Abstract
Valve-sparing aortic root replacement is not widely performed due to technical requirements. The Florida sleeve technique (FST) is a new technique for aortic root remodeling with the preservation of the aortic valve without aortic root wall resection and coronary artery reconstruction. We successfully treated with the FST for a Marfan syndrome patient with an aortic root aneurysm and aortic valve insufficiency. We believe that this technique is very suitable for cases with moderately enlarged aortic roots. It could reduce surgical risks and prevent dilatation of the aortic root through coverage with a graft for a long time.
Keywords: aortic valve sparing, Marfan syndrome, Florida sleeve
Introduction
Surgical techniques for aortic root dilatation combined with aortic valve insufficiency (AI) include conventional root replacement (Bentall operation) and valve-sparing aortic root replacement (VSARR), remodeling (Yacoub procedure), or reimplantation (David procedure).1,2) Although VSARR has been reported to show excellent results in selected patients, it is not widely performed because of the technical demands. Therefore, many surgeons still prefer the Bentall operation rather than VSARR for aortic insufficiency associated with aortic root aneurysms. VSARR is attractive, but these surgical techniques are delicate and depend on experience. After seeking to simplify the surgical procedure, the “Florida sleeve” technique (FST) was reported by the University of Florida as a new technique for VSARR that does not require total aortic root wall resection and coronary artery reconstruction.3) Preservation of the shape of the sinus of Valsalva and prevention of dilatation of the aortic annulus are necessary to obtain long-term durability. We report a case of Marfan syndrome associated with aortic root aneurysm that was successfully treated using FST.
Case Report
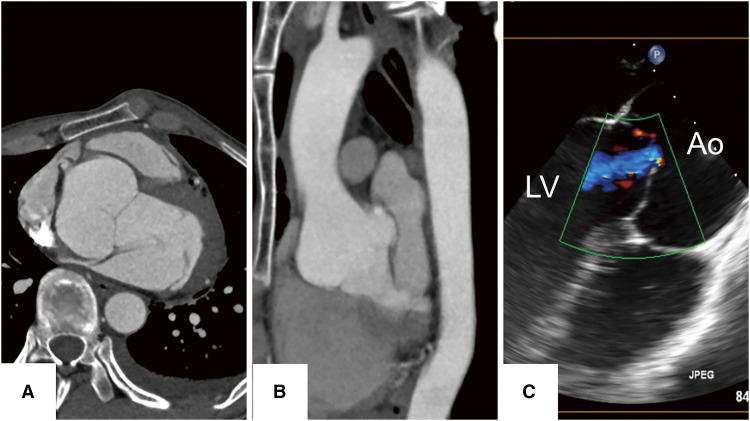
A 26-year-old man was admitted for the surgical treatment of a left spontaneous pneumothorax. He was tall and thin, with scoliosis and typical Marfanoid habitus (height 191 cm, weight 56 kg, BMI = 15.4). His past medical history revealed surgical therapy for right pneumothorax 10 years ago. Computed tomography (CT) revealed an aortic root aneurysm with measurements of the aortic annulus, Valsalva sinus, and sinotubular junction (STJ) being 33 mm, 52 × 55 mm, and 35 mm, respectively (Figs. 1A and 1B). It has dilated 14 mm compared to CT 10 years ago. He first underwent surgery for left pneumothorax. Preoperative echocardiography revealed an ejection fraction (EF) of 57.3%, with left ventricular diastolic and systolic dimensions (LVDd/Ds) measuring 48 mm and 34 mm, respectively. In addition, mild type I aortic regurgitation originating from the center, attributed to tethering associated with aortic root aneurysm, was observed (Fig. 1C). He was referred to our department for surgical management of aortic root aneurysm and AI found during a preoperative work-up for lung surgery. We diagnosed Marfan syndrome with aortic root enlargement combined with AI. Then, we performed aortic root surgery with the FST.
Fig. 1 Findings of preoperative examinations. (A) The axial image of the preoperative CT scan revealed a dilated sinus of Valsalva with a size of 55 mm, which dilated up to 14 mm per 10 years. (B) The sagittal image of CT showed a dilated Valsalva sinus. (C) Echocardiography showed aortic root enlargement and AI. At the end of the diastolic period, a central coaptation defect was observed. AI: aortic valve insufficiency; Ao: aorta; CT: computed tomography; LV: left ventricle.
