Abstract
Midwife-led continuity of care models have been linked to better clinical outcomes in certain developed countries. However, there is a paucity of research on these models in developing nations. This quasi-experimental study was conducted on primiparous women who referred to one private midwifery center and two public hospitals in Ahvaz, Iran to evaluate the effect of team midwifery care on maternal and neonatal outcomes of pregnant women in Iran. Two hundred women were allocated either into the experimental (n = 100) or control (n = 100) groups. Women in the experimental group, received team midwifery care, while women in the control group, received routine care. Data were collected using a demographic questionnaire, Mackey questionnaire, and a checklist. Women in the team midwifery care group experienced significantly higher rates of normal vaginal birth and exclusive breastfeeding compared to women in the control group. No statistically significant difference was observed between the two groups in terms of the rate of induction of labor and postpartum hemorrhage. The duration of labor was longer in the team midwifery care compared to the control group. Women in the team midwifery care group had a significantly higher rate of exclusive breastfeeding at six weeks postpartum compared to the control group (80 vs. 61%, p = 0.001). After excluding women with ruptured membranes and prolonged pregnancies, neonates in the intervention group had significantly higher first- and fifth-minute Apgar scores (p < 0.0001), and a lower rate of admission to intensive care unit in the intervention group compared to the control group (1 vs. 9%, p = 0.04). Also, women in the team midwifery group had skin-to-skin contact significantly earlier than those in the control group (33.87 ± 66.26 min vs. 111.98 ± 247.31 min, p = 0.578). Given the positive impact of continuous team midwifery care on maternal and neonatal outcomes, its implementation in maternity care systems, particularly in countries like Iran with high cesarean section rates, is strongly recommended.
Keywords: Continuity, Maternal outcomes, Neonatal outcomes, Midwifery
Subject terms: Health care, Medical research
Introduction
Providing high quality maternal and neonatal care is an important global goal, and midwifery care has a remarkable role in delivering high-quality services in this regard1,2. Studies conducted in Iran have consistently indicated that the quality of care provided during pregnancy, childbirth, and the postpartum period is often subpar. This highlights a pressing need for reforms to enhance the quality of midwifery care in the country3. In Pazandeh et al. study, for example, which evaluated the quality of care in women with low-risk pregnancies in Iran, high rates of interventions such as augmentation of labor (45%), fundal pressure (59%), episiotomy (76%) and amniotomy (71%) were reported. Such interventions may contribute to adverse pregnancy outcomes4,5. Medical interventions have been indicated as one of the main obstacles of performing physiological birth in Iran. However, a majority of women express a desire for a physiological and natural childbirth with minimal interventions6,7. In Iran, the rate of caesarean section is about 47%,which is three times higher than the rate recommended by the World Health Organization8,9. Most caesarean sections costs are paid out of pocket. In addition to the economic burden, caesarean section increases the rate of short- and long-term complications for women and their neonates10. It is believed that some interventions like antenatal education, implementation of evidence based guidelines and midwife-led continuity of care may reduce unnecessary cesareans11.
Qualitative studies conducted in Iran, have pointed out the lack of continuity of care especially by midwives, as one of the major challenges in providing maternal health services12,13. In Iran, maternity care is fragmented and managed based on a biomedical approach. The disconnected relationship between expectant mothers and caregivers coupled with instrumental-focused care can lead to negative or traumatic birth experiences14. Ghanbari-Homayi et al. (2019) reported a high prevalence (37%) of traumatic experience among Iranian primiparous women15.
In Iran, all care provided during pregnancy, childbirth, and the postpartum period adheres to national maternity guidelines. In healthcare centers, midwives are primarily responsible for prenatal care, with referrals to obstetricians or other specialists made as needed. Midwives provide standard care during labor and birth in hospitals under the supervision of the gynecologists. Midwives are the primary providers of maternity care throughout the antenatal, intrapartum, and postpartum periods. However, ultimate responsibility for the care of pregnant women rests with the gynecologist16. Some midwives establish private practices, becoming members of the Iranian Medical Council. They carry out their professional duties privately, adhering to guidelines developed and regularly updated by the Ministry of Health17. While some midwives offer comprehensive care throughout the antenatal, intrapartum, and postpartum periods, others may limit their services to antenatal or postpartum care. In cases of pregnancy complications, midwives refer patients to obstetricians for consultation. When attending births in hospitals, midwives manage all aspects of care for the birthing person, adhering to national maternity guidelines. In complicated labors and deliveries, on-call obstetricians are involved and consider alternative approaches to facilitate successful childbirth, including emergency cesarean sections when necessary. Except for the first postpartum care, which is provided in hospital, women receive the second and third postpartum visits on 10th -15th and 42th-60th days postpartum respectively from different midwives in health centers. While national guidelines for maternal and neonatal care in Iran are primarily developed by gynecologists, a lack of continuity of care provided by a single healthcare provider or a dedicated team is a recognized issue. Also, in a fragmented model of care, there are fewer opportunities for individual care18. Studies have shown that women do not like fragmented care and conflicting advice, and midwife-led continuity of care models are outlined as one way to solve these problems19. These models of midwifery care ensure that mothers receive prenatal, childbirth, and postpartum care from a single midwife or a small team of midwives, fostering strong communication and continuity of care20.
