Abstract
Background:
Skin conditions form a major bulk of diseases in the community. With a disproportionately low number of dermatologists in the country, and a greatly unequal distribution between urban versus rural areas, ineffective treatment and mismanagement of skin conditions are, however, commonplace.
Objective:
To develop standard treatment workflows (STWs) for certain skin diseases for use by clinicians at primary, secondary, and tertiary care centers.
Methodology:
Seven members, from various academic institutes across the country, were selected for formulation of the STWs. They were provided logistic and technical support by the ICMR, Department of Health Research (DHR), and WHO India office. Multiple rounds of online and physical discussions were performed to identify topics that would be most useful in the management of skin diseases for the health care personnel (HCP) and subsequently to frame the STW content.
Results:
The selected diseases included acne and rosacea, alopecia, bacterial skin infections, cutaneous adverse drug reactions, dermatophytosis, eczema/dermatitis, immunobullous dermatoses, psoriasis, scabies, varicella and herpes, vitiligo, and urticaria. There was one separate module on rational use of topical corticosteroids. The STWs for these conditions have been finalised and are available as physical posters in health centers and can also be accessed online and through mobile applications.
Conclusion:
Thirteen STW modules have been prepared with a view to optimize management of skin diseases at various levels of health care system of the country.
Keywords: ICMR, primary health care, skin diseases, standard treatment workflow
Introduction
Ensuring health of the citizens and providing quality medical services to all is an important concern of the government and the major motivating force behind the Standard Treatment Workflow (STW) project.[1] STWs catering to 21 specialties have been formulated by the Indian Council of Medical Research (ICMR) in collaboration with National Health Authority (NHA), Government of India, specialists from the concerned specialties, and World Health Organization (WHO) India country office, for utilization at various levels of health care system of the country. These have now been made available in four ways by Government of India to be adopted and followed by all healthcare providers, with the objective of providing quality healthcare at an affordable cost as a part of Universal Health Coverage (UHC). UHC entails ensuring all people have access to quality health services – including prevention, promotion, treatment, rehabilitation, and palliation – without incurring financial hardship.[2]
Dermatological diseases form a significant share of health conditions presenting to all levels of healthcare system – primary, secondary, and tertiary, and of health economics of a community. Many cross-sectional surveys have estimated a high prevalence of skin diseases of around 10%–87% in varied populations from India and abroad.[3,4,5,6,7] Skin diseases contribute 1.79% to the global burden of disease measured in disability-adjusted life years (DALYs) and form the fourth leading cause of nonfatal disease burden at the global level [after iron deficiency anemia (43.7 million DALYs), tuberculosis (49.8 million DALYs), and sense organ diseases (54.4 million DALYs)]. As per the global burden of disease study in 2013, skin and subcutaneous diseases were responsible for 41.6 million DALYs and 39.0 million years lived with disability (YLDs).[8,9] Individual skin diseases varied in size from 0.38% of total burden for dermatitis (atopic, contact, and seborrheic dermatitis), 0.29% for acne vulgaris, 0.19% for psoriasis, 0.19% for urticaria, 0.16% for viral skin diseases, 0.15% for fungal skin diseases, 0.07% for scabies, 0.06% for malignant skin melanoma, 0.05% for pyoderma, 0.04%for cellulitis, 0.03% for keratinocyte carcinoma, 0.03% for decubitus ulcer, and 0.01% for alopecia areata. All other skin and subcutaneous diseases composed 0.12% of total DALYs.[8,9]
The negative psychological effects of even localized skin disorders have been highlighted in literature. Low self-esteem, anxiety, social embarrassment, depression, and stigmatization are associated with most chronic skin disorders. A multicentric study involving 3,635 patients with various common dermatological diseases (psoriasis, infections, eczema, acne, atopic eczema, hand eczema, etc) and 1,359 controls reported a significantly higher prevalence of clinical depression (10.1% vs. 4.3%), anxiety disorder (17.2% vs. 11.1%), and suicidal ideation (12.7% vs. 8.3%) among patients as compared with controls.[10] Expectedly, chronic skin conditions also impair the quality of life of cohabitants apart from patients. Caregiver burnout syndrome expressed as stress, anxiety, or depression has been observed in cohabitants of patients with chronic cutaneous conditions.[11,12,13,14] This is in addition to a significant economic burden of skin diseases on families, especially those belonging to lower socioeconomic strata.
