Abstract
Backgroud
Approximately 5%–7% of patients who have had Achilles tendon rupture (ATR) suffer from contralateral ATR. However, no studies have evaluated the clinical outcomes of contralateral ATR in patients with an existing ATR. Therefore, in this study, we aimed to investigate patient-reported ankle function and activity levels in patients with nonconcurrent bilateral ATR.
Methods
We retrospectively reviewed the data of 222 patients with an acute ATR who presented at our 2 institutions between 2005 and 2017. All patients had a minimum 2-year follow-up period, with no other major injuries to the ankle joint. Of these patients, 17 patients had nonconcurrent bilateral ATR. Patient-reported outcomes were assessed by telephone interview, using the Achilles tendon Total Rupture Score (ATRS), the ankle activity score, and a patient satisfaction questionnaire. Telephonic interviews were conducted by 2 authors, using a prepared script to minimize bias owing to individual interviewers.
Results
The mean age of the patients was 45.1 ± 9.8 years, and 89% were men. Patients with nonconcurrent bilateral ATR had significantly lower values in terms of ATRS, ankle activity score, and satisfaction with current activity level, compared to patients who had unilateral ATR (p < 0.001, p = 0.027, and p = 0.012, respectively).
Conclusions
Patients with nonconcurrent bilateral ATR had poorer ankle function, activity levels, and satisfaction than those with unilateral ATR in terms of patient-reported outcome measures with an intermediate-term result and a 2-year minimum follow-up period. These results emphasize the importance of the impact of contralateral injury on the prognosis of patients with ATR and the need for efforts to prevent contralateral rupture.
Keywords: Ankle, Recovery of function, Outcome assessment, Tendon injuries
The incidence of acute Achilles tendon rupture (ATR) in the general population is 7 to 40 per 100,000 people per year.1,2,3,4,5,6) As a result of growing participation in recreational and competitive sports, the incidence of ATR has increased rapidly in recent decades.2,3,4,7) Along with this trend, the number of patients who suffer a contralateral ATR after unilateral ATR, called nonconcurrent bilateral ATR, is also increasing because the risk of contralateral ATR in patients with unilateral ATR is significantly higher than that of the general population owing to genetic predisposition, degenerative changes, and atrophy of the contralateral tendon.8,9,10,11) Accordingly, interest in the prognosis of nonconcurrent bilateral ATR is gradually increasing.
Although there may be individual differences, depending on the severity and location of the injuries, bilateral injuries in musculotendinous structures are generally known to have a poor prognosis, compared to unilateral injuries. Faltstrom et al.12) reported that in cases of anterior cruciate ligament (ACL) injury, patients with bilateral injuries reported poorer knee function and quality of life compared to those who had unilateral injury. Chang et al.13) found that the clinical outcomes of patients with bilateral quadriceps tendon ruptures were lower than those of patients with similar, but unilateral, injuries. In addition, Nove-Josserand et al.14) reported that patients with bilateral rotator cuff tears seem to have worse occupational outcomes in private sector employed patients.
Having a contralateral ATR in addition to an existing ATR is considerably traumatic for the patient, and this subsequent injury can have a significant impact on the patient’s return to preinjury activities. However, to date, no studies have evaluated the clinical outcomes of contralateral ATR in patients with an existing ATR. Therefore, this study aimed to investigate the patient-reported ankle function and activity level of nonconcurrent bilateral ATR and to compare them with those of patients with unilateral ATR. We hypothesized that patients with nonconcurrent bilateral ATR would report lower values on these parameters, compared with patients with unilateral ATR.
METHODS
This study was approved by the Ethics Committee of Korea University Guro Hospital (IRB No. 2019GR0380), and informed consent was obtained from all enrolled patients via telephone interviews.