With increasing evidence of improved clinical outcomes and care satisfaction in pregnant women, interest in midwife-led continuity models of care is growing. However, the majority of existing studies on this topic have been conducted in developed countries, limiting their generalizability to low- and middle-income contexts21,22. In low- and middle-income countries, the unique needs and challenges necessitate a culturally sensitive and context-specific approach when introducing new strategies23. To the best of our knowledge, no study has yet been conducted on team midwifery care and its consequences in Iran. Therefore, this study aimed to assess the effect of continuity of team midwifery care on the maternal and neonatal outcomes among Iranian pregnant women.
Methods
Design
This quantitative (quasi-experimental) research is part of a mixed-methods project designed to evaluate the impact of continuous team midwifery care on maternal and neonatal outcomes in Ahvaz, Iran.
Outcome variables
The following outcomes were considered:
Maternal outcomes
Mode of delivery
Duration of different stages of labor
Induction of labor
Postpartum hemorrhage
Childbirth satisfaction
-
b.
Neonatal outcomes
First- and fifth-minute Apgar scores
Skin-to-skin contact
Admission to neonatal intensive care unit (NICU)
Exclusive breastfeeding within six weeks after birth
Settings
This study was conducted in a private midwifery clinic and two public hospitals (Sina and Alameh Karami). The Sina Hospital is a non-educational public hospital while Alameh Karami is a charitable public hospital. Midwife-led continuity of care is not implemented in almost any hospital in Ahvaz.
Intervention
A team of three licensed midwives including two self-employed midwives and one Ph.D. student in midwifery (SS) provided continuous care for the participants in the intervention group during antenatal, intrapartum and postpartum periods. Women’s first visit with the midwifery team was earlier than 24 weeks of pregnancy (mostly 10–12 weeks of pregnancy). At least eight prenatal care and two routine postpartum visits during the first six weeks after birth were provided in the private midwifery clinic. The team midwives were present at the clinic every other day and available 24/7 on call. The midwifery care plan was in accordance with the national maternity guidelines, and in case of any complication, participants were referred to a gynecologist for consultation. All participants gave birth at one of two designated hospitals, with a team midwife present for labor and childbirth. Phone calls were made to participants on an ad-hoc basis to address any problems such as ruptured membranes, spotting, or back pain.
While the control group received eight prenatal care sessions, their care was fragmented, provided by multiple midwives or gynecologists throughout the pregnancy, childbirth, and postpartum periods, in accordance with national guidelines at health centers or private clinics. The midwives or gynecologists who delivered the babies were not involved in the prenatal or postpartum care of the women in the control group, nor was the researcher involved in the process of caring for this group.
Recruitment of participants
A total of 200 women (n = 100 in each group) were recruited from a private midwifery clinic (intervention group) and public health centers and hospitals (control group) through convenience sampling method.
Inclusion criteria were as follows: nulliparity, having a singleton fetus, age 18 years or older, low-risk pregnancy, being under 24 weeks of gestation (most participants recruited were in 10–12 weeks of pregnancy). Women who requested a planned caesarean section and those with previous or current obstetric or medical problems were excluded from the study. A written informed consent was obtained from all study participants. Also, the design of the study was approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (Ref No: IR.AJUMS.REC.1398.096).
Sample size
The sample size was calculated according to the objectives of the study, the rate of cesarean section in hospitals of Ahvaz, and a pilot study (using 10 participants who met the inclusion criteria). Using the following formula
 |
and assuming a power of 80%, an alpha level of 0.05, and expected proportions of 34.3 and 17.15%, a sample size of 100 women per group was determined to be sufficient.
Data collection
A demographic questionnaire (including age, employment status, education level, weight, height, body mass index (BMI), and number of pregnancies, births and abortions), a checklist (including results of vaginal examinations, mode of birth, duration of different stages of labor, episiotomy rate, rate of induction of labor, rate of postpartum hemorrhage, first- and fifth-minute Apgar scores, rate of NICU admission, exclusive breastfeeding rate, and average time of initiation of skin-to-skin contact), and Mackey Childbirth Satisfaction Rating Scale (MCSRS) were used for data collection in intervention and control groups. The demographic questionnaire was completed upon recruitment, but the MCSRS questionnaire and the checklist were completed after childbirth. No data was collected between the completion of the demographic questionnaire and the recording of labor and postpartum. MCSRS measures childbirth satisfaction and consists of six subscales: “self “, “nurse (midwife)”, “partner”, “baby”, “physician” and “overall” childbirth satisfaction. Women expressed their satisfaction or dissatisfaction with each item on a five-point Likert scale: 1 = very dissatisfied, 2 = dissatisfied, 3 = neither satisfied nor dissatisfied, 4 = satisfied, and 5 = very satisfied24. Due to hospital policies, our study was unable to include two subscales of partner and physician. The BMI of mothers was calculated using measured height and the first trimester weight or pre-pregnancy self- reported weight. Immediate postpartum hemorrhage was measured by visual estimation.
