Abstract
Background
The treatment of chronic scapholunate dissociation (SLD) can be challenging due to several factors such as poor quality of ligament, malalignment of the carpus, limited surgical options, and risk of recurrent instability. Various surgical techniques have been developed, but there is ongoing debate regarding the optimal surgical technique. This study aimed to report the clinical and radiological outcomes after dorsal scapholunate (SL) ligament complex reconstruction using suture tape-augmented autologous tendon graft.
Methods
The study included patients with Garcia-Elias stage 3–4 chronic SLD, SL advanced collapse (SLAC) stage 1, and a follow-up period exceeding 1 year. Pre- and postoperative SL gap, SL angle (SLA), radiolunate angle (RLA), and dorsal scaphoid translation (DST) were measured, and wrist active range of motion, Modified Mayo Wrist Score (MMWS), and visual analog scale (VAS) were evaluated.
Results
Nine patients were included in this study with a mean follow-up period of 17 months (range, 15–31 months). All patients were male, with a mean age of 49 years (range, 30–62 years). Eight patients were classified as Garcia-Elias stage 4, while one was classified as SLAC 1. The median (range) of preoperative, immediate postoperative, and final follow-up measurements for SL gap, SLA, RLA, and DST were 5.4 mm (4.5–5.9), 2.1 mm (1.8–2.5), and 2.5 mm (2.0–2.8) (p = 0.008); 76° (69°–88°), 50° (32°–56°), and 54° (50°–64°) (p = 0.008); 22° (11.5°–33°), 2.8° (0.5°–3.8°), and 3.8° (2.2°–5.6°) (p = 0.008); and 2.8 mm (2.0–3.4), 0.8 mm (0.1–1.2), and 1.0 mm (0.1–2.0) (p = 0.008), respectively. Immediately after surgery, all radiological measurements showed significant improvement, which persisted up to 15 months postoperatively. The preoperative and final follow-up measurements of active flexion, extension, radial deviation, and ulnar deviation of the wrist showed significant improvement. The median preoperative and final follow-up values of MMWS were 51.1 (range, 40–60) and 88.3 (range, 85–95) (p = 0.007), respectively, and those of VAS were 7 (range, 6–8) and 2 (range, 1–3) (p = 0.007), respectively.
Conclusions
Dorsal SL ligament complex reconstruction using suture tape-augmented autologous free tendon graft could be regarded as a feasible and straightforward technique for addressing irreparable chronic SLD.
Keywords: Scapholunate dissociation, Reconstruction, Autologous tendon graft, Synthetic tape
Scapholunate dissociation (SLD), also known as scapholunate (SL) instability, is one of the most common forms of carpal instability, and its incidence can vary depending on the population studied and the diagnostic criteria used. In the general population, the reported incidence of SLD ranges from approximately 3% to 5%.1,2) It is rare, but more frequently observed in individuals involved in high-impact or repetitive activities, such as athletes, manual laborers, and young individuals participating in wrist-intensive activities.
SLD is caused by disruption of the SL interosseous ligament (SLIL) and associated with an attenuated secondary stabilizer, such as the dorsal intercarpal (DIC) ligament, scaphotrapeziotrapezoid (STT) ligament, and long radiolunate ligament.3,4) Repair of the SLIL can be attempted if feasible; however, repair of a chronically ruptured SLIL may be challenging or even impossible due to the prolonged duration of the injury or poor quality of the SLIL.
The treatment of SLD aims to restore the stability of the SL joint and to prevent arthritic changes of the radiocarpal and intercarpal joints. Garcia-Elias stage 3 or 4 chronic SLD and SL advanced collapse (SLAC) stage 1 are the indications for ligament reconstruction. Various reconstruction techniques have been introduced over time, including tenodesis,5,6) the reduction and association of the scaphoid and lunate procedure,7) capsulodesis,8,9) bone-ligament-bone grafts,10) and the SL axis method procedure.11) Most recently, the SL ligament internal brace 360° tenodesis (SLITT) procedure12,13) and the anatomical front and back (ANAFAB) repair procedure14) have been introduced for both dorsal and volar ligament reconstruction. However, the surgical outcomes of these procedures are still a topic of debate and the single most effective treatment for chronic SLD is yet to be determined.
Recently, dorsal SL ligament complex reconstruction using suture tape-augmented autologous free tendon graft has emerged as a promising treatment option, and favorable outcomes have been reported.15,16) The use of a synthetic tape may mitigate the stretching and weakening of the grafted tendon, and suture anchors can enhance the fixation strength. The short transverse limb may play a role as the dorsal SLIL, while the long oblique limb may serve as the DIC ligament.17) The aim of this study was to report the clinical and radiological outcomes after dorsal SL ligament complex reconstruction using suture tape-augmented autologous free tendon graft for the treatment of patients with chronic SLD. While there have been a few prior studies on internal brace-augmented SL reconstruction, they primarily focused on surgical techniques, and few patients were followed up for more than 1 year.15) Additionally, there is a lack of information regarding radiological and clinical outcomes. In contrast, this study provides valuable insights from 9 patients followed up for at least 15 months, which we believe adds significant value.
