Abstract
Aim
Knee stiffness limits activities of daily living with treatment having no gold standard technique currently. We present follow-up data 1-year after quadricepsplasty using the Adolphson–Cerqueira technique for the treatment of knee stiffness in a Brazilian population sample.
Materials and methods
This retrospective study included patients who underwent a quadricepsplasty using the Adolphson–Cerqueira technique between January 2006 and March 2023 at our institution. The inclusion criteria were: (1) Knee stiffness with a range of motion <70°; (2) Patellar excursion ≥2 mm on physical examination; (3) Available knee radiography in the anteroposterior and lateral views; and (4) A follow-up at 1 year postoperatively. The Judet Classification was used to assess the outcome of the quadricepsplasty.
Results
Sixty-seven patients were included. The results were 6% poor, 31.3% fair, 44.8% good, and 17.9% excellent according to the Judet Classification. A correlation was observed between age and the gain in range of motion at the 1-year postoperative follow-up, and between the gain in range of motion intraoperatively and that at the 1-year follow-up. There were five cases of complications (7.46%): one of patellar fracture, three of quadriceps tendon rupture, and one of avulsion fracture in the superior pole of the patella.
Conclusion
Quadricepsplasty using the Adolphson–Cerqueira technique produced satisfactory results overall for improving knee joint stiffness and had a complication rate comparable with other currently used techniques.
Clinical significance
Loss of knee range of motion remains a difficult problem without there being a clear gold standard in treatment. Many different options are described in the literature. We provide a further option with follow-up results.
How to cite this article
Cerqueira FS, Silva L, Kropf LL, et al. Minimally Invasive Quadricepsplasty Using the Adolphson–Cerqueira Technique: A Retrospective Study after 1-Year of Follow-up. Strategies Trauma Limb Reconstr 2024;19(2):87–93.
Keywords: Follow-up studies, Knee injuries, Observational studies, Range of motion, Retrospective studies
Introduction
Knee stiffness is difficult to treat. Possible causes range from prolonged immobilisation due to a fracture, after surgical treatment of a fracture of the distal third of the femur, patella, or tibial plateau, or from complications of total knee arthroplasty.1–4 An individual requires 67° of knee flexion to walk; however, a knee range-of-motion of 0°–125° is adequate for nearly all activities of daily living. A loss of 5° of knee extension increases the energy expenditure of the quadriceps muscle during walking, leading to gait alterations.3,5
The options for surgical treatment are many with no gold standard. The first technique used for this problem was proposed by Bennett6 in 1922. However, Thompson7 and Judet8 demonstrated techniques that were more widely used later. In 1964, Nicoll9 described the points of adherence of the structures of the anterior compartment of the knee and thigh, which led to the modification of the classic techniques and the creation of new ones.10,11 More recently, Cerqueira et al. described a minimally invasive surgical technique based on the adhesion points described by Nicoll and colleagues. The developed techniques vary from minimally invasive open surgeries through limited access incisions or arthroscopy, to open surgeries with wide surgical access and extensive dissection of the thigh muscle planes.5,12–14 In all cases, postoperative physiotherapy is important to maintain the range of movement acquired during the surgical procedure and reduce its subsequent loss.14,15
This study aims to present 1-year follow-up results after quadricepsplasty using the Adolphson–Cerqueira technique in a sample of Brazilian patients.
Materials and Methods
Study Design, Setting, and Participants
This was a retrospective case series of patients who underwent quadricepsplasty using the Adolphson–Cerqueira technique between January 2006 and March 2023 by surgeons of Centre for Specialized Care of the Treatment Area of Dysmetry and Deformities of the Locomotor System at the National Institute of Traumatology and Orthopaedics of Rio de Janeiro. An active search for patients was performed using the INTO Hospital Information System database according to the procedure code registered with the Unified Health System.
The inclusion criteria were as follows:
Knee stiffness with a range of motion of less than 70°;
Patellar excursion of 2 mm or more on physical examination;
Available anteroposterior and lateral radiographs of the knee; and
1-year postoperative follow-up.
