Abstract
Background
Carpal tunnel syndrome (CTS) and trigger finger are representative pathologic conditions of the hand. Although several studies have evaluated the epidemiology of these diseases as nationwide population-based research, they had several limitations including old data and short study period.
Methods
We conducted a retrospective cohort study of patients aged ≥ 20 years diagnosed with CTS or trigger finger between 2009 and 2019 using the Korean Health Insurance Review and Assessment Service database. The annual incidence of these diseases was standardized based on age and sex. The proportion of patients who received corticosteroid injections or surgery within 1 year of their diagnoses was calculated annually.
Results
The mean annual incidence of CTS was 360.26 per 100,000 person-years and that of trigger finger was 63.09 per 100,000 person-years. The annual incidence of CTS (incidence rate ratio [IRR], 0.979; 95% confidence interval [CI], 0.972–0.985; p < 0.001) and trigger finger (IRR, 0.976; 95% CI, 0.967–0.985; p < 0.001) significantly decreased. The proportion of patients who received corticosteroid injections for CTS significantly increased (relative risk [RR], 1.025; 95% CI, 1.020–1.031; p < 0.001), while the number of surgeries significantly decreased (RR, 0.949; 95% CI, 0.940–0.957; p < 0.001). The proportion of patients who received corticosteroid injections for trigger finger significantly increased (RR, 1.021; 95% CI, 1.009–1.033; p < 0.001), while the number of surgeries did not change significantly (RR, 1.006; 95% CI, 0.988–1.023; p = 0.523).
Conclusions
In the past 10 years, the incidence of CTS and trigger finger decreased. The portion of patients who received corticosteroid injections increased for both diseases, but the portion of patients who had surgery decreased for CTS within 1 year after diagnosis. This study provides insight into the epidemiology of these diseases in an Asian population and may inform estimates of healthcare costs.
Keywords: Carpal tunnel syndrome, Epidemiology, Trigger finger
Carpal tunnel syndrome (CTS) and trigger finger are representative pathologic conditions of the hand.1,2,3,4) CTS is the most common compressive neuropathy of the upper extremities and presents with a tingling sensation or numbness in the region of the median nerve and/or atrophy of the thenar muscles.5,6) Trigger finger is stenosing tenosynovitis of the finger flexor tendon caused by inflammation around the flexor tendon and narrowing of the A1 pulley.2,7) Patients with trigger finger present with pain or triggering when the finger is flexed.2) Since these 2 representative hand diseases are very common, it is important to understand their epidemiology considering their socioeconomic burden.
Several nationwide, population-based studies have evaluated the epidemiology of CTS. However, these studies have several limitations including outdated data,8,9,10) short study duration,8,10) a focus on prevalence rather than incidence,8) and incomplete coverage of the entire population.11) Even fewer studies have evaluated the epidemiology of trigger finger in an entire population.
Since the treatment strategies for specific diseases are highly dependent on clinicians and patients, whole population-based information is useful for understanding the treatment status for specific diseases.6,12,13,14) The purpose of this study was to analyze the epidemiology and treatment status of CTS and trigger finger in a nationwide, population-based cohort. Therefore, we asked the following questions. (1) What are the incidence and prevalence of CTS and trigger finger? (2) What are the trends of incidence and prevalence of CTS and trigger finger over 10 years? (3) What are the trends of CTS and trigger finger in treatments applied over 10 years, including corticosteroid injections and surgery?
METHODS
This study protocol was exempted from review by the Institutional Review Board of Asan Medical Center (No. 2021-0975) in accordance with the exemption criteria. Informed consent was not required for this study, as it was a retrospective cohort study.
Data Source
In Korea, the National Health Insurance Service covers 100% of the population; 97% have health insurance and 3% have medical aid.15) All healthcare providers submit claims data for inpatient and outpatient management to the Health Insurance Review and Assessment service (HIRA) for reimbursement of medical costs. These include diagnosis codes (classified according to the International Classification of Diseases, 10th revision [ICD-10]), procedure codes, medication codes, and demographic information. HIRA provides some of this national data to support public policy development and research activities when requested.
