Abstract
Background
Patient-reported satisfaction following total knee arthroplasty (TKA) can be affected by various factors. This study aimed to assess patient satisfaction rates and identify factors related to patients, surgery, and postoperative knee motion associated with satisfaction in posterior-stabilized TKA among Asian patients.
Methods
A retrospective cross-sectional study was conducted in patients with primary osteoarthritis who underwent TKA and had a follow-up period of over 2 years. Patient satisfaction was measured using a 5-point Likert scale, and the patients were divided into satisfied and dissatisfied groups. The factors potentially affecting satisfaction were collected, including demographics, comorbidities, surgical options, and knee motion. Univariate and multivariate regression analyses were performed.
Results
Of the 858 patients included, 784 (91.4%) were satisfied and 74 (8.6%) were dissatisfied. Fixed-bearing implants and higher postoperative knee flexion angles were associated with satisfaction (odds ratio [OR], 2.366; p = 0.001 and OR, 1.045; p < 0.001, respectively), whereas cerebrovascular disease was related to dissatisfaction (OR, 0.403; p = 0.005). The regression model demonstrated moderate predictability (R2 = 0.112).
Conclusions
Fixed-bearing implants and higher postoperative knee flexion angles were associated with patient satisfaction following TKA, whereas cerebrovascular disease was associated with dissatisfaction. The identification of these factors could help improve surgical outcomes and patient satisfaction following TKA.
Keywords: Total knee arthroplasty, Patient satisfaction, Fixed-bearing, Knee flexion angle, Cerebrovascular disease
Total knee arthroplasty (TKA) is an effective treatment for patients with advanced knee osteoarthritis.1) The global prevalence of knee osteoarthritis among people aged 60 years and above was estimated at approximately 13% of women and 10% of men,2) leading to a significant increase in the demand for TKA. Advances in surgical techniques, implant materials, and biomechanics have led to further improvements in TKA outcomes.3) However, as patients engage in social and sports activities even in older age, their expectations for TKA have risen, resulting in a wide range of reported satisfaction rates (80% to 100%) in previous studies.4,5)
Patient satisfaction following TKA is subjective and related to clinical outcomes, such as function and pain relief after surgery.5,6) However, other factors, such as physical health status, surgical techniques, and postoperative exercise levels, can also impact satisfaction. The presence of medical or psychological comorbidities during the time of surgery can influence postoperative pain, rehabilitation processes, and mental health, potentially altering the levels of patient satisfaction.4,7,8) Therefore, it is crucial to analyze these factors to understand how to maximize patient satisfaction after surgery, as identifying the factors associated with patient satisfaction is critical for improving surgical outcomes.4,9)
The aim of this study was to assess patient satisfaction rates following TKA and identify the factors related to patients, surgery, and postoperative knee motion that are associated with satisfaction. It was hypothesized that differences in demographic characteristics, patient comorbidity, knee alignment, surgical option, and knee motion would be observed between patients who reported satisfaction and those who did not.
METHODS
This retrospective cross-sectional study was approved by the Institutional Review Board of Seoul National University Hospital (IRB No. 2304-001-1416). Informed consent was waived due to its retrospective nature.