The exclusion criteria were as follows:
Total joint block to any movement;
Femorotibial or patellofemoral ankylosis observed on knee radiographs;
Lack of data or knee radiographs in medical or radiological records respectively;
Active infection; and
Loss to outpatient follow-up.
Participants were divided into three groups according to the cause of the decrease in knee range of motion. Group A had a postoperative fracture aetiology; group B had a previous surgical procedure of bone lengthening, bone transportation, pelvic support osteotomy or other types of osteotomy to correct deformities in the lower limbs; and group C had either post-vaccination, conservative fracture treatment, or post-skeletal traction aetiologies.
Surgical Technique
Using the Adolphson–Cerqueira technique, the patient was placed in the supine position and a 6 cm incision was made proximal to the superior pole of the patella (see Supplemental video). Five main steps are described. The first step was to isolate the quadriceps tendon, releasing it from the vastus medialis and lateralis and with subsequent release of the adhesions between the quadriceps tendon and the anterior surface of the femur (first extra-articular adhesion point). The second step involved releasing the medial and lateral retinacula of the patella as well as the infrapatellar adhesions (first intra-articular adhesion point). The third step involved separating the quadriceps tendon into two portions: the vastus intermedius and rectus femoris portions. When performing the tenotomy of the vastus intermedius tendon, the rectus femoris tendon was protected using a surgical retractor. The fourth step was performed using long scissors or finger pressure to release adhesions from the subcutaneous cellular tissue (second extra-articular adhesion point). The fifth step involved gentle manipulation of the knee into flexion, requiring two orthopaedic surgeons, one of whom was responsible for maintaining the hip at 90° flexion while the other was responsible for flexing the knee and applying increasing flexion pressure to the patient's leg. If resistance is felt, the previous steps were reviewed. The objective was to achieve knee flexion of between 120° and 130°.
Finally, only the skin was sutured, and a sterile dressing was applied to prevent the knee from flexing during the postoperative period.
Immediate Postoperative Period
A femoral nerve block catheter was placed prior to the patient leaving the operating room for continuous postoperative analgesia. Patients were administered continuous passive motion therapy for at least 24 hours under medical and physiotherapy supervision to maintain the range of motion obtained during the surgical procedure.
After 24–48 hours, the catheter was removed. At this point, all patients in the three groups were encouraged to maintain the range of motion both passively and actively. Follow-up with a physiotherapist was essential. Techniques to gain knee flexion with the patient in prone and sitting positions pulling on the foot, using pain control with electrotherapy devices and regular oral analgesia were essential. The physiotherapy protocol has remained the same since 2006.
Outpatient Follow-up
All the patients had the same protocol after surgery and returned to the outpatient clinic weekly for the first month. At the first appointment, the surgical wound was inspected, active and passive knee flexion was encouraged and the patient was then referred for rehabilitation. In the third week after surgery, the sutures were removed.
At every outpatient visit, patients were encouraged to flex the knee actively and passively and continue physiotherapy. After the first postoperative month, follow-up appointments were scheduled at 3, 6, and 12 months.
Judet Classification
The Judet Classification is a classification system for assessing the outcome of quadricepsplasty. This classification grades the degree of knee flexion achieved as follows: flexion of more than 100° was considered excellent; 81°–100° as good; 50°–80° as fair; and less than 50° as poor.7,16
In our study, this classification is used in the preoperative, immediate postoperative, 6-month and 12-month postoperative periods.
Statistical Analysis
Descriptive and inferential statistical methods were used to analyse the data of 67 patients, divided into three groups: Group A (post-fracture osteosynthesis), group B (post-lengthening, bone transport, pelvic support osteotomy or varus osteotomy) and group C (post-vaccination, conservative treatment, post-skeletal traction). Qualitative variables are presented as absolute and relative frequency distributions. Quantitative variables are presented using measures of central tendency and variation, and normality was assessed using the Shapiro–Wilk test. The following inferential methods were used: (a) the Chi-square test of independence was used to compare the distribution of the qualitative variables; (b) Spearman's correlation was used to assess the correlation between age and the other quantitative variables; and (c) the Kruskal–Wallis test with Dunn's post-test was used to compare the groups with regard to the quantitative variables.
