Abstract
Backgroud
Internal fixation has been established as a treatment of choice in relatively young patients with femoral neck fractures. Due to the characteristics of femoral neck anatomy and blood supply, complications such as malunion, nonunion, avascular necrosis, and femoral neck shortening can occur after internal fixation of femoral neck fractures. Unlike other complications such as avascular necrosis or nonunion, femoral neck shortening has not been relatively well studied. This study aimed to investigate the risk factors and clinical outcomes of femoral neck shortening after internal fixation of femoral neck fractures.
Methods
From June 2012 to July 2022, among 102 patients who underwent internal fixation of femoral neck fractures, 94 patients who met inclusion and exclusion criteria were retrospectively analyzed. Internal fixation of the femoral neck was done with cannulated compression screws or a femoral neck system. Patients were divided into 2 groups; femoral neck shortening (≥ 5 mm) and no shortening (< 5 mm) according to measurement on follow-up hip anteroposterior (AP) simple radiographs compared with postoperative hip AP simple radiographs. Demographic and radiographic data were compared between the 2 groups. The modified Harris Hip Score (mHHS) and a visual analog scale (VAS) were used to evaluate the clinical outcomes.
Results
Among 94 patients, femoral neck shortening was observed in 33 (35.1%). In chi-square test, Pauwels angle, Garden type III or IV (displacement), and cortical comminution were significantly correlated with neck shortening (p < 0.05). In the multifactorial logistic regression test, cortical comminution was significantly correlated with femoral neck shortening (p < 0.01). The shortening group showed significantly lower clinical scores in terms of mHHS and VAS (p < 0.01).
Conclusions
The femoral neck shortening group showed significantly lower clinical scores of mHHS and VAS than the no-shortening group. The presence of cortical comminution in preoperative hip computed tomography is a risk factor of femoral neck shortening after internal fixation of femoral neck fractures.
Keywords: Femur neck, Femoral neck fractures, Internal fracture fixation, Comminuted fracture, Postoperative complications
Femoral neck fracture (FNF) is a devastating problem for the health care system and social development.1,2) Internal fixation and arthroplasty have been introduced as the most common treatments of FNF and choice of treatment has been challenging to hip surgeons.3,4) Internal fixation with a cannulated compression screw (CCS) or a femoral neck system (FNS) intends to promote fracture healing using the compression force of screws and has shown successful results in young patients with FNF.5,6) However, arthroplasty has been established as a treatment of choice in elderly patients over 60 years with displaced FNF who showed unsatisfactory results to internal fixation.7,8,9) Due to characteristics of femoral neck anatomy and blood supply that can lead to many complications such as malunion, nonunion, avascular necrosis, and femoral neck shortening after internal fixation, surgical options can vary depending on the surrounding situations such as age, fracture type, etc.10,11) Therefore, analyzing risk factors of complications after internal fixation of FNF can be helpful to surgeons in selecting treatment options suitable for the patient-specific situation. The principle of internal fixation in FNF is to provide the compression force on the fracture site. However, because of this mechanism, femoral neck shortening can occur, and several studies have shown that femoral neck shortening after internal fixation of FNF lowers abductor functions of the hip by changing the moment arm for the abductor muscles of the affected aspect.12,13) Zielinski et al.14) reported that femoral neck shortening after internal fixation of FNF can impair gait velocity and gait symmetry and lead to permanent physical limitations. However, unlike other complications such as avascular necrosis or nonunion, femoral neck shortening has not been well studied. In this study, we analyzed the risk factors and clinical outcomes of femoral neck shortening after FNF.
METHODS
This study was approved by the Institutional Review Board at Dankook University Hospital (IRB No. 2024-04-022). Informed consent was waived because of the retrospective nature of the study.
