Abstract
Opioid overdose is a leading cause of death in the United States, and engaging with patients following overdose to provide harm reduction and recovery resources can prove difficult. Quick response models use mobile, multidisciplinary teams to establish a time-sensitive connection between individuals who overdosed and harm reduction and recovery resources that improve outcomes. These quick response models are consistent with the broader field of mobile-integrated health programs that are growing in number and acceptability, though the literature base is sparse and programs vary. We describe the 5-year reach, effectiveness, adoption, implementation and maintenance (RE-AIM) framework of the Rapid Response Emergency Addiction and Crisis Team (RREACT), a fire/emergency medical services-led, multidisciplinary (firefighter/paramedic, law enforcement officer, social worker) mobile outreach team. RREACT provides harm reduction, linkage/transportation to care and wrap-around services to individuals following a nonfatal opioid overdose that resulted in an emergency response in Columbus, Franklin County, Ohio, United States. Between 2018 and 2022, RREACT made 22,157 outreach attempts to 11,739 unique patients. RREACT recorded 3,194 direct patient contacts during this time, resulting in 1,200 linkages to care: 799 direct transports to opioid use disorder treatment and 401 warm handoffs to community treatment agencies. Furthermore, RREACT’s staffing increased from 4 full-time equivalent staff in 2018 to 15.5 in 2022 and was supported by the surrounding community through 287 community outreach events and the development of an alumni program. These preliminary results further support the deployment of multidisciplinary mobile outreach teams to increase access to harm reduction and recovery resources following opioid overdose.
Keywords: Opioid-related disorders, quick response team, harm reduction, mobile integrated healthcare, multidisciplinary care team
INTRODUCTION
Accidental opioid overdose resulted in over 200,000 emergency medical responses in the United States in 2022, a rate that has doubled over the past 4 years (Casillas et al., 2022). Approximately 1 in 12 individuals who survive an accidental opioid overdose are expected to die annually, resulting in over 100,000 preventable deaths each year (Centers for Disease Control and Prevention, National Center for Health Statistics, 2021; Florence et al., 2021; King et al., 2021; Stoove et al., 2009). The best chance at long-term survival for individuals with opioid use disorder (OUD) includes a combination of harm-reduction techniques, cognitive-behavioural approaches and medication-assisted treatment (Hawk et al., 2015; National Institute on Drug Abuse, 2018; Schuckit, 2016; Sharma et al., 2017). However, contacting individuals at places and moments in time when they are accepting of these interventions can be difficult and is often compounded by personal, financial and logistic barriers to treatment (Powell et al., 2019; Wollschlaeger et al., 2017).
While many individuals living with OUD can connect to recovery resources through medical facilities (e.g., emergency department (ED), outpatient clinics), approximately 60–80% of overdoses responded to by emergency medical services (EMSs) are transported to an ED (Bergstein et al., 2021; The Office of National Drug Control Policy, 2024). Concerningly, the mortality rate for individuals refusing EMS transportation following an overdose is up to 66% higher than that of those who accepted transportation to a healthcare facility (Zozula et al., 2022). First responders (firefighters, EMS providers, law enforcement (LE) officers) may represent an under-utilized resource for connecting high-risk patients to OUD treatment, as they are oftentimes the only providers who have contact with individuals following an overdose, particularly when patients decline transportation to an ED or live in an “opioid treatment desert” (Allen et al., 2021; Cao et al., 2019; Centers for Disease Control and Prevention National Center for Injury Prevention and Control, 2021; Hyder et al., 2021). Thus, programs that leverage first responders’ access to patients to provide harm reduction and connection to recovery resources may increase the chances of long-term recovery after an overdose (Diriba & Whitlock, 2022; Langabeer et al., 2020; Wagner et al., 2019; Xuan et al., 2023). Preliminary reports suggest that mobile multidisciplinary teams are effective in providing proactive outreach and harm reduction to these patients; however, little is known about program design and outcomes (Bagley et al., 2019; Langabeer et al., 2020; Xuan et al., 2023).
The purpose of this program evaluation is to describe a fire/EMS-led post-overdose multidisciplinary mobile outreach program (Rapid Response Emergency Addiction and Crisis Team (RREACT)), its implementation and program outcomes over a 5-year period.
METHODS
Study Design
This retrospective evaluation of the RREACT program using a deidentified dataset was determined to be exempt from review by The Ohio State University Institutional Review Board (#2023E0544).
Setting
The state of Ohio is widely considered an epicentre of the opioid crisis (Lyle Cooper et al., 2020; MacKinnon & Privitera, 2020). Franklin County, the most-populated county and home to the state capital of Columbus, reported a three-fold increase in opioid-related deaths per capita between 2007 and 2017 (16.3–44.1 per 100,000) (Columbus and Franklin County Addiction Plan, 2023). Furthermore, Ohio has one of the nation’s worst overdose deaths-to-available treatment facility ratios, with an average of one program for every 8.5 deaths (Langabeer et al., 2019).