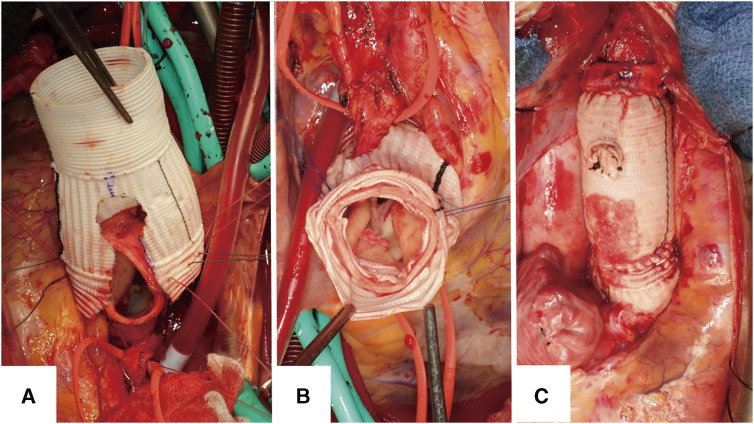
After establishing cardiopulmonary bypass (CPB) and aortic clamping, the cardioplegic solution was delivered in both an antegrade and a retrograde manner. The ascending aorta was transected above the STJ, the aortic root was mobilized to the aortic annular level, and the origins of the coronary arteries were mobilized. After measuring the aortic annular size (the 27 mm Hegar just passed the annulus) and geometric height (gH) of 20 mm, the target valve annulus diameter was established at 27 mm, and consequently, a graft upsized by 3 mm was selected for use. A 30-mm vascular graft (Gelweave Valsalva; Terumo Inc., Tokyo, Japan) was trimmed with two keyholes aligned with the height of the coronary orifice (Fig. 2A). Then, six anchoring sutures were made on the lowest level of the annulus at the commissure and midpoint of each leaflet to fix the wrapping graft. The sleeve graft was located at the aortic root, and a Hegar dilator was placed through the annulus into the left ventricle to prevent purse-stringing the annulus when the sutures were tied down. Then, resuspension sutures at the commissures are placed. A running horizontal mattress suture was employed at the level of the STJ, securing the aorta and the graft to a felt strip circumferentially (Fig. 2B). The aortic valve was confirmed for adequate coaptation of the leaflets with static saline testing. The new STJ was anastomosed to the distal ascending aorta to complete the Florida sleeve root repair (Fig. 2C). After CPB weaning, transesophageal echocardiography confirmed the morphology of the aortic root and elimination of regurgitation. Aortic clamping and CPB times were 213 and 270 minutes, respectively. Red blood cells were not needed; however, due to low fibrinogen and platelets, 4 units of FFP (Fresh Frozen Plasma) and 20 units of platelets were transfused. An additional movie file shows this in more detail (Supplementary Movie).
Fig. 2 Operative findings. (A) A “keyhole” was designed for the location of the coronary arteries. (B) The graft sleeve was secured underneath the coronary arteries. To achieve graft positioning below the coronary arteries, a horizontal mattress suture was placed on the base of the “keyhole”. (C) The graft from the ascending aorta and sleeve was sutured. This completes the Florida sleeve procedure.