Study Design and Patients
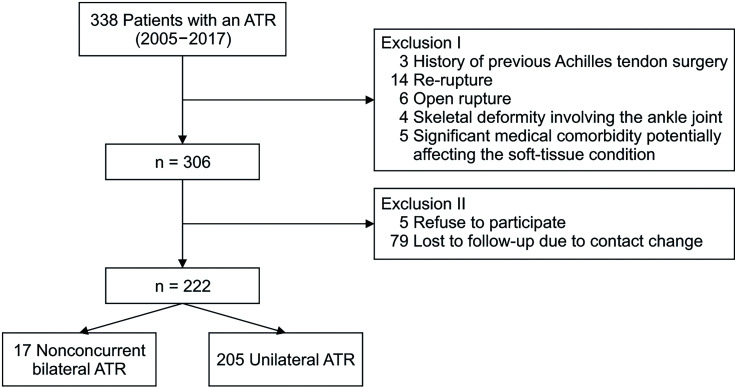
The study had a cross-sectional design. All patients who underwent surgical treatment for their first acute ATR at our 2 institutions (Korea University Guro Hospital, Korea University Ansan Hospital) between 2005 and 2017 were reviewed. This study included the patients from our previous study,8) which investigated the risk factor of nonconcurrent bilateral ATR. Patients were excluded if they had a history of previous surgery of the Achilles tendon, Achilles tendon re-rupture, open rupture, avulsion fracture, skeletal deformities around the ankle joint (varus and valgus deformity of the distal tibia and cavovarus deformity of the calcaneus), or a significant medical comorbidity that would potentially affect the Achilles tendon (hypercholesterolemia with xanthoma, generalized laxity, and uncontrolled diabetes combined with diabetic foot). The occurrence of contralateral ATR in addition to an existing ATR was identified via patient medical records of the emergency department and outpatient clinic. For the cases of contralateral ATR that occurred after the end of the follow-up for the first injury and treated at other institutions, the occurrence of contralateral ATR was also surveyed during telephone interviews. During the 12-year period, 338 patients presented with an acute ATR and 306 patients met the inclusion criteria. Telephone interviews were conducted for this group. Among 306 patients, 205 of 287 patients with unilateral ATR (71.4%) and 17 of 19 patients with nonconcurrent bilateral ATR (89.5%) participated and responded to the questionnaires. Finally, 222 patients were enrolled for the analysis (Fig. 1).
Fig. 1. Flowchart of patient enrollment. ATR: Achilles tendon rupture.
Data Collection
The data for patient demographics and pre-injury activity level were collected from medical records. To assess pre-injury activity level, the ankle activity score (categorizing sports activity from 0 to 10) was used.15) A higher score indicates more intense physical activity. The score was originally developed to indicate sports-related ankle function, but it has also been used to assess the level of sports activity in patients with acute ATR.16) Sports not included in the original ankle activity score were also graded, based on the consensus of 2 authors who were in charge of the telephone interviews (YHP and YBL). Any discrepancies between the 2 authors were resolved by consensus discussion with a third author (HJK).
The Achilles tendon Total Rupture Score (ATRS)17) was used as a primary outcome measurement to evaluate the patient-reported Achilles tendon function, and the questionnaires were completed via a telephone interview. The patients were asked to respond to the 10 items of the ATRS using a 0–10 scale; a score of 0 is equivalent to having major limitations, and a score of 10 is equivalent to having no limitations. The sum of these scales represented the final ATRS value (range, 0–100).
As a second outcome measurement, the current ankle activity level and patient satisfaction with activity were surveyed. As with the pre-injury activity level, the current activity level was scored by the ankle activity score. Patient satisfaction was measured using a 7-point Likert scale with the following question: “ If you had to live with your current ankle function for the rest of your life, would you feel…?” with the following choices: delighted, pleased, mostly satisfied, mixed, mostly dissatisfied, unhappy, and terrible.12,18)
The patients were randomly assigned to the 2 telephone interviewers. To minimize bias due to the individual interviewer, the interviews were conducted based on the scripts prepared in advance, and other conversations that could affect the answers were restricted.
Surgical Treatment and Postoperative Rehabilitation
All the ATRs, including nonconcurrent bilateral ATRs, were surgically repaired using the Krackow suture technique within 1 week after injury. After surgery, a non-weight-bearing short leg splint in 20° plantarflexion was maintained for 2 weeks. Patients were transitioned to tolerable weight-bearing activity with a controlled ankle motion (CAM) boot 2 weeks postoperatively, which was initially set at 20° plantarflexion and gradually increased to neutral at 4–5 weeks following surgery. Patients were weaned from the CAM boot beginning on postoperative week 9 and instructed to start an exercise program. These protocols were identically applied to contralateral ATR patients except for 5 patients who underwent surgical treatment elsewhere.