Follow-up
Women in the team midwifery group received regular antenatal and postpartum care from 10 to 12 weeks of pregnancy until six weeks after delivery. Pregnant women in the control group received prenatal care from health centers, midwifery offices, or medical practices. At the time of childbirth, the researcher attended one of the mentioned hospitals and recruited eligible women in labor with routine care who were willing to participate in the study.
Analysis
Data were analyzed using SPSS version 26. Descriptive statistics were used to compare baseline demographic data. The Shapiro-Wilk Test was used for checking the normality of data. The chi-square test and independent-sample t-test were used for analysis of categorical (education level, employment status, abortion, induction of labor, postpartum hemorrhage, mode of birth, NICU admission, and exclusive breast feeding) and continuous (BMI) data, respectively. Mann-Whitney U test was used for variables like gestational age at first visit and different stages of labor. To examine the effect of intervention on maternal and neonatal outcomes, the multiple linear and logistic regression with adjustment for confounding variables (age, education level, employment status of the mother and that of her husband and weight gain during pregnancy) were used). A p-value less than 0.05 was considered statistically significant.
Results
Demographic characteristics
Women in the team midwifery care group were significantly older than those in the routine care group. In addition, there were significant differences between the two study groups in terms of education level, occupation, and weight gain during pregnancy. Women in the two groups did not have any significant difference in terms of body mass index, gestational age at first visit, and abortion (Table 1).
Table 1.
Comparison of demographic characteristics between team midwifery and routine care groups.
| Demographic characteristics | Team care group N = 100 |
Routine care group N = 100 |
p-value | |
|---|---|---|---|---|
| No.(%) / Mean(SD) | ||||
| Age (Y) | 24.02 ± 4.50 | 22.57 ± 5.04 | 0.006 | |
| Body mass index (Kg/m2) | 23.78 ± 4.07 | 23.41 ± 4.46 | 0.54 | |
| Weight gain during pregnancy (Kg) | 12.93 ± 5.47 | 9.17 ± 4.78 | < 0.0001 | |
| Gestational age at first visit (wk) | 11.29 ± 6.33 | 9.05 ± 4.02 | 0.07 | |
| Education Level | Primary | 7(7) | 28(28) | < 0.0001 |
| High school | 49 (49) | 60(60) | ||
| University | 44(44) | 12(12) | ||
| Employment status | Housewife | 81 (81) | 93(93) | 0.039 |
| Employed | 19 (19) | 7(7) | ||
| Abortion | 0 | 82 (82) | 86(86) | 0.69 |
| 1 | 14 (14) | 12(12) | ||
| ≥ 2 | 4(4) | 2(2) | ||
Maternal outcomes
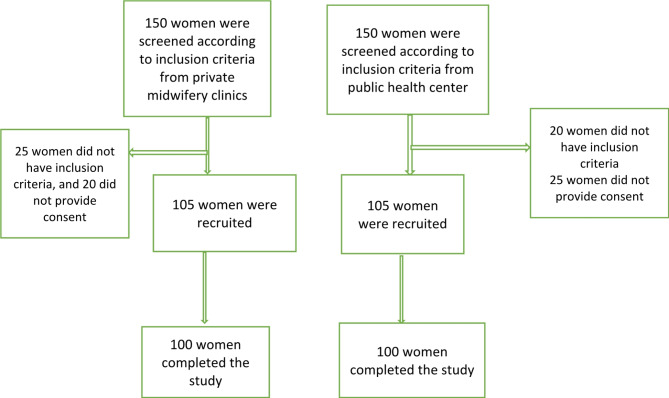
In this study, 105 women were recruited in each group, and 100 women completed the study (Fig. 1). Table 2 represents the maternal and neonatal outcomes after adjustment for potential confounders. Women in the team midwifery group had a significantly higher rate of normal vaginal birth than those in the control group. (84 vs. 61%) (p = 0.001).
Fig. 1.
Flow-diagram of recruitment of participants for the study.
Table 2.