Program Description
In response to the opioid epidemic and the need for community-based treatment resources for individuals with OUD, the City of Columbus Department of Public Safety developed RREACT – a multidisciplinary mobile outreach program spearheaded by fire/EMS, crisis-trained LE officers and behavioural health/social work. RREACT was established in May 2017 following a 6-month City of Columbus grant-funded pilot and is housed within the Columbus Division of Fire (CFD), which employs dual-trained firefighter-EMS clinicians. Using post-overdose outreach protocols, RREACT reduces barriers to OUD treatment through direct linkage and/or transportation to treatment, harm reduction and case management. RREACT staff receive additional training about the science, nature and course of addiction, and trauma-informed care which are refreshed on a regular basis. Best practices for providing EMS care in the context of opioid and drug-related events follow those suggested by Keseg et al. (2019).
An interdisciplinary data management system housed within CFD allows for patient identification using the following criteria: fire/EMS or LE reports a suspected opioid overdose or evidence of naloxone administration. Fire/EMS personnel review the run report to manually confirm suspicion of an overdose and eliminate lower-risk encounters (e.g., naloxone administered to an unresponsive person who had a medical emergency not caused by an opioid overdose). The Columbus Division of Police (CPD) then reviews the patients’ addresses for safety concerns and the likelihood of patient contact at this address. Once verified, the case is assigned for outreach, and a RREACT firefighter, plain-clothes LE officer and social worker visit the address. Team members wear a RREACT uniform and travel in a vehicle marked with the RREACT logo. The branding is intended to increase trust in the community and the likelihood that individuals will open their doors to RREACT. If the individual who experienced an overdose is present and willing to speak to the team, RREACT offers the following services: (1) access to behavioural health treatment (including direct transportation or warm handoff); (2) resources and support to stabilize households, including basic needs, kinship supports and counselling; (3) education and training on trauma, substance use disorders, the administration and handling of naloxone (including leave-behind naloxone); and (4) case management and patient advocacy for patients, whether or not they immediately choose to enter treatment. If the individual who experienced an overdose is not present, team members leave RREACT contact information at the address they visited. Outreach occurs Monday to Friday, 9 am to 5 pm with variable evening and weekend coverage. The structure and activities of RREACT are summarized in Figure 1.
FIGURE 1.
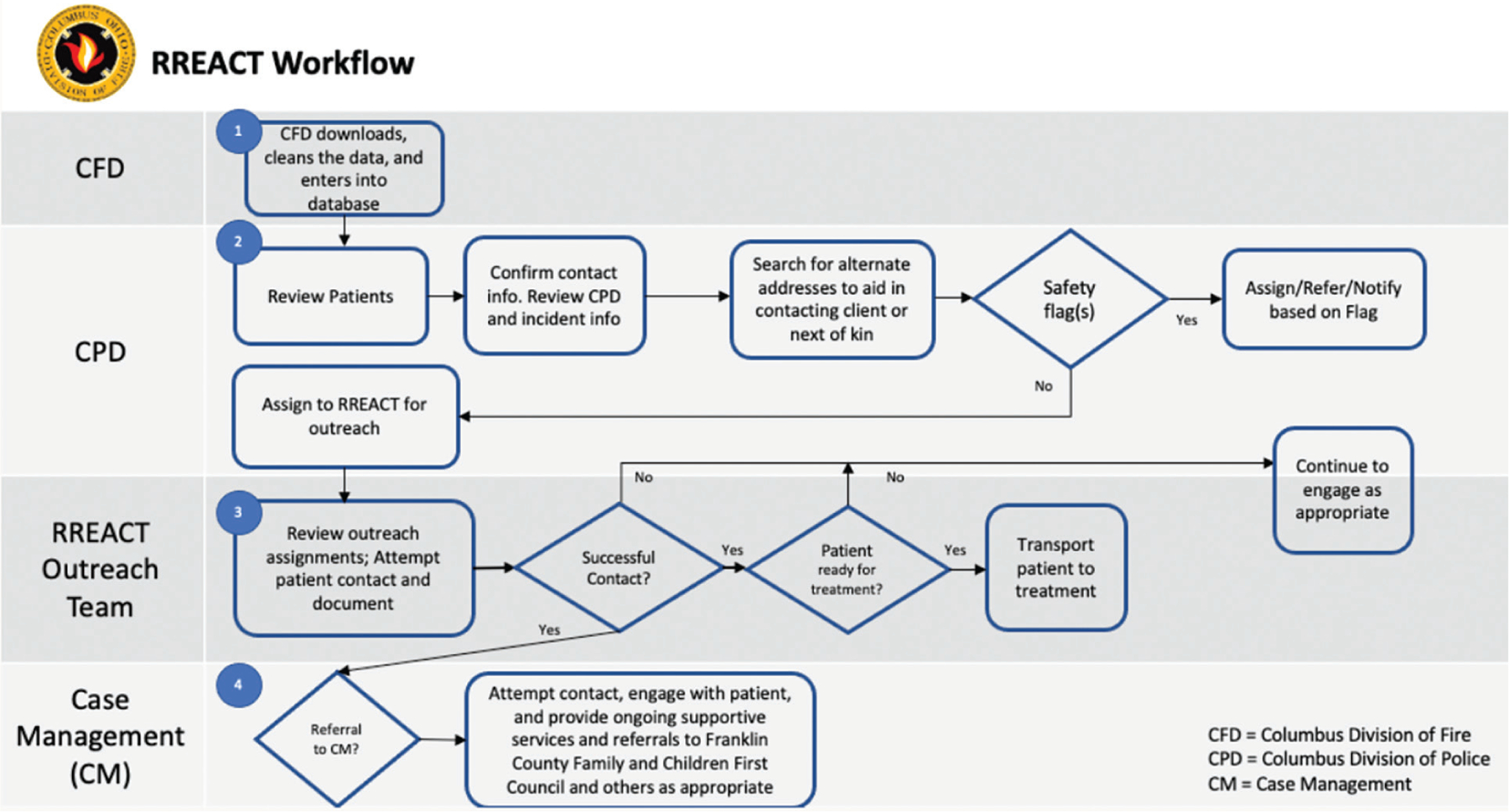
Swimlane diagram summarizing individual roles in the overall program process
Data Source and Patient Identification
At the program’s inception, programmatic data were documented on paper and in Microsoft Excel; thus, some data metrics for 2018–2019 were not available for analysis. Since 2020, RREACT has utilized a unique case record database that imports data from CPD’s documentation and CFD’s electronic health record, including dispatch information, EMS response and RREACT outreach data (EMS & Fire Software, 2023). For this program evaluation, we utilized a convenience sample of patients who refused transport to the ED following overdose (as this represents a high-risk population who may not have accessed resources otherwise) with whom RREACT attempted outreach between 2018 and 2022. Additionally, we analyzed RREACT’s community outreach events and case management databases.