Data Collection and Analysis
We identified patients aged ≥ 20 years who were diagnosed with CTS (G560) or trigger finger (M653) between 2009 and 2019 in the HIRA database. More specifically, we identified patients with CTS or trigger finger only when the diagnosis codes for both diseases were registered as the main diagnosis or first accessory diagnosis. This was done to prevent overestimation of the number of patients and to accurately assess their treatment status. For these cohorts, demographic information and all applied diagnosis, procedure, and medication codes between 2009 and 2020 were identified. Since incidence refers to a measure of the number of new cases of a characteristic that develop in a population in a specified time period,16) we set a washout period of more than 1 year to ensure patients newly diagnosed with either disease were included. Therefore, patients newly diagnosed with CTS or trigger finger between 2010 and 2019 were analyzed to yield the incidence. On the other hand, prevalence represents the proportion of a population with a specific characteristic over a given time period, regardless of when they first developed the characteristic.16) So, the total number of patients treated under the diagnosis code of CTS or trigger finger was identified to evaluate the prevalence of both diseases between 2009 and 2019.
For treatment status, registered patients with prescriptions for injectable corticosteroid injections (triamcinolone acetonide or dexamethasone) under the diagnostic code of each disease were defined as receiving corticosteroid injections for CTS or trigger finger. In addition, patients registered with operation codes under the diagnostic code of each disease were defined as having surgery. We identified all possible codes for the surgical treatment of CTS or trigger finger (Table 1). Since the data were collected until the end of 2020, treatments conducted within at least 1 year of the initial diagnosis were included. In addition, we set the available period of the initial diagnosis as 5 years to prevent overestimation of the treatments.17,18) For patients who underwent several corticosteroid injections or surgeries based on the diagnostic codes, only the first event was analyzed since we could not evaluate the laterality of the involved hand and the location of the involved digit.
Table 1. Available Operation Codes of Health Insurance Review and Assessment Service of South Korea for Carpal Tunnel Syndrome or Trigger Finger.
| Disease | Description | Code |
|---|---|---|
| Carpal tunnel syndrome or trigger finger | Reconstruction of tendon and ligament | N0931 (simple: resection, suture, or release) and N0932 (complex: graft, transfer, or reconstruction with allograft) |
| Excision of the joint, including synovectomy | N0704 (finger) | |
| Carpal tunnel syndrome only | Neuroplasty | S4595 (major peripheral plexus) and S4596 (hand) |
| Trigger finger only | Operation for trigger finger | N0830 |
| Fasciotomy | N0922 (simple) |
The annual incidence and prevalence were standardized by age and sex based on the population in 2015 to analyze the annual trends of incidence and prevalence of these diseases. In addition, the ratios of surgeries and corticosteroid injections performed within 1 year of diagnosis were calculated to analyze the annual treatment trends for both diseases during the study period.
Statistical Analysis
Continuous data are presented as means ± standard deviations (SDs), and categorical data are presented as numbers and percentages. We calculated the annual incidence and prevalence of CTS and trigger finger (per 100,000 person-years) in men and women assuming a Poisson distribution. Poisson regression analysis was used to analyze trends in the annual incidence and prevalence of each disease and the number of corticosteroid injections and surgeries received as treatment for each disease. A p-value < 0.05 was interpreted as statistically significant. All statistical analyses were performed using the SAS Enterprise Guide software version 7.1 (SAS Institute).
RESULTS
Incidence and Prevalence of CTS and Trigger Finger
A total of 1,449,284 patients ≥ 20 years old were newly registered with CTS from 2010 to 2019 including 392,226 men and 1,057,058 women. The mean annual incidence of CTS was 360.26 per 100,000 person-years (95% confidence interval [CI], 359.67–360.85), and it was significantly higher in women (519.82 per 100,000 person-years; 95% CI, 518.83–520.81) than men (197.16 per 100,000 person-years; 95% CI, 196.55–197.78) (p < 0.001). In addition, a total of 253,817 patients over the age of 20 years were newly registered with trigger finger from 2010 to 2019 including 43,595 men and 210,222 women. The mean annual incidence of trigger finger was 63.09 per 100,000 person-years (95% CI, 62.85–63.34), and it was also significantly higher in women (103.38 per 100,000 person-years; 95% CI, 102.94–103.82) than men (21.91 per 100,000 person-years; 95% CI, 21.71–22.12) (p < 0.001) (Table 2).