Patient Selection
From June 2012 to July 2022, among 102 patients who underwent internal fixation of FNF, 94 patients who met inclusion and exclusion criteria were retrospectively analyzed. Inclusion criteria were patients diagnosed with unilateral FNF, treated with CCS or FNS devices, and had at least 1 year of follow-up after surgery. Exclusion criteria were patients who had comorbid fractures of the ipsilateral lower extremity, had a history of hip fracture or surgery, and were diagnosed with pathologic fractures. Numerous variables such as age, sex, body mass index (BMI), smoking status, injury mechanisms, reduction quality, time to surgery, and type of internal fixation devices (CCS/FNS) were assessed for their correlation with FNS. In the case of internal fixation with CCS, we used three 6.5-mm diameter partially threaded CCSs. Clinical outcomes were evaluated using the modified Harris Hip score (mHHS) and a visual analog scale (VAS) at 1 month and 1 year after surgery.
Radiologic Measurement
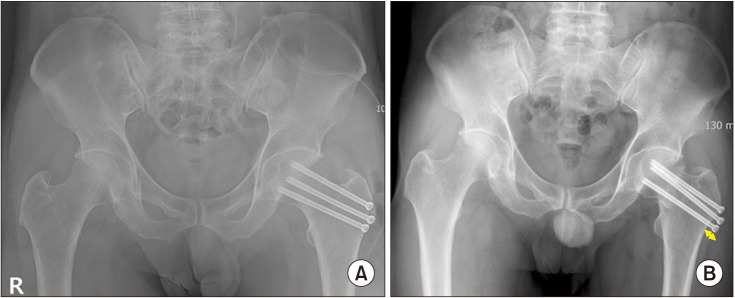
Radiological assessments were performed on anteroposterior (AP) and translateral views of the hip simple radiographs preoperatively, postoperatively, and at 1-year follow-up. On preoperative hip simple radiographs, Pauwels angle was measured and fractures were classified by Garden and Pauwels. Garden classification is subdivided into 4 types, and we considered Garden type III or IV as displaced fractures. Pauwels classification is subdivided into 3 types according to Pauwels angle: type 1 (< 30°), type II (30°–50°), and type III (> 50°). In preoperative hip 3-dimensional computed tomography (3D-CT), whether there is cortical comminution or not was checked (Fig. 1). The reduction quality was assessed by measuring the Garden’s angle, and the angle less than 155° or more than 180° in both the hip AP and translateral simple radiographs was defined as malreduction.15)
Fig. 1. Presence of cortical comminution (arrows) in preoperative hip 3-dimensional computed tomography. (A) Inferior view. (B) Coronal view.
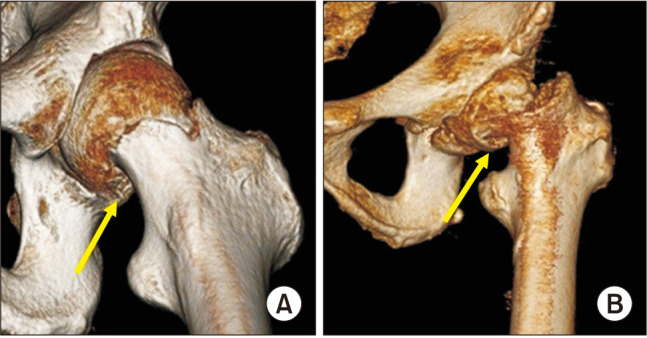
Femoral neck shortening was defined as shortening of ≥ 5 mm on the 1-year follow-up hip AP radiograph compared with the postoperative hip AP radiograph. Femoral neck shortening < 5 mm was defined as no shortening; 5–10 mm as mild shortening; and > 10 mm as severe shortening.16) Femoral neck shortening was measured by the change in the largest length of lateral protuberance of the internal fixation device along the screw trajectory on the follow-up hip AP simple radiograph compared with the postoperative hip AP view (Fig. 2). Although several techniques exist for measuring the femoral neck shortening, this technique is simple and convenient because it does not require contralateral hip radiographs and additional programs.
Fig. 2. Measurement of femoral neck shortening in a 42-year-old man. (A) Immediate postoperative hip anteroposterior (AP) simple radiograph. (B) Hip AP simple radiograph at 1 year after surgery. Arrow: largest length of lateral protuberance of the internal fixation device.
