Abstract
Background
Health issues caused and/or exacerbated by work are common in patients seeking primary health care. Yet, primary care providers generally receive little or no training in the assessment and management of occupational injuries and illnesses.
Aims
To conduct a pilot project to develop, implement and evaluate a programme to teach occupational and environmental medicine to primary healthcare providers.
Methods
We followed the Extensions for Community Healthcare Outcomes (ECHO) model to connect primary healthcare providers with experts in Occupational and Environmental Medicine (OEM). We employed an observational pre–post study design to assess changes in self-efficacy, knowledge, attitudes and beliefs towards OEM.
Results
From September 2021 to June 2022, we offered two cycles of 12 sessions each. Participants came from medicine, nursing, psychology, occupational and physical therapy, chiropractic, kinesiology, social work, and pharmacy. Sixty-seven participants completed both pre- and post-ECHO questionnaires. Self-efficacy and knowledge ratings significantly increased after attendance at ECHO compared to the pre-ECHO responses. Attitudes and beliefs were unchanged in most of the items assessed. Participants rated their satisfaction with ECHO between 59% and 97%.
Conclusions
Our pilot study demonstrated the challenges in implementing the first ECHO OEM in Canada. Findings show acceptability and satisfaction, improved self-efficacy, and small increases in knowledge, but not overall attitudes and beliefs. There is a need to understand barriers to participation and to target participants with less knowledge and experience in occupational and environmental medicine.
Primary care providers receive little training in occupational and environmental medicine. We developed and evaluated an innovative virtual programme to teach occupational and environmental medicine to primary care providers in Ontario. Participants came from medicine, nursing, psychology, occupational and physical therapy, chiropractic, kinesiology, social work, and pharmacy. Sixty-seven participants completed both pre- and post-questionnaires. There was high acceptability and satisfaction, with gains in self-efficacy and, to a lesser extent, knowledge after the programme.
Introduction
Patients presenting with occupational health issues are common in primary care [1–3]. Healthcare providers (HCPs) must be able to take an effective occupational history to determine if an exposure in the workplace (chemical, biological, physical, ergonomic or psychological) is causing or aggravating a patient’s disease or injury [4]. HCPs must also be able to advise patients with disabling health conditions, who want to return to or remain at work, about appropriate workplace adjustments that may overcome obstacles to work arising from ill health.
Despite the need for HCPs to have knowledge of occupational health, HCPs receive limited training in occupational and environmental medicine in undergraduate and graduate programmes, and there is also a paucity of continuing education opportunities for HCPs in this area [5–7]. HCP confidence in assessing and facilitating return-to-work (RTW) for their patients is particularly important. A cross-sectional study conducted in Ontario demonstrated that HCPs are key players in the RTW process [8]. In general, positive and encouraging messages from physicians, and provision of a date when a patient can expect to RTW, are associated with better RTW outcomes. Patients who receive information about injury prevention, pain management and work accommodation are also more likely to RTW [9,10]. A need for interdisciplinary working is recognized to achieve optimal outcomes [11], and evidence indicates interprofessional teams achieve better vocational outcomes for chronic pain [12], mental illness [13] and severe trauma such as burns [14]. To fulfil their role in supporting the occupational health of patients, HCPs need to develop skills and learn about resources that enable them to work collaboratively. It is important to ensure the teaching of HCPs does not unduly increase demands on those who are already overburdened by increasing caseloads and demands on their time, especially in rural, remote and underserved areas.
Project ECHO (Extensions for Community Healthcare Outcomes) connects HCPs in primary care with experts using weekly videoconference sessions to discuss cases and deliver didactic presentations. Project ECHO was developed in 2003 for the treatment of individuals with Hepatitis C at the University of New Mexico (https://hsc.unm.edu/echo/) [15] and has expanded beyond healthcare outcomes in the USA (e.g. climate change, education and policing) and to other health conditions [16,17]). ECHO combines several medical education methods to enhance practice in primary care. There are four pillars of ECHO to break down the walls between specialists and primary HCPs through regular videoconferencing sessions connecting rural and remote HCPs, where de-identified patient cases are presented to an academic expert interprofessional team who then provide guidance to enable the HCPs to treat their own patients: To provide a channel where specialist mentors can share best practices with primary HCPs, reducing variation in care to improve health outcomes; to use a case-based learning process, similar to the supervised apprenticeship characteristics of medical training, as opposed to a purely didactic approach; and to use continuous outcome monitoring for quality improvement and programme evaluation.
