Abstract
Backgroud
Conservative treatment of intra-articular lateral head fracture of the proximal phalanx (LHFPP) of the great toe in young children has a high rate of nonunion, leading to hallux valgus interphalangeus (HVIP). This study presents a case series of surgically managed, late-diagnosed LHFPP, highlighting the difficulties of the surgery and presenting satisfactory results.
Methods
Nine unilateral cases (8 late-diagnosed and 1 acute) were treated by open reduction and Kirchner wire fixation. The average time from trauma to surgery was 2.9 years (range, 0.5–10.1 years) in our late-diagnosed cases. The average age at the time of operation was 9.2 years (range, 3.4–16.3 years). The causes of injury were various. Intraoperative findings were reviewed through medical records and photographs. Pre- and postoperative HVIP angle, American Orthopedic Foot and Ankle Society (AOFAS) score, and range of motion of the interphalangeal joint were measured and compared statistically.
Results
Progressive HVIP was a chief complaint in all 8 late-diagnosed cases. Bony fragment size depended on the time elapsed after trauma (fragments increased in size due to ossification of cartilage) with a mean of 23.5% articular involvement. Four cases required bone graft, and union was achieved in all cases. The mean HVIP angle improved from a mean of 17.8° to 10.5°. The average AOFAS score and range of motion were significantly improved after surgery.
Conclusions
Although LHFPP is rare and difficult to diagnose, even cases detected long after the initial trauma can be successfully treated, albeit with difficulty. All 9 of our patients had successful outcomes when treated by open reduction and internal fixation.
Keywords: Pediatric toe fracture, Great toe intra-articular fracture, Delayed diagnosis, Treatment outcome
Phalangeal fractures account for approximately 18% of pediatric foot fractures,1,2) but intra-articular fractures of the phalanges are rare.3,4,5) In the great toe, most intra-articular fractures of the proximal phalanx are located proximally (base fractures). Distal head fractures are rare. The incidence of the latter and its biomechanical causes have not been well studied, but reports included various sports activities, impact from heavy objects, and collision with walls or vehicles.6,7,8)
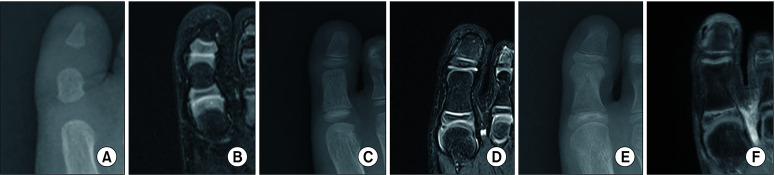
The lateral head fracture of the proximal phalanx (LHFPP) involving cartilage occurs more often than the medial head fracture. It is frequently misdiagnosed as a contusion or sprain and treated conservatively. The main reason for these errors is the rarity of this fracture and the mild to moderate symptoms. In addition, fracture fragments that are mostly cartilage with a tiny bony component are not evident in radiographs. Initially, the head of the proximal phalanx is mainly cartilage, but it is gradually ossified beginning as early as 1.5 to 2 years of age and fully replaced by bone and develops a mature articular surface around age 8 (Fig. 1).9,10) Therefore, LHFPP should be dealt with very carefully because it has a high incidence of nonunion, subsequent toe deformity, and decreased joint motion when not adequately treated.
Fig. 1. A series of radiographs and magnetic resonance imaging (MRI) images of the great toe in normal children. (A-F) The changes of the cartilaginous epiphyseal (base) and non-epiphyseal (head) end of the proximal phalanx with age (MRI images with 3-year age gap were from the MRI data pool at our institution, which clearly show both metatarsophalangeal and interphalangeal joint cartilages). A radiograph of the right great toe (A) and corresponding T2-weighted MRI image (B) in a 2-year-old boy showing a hyperintense, transverse physis of the proximal epiphyseal end and curved physis of the distal non-epiphyseal end in the MRI image. Before epiphyseal ossification, both ends were capped by unossified hyaline cartilage, the chondroepiphysis. A radiograph of the right great toe (C) and corresponding T2-weighted MRI image (D) in a 5-year-old boy showing the secondary ossification center in the proximal epiphyseal end and its endochondral bone growth in the MRI image. At the distal non-epiphyseal end, bone formation occurred as a direct central extension from the metaphysis. This process began as early as 2 years of age. The MRI shows chondroepiphysis remaining on the medial and lateral corners. (E) A radiograph of the right great toe and corresponding T1-fat suppression (contrast enhanced) MRI image. (F) In an 8-year-old boy, the secondary ossification center continued to fully replace the epiphyseal cartilage and did not contribute much to bone elongation. The nonepiphyseal end was also fully replaced by bone and the distal physis was no longer visible.