Patients
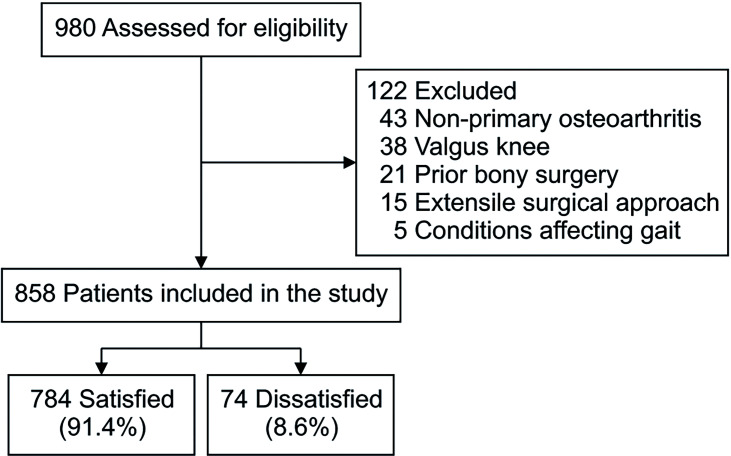
The present study included patients with primary osteoarthritis who underwent TKA and had a follow-up period of over 2 years, with data collected from January 2018 to January 2021. The exclusion criteria for this study were patients with non-primary osteoarthritis, such as rheumatoid arthritis and posttraumatic arthritis. Patients with valgus knees were excluded due to their limited prevalence and the potential confounding effect they could have on the analysis of preoperative coronal alignment distribution. In addition, patients with severe preoperative reduced knee joint range of motion (ROM) requiring an extensile surgical approach, patients with a history of bony surgery in the ipsilateral knee (e.g., knee realignment surgery or previous joint replacement), arthrodesis surgery in other joints, or conditions affecting gait were excluded (Fig. 1). Furthermore, patients who underwent revision surgery due to complications such as postoperative infection, instability, bearing dislocation, early loosening, and periprosthetic fracture were not included in the study, as these are widely recognized contributors to dissatisfaction following TKA.5)
Fig. 1. Flowchart of patient inclusion.
Surgery and Rehabilitation Protocol
All TKA procedures were performed by a senior surgeon (MCL) with over 20 years of experience at a tertiary hospital. A standard medial parapatellar arthrotomy was performed. A modified gap-balancing technique was used, in which the size and rotational alignment of the femoral component were determined from the ligament tension and trans-epicondylar axis. Tibial cutting was made perpendicular to the mechanical axis of the tibia, while the overall alignment aimed to position the weight-bearing line through the center of the knee. Posterior-stabilized (PS) implants were used, and selective patellar resurfacing was performed only for patients with a patellar thickness greater than 20 mm and an International Cartilage Repair Society grade of 3 or higher. The choice between fixed- and mobile-bearings was not based on differing indications, but instead was determined by the surgeon’s involvement in clinical trials at the time of surgery. The implants used included the PFC Sigma RP-F mobile (DePuy Synthes), Vanguard (Zimmer Biomet), Lospa (Corentec), LCS (DePuy Orthopaedics), E-motion (Aesculap), NexGen LPS-flex (Zimmer Biomet), Attune (DePuy Synthes), B-P Knee (Endotec), and Persona (Zimmer Biomet).
A standardized rehabilitation protocol was applied to all patients. Following surgery, the patients were instructed to use a knee immobilizer and walker to walk in the ward. Continuous passive motion machine use was initiated on the first postoperative day. From the third postoperative day, patients received passive ROM exercises under the guidance of experienced physical therapists. Patients were also educated on performing quadriceps strengthening and straight leg raising exercises before being discharged on postoperative day 7.
Data Collection
Satisfaction was assessed in this study using a 5-point Likert scale, with scores ranging from 1 to 5 for the descriptors “very dissatisfied,” “dissatisfied,” “neutral,” “satisfied,” and “very satisfied,” respectively. Patients who rated their satisfaction as “very satisfied” or “satisfied” were grouped as satisfied, while those who rated their satisfaction as “neutral,” “dissatisfied,” or “very dissatisfied” were classified as dissatisfied.
Various factors that could potentially affect patient satisfaction were collected. These included demographic information, preoperative and postoperative coronal alignment (hip-knee-ankle angle), and the preoperative Kellgren-Lawrence grade. Implant malalignment was also checked postoperatively, and outliers were defined as a distal femoral angle 3° deviated from 5° valgus, posterior tibial angle 3° deviated from the mechanical axis, and posterior tibial slope outside of 0°–5° range.10) Physical status was assessed according to the American Society of Anesthesiologists physical status classification system and the Western Ontario and McMaster Universities Osteoarthritis Index. Additionally, comorbidities such as cerebrovascular disease, diabetes mellitus, hypertension, ischemic heart disease, chronic liver disease, chronic kidney disease, and psychological disease were collected. These comorbidities were selected based on prior studies that investigated satisfaction after TKA4,7,8,11,12) and also considered the high prevalence of hypertension and diabetes mellitus among the elderly in South Korea.13) Identification of underlying comorbidities was conducted through a review of patients’ medical histories, which included treatment for the associated disease or diagnosis by preoperative work-up examinations. Surgical factors, such as patellar resurfacing and bearing type (fixed vs. mobile) were documented, and physical examination results, including knee flexion contracture and knee flexion angle, were also analyzed.