An alpha error of 5% was set for rejection of the null hypothesis, and statistical analysis was conducted using BioEstat Version 5.3 and SPSS Version 27 (IBM Corp., Armonk, NY, USA).
Results
A total of 74 patients who underwent quadricepsplasty procedures using the Adolphson–Cerqueira technique were included; however, seven patients were lost to outpatient follow-up. In the final sample, there was a higher proportion of male (88.1%) than female (11.9%) patients (Flowchart 1).
Flowchart 1.
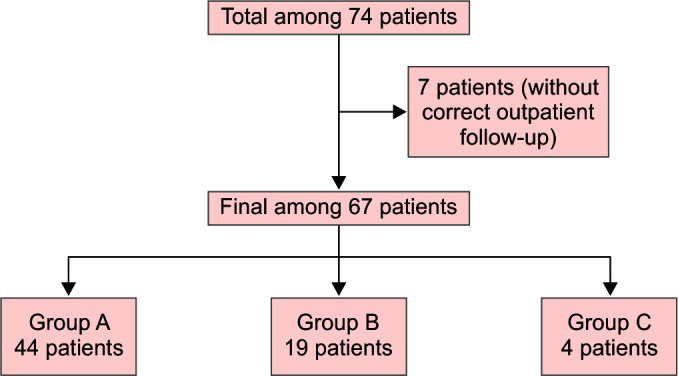
Step by step of groups design
The mean age of the participants was 35.8 years (SD = 11), with a minimum age of 9 years and a maximum age of 68 years. The most frequent age group was 30–39 years (34.3%), and the least frequent was 50 years or older (13.4%). The average duration of knee stiffness was 6.35 years (SD = 6.09), with a minimum of 0.75 years and a maximum of 33 years.
In the analysis of the Judet Classification obtained intraoperatively, at 6 months and at 1-year of follow-up, it was observed that there was a decrease in knee flexion considered to be excellent intraoperatively (68.7%) and at 1-year follow-up when there were 12 cases (17.9%). However, there was an improvement in the percentage of participants with knee flexion classified as good, with nine cases (13.4%) intraoperatively and 30 cases (44.8%) at the 1-year follow-up (Table 1).
Table 1.
Epidemiological data and Judet Classification in the three groups and in the total sample
| Variables | GA | GB | GC | Total sample | p-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| (n = 44) | % | (n = 19) | % | (n = 4) | % | (n = 67) | % | ||
| Sex | 0.7051 | ||||||||
| Male | 39 | 88.6 | 17 | 89.5 | 3 | 75.0 | 59 | 88.1 | |
| Female | 5 | 11.4 | 2 | 10.5 | 1 | 25.0 | 8 | 11.9 | |
| Age (years) | 0.1279 | ||||||||
| 9–29 | 10 | 22.7 | 8 | 42.1 | 3 | 75.0 | 21 | 31.3 | |
| 30–39 | 15 | 34.1 | 7 | 36.8 | 1 | 25.0 | 23 | 34.3 | |
| 40–49 | 10 | 22.7 | 4 | 21.1 | 0 | 0.0 | 14 | 20.9 | |
| ≥ 50 | 9 | 20.5 | 0 | 0.0 | 0 | 0.0 | 9 | 13.4 | |
| Laterality | 0.4020 | ||||||||
| Right | 20 | 45.5 | 11 | 57.9 | 3 | 75.0 | 34 | 50.7 | |
| Left | 24 | 54.5 | 8 | 42.1 | 1 | 25.0 | 33 | 49.3 | |
| Judet classification intraoperative | 0.2495 | ||||||||