In 2020, our team was funded by the Ontario Workplace Safety and Insurance Board (WSIB) for a 2-year pilot study. The WSIB is the provincial worker’s compensation agency providing wage-loss benefits, medical coverage and support to help people RTW after a work-related injury or illness. The goal of the ECHO OEM is to increase capacity among HCPs in primary care to manage cases related to occupational and environmental medicine. The aim of this pilot project was to successfully develop, implement and evaluate this ECHO OEM.
Methods
We followed the recommendations of the ECHO Institute in New Mexico [15] and the ECHO Ontario Superhub [18] for ECHO implementation and evaluation.
We employed an observational pre–post study design to assess changes in self-efficacy and knowledge about OEM topics, as well as attitudes and beliefs related to WSIB interactions among participants who attended ECHO OEM. The study was approved by the Research Ethics Board at the University of Toronto (Protocol 40747).
Participating HCPs were recruited from September 2021 to November 2021 for cycle 1 and from April 2022 to June 2022 for cycle 2. Eligibility for this study included any HCP working in primary care in Ontario in a regulated profession (physicians, physician assistants, nurse practitioners, registered nurses, pharmacists, psychologists, social workers, chiropractors, registered massage therapists, and physical and occupational therapists), working in any type of practice (solo or team practice), and having the ability to present at least one case in English. We also included any professional with a role in occupational health and safety, and students in healthcare programmes in Ontario.
We offered two cycles of 12 sessions each, the first in the Fall of 2021 and the second in the Spring of 2022. The topics were the same for both cycles. The topics and presenters’ areas of expertise for cycle 2 are shown in Table 1. One slight modification was made to cycle 2 based on feedback received in cycle 1, that is, we invited a person with live experience of chronic pain and workplace injury to co-present in one session with the expert hub member.
Table 1.
The didactic curriculum of ECHO OEM cycle 2 and presenters’ areas of expertise
| Topic and learning objectives | Presenters’ area of expertise | |
|---|---|---|
| 1 | Overview of occupational and environmental medicine Learn about the roles and functions of an occupational physician and occupational health teams, the common categories of occupational medical conditions and the relationship between the occupational and environmental aspects of OEM |
Occupational Medicine |
| 2 | Engaging with the WSIB/insurance systems 1 Learn what the WSIB is and how it functions, the role of healthcare providers in the workers’ compensation system, and how to effectively complete Form 8s for your patients |
Occupational Medicine, WSIB Chief Medical Officer |
| 3 | Diagnosis and management of work-related injuries and illnesses Learn how to define occupational illness and injury, how to evaluate a patient for a suspected occupational or environmental illness or injury, and outline a return-to-work plan |
Occupational Medicine |
| 4 | Return to work and disability management Learn about the role of allied health practitioners in return to work and disability management, key principles for successful return to work and identifying resources for suitable workplace accommodations |
Occupational Therapy |
| 5 | Mental health and work 1 Learn how employers and healthcare providers can work collaboratively to support and facilitate return to work in an individual with a mental health condition, the organizational factors required to provide a healthy work environment, and how stigma impacts the ability to obtain appropriate healthcare services |
Occupational Health Nursing |
| 6 | Mental health and work 2 Learn the difference between mental stress and illness, presentations and impact of mental illness in the workplace, and how to develop an approach to case management of mental health claims |
Psychiatry |
| 7 | Recognizing occupational and environmental hazards Learn common types of occupational hazards, questions that can help you understand a worker’s occupational exposures and exposure limits that may apply to an individual worker’s job |
Occupational Hygiene |
| 8 | Assessment of fitness for work Learn about the concept of ‘workability’, how to apply functional principles to facilitate ‘workability’, the types of barriers to return to work and the physician’s role in helping to overcome them |
Occupational Medicine |
| 9 | Engaging with the WSIB/insurance systems 2 Learn about healthcare programmes offered by the WSIB and how the return-to-work services work, how primary care providers are integrated into the continuum of care in WSIB programmes, and how to interact with WSIB programmes |
Occupational Medicine, WSIB Chief Medical Officer |
| 10 | Musculoskeletal conditions and chronic pain among working patients Learn about an approach to examining a person with a musculoskeletal condition, treatments for low back pain and indications of opioids for nociceptive, neuropathic and nociplastic chronic pain |
1. Physical medicine and rehabilitation, pain medicine 2. Person with lived experience of chronic pain and workplace injury |
| 11 | Engaging with relevant workplace parties Learn when, why and how physicians should engage with workplace parties |
Occupational Medicine |
| 12 | Ethics and legal issues in occupational medicine Learn about the inherent conflicts related to work and health that may arise for healthcare providers, the role that healthcare providers play in helping their clients/patients navigate systems related to work and health, and some of the system supports that exist to aid both workers and healthcare providers involved in their care |
Occupational Medicine |
The ECHO sessions were held once a week for 12 consecutive weeks and of 90-minute duration. Each included introductions and announcements (5 minutes), didactic with questions and answers (35 minutes), and case presentation and discussion (50 minutes). Sessions were held using Zoom software and moderated by a hub member. Case presenters submitted their de-identified patient cases using a case presentation form before the sessions.