The low exposure of Indian medical graduates to dermatology in the undergraduate curriculum sharply contrasts with the volume of dermatological conditions at the primary health care level. Furthermore, owing to low coverage of specialized dermatology services in communities, and aggregation of dermatologists in urban areas, large swathes of the country remain poorly covered with respect to dermatologic care.[15] As per a report of Ministry of Health and Family Welfare, there are only 1.9 dermatologists per million in rural India as compared to 23.4 per million in urban areas.[16] Therefore, the STWs for Dermatology were conceptualized with an aim to provide a simplified approach to treatment of skin diseases of public health importance at all levels of healthcare.
Methodology
Selection of expert group for dermatology
The initial selection of the expert group, including the chairperson and cochairperson, was by the Department of Health Research, Government of India. The selection ensured representation from medical colleges in various parts of the country to have a broad perspective. After the first meeting, the group was further expanded to a total of seven members with expertise in the decided STW topics. The process began in 2019, and logistic support was provided by the ICMR throughout the process of STW development.
Selection of skin diseases for formulating individual STWS
The first task of the team of experts selected for formulating dermatology STWs was to narrow down the skin diseases of importance at the community level. After much deliberation, 13 disorders [Box 1] were chosen. The selection was based on public health importance of the diseases and the frequency of these disorders in dermatologic set-ups from various parts of the country.[3,4,5,6,7,8,17,18,19,20,21,22] It can be a challenge for primary care providers to differentiate routine skin ailments from more serious, life-threatening dermatologic emergencies that require immediate intervention, leading to mismanagement and even mortality.[23] Therefore, some severe life-threatening skin diseases (severe cutaneous adverse drug reactions and immune-bullous disorders) were also incorporated with a view to apprise healthcare providers at all levels about their presentation and initial management. In addition, an STW was also dedicated to rational use of topical steroids, an emergent issue in dermatologic practice. Notably, dermatology had the maximum number of STWs pertaining to a single speciality.
Box 1.
The 13 dermatologic disorders/scenarios chosen for formulating STWs
| 1. Acne and rosacea |
| 2. Alopecia |
| 3. Bacterial skin infections |
| 4. Cutaneous adverse drug reactions (in two parts – A and B) |
| 5. Dermatophytosis |
| 6. Eczema/dermatitis |
| 7. Immunobullous dermatoses |
| 8. Psoriasis |
| 9. Rational use of topical steroids |
| 10. Scabies |
| 11. Varicella and herpes |
| 12. Vitiligo |
| 13. Urticaria |
Formulation and designing of dermatologic STWs [Figure 1]
Figure 1.
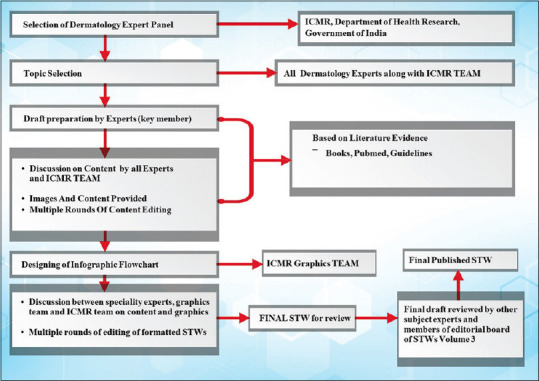
The steps in the process of development of Dermatology STWs
The STWs were based on updated and recent scientific evidence available to the expert group till the time of preparation of the documents. However, we faced certain challenges in the process of formulating the STWs, and prominent ones among them are as follows:
Catering to a varied audience: the target readership of the STWs includes primary care providers, medical undergraduates and postgraduate students, general practitioners, and specialists. The language was thus kept simple and clear.
Content: The idea of STWs has been to compress all useful content within a single-page infographic flowchart. This was a significant challenge for experts as each STW covered not only treatment but also clinical presentations and diagnoses.
Images: Dermatology being a visual specialty, it was imperative to include as many clinical images as possible in each STW to give a clear idea of the presentation/s to a reader. This, however, led to further space constraints.