METHODS
This study was approved by the Institutional Review Board of the Catholic University of Korea (IRB No. HC23RASC0066). This study was a retrospective small case series; therefore, the informed consent for the study was waived.
Study Design
We retrospectively reviewed 37 patients diagnosed and treated for chronic SLD between May 2020 and September 2022. Indications for reconstruction surgery were Garcia-Elias stage 3 or 4, chronic SLD, and SLAC stage 1. Garcia-Elias stage 3 means that the SLIL has insufficient tissue to be repaired and the scaphoid is aligned normally, and stage 4 is defined as the characteristics of stage 3 plus easily reducible carpal malalignment. SLAC stage 1 is characterized by narrowing and sclerosis of the joint space between the scaphoid and radial styloid processes. Inclusion criteria were patients who underwent dorsal SL ligament complex reconstruction using suture tape-augmented autologous free tendon graft with at least 1 year of follow-up after surgery. Exclusion criteria included Garcia-Elias stage 1, 2 chronic SLD (n = 3), less than 1 year of follow-up (n = 2), other reconstruction methods (n = 3), concurrent distal radius malunion (n = 6), history of previous surgery for SLD (n = 3), and advanced arthritic changes in the radiocarpal or midcarpal joints (SLAC stages 2, 3, and 4) (n = 11). Nine patients with the average age of 49 years (range, 30–62 years) were included in this study, and the mean follow-up period was 17 months (range, 15–31 months).
Surgical Procedures
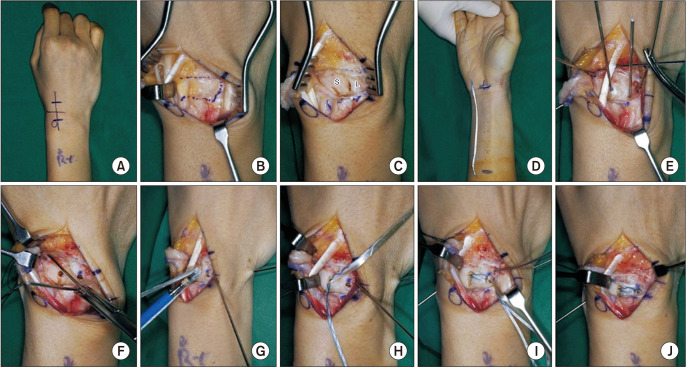
Surgery was performed by 2 surgeons (IJP and SC) in the same manner, as depicted in Fig. 1. A 6-cm longitudinal incision was made along the ulnar edge of Lister’s tubercle on the dorsum of the wrist (Fig. 1A). The terminal branch of the posterior interosseous nerve was resected, and dorsal ligament-sparing capsulotomy was performed (Fig. 1B). After exposing the scaphoid and lunate, we were able to confirm that all 3 components of the SLILs were completely ruptured, and no arthritic changes were observed in the radiocarpal and midcarpal joints (Fig. 1C). Given the absence of repairable ligaments, we opted to proceed with ligament reconstruction. The autologous palmaris longus (PL) tendon was harvested (Fig. 1D). A joystick technique using 2 Kirschner wires (K-wires) was employed to correct the flexion deformity of the scaphoid and the extension deformity of the lunate. Three guidewires were placed into the proximal pole of the scaphoid, central on the lunate, and the distal pole of the scaphoid (Fig. 1E). After confirming the guidewire position under fluoroscopy, we created a 3.5-mm-diameter hole for the autologous PL tendon and synthetic tape (SutureTape, Arthrex) with the cannulated 3.5-mm gold drill bit (Fig. 1F). The positioning of the holes was crucial, especially at the proximal pole of the scaphoid, as cortical breakage could lead to insecure graft fixation. To avoid this complication, the guidewire position was confirmed under fluoroscopy, and the drill guide had a 1-cm depth stop to prevent overdrilling. Suture anchors (3.5-mm DX SwiveLock SL, Arthrex) were used for secure reconstructions (Fig. 1G), and the fixation sequence was as follows: (1) scaphoid proximal pole, (2) lunate center, and (3) scaphoid distal pole (Fig. 1H–J). The anchors were inserted at a 90° angle, as anchor insertion at obtuse angles may diminish the pullout strength. The Berger-type capsulodesis technique was utilized for capsule repair, which included rotating the distal portion of the capsule (proximal strip of the DIC ligament) proximally and securing it to the dorsal lunate.18) In the first 3 of the 9 patients, the capsule was sutured to the grafted autologous PL tendon, but the procedure was not easy. Subsequently, in 6 patients, capsulodesis was performed by fixing 2-0 or 0 Ethibond sutures (Ethicon, Johnson & Johnson) to the center of the lunate bone (Fig. 2). The 1.4-mm K-wires were inserted for the intercarpal fixation. Once the alignment of the carpal bones was confirmed to be adequate, K-wires were buried subcutaneously. A sugar-tong splint and a short-arm cast were applied for 3 weeks each. After 6 weeks, the cast and K-wires were removed, and physiotherapy was initiated to regain grip strength and active range of motion. Daily activities were allowed, but excessive wrist movements were avoided for up to 3 months after surgery. Return to the previous job was usually allowed at 3 months postoperatively.