Radiological assessment of shortening was measured by 2 orthopedic surgeons (KCK and JHK) before the assessment of functional outcome to prevent measurement bias. Nonunion was defined when 3 of 4 cortices of the fracture site had not shown continuity over 6 months on plain radiographs. Avascular necrosis was diagnosed by simple radiography and magnetic resonance imaging based on the Ficat and Arlet classification.17)
Surgical Protocol
Under spinal or general anesthesia, patients were placed in the supine position with traction using a fracture table. After closed reduction under fluoroscopy, the greater trochanter was exposed through a standard lateral approach. Internal fixation using either CCS (TDM) or FNS (DepuySynthes) was performed. In the case of fixation with CCS, 3 screws were inserted in an inverted triangle configuration, parallel to the femoral neck axis.18) The most inferior screw was inserted in the calcar region. The remaining 2 cephalad screws were positioned superiorly, 5 mm from the anterior and posterior cortices of the femoral neck, and 5 mm from the subchondral bone.18)
Statistical Analysis
For comparisons between the shortening and no-shortening groups, the chi-square test and independent t-test were used to compare the demographic parameters. The variables confirmed as statistically significant by chi-square test were brought into a multifactorial logistic regression model. To test the assumption of normal distribution and homogeneity of variance, the independent t-test and Kolmogorov-Smirnov test were performed. Statistical significance was set at p < 0.05. Data were analyzed using SPSS Statistics version 26.0 statistical software (IBM Corp.) and GraphPad Prism version 8 (GraphPad Software Inc.).
To evaluate interobserver reliability, Fleiss-Kappa coefficient (κ) and the intraclass correlation coefficient with 95% confidence interval were used. Values were defined as follows: (1) below 0.5, poor reliability, (2) between 0.5 and 0.75, moderate reliability, (3) between 0.75 and 0.9, good reliability, and (4) above 0.90, excellent reliability. On interobserver reliability, there was excellent reliability between 2 measurements (intraclass correlation, 0.98; 95% confidence interval [CI], 0.97–0.99; p < 0.001).
RESULTS
Among the 94 patients, femoral neck shortening occurred in 33 patients, and the incidence of shortening was 35.1%. In comparing demographic data between the 2 groups (no-shortening group vs shortening group), there were no statistically significant differences in age, sex, BMI, smoking status, injury mechanisms, postoperative reduction quality, time to surgery, and methods of internal fixation (CCS or FNS) (Table 1). There was no significant difference in terms of the anatomical location of fractures and Pauwels type, while significant difference was observed in preoperative fracture morphology including Pauwels angle, displacement (Garden type III and IV), and cortical comminution (Table 2).
Table 1. Comparisons of Demographics Variables.
| Variable | Total (n = 94) | Shortening(–) (n = 61) | Shortening (+) (n = 33) | p-value | |
|---|---|---|---|---|---|
| Age (yr) | 53.5 (20–97) | 52.8 (20–97) | 54.8 (22–69) | 0.06 | |
| Sex | 0.17 | ||||
| Male | 41 (44) | 23 (37.7) | 18 (54.5) | ||
| Female | 53 (56) | 38 (62.3) | 15 (45.5) | ||
| Height (cm) | 164.9 | 165.1 | 164.5 | 0.85 | |
| Weight (kg) | 60.7 | 59.5 | 62.9 | 0.28 | |
| Body mass index (kg/m2) | 22.3 | 21.9 | 23.2 | 0.12 | |
| Smoking | 0.21 | ||||
| Yes | 32 (34) | 18 (29.5) | 14 (42.4) | ||
| No | 62 (66) | 43 (70.5) | 19 (57.6) | ||
| Injury mechanism | 0.15 | ||||
| Fall down | 69 (73.4) | 48 (78.7) | 21 (63.6) | ||
| Fall from height (> 2 m) | 16 (17.0) | 7 (11.5) | 9 (27.3) | ||
| Traffic accident | 9 (9.6) | 6 (9.8) | 3 (9.1) | ||
| Time to surgery | 0.35 | ||||
| <12 hr | 34 (36.2) | 20 (32.8) | 14 (42.4) | ||
| >12 hr | 60 (63.8) | 41 (67.2) | 19 (57.6) | ||
| Product | 0.55 | ||||
| Cannulated screw | 69 (73.4) | 46 (75.4) | 23 (69.7) | ||
| Femur neck system | 25 (26.6) | 15 (24.6) | 10 (30.3) | ||
Values are presented as median (range) or number (%).