| Poor | 0 | 0.0 | 2 | 10.5 | 0 | 0.0 | 2 | 3.0 | |
| Fair | 6 | 13.6 | 4 | 21.1 | 0 | 0.0 | 10 | 14.9 | |
| Good | 7 | 15.9 | 1 | 5.3 | 1 | 25.0 | 9 | 13.4 | |
| Excellent | 31 | 70.5 | 12 | 63.2 | 3 | 75.0 | 46 | 68.7 | |
| Judet classification at 6 months | 0.3317 | ||||||||
| Poor | 3 | 6.8 | 3 | 15.8 | 0 | 0.0 | 6 | 9.0 | |
| Fair | 15 | 34.1 | 7 | 36.8 | 1 | 25.0 | 23 | 34.3 | |
| Good | 18 | 40.9 | 9 | 47.4 | 3 | 75.0 | 30 | 44.8 | |
| Excellent | 8 | 18.2 | 0 | 0.0 | 0 | 0.0 | 8 | 11.9 | |
| Judet classification at 12 months | 0.9703 | ||||||||
| Poor | 2 | 4.5 | 2 | 10.5 | 0 | 0.0 | 4 | 6.0 | |
| Fair | 14 | 31.8 | 6 | 31.6 | 1 | 25.0 | 21 | 31.3 | |
| Good | 20 | 45.5 | 8 | 42.1 | 2 | 50.0 | 30 | 44.8 | |
| Excellent | 8 | 18.2 | 3 | 15.8 | 1 | 25.0 | 12 | 17.9 | |
GA, group A; GB, group B; GC, group C. Chi-square test of independence
The preoperative assessment of the knee range of motion of the total sample revealed a mean of 20.1° (SD = 14.1), with a minimum of 5° and a maximum of 70°. The average preoperative range of motion was greater in group A than in groups B and C. During the surgical procedure, group C showed the greatest gain in range of motion (140°), ranging between 90° and 140°. Group B showed the smallest intraoperative gain in range of motion at 15°. Both groups A and B had cases of range of motion loss at the 6-month follow-up, with losses of 20° and 15°, respectively. At the 1-year follow-up, the maximum range of motion obtained was similar in the three groups (110° in groups A and B and 100° in group C), with the average gain in group B being higher than that in groups A or C (Table 2).
Table 2.
Preoperative angular parameters and evolution of sample groups
| GA | GB | GC | p-value | |
|---|---|---|---|---|
| (n = 44) | (n = 19) | (n = 4) | ||
| ROM preoperative (degrees) | 0.2584 | |||
| Min–Max | 5.0–70.0 | 0.0–40.0 | 10.0–30.0 | |
| Mean–SD | 15.4 ± 21.9 | 10.3 ± 15.2 | 9.5 ± 22.5 | |
| Median (1st IQ–3rd IQ) | 17.5 (10.0–30.0) | 15.0 (7.5–20.0) | 25.0 (17.5–30.0) | |
| ROM intraoperative (degrees) | 0.9386 | |||
| Min–Max | 50.0–130.0 | 15.0 –130.0 | 90.0–140.0 | |
| Mean–SD | 20.8 ± 111.4 | 37.2 ± 98.4 | 22.1 ± 117.5 | |
| Median (1st IQ–3rd IQ) | 120.0 (90.0–130.0) | 120.0 (80.0–122.5) | 120.0 (105.0–132.5) | |