We limited the cases to working-age individuals who had a health condition caused or exacerbated by work or where the health condition was impacting RTW or stay-at-work independent of the cause of the health condition. We excluded cases where the patient did not reside in Ontario.
Data were collected using online questionnaires in Qualtrics. Pre-ECHO questionnaires were administered after registration in the ECHO programme, but prior to commencement of the cycle. Post-ECHO questionnaires were administered at the end of each cycle. Participants who attended both cycles were assessed before cycle 1 and after cycle 2.
Participant demographics and practice characteristics were measured using eight items in the pre-ECHO questionnaire only. Information included age, gender, years in practice, primary profession, country where professional training was completed, number of patients in practice, number of sick notes written per month for patients off work, and estimated number of patients seen per month with injuries or illnesses caused by or worsened by work.
Attendance and participation data were collected at every session and included individual attendance and presentation of cases.
Acceptability and satisfaction with ECHO were measured using 11 items, post-ECHO only. Participants indicated their level of agreement with statements adapted from ECHO Institute in New Mexico to measure the satisfaction and impact of ECHO OEM. Statements were rated using a 6-point Likert scale from 1 (strongly disagree) to 5 (strongly agree), with 6 representing ‘not applicable’ (Appendix 1, available as Supplementary data at Occupational Medicine Online) [4].
Self-efficacy was measured pre- and post-ECHO using a 21-item scale adapted from the ECHO Institute in New Mexico [19]. Participants indicated their level of agreement with statements about their skills, knowledge or competence in the 12 ECHO OEM curriculum topics. Statements began with the phrase, ‘I am confident in my ability to ...’ (e.g. I am confident in my ability to make modified work recommendations for my patients). Items were assessed on a 6-point Likert scale from 1 (strongly disagree) to 5 (strongly agree), with 6 representing ‘not applicable’ (Appendix 2, available as Supplementary data at Occupational Medicine Online).
Knowledge was assessed pre- and post-ECHO using 23 items developed by the ECHO OEM expert hub members. Knowledge test questions included statements related to the information covered in the 12 curriculum didactics. Some questions were also adapted from Braeckman et al. [20]. The response options for the first 10 of 23 questions were ‘true’ or ‘false’ (e.g. An activity limitation describes the difficulties a worker may have in executing the job tasks‘). The last 13 knowledge questions included multiple choice response options (‘a’, ‘b’, ‘c’ or ‘d’; e.g. ‘Which of the following questions is most likely to provide the best information about a worker’s exposure to workplace hazards?’. A score was assigned for correct answers only. Total knowledge scores could range from 0 to 23 (Appendix 3, available as Supplementary data at Occupational Medicine Online).
Attitudes and beliefs related to the WSIB and the management of conditions that affect a patient’s ability to RTW was measured using a 10-item scale adapted from other Project ECHO hubs [21,22]. However, one item was dropped from analysis (‘I believe that multiple chemical sensitivity is a valid diagnosis to obtain compensation benefits’) as this topic was not discussed either in the didactic or case presentations of any ECHO session. Participants reported attitudes and beliefs using a 5-point Likert scale from 1 ‘strongly disagree’ to 5 ‘strongly agree’ (e.g. I believe that most workers’ compensation recipients fake their injuries because they want to get paid not to work”).