Table 2. Comparisons of Radiologic Measurements.
| Variable | Total | Shortening (–) | Shortening (+) | p-value | |
|---|---|---|---|---|---|
| Reduction quality | 0.12 | ||||
| Good | 92 (97.9) | 61 (100) | 31 (93.9) | ||
| Worse | 2 (2.1) | 0 | 2 (6.1) | ||
| Anatomical type | 0.07 | ||||
| Subcapital | 18 (19.1) | 15 (24.6) | 3 (9.1) | ||
| Transcervical | 76 (80.9) | 46 (75.4) | 30 (90.9) | ||
| Base of neck | 0 | 0 | 0 | ||
| Pauwels classification | 0.10 | ||||
| I (< 30) | 5 (5.3) | 4 (6.6) | 1 (3.0) | ||
| II (30–50) | 46 (48.9) | 34 (55.7) | 12 (36.4) | ||
| III (> 50) | 43 (45.7) | 23 (37.7) | 20 (60.6) | ||
| Pauwels angle | - | 45.8±10.8 | 51.6±9.2 | 0.01 | |
| Garden type | < 0.001 | ||||
| I | 3 (3.2) | 3 (4.9) | 0 | ||
| II | 45 (47.9) | 37 (60.7) | 8 (24.2) | ||
| III | 38 (40.4) | 20 (32.8) | 18 (54.5) | ||
| IV | 8 (8.5) | 1 (1.6) | 7 (21.2) | ||
| Comminution | < 0.001 | ||||
| Yes | 43 (45.7) | 15 (24.6) | 28 (84.8) | ||
| No | 51 (54.3) | 46 (75.4) | 5 (15.2) | ||
Values are presented as number (%).
In multifactorial logistic regression analysis, cortical comminution showed significant relevance to femoral neck shortening (Table 3). The clinical scores were significantly poor in the shortening group (VAS, 3.9 ± 1.3; mHHS, 75.5 ± 13.3) compared to those in the no-shortening group (VAS, 2.4 ± 1.1; mHHS, 85.0 ± 7.5) (Table 4).
Table 3. Multi-factorial Logistic Regression Analysis of Femoral Neck Shortening.
| Influencing factor | B | Wald | OR | 95% CI | p-value |
|---|---|---|---|---|---|
| Cortical comminution | 2.843 | 24.943 | 17.173 | 5.627–52.415 | < 0.001 |
| Age | –0.01 | 0.543 | 0.991 | 0.951–1.031 | 0.643 |
| Garden type (III, IV) | 0.816 | 1.836 | 2.262 | 0.695–7.370 | 0.175 |
| Pauwels angle | 0.003 | 0.011 | 1.003 | 0.951–1.058 | 0.917 |
Table 4. Clinical Outcomes of Femoral Neck Shortening.
| Variable | Shortening (–) | Shortening (+) | p-value |
|---|---|---|---|
| VAS | 2.4 ± 1.1 | 3.9 ± 1.3 | < 0.001 |
| MHHS | 85.0 ± 7.5 | 75.5 ± 13.3 | < 0.001 |
Values are presented as mean ± standard deviation.
VAS: visual analog scale, MHHS: modified Harris Hip Score.
DISCUSSION
In the present study, the risk factors and clinical outcomes of femoral neck shortening after FNF were retrospectively analyzed. Femoral neck shortening was defined as shortening of ≥ 5 mm on the follow-up hip AP radiograph compared with the postoperative hip AP radiograph, and it occurred in 33 of the total 94 patients (35.1% in this study. In comparing the 2 groups (no-shortening group vs shortening group), although there were no statistical differences in demographic data, the presence of cortical comminution in preoperative hip CT was the single risk factor of femoral neck shortening in the multifactorial logistic regression analysis. In addition, clinical scores were significantly lower in the shortening group than in the no-shortening group. We compared and analyzed several studies that dealt with the effects and clinical outcomes of femoral neck shortening.