Statistical Analysis
The normality of the data was determined using the Shapiro-Wilk test. Variables with a normal distribution (age, body mass index, and ATRS) were presented as mean and standard deviation and were analyzed using Student t-test. Variables with non-normal distribution (ankle activity score and time between injury and follow-up) were presented as median and interquartile range and were analyzed using the Mann-Whitney test. Categorical variables such as sex and patient satisfaction were compared using the chi-square test and the diabetes and activity performed at injury were compared using the Fisher exact test. Statistical significance was accepted when p < 0.05. Statistical analyses were performed with IBM SPSS version 23.0 (IBM Corp.). A post-hoc power analysis was performed with G*Power software, version 3.01 (Franz Faul, Christian-Albrechts-Universität Kiel).19)
RESULTS
Patient Characteristics
A summary of the patient characteristics is in Table 1. There was no significant difference in patient characteristics between those having unilateral ATR and those having the first injury of bilateral ATR. The preinjury activity level in 13 patients was not determined because their preferred sports were not categorized on the ankle activity score. Of these, 9 were graded by consensus of the 2 interviewers (kappa coefficient, 0.55), and 4 were graded by the third author. In the bilateral ATR group, the mean age was 36.4 ± 10.0 years (range, 19–61 years) at the first injury and 43.0 ± 8.5 years (range, 30–66 years) at the second injury. The mean time between the first injury and the second injury was 61.3 ± 42.3 months (range, 13–155 months).
Table 1. Characteristics of Patients.
| Variable | Bilateral ATR (n = 17)* | Unilateral ATR (n = 205) | p-value | |
|---|---|---|---|---|
| Age (yr) | ||||
| At injury | 36.4 ± 10.0 (19–61) | 39.3 ± 9.9 (19–66) | 0.296 | |
| Current | 46.7 ± 8.7 (32–68) | 44.6 ± 9.9 (24–72) | 0.429 | |
| Sex | 0.702 | |||
| Male | 16 (94.1) | 182 (88.8) | ||
| Female | 1 (5.9) | 23 (11.2) | ||
| BMI (kg/m2) | 23.0 ± 2.8 (18.8–25.5)† | 25.2 ± 3.1 (17.7–36.3) | 0.154 | |
| Diabetes | 1 (5.9) | 8 (3.9) | 0.519 | |
| Activity performed at injury | 0.476 | |||
| Football | 6 (35.3) | 66 (32.2) | ||
| Foot volleyball | 3 (17.6) | 23 (11.2) | ||
| Basketball | 4 (23.5) | 21 (10.2) | ||
| Badminton | 0 | 19 (9.3) | ||
| Jogging | 2 (11.8) | 16 (7.8) | ||
| Volleyball | 0 | 11 (5.4) | ||
| Tennis | 0 | 8 (3.9) | ||
| Jump rope | 1 (5.9) | 6 (2.9) | ||
| Other sports (baseball, ballet, skiing, etc.) | 0 | 20 (9.8) | ||
| Daily living activities | 1 (5.9) | 15 (7.3) | ||
Values are presented as mean ± standard deviation (range) or number (%).
ATR: Achilles tendon rupture, BMI: body mass index.
*Data at the time of the first Achilles tendon rupture. †n = 12 (5 missing) as 5 patients were treated elsewhere.
Achilles Tendon Function and Activity Level
Results of the questionnaires for patient-reported outcomes are summarized in Table 2. The ATRS of the second injured ankle of the bilateral ATR group was significantly lower than that of the unilateral ATR group, but the ATRS of the first injured ankle of the bilateral ATR group did not show significance, despite its trend of having a lower score than the unilateral ATR group.