Fig. 1. A dorsal scapholunate ligament complex reconstruction using suture tape-augmented autologous free tendon graft was performed. A dorsal skin incision was made (A), and a ligament-sparing capsulotomy was carried out (B). (C) After exposing the scaphoid and lunate, the authors confirmed a completely ruptured scapholunate interosseous ligament and observed no arthritic changes in the radiocarpal and midcarpal joints. (D) Autologous palmaris longus tendon was harvested. We reduced the scaphoid and lunate with the use of the joystick technique. (E) Three guidewires were placed in the lunate center, the scaphoid proximal pole dorsum, and scaphoid distal pole dorsum. (F) After confirming the guidewire position under fluoroscopy, we created a 3.5-mm-diameter hole for the autologous palmaris longus tendon and synthetic tape (SutureTape, Arthrex) with the cannulated 3.5-mm gold drill bit. (G) Suture anchors (3.5 mm DX SwiveLock SL, Arthrex) were used for secure reconstruction. The fixation sequence was as follows: scaphoid proximal pole (H), lunate center (I), and scaphoid distal pole (J). S: scaphoid, L: lunate.
Fig. 2. Sequential fixation: scaphoid proximal pole (A), lunate center (B), and scaphoid distal pole (C). (B) Ethibond sutures (Ethicon, Johnson & Johnson) were fixed together at the center of the lunate to perform the capsulodesis. (D, E) The distal part of the capsule (proximal strip of the DIC ligament, asterisk) was rotated proximally and anchored to the dorsal lunate. S: scaphoid, L: lunate.
Measurement of Outcomes
The radiological outcomes were evaluated by the SL gap, SL angle (SLA), radiolunate angle (RLA), and dorsal scaphoid translation (DST). The SL gap refers to the distance between the scaphoid and lunate at the midpoints of Gilula’s lines for the proximal carpal row.19) The SLA is determined by a line drawn tangent to the volar surface of the scaphoid and an axis line of the lunate on a wrist lateral view. The RLA is formed by the radial axis and a line that is perpendicular to the tangent drawn from the dorsal and palmar poles of the lunate.20) DST is the distance between a line tangential to the proximal articular surface of the scaphoid, parallel to the longitudinal axis of the radius, and a line drawn through the dorsal scaphoid facet of the distal part of the radius.21) All radiological measurements were performed using nU ViewRex PACS system (TechHeim). Each image was evaluated by 2 experienced hand surgeons (IJP and SC) independently. The observers were unaware of each other’s measurements. Each observer repeated measurements at least 1 week apart. Clinical outcomes were assessed by range of motion of the wrist, Modified Mayo Wrist Score (MMWS) for evaluating the function, and a visual analog scale (VAS) for pain. Preoperative and final follow-up range of motion of the wrist was measured by 2 experienced hand surgeons (IJP and SC) in an outpatient clinic. Wrist movements include flexion, extension, radial deviation, and ulnar deviation. MMWS, a physician-based scoring system, including pain, functional status, range of motion, and grip strength, was evaluated (Table 1).22) Grip Strength was measured using a hand dynamometer. Pain was measured using the VAS, where patients selected the intensity of pain on a numerical scale ranging from 0 to 10 to quantify the level of pain experienced by the patient before and after surgery.
Table 1. Modified Mayo Wrist Score.
| Category | Score | Findings |
|---|---|---|
| Pain | 25 | No pain |
| 20 | Mild, occasional | |
| 15 | Moderate | |
| 0 | Severe, intolerable | |
| Functional status | 25 | Returned to regular employment |
| 20 | Restricted employment | |
| 15 | Able to work, unemployed | |
| 0 | Unable to work because of pain | |
| Range of motion (flexion–extension arc) (°) | 25 | ≥ 120 |
| 20 | 100–119 | |
| 15 | 90–99 | |
| 10 | 60–89 | |
| 5 | 30–59 | |
| 0 | 0–29 | |
| Grip strength (% of normal, range) | 25 | 90–100 |
| 15 | 75–89 | |
| 10 | 50–74 | |
| 5 | 25–49 | |
| 0 | 0–24 |
Statistical Analysis
Radiological results were evaluated by 2 specialists in hand surgery (IJP and SC), and the average value of their measurements was recorded. Baseline characteristics and continuous variables of the patients were presented as median and range. Statistical differences between groups were assessed using Wilcoxon signed-rank test with IBM SPSS software ver. 21.0 (IBM Corp.). Statistical significance was set at p < 0.05.