Data Analysis
The statistical significance of the factors was initially assessed using univariate analysis by comparing the satisfied and dissatisfied groups. Subsequently, factors with a p-value of less than 0.2 in the univariate analysis were selected for inclusion in the multivariate regression analyses. A p-value of less than 0.05 was considered statistically significant. To evaluate the predictability of the final model, explained variances (R2) above 0.25 were considered good, R2 values between 0.10 and 0.25 were considered moderate, and R2 values below 0.1 were considered poor. IBM SPSS Statistics for Windows, version 24 (IBM Corp.) was utilized for statistical analyses.
RESULTS
A total of 858 patients were investigated, of whom 784 (91.4%) reported being satisfied with the surgery, while 74 patients (8.6%) were dissatisfied. The mean follow-up period was 7.4 ± 3.9 years (mean ± standard deviation). The results of logistic regression analyses are presented in Table 1.
Table 1. Logistic Regression Analysis for Patient Satisfaction.
| Variable | Satisfied (n = 784) | Dissatisfied (n = 74) | Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | ||||
| Age (yr) | 74.5 ± 7.0 (50 to 94) | 73.9 ± 7.3 (58 to 86) | 1.035 (0.992 to 1.080) | 0.115 | 1.019 (0.984 to 1.055) | 0.291 | |
| Sex | Male (ref) | 45 (5.7) | 3 (4.1) | ||||
| Female | 739 (94.3) | 71 (95.9) | 0.754 (0.185 to 3.066) | 0.693 | |||
| Body mass index (kg/m2) | 26.8 ± 3.4 (15.8 to 38.1) | 26.2 ± 3.5 (20.4 to 37.7) | 1.040 (0.954 1.134) | 0.376 | |||
| Preoperative HKAA | 10.4 ± 5.0 (0.1 to 30.8) | 10.4 ± 4.4 (2.5 to 21.9) | 1.009 (0.951 to 1.072) | 0.785 | |||
| Postoperative HKAA | 1.5 ± 1.7 (–5.5 to 6.5) | 1.1 ± 1.8 (–5.0 to 5.2) | 1.102 (0.944 to 1.286) | 0.219 | |||
| Kellgren-Lawrence grade | 3 (ref) | 73 (9.3) | 4 (5.4) | ||||
| 4 | 711 (90.7) | 70 (94.6) | 0.593 (0.196 to 1.797) | 0.355 | |||
| Implant malalignment | No (ref) | 745 (95.0) | 69 (93.2) | ||||
| Yes | 39 (5.0) | 5 (6.8) | 1.247 (0.38 to 4.063) | 0.715 | |||
| ASA physical status classification | 1 (ref) | 155 (19.8) | 16 (21.6) | ||||
| 2 | 599 (76.4) | 53 (71.6) | 0.816 (0.358 to 1.858) | 0.628 | |||
| 3 | 30 (3.7) | 5 (6.8) | 0.349 (0.093 to 1.303) | 0.117 | 0.671 (0.215 to 2.089) | 0.491 | |
| Preoperative WOMAC | 48.3 ± 16.3 (11 to 96) | 48.0 ± 15.3 (23 to 85) | 1.004 (0.985 to 1.023) | 0.711 | |||
| Cerebrovascular disease | No (ref) | 710 (90.5) | 58 (78.4) | ||||
| Yes | 74 (9.5) | 16 (21.6) | 0.363 (0.169 to 0.777) | 0.009* | 0.403 (0.212 to 0.765) | 0.005* | |
| Diabetes mellitus | No (ref) | 572 (73.0) | 59 (79.7) | ||||
| Yes | 212 (27.0) | 15 (20.3) | 1.648 (0.781 to 3.481) | 0.19 | 1.629 (0.881 to 3.012) | 0.12 | |
| Hypertension | No (ref) | 285 (36.4) | 27 (36.5) | ||||
| Yes | 499 (63.6) | 47 (63.5) | 0.722 (0.355 to 1.467) | 0.367 | |||
| Ischemic heart disease | No (ref) | 705 (89.9) | 68 (91.9) | ||||