Data were analysed using parametric and non-parametric statistics. We only included participants who completed both pre- and post-ECHO evaluations. Self-efficacy and knowledge tests were aggregated as scores for each participant.
The knowledge test was analysed in two subgroups participants with some expertise (‘informed participants’) and participants without expertise in OEM. Repeated-measures analysis of variance (ANOVA) was performed to assess differences in knowledge before and after ECHO participation within and between informed and non-informed groups.
Results
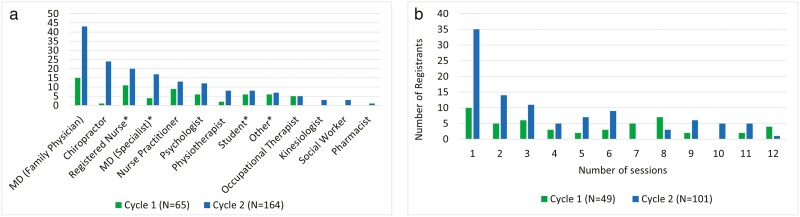
In total, 229 participants registered for the programme: 65 for cycle 1 and 164 for cycle 2 (Figure 1a). Seventy-nine registrants never attended any sessions: 16 in cycle 1 and 63 in cycle 2. Of the remaining 150 people who attended at least one session, more than 50% attended six or fewer sessions (Figure 1b). A total of 124 people completed at least one of the questionnaires (pre- or post-ECHO). Of these, 67 completed both pre- and post-ECHO questionnaires. The subsample of the 67 people with complete data was similar, in demographics and practice characteristics, to the total sample of 124 participants who completed at least one questionnaire (data available in Appendix 4, available as Supplementary data at Occupational Medicine Online). Although the target audience of ECHO programmes are non-experts, some registrants had experience in occupational health, such as non-academic occupational physicians and occupational therapists who work full time with injured workers.
Figure 1.
(a) Registrants’ professions. (b) Number of sessions attended.
There were 25 cases presented over the course of the two cycles: 13 cases in cycle 1 and 12 in cycle 2. The types of cases presented included musculoskeletal injuries (6), post-traumatic stress disorders (4), chemical exposures (2), concussions (2), mental health conditions (2), caregiver strain (2), pain (2), non-adherence to treatment (2), occupational dust exposure risk (1), low visual acuity (1) and pregnancy (1).
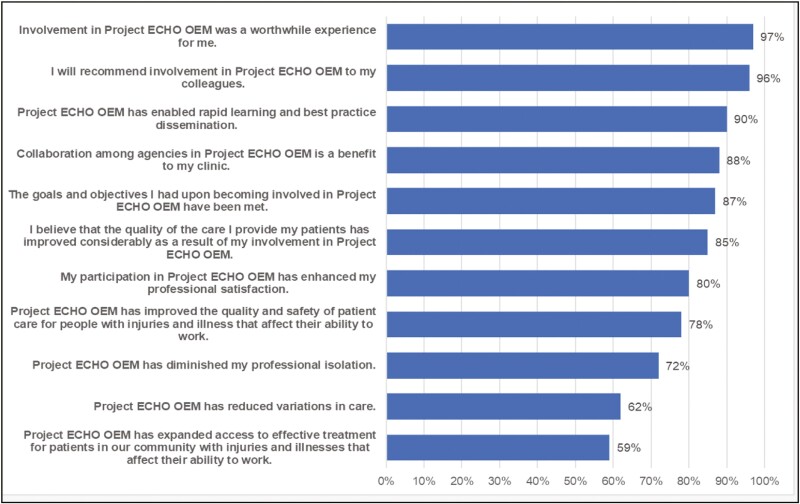
Respondents reported high levels of acceptability and satisfaction with ECHO OEM on 11 measures post-ECHO (Figure 2). Measures relating to acceptability and personal satisfaction (worthwhile experience, learning, benefit to patient care and professional satisfaction) were rated highest (≥80%), and questions related to general care considerations in the community (access, variations in care) were rated lower (59–78%).
Figure 2.
Percentage of participants who selected agree/strongly agree on the 11-item Acceptability and Satisfaction with ECHO OEM scale (n = 67).