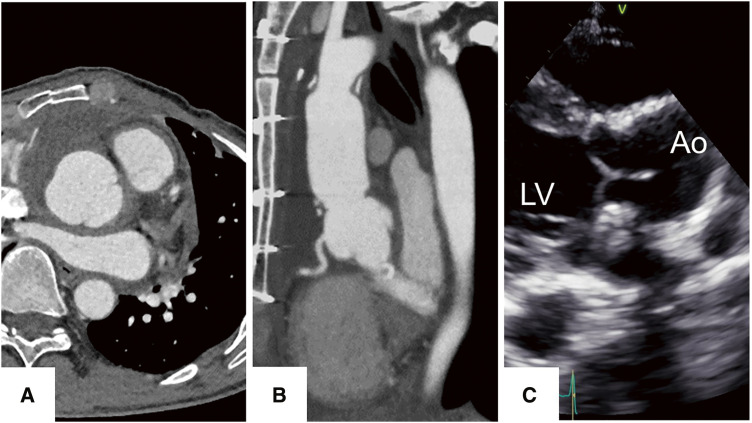
The postoperative course was uneventful, and CT and echocardiographic evaluations were performed a week after surgery. They demonstrated a competent aortic valve with no regurgitation, excellent coaptation height (9 mm) of the aortic valve, and a stable aortic graft without any distortion or leakage. Serial follow-up echocardiographic assessments were performed up to 1 year after surgery. The morphological changes in the aortic root were noted by comparing the imaging findings before surgery. CT showed a reduction of Valsalva from 55 to 39 mm and annulus from 32 to 28 mm (Figs. 3A and 3B). In the echocardiographic assessment, EF was 68.8%, with LVDd/Ds measuring 46 mm and 29 mm, respectively. Coaptation height and effective height were measured at 8 mm and 11 mm, respectively, and the annular diameter was 26 mm, with no AI observed (Fig. 3C).
Fig. 3 Findings of postoperative examinations. (A) The axial image of postoperative CT revealed the Valsalva sinus was an excellent form contained without a gap. The Valsalva diameter was reduced from 55 mm to 39 mm. (B) The sagittal image of CT showed no distortion and no stenosis of the bilateral coronary arteries associated with the covered graft. The annulus diameter decreased from 32 mm to 28 mm. (C) The postoperative echocardiography showed that the valve leaflets motion was not restricted and had adequate coaptation without regurgitation. Coaptation height and effective height were measured at 8 mm and 11 mm, respectively. Ao: aorta; CT: computed tomography; LV, left ventricle.
Discussion
VSARR has been established for aortic root dilatation with or without aortic valve regurgitation. In these operations, the wall of the sinus of Valsalva is usually resected, and the creation of a neoaortic sinus is necessary. The procedures involved in forming the proper shape of the sinus of Valsalva and precisely tailoring the graft are complex; therefore, this approach has technical challenges and a learning curve. Hess et al.3) described a new technique, the “Florida sleeve,” for aortic root remodeling. This valve-sparing technique involves protecting the aortic root with a Dacron graft sleeve without resection to preserve native tissue in place. The most important advantage of this technique is its technical simplicity, which eliminates the need for coronary artery reconstruction and greatly reduces the suturing of the Valsalva sinus. As a result, this technique can shorten the procedural time and reduce anastomotic bleeding (intraoperative complications). Therefore, it may be more easily reproducible than conventional VSARR. The coronary keyhole was created as previously described.3) We made it approximately 10mm in diameter to not interfere with the coronary origin. Gamba et al.4) also reported that keyholes were created approximately 1cm in diameter. There were no complications of coronary kinking or stenosis in either report.4,5) Because of its minimal invasiveness, this procedure is considered appropriate for elderly patients. Hess et al.5) reported that clinical and echocardiographic outcomes showed excellent results at mid-term follow-up. No patient needed reoperation or reintervention of the aortic valve, proximal coronary arteries, or ascending aorta. According to the authors, the reduction of the left ventricular dimension 3years after surgery suggested that FST is a durable valve repair approach.
The FST, however, has several potential drawbacks. Since the enlarged aortic sinus has to be inserted in a smaller graft, anatomical distortion of the aortic root can be created. The distortion between the residual aortic sinus and vascular graft can cause aortic insufficiency and coronary malperfusion, both of which can be fatal. Therefore, extreme caution should be taken while tailoring the artificial graft and anchoring it to the native aortic wall. The coronary ostium should also be positioned as carefully as possible to prevent kinking or obstruction of the origins of the coronary artery. Although, in the present case, the enlargement of the sinus of Valsalva was not very severe, considering that the patient had Marfan syndrome, there was a very high likelihood of further deterioration of the aortic root, necessitating relatively early surgical intervention. We suggest that FST is a good indication of this degree of Valsalva morphology change. However, as David commented,6) FST for severe enlargement is expected to distort the aortic wall, so VSARR is preferred. We believe that this technique is highly suitable for cases with moderately enlarged Valsalva sinus diameters of 55–60 mm accompanied by concentric regurgitation jets. When a root aneurysm is >6 cm, redundant tissue could create turbulent flow in the remodeled aortic root, which may reduce the durability of the sleeve technique.