| Yes | 79 (10.1) | 6 (8.1) | 1.089 (0.391 to 3.035) | 0.870 | |||
| Chronic liver disease | No (ref) | 754 (96.2) | 70 (94.6) | ||||
| Yes | 30 (3.8) | 4 (5.4) | 0.291 (0.067 to 1.264) | 0.099 | 0.441 (0.139 to 1.398) | 0.164 | |
| Chronic kidney disease | No (ref) | 759 (96.8) | 71 (95.9) | ||||
| Yes | 25 (3.2) | 3 (4.1) | 0.391 (0.088 to 1.726) | 0.215 | |||
| Psychological disease | No (ref) | 755 (96.3) | 70 (94.6) | ||||
| Yes | 29 (3.7) | 4 (5.4) | 0.550 (0.147 to 2.052) | 0.374 | |||
| Patella resurfacing | No (ref) | 275 (35.1) | 41 (55.4) | ||||
| Yes | 509 (64.9) | 33 (44.6) | 1.238 (0.627 to 2.443) | 0.538 | |||
| Implant bearing | Mobile (ref) | 268 (34.2) | 42 (56.8) | ||||
| Mobile/fixed | Fixed (ref) | 516 (65.8) | 32 (43.2) | 2.227 (1.110 to 4.467) | 0.024* | 2.366 (1.398 to 4.004) | 0.001* |
| Postop flexion contracture | 0.4 ± 2.2 (–5 to 20) | 0.5 ± 2.6 (–5 to 10) | 1.019 (0.896 to 1.158) | 0.779 | |||
| Postop flexion angle | 128.0 ± 10.2 (80 to 150) | 122.2 ± 13.1 (70 to 145) | 1.061 (1.033 to 1.089) | < 0.001* | 1.045 (1.023 to 1.068) | < 0.001* | |
| Change in flexion contracture | –8.7 ± 7.1 (–30 to 20)† | –7.8 ± 7.2 (–30 to 10)† | 0.965 (0.922 to 1.011) | 0.130 | 0.964 (0.929 to 1.000) | 0.052 | |
| Change in flexion angle | 2.7 ± 13.8 (–45 to 60) | –0.1 ± 14.7 (–30 to 45)† | 0.984 (0.963 to 1.006) | 0.148 | 0.995 (0.977 to 1.013) | 0.581 | |
Values are presented as mean ± standard deviation (range) or number (%).
OR: odds ratio, CI: confidence interval, ref: reference value, HKAA: hip-knee-ankle angle, preop: preoperative, postop: postoperative, ASA: American Society of Anesthesiologists, WOMAC: Western Ontario and McMaster Universities Osteoarthritis index.
*Statistically significant at p < 0.05. †Negative values indicate a decrease.
Univariate Analyses
Cerebrovascular disease was significantly related to patient dissatisfaction (odds ratio [OR], 0.363; 95% confidence interval [CI], 0.169–0.777; p = 0.009). Patients with fixed-bearing implants had a higher satisfaction rate (OR, 2.227; 95% CI, 1.110–4.467; p = 0.024), and higher postoperative knee flexion angle was associated with greater satisfaction (OR, 1.061; 95% CI, 1.033–1.089; p < 0.001).
Multivariate Analyses
In variables with p-values of less than 0.2 in univariate analysis, the use of fixed-bearings and higher postoperative flexion angle were associated with patient satisfaction (OR, 2.366; 95% CI, 1.398–4.004; p = 0.001 and OR, 1.045; 95% CI, 1.023–1.068; p < 0.001, respectively). Each 1° increase in postoperative knee flexion angle was associated with 1.045 times higher odds of satisfaction. Cerebrovascular disease was a factor in dissatisfaction (OR, 0.403; 95% CI, 0.212–0.765; p = 0.005). The goodness of fit test was satisfactory (p = 0.643), with an R2 of 0.112. The model showed moderate predictability, correctly predicting 91.5% of the observed values, with 100.0% for satisfaction and 1.4% for dissatisfaction.