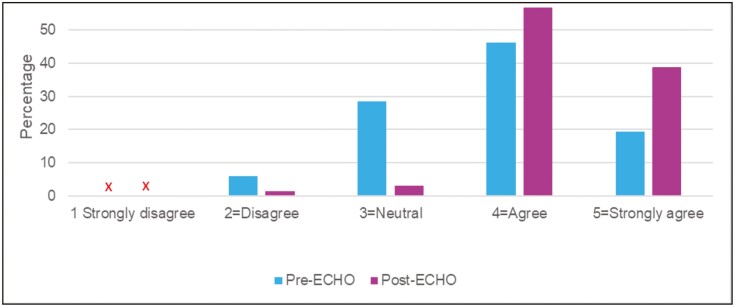
Self-efficacy significantly increased in the post-ECHO compared to pre-ECHO, F(1, 64) = 64.11, P < 0.001 (Figure 3). There was no difference in the average self-efficacy score between informed and non-informed participants, F(1, 64) = 3.03, Pnon-significant.
Figure 3.
Percentage distribution of median pre-ECHO and post-ECHO self-efficacy scores across 21 items for subgroup of participants (n = 67).
Knowledge was assessed in the subgroup of non-informed participants (n = 48) and in the informed subgroup (n = 18) (Table 2). On average, there was no difference in knowledge scores between informed and non-informed, F(1, 64) = 8.9, Pnon-significant. The within-subject main effect test was significant (F(1, 64) = 8.9, P < 0.01); therefore, we can conclude that the knowledge score increased significantly after ECHO. Since the interaction term of informed participant by time was not significant (F(1, 64) = 1.36, Pnon-significant), there was no significant difference in knowledge change between informed and non-informed (Table 2).
Table 2.
Knowledge test scores pre-ECHO and post-ECHO
| ECHO participant’s background related to occupational and environmental medicine | n | Knowledge test | |
|---|---|---|---|
| Pre-ECHO mean (SD) | Post-ECHO mean (SD) | ||
| Informed participant | 18 | 16.0 (2.0) | 17.3 (2.2) |
| Non-informed participant | 48 | 15.8 (3.0) | 16.4 (2.5) |
| Missing information | 1 | 16.0 | 15.0 |
| Whole sample | 67 | 15.9 (2.7) | 16.6 (2.5) |
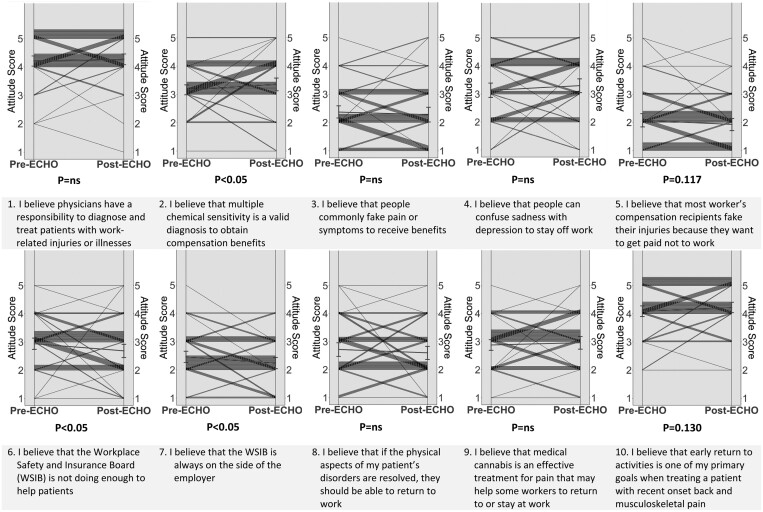
Figure 4 presents individual pre- and post-test responses to the 10 items assessing attitudes and beliefs. Of the 10 items assessed before and after ECHO, only 2 items significantly changed pre- and post-ECHO. Both items were related to perceptions and the role of the WSIB. For item 6 ‘I believe that the Workplace Safety and Insurance Board (WSIB) is not doing enough to help patients’, participants showed an overall improvement in confidence in the WSIB (i.e. WSIB working to help patients) and for item 7 ‘I believe that the WSIB is always on the side of the employer’, participants showed an average decrease in belief that WSIB was biased towards employers.
Figure 4.
Responses to the pre- and post-test questions regarding beliefs and attitudes.