Numerous complications have been observed even in the early surgical treatment of LHFPP, including nonunion (the most common) necessitating revision surgery, Kirschner wire (K-wire) migration, re-displacement of the fragment, avascular necrosis of the fragment, and arthritis of the joint.6,7,8,11) Therefore, delayed surgery for LHFPP may produce more complications and worsen the final outcomes. The purpose of this study was to present satisfactory surgical outcomes in a case series of late-diagnosed LHFPP, highlighting the inherent difficulties in initial diagnosis and surgical treatment.
METHODS
Institutional Review Board approval was obtained for this retrospective study (Pusan National University Hospital, IRB No. 2307-013-129). From 2010 to 2022, we treated 9 cases of LHFPP (8 late-diagnosed and 1 acute) by open reduction and K-wire fixation (Table 1). There were 5 girls and 4 boys with a mean age of 9.2 years (range, 3.4–16.3 years) at the time of surgery. Hallux valgus interphalangeus (HVIP) was the chief complaint in all 8 late-diagnosed cases. The fractures were initially misdiagnosed and treated conservatively at the primary clinic (n = 7) or unrecognized by the patient and untreated (n = 1). The cause of injury was pedestrian injury in 2 patients, hitting a wall in 2, kicking during Taekwondo in 2, combined with ankle sprain in 1, dropping a heavy item in 1, and unclear in 1. We used the digital tools available in picture archiving and communication system (PACS) to measure the bony fragment size and displacement distance in radiographs. The mean size of the fragment was 15.7 mm2 (range, 1.6–40.1 mm2). The mean displacement gap of the fragment was 1.8 mm (range, 0.4–3.7 mm). The articular defect was measured on radiographs as a percentage of total articular surface width. The mean ratio of articular involvement was 23.5% (range, 20.3%–28.3%). Fragments were detached from the lateral corner of the head including the plantar and dorsal articular surface in 8 of 9 cases. In case 3, it was detached from the lateral-plantar corner with a lower HVIP angle.
Table 1. Patient Data.
| Case | Sex | Affected side | Cause of injury | Age at | Surgical delay (duration) | FU period after surgery (yr) | HVIP angle (°) | Bony fragment size (mm2) | Bony displacement gap (mm) | Articular defect (%) | Bone graft | Other intraoperative procedure | AOFAS score | ROM(°) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Injury (yr) | Surgery (yr) | Affected side | Unaffected side | Preop | Last | Preop | Last | ||||||||||||
| Preop | Last FU | ||||||||||||||||||
| 1 | M | Lt | W/ankle sprain | 2.9 | 3.4 | 0.5 yr | 3.8 | 13.6 | 6.2 | 7.3 | 1.7 | 2.1 | 20.4 | Yes | 85 | 90 | 50 | 70 | |
| 2 | F | Lt | Pedestrian injury | 4.4 | 5.2 | 0.8 yr | 8.9 | 11.3 | 8.1 | 8.7 | 1.6 | 0.4 | 20.3 | 78 | 88 | 80 | 80 | ||
| 3 | F | Lt | Dropping heavy item | 2.9 | 5.1 | 2.2 yr | 1.0 | 12.7 | 9.6 | 9.2 | 11.4 | 1.9 | 27.1 | 77 | 95 | 55 | 70 | ||
| 4 | F | Lt | Pedestrian injury | 9.1 | 9.1 | 3 day | 10.9 | 10.4 | 6.5 | 7.2 | 19.7 | 0.9 | 20.6 | 75 | 100 | 30 | 80 | ||
| 5 | M | Rt | Kicking (Taekwondo) | 5.3 | 9.4 | 4.1 yr | 8.8 | 28.0 | 8.1 | 12.4 | 10.3 | 1.8 | 22.4 | 75 | 93 | 50 | 80 | ||
| 6 | F | Rt | Kicking (Taekwondo) | 8.4 | 9.5 | 1.1 yr | 8.8 | 14.3 | 9.5 | 12.1 | 4.5 | 3.7 | 28.3 | Yes | 75 | 95 | 45 | 80 | |
| 7 | M | Rt | Hitting a wall | 10.1 | 11.4 | 1.3 yr | 5.7 | 15.5 | 11.2 | 10.2 | 18.4 | 1.6 | 22.7 | 78 | 100 | 60 | 80 | ||
| 8 | M | Rt | Hitting a wall | 3.3 | 13.4 | 10.1 yr | 4.5 | 26.8 | 14.9 | 13.4 | 33.6 | 1.5 | 24.3 | Yes | 75 | 100 | 80 | 80 | |
| 9 | F | Rt | Unclear | Unknown | 16.3 | Unknown | 1.5 | 27.3 | 20.5 | 21.5 | 40.1 | 1.9 | 25.1 | Yes | Akin osteotomy | 79 | 95 | 55 | 70 |
| Mean | 5.8* | 9.2 | 2.9 yr† | 6.0 | 17.8 | 10.5 | 11.3 | 15.7 | 1.8 | 23.5 | 77.4 | 95.1 | 56.1 | 76.7 | |||||
FU: follow-up, HVIP: hallux valgus interphalangeus, Preop: preoperative, AOFAS: American Orthopedic Foot and Ankle Society, ROM: range of motion, Lt: left, Rt: right.