The COVID-19 pandemic: The process was started in mid-2019, and the group had several face-to-face meetings in the first few months. Further on, however, we faced major hurdles with the onset of the COVID-19 pandemic slowing the progress significantly, leading to delay in the finalization of the whole set of STWs.
A constant format was followed across all dermatology STWs to bring uniformity and clarity. The process of formulation of STWs involved the following steps and processes [Figure 1]:
The expert group was headed by a chairperson and cochairperson to facilitate discussions and achieve consensus among group members.
A key member was selected for preparation of the draft STW: This was based on discussions among all members, keeping in mind individual interests and expertise of members. The discussions also included members from ICMR STW team.
The constraints of infrastructure and availability of drugs at various health care levels were also kept in mind while formulating the STWs.
The diagnostic and treatment content were based on literature evidence and existing guidelines (wherever applicable) along with experts’ opinions.
The flow of diagnostic and treatment recommendations for each condition began with those for primary health centres first, followed by secondary and tertiary care centres.
Red flags were highlighted to apprise the reader of scenarios that would require emergency and immediate management, along with warning signs for quick management and referral.
Disclaimers were inserted at the end of each STW which discuss applicability as well as limitations of the STW.
ICD-10 codes for diseases were included in all STWs.
Important messages regarding the condition covered were added with a pointing-finger sign at the bottom of each module.
Infographics were given special attention so that the final document would be both detailed and easy to follow by all target healthcare professionals. These were prepared by the graphics team of ICMR and reviewed and edited by subject experts.
After multiple rounds of discussions on draft STWs, and after achieving a consensus among all members, the flow and content of each STW was finalized. After an internal validation by the expert group, the draft documents were sent out for external validation to editorial team members of the STW -3rd Volume, and 2 experts from other specialties gave pointwise suggestions for improving clarity of each STW. The feedback provided was incorporated, and final STWs were generated. These were released on July 12th, 2022, by the ICMR as a part of the 3rd Volume of ICMR STWs.
Results
All individual STWs can be accessed at https://stw.icmr.org.in/ and also through mobile applications (see below). Some prominent highlights of the individual STWs are mentioned below.
BACTERIAL SKIN INFECTIONS STW (ICD-10-L01, L73.9, L08, L02, L03, A46 and L00) (https://stw.icmr.org.in/images/pdf/Dermatology/BACTERIAL_SKIN_INFECTIONS.pdf) Bacterial infections constitute about 10-35% of skin diseases in the community as per various estimates, making these an important public health concern.[3,6,24,25] The STW covers nine conditions – starting from impetigo, ecthyma, folliculitis, and furuncles, to carbuncle, abscess, cellulitis, erysipelas, and staphylococcal scalded skin syndrome. The STW starts with general principles of management common to all pyodermas and then goes on to details of individual infections. A brief clinical description and a typical image provided for all conditions. Topical, oral, and intravenous drugs (as indicated) have been mentioned with doses, along with investigations wherever indicated. The STW also covers treatment of nasal staphylococcal carriers, options for penicillin-allergic individuals, and a section on treatment of methicillin-resistant Staphylococcus aureus infection, since the latter has become common in community-acquired skin and soft tissue infections in the country.[26,27] The red flag signs include signs of progression to necrotising fasciitis and sepsis, and a note has been put at the end about changes in antibiotic susceptibility patterns with region and time.
-
SCABIES (ICD-10-B86)
(https://stw.icmr.org.in/images/pdf/Dermatology/SCABIES.pdf)
Scabies is the commonest parasitic skin infections encountered by primary care physicians in both developing and developed countries and is prone to be misdiagnosed by an untrained eye.[24,28] Thus, the scabies STW includes many classical images of scabies, showing lesions at various commonly affected sites, along with images of acral-crusted scabies and a microscopic image of Sarcoptes scabiei. Treatment section stresses advice on general measures, treatment of entire skin rather than lesions alone, family treatment, reinfestations, and management of crusted scabies and persistent nodules, apart from drug treatment of uncomplicated scabies and of secondarily infected scabies.
-
ECZEMA/DERMATITIS (ICD-10-L20)
(https://stw.icmr.org.in/images/pdf/Dermatology/ECZEMA.pdf)
Eczemas form the second most common skin disease encountered in community settings after infections.[3,24] The STW apprises the reader about various types and presentations of eczemas, differential diagnoses, and basics of treatment. Use of systemic drugs for the condition has been kept only in the domain of tertiary-level care.