| Gain at 6 months (6 months–preoperative) (degrees) | 0.6470 | |||
| Min–Max | (–20.0)–120 | (–15.0)–100.0 | 60.0–80 | |
| Mean–SD | 24.3 ± 61.9 | 29.4 ± 54.5 | 9.5 ± 67.5 | |
| Median (1st IQ–3rd IQ) | 60.0 (50.0–76.2) | 60.0 (40.0–72.5) | 65.0 (60.0–72.5) | |
| Gain at 12 months (12 months–preoperative) (degrees) | 0.4951 | |||
| Min–Max | 0.0–110.0 | (–15.0)–110.0 | 60.0–100.0 | |
| Mean–SD | 22.4 ± 61.8 | 29.3 ± 58.9 | 19.1 ± 75.0 | |
| Median (1st IQ–3rd IQ) | 60.0 (50.0–76.5) | 60.0 (42.5–80.0) | 70.0 (60.0–85.0) | |
GA, group A; GB, group B; GC, group C; Min, minimum; Max, maximum; ROM, range of motion; SD, standard deviation; 1st IQ, first interquartile range; 3rd IQ, third interquartile range. Kruskal–Wallis test
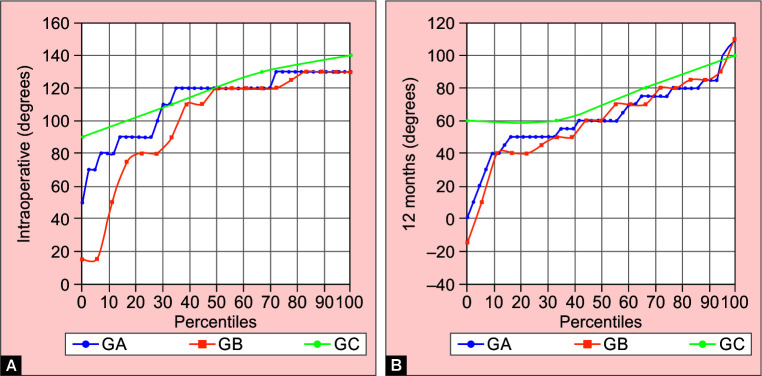
Intraoperatively, although group C comprised only four participants, this group gained more knee range of motion than groups A and B did. This was also the case at the 1-year postoperative follow-up (Fig. 1A). Group B showed the greatest variation in maximum range of motion gain both intraoperatively and at the 1-year postoperative follow-up (Fig. 1B).
Figs 1A and B.
Distribution of participants by group. (A) Intraoperative moment; (B) With 12 months of follow-up
GA, group A; GB, group B; GC, group C
When assessing the correlation between the patients' age and the gain in knee range of motion at the different time points, a weak correlation was observed only at the 1-year follow-up (r = −0.2457, p = 0.049) (Fig. 2).
Fig. 2.
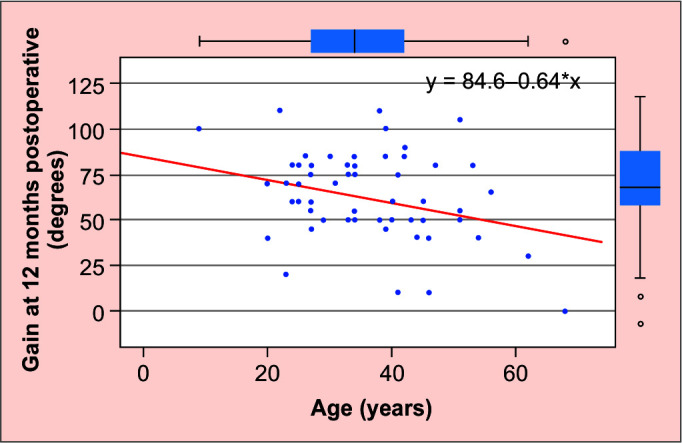
Relationship between the gain of the range of motion with one year of follow-up and the age of the participant
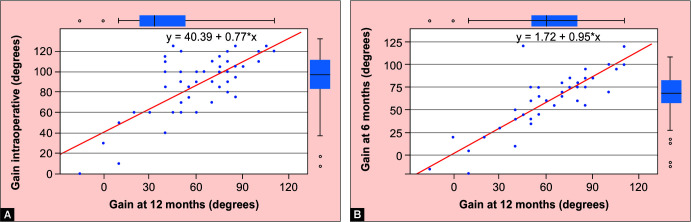
A strong correlation was found between the gain in range of motion intraoperatively and that at the 1-year follow-up (r = 0.561, p < 0.01) (Fig. 3A), as well as between the gain in range of motion at the 6-month and 1-year follow-up (r = 0.879, p < 0.01) (Fig. 3B).
Figs 3A and B.
Relationship between the gain of the range of motion. (A) Intraoperative and 12 months of follow-up; (B) 6 months and 12 months of follow-up
However, a moderate correlation was found between the intraoperative and 6-month follow-up gain in range of motion (r = 0.484, p < 0.01) (Fig. 4).
Fig. 4.