Outcomes
The primary outcome was program growth, defined as both patient contacts and number of full-time RREACT staff over a 5-year period. Secondary outcomes included the remaining elements of the RE-AIM framework (Glasgow et al., 1999), including reach (outreach attempts), effectiveness (number of patients who were directly transported to treatment or received a warm handoff to a community resource), adoption (increase in full-time equivalent (FTE) support), implementation (programmatic changes and use of resources) and maintenance (community adoption and external funding support).
Analysis
We conducted a descriptive data analysis by year to assess RREACT’s growth, reach, effectiveness, adoption and maintenance. Data were categorized as program outreach, program outcomes and patient demographics.
RESULTS
Reach
The program’s reach increased annually: from 2018 to 2022, there was an eight-fold increase in the annual number of outreach attempts (n = 661 in 2018 to n = 6,196 in 2022) and a four-fold increase in the number of unique patients receiving an outreach attempt (n = 520 in 2018 to n = 2,963 in 2022). We also observed an increase in the number of patients who RREACT made direct contact with (i.e., spoke directly with the patient in person or by phone rather than to a friend or family member) between 2018 (n = 208) and 2022 (n = 868). Further, RREACT’s social worker actively engaged 125–127 patients in case management services each year from 2020 to 2022 (Table I). Data from 2020 to 2022 show that participants were predominantly male (61%), 25–34 years of age (34%), and either White (64%) or Black/African American (28%) (Table II).
TABLE I.
RREACT program characteristics and outcomes 2018–2022
| Descriptive Characteristics and Outcomes | 2018 |
2019 |
2020 |
2021 |
2022 |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| Full-time staff members | 4 | 12.5 | 14 | 14.5 | 15.5 |
| Fire | 2 | 3.5 | 3.5 | 3.5 | 5.5 |
| Police | 1 | 5 | 5 | 5 | 5 |
| Social work/behavioural health | 1 | 2 | 2 | 2 | 2 |
| Other (program manager, liaison, data analyst) | 0 | 2 | 3.5 | 4 | 3 |
| Community outreach events | * | * | * | 142 | 145 |
| Community outreach event attendees | 2,890 | 2,775 | |||
| Outreach contact attempts | 661 | 1,830 | 5,145 | 8,325 | 6,196 |
| Unique patients for attempted outreach | 520 | 1,362 | 3,256 | 3,638 | 2,963 |
| Case management patients | * | * | 127 | 125 | 150 |
| Outcomes of outreach contact attempts | |||||
| No contact and unknown | 235 (36%) | 418 (23%) | 329 (6%) | 442 (5%) | 454 (7%) |
| Left message/contact information | 223 (34%) | 783 (43%) | 4,168 (81%) | 7,037 (85%) | 4874 (79%) |
| Direct contact with patient | 203 (31%) | 629 (34%) | 648 (13%) | 846 (10%) | 868 (14%) |
| Linkages/referrals to treatment | 21 (3%) | 72 (4%) | 34 (1%) | 148 (2%) | 126 (2%) |
| Direct transports to treatment | 35 (5%) | 140 (8%) | 164 (3%) | 204 (3%) | 256 (4%) |
Notes:
Data not available.
TABLE II.