RESULTS
All 9 patients were men, and they were classified into Garcia-Elias stage 4 in 8 patients and SLAC 1 in 1 patient. Preoperative and postoperative radiological outcomes, range of motion of the wrist, and clinical outcomes of each patient are shown in Table 2. The preoperative SL gap, SLA, RLA, and DST were 5.4 mm (range, 4.5–5.9 mm), 76° (range, 69°–88°), 22° (range, 11.5°–33°), and 2.8 mm (range, 2.0–3.4 mm), respectively. The immediate postoperative and final follow-up SL gap, SLA, RLA, and DST were 2.1 mm (range, 1.8–2.5 mm) and 2.5 mm (range, 2.0–2.8 mm) (p = 0.008), 50° (range, 32°–56°) and 54° (range, 50°–64°) (p = 0.008), 2.8° (range, 0.5°–3.8°) and 3.8° (range, 2.2°–5.6°) (p = 0.008), and 0.8 mm (range, 0.1–1.2 mm) and 1.0 mm (range, 0.1–2.0 mm) (p = 0.008), respectively. Immediately after surgery, there was a significant improvement in all radiological measurements and these improvements were sustained up to 15 months postoperatively. Clinically, patients demonstrated improvements in function and pain. The preoperative and final follow-up range of motion of the wrist were 50° (range, 30°–65°) and 60° (range, 45°–75°) in flexion (p = 0.012), 50° (range, 40°–65°) and 60° (range, 50°–80°) in extension (p = 0.016), 10° (range, 5°–15°) and 15° (range, 10°–20°) in radial deviation (p = 0.011), and 20° (range, 15°–20°) and 25° (range, 20°–30°) (p = 0.007) in ulnar deviation, respectively. The preoperative and final follow-up MMWS values were 51.1 (range, 40–60) and 88.3 (range, 85–95) (p = 0.007), respectively. The preoperative and final follow-up VAS scores were 7 (range, 6–8) and 2 (range, 1–3) (p = 0.007), respectively (Table 3).
Table 2. Radiological and Clinical Outcome Measurements of Each Patient Preoperatively, Immediate Postoperatively, and Final Follow-up after Dorsal Scapholunate Ligament Complex Reconstruction Using Suture Tape-Augmented Autologous Free Tendon Graft.
| No. of patients | Radiological outcome | Range of motion of the wrist | Clinical outcome | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SL gap (mm) | SLA (°) | RLA (°) | DST (mm) | Flex (°) | Ext (°) | RD (°) | UD (°) | MMWS | VAS | |||||||||||||||
| Pre | Post | Final | Pre | Post | Final | Pre | Post | Final | Pre | Post | Final | Pre | Final | Pre | Final | Pre | Final | Pre | Final | Pre | Final | Pre | Final | |
| 1 | 5.8 | 2.5 | 2.8 | 72 | 54 | 60 | 22 | 0.6 | 3.8 | 2.8 | 0.1 | 0.2 | 50 | 45 | 50 | 60 | 10 | 15 | 20 | 20 | 40 | 85 | 6 | 1 |
| 2 | 5.2 | 2.2 | 2.5 | 69 | 39 | 51 | 12.8 | 0.5 | 3.4 | 2 | 0.1 | 0.1 | 50 | 75 | 50 | 75 | 10 | 15 | 20 | 25 | 60 | 90 | 6 | 1 |
| 3 | 4.5 | 1.9 | 2.2 | 70 | 56 | 64 | 11.5 | 3.2 | 5.6 | 2 | 0.1 | 0.6 | 30 | 40 | 40 | 50 | 5 | 10 | 20 | 25 | 50 | 85 | 8 | 2 |
| 4 | 5.5 | 1.8 | 2 | 88 | 32 | 53 | 33 | 3.6 | 4.8 | 3.2 | 0.8 | 1 | 65 | 60 | 50 | 60 | 5 | 15 | 15 | 20 | 60 | 95 | 7 | 2 |
| 5 | 5.9 | 1.9 | 2.7 | 76 | 54 | 60 | 18 | 3.8 | 3.9 | 2.9 | 0.8 | 2 | 50 | 40 | 40 | 60 | 10 | 15 | 15 | 20 | 45 | 85 | 8 | 3 |
| 6 | 5.8 | 2.1 | 2.3 | 80 | 54 | 56 | 24 | 2.5 | 4.5 | 2 | 0.4 | 0.4 | 65 | 60 | 40 | 50 | 10 | 15 | 20 | 25 | 55 | 90 | 8 | 1 |
| 7 | 5.4 | 2.5 | 2.6 | 76 | 50 | 54 | 26 | 2.8 | 3.8 | 2.2 | 0.8 | 1 | 65 | 60 | 65 | 60 | 10 | 15 | 20 | 25 | 45 | 90 | 8 | 2 |
| 8 | 5.2 | 2.4 | 2.5 | 85 | 48 | 52 | 30 | 2.8 | 3.2 | 3.4 | 1.2 | 1.4 | 60 | 70 | 60 | 80 | 15 | 20 | 20 | 30 | 55 | 85 | 6 | 1 |
| 9 | 5 | 1.9 | 2.1 | 72 | 48 | 50 | 12 | 0.8 | 2.2 | 2.8 | 1 | 1.2 | 50 | 45 | 50 | 60 | 10 | 15 | 20 | 20 | 50 | 90 | 6 | 2 |
SL: scapholunate, SLA: scapholunate angle, RLA: radiolunate angle, DST: dorsal scaphoid translation, Flex: flexion, Ext: extension, RD: radial deviation, UD: ulnar deviation, MMWS: modified Mayo Wrist Score, VAS: visual analog scale, Pre: preoperative, Post: immediate postoperative, Final: final follow-up.