Comparison of maternal and neonatal outcomes between team midwifery and routine care groups
| Outcome | Team care group N=100 | Routine care group N=100 | p-value | Logistic regression | p-value | ||
|---|---|---|---|---|---|---|---|
| aOR | 95% CI | ||||||
| No (%)/Mean(SD) | |||||||
| Mode of birth | NVD | 84(84) | 61(61) | <0.0001 | 3.864 | 1.717, 8.697 | 0.001 |
| CS | 16(16) | 39(39) | |||||
| Induction of labor | Yes | 25(25) | 34(34) | 0.21 | 1.308 | 0.684, 2.643 | 0.454 |
| No | 75(75) | 66(66) | |||||
| Postpartum Hemorrhage | Yes | 8(8) | 11(11) | 0.63 | 1.918 | 0.630,5.844 | 0.252 |
| No | 92(92) | 89(89) | |||||
| NICU admission | Yes | 1(1) | 9(9) | 0.018 | 11.821 | 1.093,127.830 | 0.042 |
| No | 99(99) | 91(91) | |||||
| Exclusive breastfeeding | Yes | 80(80) | 61(61) | 0.005 | 3.258 | 1.537,6.903 | 0.002 |
| No | 20(20) | 39(39) | |||||
| Linear regression | p-value | ||||||
|---|---|---|---|---|---|---|---|
| β | 95% CI | ||||||
| Time interval between active phase till the end of third stage (min) | 295.82±175.35 | 211.50±141.08 | <0.0001 | 267.655 | 56.010,479.299 | 0.013 | |
| Length of active phase | 252.55±160.50 | 168.60±128.64 | <0.0001 | 234.268 | 42.355,462.182 | 0.017 | |
| Length of second stage | 35.77±25.45 | 36.31±33.65 | 0.396 | 27.677 | −10.319,65.673 | 0.153 | |
| Length of third stage | 7.54±4.06 | 7.00±3.67 | 0.146 | 6.615 | −1.445,11,785 | 0.012 | |
| Initiation skin to skin contact (min) | 33.87±66.26 | 111.98±247.31 | 0.003 | −55.289 | −250.327,139.750 | 0.578 | |
| 1 min Apgar | 0.31±8.96 | 0.59±8.84 | 0.052 | 9.363 | 8.862,9.865 | <0.0001 | |
| 5 min Apgar | 0.20±9.98 | 9.87±0.52 | 0.031 | 10.130 | 9.704,10.555 | <0.0001 | |
The mean length of the active phase (p = 0.017), the time interval between the commencement of the active phase and the end of the third stage (p = 0.013) and the third stage (p = 0.012) were significantly longer in the team midwifery group compared to the control group. No statistically significant difference was found between groups in terms of the length of the second stage of labor.
However, the rate of induction of labor was lower in the team midwifery care group compared to the control group (25 vs. 34%), but the difference was not statistically significant (p = 0.454).
Women in the two groups did not have any significant difference in terms of the rate of postpartum hemorrhage (8 vs. 11%) (p = 0.252).
Women in the team midwifery group were more satisfied with “self”, “midwife”, and “overall” process of childbirth (p < 0.05). No significant difference was observed between team midwifery care and routine care groups regarding the “baby” subscale, but following subgroup analysis, the women in the team care group received higher mean score in this subscale (Table 3).
Table 3.
Comparison of mean scores of childbirth satisfaction between team midwifery and routine care groups.
| Subscale | Team midwifery care group N = 100 | Routine care group N = 100 | P-value | Linear regression | p-value | |
|---|---|---|---|---|---|---|
| Mean± SD | β | 95% CI | ||||
| Self | 35.54 ± 4.92 | 27.88 ± 9.44 | < 0.0001 | 35.526 | 26.293,44.760 | < 0.0001 |
| Midwife | 40.24 ± 5.6 | 34.37 ± 6.45 | 0.0002 | 32.198 | 24.448,39.948 | < 0.0001 |
| Baby | 12.73 ± 1.56 | 13.01 ± 14.55 | 0.88 | 11.708 | − 0.770, 24.185 | < 0.0001 |
| Overall | 9.39 ± 1.93 | 7.17 ± 2.35 | < 0.0001 | 8.346 | 5.617,11.075 | < 0.0001 |
Neonatal outcomes
Newborns in the team midwifery care group had a significantly lower admission rate to the NICU compared to those in the control group (1 vs. 9%, p = 0.04). There was a significant difference between team midwifery care group and the control group regarding first- and fifth-minute Apgar scores (P < 0.0001).
Women in the two groups had no significant differences regarding initiation of skin-to-skin contact, but the result of sub-analyses showed women in the team midwifery group had significantly earlier skin-to-skin contact than those in the control group (p = 0.04).
Exclusive breastfeeding rates at six weeks postpartum were significantly higher in the team midwifery care group compared to the control group (80% vs. 61%) (p = 0.001) (Table 2).