-
DERMATOPHYTOSES (ICD-10-B35.9)
(https://stw.icmr.org.in/images/pdf/Dermatology/DERMATOPHYTOSES.pdf)
Owing to the changing dynamics of dermatophytic infections in the country, this has become an important condition to be managed at all levels of healthcare.[29,30] Taking into consideration the significant rate of topical steroid abuse among dermatophytosis patients, a special advisory has been added at the top to impress upon all healthcare professionals, the need to counsel patients on perils of self-medication with steroids.[31] Variant presentations of steroid-modified tinea skin infections have been discussed briefly in the STW. Treatment at primary and secondary health centres has been detailed, followed by recommended treatment options at tertiary care centres. Alongside, since conventional treatment durations do not suffice for treatment of dermatophytic skin infections anymore, treatment till cure has been impressed upon. The scenarios which need referral to tertiary care have been enlisted. Tinea pedis, tinea manuum, and onychomycosis have also been covered from clinical diagnostic, and treatment aspects.
-
VARICELLA AND HERPES ZOSTER (ICD-10-B01-02)
(https://stw.icmr.org.in/images/pdf/Dermatology/VARICELLA__HERPES_ZOSTER.pdf)
The clinical spectrum and treatment of both diseases has been covered, along with important special scenarios, red flag signs for referral to tertiary centres, complications, and preventive measures. A stepwise management of herpetic/post-herpetic neuralgia has been provided as well.
-
RATIONAL USE OF TOPICAL MEDICATIONS
(https://stw.icmr.org.in/images/pdf/Dermatology/RATIONAL_USE_OF_TOPICAL_MEDICATIONS.pdf) With a significant reliance on topical drugs in the specialty, the expert group felt it was essential to include a document detailing rationalisation of topical drug application. The STW details principles of topical drug use, with special emphasis on topical steroid use. Imagery of topical steroid-related cutaneous adverse effects have been included to make all levels of healthcare professionals aware of this important issue. The STW mentions various formulations of topical drug delivery, rational and irrational topical drug combinations, finger-tip unit method of application, and about correct use of sunscreens and moisturizers in dermatology.
-
Alopecia (ICD-10-L63.9)
(https://stw.icmr.org.in/images/pdf/Dermatology/ALOPECIA.pdf)
The STW focuses on common causes of alopecia, categorizing them into scarring and non-scarring groups, with pointers to differentiate between the two. Clinical morphology to diagnose individual conditions, with clinical images for each, have been provided. Management of tinea capitis, alopecia areata, and patterned hair loss has been given, with a brief on scenarios requiring referral to tertiary centres. Specialist referrals have been suggested for all scarring alopecias and congenital alopecias, and for systemic management of extensive alopecia areata.
-
Cutaneous adverse drug reactions (Part A and B) ICD-10-L27.0
(https://stw.icmr.org.in/images/pdf/Dermatology/CUTANEOUS_PART_A.pdf and https://stw.icmr.org.in/images/pdf/Dermatology/CUTANEOUS_PART_B.pdf)
The cutaneous adverse drug reactions (cADRs) have been divided into non-severe (Fixed drug eruption and maculopapular eruptions) and severe (acute generalized exanthematous pustulosis, angioedema/anaphylaxis and erythema multiforme/Stevens-Johnson syndrome/Toxic epidermal necrolysis). The former has been covered in part A and the latter in part B of the STWs on cADRs. Basic principles of management of all cADRs have been discussed followed by individual cADRs. Clinical descriptions have been provided along with images to aid in accurate diagnosis. Treatment at primary, secondary, and tertiary levels have been detailed. Red flag signs to differentiate maculopapular reactions from more severe cADRs have been highlighted. Drug provocation testing has been briefly discussed.
-
Immunobullous dermatoses (ICD-10-L13.8)
(https://stw.icmr.org.in/images/pdf/Dermatology/IMMUNOBULLOUS.pdf)
The STW describes pointers to diagnose immunobullous dermatoses, with brief description of important entities. Red flag signs indicating sepsis have been highlighted. General measures have been detailed for all levels of healthcare, while specific management is recommended to be started only in centres where facility for monitoring and management of complications of treatment is available.