Table 3. Preoperative and Postoperative Radiological Outcomes, Range of Motion of the Wrist, and Patient-Reported Outcomes.
| Variable | Preoperative | Postoperative | p-value | Last follow-up | p-value | |
|---|---|---|---|---|---|---|
| Radiological outcome | ||||||
| Mean SL gap (mm) | 5.4 (4.5–5.9) | 2.1 (1.8–2.5) | 0.008 | 2.5 (2.0–2.8) | 0.008 | |
| Mean SLA (°) | 76 (69–88) | 50 (32–56) | 0.008 | 54 (50–64) | 0.008 | |
| Mean RLA (°) | 22 (11.5–33.0) | 2.8 (0.5–3.8) | 0.008 | 3.8 (2.2–5.6) | 0.008 | |
| Mean DST (mm) | 2.8 (2.0–3.4) | 0.8 (0.1–1.2) | 0.008 | 1.0 (0.1–2.0) | 0.008 | |
| Range of motion of the wrist | ||||||
| Flexion (°) | 50 (30–65) | - | - | 60 (45–75) | 0.012 | |
| Extension (°) | 50 (40–65) | - | - | 60 (50–80) | 0.016 | |
| Radial deviation (°) | 10 (5–15) | - | - | 15 (10–20) | 0.011 | |
| Ulnar deviation (°) | 20 (15–20) | - | - | 25 (20–30) | 0.007 | |
| Patient-reported outcome | - | |||||
| MMWS | 51.1 (40–60) | - | - | 88.3 (85–95) | 0.007 | |
| VAS | 7 (6–8) | - | - | 2 (1–3) | 0.007 | |
Values are presented as median (range).
SL: scapholunate, SLA: scapholunate angle, RLA: radiolunate angle, DST: dorsal scaphoid translation, MMWS: modified Mayo Wrist Score, VAS: visual analog scale.
DISCUSSION
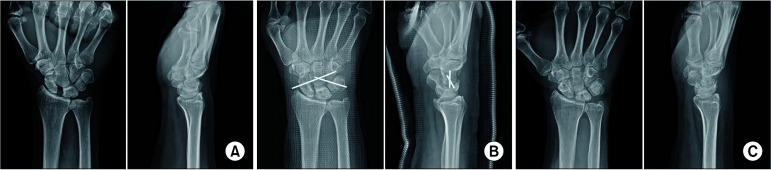
Potential complications after SL ligament reconstruction include recurrence of SL dissociation and residual instability. The treatment goal of chronic SLD extends beyond addressing the SL gap in the coronal plane; it also aims to resolve scaphoid flexion deformity in the sagittal plane, thereby restoring normal kinematics and preventing degenerative changes. This study demonstrates that dorsal SL ligament complex reconstruction using suture tape-augmented autologous free tendon graft could be one of the potential techniques. This technique consists of 2 components: a short transverse limb for correcting the SL interval (coronal plane correction) and a long oblique limb for addressing scaphoid rotatory subluxation and dorsal intercalated segment instability (sagittal plane correction). The radiological outcomes, range of motion, functional scores, and pain scores improved significantly at a mean follow-up of 18 months (range, 15–31 months), suggesting sustainable alignment correction (Fig. 3).
Fig. 3. A 62-year-old man presented with left wrist pain for 4 months after a traffic accident. (A) Preoperative posteroanterior and lateral radiographs showing widening of the scapholunate distance and dorsal intercalated segmental instability (DISI) deformity. (B) Immediate postoperative radiographs demonstrating the scapholunate distance addressed and the DISI deformity corrected. (C) Final follow-up (18 months after surgery) radiographs showing the alignment correction maintained.