Table 2. Incidence and Total Number of Patients with Carpal Tunnel Syndrome and Trigger Finger According to Age and Sex.
| Age | Carpal tunnel syndrome | Trigger finger | ||||
|---|---|---|---|---|---|---|
| Male | Female | Total | Male | Female | Total | |
| 20–29 yr | 78.53 (27,626) | 131.44 (42,017) | 103.72 (69,643) | 5.06 (1,781) | 8.28 (2,647) | 6.59 (4,428) |
| 30–39 yr | 128.08 (50,686) | 256.31 (972,271) | 190.85 (147,957) | 11.21 (4,435) | 24.31 (9,226) | 17.62 (13,661) |
| 40–49 yr | 189.27 (83,336) | 533.08 (227,313) | 358.42 (310,649) | 21.34 (9,395) | 84.99 (36,240) | 52.65 (45,635) |
| 50–59 yr | 280.83 (111,331) | 1014.62 (398,311) | 645.93 (509,642) | 34.12 (13,527) | 266.10 (104,462) | 149.54 (117,989) |
| 60–69 yr | 323.86 (76,072) | 718.59 (179,836) | 527.48 (255,908) | 40.51 (9,515) | 163.37 (40,886) | 103.89 (50,401) |
| 70–79 yr | 272.29 (35,570) | 506.40 (88,862) | 406.49 (124,432) | 31.55 (4,122) | 80.39 (14,106) | 59.55 (18,228) |
| ≥ 80 yr | 192.38 (7,605) | 261.65 (23,448) | 240.45 (31,053) | 20.74 (820) | 29.63 (2,655) | 26.91 (3,475) |
| Total | 197.16 (392,226) | 519.82 (1,057,058) | 360.26 (1,449,284) | 21.91 (43,595) | 103.38 (210,222) | 63.09 (253,817) |
Values are indicated as incidence per 100,000 person-years (number of patients).
From 2009 to 2019, the total number of adults over the age of 20 years was 440,115,756 in Korea.19) A total of 2,448,100 patients were diagnosed with CTS during this period, of whom 560,309 were men and 1,887,791 were women. The mean prevalence of CTS was 556.24 per 100,000 person-years, 848.41 per 100,000 person-years for women, and 257.49 per 100,000 person-years for men. During the same period, the total number of patients over the age of 20 years diagnosed with trigger finger was 493,634, of whom 80,736 were men and 412,898 were women. The mean prevalence of trigger finger was 112.16 per 100,000 person-years, 185.56 per 100,000 person-years for women, and 37.10 per 100,000 person-years for men.
Annual Trends of Incidence and Prevalence of CTS and Trigger Finger
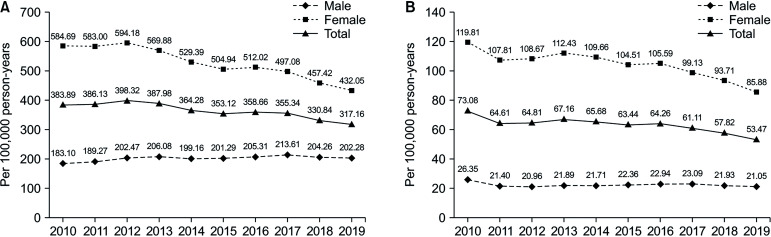
The annual incidence of CTS (incidence rate ratio [IRR], 0.979; 95% CI, 0.972–0.985; p < 0.001) and trigger finger (IRR, 0.976; 95% CI, 0.967–0.985; p < 0.001) significantly decreased during the study period. This decrease was more evident in women with CTS (IRR, 0.967; 95% CI, 0.960–0.974; p < 0.001) or trigger finger (IRR, 0.973; 95% CI, 0.964–0.982; p < 0.001). For men, the incidence of CTS (IRR, 1.010; 95% CI, 1.003–1.017; p < 0.001) was significantly increased, but that of trigger finger (IRR, 0.992; 95% CI, 0.977–1.007; p = 0.292) did not change significantly (Fig. 1).
Fig. 1. The age- and sex-standardized annual incidence (per 100,000 person-years) of carpal tunnel syndrome (A) and trigger finger (B).