RREACT patient demographics, 2018–2022
| Demographic Variables | 2018 |
2019 |
2020 |
2021 |
2022 |
|---|---|---|---|---|---|
|
n = 520 |
n = 1,362 |
n = 3,256 |
n = 3,638 |
n = 2,963 |
|
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| Age (mean years) | * | * | 39 | 39 | 39 |
| <18 | * | * | 19 (1%) | 17 (0%) | 15 (0%) |
| 18–24 | * | * | 248 (8%) | 293 (8%) | 242 (8%) |
| 25–34 | * | * | 1151 (35%) | 1214 (33%) | 988 (33%) |
| 35–44 | * | * | 912 (28%) | 999 (27%) | 831 (28%) |
| 45–54 | * | * | 492 (15%) | 592 (16%) | 458 (15%) |
| 55–64 | * | * | 317 (10%) | 385 (11%) | 298 (10%) |
| 65–74 | * | * | 75 (2%) | 106 (3%) | 104 (4%) |
| 75 and older | * | * | 15 (0%) | 11 (0%) | 9 (0%) |
| Unknown | * | * | 27 (1%) | 21 (1%) | 18 (1%) |
| Gender | |||||
| Male | * | * | 1978 (61%) | 2229 (61%) | 1794 (61%) |
| Female | * | * | 1259 (39%) | 1362 (37%) | 1154 (39%) |
| Unknown | * | * | 19 (0%) | 47 (1%) | 15 (0%) |
| Race/ethnicity | |||||
| American Indian or Alaskan Native | * | * | 1 (0%) | 1 (0%) | 1 (0%) |
| Asian | * | * | 6 (0%) | 15 (0%) | 24 (1%) |
| Black/African American | * | * | 868 (28%) | 959 (25%) | 954 (32%) |
| Hispanic or Latino | * | * | 46 (1%) | 74 (2%) | 89 (3%) |
| Native Hawaiian or Other Pacific Islander | * | * | 4 (0%) | 6 (0%) | 9 (0%) |
| White | * | * | 2,229 (68%) | 2,226 (62%) | 1798 (61%) |
| Other | * | * | 4 (1%) | 60 (2%) | 23 (1%) |
| Unknown | * | * | 98 (3%) | 297 (8%) | 65 (2%) |
Notes:
Data not available.
Effectiveness
The number of direct transports to treatment facilities (n = 799) and warm handoffs to community-based care (n = 401) via RREACT increased annually (from 56 in 2018 to 382 in 2022) (Table I). Notably, transport to treatment was more common than a warm handoff to community-based resources after interacting with RREACT. In 2018, 17% of patients who had direct contact with RREACT accepted transportation to OUD treatment; in 2022, that proportion increased to 29%.
Adoption
RREACT began in 2017 with one CFD program supervisor and one firefighter to review nonfatal overdose cases and attempt outreach to the patient alongside a community behavioural health social worker. Program adoption increased yearly as grant funding increased. In 2018, RREACT expanded outreach hours and increased its number of firefighters/paramedics and CPD officers, though additional needs were met using overtime. In 2019, RREACT added a project director, supervisors, a grants manager and additional CPD officers, and its first behavioural health specialist. In 2020, a social worker, behavioural health specialist liaison and data analyst were hired. By the end of 2022, RREACT had 15.5 FTE including five and a half firefighters/EMS, five LE officers, two social workers and three individuals serving in the roles of data analyst, grant manager/program director and behavioural health liaison (Table I).
Implementation, Maintenance and Sustainability
Beginning in 2020, adaptations to the COVID-19 pandemic allowed for program continuation despite new and rapidly changing barriers to contacting patients and connecting patients to care. For example, the location of outreach interventions changed from in-home to the patient’s front door (wearing standard EMS personal protective equipment and social distancing), telephone encounters increased and naloxone distribution occurred in high-need areas. We did not observe a significant decrease in patient participation during this time, supporting consistent implementation despite a change in how participants interacted with the program. RREACT became more sustainable as additional grant funding allowed for expansion outside of Columbus and into all of Franklin County. RREACT also proactively uses data for quality improvement efforts.
Maintenance of RREACT has been supported by its community outreach events and the use of wristbands and business cards with RREACT’s contact information, both of which have enhanced visibility. Through these 287 community events over 2 years, RREACT connected with over 5,000 individuals, made them aware of RREACT’s services and provided harm reduction training and naloxone distribution. Additionally, RREACT established partnerships with numerous community organizations, including refugee and immigrant groups, community businesses, social service agencies and behavioural health treatment facilities, health departments and faith-based communities. Further, in partnership with RREACT patients in long-term recovery, the RREACT alumni group was formed. Alumni share RREACT’s story and plan monthly recovery-focused events, increasing RREACT’s recognition in the community and providing peer support to patients starting their recovery. These events are funded through donations and individual contributions from RREACT team members.
DISCUSSION
Over a 5-year period, RREACT – a Fire/EMS-led multidisciplinary mobile outreach program following a nonfatal opioid overdose – grew in staff, referrals, successful contacts and linkages to treatment. Program reach increased annually and demonstrated increased capacity to adjust to the ongoing opioid epidemic. RREACT contacted higher numbers of patients and transported increasing proportions to treatment annually. Adoption was noted by increased first-responder staffing. Implementation was challenged by the COVID-19 pandemic, but sustained patient engagement supported effective implementation. Program sustainability was noted through progressive integration with city and county resources along with the development of an alumni group.