A synthetic suture tape provides additional biomechanical strength and support before graft incorporation, resulting in a stronger construct. In the long-term results of the previously reported tenodesis technique for chronic SLD, pain relief and improved grip strength were observed; however, radiological recurrence of the deformity was often noted.23,24) This may be attributed to tendon graft stretching and weakening, as well as to sufficient fixation strength.23,25) Even if symptoms improve, disruption of realignment can potentially lead to recurring symptoms in the future. Suture augmentation, known as internal bracing, has recently become widely adopted in the field of orthopedics, with several studies confirming its effectiveness.15,26) In the cadaveric biomechanical study by Dugas et al.,27) the internal bracing group was compared with the ligament reconstruction group using the PL tendon for the ulnar collateral ligament of the elbow. This study showed that the internal bracing group demonstrated greater resistance to gapping. Park et al.28) tested the load to failure and linear stiffness in 21 fresh-frozen cadaver wrists and found that while it did not recreate biomechanical properties equivalent to native intact SLIL, SLIL repair with internal brace augmentation had significantly higher strength than repair alone. The use of a synthetic tape may mitigate stretching and weakening of the tendon, while suture anchors can enhance fixation strength, providing long-term stability.
A concern associated with this method is that the reconstruction procedure mainly focuses on the dorsal ligaments, which may potentially lead to excessive tightness on the dorsal side and create a hinge effect on the volar side.17) For this reason, techniques that address both dorsal and volar ligaments have been introduced.14,29,30) In particular, the recently introduced SLITT procedure13) and ANAFAB repair procedure14) are receiving ample attention from many surgeons despite the lack of long-term follow-up results. However, it remains uncertain whether reconstruction of the volar SLIL is necessary. Some reports suggest that the rotation axis of the SL joint should be located along the dorsal SLIL rather than in the center of the SL joint.31,32) Excessively strong reconstruction of the volar SLIL may potentially disrupt the normal rotation axis of the SL joint. A recent study indicated that SL instability results from a compromised dorsal SL ligament complex.33) This study suggests that the STT and volar carpal ligaments are unlikely to be disrupted, and thus do not necessitate surgical intervention. Although the STT and volar ligament complex play an important role as a secondary stabilizer in SL instability,34) we believe that focusing primarily on the dorsal aspect should not pose a problem because it is the critical component of the SL ligament complex reconstruction.
This technique offers high accessibility and a fast-learning curve as its advantages.15,35) It is a more efficient technique in terms of operating time and reduces complications related to multiple incisions, transosseous tunnels, and complicated shuttling.15,35) Multiple transosseous tunnels and complicated shuttling can not only extend the surgical time but also potentially cause complications such as fracture, avascular necrosis of the lunate, and cartilage degeneration.34,36,37) Starr et al.35) reported 6-month and 1-year outcomes following all dorsal internal bracing for intercarpal ligament reconstruction, showing restored grip strength and range of motion, as well as improvements in patient-reported pain and functional scores. Ahmad et al.16) found that internal bracing for the SL ligament showed early signs of success in patient-reported outcomes. This technique offers a more straightforward, safe, and readily available approach to reconstruction for chronic SLD, with initial outcomes comparable or superior to those of alternative techniques.
This study has some limitations that should be considered. First, the sample size was small because the indication for this technique was applied to only Garcia-Elias stage 3 or 4, chronic SLD, and SLAC stage 1. Second, although all patients were followed up for more than 15 months, the long-term outcomes were lacking. One patient completed the follow-up for more than 2 years; however, long-term follow-up is needed to evaluate the radiological outcomes and potential complications associated with synthetic tapes. Lastly, this study is a case series without a control group. Future studies comparing the results with other reconstruction methods are warranted to provide further insights.
In conclusion, this study showed excellent radiological and clinical results when biomechanically proven autologous tendon grafting and synthetic tape augmentation were applied to actual patients with a follow-up of more than 15 months. We believe that this method provides a simple and straightforward approach when treating patients with chronic SLD.
ACKNOWLEDGEMENTS
We express our gratitude to Chang Deok Weon, a medical photographer at Bucheon St. Mary’s Hospital, the Catholic University of Korea, for assisting in preparing the photographs.
This work was supported by the Institute of Clinical Medicine Research of Bucheon St. Mary’s Hospital, Research Fund, 2024 (BCMC24IH01).