Subgroup analysis
A subgroup analysis was conducted to examine outcomes in women who presented to the labor ward with only labor pain and no other complications, such as premature rupture of membranes. Eleven women in the team midwifery care group and 17 women in the routine care group were admitted due to rupture of membranes. In addition, 11 women in the team midwifery care group and 14 women in the routine care group were admitted for post-term pregnancy. After exclusion of women with ruptured membrane and prolonged pregnancy, 72 women in the team midwifery care group and 50 women in the routine care group who were admitted to the labor ward because of labor pain were included in subgroup analysis.
Based on the results of linear regression test, the mean length of the active phase (P = 0.01), the time interval between the commencement of active phase and the end of the third stage (P = 0.02), overall satisfaction with childbirth, satisfaction of self, and satisfaction of midwife remained significantly different between the two groups. Also, based on the results of the logistic regression test, mode of birth (P = 0.009) and exclusive breastfeeding (P = 0.005) were significantly different between the two groups. After sub-group analyses, the initiation of skin-to-skin contact (P = 0.04) and satisfaction with baby (P < 0.0001) became statistically different between the two groups. The initiation of skin-to-skin contact was earlier and satisfaction with baby was higher in the midwifery team care group compared with the control group (data are not shown in tables).
Discussion
Maternal and neonatal outcomes
In the present study, the birth outcomes of women who received team midwifery care was compared with women receiving routine care. Women with team care were more likely to give birth vaginally than those in the control group, which is consistent with findings of some previous studies25,26 but in contrast to the results of others27,28. As McLachlan et al. found in their study, reducing the rate of cesarean section in regions with high baseline rates, such as our study setting, may be more feasible25,29. The team midwives’ education, combined with their ongoing support and trusting relationships with women, enhanced their ability to facilitate normal birth. Additionally, their belief in the natural process of childbirth was a crucial factor in achieving positive outcomes.
Our results showed that the mean length of labor, with the exception of the second stage, was longer in the midwifery team care group compared to the routine care group. These findings align with a Cochrane review of 15 studies by Sandal et al. (2016), which reported that women receiving midwife-led continuity models of care had longer mean lengths of labor than those in other models of care30. The reduced rate of interventions during labor, such as amniotomy and membrane stripping, in the team midwifery care group may have contributed to these findings. Although care was provided according to national guidelines in both groups, team midwives avoided unnecessary interventions whenever possible. It’s noteworthy that despite the longer mean length of labor, the rates of cesarean section and postpartum hemorrhage were lower in the team midwifery care group, suggesting the midwives’ successful efforts to facilitate normal birth and avoid unnecessary interventions.
In the present study, no significant difference was found between the two groups in terms of labor induction, which confirms the results of some previous studies25,30,31. However, there are some studies with different findings10,32. Since premature rupture of membrane was the most common cause of induction in both groups in our study, which necessitates administration of oxytocin for termination of pregnancy, the absence of any significant difference between the two groups in terms of induction rate seems logical. Although the practice and profession of midwifery is grounded in preserving normal pregnancy and childbirth, sometimes midwives face a situation in which they are required to interfere potentially, and in these cases the benefits outweigh the disadvantages33.
Our findings showed that no statistically significant difference in postpartum hemorrhage was observed between the two groups, which is in line with the result of other studies31,34. Since in this study, the management of the third stage of labor in both groups was performed according to the national guidelines, no major difference in the rate of postpartum hemorrhage was observed.
In the present study, the number of neonates admitted to NICU was significantly higher in the routine care, which is in accordance with McLachlan et al. (2012) who concluded that neonates of women allocated to caseload were less likely to be admitted to NICU25. Of course, in two other studies, no differences were reported between the two comparison groups in this regard29,35.
Our results revealed that neonates in the team midwifery care group demonstrated significantly higher first- and fifth-minute Apgar scores compared with those in the routine care group. This finding is inconsistent with some of the previous studies, which reported no difference between intervention and control groups in terms of the first- and fifth-minute Apgar scores36,37. Improved neonatal health outcomes in our study suggest that there could be an association between team midwifery model of care and these outstanding results. High-quality maternal care, including continuous supervision by midwives who are familiar with the mother’s needs and physical condition, is associated with improved maternal and neonatal well-being.
Our results of sub-group analyses showed a significantly higher rate of skin-to-skin contact immediately after birth in women who received team midwifery care compared to those receiving routine care. This finding is in line with Allen et al. (2019), who reported that a known midwife can positively influence other aspects of care like skin-to-skin contact. When a midwife is unfamiliar with a woman, the third and fourth stages of labor are more likely to follow standard protocols, often involving routine interventions. However, continuity of care can foster a relationship between the midwife and the woman, encouraging the midwife to provide personalized support throughout the birthing process38. Despite the emphasis of the Iranian Ministry of Health on the implementation of mother-infant skin-to-skin contact, it has not yet been performed appropriately in Iran39. Therefore, continuity of team midwifery care can be one of the options for improving neonatal health in this country.