DISCUSSION
The most important finding of this study is the association between fixed-bearing implants and higher postoperative flexion angles with patient satisfaction. Conversely, cerebrovascular disease was related to decreased satisfaction. In this study, fixed-bearing implants were correlated with higher satisfaction compared to mobile-bearing implants. Among the 548 patients with fixed-bearing implants, 516 (94.2%) expressed satisfaction with their outcomes, while among the 310 patients with mobile-bearing implants, 268 (86.5%) reported satisfaction. The influence of the implant bearing type on patient satisfaction remains a topic of debate, with prior research yielding conflicting results.14,15,16) For instance, Thienpont and Zorman17) found higher Forgotten Joint Scores were indicative of better satisfaction in patients with fixed-bearing implants and proposed that a more anterior contact point in mobile-bearing implants could be the underlying reason. van Stralen et al.18) observed a higher incidence of patients with mobile-bearing TKA having trouble getting out of a chair. In contrast, Lizaur-Utrilla et al.19) found greater satisfaction in older patients with mobile-bearing TKA implants, suggesting that earlier gain of knee flexion in mobile-bearing implants contributed to higher satisfaction. Generally, meta-analyses on clinical outcomes have shown satisfactory results for both bearing types.20,21) However, some randomized controlled studies noted more complications with mobile-bearings, such as bearing dislocation, instability, and early component loosening.22,23,24) However, the studies were not adequately powered to conclusively determine a significant increase in complications with mobile-bearings. In the present study, although these complications were excluded from the analysis, mobile-bearing implants exhibited lower satisfaction levels compared to fixed-bearing implants. Therefore, the findings of this study further support the recommendation to consider fixed-bearing implants for maximizing satisfaction, while acknowledging that mobile-bearing implants still have a high satisfaction rate.
Knee motion has been extensively studied as a factor affecting patient satisfaction following TKA. Previous studies reported conflicting findings regarding the association between knee motion and patient satisfaction, with some studies suggesting that higher knee flexion angles were associated with greater satisfaction, whereas others reported that knee ROM did not significantly impact patient satisfaction.25,26,27) In this study, both knee flexion contracture and flexion angles were analyzed and postoperative knee flexion angle demonstrated a significant association with patient satisfaction. This finding is consistent with previous studies suggesting that a higher flexion angle benefited daily activities requiring deep flexion, such as squatting and cross-legged sitting.28,29) Although not reaching statistical significance in this study (p = 0.052), improvements in flexion contracture could potentially enhance patient satisfaction, as flexion contracture may cause discomfort during walking, increase energy loss, and alter gait patterns.28,29) A previous study by Kubo et al.28) found a significant association between improvement in the flexion angle and patient satisfaction, with a cutoff value of 5° for improvement in the flexion angle and 120° for the knee flexion angle. According to Oka et al.,30) achieving a knee flexion angle of 105° within 1 month after TKA was proposed as a predictor for reaching 120° at 1 year. Additionally, failure to achieve a flexion angle of 85° within 5 days would result in not reaching 120° at 1 year. Therefore, it is important to actively encourage patients to engage in ROM exercises following surgery to potentially increase their level of satisfaction.