*Mean of 8 patients (except case 9). †Mean of 7 old cases (except case 4-acute and case 9-unknown).
The average time from trauma to surgery in 7 late-diagnosed cases was 2.9 years (range, 0.5–10.1 years). One late-diagnosed case did not have a known trauma history. The mean follow-up period after surgery was 6.0 years (range, 1.5–10.9 years). Intraoperative findings were reviewed through operation notes and photographs taken during surgery. Medical records were reviewed to identify the cause of trauma, time from initial injury to surgery, and complications. Available magnetic resonance imaging (MRI) and computed tomography images were additionally reviewed for detailed information.
HVIP angle was measured in standing anteroposterior views of the foot taken before surgery and at the last follow-up. The pre- and postoperative American Orthopedic Foot and Ankle Society (AOFAS) scores and range of motion of the interphalangeal joints using a short arm universal goniometer were also evaluated. The Wilcoxon signed-rank test was used for statistical analysis. Values of p < 0.05 were considered statistically significant.
Surgical Procedures
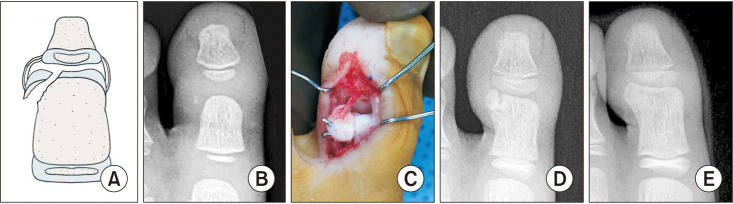
We used a lateral longitudinal incision over the fragment in the interphalangeal joint and a dorsal approach to the neurovascular structures. Neurovascular structures running laterally along the incision were carefully protected during the entire procedure. The interphalangeal joint was reached from its dorsolateral aspect. After confirming the exact location of the fragment, careful dissection was performed to find the attached lateral collateral ligament to the fragment. However, this was not successful in the late-diagnosed cases. In all 8 of our late-diagnosed cases, the fragments were freely detached from the adhered soft tissues during dissection. The detached fragments were round and larger than the defects due to ossification and were covered with fibrous tissues.
The first step was to find the articular surface of the fragment. As the fractures were diagnosed late, recognition of the articular surface was difficult due to the covering fibrous tissues. The bony part was often identified under C-arm fluoroscopy. We tried to find the most congruent articular part of the fragment, matching the articular surface of the defect. The articular surface of the fragment also needed to be congruent with the proximal articular surface of the distal phalanx. The opposite side of the articular surface of the fragment and the defect of the lateral head where the fragment would be seated were carefully debrided with a No. 10 or 11 surgical blade, curettes, and small rongeur and ground down with a carbide burr until the cancellous bone was exposed. Cancellous bone in the fragment was preserved as much as possible to avoid fibrous union because a large portion of the fragment was composed of cartilage in young children. We strove to achieve bone to bone contact between the defect and the fragment and to make a congruous articular surface to support the articular surface of the distal phalanx. Careful carving of the fragment to fit the defect was essential. The indication for bone graft was (1) when the fragment’s articular surface was lower than the level of the original articular surface, (2) when nonunion was a concern due to a large bone defect after debridement in the detached site, or (3) when there was insufficient cancellous bone remaining in the fragment on the side opposing the defect. We preferred iliac bone as a donor rather than any other site based on our belief in more active osteogenesis in the former, but other sources might also be suitable.