In the present study, women in the team midwifery care had significantly higher rates of exclusive breastfeeding within six weeks postpartum compared to the routine care. Mortensen et al. (2019) found an association between receiving the midwife-led model of care and increased duration of exclusive breastfeeding. They argued that this model of care provides ongoing information and support about breastfeeding during pregnancy and postpartum, which may increase the duration of exclusive breastfeeding40. On the other hand, the continuity of care within the team midwifery care group fosters trust between women and their midwives, leading to greater confidence and satisfaction with the breastfeeding information received41.
In the present study, women in the team midwifery group were more satisfied with “self”, “midwife” and “overall” satisfactions with the childbearing process.
More women in the team midwifery care group compared to the routine group indicated that they were able to manage their labor contractions, had control over their emotions and actions and could participate in decision making during labor and birth. These findings are in line with previous studies on women’s childbirth experiences42,43.
Childbirth satisfaction
In our study, women in the intervention group reported significantly higher satisfaction with midwives’ knowledge, clinical skills, positive behaviors, and attitudes, which is in line with Lyberg et al. (2010). Participants in their study reported that midwives’ strong teamwork, dedication to presence, and extensive experience in maternal care contributed to their perception of midwives as highly professional44.
In this study, the mean scores of satisfaction with the overall labor and birth experiences in the team midwifery care group were higher than those in the routine care group, which is consistent with the results of other published studies19,28,40. Both team and caseload midwifery models have been shown to increase women’s overall satisfaction with care. There is ongoing debate about whether the type of continuity of care is the primary determinant of maternal satisfaction or if other factors, such as care content, caregiver attitudes, care philosophy, and care delivery environment, play a more significant role45. According to the quantitative findings of the present study, it can be concluded that all of the mentioned factors are important in achieving maternal satisfaction, as women have diverse needs, desires, and expectations that must be met to ensure positive experiences with their care.
Strengths and limitations of the study
As a pioneering mixed-method study in Iran, this research offers unique insights. However, it is important to acknowledge certain limitations. First, since randomization was impossible in the present study, some demographic characteristics were statistically different between the two groups, which were adjusted by logistic and linear regression. Second, Iranian midwives work under the supervision of gynecologists, and they have to follow the national guidelines ( developed by gynecologists) which often mandate interventions such as induction for women who had a ruptured membrane or the use episiotomy in most cases. Also, participation in childbirth preparation classes was optional for women in the control group, which are held in a number of hospitals and midwifery clinics. But all the women in midwifery team care group participated in these classes.
Conclusion
The findings of this study showed that continuity of team midwifery of care could significantly increase the normal vaginal birth and lead to greater maternal satisfaction. In addition, this model of care contributed to a significant increase in exclusive breastfeeding rate and earlier initiation of skin-to-skin contact. These results suggested that continuity of team midwifery of care is a suitable and useful model to be implemented in the maternity care system of Iran.
Acknowledgements
This research was extracted from the PhD. dissertation of the lead author (SS). All expenses of this research were provided by Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran. The authors are grateful to all women who participated in this research and midwives who assisted us in this study.
Abbreviations
- AOR
Adjusted odds ratio
- BMI
Body mass index
- MCSRS
Mackey childbirth satisfaction rating scale
- NICU
Neonatal intensive care unit
- SD
Standard deviation
Author contributions
All authors were equally contributed to design of the study. SS collected the data. SS, PA, EM, ZA, and EM were contributed to data analyzing and interpretation. SS and PA prepared the first draft of manuscript. All authors read and approved the final version of manuscript.
Funding
This study was financially supported by Ahvaz Jundishapur University of Medical Sciences. The funder had no role in study design, data collection and analysis, and submission of the manuscript.
Data availability
Data of this study will be available upon the request from corresponding author.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Koblinsky, M. et al. Going to scale with professional skilled care. Lancet 368, 1377–1386 (2006). [DOI] [PubMed] [Google Scholar]
- 2.Renfrew, M. J. et al. Midwifery and quality care: findings from a new evidence-informed framework for maternal and newborn care. Lancet 384, 1129–1145 (2014). [DOI] [PubMed] [Google Scholar]
- 3.Bagheri, A., Simbar, M., Samimi, M., Nahidi, F. & Majd, H. A. Exploring the concept of continuous midwifery-led care and its dimensions in the prenatal, perinatal, and postnatal periods in Iran (Kashan). Midwifery 51, 44–52 (2017). [DOI] [PubMed] [Google Scholar]
- 4.de Jonge, A. et al. The importance of evaluating primary midwifery care for improving the health of women and infants. Front. Med. 2, 17 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pazandeh, F., Huss, R. & Hirst, J. An evaluation of the quality of care for women with low risk pregnancy: The use of evidence-based practice during labour and childbirth in four public hospitals in Tehran. Midwifery. (2018). [DOI] [PubMed]
- 6.Makvandi, S., Mirzaiinajmabadi, K. & Tehranian, N. The challenges of the physiologic childbirth program from the perspective of service providers: a qualitative approach. Hayat 24 (2018).