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Andersson JK. Treatment of scapholunate ligament injury: current concepts. EFORT Open Rev. 2017;2(9):382–393. doi: 10.1302/2058-5241.2.170016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jones WA. Beware the sprained wrist: the incidence and diagnosis of scapholunate instability. J Bone Joint Surg Br. 1988;70(2):293–297. doi: 10.1302/0301-620X.70B2.3346308. [DOI] [PubMed] [Google Scholar]
- 3.Michelotti BF, Adkinson JM, Chung KC. Chronic scapholunate ligament injury: techniques in repair and reconstruction. Hand Clin. 2015;31(3):437–449. doi: 10.1016/j.hcl.2015.04.013. [DOI] [PubMed] [Google Scholar]
- 4.Perez AJ, Jethanandani RG, Vutescu ES, Meyers KN, Lee SK, Wolfe SW. Role of ligament stabilizers of the proximal carpal row in preventing dorsal intercalated segment instability: a cadaveric study. J Bone Joint Surg Am. 2019;101(15):1388–1396. doi: 10.2106/JBJS.18.01419. [DOI] [PubMed] [Google Scholar]
- 5.Brunelli GA, Brunelli GR. A new surgical technique for carpal instability with scapholunate dissociation. Surg Technol Int. 1996;5:370–374. [PubMed] [Google Scholar]
- 6.Garcia-Elias M, Lluch AL, Stanley JK. Three-ligament tenodesis for the treatment of scapholunate dissociation: indications and surgical technique. J Hand Surg Am. 2006;31(1):125–134. doi: 10.1016/j.jhsa.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 7.Rosenwasser MP, Miyasajsa KC, Strauch RJ. The RASL procedure: reduction and association of the scaphoid and lunate using the Herbert screw. Tech Hand Up Extrem Surg. 1997;1(4):263–272. [PubMed] [Google Scholar]
- 8.Gajendran VK, Peterson B, Slater RR, Jr, Szabo RM. Long-term outcomes of dorsal intercarpal ligament capsulodesis for chronic scapholunate dissociation. J Hand Surg Am. 2007;32(9):1323–1333. doi: 10.1016/j.jhsa.2007.07.016. [DOI] [PubMed] [Google Scholar]
- 9.Megerle K, Bertel D, Germann G, Lehnhardt M, Hellmich S. Long-term results of dorsal intercarpal ligament capsulodesis for the treatment of chronic scapholunate instability. J Bone Joint Surg Br. 2012;94(12):1660–1665. doi: 10.1302/0301-620X.94B12.30007. [DOI] [PubMed] [Google Scholar]
- 10.Harvey EJ, Berger RA, Osterman AL, Fernandez DL, Weiss AP. Bone-tissue-bone repairs for scapholunate dissociation. J Hand Surg Am. 2007;32(2):256–264. doi: 10.1016/j.jhsa.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 11.Yao J, Zlotolow DA, Lee SK. ScaphoLunate axis method. J Wrist Surg. 2016;5(1):59–66. doi: 10.1055/s-0035-1570744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kakar S, Greene RM. Scapholunate ligament internal brace 360-degree tenodesis (SLITT) procedure. J Wrist Surg. 2018;7(4):336–340. doi: 10.1055/s-0038-1625954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kakar S, Logli AL, Ramazanian T, Gaston RG, Fowler JR. Scapholunate ligament 360° procedure. Bone Joint J. 2021;103(5):939–945. doi: 10.1302/0301-620X.103B5.BJJ-2020-1964.R2. [DOI] [PubMed] [Google Scholar]
- 14.Sandow M, Fisher T. Anatomical anterior and posterior reconstruction for scapholunate dissociation: preliminary outcome in ten patients. J Hand Surg Eur Vol. 2020;45(4):389–395. doi: 10.1177/1753193419886536. [DOI] [PubMed] [Google Scholar]
- 15.Starr BW, Ono S, Seyferth A, Chung KC. InternalBrace for intercarpal ligament reconstruction. Plast Reconstr Surg. 2023;151(1):143–147. doi: 10.1097/PRS.0000000000009786. [DOI] [PubMed] [Google Scholar]
- 16.Ahmad K, Al-Najjim M, Malhotra A. Scapholunate ligament reconstruction using the Internal Brace™: a patient-reported outcomes perspective. J Hand Surg Eur Vol. 2023;48(2):151–153. doi: 10.1177/17531934221135072. [DOI] [PubMed] [Google Scholar]
- 17.Park IJ, Lim D, Maniglio M, et al. Comparison of three different internal brace augmentation techniques for scapholunate dissociation: a cadaveric biomechanical study. J Clin Med. 2021;10(7):1482. doi: 10.3390/jcm10071482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berger RA, Bishop AT, Bettinger PC. New dorsal capsulotomy for the surgical exposure of the wrist. Ann Plast Surg. 1995;35(1):54–59. doi: 10.1097/00000637-199507000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Lee SK, Desai H, Silver B, Dhaliwal G, Paksima N. Comparison of radiographic stress views for scapholunate dynamic instability in a cadaver model. J Hand Surg Am. 2011;36(7):1149–1157. doi: 10.1016/j.jhsa.2011.05.009. [DOI] [PubMed] [Google Scholar]