Table 2. Results of the Questionnaires for Patient-Reported Outcomes.
| Variable | Bilateral ATR (n = 17) | Unilateral ATR (n = 205) | p-value | |
|---|---|---|---|---|
| ATRS | ||||
| First injured ankle | 81.2 ± 11.2 (61–100) | 86.8 ± 11.8 (31–100) | 0.056 | |
| Second injured ankle | 75.7 ± 10.7 (57–92) | - | < 0.001* | |
| Ankle activity score | ||||
| Before the first injury | 8 (4–8, 6–8) | 7 (3–9, 5–8) | 0.103 | |
| Before the second injury | 6 (3–8, 5–7) | - | 0.390† | |
| At follow-up | 5 (2–7, 4–6) | 6 (3–8, 5–7) | 0.027 | |
| Satisfaction with current activity level | 0.012 | |||
| Delighted to pleased | 1 (5.9) | 86 (42.0) | ||
| Unhappy to terrible | 5 (29.4) | 35 (17.1) | ||
| Time between injury and follow-up (mo) | ||||
| From the first injury | 122 (42–293, 69–162) | 69 (24–174, 39–97) | < 0.001 | |
| From the second injury | 58 (24–138, 28–77) | - | 0.135‡ | |
Values are presented as mean ± standard deviation (range), median (range, interquartile range), or number (%).
ATR: Achilles tendon rupture, ATRS: Achilles tendon Total Rupture Score.
*ATRS of the second injured ankle compared to that of unilateral ATR patients. †Ankle activity score before the second injury compared to that of unilateral ATR patients at follow-up. ‡Time between the second injury and follow-up compared to time between the first injury and follow-up for unilateral ATR patients.
The ankle activity scores of the bilateral ATR group (before the first injury) were similar to those of the unilateral ATR group. Before their second injury, the ankle activity scores in the bilateral ATR group recovered after the first injury but showed no significant difference compared to follow-up ankle activity scores in the unilateral ATR group. However, after the second injury, the follow-up ankle activity score of the bilateral ATR group was significantly lower than that of the unilateral ATR group. When the patients were asked about their satisfaction with their current activity level, those in the bilateral ATR group were less satisfied than those in the unilateral ATR group.
Post-Hoc Power Analysis
A post-hoc power analysis indicated that this study had 0.99 power to detect an effect size of 1.49 in ATRS between the bilateral ATR and unilateral ATR groups, with a type I error probability of 0.05.
DISCUSSION
The primary finding of this study is that the patients with nonconcurrent bilateral ATR showed poorer self-reported Achilles function than the patients with unilateral ATR at a minimum 2-year follow-up after their second injury. The reduced Achilles tendon function significantly affected their prognosis; at follow-up, the return to the pre-injury activity and activity level in patients who had nonconcurrent bilateral ATR was lower compared to patients who had unilateral ATR. Satisfaction with the current activity level was also lower in nonconcurrent bilateral ATR, reflecting functional outcomes.
Generally, assessment of patient-reported outcomes is performed by the patients filling out questionnaires themselves, following instructions provided by investigators. Therefore, there may be concerns about the use of telephone interviews to fill out the questionnaires in our study. However, assessment of patient-reported outcomes by telephone interview has often been used in previous studies, not only ATRS,20) but also other questionnaires for the Achilles tendon,21,22,23,24) either alone or in combination with email surveys. In the study of ATR, the long-term follow-up visit for clinical evaluation is difficult because the majority of ATR patients have returned to their daily activities and recreational sports satisfactorily, although their function has been somewhat reduced. Therefore, considering the incidence of nonconcurrent bilateral ATR, the authors thought that a telephone interview technique, which could involve a large number of patients, was the best option.
The ATRS, which is a primary outcome measure of this study, is derived from a validated questionnaire; it is widely used to evaluate the outcome of ATR. Nilsson-Helander et al.25) reported a mean of 88 points at 1-year follow-up after surgery, and Olsson et al.26) reported a mean of 90 points at their 2-year follow-up. In a long-term follow-up, Rosso et al.27) reported a mean score of 91 at 8 years after surgery. In our study, the ATRS in the unilateral ATR group showed a mean score of 87 points, which was considered comparable to the scores in previous studies because a 10-point difference was reported to have clinical relevance.17) However, the second injured side, in the cases of bilateral ATR, showed a mean ATRS score of 76 points, indicating that these patients reported impaired Achilles tendon function, compared to previous studies and our control group.
