Abstract
Introduction and importance:
When compared to other cranial nerve palsies idiopathic unilateral oculomotor nerve palsy with pupillary sparing is one of the least noted neurological conditions. Moreover, there lies a series of diagnostic dilemmas to come into a final diagnosis resulting in several array of clinical investigations. Hence, there is a delay in prompt management.
Case summary:
An elderly female without any known comorbidities presented with the complaint of headache, dizziness and dropping of left eyelid. Several arrays of diagnostic workups was done to come to a diagnosis, but even with rigorous laboratory investigations and radiological examinations, a common working diagnosis could not be made. Hence with a diagnosis of exclusion after proper neurological and neuro-ophthalmological examination, idiopathic unilateral common oculomotor nerve palsy was identified for which improvement with steroids was noted in the patient.
Discussion:
Idiopathic unilateral complete oculomotor nerve palsy is considered as a diagnosis of exclusion when all the diagnostic parameters fail to signify and positive results. The vague symptomatic presentation of the disease condition further compels the treating physician to carry out several panels of laboratory to radiological investigations. But if identified in time the treatment modality is straightforward.
Conclusion:
The diagnostic quandary in timely identification of such disease conditions needs a pertinent diagnostic guideline so as to avoid the unwanted panel of investigations.
Keywords: cranial nerves, diagnostic quandary, idiopathic, oculomotor nerve palsy
Introduction
Highlights
Isolated cranial nerve III palsy is a common neurosurgical presentation. It can result from either congenital or acquired causes.
There lies a series of diagnostic dilemmas to come into a final diagnosis resulting in several array of clinical investigations.
Although recent advances in neuroimaging have made early diagnosis easier, management of patients with isolated cranial nerve III palsies still remains challenging.
The diagnostic quandary in timely identification of such disease conditions needs a pertinent diagnostic guideline.
Isolated cranial nerve III palsy is a common neurosurgical presentation. It can result from either congenital or acquired causes. Intrauterine infection and trauma during delivery are common congenital causes of oculomotor nerve palsy1. Acquired causes can be due to trauma, intracranial neoplasm, meningitis, encephalitis, cerebral artery aneurysm, and blockage of small vasculature in hypercoagulable states2. Overall the incidence of acquired third nerve palsy is also quite minimal with older age group and elderly demographic groups of people under high risk. However, in a few cases, the etiology remains hidden, and literature shows that such idiopathic cases are sporadic, and only a few case reports shed light on its occurrence. The reported incidence of such idiopathic cases is 12–14% in children, but data are lacking in terms of incidence in adults3. Diagnostic workup is demanding in such a way that an in-depth, comprehensive laboratory and radiological workup becomes mandatory so as to accurately pinpoint the correct diagnosis. Details regarding its diagnosis and treatment are lacking in the literature, and the management is thus individualized and depends upon the expertise of the treating physician4,5. Moreover, a controversy always exists regarding several arrays of diagnostic workups and lines of management, due to a lack of evidence-based guidelines. We here report a case of idiopathic unilateral cranial nerve palsy along with the diagnostic workup and a review of the literature. This case report has been written in line with Surgical Case Reports (SCARE) guideline6.