Cerebrovascular disease has been identified as a factor that can limit the activities of daily living following TKA.31) In this study, only cerebrovascular disease was found to be associated with patient satisfaction among various comorbidities. The cerebrovascular diseases included in this study encompassed a history of brain aneurysm, arteriovenous malformation, intracranial hemorrhage, carotid artery disease, transient ischemic attack, and stroke. The precise mechanism underlying the impact of cerebrovascular disease on post-TKA satisfaction remains unclear. However, the potential explanations proposed in previous research include an increased risk of postoperative events such as stroke, which could result in delayed recovery and rehabilitation, subsequently lowering satisfaction levels compared to individuals without a preexisting cerebrovascular disease.31) Furthermore, medications related to the management of cerebrovascular disease may adversely affect the quality of life and satisfaction.8) A comprehensive analysis of the impact of cerebrovascular disease on patient satisfaction could not be conducted in this study because not all patients with cerebrovascular disease received treatment for their condition at the authors’ institution. In contrast, other studies suggested that various comorbidities could affect patient satisfaction. For instance, Walker et al.12) reported an association between lower satisfaction and pulmonary disease, diabetes, gastric ulcer, renal disease, liver disease, depression, back pain, and lower preoperative functional scores. Similarly, Pivec et al.11) found that diabetes, gastrointestinal disease, hypertension, psychiatric disease, and neurological disease were associated with lower satisfaction, while Clement and Burnett7) identified increasing age, anemia, and pain in other joints as factors contributing to poor satisfaction. Therefore, it is important to inform patients with these medical conditions about the potential for lower satisfaction, which can assist in the process of shared decision-making.
The satisfaction rate of 91.4% aligns with previous studies reporting rates between 80% and 100%.4,5,32) The wide range in patient satisfaction highlights its complex nature, which is influenced by combination of factors such as patient characteristics, surgical technique, rehabilitation protocol, functional outcomes, and patient expectations. The findings of this study imply that satisfaction may be optimized by correcting modifiable factors, while maintaining awareness of unmodifiable factors such as cerebrovascular disease.
This study had inherent limitations as a cross-sectional study and, therefore, could not account for changes over time. Furthermore, the inclusion of patients with different postoperative timeframes may have introduced bias in the satisfaction rate. Second, as the study only included Asian patients, who frequently require a high knee flexion angle in daily life, generalization to other ethnicities may be limited. In a similar context, since PS type implants provide greater ROM gains compared to cruciate-retaining type implants,33) this study used PS type implants. Thus, the results may not be generalizable to patients with different implant characteristics. In addition, cerebrovascular disease encompasses a range of severities and types that were not specifically analyzed in this study. Also, patients with postoperative complications such as infection, instability, bearing dislocation, early loosening, and periprosthetic fractures were excluded. Lastly, the regression formula demonstrated moderate predictability, limiting its generalized application.
The use of fixed-bearing implants and higher postoperative knee flexion angle were associated with patient satisfaction following TKA, whereas cerebrovascular disease was associated with dissatisfaction. The identification of these factors could help improve surgical outcomes and patient satisfaction following TKA.
ACKNOWLEDGEMENTS
This research was supported by a grant of the Korea Health Technology R&D Project through the Patient-Doctor Shared Decision Making Research center, funded by the Ministry of Health & Welfare, Republic of Korea (grant no. HV23C1803).