In this study, the ankle activity score after the first injury was not different between bilateral ATR and unilateral ATR cases, but the final ankle activity score of the cases of bilateral ATR after the second injury was significantly lower than that of the cases of unilateral ATR. Compared to the first injury, the impact of contralateral injury on the prognosis of the patients with ATR was substantial. As the clinical outcomes in nonconcurrent bilateral ATR were worse than those in unilateral ATR, the authors thought that the strength and flexibility of the second ruptured Achilles tendon may have played a role in the poor clinical symptoms of these patients, although the psychological factors of these patients related to additional rupture may also have played a role.28) Therefore, knowledge of the risk factors of bilateral ATR is important to help prevent contralateral injury. However, in contrast to bilateral ACL injury, for which many risk factors (being female, adolescent, high activity level, etc.) have been found to be related to contralateral injury,29,30,31) there was only 1 study investigating the risk factors of bilateral ATR, which found that patients who suffered ATR in their 30s had an increased risk of contralateral injury.8) The authors thought the lack of study on the risk factors for bilateral ATR was due to the relatively small number of patients with bilateral ATR at each institution. Studies involving a large number of patients may reveal factors other than age, so further multicenter studies are needed.
This study has 3 limitations. First, we only evaluated patients’ subjective outcomes related to their perception of health status, activity level, and satisfaction, without objective assessments for ankle function, such as muscle strength or stiffness of the Achilles tendon. Additionally, we relied solely on telephone interviews, which have not been commonly used in the literature. This was inevitable because of the small number of patients who visited for an objective assessment. Therefore, the purpose of the study was confined to the investigation of patient-reported outcomes. Thus, readers should be mindful of this limitation when accepting our findings, as patient’s subjective outcomes do not always correspond to their objective outcomes. Second, this study has a possibility of interviewer bias. Since the answers to the questionnaire could have been affected by what the interviewers “wanted to hear,” outcome assessment over the telephone is inherently vulnerable to interviewer bias. Although the interviews were performed based on the scripts prepared in advance (to minimize the influence from the interviewer), the possibility of bias cannot be completely excluded. Third, the patients in this study underwent surgical treatment by different orthopedic surgeons. Thus, according to the surgeons, an initial concern regarding bias in the results existed. However, except for 5 surgeries performed elsewhere, all surgeries were performed in our 2 chosen institutions with similar surgical timing, surgical method, and rehabilitation protocols. Additionally, there was no difference in the overall outcomes between the surgeons and institutions in the preliminary result comparison conducted before the start of the study. Therefore, it is unlikely that the surgeon’s identity significantly affected the results of this study.
In conclusion, patients with nonconcurrent bilateral ATR reported poorer ankle function, activity level, and satisfaction than those with unilateral ATR having an intermediate-term result with a 2-year minimum follow-up. They had a similar activity level to patients with unilateral ATR after their first injury, but showed an impaired activity level after their contralateral injury. These results emphasize the importance of the impact of contralateral injury on the prognosis of patients with ATR and the need of efforts to prevent contralateral rupture.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Houshian S, Tscherning T, Riegels-Nielsen P. The epidemiology of Achilles tendon rupture in a Danish county. Injury. 1998;29(9):651–654. doi: 10.1016/s0020-1383(98)00147-8. [DOI] [PubMed] [Google Scholar]