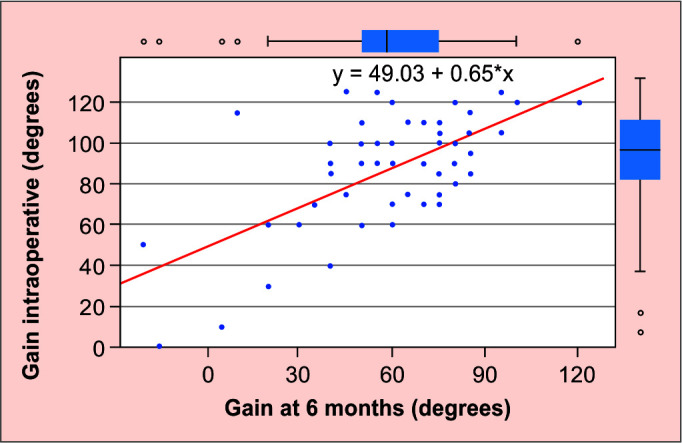
Relationship between the gain of the range of motion intraoperative and 6 months follow-up
In this study, complications were observed in five cases (7.46%). Among them, intraoperatively and during the knee manipulation, there was one case of patellar fracture requiring osteosynthesis at the same time, which led to a Judet Classification grade of fair at the 1-year follow-up; three cases of rupture of the quadriceps tendon requiring primary suture, resulting in a Judet Classification grade at the 1-year follow-up of poor in two cases and fair in one case; and one case of avulsion fracture of the superior pole of the patella requiring primary suture, leading to a Judet Classification grade of poor at the 1-year follow-up. In one case graded as poor at follow-up, we recorded there was a lack of adherence to the postoperative protocol.
Discussion
The technique used in this study is proposed for treating knee stiffness and is based on anatomical principles and knowledge of pathoanatomy. Complications which occurred were solved intraoperatively and did not require returns to the operating room. There have been no prior studies reporting quadricepsplasty on this sample size and with 1-year outcomes.
There is, as yet, no gold standard for the treatment of knee stiffness. Since the 2000s, the techniques described have used smaller surgical incisions or arthroscopic portals to release the adherence points described by Nicoll.9 The so-called classic techniques, in particular those of Judet and Thompson, involve extensive surgical incisions and are associated with significant morbidity, extension lag in 10–66.7% of cases and problems with wound healing.13 Not only is the surgical procedure labour-intensive, but the patient's recovery from physiotherapy can be painful and prolonged.12
The proposed technique is based on minimal access and knowledge of the location of the adhesion points. Blanco et al.12 performed arthroscopic release of both intra- and extra-articular adhesions in a case series of 26 patients. The protocol included ultrasonography to diagnose adhesion of the quadriceps muscle to the anterior surface of the femur and surgery scheduled only after attempted rehabilitation for 3 months had not increased knee flexion. Having access to a professional specialised in musculoskeletal ultrasonography is the first factor hindering this method from having widespread adoption. The duration of joint stiffness and restriction of knee range of motion in the preoperative period of the cases in the sample were not described. Complications occurred in 38% of patients, with five cases of haemarthrosis, including two of scrotal oedema, two of reflex sympathetic dystrophy and one of deep vein thrombosis, despite the procedure being performed arthroscopically. There was a gain in knee range of motion of more than 90° in eight patients, between 70° and 89° in nine patients, between 50° and 69° in seven patients and between 20° and 49° in two patients.12
The established techniques started the release of the stiff knee using wide incisions, but other authors have modified these aiming at lowering complication rates. Hussein et al.17 made a similar incision using the Thompson technique, approximately 15 cm from the patella to the tibial tuberosity, without resecting the vastus intermedius or resuturing the rectus femoris muscle to the vastus medialis and lateralis muscles. The observed gain in range of motion was between 95° and 110°, with two excellent and one good functional outcome according to the Judet Classification. However, the complications included the need to manipulate the knee in two cases and a decrease in the strength of the quadriceps muscle in two cases (grade 4 strength).17
In their case series of 40 patients, Hahn et al.18 performed quadricepsplasty using the modified Thompson technique at an average of 40.3 months from trauma to surgery. The gain in range of motion ranged from 5° to 110°, with excellent functional results in 30 cases, good results in 7 cases and fair results in 3 cases. Complications occurred in 12.5% of the total sample, with one case each of deep infection, patellar tendon rupture, avulsion of the anterior tibial tuberosity, patellar fracture and patellar instability.18