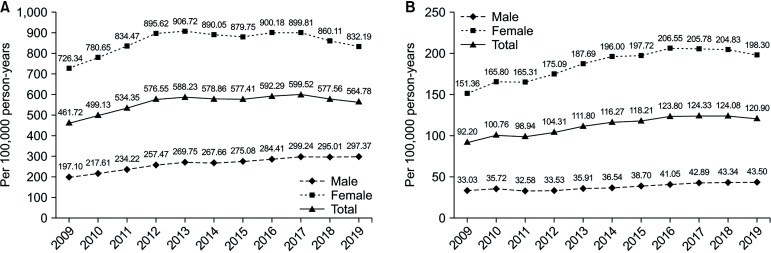
In contrast to the incidence, the annual prevalence of CTS (prevalence ratio [PR], 1.017; 95% CI, 1.006–1.028; p = 0.002) and trigger finger (PR, 1.030; 95% CI, 1.022–1.037; p < 0.001) significantly increased during the study period. This increase was more evident in men with CTS (PR, 1.038; 95% CI, 1.028–1.047; p < 0.001) or trigger finger (PR, 1.032; 95% CI, 1.025–1.040; p < 0.001). For women, the prevalence of CTS (PR, 1.011; 95% CI, 0.99950–1.023; p = 0.060) did not change significantly, but that of trigger finger (PR, 1.029; 95% CI, 1.020–1.038; p < 0.001) increased significantly (Fig. 2).
Fig. 2. The age- and sex-standardized annual prevalence (per 100,000 person-years) of carpal tunnel syndrome (A) and trigger finger (B).
Age and Sex Differences in the Incidence of CTS and Trigger Finger
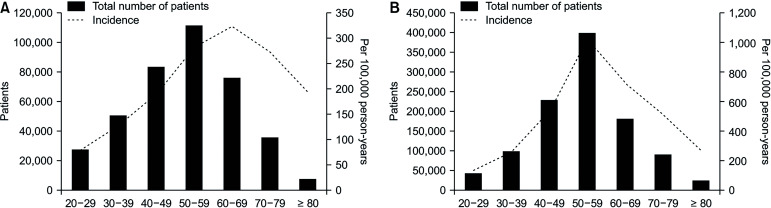
For both diseases, women of all ages had a higher incidence compared with men of the same age, especially those in their 50s. In addition, women showed a peak incidence of both diseases from 50 to 59 years of age, while men showed a peak incidence from 60 to 69 years of age. However, the number of patients for both diseases was highest from 50 to 59 years of age in both men and women (Table 2, Figs. 3 and 4).
Fig. 3. The total number of patients and incidence (per 100,000 person-years) of carpal tunnel syndrome according to age group in men (A) and women (B).
Fig. 4. The total number of patients and incidence (per 100,000 person-years) of trigger finger according to age group in men (A) and women (B).
Treatment Status of CTS and Trigger Finger
Among 1,449,284 patients who were newly diagnosed with CTS from 2010 to 2019, 173,202 patients (12.0%) had operations and 415,364 patients (28.7%) had corticosteroid injections. The median time to operation from the diagnosis was 52 days (interquartile range [IQR], 7–455 days). Among 415,364 patients who had corticosteroid injections, triamcinolone was prescribed in 336,816 patients (81.1%) and dexamethasone was prescribed in 116,390 patients (28.0%).
Among 253,817 patients who were newly diagnosed with trigger finger from 2010 to 2019, 13,839 patients (5.5%) had operations and 120,548 patients (47.5%) had corticosteroid injections. The median time to operation from the diagnosis was 33 days (IQR, 1–451 days). Among 120,548 patients who had corticosteroid injections, triamcinolone was prescribed in 108,070 patients (89.6%) and dexamethasone was prescribed in 23,014 patients (19.1%).
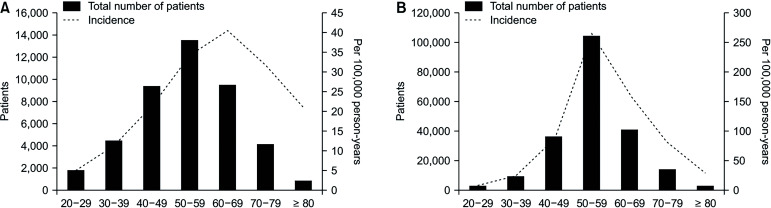
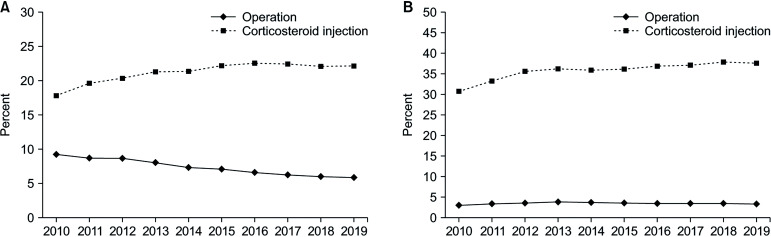
Within 1 year after diagnosis, 8.6% of CTS patients underwent surgeries, and 24.6% received corticosteroid injections. In addition, 3.9% of trigger finger patients underwent surgeries, and 41.6% received corticosteroid injections within 1 year of diagnosis. The annual surgery ratio (relative risk [RR], 0.949; 95% CI, 0.940–0.957; p < 0.001) significantly decreased, while the annual ratio of corticosteroid injections (RR, 1.025; 95% CI, 1.020–1.031; p < 0.001) significantly increased in CTS. For trigger finger, the annual surgery ratio (RR, 1.006; 95% CI, 0.988–1.023; p = 0.523) did not change significantly, but the annual ratio of corticosteroid injections (RR, 1.021; 95% CI, 1.009–1.033; p < 0.001) increased significantly (Fig. 5).