- 2.Huttunen TT, Kannus P, Rolf C, Fellander-Tsai L, Mattila VM. Acute achilles tendon ruptures: incidence of injury and surgery in Sweden between 2001 and 2012. Am J Sports Med. 2014;42(10):2419–2423. doi: 10.1177/0363546514540599. [DOI] [PubMed] [Google Scholar]
- 3.Maffulli N, Waterston SW, Squair J, Reaper J, Douglas AS. Changing incidence of Achilles tendon rupture in Scotland: a 15-year study. Clin J Sport Med. 1999;9(3):157–160. doi: 10.1097/00042752-199907000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Nyyssonen T, Luthje P, Kroger H. The increasing incidence and difference in sex distribution of Achilles tendon rupture in Finland in 1987-1999. Scand J Surg. 2008;97(3):272–275. doi: 10.1177/145749690809700312. [DOI] [PubMed] [Google Scholar]
- 5.Suchak AA, Bostick G, Reid D, Blitz S, Jomha N. The incidence of Achilles tendon ruptures in Edmonton, Canada. Foot Ankle Int. 2005;26(11):932–936. doi: 10.1177/107110070502601106. [DOI] [PubMed] [Google Scholar]
- 6.Park HG, Youn D, Baik JM, Hwang JH. Epidemiology of Achilles tendon rupture in South Korea: claims data of the National Health Insurance Service from 2009 to 2017. Clin Orthop Surg. 2021;13(4):539–548. doi: 10.4055/cios20255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lantto I, Heikkinen J, Flinkkila T, Ohtonen P, Leppilahti J. Epidemiology of Achilles tendon ruptures: increasing incidence over a 33-year period. Scand J Med Sci Sports. 2015;25(1):e133–e138. doi: 10.1111/sms.12253. [DOI] [PubMed] [Google Scholar]
- 8.Park YH, Kim TJ, Choi GW, Kim HJ. Age is a risk factor for contralateral tendon rupture in patients with acute Achilles tendon rupture. Knee Surg Sports Traumatol Arthrosc. 2020;28(5):1625–1630. doi: 10.1007/s00167-019-05380-y. [DOI] [PubMed] [Google Scholar]
- 9.Aroen A, Helgo D, Granlund OG, Bahr R. Contralateral tendon rupture risk is increased in individuals with a previous Achilles tendon rupture. Scand J Med Sci Sports. 2004;14(1):30–33. doi: 10.1111/j.1600-0838.2004.00344.x. [DOI] [PubMed] [Google Scholar]
- 10.Raikin SM, Garras DN, Krapchev PV. Achilles tendon injuries in a United States population. Foot Ankle Int. 2013;34(4):475–480. doi: 10.1177/1071100713477621. [DOI] [PubMed] [Google Scholar]
- 11.Park SH, Lee HS, Young KW, Seo SG. Treatment of acute Achilles tendon rupture. Clin Orthop Surg. 2020;12(1):1–8. doi: 10.4055/cios.2020.12.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Faltstrom A, Hagglund M, Kvist J. Patient-reported knee function, quality of life, and activity level after bilateral anterior cruciate ligament injuries. Am J Sports Med. 2013;41(12):2805–2813. doi: 10.1177/0363546513502309. [DOI] [PubMed] [Google Scholar]
- 13.Chang ES, Dodson CC, Tjoumakaris F, et al. Functional results following surgical repair of simultaneous bilateral quadriceps tendon ruptures. Phys Sportsmed. 2014;42(2):114–118. doi: 10.3810/psm.2014.05.2063. [DOI] [PubMed] [Google Scholar]
- 14.Nove-Josserand L, Liotard JP, Godeneche A, et al. Occupational outcome after surgery in patients with a rotator cuff tear due to a work-related injury or occupational disease: a series of 262 cases. Orthop Traumatol Surg Res. 2011;97(4):361–366. doi: 10.1016/j.otsr.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 15.Halasi T, Kynsburg A, Tallay A, Berkes I. Development of a new activity score for the evaluation of ankle instability. Am J Sports Med. 2004;32(4):899–908. doi: 10.1177/0363546503262181. [DOI] [PubMed] [Google Scholar]