Among several complications after internal fixation of FNF, several studies suggested that femoral neck shortening was associated with pain and lower functional outcomes.11,16) Zlowodzki et al.16) evaluated the functional outcomes of femoral neck shortening and varus collapse in 70 patients and found femoral neck shortening was the single factor that negatively affects the 36-item short form survey (SF-36) physical functioning outcome. In a multicenter prospective study, Slobogean et al.19) reported that femoral neck shortening ≥ 10 mm negatively affected the functional scores (HHS, Timed Up and Go, and SF-36 scores). In the current study, femoral neck shortening ≥ 5 mm was significantly associated with poor clinical outcomes in terms of VAS and mHHS.
There are several factors known to be important in femoral neck shortening in other studies. First, Gregersen et al.20) reported that poor quality of fracture reduction is one of the factors that influence the risk of secondary surgery. Similarly, Kim et al.21) emphasized the importance of fracture reduction; in situ fixation in cases of valgus deformity in nondisplaced FNF can lead to hip joint narrowing. However, in this study, there were only 2 cases of poor reduction quality and it was not able to estimate the effect of poor reduction quality on femoral neck shortening and its outcomes.
Second, although several studies stated that FNS showed better clinical outcomes than CCS in FNFs,22,23) there were no significant differences in femoral neck shortening between the 2 devices in the present study (p = 0.55). In addition, Wang et al.2) reported that the presence of cortical comminution, displacement (Garden type III and IV), and reduction quality (grade III and IV) were statistically associated with femoral neck shortening. In the present study, among Pauwels angle, displacement (Garden type III and IV), and cortical comminution that showed statistical relevance to femoral neck shortening, cortical comminution was the single risk factor of femoral neck shortening in the multifactorial logistic regression study.
Furthermore, several studies demonstrated that cortical comminution was significantly related to femoral neck shortening.14,24) After internal fixation of FNFs with cortical comminution, compression of the longitudinal load along the internal fixation causes more severe shortening after weight-bearing starts.25) Despite several studies that tried to overcome the negative effects of cortical comminution,26,27) there is a lack of research about whether other treatment options including arthroplasty and other internal fixation devices other than CCS or FNS should be considered in the presence of cortical comminution of FNF. In the case of FNF with cortical comminution, further studies are needed to establish treatment indications including appropriate internal fixation devices and the need for arthroplasty.
There are several limitations in this study. First, this study was a retrospective study using data from a single medical center. The data from the 2 groups were collected from different periods to eliminate patient selection bias, but doing so might have influenced the clinical results. Second, the bone mineral density was not involved. Several studies reported the relevance between the bone quality or associated laboratory factors and outcomes of patients with hip and femur fractures.28,29) In our study, since the average age of the patients (53.5 years) was relatively young and the bone quality of several patients appeared not osteoporotic, many of the patients did not undergo the bone mineral density test. It could have been helpful for surgeons to reduce femoral neck shortening incidence by analyzing the bone quality of all patients and suggesting proper osteoporosis management such as injection or exercise.30) Therefore, the assessment of the effect of bone mineral density data will be required in further studies.