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Price AJ, Alvand A, Troelsen A, et al. Knee replacement. Lancet. 2018;392(10158):1672–1682. doi: 10.1016/S0140-6736(18)32344-4. [DOI] [PubMed] [Google Scholar]
- 2.Cross M, Smith E, Hoy D, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–1330. doi: 10.1136/annrheumdis-2013-204763. [DOI] [PubMed] [Google Scholar]
- 3.Batailler C, Swan J, Sappey Marinier E, Servien E, Lustig S. New technologies in knee arthroplasty: current concepts. J Clin Med. 2020;10(1):47. doi: 10.3390/jcm10010047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choi YJ, Ra HJ. Patient satisfaction after total knee arthroplasty. Knee Surg Relat Res. 2016;28(1):1–15. doi: 10.5792/ksrr.2016.28.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kahlenberg CA, Nwachukwu BU, McLawhorn AS, Cross MB, Cornell CN, Padgett DE. Patient satisfaction after total knee replacement: a systematic review. HSS J. 2018;14(2):192–201. doi: 10.1007/s11420-018-9614-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ko K, Kim KH, Ko S, et al. Total knee arthroplasty: is it safe? A single-center study of 4,124 patients in South Korea. Clin Orthop Surg. 2023;15(6):935–941. doi: 10.4055/cios22088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clement ND, Burnett R. Patient satisfaction after total knee arthroplasty is affected by their general physical well-being. Knee Surg Sports Traumatol Arthrosc. 2013;21(11):2638–2646. doi: 10.1007/s00167-013-2523-y. [DOI] [PubMed] [Google Scholar]
- 8.Singh JA, Lewallen DG. Medical and psychological comorbidity predicts poor pain outcomes after total knee arthroplasty. Rheumatology (Oxford) 2013;52(5):916–923. doi: 10.1093/rheumatology/kes402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shon OJ, Kim GB. Does the degree of intraoperatively identified cartilage loss affect the outcomes of primary total knee arthroplasty without patella resurfacing? A prospective comparative cohort study. Knee Surg Relat Res. 2022;34(1):36. doi: 10.1186/s43019-022-00161-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kazarian GS, Haddad FS, Donaldson MJ, Wignadasan W, Nunley RM, Barrack RL. Implant malalignment may be a risk factor for poor patient-reported outcomes measures (PROMs) following total knee arthroplasty (TKA) J Arthroplasty. 2022;37(6S):S129–S133. doi: 10.1016/j.arth.2022.02.087. [DOI] [PubMed] [Google Scholar]
- 11.Pivec R, Issa K, Given K, et al. A prospective, longitudinal study of patient satisfaction following total knee arthroplasty using the Short-Form 36 (SF-36) survey stratified by various demographic and comorbid factors. J Arthroplasty. 2015;30(3):374–378. doi: 10.1016/j.arth.2014.10.013. [DOI] [PubMed] [Google Scholar]
- 12.Walker LC, Clement ND, Bardgett M, et al. The WOMAC score can be reliably used to classify patient satisfaction after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2018;26(11):3333–3341. doi: 10.1007/s00167-018-4879-5. [DOI] [PubMed] [Google Scholar]
- 13.Chin YR, Lee IS, Lee HY. Effects of hypertension, diabetes, and/or cardiovascular disease on health-related quality of life in elderly Korean individuals: a population-based cross-sectional survey. Asian Nurs Res (Korean Soc Nurs Sci) 2014;8(4):267–273. doi: 10.1016/j.anr.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 14.Bo ZD, Liao L, Zhao JM, Wei QJ, Ding XF, Yang B. Mobile bearing or fixed bearing? A meta-analysis of outcomes comparing mobile bearing and fixed bearing bilateral total knee replacements. Knee. 2014;21(2):374–381. doi: 10.1016/j.knee.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 15.van der Voort P, Pijls BG, Nouta KA, Valstar ER, Jacobs WC, Nelissen RG. A systematic review and meta-regression of mobile-bearing versus fixed-bearing total knee replacement in 41 studies. Bone Joint J. 2013;95(9):1209–1216. doi: 10.1302/0301-620X.95B9.30386. [DOI] [PubMed] [Google Scholar]
- 16.Chaudhry A, Goyal VK. Fixed-bearing versus high-flexion RP total knee arthroplasty (TKA): midterm results of a randomized controlled trial. J Orthop Traumatol. 2018;19(1):2. doi: 10.1186/s10195-018-0493-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thienpont E, Zorman D. Higher forgotten joint score for fixed-bearing than for mobile-bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24(8):2641–2645. doi: 10.1007/s00167-015-3663-z. [DOI] [PubMed] [Google Scholar]