Case summary
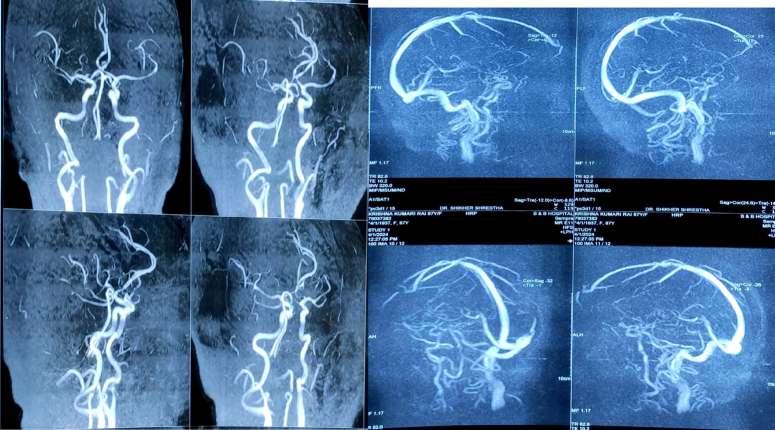
An 87-year-old female presented to the outpatient department with a complaint of headache since one week, which was insidious in onset, over left frontoparietal region sharp throbbing in type, pain non-progressive without any aggravating and relieving factors associated with left periorbital pain and mild dizziness which was non-rotatory in type and associated with few episodes of vomiting, non-projectile in nature, small in amount, not blood and bile mixed. The patient also complained of associated inability to open the left eye, restricted left eye movements, and diplopia. It developed since one week and was acute in onset, but the patients relatives noticed it a few days later. Initially, it was mild difficulty in opening the left eye but later progressively worsened over the past few days until the patient has severe difficulty opening the left eye. The patient had no any features suggestive of progressive fatigability over the course of the day. The patient had no history of trauma. Past medical and surgical history was non-significant. Clinical examination revealed left upper lid complete ptosis with pupillary sparing with impaired levator function, and anomalous eye movements when attempting elevation, depression, or adduction of the left eye in motility testing. (Table 1) Ptosis was associated with pain and tearing in the left eye periodically. (Fig. 1) A detailed workup was performed: neurological and ophthalmological examination, blood pressure measurement, laboratory tests, and MRI of the brain,(Fig. 2)(Fig. 3) magnetic resonance venography (MRV), magnetic resonance angiography (MRA) of the brain(Fig. 4) of the brain was done. (see Table 4 for the diagnostic workup and the results). Basic laboratory tests consisted of complete blood count (CBC), blood chemistry, coagulation screening, inflammatory markers, urinalysis, fibrinogen degradation products (FDP), D-dimer. The patient’s routine laboratory examination was normal with no evidence of diabetes mellitus (DM), hyperlipidemia, inflammation, and infection.(Table 2) MRI was also unremarkable without intracranial mass lesions and acute infarction. The authors ruled out various possible underlying causes, including microvascular ischemia, aneurysm, trauma, neoplasm, inflammation, and neurosurgical intervention. The systemic review was unremarkable for any central nervous system (CNS), cardiovascular or systemic illness. No drug history or allergies were reported by the family.
Table 1.
Ophthalmological examination findings.
| Left eye | Right eye | |
|---|---|---|
| Upper eyelid | Drooping until covering the limbus lid swelling |
Normal |
| Sclera | Normal | Normal |
| Cornea | Normal | Normal |
| Conjunctiva | Congested | Normal |
| Pupil size | 3mm, round | 3mm,round |
| Direct light reflex | Normal | Normal |
| Consensual light reflex | Normal | Normal |
| Accommodation reflex | Impaired | Normal |
| Fundus | Normal | Normal |
| Visual acuity | 6/6 | 6/6 |
| Medial movement | Restricted | Intact |
| Lateral movement | Restricted | Intact |
| Downward movement | Restricted | Intact |
| Upward movement | Restricted | Intact |
Figure 1.

Picture depicting left sided complete ptosis.
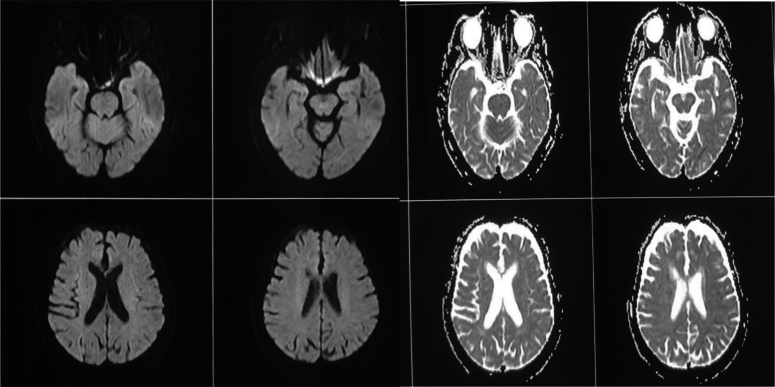
Figure 2.
MRI brain ADC and DWI sequence suggestive of no any gross abnormality in the brain. ADC, apparent diffusion coefficient; DWI, diffusion weighted imaging.
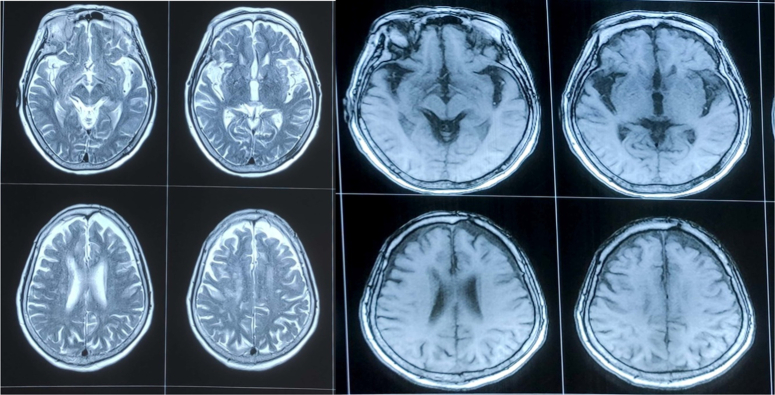
Figure 3.