In conclusion, the femoral neck shortening group (shortening ≥ 5 mm) showed significantly lower clinical scores in terms of mHHS and VAS than the no-shortening group. The presence of cortical comminution in preoperative hip CT was the risk factor of femoral neck shortening after internal fixation of FNF.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Backer HC, Wu CH, Maniglio M, Wittekindt S, Hardt S, Perka C. Epidemiology of proximal femoral fractures. J Clin Orthop Trauma. 2021;12(1):161–165. doi: 10.1016/j.jcot.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang K, Lin D, Chen P, et al. Incidence and factors influencing neck shortening after screw fixation of femoral neck fractures with the femoral neck system. J Orthop Surg Res. 2023;18(1):317. doi: 10.1186/s13018-023-03787-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levack AE, Gausden EB, Dvorzhinskiy A, Lorich DG, Helfet DL. Novel treatment options for the surgical management of young femoral neck fractures. J Orthop Trauma. 2019;33(Suppl 1):S33–S37. doi: 10.1097/BOT.0000000000001368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.HEALTH Investigators. Bhandari M, Einhorn TA, et al. Total hip arthroplasty or hemiarthroplasty for hip fracture. N Engl J Med. 2019;381(23):2199–2208. doi: 10.1056/NEJMoa1906190. [DOI] [PubMed] [Google Scholar]
- 5.Tang Y, Zhang Z, Wang L, Xiong W, Fang Q, Wang G. Femoral neck system versus inverted cannulated cancellous screw for the treatment of femoral neck fractures in adults: a preliminary comparative study. J Orthop Surg Res. 2021;16(1):504. doi: 10.1186/s13018-021-02659-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stoffel K, Zderic I, Gras F, et al. Biomechanical evaluation of the femoral neck system in unstable Pauwels III femoral neck fractures: a comparison with the dynamic hip screw and cannulated screws. J Orthop Trauma. 2017;31(3):131–137. doi: 10.1097/BOT.0000000000000739. [DOI] [PubMed] [Google Scholar]
- 7.Lee YK, Ha YC, Park C, Koo KH. Trends of surgical treatment in femoral neck fracture: a nationwide study based on claim registry. J Arthroplasty. 2013;28(10):1839–1841. doi: 10.1016/j.arth.2013.01.015. [DOI] [PubMed] [Google Scholar]
- 8.Rogmark C, Leonardsson O. Hip arthroplasty for the treatment of displaced fractures of the femoral neck in elderly patients. Bone Joint J. 2016;98(3):291–297. doi: 10.1302/0301-620X.98B3.36515. [DOI] [PubMed] [Google Scholar]
- 9.Bhandari M, Devereaux PJ, Swiontkowski MF, et al. Internal fixation compared with arthroplasty for displaced fractures of the femoral neck: a meta-analysis. J Bone Joint Surg Am. 2003;85(9):1673–1681. doi: 10.2106/00004623-200309000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Kyle RF, Gustilo RB, Premer RF. Analysis of six hundred and twenty-two intertrochanteric hip fractures. J Bone Joint Surg Am. 1979;61(2):216–221. [PubMed] [Google Scholar]
- 11.Slobogean GP, Sprague SA, Scott T, Bhandari M. Complications following young femoral neck fractures. Injury. 2015;46(3):484–491. doi: 10.1016/j.injury.2014.10.010. [DOI] [PubMed] [Google Scholar]
- 12.Charles MN, Bourne RB, Davey JR, Greenwald AS, Morrey BF, Rorabeck CH. Soft-tissue balancing of the hip: the role of femoral offset restoration. Instr Course Lect. 2005;54:131–141. [PubMed] [Google Scholar]
- 13.McGrory BJ, Morrey BF, Cahalan TD, An KN, Cabanela ME. Effect of femoral offset on range of motion and abductor muscle strength after total hip arthroplasty. J Bone Joint Surg Br. 1995;77(6):865–869. [PubMed] [Google Scholar]
- 14.Zielinski SM, Keijsers NL, Praet SF, et al. Femoral neck shortening after internal fixation of a femoral neck fracture. Orthopedics. 2013;36(7):e849–e858. doi: 10.3928/01477447-20130624-13. [DOI] [PubMed] [Google Scholar]
- 15.Garden RS. Malreduction and avascular necrosis in subcapital fractures of the femur. J Bone Joint Surg Br. 1971;53(2):183–197. [PubMed] [Google Scholar]