Discussion
The results of this pilot study demonstrated the challenges to implement the first ECHO OEM in Canada. We delivered two cycles of 12 sessions each and discussed 25 cases of people with work-related health issues. Although we initially recruited 229 HCPs, only 150 (66%) attended at least one session, suggesting improvements are necessary to achieve greater participation from primary healthcare providers. Importantly, individuals who participated and completed all questionnaires reported moderate to high acceptability and satisfaction with the programme and increased self-efficacy. Increases in knowledge scores about OEM, while statistically significant, were small and only two of nine valid items improved in the attitudes and beliefs questionnaire.
Our results are similar to those from other ECHO programmes in Ontario for chronic pain [23,24], COVID-19 [25] and mental health [26]. In the pilot evaluation of the ECHO chronic pain, 296 people registered to the programme, 170 (64%) completed the pre-ECHO questionnaires, there were 51 dropouts (30%) and 119 (70%) who completed both pre- and post-ECHO questionnaires. There was a significant increase in self-efficacy and knowledge. Self-efficacy improvement was significantly higher among physicians, physician assistants and nurse practitioners than non-prescribers group. On average, 96% of participants were satisfied with ECHO chronic pain, and satisfaction was higher among those who presented cases and attended more sessions [23]. There is a need to employ qualitative research methods to understand the reasons and intentions of the ECHO participants when they register.
Our study did not collect patient data, and we cannot determine if the changes in knowledge, self-efficacy and beliefs demonstrated by participants in ECHO OEM also translated into changes in patients’ outcomes. The 25 cases presented were de-identified, and we did not follow up with the recommendations made during the session.
The main goal of ECHO OEM was to increase capacity among primary healthcare providers to manage patients with occupational and environmental health issues in Ontario. This was the first ECHO OEM in Canada, and the first ECHO in the world to consider all forms of occupational injury and diseases. We demonstrated that it is possible to implement this type of programme. Although there was considerable interest in the programme, with 229 healthcare providers registering to participate, participation and retention in the programme were poor. Future studies need to employ principles of implementation science to understand the barriers to participation and retention in continuing education programmes like ECHO. The time commitment of 90 minutes per week for 12 weeks might need to be re-evaluated. A secondary goal of ECHO OEM was to identify strategies to improve physician engagement with the WSIB. To assess if we had achieved this goal, we included a series of questions on the WSIB in the knowledge, behaviours and attitudes questionnaires. Although WSIB is the main funder, our project was conducted under the auspices of a broader Advisory Committee, and the WSIB had no influence on the questionnaires or data collection.
Participants in the programme also reported acceptability of and satisfaction with ECHO OEM. However, the magnitude of the changes in self-efficacy, knowledge, and attitudes and beliefs were small. This may reflect the fact that the programme seemed to have attracted some participants with some pre-existing expertise in occupational and environmental health, as demonstrated by the high baseline scores in these measures. This type of continuing medical education programme may also be more likely to be attended by those interested in the topic. As such, there may have been less room for improvement in scores. The attitudes and beliefs questions will need to be revised in future offers of this programme, and they need to reflect content that is discussed during the ECHO sessions.
This ECHO OEM provided knowledge and skills to HCP in primary care to manage patients with work-related problems, occupational illnesses and RTW strategies. Although the intended audience was primary HCPs with minimal occupational and environmental medicine knowledge, our programme attracted participants with some expertise and experience in this topic area. Future offerings of this programme should focus on recruiting participants in primary care with minimal expertise and experience.
Levels of knowledge and self-efficacy were assessed immediately after the end of the ECHO cycle, and we do not know if any changes to these measures were sustained after the programme ended. It is also important to assess if there is a spill-over effect on other patients seen by the participating HCPs, and if they share their knowledge with other HCPs. Diffusion and penetration of ECHO are defined as the influence on the treatment of other patients seen by the same HCP, transfer of knowledge to other HCPs within the same team, and transfer of knowledge to other HCPs in the same geographical area. Qualitative research methods are also important to assess if there is a better understanding of the role of WSIB after participants attended ECHO OEM.
Key learning points.
What is already known about this subject:
Health conditions caused and/or exacerbated by work are commonly seen in primary care settings.
Primary care providers receive little to no training in occupational or environmental medicine.
As a result, primary care clinicians lack knowledge of their role in return to work or how to engage with other partners in the return-to-work process.