- 7.Skrondal, T. F., Bache-Gabrielsen, T. & Aune, I. All that I need exists within me: a qualitative study of nulliparous norwegian women’s experiences with planned home birth. Midwifery 86, 102705 (2020). [DOI] [PubMed] [Google Scholar]
- 8.Bahri, N., Mohebi, S., Bahri, N., Davoudi Farimani, S. & Khodadoost, L. Factors related to the decision making process of primigravid women about mode of delivery: a theory-based study. Iran. J. Obstet. Gynecol. Infertil. 20, 42–50 (2017). [Google Scholar]
- 9.Faghani Aghoozi, M., Amerian, M., Mohammadi, S., Yazdanpanah, A. & Azarabadi, S. A review of the quality of midwifery care in Iran. Educ. Ethics Nurs. 9, 52–62 (2020). [Google Scholar]
- 10.Chapman, A. et al. Maternity service organisational interventions that aim to reduce caesarean section: a systematic review and meta-analyses. BMC Pregnancy Childbirth 19, 1–21 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keedle, H. et al. Women’s experiences of planning a vaginal birth after caesarean in different models of maternity care in Australia. BMC Pregnancy Childbirth 20, 1–15 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tabrizi, J. S., Askari, S., Fardiazar, Z., Koshavar, H. & Gholipour, K. Service quality of delivered care from the perception of women with caesarean section and normal delivery. Health Promot. Perspect. 4, 137 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Firouznia, R., Dargahi, H., Koshki, T. J. & Khaledian, Z. Challenges of Iranian maternal health program from midwives’ perspectives: a qualitative study. Jundishapur J. Health Sci. 11 (2019).
- 14.Stankovic, B. Women’s experiences of childbirth in serbian public healthcare institutions: a qualitative study. Int. J. Behav. Med. 24, 803–814 (2017). [DOI] [PubMed] [Google Scholar]
- 15.Ghanbari-Homayi, S. et al. Predictors of traumatic birth experience among a group of Iranian primipara women: a cross sectional study. BMC Pregnancy Childbirth 19, 1–9 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moghasemi, S., Vedadhir, A. & Simbar, M. Models for providing midwifery care and its challenges in the context of Iran. J. Holist. Nurs. Midwifery 28, 64–74 (2018). [Google Scholar]
- 17.Hakimi, S. A century (1919-2019) of academic midwifery in Iran: From traditional midwives to PhD graduates. Eur. J. Midwifery 3 (2019). [DOI] [PMC free article] [PubMed]
- 18.Aune, I., Dahlberg, U., Backe, B. & Haugan, G. Comparing standard maternity care with team midwifery care provided by student midwives—A pilot study: women’s experiences and clinical outcomes. Vård i Norden 33, 14–19 (2013). [Google Scholar]
- 19.Waldenström, U., Brown, S., McLachlan, H., Forster, D. & Brennecke, S. Does team midwife care increase satisfaction with antenatal, intrapartum, and postpartum care? A randomized controlled trial. Birth 27, 156–167 (2000). [DOI] [PubMed] [Google Scholar]
- 20.Larsson, B., Rubertsson, C. & Hildingsson, I. A modified caseload midwifery model for women with fear of birth, women’s and midwives’ experiences: a qualitative study. Sex. Reprod. Healthc. 24, 100504 (2020). [DOI] [PubMed] [Google Scholar]
- 21.Homer, C. S., Leap, N., Edwards, N. & Sandall, J. Midwifery continuity of carer in an area of high socio-economic disadvantage in London: A retrospective analysis of Albany Midwifery Practice outcomes using routine data (1997–2009). Midwifery 48, 1–10 (2017). [DOI] [PubMed]
- 22.Homer, C. S. Models of maternity care: evidence for midwifery continuity of care. Med. J. Aust. 205, 370–374 (2016). [DOI] [PubMed] [Google Scholar]
- 23.Mortensen, B. et al. Improving maternal and neonatal health by a midwife-led continuity model of care–an observational study in one governmental hospital in Palestine. EClinicalMedicine 10, 84–91 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moudi, Z. & Tavousi, M. Evaluation of mackey childbirth satisfaction rating scale in Iran: what are the psychometric properties? Nurs. Midwifery Stud. 5 (2016). [DOI] [PMC free article] [PubMed]
- 25.McLachlan, H. L. et al. Effects of continuity of care by a primary midwife (caseload midwifery) on caesarean section rates in women of low obstetric risk: the COSMOS randomised controlled trial. BJOG: Int. J. Obstet. Gynecol. 119, 1483–1492 (2012). [DOI] [PubMed] [Google Scholar]