Other authors, as well as Adolphson and Cerqueira, have attempted to solve these cases with techniques other than those previously established. Shen et al.13 performed patellar traction by using the modified Judet technique to reduce knee stiffness. The study started with 29 patients but 8 were lost, 6 due to complications and 2 due to loss to follow-up, resulting in a sample of 21 patients. The complications observed (21.42% of the total sample) included one case of ischaemia and necrosis of the suprapatellar skin, one case of patellar fracture due to traction, three cases of intolerable pain even with the use of analgesic medication and one case requiring a repeat patellar traction procedure. The gain in range of motion observed in the sample was between 40° and 100°. The functional outcome according to the Judet Classification of the patients who remained in the study was excellent in 14 cases, good in 6 cases and fair in 1 case. However, in three cases (14% of those who remained in the study), extension lag was observed at the end of treatment.13
The duration of joint stiffness can generate structural changes in muscle-tendon structures which, in the long term, alters the tendon's ability to stretch as well as its resistance. During knee manipulation, there is a risk of injury to the knee extensor mechanism with rupture of the quadriceps and patellar tendons and patellar fracture.19,20 Saini and Trikha cite in their study the failure of 9 patients out of 48 who underwent manipulation, with a maximum of 272 days from fracture to manipulation, with 2 cases of tibial tuberosity avulsion, 3 patella fracture, 1 patellar tendon avulsion, 1 quadriceps tear and 2 skin breakdown.20–22
There were limitations in our study. The final sample was noted to have certain characteristics—there were intervals of 0.75–33 years before surgery—which can lead to further structural changes of the tendon. Seven patients did not undergo outpatient follow-up as required by the protocol and others due to missing data in their medical records, thereby reducing the final sample size. Another limitation was the difficulty in providing physiotherapy through Brazil's Unified Health System for all the patients, which may have led to an increase in the loss of knee flexion and, consequently, a worsening of the Judet Classification of the final outcomes. A direct comparison with other techniques is not possible because of the different types of techniques used and variations in the size of incisions, as well as the lack of uniformity in the postoperative rehabilitation protocol.
Conclusion
Quadricepsplasty using the Adolphson–Cerqueira technique showed satisfactory results for improving knee joint stiffness. These were comparable to the results in the current literature. Furthermore, the complication rate is no different from that described for other currently used techniques.
Ethical Considerations
This study was approved by the Research Ethics Committee (Comitê de Ética em Pesquisa – CEP) of National Institute of Traumatology and Orthopedics of Rio de Janeiro under the Ethical Approval Certificate (Certificado de Apresentação de Apreciação Ética – CAAE) opinion 67137023.1.0000.5273 of March 2023.
Supplementary Material
The supplementary video are available online on the website of www.stlrjournal.com
Supplementary video: Animation of techinic
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Pujol N, Boisrenoult P, Beaufils P. Post-traumatic knee stiffness: Surgical techniques. Orthop Traumatol Surg Res. 2015;101(1):S179–186. doi: 10.1016/j.otsr.2014.06.026. [DOI] [PubMed] [Google Scholar]
- 2.Vaish A, Vaishya R, Bhasin VB. Etiopathology and management of stiff knees: A current concept review. Indian J Orthop. 2020;55(2):276–284. doi: 10.1007/s43465-020-00287-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reahl GB, Marinos D, O–Hara NN, et al. Risk factors for knee stiffness surgery after tibial plateau fracture fixation. J Orthop Trauma. 2018;32(9):e339–343. doi: 10.1097/BOT.0000000000001237. [DOI] [PubMed] [Google Scholar]