The program structure had important similarities and differences to other post-overdose models of care, such as the sequential intercept model, diversion programs, quick response team (QRT) or community paramedicine/mobile integrated healthcare approaches. First, RREACT’s opt-out structure yielded a higher referral rate (near 100%, due to automated referrals) compared to the 66% referral rate of the opt-in structure used in Tacoma Fire’s CARES program, but an overall lower contact rate due to this larger referral denominator (Bagley et al., 2019; Scott et al., 2020). The ideal patient contact strategy (opt-in versus opt-out) remains unclear and should continue to be investigated in future work. Second, as RREACT evolved, it concentrated on its firefighter/paramedic–LE officer–social worker triad and later expanded to include case management and additional support services for families, similar to Massachusetts’ PORT and CO-OP programs (Bagley et al., 2019; Formica et al., 2018). Third, though RREACT did not include peer support professionals during initial outreach, as was done by QRTs in North Carolina, the RREACT alumni group in some ways serves a similar function (Bagley et al., 2019). Finally, one area that RREACT did not document formally exploring was community health workers and/or registered nurses, as was done in West Virginia and Washington state QRT pilot programs (Bagley et al., 2019), though RREACT did have a registered nurse on its team in the role of behavioural health liaison.
RREACT’s multidisciplinary mobile outreach program’s contact rate of 89% was higher than the 53–58% reported by similarly structured QRTs in Ohio and Massachusetts, but the direct contact rate was lower (Formica et al., 2022; Manchak et al., 2022). One plausible explanation is that the study population analyzed here (post-overdose but not transported to an ED) is different from the study population of similarly structured programs (e.g., self-referral, community referral, court referral, hospital referral) but may have been more likely to accept outreach. Though our findings in this high-risk cohort are important, they do make direct comparisons to other programs more difficult, and future work should investigate how unique program aspects, including the patient population and team composition, impact patient engagement.
The demographic description of individuals engaged by RREACT was similar to the population of individuals in Franklin County, OH, who overdosed on opioids during the same time period (56% male, 57% White), though RREACT’s population was slightly older (25–34 years old versus 18–24 years old) (Columbus and Franklin County Addiction Plan, 2023). RREACT’s demographic data also mirror those from a 2019 statewide description of 25 similar post-overdose programs in Ohio, suggesting that the target population reached is similar despite using slightly different program structures (Firesheets et al., 2022).
The number of RREACT outreach contacts exceeded the number of unique individuals seen by RREACT, suggesting that some individuals required repeated contact. This emphasizes the need for multiple outreach attempts, similar to findings reported by Langabeer et al. (2020) demonstrating that 86% of participants in Houston Fire’s HEROES program declined treatment at least once prior to enrolment. Notably, as RREACT expanded its FTE, this allowed for increased outreach efforts, the introduction of community events and broader community advocacy and training efforts.
One unique aspect of RREACT was the role of LE officers. Prior studies of LE-led diversion programs (e.g., DART, Massachusetts; Hope Not Handcuffs, Michigan; Plymouth County Outreach, Massachusetts) demonstrate the ability to disengage individuals who used opiates from the legal system and engage them in the community-based recovery (Bagley et al., 2019; Cruz, 2017; Schiff et al., 2017; White et al., 2021). Other programs have leveraged fire/EMS-based resources to identify and reach out to at-risk individuals (Langabeer et al., 2021; Mechem et al., 2020). The RREACT approach leveraged elements of each of these models by using a unified referral database to synergize LE and fire/EMS calls into a single referral pool for outreach (similar to Houston Fire HEROES) and leveraged LE in scene safety and patient identification roles. Notably, RREACT’s success would likely not have been possible without intentional efforts to secure multisector collaboration and community trust; without these elements, individuals in need may be less likely to seek and receive care and resources from first responders (Zakrison et al., 2004). These findings, collectively, support the role of multidisciplinary teams and interagency collaboration in identifying at-risk individuals and connecting them to treatment, though future research may consider identifying ways to optimize each agency’s role (Yatsco et al., 2020).
RREACT’s multidisciplinary mobile outreach was also unique and differed slightly from the more episodic QRT model. Many QRTs prioritize the “quick” aspect and either allow the patient to reach out directly or attempt to make contact within 2–7 days of overdose and may provide services for up to 90 days (Bagley et al., 2019; Sacco et al., 2018). RREACT’s design included intentional longitudinal follow-up and unlimited contact as needed by the patient, a unique aspect not reported elsewhere. Additionally, while the role of peer support is established in other community-based post-overdose interventions (e.g., North Carolina’s Rapid Response Teams and Delaware), the evolution of an alumni group to support ongoing recovery was a distinctive finding, and its presence ties the episodic public safety intervention to a more sustainable, long-term recovery response.
Limitations
First, this study is limited by its use of a programmatic database that transitioned during the observation period, resulting in missing data from the first 2 years of implementation. To reduce this limitation, we worked directly with the program and database vendor to ensure the most accurate data were used. Second, selection bias was present in our inclusion of a subset of high-risk patients, making it difficult to compare results to the more robust literature based on patients from multiple referral sources. Third, our study design does not allow us to draw conclusions between the program and rates of opioid deaths in the target population; however, to provide additional context, we have provided county-level incidence of fatal opioid overdose prior to RREACT’s inception (2017) through the last available year of data (2022) in Figure 2 using data from the Columbus and Franklin County Addiction Plan. Finally, there is an absence of universal taxonomy in the literature about how to refer to post-overdose response programs (e.g., sequential intercept, QRT, diversion, community paramedicine, mobile integrated healthcare) and we may have unintentionally excluded reference to similar programs in our discussion.
FIGURE 2.