Fig. 5. The ratio of patients who had surgery and corticosteroid injections within 1 year of diagnosis. (A) Carpal tunnel syndrome. (B) Trigger finger.
DISCUSSION
In this study, the incidence of CTS was 360.26 per 100,000 person-years, and it was higher in women than men by 2.64 times. In previous studies, the incidences of CTS varied from 276 to 496 per 100,000 person-years, and the ratios of incidences of women to men ranged from 2 to 3.6, which is comparable with the results of this study.9,10,14,20) The incidence of CTS was higher in studies, in which clinical criteria were applied for the diagnosis of CTS.1,10) For women, the incidence of CTS peaked in their 50s, which is similar to previous studies.9,10,21) For men, the incidence of CTS peaked in their 60s. The peak incidences in men varied among studies between their 50s and 70s;10,11,21) the reason for this phenomenon is not evident. Several studies have indicated there could be effects of occupation and physical work intensity on the incidence of CTS, especially in men.11,22) Further studies are needed to clarify this point. The incidence of trigger finger was 63.09 per 100,000 person-years, and it was higher in women than in men by 4.72 times. Unlike CTS, the epidemiology of trigger finger has not been well-studied. The age groups of peak incidences for trigger finger in women and men were similar to those of CTS. This similarity could be explained by the common pathophysiology of these 2 diseases.8)
During the past 10 years, the incidence of both diseases has decreased significantly, but their prevalence has significantly increased. To explain this, we should consider trends in treatment status and risk factors for both diseases and the life expectancy of the population. One possible explanation is that as social awareness of both diseases increases, patients at high risk for both conditions are more cautious about excessive use of their hands and may visit the clinic with mild symptoms before meeting the diagnostic criteria of both diseases. Further studies are needed to validate this hypothesis. The increased number of patients with mild symptoms could be related to the increased portion of patients who were treated with less invasive corticosteroid injections. Since considerable numbers of patients experience symptom relapse after treatment using corticosteroid injections for both diseases,23,24) the treatment periods for both diseases could be elongated over time, which could be related to their increased prevalence. In terms of risk factors for both diseases, the incidence of hypothyroidism in Korean women decreased from 2012 to 2015,25) but the prevalence of menopausal hormone therapy did not change significantly from 2009 to 2013.26) In addition, the prevalence of rheumatoid arthritis increased from 2012 to 2016 in Korea.27) Therefore, we were unable to confirm the impact of epidemiological changes in specific risk factors on the incidence or prevalence of these diseases. Instead, the increased average life expectancy of the Korean population from 80.2 years in 2010 to 83.3 years in 201919) could influence the increased prevalence of both diseases.
The portion of patients who had surgery was low for both diseases: 12.0% for CTS and 5.5% for trigger finger. This could be explained by the wide coverage of the population by the Korean national insurance system and the highly accessible medical care of Korean citizens.28) Since patients could be diagnosed and treated in the early stages of CTS and trigger finger, less invasive conservative treatments would be needed. In addition, many conservative treatments, including corticosteroid injections, are covered by the national insurance system; therefore, patients are less reluctant to pay for repeated conservative management after treatment failure. This could be related to increased treatment using corticosteroid injections for both diseases in the past 10 years.