After confirming satisfactory reduction, the fragment was fixed with K-wires. The first K-wire was carefully inserted into the fragment while allowing room for a second one. We used small K-wires (0.9 mm, 1.0 mm, and 1.1 mm) according to the fragment size. At least 2 K-wires were inserted into the fragment to minimize movement and provide stability. These were cut and bent on the insertion side and impacted at the ends with a small impactor and mallet so that the opposite ends would not protrude and irritate the soft tissues and skin. The bent end of each K-wire was buried under the skin. Although some physicians leave the bent tip of the K-wire outside of the skin on the opposite side to avoid skin incision upon removal, we felt that this might allow slippage of the fragment from the K-wire tips on the insertion side, resulting in nonunion. Thus we preferred to keep the K-wires under the skin until bony union was confirmed.
K-wire removal after union was accomplished in all patients with gentle dissection around the united fragment under general anesthesia in the operation room. Although strict radiological bone union means the absence of a fracture gap, we considered a partial bony bridge between the fixed fragment and the main body of the phalanx to be in a state of bony union. Clinically all patients showed no symptoms during vigorous motion of the great toe before and after K-wire removal.
RESULTS
The data in Table 1 show that the mean HVIP angle, AOFAS score, and range of motion of the affected side were all significantly improved after surgery. Bony union was achieved after a mean of 12 weeks (range, 8–20 weeks). Case 1 (3-year-old boy) had fibrous union on the medial side of the fragment until 3 years after surgery, while the proximal side had bony union (Fig. 2A-D). Four years after surgery, a radiograph showed complete bony union on both sides (Fig. 2E). Case 9 (16-year-old girl) underwent an Akin type medial closing osteotomy simultaneously in the proximal phalanx to obtain the same HVIP angle with the unaffected side. In this girl, open reduction of the fragment alone could not produce the same HVIP angle as on the unaffected side due to excessive lateral tilting of the articular surface of the head. There were no complications such as neurological issues and avascular necrosis of the fragment.
Fig. 2. (A) Schematic drawing of a lateral head fracture of the left great toe showing the fragment attached to the capsule and lateral collateral ligament (LCL). (B) Case 1: anteroposterior radiograph of the left great toe in a 3-year-old boy, taken 6 months after hitting a wall, showing a tiny bony fragment (diameter about 1 mm) on the lateral side of the distal head. He was brought to our clinic because of increasing hallux valgus interphalangeus. (C) During surgery, we found that the cartilaginous portion was larger than we had envisioned (7 mm × 3 mm). It was easy to misdiagnose the fracture because the fragment was mostly cartilage. The bone fragment was flipped by the LCL and it was hard to find the cancellous bone portion. It was necessary to grind the opposite side of the LCL attachment surface to expose the cancellous bone and then to fix it using 2 Kirchner wires with iliac bone graft. (D) A radiograph taken 3 years after surgery showing the bony portion of the fragment had enlarged by ossification. Although the medial side of the fragment showed fibrous union, maintenance of the articular surface was satisfactory due to bony union on the proximal side where iliac bone graft was used. The hallux valgus did not worsen after surgery. (E) A radiograph taken 4 years after surgery showing complete bony union on both sides.
DISCUSSION
In children, intra-articular fractures of the proximal phalanx of the great toe are rare,3,4,5) and those that occur are mostly proximal, where the physis is located. As the child nears skeletal maturity, the proximal physis is more susceptible to mechanical failure as it thickens while the periosteum and perichondrium are thinner and provide less support against external forces.12) Thus external forces can cause the mobile great toe to hinge on the fixed metatarsophalangeal joint by multiple ligaments and muscles, resulting in intra-articular base fracture of the proximal phalanx.7,13,14)
On the other hand, distal head fracture is much less often reported6,7,8,11) and mostly occurs in the lateral head. The head of the proximal phalanx is capped by unossified hyaline cartilage and the cartilage is replaced by bone following the central bony extension from the metaphysis as early as 2 years of age.9,10) This process continues with cartilage remaining on the medial and lateral corner of the head around age 6, which is fully replaced by bone and finally completes articular cartilage around age 8 years. We believe that the curved shape of the distal physis and anatomical changes of distal cartilage along central bone extension from the metaphysis with cartilage remaining on the medial and lateral corner of the head may contribute to LHFPP. In our MRI study, the head of the proximal phalanx was finally completed on both corners showing a matured shape of articular cartilage around age 8 to 10 (Fig. 1). Abduction external forces, more frequently applied in the great toe than adduction forces in daily activities, imply that LHFPP is caused mainly by hyperabduction and rotational forces on the anatomically weak cartilaginous lateral corner of the head by compression forces acting upon it.