-
Vitiligo (ICD-10-L80)
(https://stw.icmr.org.in/images/pdf/Dermatology/VITILIGO.pdf)
Vitiligo is a disease associated with significant stigma in our society. Also, the disease is often misdiagnosed/overdiagnosed at primary-level centres. Thus, the focus of vitiligo STW is to make healthcare professionals at all levels, aware of the clinical presentations of vitiligo and the various differential diagnoses. Treatment at primary, secondary, and tertiary level centres have been detailed under categories of acrofacial, generalized, universal, and segmental vitiligo.
-
Psoriasis (ICD-10-L40)
https://stw.icmr.org.in/images/pdf/Dermatology/PSORIASIS.pdf
The various clinical presentations have been detailed along with clinical images for each. Treatment of limited plaque psoriasis, generalized plaque psoriasis, guttate psoriasis, and palmoplantar psoriasis has been described for primary, secondary, and tertiary care centres. For erythrodermic psoriasis and pustular psoriasis, only stabilization and basic management has been advised for primary and secondary centres and specific management has been kept in the domain of tertiary centres only. General principles of management applicable to all levels of healthcare have been added at the beginning, along with an overview of topical and systemic drugs used for the disease.
-
URTICARIA (ICD-10-L50.9)
https://stw.icmr.org.in/images/pdf/Dermatology/URTICARIA_AND_ANGIOEDEMA.pdf
The STW apprises the reader of the typical presentation of urticaria and angioedema and the possible differentials. A brief on clinical classification of chronic urticaria has been added. Treatment at primary level has been restricted to antihistamines, with suggested updosing in case of unresponsiveness. Systemic treatment with conventional drugs is suggested at secondary care level, in case of lack of complete response with antihistamines alone. Use of Omalizumab has been suggested only in tertiary care centres. A caution has been added to avoid use of oral or parenteral steroids for routine care of urticaria, except in few mentioned scenarios, and only as suggested in the STW. Avoidance of possible triggers has been added as a part of management principles.
-
Acne and Rosacea (ICD-10-L70-71)
https://stw.icmr.org.in/images/pdf/Dermatology/Acne_Roseacea.pdf
Being a common disorder of the adolescents, often persisting into adulthood, acne is an important skin disease in the community. Clinical differentiation of acne and rosacea has been mentioned along with potential differentials and variant presentations. Role of drugs, especially topical steroids, in causing acne has been highlighted. Management at the level of primary healthcare centres has been restricted to topical drugs and combinations as mentioned in the STW. Systemic treatment has been kept in the domain of secondary and tertiary level healthcare centres only.
Discussion
An important aspect of the STWs is to improve quality of healthcare at primary and secondary levels. This is an urgent need, as various estimates indicate inadequacy of treatment of skin diseases at these levels. The WHO report on Epidemiology and Management of Common Skin Diseases in Children in Developing Countries observed that treatment of skin diseases was not considered efficacious in a worrisome majority.[24] As per the Bamako Pilot Project, only 42% of patients visiting primary healthcare centres for skin disease benefited from both a clear diagnosis and an adequate treatment.[27] Similarly, a poor agreement of 56% was observed between the diagnosis made by a primary care physician and a tele-dermatologist in a north Indian study.[25] The treatment of skin diseases by the primary healthcare system was considered inappropriate or ineffective in 69% of cases from mountainous regions of North India,[7] in 66% of cases in Ethiopia,[32] and 70% in Mexico.[33] To add to this, the cost of ineffective treatments of skin diseases borne hence, has been shown to be a major financial burden on the patients’ families, underscoring the need for developing efficient and cost-effective dermatologic treatments at all levels of healthcare.[33]
National guidelines and programmes cover a very small fraction of cutaneous diseases encountered at the community level. Apart from leprosy, post kala azar dermal leishmaniasis, sexually transmitted diseases and tuberculosis, none of the other skin diseases are covered by national programmes, despite the very high prevalence of many skin disorders in communities, and frequent ineffective management of skin diseases at primary health level as previously highlighted. Although short training sessions of healthcare staff have been shown to improve the ability to diagnose and manage skin diseases,[34] it is not logistically and economically feasible to cover extensive areas with this approach. Tele-dermatology has been shown to be an effective approach to improve healthcare delivery in resource-poor primary care settings, and its scope has vastly broadened after the COVID-19 pandemic.[35,36] Telemedicine has been given a legal status in India, and a framework of rules are available to guide the use of the same.[37,38] However, technical and logistic constraints limit its wider use at the moment. Further, the list of drugs approved for prescription by tele-dermatology lack most topical and systemic treatment options for management of common dermatoses. Therefore, the STWs were planned to be systematically developed documents to guide healthcare professionals in their clinical decision-making. The scope of the document was however not restricted to primary care only, and algorithms for secondary and tertiary level care were also added with an aim to empower healthcare professionals at all levels with clear and concise treatment pathways. Another prominent advantage is the inclusion of guidance on referrals to higher centres, thus ensuring smooth integration and efficient coordination between different levels of healthcare.