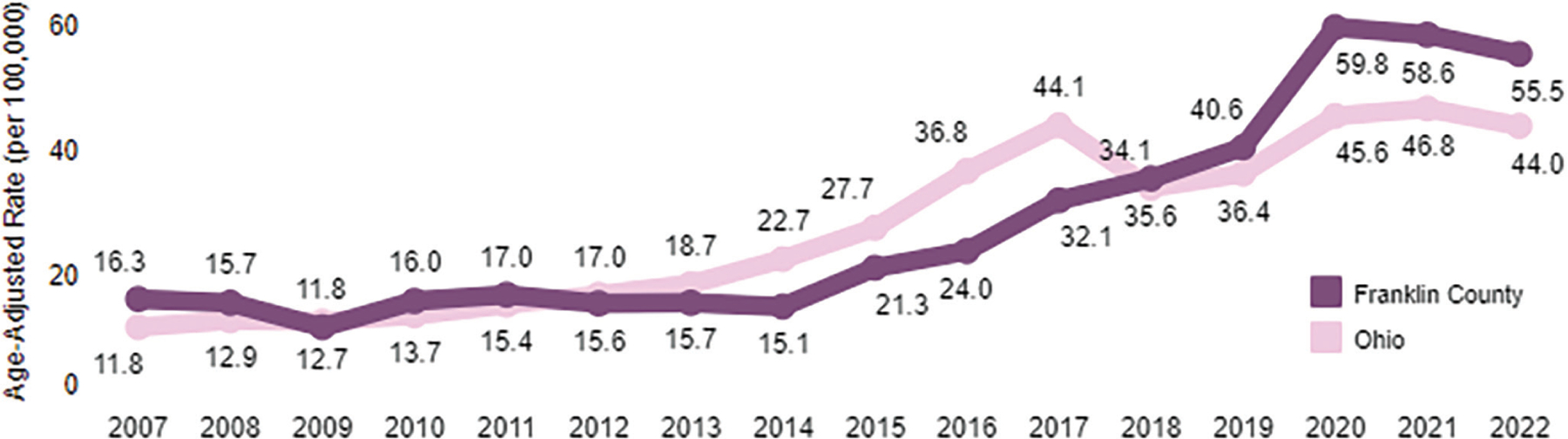
Rate of Franklin County resident deaths by year, 2007–2022. Data and figure are courtesy of Columbus and Franklin County Addiction Plan, 2023
CONCLUSIONS
This retrospective evaluation of a multidisciplinary mobile outreach program following a nonfatal opioid overdose demonstrated effective linkage to treatment and sustained growth over a 5-year observation period. The collaboration of fire/EMS, LE, and social work demonstrates one potential community-based model for linking patients to OUD treatment.
ACKNOWLEDGEMENTS
The authors thank Krescens Kok and Jin Lin for their support of this research.
Footnotes
CONFLICT OF INTEREST DISCLOSURE
Mighty Crow Media, LLC, employs an author of this article and serves as the grant evaluator for RREACT’s Bureau of Justice Assistance COSSAP grant. Grant funding does not support time or other costs associated with this publication. Alexander Ulintz was supported by AHRQ T32 grant (T32 HS029590).
REFERENCES
- Allen ST, Wedlock PT, Hamilton White R, Schneider KE, O’Rourke A, Ahmad NJ, Weir BW, Milkenny ME, & Sherman SG (2021). Engagement in drug treatment following nonfatal overdose among people who inject drugs in Appalachia. International Journal of Drug Policy, 93, 103176. 10.1016/j.drugpo.2021.103176 [DOI] [PubMed] [Google Scholar]
- Bagley SM, Schoenberger SF, Waye KM, & Walley AY (2019). A scoping review of post opioid-overdose interventions. Preventive Medicine, 128, 105813. 10.1016/j.ypmed.2019.105813 [DOI] [PubMed] [Google Scholar]
- Bergstein RS, King K, Melendez-Torres GJ, & Latimore AD (2021). Refusal to accept emergency medical transport following opioid overdose, and conditions that may promote connections to care. International Journal of Drug Policy, 97, 103296. 10.1016/j.drugpo.2021.103296 [DOI] [PubMed] [Google Scholar]
- Cao Y, Stewart K, Wish E, Artigiani E, & Sorg MH (2019). Determining spatial access to opioid use disorder treatment and emergency medical services in New Hampshire. Journal of Substance Abuse Treatment, 101, 55–66. 10.1016/j.jsat.2019.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casillas S, Pickens C, Stokes E, Walters J, & Vivolo-Kantor A (2022). Patient-level and county-level trends in nonfatal opioid-involved overdose emergency medical services encounters — 491 counties, United States, January 2018–March 2022. Morbidity and Mortality Weekly Report, 71, 1073–1080. 10.15585/mmwr.mm7134a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, National Center for Health Statistics. (2021). National vital statistics system, mortality 2018–2021 on CDC WONDER online database. https://wonder.cdc.gov/ucd-icd10-expanded.html [PubMed]
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. (2021). Partnerships between public health and public safety. Retrieved June 27, 2021, from https://www.cdc.gov/drugoverdose/strategies/public-safety.html
- Columbus and Franklin County Addiction Plan. (2023). Franklin County, Ohio addiction-related data. Columbus public health. Retrieved January 17, 2024, from https://public.tableau.com/app/profile/columbus/viz/CFCAP/MainMenu_1
- Cruz TJ (2017). “Door-to-Door Opioid Outreach in Plymouth County.” Prosecutor. Journal of the National District Attorneys Association, 49(4), 34–35. [Google Scholar]
- Diriba K, & Whitlock E (2022). Deflection to harm reduction: Public health and public safety collaborative responses to the overdose epidemic in the United States. Journal of Public Health Management and Practice, 28(3), 321–323. 10.1097/PHH.0000000000001531 [DOI] [PubMed] [Google Scholar]
- EMS & Fire Software. (2023). Emergency networking. Retrieved September 11, 2023, from https://www.emergencynetworking.com/
- Firesheets K, Juarez S, Kopak A, Ross J, Sperber K, & Reichert J (2022). Naloxone plus, plus some: Examining Ohio’s quick response teams through the lens of deflection. Journal of Public Health Management and Practice, 28(Suppl 6), S330–S338. 10.1097/PHH.0000000000001570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Florence C, Luo F, & Rice K (2021). The economic burden of opioid use disorder and fatal opioid overdose in the United States, 2017. Drug and Alcohol Dependence, 218, 108350. 10.1016/j.drugalcdep.2020.108350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Formica SW, Apsler R, Wilkins L, Ruiz S, Reilly B, & Walley AY (2018). Post opioid overdose outreach by public health and public safety agencies: Exploration of emerging programs in Massachusetts. International Journal of Drug Policy, 54, 43–50. 10.1016/j.drugpo.2018.01.001 [DOI] [PubMed] [Google Scholar]