Like any registry study, our research has several limitations. First, the data source is a registry that is imperfect for accurately identifying all CTS and trigger finger cases. Confirmation of diagnoses for both diseases typically requires clinical assessment by specialists. Second, since HIRA data did not provide information about the laterality of the involved hand and the location of the affected digit, we could not distinguish some patients who were treated with operations after the failure of corticosteroid injections and those who underwent corticosteroid injections due to symptom recurrence after surgery. Third, there were inherent limitations associated with the ambiguity in treatment codes due to HIRA database and actual clinical situations. In the case of patients with both CTS and trigger finger, it is possible that matching for each diagnosis and treatment was unclear. Therefore, attention is needed in the interpretation of the results. Finally, we set some conditions for data collection, and these could be sources of overestimation or underestimation of the treatment status. Since we included patients who were treated under primary or secondary diagnosis codes only, this could be a source of underestimation of the number of patients. In contrast, some patients who had been treated with corticosteroid injections along with another disease could be included in this analysis if they had trigger finger or CTS simultaneously. In addition, the time limitations of this study could have led to an underestimation of patients who were treated surgically. For the calculation of annual treatment trends of both diseases, cases with corticosteroid injections or surgeries that occurred outside of the 1-year limit would not have been included in the analysis.
In conclusion, during the past 10 years, the incidence of CTS and trigger finger significantly decreased, but the prevalence of both diseases significantly increased. The portion of patients who received corticosteroid injections increased for both diseases, but the portion of patients who had surgeries for CTS within 1 year of their diagnosis decreased. This study provides insight into the epidemiology of these diseases in an Asian population and may inform estimates of healthcare costs.
ACKNOWLEDGEMENTS
This study used Health Insurance Review & Assessment Service (HIRA) research data (M20210707359) made by HIRA of the Republic of Korea. The views expressed are those of the author(s) and not necessarily those of the HIRA and the Ministry of Health and Welfare of the Republic of Korea.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Padua L, Coraci D, Erra C, et al. Carpal tunnel syndrome: clinical features, diagnosis, and management. Lancet Neurol. 2016;15(12):1273–1284. doi: 10.1016/S1474-4422(16)30231-9. [DOI] [PubMed] [Google Scholar]
- 2.Jeanmonod R, Harberger S, Sina RE, Waseem M. Trigger finger [Internet] StatPearls Publishing; 2024. [cited 2024 May 1]. Available from: https://pubmed.ncbi.nlm.nih.gov/29083657/ [PubMed] [Google Scholar]
- 3.Aroori S, Spence RA. Carpal tunnel syndrome. Ulster Med J. 2008;77(1):6–17. [PMC free article] [PubMed] [Google Scholar]
- 4.Zamborsky R, Kokavec M, Simko L, Bohac M. Carpal tunnel syndrome: symptoms, causes and treatment options: literature reviev. Ortop Traumatol Rehabil. 2017;19(1):1–8. doi: 10.5604/15093492.1232629. [DOI] [PubMed] [Google Scholar]
- 5.Aboonq MS. Pathophysiology of carpal tunnel syndrome. Neurosciences (Riyadh) 2015;20(1):4–9. [PMC free article] [PubMed] [Google Scholar]
- 6.Wright AR, Atkinson RE. Carpal tunnel syndrome: an update for the primary care physician. Hawaii J Health Soc Welf. 2019;78(11 Suppl 2):6–10. [PMC free article] [PubMed] [Google Scholar]
- 7.Merry SP, O’Grady JS, Boswell CL. Trigger finger?: just shoot! J Prim Care Community Health. 2020;11:2150132720943345. doi: 10.1177/2150132720943345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shen PC, Chang PC, Jou IM, Chen CH, Lee FH, Hsieh JL. Hand tendinopathy risk factors in Taiwan: a population-based cohort study. Medicine (Baltimore) 2019;98(1):e13795. doi: 10.1097/MD.0000000000013795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang C, Chen HH, Lee MC, et al. Risk factors of carpal tunnel syndrome in Taiwan: a population-based cohort study. Ann Plast Surg. 2022;88(1):74–78. doi: 10.1097/SAP.0000000000002950. [DOI] [PubMed] [Google Scholar]
