
Figure 4.
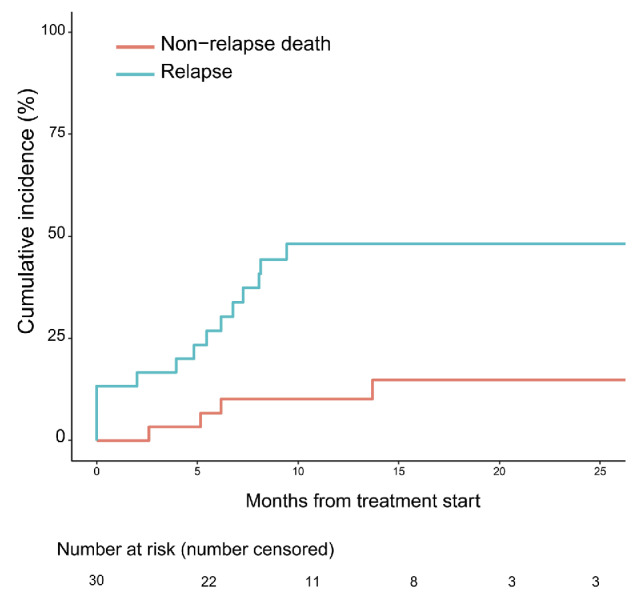
Cumulative incidence of relapses and non-relapse death. Probabilities were estimated using the Kaplan-Meier method. Patients not achieving remission were counted as event at time zero for the cumulative incidence of relapse (blue line). Patients dying while in remission achieved as a result of inotuzumab ozogamicin (InO) treatment were counted as event in the non-relapse death curve (red line).
Furthermore, it is worth noting that recent data showed that low-intensity chemotherapy schemes without asparaginase when combined with multi-agent immunotherapy can deliver very high ORR in both adults and children while sparing some of the toxicities related to chemotherapy.29,30 For example, the MD Anderson Cancer Center is developing multi-agent immune/target therapy regimens that combine low-intensity chemotherapy with blinatumomab, InO and rituximab in the so-called Pedi-cRIB regimen (clinicaltrials gov. Identifier: NCT05645718). Early results have described that the combination of mini-hyper-CVD with cRIB (InO at 1.2 mg/m2/cycle: 0.6 + 0.3 + 0.3 mg/m2) is well-tolerated also in heavily pretreated pediatric patients.31 In adults, mini-Hyper-CVD was administered with InO at a dose of 1.3-1.8 mg/m2 in cycle 1, which was later amended to lower dosages to mitigate the risk of liver toxicities. Rituximab was added in CD20+ patients only and patients subsequently received consolidation with blinatumomab. The combination yielded a remission rate of 89%, and the 5-year progression-free survival was 44.0% (95% CI: 31.2-54.3), in elderly newly diagnosed patients (N=80, median age 68; IQR, 63-72); while in younger subjects (N=31, median age 25; range, 18-57) the remission rate and 1-year OS probability were both 100%, although three patients (10%) had isolated CNS relapse (clinicaltrials gov. Identifier: NCT01371630).32-34 Such regimens, developed due to the poor tolerance of high-intensity chemotherapy in elderly patients, are now being integrated into frontline setting followed by CAR T-cell consolidation. This represents a new paradigm for front-line ALL treatment which might impact also future pediatric regimens currently still relying on conventional chemotherapy, particularly for the induction phase of the treatment.35
In the context of R/R pediatric patients, the trial clinicaltrials gov. Identifier: NCT05748171 will randomize InO as single agent against the UKALL-R3 regimen in high-risk first relapse ALL patients. In newly diagnosed pediatric patients, a phase III randomized trial in high-risk CD22+ BCP-ALL (AALL1732) sponsored by COG, is evaluating two cycles of single agent InO at 1.2 mg/m2 after standard induction and post-induction chemotherapy. Following consolidation, patients with MRD >0.01% were randomized 1:1 (N=50) to chemotherapy (arm A) or chemotherapy plus two cycles of InO (arm B), one before the high-dose methotrexate interim maintenance and the other before proceeding to the delayed intensification blocks. From an interim analysis, no differences in grade ≥3 ALT or bilirubin elevations were recorded between arm A and B, but patients treated with InO showed a significant higher incidence of neutropenia (87.5% vs. 50%) and sepsis during delayed intensification (10 cases in arm B, 1 case in arm A), as well as SOS (4 cases in arm B, 0 in arm A). The enrolment was halted and treatment was amended to mitigate toxicity during post InO chemotherapy blocks.36 In Europe, the ‘AllTogether1’ group (clinicaltrials gov. Identifier: NCT03911128) will test InO given at 0.5 mg/m2/week for 6 weeks as additional consolidation block in a randomized fashion within the intermediate-high risk group in patients with high MRD levels. Patients randomized to receive InO, will be given two cycles of InO during consolidation.