MRI brain T2 and FLIAR axial section suggestive of no any gross abnormality in the brain parenchyma. FLIAR, fluid attenuated inversion recovery.
Figure 4.
Magnetic resonance angiography and magnetic resonance venography of brain suggestive of normal findings hence excluding chances of aneurysm and cerebral venous sinus thrombosis in the patient.
Table 4.
The results of diagnostic workup for cranial nerve III palsy.
| Underlying cause | Diagnostic test | Results |
|---|---|---|
| Inflammatory and paraneoplastic process | Lumbar puncture | Normal |
| Intracranial mass lesions and acute infarction | MRI brain and orbits | Unremarkable |
| Diabetes | HbA1C | Normal |
| Inflammatory process or infection | CBC and inflammatory markers | Normal |
| Aneurysm | MRA | Unremarkable |
| trauma and neurosurgical intervention | MRI, CT and past history | Unremarkable |
| Alcohol | Urinalysis | Negative |
CBC, complete blood count; CT, computed tomography; MRA, magnetic resonance angiography.
Table 2.
Initial laboratory investigations.
| Investigation | Result | Unit | Reference range |
|---|---|---|---|
| Hemoglobin | 12.1 | g/dl | 13–17.5 |
| White blood cell count | 7800 | Cells/mcl | 4500–11 000 |
| Red blood cell count | 348 000 | Cells/mcl | 450 000–600 000 |
| Platelet count | 225 000 | Cells/mcl | 150 000–450 000 |
| Mean corpuscular volume | 76 | Fl | 80–100 |
| Mean corpuscular hemoglobin concentration | 32.2 | g/dl | 32–36 |
| RDW | 47.4 | % | 12–16 |
| CRP | 21 | ||
| Blood random sugar | 96 | mg/dl | 80–126 |
CRP, C reactive protein: RDW, red cell distribution width.
An ophthalmological examination was done, and findings have been shown in Table 1.
Initial laboratory investigation including complete blood count, C reactive protein, and blood random sugar was unremarkable, as shown in Table 2.
MRI brain has been ordered for intracranial anomalies reporting no obstructive lesion in the orbit and anterior cranial fossa as given in (Figs. 2, 3)
Further tests were ordered for hypercoagulability and systemic illness and the results have been shown in Table 3.
Table 3.
Hypercoagulability and systemic illness results.
| Investigation | Result | unit | Reference range |
|---|---|---|---|
| ANA | 1:40 (negative) | ||
| Protein C | 124.1 | % | 72–160 |
| Protein S | 81.7 | % | 60–150 |
| Antithrombin 3 | 96 | % | 80–120 |
| Factor V laden mutation | Negative | ||
| Fibrinogen degradation product (FDP) | >160 <320 | Ug/ml | <5.0 |
| D-dimer | 0.4 | Mg/l | 0-0.50 |
ANA, anti nuclear antibody.
Despite the detailed history and laboratory workup, the exact cause of the disease remained unknown, and the condition has been labeled as idiopathic unilateral cranial nerve palsy. The recommended therapy was steroid treatment. The patient, therefore, received intravenous methylprednisolone 1 gm once a day for total of 5 days then patient was discharged on oral corticosteroid (DEFLACORT) 60 mg once a day with tapering for 2 weeks. After diagnosis and symptomatic improvement patient was discharged after 10 days, during discharge there was significant improvement in diplopia, angle of squint, ocular movement and mild improvement in ptosis(Fig. 5) and the patient was instructed for regular follow-up.
Figure 5.

Picture representing mild improvement of left sided ptosis after IV steroids.