STWs pertaining to 122 conditions covering 23 disciplines have been published by the ICMR in three volumes for use at all levels of healthcare. Dermatology STWs are included in volume 3 of the same. To facilitate greater access, STWs are also available as stickable posters to be put up in healthcare centres, whereas the e-versions are available online at https://stw.icmr.org.in/A mobile application including all STWs has also been released by the ICMR, which is downloadable on android (www.bit.ly/3BtLcmL) and IOS (https://apple.co/3zMO5xF) platforms. Many specialty-wise webinars have been organized by the ICMR to promote use of the STWs across specialties.
NHA, a partner agency with ICMR STW, is implementing and disseminating the STWs through the Ayushman Bharat Scheme (ABS) and Ayushman Bharat Digital India (ABDI) scheme in various states and districts. Once completely integrated and implemented into the healthcare system, STWs will be instrumental in achieving the goal of UHC for all Indian citizens, providing equitable and high-quality healthcare across the nation.
Limitations and Future Directions
The STWs cover only certain skin diseases as selected by expert consensus. Although the documents have been prepared with great care by experts in the field while keeping in mind the best literature evidence existing at the time of formulation, the content would need to be regularly updated to incorporate newer conditions, evidence, drugs, and diagnostic techniques in future. Special situations have been incorporated as far as possible, but complexities of individual cases may go beyond the areas covered by the STWs e.g. concerns of co-morbidities, polypharmacy, etc., Because of space constraints and the need for clarity in presentation, focus was given to major actionable items. Revisions may also be required in future based on feedback received from various healthcare professionals, once the STWs are completely integrated into the healthcare systems. The STWs also urgently need community validation to confirm their desired utility and to generate evidence for their wider use. Implementation research would be the next step in the process and the planning for the same is already underway by the concerned agencies.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.ICMR Standard Treatment Workflows. [[Last accessed on 2023 Sep 11]]. Available from: https://main.icmr.nic.in/content/standard-treatment-workflows-stws .
- 2.Booklet on Universal Health Coverage (UHC) [[Last accessed on 2023 Sep 11]]. Available from: https://main.mohfw.gov.in/newshighlights/booklet-universal-health-coverage-uhc .