In conclusion, preliminary efficacy and safety data underscore the possibility to combine InO up to 1.8 mg/m2 with vincristine, dexamethasone and IT therapy in a safe manner. Nevertheless, a noticeable advantage of this combination regimen in terms of ORR when compared to the single agent arms of the same trial was not observed in these heavily pretreated patients. This study contributes to the knowledge on safety and efficacy of InO in pediatric patients, and opens the possibility to use less chemo-intensive treatments in pediatric ALL by either using InO as a single agent or in combination with immunotherapies such as blinatumumab and rituximab as already done in adults.
Supplementary Material
Acknowledgments
The authors would like to thank all patients participating in the trial and their parents, as well as all colleagues involved in patient care and in all aspects of the trial. They also would like to thank the ITCC consortium and the I-BFM study group for providing the infrastructure and the collaborative environment to run early clinical trials in pediatric oncology, and Pfizer Inc. for providing funding and a clinical research collaboration to implement the study. Authors are grateful to the technicians of the Laboratory of Medical Immunology at the Erasmus MC, and to the technicians of the M. Den Boer Laboratory at the Princess Máxima Center, for their contribution to the laboratory data. Authors acknowledge Dr David Ziegler, for his work in the initial set-up and writing phase of this trial.
Funding Statement
Funding: This trial was funded by Pfizer Inc.
Data-sharing statement
Anonymized data are available in consultation with the sponsor and subject to review.
References
- 1.Pui CH, Yang JJ, Hunger SP, et al. Childhood acute lymphoblastic leukemia: Progress through collaboration. J Clin Oncol. 2015;33(27):2938-2948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oskarsson T, Söderhäll S, Arvidson J, et al. Relapsed childhood acute lymphoblastic leukemia in the Nordic countries: prognostic factors, treatment and outcome. Haematologica. 2016;101(1):68-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rheingold SR, Ji L, Xu X, et al. Prognostic factors for survival after relapsed acute lymphoblastic leukemia (ALL): a Children’s Oncology Group (COG) study. J Clin Oncol. 2019;37:(Suppl 15):10008. [Google Scholar]
- 4.Parker C, Waters R, Leighton C, et al. Effect of mitoxantrone on outcome of children with first relapse of acute lymphoblastic leukaemia (ALL R3): an open-label randomised trial. Lancet. 2010;376(9757):2009-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Von Stackelberg A, Bourquin J-P, Zimmermann M, et al. ALL-REZ BFM 2002 is associated with improved outcome as compared to ALL-R3 strategy in children with standard risk isolated CNS relapse of acute lymphoblastic leukemia, while maintaining comparable efficacy in patients with bone marrow relapse. results of the multi-national, multi-center Trial IntReALL SR 2010. Blood. 2022;140(Suppl 1):3247-3249. [Google Scholar]
- 6.Von Stackelberg A, Locatelli F, Zugmaier G, et al. Phase I/phase II study of blinatumomab in pediatric patients with relapsed/refractory acute lymphoblastic leukemia. J Clin Oncol. 2016;34(36):4381-4389. [DOI] [PubMed] [Google Scholar]