- 16.Young SW, Patel A, Zhu M, et al. Weight-bearing in the nonoperative treatment of acute Achilles tendon ruptures: a randomized controlled trial. J Bone Joint Surg Am. 2014;96(13):1073–1079. doi: 10.2106/JBJS.M.00248. [DOI] [PubMed] [Google Scholar]
- 17.Nilsson-Helander K, Thomee R, Silbernagel KG, et al. The Achilles tendon Total Rupture Score (ATRS): development and validation. Am J Sports Med. 2007;35(3):421–426. doi: 10.1177/0363546506294856. [DOI] [PubMed] [Google Scholar]
- 18.Cherkin DC, Deyo RA, Street JH, Barlow W. Predicting poor outcomes for back pain seen in primary care using patients’ own criteria. Spine (Phila Pa 1976) 1996;21(24):2900–2907. doi: 10.1097/00007632-199612150-00023. [DOI] [PubMed] [Google Scholar]
- 19.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 20.Bakowski P, Rubczak S, Wolff-Stefaniak M, Grygorowicz M, Piontek T. Reliability and validity of the Polish version of the Achilles tendon Total Rupture Score. Knee Surg Sports Traumatol Arthrosc. 2018;26(7):2074–2079. doi: 10.1007/s00167-017-4764-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Strauss EJ, Ishak C, Jazrawi L, Sherman O, Rosen J. Operative treatment of acute Achilles tendon ruptures: an institutional review of clinical outcomes. Injury. 2007;38(7):832–838. doi: 10.1016/j.injury.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 22.Ingvar J, Tagil M, Eneroth M. Nonoperative treatment of Achilles tendon rupture: 196 consecutive patients with a 7% re-rupture rate. Acta Orthop. 2005;76(4):597–601. doi: 10.1080/17453670510041619. [DOI] [PubMed] [Google Scholar]
- 23.Fox G, Gabbe BJ, Richardson M, et al. Twelve-month outcomes following surgical repair of the Achilles tendon. Injury. 2016;47(10):2370–2374. doi: 10.1016/j.injury.2016.07.013. [DOI] [PubMed] [Google Scholar]
- 24.Stauff MP, Kilgore WB, Joyner PW, Juliano PJ. Functional outcome after percutaneous tendo-Achilles lengthening. Foot Ankle Surg. 2011;17(1):29–32. doi: 10.1016/j.fas.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 25.Nilsson-Helander K, Silbernagel KG, Thomee R, et al. Acute achilles tendon rupture: a randomized, controlled study comparing surgical and nonsurgical treatments using validated outcome measures. Am J Sports Med. 2010;38(11):2186–2193. doi: 10.1177/0363546510376052. [DOI] [PubMed] [Google Scholar]
- 26.Olsson N, Nilsson-Helander K, Karlsson J, et al. Major functional deficits persist 2 years after acute Achilles tendon rupture. Knee Surg Sports Traumatol Arthrosc. 2011;19(8):1385–1393. doi: 10.1007/s00167-011-1511-3. [DOI] [PubMed] [Google Scholar]
- 27.Rosso C, Vavken P, Polzer C, et al. Long-term outcomes of muscle volume and Achilles tendon length after Achilles tendon ruptures. Knee Surg Sports Traumatol Arthrosc. 2013;21(6):1369–1377. doi: 10.1007/s00167-013-2407-1. [DOI] [PubMed] [Google Scholar]
- 28.Slagers AJ, Dams OC, van Zalinge SD, et al. Psychological factors change during the rehabilitation of an Achilles tendon rupture: a multicenter prospective cohort study. Phys Ther. 2021;101(12):pzab226. doi: 10.1093/ptj/pzab226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maletis GB, Inacio MC, Funahashi TT. Risk factors associated with revision and contralateral anterior cruciate ligament reconstructions in the Kaiser Permanente ACLR registry. Am J Sports Med. 2015;43(3):641–647. doi: 10.1177/0363546514561745. [DOI] [PubMed] [Google Scholar]
- 30.Snaebjornsson T, Hamrin Senorski E, Sundemo D, et al. Adolescents and female patients are at increased risk for contralateral anterior cruciate ligament reconstruction: a cohort study from the Swedish National Knee Ligament Register based on 17,682 patients. Knee Surg Sports Traumatol Arthrosc. 2017;25(12):3938–3944. doi: 10.1007/s00167-017-4517-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sward P, Kostogiannis I, Roos H. Risk factors for a contralateral anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2010;18(3):277–291. doi: 10.1007/s00167-009-1026-3. [DOI] [PubMed] [Google Scholar]