- 4.Alıcı T, Buluç L, Tosun B, et al. Modified Judet's quadricepsplasty for loss of knee flexion. Knee. 2006;13(4):280–283. doi: 10.1016/j.knee.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 5.Ding BTK, Khan SA. The Judet quadricepsplasty for elderly traumatic knee extension contracture: A case report and review of the literature. Biomedicine (Taipei) 2019;9(3):21. doi: 10.1051/bmdcn/2019090321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bennett GE. Lengthening of the quadriceps tendon. J Bone Joint Surg. 1922;4:279–316. [Google Scholar]
- 7.Thompson T. Quadricepsplasty to improve knee function. J Bone Joint Surg. 1944;26:366–379. [Google Scholar]
- 8.Judet R. Mobilization of the stiff knee. J Bone Joint Surg Br. 1959;41:856–857. [Google Scholar]
- 9.Nicoll EA. Quadricepsplasty: The treatment of stiff knee following trauma. Postgrad Med J. 1964;40(467):521–526. doi: 10.1136/pgmj.40.467.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daoud H, O'Farrell T, Cruess RL. Quadricepsplasty. The Judet technique and results of six cases. J Bone Joint Surg Br. 1982;64(2):194–197. doi: 10.1302/0301-620X.64B2.7068739. [DOI] [PubMed] [Google Scholar]
- 11.Thompson TC. Quadricepsplasty. Ann Surg. 1945;121(5):751–754. doi: 10.1097/00000658-194505000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blanco CE, Leon HO, Guthrie TB. Endoscopic quadricepsplasty: A new surgical technique. Arthroscopy. 2001;17(5):504–509. doi: 10.1053/jars.2001.24062. [DOI] [PubMed] [Google Scholar]
- 13.Shen Z, Deng Y, Peng A, et al. Modified Judet's quadricepsplasty plus patellar traction for knee stiffness after femoral fracture surgery. Int Orthop. 2021;45(5):1137–1145. doi: 10.1007/s00264-020-04823-3. [DOI] [PubMed] [Google Scholar]
- 14.Dos Santos Cerqueira F, T Araújo Motta GA, Rocha de Faria JL, et al. Minimally invasive quadricepsplasty. Arthrosc Tech. 2019;8(3):e343–347. doi: 10.1016/j.eats.2018.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khakharia S, Fragomen AT, Rozbruch SR. Limited quadricepsplasty for contracture during femoral lengthening. Clin Orthop Relat Res. 2009;467(11):2911–2917. doi: 10.1007/s11999-009-0951-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kundu Z, Sangwan S, Guliani G, et al. Thompson's quadricepsplasty for stiff knee. Indian J Orthop. 2007;41(4):390–394. doi: 10.4103/0019-5413.37004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hussein R, Miles J, Garlick N, et al. A conservative approach to quadricepsplasty – Description of a modified surgical technique and a report of three cases. J Knee Surg. 2008;21:39–42. doi: 10.1055/s-0030-1247790. [DOI] [PubMed] [Google Scholar]
- 18.Hahn SB, Choi YR, Kang HJ, et al. Prognostic factors and long-term outcomes following a modified Thompson's quadricepsplasty for severely stiff knees. J Bone Joint Surg Br. 2010;92(2):217–221. doi: 10.1302/0301-620X.92B2.22936. [DOI] [PubMed] [Google Scholar]
- 19.Mittal R, Digge V, Jain S. Judet's quadricepsplasty technique offers excellent functional outcome without an extension lag for extension contracture of the knee: A retrospective cohort of 33 patients. Indian J Orthop. 2022;56(11):1913–1917. doi: 10.1007/s43465-022-00696-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bidolegui F, Pereira SP, Pires RE. Safety and efficacy of the modified Judet quadricepsplasty in patients with post-traumatic knee stiffness. Eur J Orthop Surg Traumatol. 2021;31(3):549–555. doi: 10.1007/s00590-020-02802-3. [DOI] [PubMed] [Google Scholar]
- 21.Lee D, Stinner D, Mir H. Quadriceps and patellar tendon ruptures. J Knee Surg. 2013;26(5):301–308. doi: 10.1055/s-0033-1353989. [DOI] [PubMed] [Google Scholar]
- 22.Saini P, Trikha V. Manipulation under anesthesia for post traumatic stiff knee-pearls, pitfalls and risk factors for failure. Injury. 2016;47(10):2315–2319. doi: 10.1016/j.injury.2016.07.012. [DOI] [PubMed] [Google Scholar]