- 7.Locatelli F, Zugmaier G, Mergen N, et al. Blinatumomab in pediatric patients with relapsed/refractory acute lymphoblastic leukemia: results of the RIALTO trial, an expanded access study. Blood Cancer J. 2020;10(7):77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Queudeville M, Ebinger M. Blinatumomab in pediatric acute lymphoblastic leukemia -from salvage to first line therapy (a systematic review). J Clin Med. 2021;10(12):2544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maude SL, Frey N, Shaw PA, et al. Chimeric antigen receptor T cells for sustained remissions in leukemia. N Engl J Med. 2014;371(16):1507-1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laetsch TW, Maude SL, Rives S, et al. Three-Year update of tisagenlecleucel in pediatric and young adult patients with relapsed/refractory acute lymphoblastic leukemia in the ELIANA Trial. J Clin Oncol. 2023;41(9):1664-1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Vries JF, Zwaan CM, De Bie M, et al. The novel calicheamicin-conjugated CD22 antibody inotuzumab ozogamicin (CMC-544) effectively kills primary pediatric acute lymphoblastic leukemia cells. Leukemia. 2012;26(2):255-264. [DOI] [PubMed] [Google Scholar]
- 12.Kantarjian HM, DeAngelo DJ, Stelljes M, et al. Inotuzumab ozogamicin versus standard of care in relapsed or refractory acute lymphoblastic leukemia: final report and long-term survival follow-up from the randomized, phase 3 INO-VATE study. Cancer. 2019;125(14):2474-2487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brivio E, Locatelli F, Lopez-Yurda M, et al. A phase 1 study of inotuzumab ozogamicin in pediatric relapsed/refractory acute lymphoblastic leukemia (ITCC-059 study). Blood. 2021;137(12):1582-1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O’Brien MM, Ji L, Shah NN, et al. Phase II trial of inotuzumab ozogamicin in children and adolescents with relapsed or refractory B-cell acute lymphoblastic leukemia: Children’s Oncology Group protocol AALL1621. J Clin Oncol. 2022;40(9):956-967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bhojwani D, Sposto R, Shah NN, et al. Inotuzumab ozogamicin in pediatric patients with relapsed/refractory acute lymphoblastic leukemia. Leukemia. 2019;33(4):884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pennesi E, Michels N, Brivio E, et al. Inotuzumab ozogamicin as single agent in pediatric patients with relapsed and refractory acute lymphoblastic leukemia: results from a phase II trial. Leukemia. 2022;36(6):1516-1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jabbour E, Sasaki K, Ravandi F, et al. Chemoimmunotherapy with inotuzumab ozogamicin combined with mini-hyper-CVD, with or without blinatumomab, is highly effective in patients with Philadelphia chromosome-negative acute lymphoblastic leukemia in first salvage. Cancer. 2018;124(20):4044-4055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Advani AS, Moseley A, Liedtke M, et al. SWOG 1312 final results: a phase 1 trial of inotuzumab in combination with CVP (cyclophosphamide, vincristine, prednisone) for relapsed/refractory CD22+ acute leukemia. Blood. 2019;134(Suppl 1):227.31003999 [Google Scholar]
- 19.Pfizer Inc. BESPONSA® (inotuzumab ozogamicin) Dosing & administration |Safety Info. https://besponsa.pfizerpro.com/dosing Accessed April 15, 2022. [Google Scholar]
- 20.Parker C, Krishnan S, Hamadeh L, et al. Outcomes of patients with childhood B-cell precursor acute lymphoblastic leukaemia with late bone marrow relapses: long-term follow-up of the ALLR3 open-label randomised trial. Lancet Haematol. 2019;6(4):e204-e216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Skolnik JM, Barrett JS, Jayaraman B, Patel D, Adamson PC. Shortening the timeline of pediatric phase I trials: the rolling six design. J Clin Oncol. 2008;26(2):190-195. [DOI] [PubMed] [Google Scholar]
- 22.Theunissen P, Mejstrikova E, Sedek L, et al. Standardized flow cytometry for highly sensitive MRD measurements in B-cell acute lymphoblastic leukemia. Blood. 2017;129(3):347-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van der Velden VHJ, Panzer-Grümayer ER, Cazzaniga G, et al. Optimization of PCR-based minimal residual disease diagnostics for childhood acute lymphoblastic leukemia in a multi-center setting. Leukemia. 2007;21(4):706-713. [DOI] [PubMed] [Google Scholar]