Patients with more common proximal base fractures present moderate to severe pain, hallux valgus deformity, and functional limitations. However, in the case of LHFPP, there is mild to moderate pain and less functional limitation initially, making early diagnosis difficult. The patients then must seek help for progressively worsening HVIP after primary treatment administered for contusion or sprain. Often the bone fracture is not clear in radiographs when the metaphyseal fragment is tiny, as also occurs in fractures of the elbow in young children. Pain and swelling after trauma in the interphalangeal joint, and tenderness especially on the lateral side of the head, should alert the physician to suspect LHFPP and perform further evaluation with ultrasonography or soft-tissue radiography. As LHFPP is an intra-articular Salter-Harris type III or IV fracture, open reduction and internal fixation is absolutely indicated because the fragment is purely cartilaginous or a cartilaginous fragment with a tiny metaphysis.
Kay and Tang2) recommended operative intervention for fractures that involve > 25% of the articular surface or with displacement > 2 mm. However, in our series, radiographs were not sufficient to characterize the initial fractures. Although we agree with these criteria in mild cases of basal fracture of the proximal phalanx, we believe that when a child is diagnosed with LHFPP, the physician should always intervene surgically due to the high incidence of nonunion, regardless of the above criteria. As the distal head is mainly cartilaginous before ossification starts, it is difficult to accurately measure the size and displacement gap of the bone fragments in initial radiographs. Park et al.8) also emphasized that LHFPP has a high risk of nonunion and treatment should rely on surgery. In their cases of nonunion, the size of the fragment was less than one third of the joint surface width and smaller fragments had a higher likelihood of nonunion.
Conservative treatment such as a splint, boot, and cast shoe was initially performed in 7 of the 8 late-diagnosed cases at their primary hospitals, except 1 who did not recognize the fracture (case 3). But eventually, all of these cases (including the unrecognized one) required surgical treatment for nonunion and progressively worsening HVIP. One of the limitations of this study is that we do not have reliable data about LHFPP healed with conservative treatment because our institution is a tertiary university hospital, and the majority of our patients are transferred from primary and secondary hospitals. But in consideration of Salter Harris type III or IV fracture pattern in LHFPP and mostly cartilaginous small fragments, we strongly recommend open reduction and internal fixation in all acute cases. Regarding the incidence of LHFPP in our institution, we had 9 cases among 231 great toe injuries during a 12-year study period, but 8 cases were transferred from other hospitals and only 1 came directly to our institution. Therefore, we cannot estimate the incidence of LHFPP.
Our cases with nonunion and toe deformity had a mean of 23.5% articular surface involvement leading to HVIP. Kim et al.11) reported that 13 of 16 cases with LHFPP (81.3%) showed HVIP. They did not clearly state the time from trauma to surgery but simply recommended operative treatment as soon as possible after the fracture occurs. This agrees with our belief that nonoperative treatment alone cannot heal the fracture.
The delay in surgical treatment made anatomical reduction difficult and necessitated the removal of surrounding soft tissues and grinding to expose cancellous bone or iliac bone graft to obtain stable bony union. Surgical challenges also include restoring joint surface congruity while minimizing trauma to the articular cartilage of the small fracture fragment. The soft tissues attached to the bone fragment interfered with anatomical reduction. It was necessary to remove the soft tissues from the bone fragment to check the orientation of the fragment and manipulate it. Additionally, it was often difficult to maintain fixation properly because the bone fragment was so small.
Although other workers have used cannulated or headless screws for large-size fragments,11) we found it difficult to insert more than 2 or 3 small K-wires in small fragments we encountered. Moreover, if a K-wire is not inserted correctly the first time, the misplaced holes cause loosening of subsequent wire and prevent firm fixation. The small fragment size following debridement of surrounding soft tissues to expose cancellous bone in our late-diagnosed cases led us to prefer K-wires, rather than the screws, which other workers used in (more recent) acute cases.