- 10.Roh YH, Chung MS, Baek GH, Lee YH, Rhee SH, Gong HS. Incidence of clinically diagnosed and surgically treated carpal tunnel syndrome in Korea. J Hand Surg Am. 2010;35(9):1410–1417. doi: 10.1016/j.jhsa.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 11.Rhee SY, Cho HE, Kim JH, Kim HS. Incidence and reappraisal of known risk factors associated with carpal tunnel syndrome: a nationwide, 11-year, population-based study in South Korea. J Clin Neurol. 2021;17(4):524–533. doi: 10.3988/jcn.2021.17.4.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matthews A, Smith K, Read L, Nicholas J, Schmidt E. Trigger finger: an overview of the treatment options. JAAPA. 2019;32(1):17–21. doi: 10.1097/01.JAA.0000550281.42592.97. [DOI] [PubMed] [Google Scholar]
- 13.Gil JA, Hresko AM, Weiss AC. Current concepts in the management of trigger finger in adults. J Am Acad Orthop Surg. 2020;28(15):e642–e650. doi: 10.5435/JAAOS-D-19-00614. [DOI] [PubMed] [Google Scholar]
- 14.Patijn J, Vallejo R, Janssen M, et al. Carpal tunnel syndrome. Pain Pract. 2011;11(3):297–301. doi: 10.1111/j.1533-2500.2011.00457.x. [DOI] [PubMed] [Google Scholar]
- 15.Shin YH, Baek GH, Kim YJ, Kim MJ, Kim JK. Epidemiology of congenital upper limb anomalies in Korea: a nationwide population-based study. PLoS One. 2021;16(3):e0248105. doi: 10.1371/journal.pone.0248105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Institute of Mental Health. What is Prevalence? National Institute of Mental Health; 2024. [Google Scholar]
- 17.Yiin GS, Howard DP, Paul NL, et al. Age-specific incidence, outcome, cost, and projected future burden of atrial fibrillation-related embolic vascular events: a population-based study. Circulation. 2014;130(15):1236–1244. doi: 10.1161/CIRCULATIONAHA.114.010942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lencioni R, Crocetti L, Cioni R, et al. Response to radiofrequency ablation of pulmonary tumours: a prospective, intention-to-treat, multicentre clinical trial (the RAPTURE study) Lancet Oncol. 2008;9(7):621–628. doi: 10.1016/S1470-2045(08)70155-4. [DOI] [PubMed] [Google Scholar]
- 19.Korean Statistical Information Service (KOSIS) Korea’s average life expectancy. KOSIS; 2023. [Google Scholar]
- 20.Gelfman R, Melton LJ, 3rd, Yawn BP, Wollan PC, Amadio PC, Stevens JC. Long-term trends in carpal tunnel syndrome. Neurology. 2009;72(1):33–41. doi: 10.1212/01.wnl.0000338533.88960.b9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mattioli S, Baldasseroni A, Curti S, et al. Incidence rates of in-hospital carpal tunnel syndrome in the general population and possible associations with marital status. BMC Public Health. 2008;8:374. doi: 10.1186/1471-2458-8-374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tanaka S, Wild DK, Cameron LL, Freund E. Association of occupational and non-occupational risk factors with the prevalence of self-reported carpal tunnel syndrome in a national survey of the working population. Am J Ind Med. 1997;32(5):550–556. doi: 10.1002/(sici)1097-0274(199711)32:5<550::aid-ajim18>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 23.Benson LS, Ptaszek AJ. Injection versus surgery in the treatment of trigger finger. J Hand Surg Am. 1997;22(1):138–144. doi: 10.1016/S0363-5023(05)80194-7. [DOI] [PubMed] [Google Scholar]
- 24.Jenkins PJ, Duckworth AD, Watts AC, McEachan JE. Corticosteroid injection for carpal tunnel syndrome: a 5-year survivorship analysis. Hand (N Y) 2012;7(2):151–156. doi: 10.1007/s11552-012-9390-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kwon H, Jung JH, Han KD, et al. Prevalence and annual incidence of thyroid disease in Korea from 2006 to 2015: a nationwide population-based cohort study. Endocrinol Metab (Seoul) 2018;33(2):260–267. doi: 10.3803/EnM.2018.33.2.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Park CY, Lim JY, Kim WH, Kim SY, Park HY. Evaluation of menopausal hormone therapy use in Korea (2002-2013): a nationwide cohort study. Maturitas. 2021;146:57–62. doi: 10.1016/j.maturitas.2021.02.003. [DOI] [PubMed] [Google Scholar]
- 27.Kim H, Cho SK, Kim JW, et al. An increased disease burden of autoimmune inflammatory rheumatic diseases in Korea. Semin Arthritis Rheum. 2020;50(3):526–533. doi: 10.1016/j.semarthrit.2019.11.007. [DOI] [PubMed] [Google Scholar]
- 28.Organisation for Economic Co-operation and Development (OECD) OECD health statistics 2022. OECD; 2023. [Google Scholar]