- Formica SW, Reilly B, Duska M, Ruiz SC, Lagasse P, Wheeler M, Delaney A, & Walley AY (2022). The Massachusetts Department of Public Health Post Overdose Support Team Initiative: A public health-centered co-response model for post-overdose outreach. Journal of Public Health Management and Practice, 28(Suppl 6), S311–S319. 10.1097/PHH.0000000000001574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Vogt TM, & Boles SM (1999). Evaluating the public health impact of health promotion interventions: The RE-AIM framework. American Journal of Public Health, 89(9), 1322–1327. 10.2105/ajph.89.9.1322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawk KF, Vaca FE, & D’Onofrio G (2015). Reducing fatal opioid overdose: Prevention, treatment and harm reduction strategies. Yale Journal of Biology and Medicine, 88(3), 235–245. [PMC free article] [PubMed] [Google Scholar]
- Hyder A, Lee J, Dundon A, Southerland LT, All D, Hammond G, & Miller HJ (2021). Opioid treatment deserts: Concept development and application in a US Midwestern urban county. PLoS One, 16(5), e0250324. 10.1371/journal.pone.0250324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keseg DP, Augustine JJ, Fowler RL, Scheppke KA, Farcy DA, Pepe PE, & members of the Primary Writing Group for the Metropolitan Municipalities Emergency Medical Services Medical Directors, C. (2019). Annotated guidance and recommendations for the role and actions of emergency medical services systems in the current opioid and drug-related epidemics. The Journal of Emergency Medicine, 57(2), 187–194 e181. 10.1016/j.jemermed.2019.04.017 [DOI] [PubMed] [Google Scholar]
- King C, Cook R, Korthuis PT, Morris C, & Englander H (2021). Causes of death in the 12 months after hospital discharge among patients with opioid use disorder. Journal of Addiction Medicine, 16, 466–469. 10.1097/ADM.0000000000000915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langabeer JR, Gourishankar A, Chambers KA, Giri S, Madu R, & Champagne-Langabeer T (2019). Disparities between US opioid overdose deaths and treatment capacity: A geospatial and descriptive analysis. Journal of Addiction Medicine, 13(6), 476–482. 10.1097/ADM.0000000000000523 [DOI] [PubMed] [Google Scholar]
- Langabeer J, Champagne-Langabeer T, Luber SD, Prater SJ, Stotts A, Kirages K, Yatsco A, & Chambers KA (2020). Outreach to people who survive opioid overdose: Linkage and retention in treatment. Journal of Substance Abuse Treatment, 111, 11–15. 10.1016/j.jsat.2019.12.008 [DOI] [PubMed] [Google Scholar]
- Langabeer JR, Persse D, Yatsco A, O’Neal MM, & Champagne-Langabeer T (2021). A framework for EMS outreach for drug overdose survivors: A case report of the houston emergency opioid engagement system. Prehospital Emergency Care, 25(3), 441–448. 10.1080/10903127.2020.1755755 [DOI] [PubMed] [Google Scholar]
- Lyle Cooper R, Thompson J, Edgerton R, Watson J, MacMaster SA, Kalliny M, Huffman MM, Juarez P, Mathews-Juarez P, Tabatabai M, & Singh KP (2020). Modeling dynamics of fatal opioid overdose by state and across time. Preventive Medicine Reports, 20, 101184. 10.1016/j.pmedr.2020.101184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon NJ, & Privitera E (2020). Addressing the opioid crisis through an interdisciplinary task force in Cincinnati, Ohio, USA. Pharmacy (Basel, Switzerland), 8(3), 116. 10.3390/pharmacy8030116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manchak SM, Gosney ME, Haberman C, & Firesheets KC (2022). A data-driven response to the addiction crisis in Hamilton County, Ohio. Journal of Public Health Management and Practice, 28(Suppl 6), S320–S325. 10.1097/PHH.0000000000001566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mechem CC, Yates CA, Rush MS, Alleyne A, Singleton HJ, & Boyle TL (2020). Deployment of alternative response units in a high-volume, urban EMS system. Prehospital Emergency Care, 24(3), 378–384. 10.1080/10903127.2019.1657212 [DOI] [PubMed] [Google Scholar]