- 26.Tracy, S. K. et al. Caseload midwifery compared to standard or private obstetric care for first time mothers in a public teaching hospital in Australia: a cross sectional study of cost and birth outcomes. BMC Pregnancy Childbirth 14, 46 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beckmann, M., Kildea, S. & Gibbons, K. Midwifery group practice and mode of birth. Women Birth 25, 187–193 (2012). [DOI] [PubMed] [Google Scholar]
- 28.Hatem, M., Sandall, J., Devane, D., Soltani, H. & Gates, S. Midwife-led versus other models of care for childbearing women. Cochrane Database Syst. Rev. (2008). [DOI] [PubMed]
- 29.Tracy, S. K. et al. Caseload midwifery compared to standard or private obstetric care for first time mothers in a public teaching hospital in Australia: a cross sectional study of cost and birth outcomes. BMC Pregnancy Childbirth 14, 1–9 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sandall, J., Soltani, H., Gates, S., Shennan, A. & Devane, D. Midwife continuity of care models versus other models of care for childbearing women. Cochrane Database Syst. Rev. (2016). [DOI] [PMC free article] [PubMed]
- 31.Voon, S. T., Lay, J. T. S., San, W. T. W., Shorey, S. & Lin, S. K. S. Comparison of midwife-led care and obstetrician-led care on maternal and neonatal outcomes in Singapore: a retrospective cohort study. Midwifery 53, 71–79 (2017). [DOI] [PubMed] [Google Scholar]
- 32.Rowley, M. J., Hensley, M. J., Brinsmead, M. W. & Wlodarczyk, J. H. Continuity of care by a midwife team versus routine care during pregnancy and birth: a randomised trial. Med. J. Aust. 163, 289–293 (1995). [DOI] [PubMed] [Google Scholar]
- 33.Sehhatie, F., Najjarzadeh, M., Zamanzadeh, V. & Seyyedrasooli, A. The effect of midwifery continuing care on childbirth outcomes. Iran. J. Nurs. Midwifery Res. 19, 233–237 (2014). [PMC free article] [PubMed] [Google Scholar]
- 34.Gidaszewski, B., Khajehei, M., Gibbs, E. & Chua, S. C. Comparison of the effect of caseload midwifery program and standard midwifery-led care on primiparous birth outcomes: a retrospective cohort matching study. Midwifery 69, 10–16 (2019). [DOI] [PubMed] [Google Scholar]
- 35.Tumbull, D. et al. Randomised, controlled trial of efficacy of midwife-managed care. Lancet 348, 213–218 (1996). [DOI] [PubMed] [Google Scholar]
- 36.Begley, C. et al. Comparison of midwife-led and consultant-led care of healthy women at low risk of childbirth complications in the Republic of Ireland: a randomised trial. BMC Pregnancy Childbirth 11, 1–10 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Iida, M., Horiuchi, S. & Nagamori, K. A comparison of midwife-led care versus obstetrician-led care for low-risk women in Japan. Women Birth 27, 202–207 (2014). [DOI] [PubMed] [Google Scholar]
- 38.Allen, J. et al. Immediate, uninterrupted skin-to-skin contact and breastfeeding after birth: a cross-sectional electronic survey. Midwifery 79, 102535 (2019). [DOI] [PubMed] [Google Scholar]
- 39.Adeli, M. & Azmoudeh, E. Influential factors of mother-infant skin-to-skin contact based on the precede-proceed model from the perspective of midwives in Torbat Heydariyeh hospitals. (2016).
- 40.Mortensen, B. et al. Women’s satisfaction with midwife-led continuity of care: an observational study in Palestine. BMJ Open 9, e030324 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bäckström, C. A., Wahn, E. I. H. & Ekström, A. C. Two sides of breastfeeding support: experiences of women and midwives. Int. Breastfeed. J. 5, 1–8 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McLachlan, H. L. et al. The effect of primary midwife-led care on women’s experience of childbirth: results from the COSMOS randomised controlled trial. BJOG Int. J. Obstet. Gynecol. 123, 465–474 (2016). [DOI] [PubMed] [Google Scholar]
- 43.Flint, C., Poulengeris, P. & Grant, A. The ‘know your midwife’scheme—A randomised trial of continuity of care by a team of midwives. Midwifery 5, 11–16 (1989). [DOI] [PubMed] [Google Scholar]
- 44.Lyberg, A. & Severinsson, E. Fear of childbirth: mothers’ experiences of team-midwifery care–a follow‐up study. J. Nurs. Adm. Manag. 18, 383–390 (2010). [DOI] [PubMed] [Google Scholar]
- 45.Forster, D. A. et al. Continuity of care by a primary midwife (caseload midwifery) increases women’s satisfaction with antenatal, intrapartum and postpartum care: results from the COSMOS randomised controlled trial. BMC Pregnancy Childbirth 16, 1–13 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data of this study will be available upon the request from corresponding author.