- 3.Singhal RR, Talati KN, Gandhi BP, Shinde MK, Nair PA, Phatak AG. Prevalence and pattern of skin diseases in tribal villages of Gujarat: A teledermatology approach. Indian J Community Med. 2020;45:199–203. doi: 10.4103/ijcm.IJCM_76_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rao GS, Kumar SS, Sandhya Pattern of skin diseases in an Indian village. Indian J Med Sci. 2003;5:108–10. [PubMed] [Google Scholar]
- 5.Kownacki S. Skin diseases in primary care: What should GPs be doing? Br J Gen Pract. 2014;64:380–1. doi: 10.3399/bjgp14X680773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dogra S, Kumar B. Epidemiology of skin diseases in school children: A study from northern India. Pediatr Dermatol. 2003;20:470–3. doi: 10.1111/j.1525-1470.2003.20602.x. [DOI] [PubMed] [Google Scholar]
- 7.Grills N, Grills C, Spelman T, Stoove M, Hellard M, El-Hayek C, et al. Prevalence survey of dermatological conditions in mountainous north India. Int J Dermatol. 2012;51:579–87. doi: 10.1111/j.1365-4632.2011.05131.x. [DOI] [PubMed] [Google Scholar]
- 8.Karimkhani C, Dellavalle RP, Coffeng LE, Flohr C, Hay RJ, Langan SM, et al. Global skin disease morbidity and mortality: An update from the global burden of disease study 2013. JAMA Dermatol. 2017;153:406–12. doi: 10.1001/jamadermatol.2016.5538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hay RJ, Johns NE, Williams HC, Bolliger IW, Dellavalle RP, Margolis DJ, et al. The global burden of skin disease in 2010: An analysis of the prevalence and impact of skin conditions. J Invest Dermatol. 2014;134:1527–34. doi: 10.1038/jid.2013.446. [DOI] [PubMed] [Google Scholar]
- 10.Dalgard FJ, Gieler U, Tomas-Aragones L, Lien L, Poot F, Jemec GBE, et al. The psychological burden of skin diseases: A cross-sectional multicenter study among dermatological out-patients in 13 European countries. J Invest Dermatol. 2015;135:984–91. doi: 10.1038/jid.2014.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sánchez-Díaz M, Salazar-Nievas MC, Molina-Leyva A, Arias-Santiago S. The burden on cohabitants of patients with chronic spontaneous urticaria: A cross-sectional study. J Clin Med. 2022;11:3228. doi: 10.3390/jcm11113228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martínez-García E, Arias-Santiago S, Valenzuela-Salas I, Garrido-Colmenero C, García-Mellado V, Buendía-Eisman A. Quality of life in persons living with psoriasis patients. J Am Acad Dermatol. 2014;71:302–7. doi: 10.1016/j.jaad.2014.03.039. [DOI] [PubMed] [Google Scholar]
- 13.Martínez-García E, Arias-Santiago S, Herrera-Acosta E, Affleck A, Herrera-Ceballos E, Buendía-Eisman A. Quality of life of cohabitants of people living with acne. Acta Derm Venereol. 2020;100:adv00290. doi: 10.2340/00015555-3636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ramos-Alejos-Pita C, Arias-Santiago S, Molina-Leyva A. Quality of life in cohabitants of patients with hidradenitis suppurativa: A cross-sectional study. Int J Environ Res Public Health. 2020;17:6000. doi: 10.3390/ijerph17166000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ashique KT, Kaliyadan F. Teledermatology in the wake of COVID -19 scenario: An Indian perspective. Indian Dermatol Online J. 2020;11:301–6. doi: 10.4103/idoj.IDOJ_260_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. [[Last accessed on 2023 Sep 11]]. Available from: https://timesofindia.indiatimes.com/blogs/voices/top-5-specialists-that-saw-a-spike-in-2023-for-tele-opd-in-rural-areas/
- 17.Saurabh S, Sahu SK, Sadishkumar A, Kakkanattu JC, Prapath I, Ralte IL, et al. Screening for skin diseases among primary school children in a rural area of Puducherry. Indian J Dermatol Venereol Leprol. 2013;79:268. doi: 10.4103/0378-6323.107664. [DOI] [PubMed] [Google Scholar]
- 18.Emodi LJ, Ikefuna AN, Uchendu U, Duru UA. Skin diseases among children attending the out patient clinic of the University of Nigeria teaching hospital, Enug. Afr Health Sci. 2010;10:362–6. [PMC free article] [PubMed] [Google Scholar]
- 19.Grover S, Ranyal RK, Bedi MK. A cross section of skin diseases in rural Allahabad. Indian J Dermatol. 2008;53:179–81. doi: 10.4103/0019-5154.44789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agarwal S, Sharma P, Gupta S, Ojha A. Pattern of skin diseases in Kumaun region of Uttarakhand. Indian J Dermatol Venereol Leprol. 2011;77:603–4. doi: 10.4103/0378-6323.84073. [DOI] [PubMed] [Google Scholar]
- 21.Dimri D, Reddy BV, Kumar Singh A. Profile of skin disorders in unreached hilly areas of North India. Dermatol Res Pract 2016. 2016:8608534. doi: 10.1155/2016/8608534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Devi T, Zamzachin G. Pattern of skin diseases in Imphal. Indian J Dermatol. 2006;51:149–50. [Google Scholar]
- 23.Freiman A, Borsuk D, Sasseville D. Dermatologic emergencies. CMAJ. 2005;173:1317–9. doi: 10.1503/cmaj.050783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization. Epidemiology and management of common skin diseases in children in developing countries. 2005. [[Last accessed on 2023 Sep 11]]. Available from: https://apps.who.int/iris/handle/10665/69229 .