Discussion
Idiopathic unilateral third nerve palsy and it’s diagnosis and management has always been a matter of dilemma in terms of the right choice of investigation and line of management. Moreover several factors could be the possible causation leading to the condition, even the third nerve’s innate anatomy. The third cranial nerve also known as oculomotor nerve and has two major components: -Outer parasympathetic fibers that supply the ciliary muscles and the sphincter pupillae-Inner somatic fibers that supply the levator palpebrae superioris in the eyelid (which retracts the upper eyelid) and the four extra-ocular muscles (superior, middle, inferior recti, and inferior oblique)7. The nerve fibers leave the midbrain through the most medial part of the cerebral peduncle and enter the interpeduncular cistern. After the oculomotor nerve emerges from the interpeduncular fossa, it enters the cavernous sinus slightly lateral and anterior to the dorsum sellae. It enters the orbit through the superior orbital fissure, after exiting the cavernous sinus, to innervate the extra-ocular muscles7. Third, the cranial nerve’s long course through important anatomical landmarks can also be a potential hidden factor in many cases where the definitive cause has not been noted out despite rigorous diagnostic workup7,8. The age- and sex-adjusted annual incidence of acquired third nerve palsy was 4.0 per 100 0008. The annual incidence in patients older than 60 was greater than patients younger than 608. Available studies have shown that the most common causes of acquired third nerve palsy were presumed microvascular (42%), trauma (12%), compression from neoplasm (11%), post-neurosurgery (10%), and compression from aneurysm (6%). Along with it Ten patients (17%) with microvascular third nerve palsies had pupil involvement, while pupil involvement was seen in 16 patients (64%) with compressive third nerve palsies8. The lab workup for CNIII palsy involves obtaining blood pressure recordings, complete blood counts (CBC), HbA1C, erythrocyte sedimentation rate (ESR), and imaging studies using CT angiography (CTA) or MRI of brain, particularly if an aneurysm is suspected9. The evolution of new imaging techniques, such as computed tomography angiography and magnetic resonance angiography, have provided new imaging options for clinicians, which makes it easier to come to a final diagnosis10. While the use of MRI as an early diagnostic tool for isolated ocular nerve palsy remains controversial, a normal MRI obtained in patients who experience acute onset diplopia from isolated ocular motor palsy may help to allay anxiety and fears of brain tumor or other serious disease, which in turn may have significant social, psychological and even economic benefit in terms of productivity. This value is, however, inherently subjective and difficult to measure11. The diagnosis and management of third nerve dysfunction varies according to the age of the patient, characteristics of the third nerve palsy, and presence of associated symptoms and signs. Indeed, third nerve palsies may be partial or complete, congenital or acquired, isolated or accompanied by signs of more extensive neurological involvement. Depending upon the types the depth of investigations and management may vary. They can result from lesions located anywhere from the oculomotor nucleus to the termination of the third nerve in the extra-ocular muscles within the orbit12. Despite recent advances in modalities such as noninvasive neuroimaging, which facilitate early diagnosis; however, management of a patient presenting with an isolated third nerve palsy remains a challenge due to the lack of any obvious peculiar findings that may help to guide towards the diagnosis12. Oculomotor nerve palsy lacks any significant morbidity or life-threatening complications but still globally, viewed as a diagnostic concern in clinical practice due to its nature of hampering the quality of life of the patient13. Literature has also shown that there are also some untypically causes, such as schwannoma, meningioma, and radiation, which may also lead to Oculomotor Nerve Palsy13; however, despite appropriate imaging studies, clinical examination and laboratory workup and no any significant radiation history there is no such evidence of atypical pathophysiology in our case.
Although recent advances in neuroimaging have made early diagnosis easier, management of patients with isolated cranial nerve III palsies still remains challenging. Recommended treatment options vary according to the etiologies. For example, the treatment of palsies with vascular causes largely centers on supportive therapy (i.e. eye patching and prism therapy). In contrast, patients with idiopathic cranial nerve III palsies have been reported to respond well to steroid treatment and to have good prognosis14. Unilateral oculomotor palsy is more difficult to localize particularly if it is isolated with no other signs. However, unilateral oculomotor palsy with other long tract involvement indicates a fascicular lesion. Varying manifestations can be seen based on the course of the nerve as it crosses the red nucleus, superior cerebellar peduncle, substantia nigra, and cerebral peduncle, thus resulting in various syndromes15. Moreover evidence-based guidelines should be developed so as to accurately and on time diagnosis of such idiopathic causes of third nerve palsy so as to start treatment early and improve the quality of life of the patient’s.
Conclusion
Neurological conditions such as idiopathic complete oculomotor nerve palsy is a diagnosis of exclusion hence the diagnostic dilemma. Moreover, the treatment modality is not that tedious and quite straightforward along with significant improvement among the patients after prompt treatment. However, there is the utmost need of the utilization of several arrays of clinical to radiological investigations to come to a diagnosis as seen in our case (Table 4) where an in-depth diagnosis workup is mandatory.