- 16.Zlowodzki M, Brink O, Switzer J, et al. The effect of shortening and varus collapse of the femoral neck on function after fixation of intracapsular fracture of the hip: a multi-centre cohort study. J Bone Joint Surg Br. 2008;90(11):1487–1494. doi: 10.1302/0301-620X.90B11.20582. [DOI] [PubMed] [Google Scholar]
- 17.Ficat RP. Idiopathic bone necrosis of the femoral head: early diagnosis and treatment. J Bone Joint Surg Br. 1985;67(1):3–9. doi: 10.1302/0301-620X.67B1.3155745. [DOI] [PubMed] [Google Scholar]
- 18.Samsami S, Saberi S, Sadighi S, Rouhi G. Comparison of three fixation methods for femoral neck fracture in young adults: experimental and numerical investigations. J Med Biol Eng. 2015;35(5):566–579. doi: 10.1007/s40846-015-0085-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Slobogean GP, Stockton DJ, Zeng BF, Wang D, Ma B, Pollak AN. Femoral neck shortening in adult patients under the age of 55 years is associated with worse functional outcomes: analysis of the prospective multi-center study of hip fracture outcomes in China (SHOC) Injury. 2017;48(8):1837–1842. doi: 10.1016/j.injury.2017.06.013. [DOI] [PubMed] [Google Scholar]
- 20.Gregersen M, Krogshede A, Brink O, Damsgaard EM. Prediction of reoperation of femoral neck fractures treated with cannulated screws in elderly patients. Geriatr Orthop Surg Rehabil. 2015;6(4):322–327. doi: 10.1177/2151458515614369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim H, Kim JS, Sung YB. Postoperative valgus deformity and progression of ostheoarthritis in non-displaced femoral neck fractures. Hip Pelvis. 2023;35(4):259–267. doi: 10.5371/hp.2023.35.4.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huang S, Zhang Y, Zhang X, et al. Comparison of femoral neck system and three cannulated cancellous screws in the treatment of vertical femoral neck fractures: clinical observation and finite element analysis. Biomed Eng Online. 2023;22(1):20. doi: 10.1186/s12938-023-01083-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hu H, Cheng J, Feng M, Gao Z, Wu J, Lu S. Clinical outcome of femoral neck system versus cannulated compression screws for fixation of femoral neck fracture in younger patients. J Orthop Surg Res. 2021;16(1):370. doi: 10.1186/s13018-021-02517-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Felton J, Slobogean GP, Jackson SS, et al. Femoral neck shortening after hip fracture fixation is associated with inferior hip function: results from the FAITH trial. J Orthop Trauma. 2019;33(10):487–496. doi: 10.1097/BOT.0000000000001551. [DOI] [PubMed] [Google Scholar]
- 25.Liu Y, Ai ZS, Shao J, Yang T. Femoral neck shortening after internal fixation. Acta Orthop Traumatol Turc. 2013;47(6):400–404. doi: 10.3944/aott.2013.3235. [DOI] [PubMed] [Google Scholar]
- 26.Rupprecht M, Grossterlinden L, Sellenschloh K, et al. Internal fixation of femoral neck fractures with posterior comminution: a biomechanical comparison of DHS® and Intertan nail®. 11. Vol. 35. Int Orthop: 2011. pp. 1695–1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rajnish RK, Haq RU, Aggarwal AN, Verma N, Pandey R, Bhayana H. Four screws diamond configuration fixation for displaced, comminuted intracapsular fracture neck femur in young adults. Indian J Orthop. 2019;53(1):70–76. doi: 10.4103/ortho.IJOrtho_333_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spangler L, Cummings P, Tencer AF, Mueller BA, Mock C. Biomechanical factors and failure of transcervical hip fracture repair. Injury. 2001;32(3):223–228. doi: 10.1016/s0020-1383(00)00186-8. [DOI] [PubMed] [Google Scholar]
- 29.Lee SH, Kim JS, Koh JM. The fracture risk assessment tool probability and trabecular bone score mediate the relationship between sphingosine 1-phosphate levels and fracture risk. J Bone Metab. 2023;30(4):355–364. doi: 10.11005/jbm.2023.30.4.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bae S, Lee S, Park H, et al. Position statement: exercise guidelines for osteoporosis management and fall prevention in osteoporosis patients. J Bone Metab. 2023;30(2):149–165. doi: 10.11005/jbm.2023.30.2.149. [DOI] [PMC free article] [PubMed] [Google Scholar]