- 25.Patro BK, Tripathy JP, De D, Sinha S, Singh A, Kanwar AJ. Diagnostic agreement between a primary care physician and a teledermatologist for common dermatological conditions in North India. Indian Dermatol Online J. 2015;6:21–6. doi: 10.4103/2229-5178.148927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tong SY, Kearns AM. Community-associated MRSA from the Indian subcontinent. Lancet Infect Dis. 2013;13:734–5. doi: 10.1016/S1473-3099(13)70231-7. [DOI] [PubMed] [Google Scholar]
- 27.Indian network for surveillance of antimicrobial resistance group IMethicillin resistant Staphylococcus aureus (MRSA) in India: Prevalence and susceptibility pattern. Indian J Med Res. 2013;137:363–9. [PMC free article] [PubMed] [Google Scholar]
- 28.Dadabhoy I, Butts JF. Parasitic skin infections for primary care physicians. Prim Care. 2015;42:661–75. doi: 10.1016/j.pop.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 29.Chowdhary A, Singh A, Kaur A, Khurana A. The emergence and worldwide spread of the species Trichophyton indotineae causing difficult-to-treat dermatophytosis: A new challenge in the management of dermatophytosis. PLoS Pathog. 2022;18:e1010795. doi: 10.1371/journal.ppat.1010795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khurana A, Agarwal A, Agrawal D, Panesar S, Ghadlinge M, Sardana K, et al. Effect of different itraconazole dosing regimens on cure rates, treatment duration, safety, and relapse rates in adult patients with tinea corporis/cruris: A randomized clinical trial. JAMA Dermatol. 2022;158:1269–78. doi: 10.1001/jamadermatol.2022.3745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khurana A, Gupta A, Sardana K, Sethia K, Panesar S, Aggarwal A, et al. A prospective study on patterns of topical steroids self-use in dermatophytoses and determinants predictive of cutaneous side effects. Dermatol Ther. 2020;33:e13633. doi: 10.1111/dth.13633. [DOI] [PubMed] [Google Scholar]
- 32.Figueroa J, Fuller L, Abraha A, Hay R. Skin disease in southwestern Ethiopia: Rationale for a community approach. Int J Dermatol. 1998;37:752–8. doi: 10.1046/j.1365-4362.1998.00425.x. [DOI] [PubMed] [Google Scholar]
- 33.Hay RJ, Estrada Castanon R, Alarcon Hernandez H, Chavez Lopez G, Lopez Fuentes LF, Paredes Solis S, et al. Wastage of family income on skin disease in Mexico. Br Med J. 1994;309:848. doi: 10.1136/bmj.309.6958.848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mahé A, Faye O, N’Diaye HT, Konaré HD, Coulibaly I, Kéita S, et al. Integration of basic dermatological care into primary health care services in Mali. Bull World Health Organ. 2005;83:935–43. [PMC free article] [PubMed] [Google Scholar]
- 35.Nelson CA, Takeshita J, Wanat KA, Bream KD, Holmes JH, Koenig HC, et al. Impact of store-and-forward (SAF) teledermatology on outpatient dermatologic care: A prospective study in an underserved urban primary care setting. J Am Acad Dermatol. 2016;74:484–90.e1. doi: 10.1016/j.jaad.2015.09.058. [DOI] [PubMed] [Google Scholar]
- 36.Thomas J, Kumar P. The scope of teledermatology in India. Indian Dermatol Online J. 2013;4:82–9. doi: 10.4103/2229-5178.110579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Venkatesh U, Aravind GP, Velmurugan AA. Telemedicine practice guidelines in India: Global implications in the wake of the COVID-19 pandemic. World Med Health Policy. 2022;14:589–99. doi: 10.1002/wmh3.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Board of governors in supersession of the Medical Council of India-Telemedicine Practice Guidelines Enabling Registered Medical Practitioners to Provide Healthcare Using Telemedicine. 2020. [[Last accessed on 2023 Sep 11]]. Available from: https://www.mohfw.gov.in/pdf/Telemedicine.pdf .