Ethical approval
Ethical approval is exempted in case of case reports in our Institution. Whereas written informed consent have been taken from patient herself.
Consent
Written informed consent has been taken from the patient herself and can be made available if asked upon by chief editor.
Source of funding
No any funding was needed in writing of this article.
Author contribution
S.G., K.B.: conceptualization; data curation; formal analysis; methodology; project administration; supervision; writing—review and editing. K.B. : data curation; S.S., D.S., K.R., S.B.: project administration; supervision.
Conflicts of interest disclosure
The authors declare no conflicts of interest.
Research registration unique identifying number (UIN)
No clinical trials were conducted. Information was obtained from patient after written informed consent.
Guarantor
Sagun Ghimire.
Data availability statement
The dissemination of the article data is freely accessed.
Provenance and peer review
This entitled paper was not invited.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 30 August 2024
Contributor Information
Sagun Ghimire, Email: sagunghimire01@gmail.com.
Shikher Shrestha, Email: shikhershrestha@gmail.com.
Dinuj Shrestha, Email: dinuj45@gmail.com.
Kajan Ranabhat, Email: kajan@gmail.com.
Suman Bhattarai, Email: suman.bhattarai@hotmail.com.
Kritick Bhandari, Email: bhandari@gmail.com.
Rikesh Kc, Email: rikesh@gmail.com.
References
- 1.Schumacher-Feero LA, Yoo KW, Solari FM, et al. Third cranial nerve palsy in children. Am J Ophthalmol 1999;128:216–221. [DOI] [PubMed] [Google Scholar]
- 2.Khan QA, Adnan S, Ahmad N, et al. Idiopathic unilateral third nerve palsy with pupillary sparring in 10-year-old child -a case report. Ann Med Surg (Lond) 2022;82:104723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mitchell J, Fuhrman S, Gersh DB. A case of idiopathic unilateral oculomotor nerve palsy with good outcome. Vet Radiol Ultrasound 2019;60:755. [DOI] [PubMed] [Google Scholar]
- 4.Kanazawa T, Hino U, Kuramae T, et al. Idiopathic unilateral oculomotor nerve palsy: a case report. Heliyon 2020;6:e05651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park KA, Oh SY, Min JH, et al. Acquired onset of third, fourth, and sixth cranial nerve palsies in children and adolescents. Eye (Lond) 2019;33:965–973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sohrabi C, Mathew G, Maria N, et al. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg Lond Engl 2023;109:1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park HK, Rha HK, Lee KJ, et al. Microsurgical anatomy of the oculomotor nerve. Clin Anat 2017;30:21–31. [DOI] [PubMed] [Google Scholar]
- 8.Fang C, Leavitt JA, Hodge DO, et al. Incidence and etiologies of acquired third nerve palsy using a population-based method. JAMA Ophthalmol 2017;135:23–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Modi PA, Arsiwalla T. Cranial Nerve III Palsy. StatPearls Publishing; 2020. [PubMed] [Google Scholar]
- 10.Lee AG, Hayman LA, Brazis PW. The evaluation of isolated third nerve palsy revisited: an update on the evolving role of magnetic resonance, computed tomography, and catheter angiography. Surv Ophthalmol 2002;47:137–157. [DOI] [PubMed] [Google Scholar]
- 11.Tamhankar MA, Biousse V, Ying GS, et al. Isolated third, fourth, and sixth cranial nerve palsies from presumed microvascular versus other causes: a prospective study. Ophthalmology 2013;120:2264–2269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Biousse V, Newman NJ. Third nerve palsies. Semin Neurol 2000;20:55–74. [DOI] [PubMed] [Google Scholar]
- 13.Tian G, Kardon R, Feng C, et al. Oculomotor nerve palsy due to unusual causes. J Neuroophthalmol 2021;41:e244–e250. [DOI] [PubMed] [Google Scholar]
- 14.Park KA, Min JH, Oh SY, et al. Idiopathic third and sixth cranial nerve neuritis. Jpn J Ophthalmol 2019;63:337–343. [DOI] [PubMed] [Google Scholar]
- 15.Schmidt D. Die klassischen Hirnstammsyndrome. Definitionen und Geschichte [Classical brain stem syndrome. Definitions and history]. Ophthalmologe 2000;97:411–417. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dissemination of the article data is freely accessed.