- 20.Larsen CF, Mathiesen FK, Lindequist S. Measurements of carpal bone angles on lateral wrist radiographs. J Hand Surg Am. 1991;16(5):888–893. doi: 10.1016/s0363-5023(10)80156-x. [DOI] [PubMed] [Google Scholar]
- 21.Chan K, Vutescu ES, Wolfe SW, Lee SK. Radiographs detect dorsal scaphoid translation in scapholunate dissociation. J Wrist Surg. 2019;8(3):186–191. doi: 10.1055/s-0038-1677536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Slutsky DJ. Outcomes assessment in wrist surgery. J Wrist Surg. 2013;2(1):1–4. doi: 10.1055/s-0033-1333892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nienstedt F. Treatment of static scapholunate instability with modified Brunelli tenodesis: results over 10 years. J Hand Surg Am. 2013;38(5):887–892. doi: 10.1016/j.jhsa.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 24.Goeminne S, Borgers A, van Beek N, De Smet L, Degreef I. Long-term follow-up of the three-ligament tenodesis for scapholunate ligament lesions: 9-year results. Hand Surg Rehabil. 2021;40(4):448–452. doi: 10.1016/j.hansur.2021.03.020. [DOI] [PubMed] [Google Scholar]
- 25.Elgammal A, Lukas B. Mid-term results of ligament tenodesis in treatment of scapholunate dissociation: a retrospective study of 20 patients. J Hand Surg Eur Vol. 2016;41(1):56–63. doi: 10.1177/1753193415587871. [DOI] [PubMed] [Google Scholar]
- 26.Karanjia R, Rossiter D, Mokhtar MA, Narvani AA, Imam MA. Lunotriquetral ligament repair using augmented internal brace. Arch Bone Jt Surg. 2022;10(5):466–469. doi: 10.22038/ABJS.2021.59167.2944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dugas JR, Walters BL, Beason DP, Fleisig GS, Chronister JE. Biomechanical comparison of ulnar collateral ligament repair with internal bracing versus modified Jobe reconstruction. Am J Sports Med. 2016;44(3):735–741. doi: 10.1177/0363546515620390. [DOI] [PubMed] [Google Scholar]
- 28.Park IJ, Maniglio M, Shin SS, Lim D, McGarry MH, Lee TQ. Internal bracing augmentation for scapholunate interosseous ligament repair: a cadaveric biomechanical study. J Hand Surg Am. 2020;45(10):985. doi: 10.1016/j.jhsa.2020.03.017. [DOI] [PubMed] [Google Scholar]
- 29.Kakar S, Greene RM, Denbeigh J, Van Wijnen A. Scapholunate ligament internal brace 360 tenodesis (SLITT) procedure: a biomechanical study. J Wrist Surg. 2019;8(3):250–254. doi: 10.1055/s-0038-1670682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ho PC, Wong CW, Tse WL. Arthroscopic-assisted combined dorsal and volar scapholunate ligament reconstruction with tendon graft for chronic SL Instability. J Wrist Surg. 2015;4(4):252–263. doi: 10.1055/s-0035-1565927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.de Roo MG, Muurling M, Dobbe JG, Brinkhorst ME, Streekstra GJ, Strackee SD. A four-dimensional-CT study of in vivo scapholunate rotation axes: possible implications for scapholunate ligament reconstruction. J Hand Surg Eur Vol. 2019;44(5):479–487. doi: 10.1177/1753193419830924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sayuri A, Hisao M. Stage classification of scapholunate instability and its pathology. MB Orthop. 2024;37(1):1–7. [Google Scholar]
- 33.Bain GI, Amarasooriya M. Scapholunate instability: why are the surgical outcomes still so far from ideal? J Hand Surg Eur Vol. 2023;48(3):257–268. doi: 10.1177/17531934221148009. [DOI] [PubMed] [Google Scholar]
- 34.Pappou IP, Basel J, Deal DN. Scapholunate ligament injuries: a review of current concepts. Hand (N Y) 2013;8(2):146–156. doi: 10.1007/s11552-013-9499-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Starr BW, Chung KC. InternalBrace for intercarpal ligament reconstruction. Hand Clin. 2023;39(3):379–388. doi: 10.1016/j.hcl.2023.02.008. [DOI] [PubMed] [Google Scholar]
- 36.Chan K, Engasser W, Jebson PJ. Avascular necrosis of the lunate following reconstruction of the scapholunate ligament using the scapholunate axis method (SLAM) J Hand Surg Am. 2019;44(10):904. doi: 10.1016/j.jhsa.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 37.Bain GI, Watts AC, McLean J, Lee YC, Eng K. Cable-augmented, quad ligament tenodesis scapholunate reconstruction: rationale, surgical technique, and preliminary results. Tech Hand Up Extrem Surg. 2013;17(1):13–19. doi: 10.1097/BTH.0b013e31827204ba. [DOI] [PubMed] [Google Scholar]