What this study adds:
Project ECHO OEM (Extensions for Community Healthcare Outcomes Occupational and Environmental Medicine) is a virtual programme that was developed to disseminate knowledge from specialists in OEM to primary care providers in rural, remote and underserved areas.
Healthcare providers who attended ECHO and completed pre- and post-questionnaires reported gains in knowledge and self-efficacy in OEM.
What impact this may have on practice or policy:
There is a need to understand barriers to participation in programmes that teach primary care providers about occupational medicine.
Supplementary Material
Acknowledgement
We are grateful to WSIB for funding this pilot evaluation of ECHO OEM.
Contributor Information
A D Furlan, Institute for Work & Health, Toronto, Ontario, Canada; Department of Medicine, University of Toronto, Toronto, Ontario, Canada.
C Severin, Institute for Work & Health, Toronto, Ontario, Canada.
S Harbin, Institute for Work & Health, Toronto, Ontario, Canada.
E Irvin, Institute for Work & Health, Toronto, Ontario, Canada.
Nancy Carnide, Institute for Work & Health, Toronto, Ontario, Canada; Dalla Lana School of Public Health, University of Toronto, Toronto, Ontario, Canada.
Behdin Nowrouzi-Kia, Department of Occupational Science and Occupational Therapy, Temerty Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada.
Sara Macdonald, Institute for Work & Health, Toronto, Ontario, Canada.
Aaron Thompson, Institute for Work & Health, Toronto, Ontario, Canada; Department of Medicine, University of Toronto, Toronto, Ontario, Canada.
Qing Liao, Institute for Work & Health, Toronto, Ontario, Canada.
Peter Smith, Institute for Work & Health, Toronto, Ontario, Canada; Dalla Lana School of Public Health, University of Toronto, Toronto, Ontario, Canada; Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, Victoria, Australia.
Anil Adisesh, Department of Medicine, University of Toronto, Toronto, Ontario, Canada; Department of Medicine, Dalhousie University, Halifax, Nova Scotia, Canada; Faculty of Business, University of New Brunswick, Saint John, New Brunswick, Canada.
Funding
This program and research was funded by Workplace Safety and Insurance Board (WSIB) Research Grants #FURL2020.
Competing interests
A.F. is a member of the WSIB Drug Advisory Committee and the Health Advisory Committee. A.A. is Chief Medical Officer of Canadian Health Solutions, and member of the WSIB Scientific Advisory Table on Occupational Disease. A.T. is Chief Medical Officer at WSIB, medical consultant for Wawanesa insurance Company. B.N.K. is Scientific Advisor for Blue Branch Inc, research consultant for Ontario Electrical League and TELUS Health.
References
- 1. Collaborators GBDORF. Global and regional burden of disease and injury in 2016 arising from occupational exposures: a systematic analysis for the Global Burden of Disease Study 2016. Occup Environ Med 2020;77:133–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Minov J. Occupational chronic obstructive pulmonary disorder: prevalence and prevention. Expert Rev Respir Med 2022;16:429–436. [DOI] [PubMed] [Google Scholar]
- 3. Nambiema A, Bertrais S, Bodin J. et al. Proportion of upper extremity musculoskeletal disorders attributable to personal and occupational factors: results from the French Pays de la Loire study. BMC Public Health 2020;20:456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Walker-Bone K, Hollick R.. Health and work: what physicians need to know. Clin Med 2021;21:195–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Beaumont DG. The interaction between general practitioners and occupational health professionals in relation to rehabilitation for work: a Delphi study. Occup Med (Lond) 2003;53:249–253. [DOI] [PubMed] [Google Scholar]
- 6. Kek B, Buchanan J, Adisesh A.. An introduction to occupational medicine using a team-based learning methodology. J Occup Environ Med 2019;61:132–135. [DOI] [PubMed] [Google Scholar]
- 7. Furlan AD, Harbin S, Vieira FF. et al. Primary care physicians’ learning needs in returning ill or injured workers to work. a scoping review. J Occup Rehabil 2022;32:591–619. [DOI] [PubMed] [Google Scholar]