The FST is associated with encouraging results in Marfan syndrome patients with aortic root aneurysms. Aortic root aneurysm is common in patients with Marfan syndrome, and the University of Florida has been using FST in these patients since the procedure was first developed. However, some surgeons have concerns about the long-term durability and dimensional stability of this repair and about the potential need for reoperation in these patients. The FST provides more physiologic-like aortic wall stress and might prolong durability.7) A retrospective study showed that the FST is a viable option for patients with Marfan syndrome with a significant reduction in aortic insufficiency grade postoperatively, and the survival rate and freedom from reoperation were 94% and 100% at 8 years, respectively.8) Although the FST has been applied in cases with Valsalva dimensions greater than 60 mm, it should be considered cautiously as a treatment option due to the limited long-term data available. We hope that our report will lead to the indications for FST in limited patients with Marfan syndrome and may allow preservation of the native aortic valve without experiencing an aortic event.
Conclusion
In conclusion, we report a Marfan patient with an aortic root aneurysm combined with AI who was successfully treated with FST. The FST is a promising surgical option for Marfan patients who need aortic root repair. It offers many advantages, such as preservation of the native valve and a lower risk of complications and reoperation, but its long-term results are still under study. To further verify the feasibility and reproducibility of this new technique, experiences in a larger number of patients with long-term follow-up are needed.
Declarations
Acknowledgments
Not applicable.
Ethics approval and consent to participate
The Anjo Kosei Hospital IRB granted an exemption from requiring ethics approval.
Informed consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Author contributions
Study conception: SK
Data collection: SK
Investigation: SK
Manuscript preparation: SK
Funding acquisition: SK
Critical review and revision: all authors
Final approval of the article: all authors
Accountability for all aspects of the work: all authors.
Disclosure statement
The authors have no conflicts of interest.
Supplementary Materials
Operative video of the Florida sleeve technique.
References
- 1).Yacoub MH, Fagan A, Stassano P, et al. Results of valve conserving operations for aortic regurgitation. Circulation 1983; 68: 311–21. [Google Scholar]
- 2).David TE, Feindel CM. An aortic valve-sparing operation for patients with aortic incompetence and aneurysm of the ascending aorta. J Thorac Cardiovasc Surg 1992; 103: 617–21; discussion, 622. [PubMed] [Google Scholar]
- 3).Hess PJ Jr, Klodell CT, Beaver TM, et al. The Florida sleeve: a new technique for aortic root remodeling with preservation of the aortic valve and sinuses. Ann Thorac Surg 2005; 80: 748–50. [DOI] [PubMed] [Google Scholar]
- 4).Gamba A, Tasca G, Giannico F, et al. Early and medium term results of the sleeve valve-sparing procedure for aortic root ectasia. Ann Thorac Surg 2015; 99: 1228–33. [DOI] [PubMed] [Google Scholar]
- 5).Hess PJ Jr, Harman PK, Klodell CT, et al. Early outcomes using the Florida sleeve repair for correction of aortic insufficiency due to root aneurysms. Ann Thorac Surg 2009; 87: 1161–8; discussion, 1168-9. [DOI] [PubMed] [Google Scholar]
- 6).David TE. Aortic sinuses resection or external support to treat aortic root aneurysm? Oper Tech Thorac Cardiovasc Surg 2021; 26: 322–3. [Google Scholar]
- 7).Tasca G, Selmi M, Votta E, et al. Aortic root biomechanics after Sleeve and David sparing techniques: a finite element analysis. Ann Thorac Surg 2017; 103: 1451–9. [DOI] [PubMed] [Google Scholar]
- 8).Aalaei-Andabili SH, Martin T, Hess P, et al. Florida sleeve procedure is durable and improves aortic valve function in Marfan syndrome patients. Ann Thorac Surg 2017; 104: 834–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Operative video of the Florida sleeve technique.