- 18.van Stralen RA, Heesterbeek PJ, Wymenga AB. Different femorotibial contact points between fixed- and mobile-bearing TKAs do not show clinical impact. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3368–3374. doi: 10.1007/s00167-014-3178-z. [DOI] [PubMed] [Google Scholar]
- 19.Lizaur-Utrilla A, Sanz-Reig J, Trigueros-Rentero MA. Greater satisfaction in older patients with a mobile-bearing compared with fixed-bearing total knee arthroplasty. J Arthroplasty. 2012;27(2):207–212. doi: 10.1016/j.arth.2011.05.021. [DOI] [PubMed] [Google Scholar]
- 20.Smith H, Jan M, Mahomed NN, Davey JR, Gandhi R. Meta-analysis and systematic review of clinical outcomes comparing mobile bearing and fixed bearing total knee arthroplasty. J Arthroplasty. 2011;26(8):1205–1213. doi: 10.1016/j.arth.2010.12.017. [DOI] [PubMed] [Google Scholar]
- 21.Migliorini F, Maffulli N, Cuozzo F, Pilone M, Elsner K, Eschweiler J. No difference between mobile and fixed bearing in primary total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2022;30(9):3138–3154. doi: 10.1007/s00167-022-07065-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Price AJ, Rees JL, Beard D, et al. A mobile-bearing total knee prosthesis compared with a fixed-bearing prosthesis. A multicentre single-blind randomised controlled trial. J Bone Joint Surg Br. 2003;85(1):62–67. doi: 10.1302/0301-620x.85b1.13233. [DOI] [PubMed] [Google Scholar]
- 23.Woolson ST, Northrop GD. Mobile- vs. fixed-bearing total knee arthroplasty: a clinical and radiologic study. J Arthroplasty. 2004;19(2):135–140. doi: 10.1016/j.arth.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 24.Ladermann A, Lubbeke A, Stern R, Riand N, Fritschy D. Fixed-bearing versus mobile-bearing total knee arthroplasty: a prospective randomised, clinical and radiological study with mid-term results at 7 years. Knee. 2008;15(3):206–210. doi: 10.1016/j.knee.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 25.Miner AL, Lingard EA, Wright EA, Sledge CB, Katz JN Kinemax Outcomes Group. Knee range of motion after total knee arthroplasty: how important is this as an outcome measure? J Arthroplasty. 2003;18(3):286–294. doi: 10.1054/arth.2003.50046. [DOI] [PubMed] [Google Scholar]
- 26.Ha CW, Park YB, Song YS, Kim JH, Park YG. Increased range of motion is important for functional outcome and satisfaction after total knee arthroplasty in Asian patients. J Arthroplasty. 2016;31(6):1199–1203. doi: 10.1016/j.arth.2015.12.018. [DOI] [PubMed] [Google Scholar]
- 27.Van Onsem S, Verstraete M, Dhont S, Zwaenepoel B, Van Der Straeten C, Victor J. Improved walking distance and range of motion predict patient satisfaction after TKA. Knee Surg Sports Traumatol Arthrosc. 2018;26(11):3272–3279. doi: 10.1007/s00167-018-4856-z. [DOI] [PubMed] [Google Scholar]
- 28.Kubo M, Maeda T, Kumagai K, Amano Y, Kawasaki T, Imai S. Good postoperative flexion angle improves knee function and improvement of flexion angle increases patient satisfaction after total knee arthroplasty. J Arthroplasty. 2021;36(9):3137–3140. doi: 10.1016/j.arth.2021.04.040. [DOI] [PubMed] [Google Scholar]
- 29.Bellemans J, Vandenneucker H, Victor J, Vanlauwe J. Flexion contracture in total knee arthroplasty. Clin Orthop Relat Res. 2006;452:78–82. doi: 10.1097/01.blo.0000238791.36725.c5. [DOI] [PubMed] [Google Scholar]
- 30.Oka T, Wada O, Asai T, Maruno H, Mizuno K. Importance of knee flexion range of motion during the acute phase after total knee arthroplasty. Phys Ther Res. 2020;23(2):143–148. doi: 10.1298/ptr.E9996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Singh JA, Lewallen DG. Cerebrovascular disease is associated with outcomes after total knee arthroplasty: a US total joint registry study. J Arthroplasty. 2014;29(1):40–43. doi: 10.1016/j.arth.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Klem NR, Smith A, O’Sullivan P, et al. What influences patient satisfaction after TKA? A qualitative investigation. Clin Orthop Relat Res. 2020;478(8):1850–1866. doi: 10.1097/CORR.0000000000001284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bercik MJ, Joshi A, Parvizi J. Posterior cruciate-retaining versus posterior-stabilized total knee arthroplasty: a meta-analysis. J Arthroplasty. 2013;28(3):439–444. doi: 10.1016/j.arth.2012.08.008. [DOI] [PubMed] [Google Scholar]