- 8. Kosny A, Franche RL, Pole J, Krause N, Cote P, Mustard C.. Early healthcare provider communication with patients and their workplace following a lost-time claim for an occupational musculoskeletal injury. J Occup Rehabil 2006;16:27–39. [DOI] [PubMed] [Google Scholar]
- 9. Hildebrandt J, Pfingsten M, Saur P, Jansen J.. Prediction of success from a multidisciplinary treatment program for chronic low back pain. Spine 1997;22:990–1001. [DOI] [PubMed] [Google Scholar]
- 10. Scheel IB, Hagen KB, Oxman AD.. Active sick leave for patients with back pain: all the players onside, but still no action. Spine 2002;27:654–659. [DOI] [PubMed] [Google Scholar]
- 11. Collie A, Newnam S, Keleher H. et al. Recovery within injury compensation schemes: a system mapping study. J Occup Rehabil 2019;29:52–63. [DOI] [PubMed] [Google Scholar]
- 12. Pietila-Holmner E, Enthoven P, Gerdle B, Molander P, Stalnacke BM.. Long-term outcomes of multimodal rehabilitation in primary care for patients with chronic pain. J Rehabil Med 2020;52:jrm00023. [DOI] [PubMed] [Google Scholar]
- 13. Berglund E, Anderzen I, Andersen A. et al. Multidisciplinary intervention and acceptance and commitment therapy for return-to-work and increased employability among patients with mental illness and/or chronic pain: a randomized controlled trial. Int J Environ Res Public Health 2018;15:2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Stergiou-Kita M, Grigorovich A, Gomez M.. Development of an inter-professional clinical practice guideline for vocational evaluation following severe burn. Burns 2014;40:1149–1163. [DOI] [PubMed] [Google Scholar]
- 15. University of New Mexico. Project ECHO. https://hsc.unm.edu/echo/ (11 December 2023, date last accessed). [Google Scholar]
- 16. Sood A, Assad N, Jarrell W. et al. A virtual community-of-practice approach by rural stakeholders in managing pneumoconiosis in the USA: a cross-sectional analysis. Rural Remote Health 2020;20:5784. [DOI] [PubMed] [Google Scholar]
- 17. Zhou C, Crawford A, Serhal E, Kurdyak P, Sockalingam S.. The impact of project ECHO on participant and patient outcomes: a systematic review. Acad Med 2016;91:1439–1461. [DOI] [PubMed] [Google Scholar]
- 18. ECHO Ontario. Project ECHO Ontario SuperHub. https://www.echoontario.ca/Start-an-ECHO/Superhub.aspx (11 December 2023, date last accessed). [Google Scholar]
- 19. Arora S, Kalishman S, Thornton K. et al. Expanding access to hepatitis C virus treatment – Extension for Community Healthcare Outcomes (ECHO) project: disruptive innovation in specialty care. Hepatology 2010;52:1124–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Braeckman L, De Clercq B, Janssens H. et al. Development and evaluation of a new occupational medicine teaching module to advance self-efficacy and knowledge among medical students. J Occup Environ Med 2013;55:1276–1280. [DOI] [PubMed] [Google Scholar]
- 21. Hassan S, Carlin L, Zhao J, Taenzer P, Furlan AD.. Promoting an interprofessional approach to chronic pain management in primary care using Project ECHO. J Interprof Care 2020;35:464–467. [DOI] [PubMed] [Google Scholar]
- 22. Colleran K, Harding E, Kipp BJ. et al. Building capacity to reduce disparities in diabetes: training community health workers using an integrated distance learning model. Diabetes Educ 2012;38:386–396. [DOI] [PubMed] [Google Scholar]
- 23. Furlan AD, Zhao J, Voth J. et al. Evaluation of an innovative tele-education intervention in chronic pain management for primary care clinicians practicing in underserved areas. J Telemed Telecare 2019;25:484–492. [DOI] [PubMed] [Google Scholar]
- 24. Zhao J, Salemohamed N, Stinson J. et al. Health care providers’ experiences and perceptions participating in a chronic pain telementoring education program: a qualitative study. Can J Pain. 2020;4:111–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zhao J, Rozenberg D, Kaul R, et al. The positive impact of a telemedicine education program on healthcare workers during the COVID-19 pandemic in Ontario, Canada. Ann Fam Med 2022;20:3260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sockalingam S, Arena A, Serhal E, Mohri L, Alloo J, Crawford A.. Building provincial mental health capacity in primary care: an evaluation of a project ECHO mental health program. Acad Psychiatry 2018;42:451–457. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.