For 4 of our patients, iliac bone graft was necessary to remedy a defect in the bony outline. Radiologic bone union was achieved in all cases within 3 months although it was not easy to identify due to the K-wires. Kim et al.11) reported 14 among 16 LHFPP had radiologic union 6 weeks after surgery.
Our patients were treated surgically almost 3 years on average after the initial trauma, but were still satisfied with the functional and cosmetic results with no complications. Therefore, delayed treatment does not preclude patient satisfaction. However, if appropriate treatment is performed soon after the fracture occurs, anatomical reduction of the joint can be achieved, the surgery is easier, and unnecessary bone graft and additional osteotomy for remaining HVIP after fragment fixation can be avoided. Even when diagnosis is delayed, LHFPP can be successfully treated by open reduction and internal fixation. However, the surgery is much easier by prompt diagnosis.
ACKNOWLEDGEMENTS
This work was supported by Pusan National University Research Grant (2019-0631-003).
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Mizuta T, Benson WM, Foster BK, Paterson DC, Morris LL. Statistical analysis of the incidence of physeal injuries. J Pediatr Orthop. 1987;7(5):518–523. doi: 10.1097/01241398-198709000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Kay RM, Tang CW. Pediatric foot fractures: evaluation and treatment. J Am Acad Orthop Surg. 2001;9(5):308–319. doi: 10.5435/00124635-200109000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Peterson CA, Peterson HA. Analysis of the incidence of injuries to the epiphyseal growth plate. J Trauma. 1972;12(4):275–281. doi: 10.1097/00005373-197204000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Pozarny E, Kanat IO. Epiphyseal growth plate fracture: Salter and Harris type V. J Foot Surg. 1987;26(3):204–209. [PubMed] [Google Scholar]
- 5.Peterson HA, Madhok R, Benson JT, Ilstrup DM, Melton LJ. Physeal fractures: part 1. Epidemiology in Olmsted County, Minnesota, 1979-1988. J Pediatr Orthop. 1994;14(4):423–430. doi: 10.1097/01241398-199407000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Shimizu A, Watanabe S, Kamada K, Tsuboi I, Yamamoto H. Hallux valgus interphalangeus following osteochondral fracture of the proximal phalanx: a case report. Foot Ankle Int. 2005;26(11):994–996. doi: 10.1177/107110070502601116. [DOI] [PubMed] [Google Scholar]
- 7.Kramer DE, Mahan ST, Hresko MT. Displaced intra-articular fractures of the great toe in children: intervene with caution! J Pediatr Orthop. 2014;34(2):144–149. doi: 10.1097/BPO.0000000000000110. [DOI] [PubMed] [Google Scholar]
- 8.Park DY, Han KJ, Han SH, Cho JH. Barefoot stubbing injuries to the great toe in children: a new classification by injury mechanism. J Orthop Trauma. 2013;27(11):651–655. doi: 10.1097/BOT.0b013e31828e5d39. [DOI] [PubMed] [Google Scholar]
- 9.Ogden JA, Ganey TM, Light TR, Belsole RJ, Greene TL. Ossification and pseudoepiphysis formation in the “nonepiphyseal” end of bones of the hands and feet. Skeletal Radiol. 1994;23(1):3–13. doi: 10.1007/BF00203694. [DOI] [PubMed] [Google Scholar]
- 10.Laor T, Clarke JP, Yin H. Development of the long bones in the hands and feet of children: radiographic and MR imaging correlation. Pediatr Radiol. 2016;46(4):551–561. doi: 10.1007/s00247-015-3513-7. [DOI] [PubMed] [Google Scholar]
- 11.Kim S, Lee M, Seok S. Intra-articular fracture of proximal phalanx of great toe accompanied by valgus deformity associated with sports activities. J Orthop Surg (Hong Kong) 2017;25(1):2309499017690324. doi: 10.1177/2309499017690324. [DOI] [PubMed] [Google Scholar]
- 12.Devalentine SJ. Epiphyseal injuries of the foot and ankle. Clin Podiatr Med Surg. 1987;4(1):279–310. [PubMed] [Google Scholar]
- 13.Maffulli N. Epiphyseal injuries of the proximal phalanx of the hallux. Clin J Sport Med. 2001;11(2):121–123. doi: 10.1097/00042752-200104000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Buch BD, Myerson MS. Salter-Harris type IV epiphyseal fracture of the proximal phalanx of the great toe: a case report. Foot Ankle Int. 1995;16(4):216–219. doi: 10.1177/107110079501600410. [DOI] [PubMed] [Google Scholar]