- National Institue on Drug Abuse. (2018). Principles of drug addiction treatment: A research-based guide (3rd ed.). https://archives.nida.nih.gov/sites/default/files/podat-3rdEd-508.pdf [Google Scholar]
- Powell KG, Treitler P, Peterson NA, Borys S, & Hallcom D (2019). Promoting opioid overdose prevention and recovery: An exploratory study of an innovative intervention model to address opioid abuse. International Journal of Drug Policy, 64, 21–29. 10.1016/j.drugpo.2018.12.004 [DOI] [PubMed] [Google Scholar]
- Sacco P, Unick GJ, & Gray C (2018). Enhancing treatment access through “Safe Stations”. Journal of Social Work Practice in the Addictions, 4(18), 458–464. 10.1080/1533256X.2018.1517007 [DOI] [Google Scholar]
- Schiff DM, Drainoni ML, Weinstein ZM, Chan L, Bair-Merritt M, & Rosenbloom D (2017). A police-led addiction treatment referral program in Gloucester, MA: Implementation and participants’ experiences. Journal of Substance Abuse Treatment, 82, 41–47. 10.1016/j.jsat.2017.09.003 [DOI] [PubMed] [Google Scholar]
- Schuckit MA (2016). Treatment of opioid-use disorders. The New England Journal of Medicine, 375(4), 357–368. 10.1056/NEJMc1610830 [DOI] [PubMed] [Google Scholar]
- Scott CK, Dennis ML, Grella CE, Nicholson L, Sumpter J, Kurz R, & Funk R (2020). Findings from the recovery initiation and management after overdose (RIMO) pilot study experiment. Journal of Substance Abuse Treatment, 108, 65–74. 10.1016/j.jsat.2019.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma A, Kelly SM, Mitchell SG, Gryczynski J, O’Grady KE, & Schwartz RP (2017). Update on barriers to pharmacotherapy for opioid use disorders. Current Psychiatry Reports, 19(6), 35. 10.1007/s11920-017-0783-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoove MA, Dietze PM, & Jolley D (2009). Overdose deaths following previous non-fatal heroin overdose: Record linkage of ambulance attendance and death registry data. Drug and Alcohol Review, 28(4), 347–352. 10.1111/j.1465-3362.2009.00057.x [DOI] [PubMed] [Google Scholar]
- The Office of National Drug Control Policy. (2024). Nonfatal drug overdose surveillance dashboard. National EMS Information System. https://nemsis.org/nonfatal-drug-overdose-surveillance-dashboard/ [Google Scholar]
- Wagner KD, Harding RW, Kelley R, Labus B, Verdugo SR, Copulsky E, Bowles JM, Mittal ML, & Davidson PJ (2019). Post-overdose interventions triggered by calling 911: Centering the perspectives of people who use drugs (PWUDs). PLoS One, 14(10), e0223823. 10.1371/journal.pone.0223823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White MD, Perrone D, Watts S, & Malm A (2021). Moving beyond Narcan: A police, social service, and researcher collaborative response to the opioid crisis. American Journal of Criminal Justice, 46(4), 626–643. 10.1007/s12103-021-09625-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wollschlaeger BA, Willson TM, Montejano LB, Ronquest NA, & Nadipelli VR (2017). Characteristics and treatment patterns of US commercially insured and Medicaid patients with opioid dependence or abuse. Journal of Opioid Management, 13(4), 207–220. 10.5055/jom.2017.0389 [DOI] [PubMed] [Google Scholar]
- Xuan Z, Yan S, Formica SW, Green TC, Beletsky L, Rosenbloom D, Bagley SM, Kimmel SD, Carroll JJ, Lambert AM, & Walley AY (2023). Association of implementation of postoverdose outreach programs with subsequent opioid overdose deaths among Massachusetts Municipalities. JAMA Psychiatry, 80(5), 468–477. 10.1001/jamapsychiatry.2023.0109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yatsco AJ, Champagne-Langabeer T, Holder TF, Stotts AL, & Langabeer JR (2020). Developing interagency collaboration to address the opioid epidemic: A scoping review of joint criminal justice and healthcare initiatives. International Journal of Drug Policy, 83, 102849. 10.1016/j.drugpo.2020.102849 [DOI] [PubMed] [Google Scholar]
- Zakrison TL, Hamel PA, & Hwang SW (2004). Homeless people’s trust and interactions with police and paramedics. Journal of Urban Health, 81(4), 596–605. 10.1093/jurban/jth143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zozula A, Neth MR, Hogan AN, Stolz U, & McMullan J (2022). Non-transport after Prehospital Naloxone Administration is associated with higher risk of subsequent non-fatal overdose. Prehospital Emergency Care, 26(2), 272–279. 10.1080/10903127.2021.1884324 [DOI] [PubMed] [Google Scholar]