- 24.Robles-Diaz M, Lucena MI, Kaplowitz N, et al. Use of Hy’s law and a new composite algorithm to predict acute liver failure in patients with drug-induced liver injury on behalf of the Spanish DILI Registry, the SLatinDILI Network, and the Safer and Faster Evidence-based Translation Consortium. Gastroenterology. 2014;147(1):109-118.e5. [DOI] [PubMed] [Google Scholar]
- 25.Schmiegelow K, Attarbaschi A, Barzilai S, et al. Consensus definitions of 14 severe acute toxic effects for childhood lymphoblastic leukaemia treatment: a Delphi consensus. Lancet Oncol. 2016;17(6):e231-e239. [DOI] [PubMed] [Google Scholar]
- 26.King PD, Perry MC. Hepatotoxicity of chemotherapy; hepatotoxicity of chemotherapy. Oncologist. 2001;6(2):162-176. [DOI] [PubMed] [Google Scholar]
- 27.Ricart AD. Drug-induced liver injury in oncology. Ann Oncol. 2017;28(8):2013-2020. [DOI] [PubMed] [Google Scholar]
- 28.Chevallier P, Leguay T, Doubek M, et al. Fractionated inotuzumab ozogamicin combined with low-intensity chemotherapy provides very good outcome in older patients with newly diagnosed CD22+ Philadelphia chromosome-negative B-cell precursor acute lymphoblastic leukemia: first results from the EWALL-INO study. Blood. 2021;138(Suppl 1):511. [Google Scholar]
- 29.Maese L, Rau RE. Current use of asparaginase in acute lymphoblastic leukemia/lymphoblastic lymphoma. Front Pediatr. 2022;10:902117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Egler RA, Ahuja SP, Matloub Y. L-asparaginase in the treatment of patients with acute lymphoblastic leukemia. J Pharmacol Pharmacother. 2016;7(2):62-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McCall D, Jabbour E, Roth M, Nunez C, Cuglievan B. Mini-hyper CVD + CRIB (condensed rituximab, inotuzumab ozogamicin, and blinatumomab) for refractory pediatric B-acute lymphoblastic leukemia. Pediatr Blood Cancer. 2023;70(1):e29939. [DOI] [PubMed] [Google Scholar]
- 32.Jabbour E, Short NJ, Senapati J, et al. Mini-hyper-CVD plus inotuzumab ozogamicin, with or without blinatumomab, in the subgroup of older patients with newly diagnosed Philadelphia chromosome-negative B-cell acute lymphocytic leukaemia: long-term results of an open-label phase 2 trial. Lancet Haematol. 2023;10(6):e433-e444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Macaron W, Kantarjian HM, Short NJ, et al. Updated results from a phase II study of mini-hyper-CVD (mini-HCVD) plus inotuzumab ozogamicin (INO), with or without blinatumomab (Blina), in older adults with newly diagnosed Philadelphia chromosome (Ph)-negative B-cell acute lymphoblastic leukemia (ALL). J Clin Oncol. 2022;40:(Suppl 16):7011. [Google Scholar]
- 34.Short NJ, Kantarjian HM, Ravandi F, et al. A phase II study of hyper-CVAD with sequential blinatumomab (Blina), with or without inotuzumab ozogamicin (INO), in adults with newly diagnosed B-cell acute lymphoblastic leukemia (ALL). Hemasphere. 2023;7(Suppl e67564ca):poster 358. [Google Scholar]
- 35.Jabbour E, Short NJ, Jain N, et al. The evolution of acute lymphoblastic leukemia research and therapy at MD Anderson over four decades. J Hematol Oncol. 2023;61(1):22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.O’Brien MM, McNeer JL, Rheingold SR, et al. A phase 3 trial of inotuzumab ozogamicin for high-risk B-ALL: second safety phase results from Children’s Oncology Group AALL1732. J Clin Oncol. 2023;41:(Suppl 16):10016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Anonymized data are available in consultation with the sponsor and subject to review.