Abstract
The Melillo et al. article: Reliability and validity of the Veterans Administration Mobility Screening and Solutions Tool (MSST) (Melillo et al, BMC Health Serv Res 22:1323, 2022) introduces the MSST, a derivative flowchart tool in which the Banner Bedside Mobility Assessment Tool (BMAT) is embedded. The authors identify similar goals for the MSST as those for the BMAT, i.e. determine real-time mobility status and choose safe patient handling and mobility (SPHM) equipment to complete transfer and mobility tasks. Further Melillo et al. indicate that goals included “revising and enhancing” and addressing “gaps” in the BMAT, as well as creating instructions for the four BMAT levels (sit and shake, stretch and point, stand, step: march-in-place, advance step and return) that are clear, understandable and comfortable to use. The authors indicate that another goal of the VA MSST is it “enables any healthcare worker at any time to accurately measure and communicate patient mobility and transfer equipment needs.” The present article addresses inaccuracies observed in the Melillo et al. article and confusing elements found in the VA MSST flowchart. The present article is based on the author’s involvement in developing the BMAT starting in 2003 along with teams from Banner Health and Liko/Hill-Rom which incorporated use of the BMAT by unlicensed assistive personnel (UAP) as a recheck or verification of earlier testing. The 2020 BMAT 2.0 clarified confusing elements identified in BMAT 1.0, i.e. items that needed to be revised or enhanced. BMAT 2.0 covered use of SPHM when testing, when completing care tasks and when progressing patients. The BMAT is primarily a nurse-driven mobility assessment tool created to not be overly prescriptive. BMAT was validated and determined to be reliable based on years of clinical utility studies and research in various settings across the continuum of care. It continues to be supported by a large medical equipment manufacturer who maintains the copyright license. Although the VA MSST flowchart has the four BMAT assessment levels embedded within it, for reasons outlined in this article, it is not feasible to use the VA MSST flowchart alongside or in conjunction with the BMAT 2.0.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-024-11655-z.
Main text
Implementing safe patient handling and mobility (SPHM) practices is challenging [1]. Sustainable SPHM programs require standardized evaluation protocols and appropriate use of SPHM equipment [2, 3]. Although slightly modified by Melillo et al., the actual Bedside Mobility Assessment Tool (BMAT) [4–6] is embedded in the VA Mobility Screening and Solutions Tool (MSST) [7], which derives from the BMAT.
The present article is based on the author’s involvement with developing the BMAT with teams from Banner Health and Hill-Rom. The revised version of BMAT (2020 BMAT 2.0) [6] clarified confusing elements identified in early versions of BMAT 1.0 support tools, i.e. addressing bedrest/strict bedrest orders, weight-bearing restrictions, and further clarifying why a “Mobility Level 0 Patient” designation for critical care patients is unnecessary [8–10]. Further BMAT 2.0 covered using safe mode and SPHM practices when testing, completing patient care tasks, and progressing patients [6].
This article is not intended as a critique of the authors’ psychometrics testing - it is recognized that the VA authors’ methods are reasonable, further validate the BMAT as a tool that can be used by unlicensed assistive personnel (UAP) as a recheck, and supports BMAT validity and reliability [8–11]. However, inaccurate statements regarding the BMAT were observed in the Melillo et al. article and in the VA MSST flowchart that the author wishes to address. This present article maintains that while Melillo et al. stated goals were to revise and enhance the BMAT, they may have made their derivative tool more complex by reverting to language and concepts from early versions of BMAT tools (that were either eliminated or clarified after 2013) to adding confusing elements. While identifying the VA MSST flowchart as a screening tool, Melillo et al. included elements that make it function as an assessment which is outside the scope of practice for many health care workers (HCW).
Overview of mobility assessments and screenings
Many tools are available to drive mobility testing and clinical decisions supporting care. A table outlining these tools and types of practices can be found in [6, 8, 12] and in Table 1.
Table 1.
Summary of selected mobility assessments and screenings
| Name | Description |
|---|---|
| 1957 PULSES Profile | Six components: Physical Condition, Upper Extremities, Lower Extremities, Sensory Function, Excretory Function, and Social and Mental Status; scored from 1 to 4 (1 = Normal, 2 = Mild, 3 = Moderately Severe, 4 = Severe; with descriptors for each level); designed to evaluate functional independence in ADLs with elderly institutionalized population. Administered by clinical staff. Validated: UTD* |
| 1965 Barthel Index of Activities of Daily Living (BI) | Ten-item ordinal scale that measures functional independence using the following components: Transfers (0 - unable, no sitting balance to 15 - independent); Mobility on level surfaces (0 - immobile of < 50 yards to 15 - independent but may use any aid > 50 yards); Stairs (0 - unable to 10 - independent). For assessing mobility in acute care and with rehabilitation patients to predict length of stay and amount of nursing care needed. Administered by clinical staff. Validated: UTD |
|
1986 Timed Up and Go Test (TUG) Get Up and Go Test |
One timed sequence: (1) On “Go:” Stand up from the chair; Walk to the line on the floor at normal pace; Turn; Walk back to the chair at normal pace; Sit down again. (2) On the word “Go,” begin timing. (3) Stop timing after patient sits back down. (4) Record time (in seconds). Older adult who takes ≥ 12 s to complete the TUG is at risk of falling. Common instrument for assessing mobility in acute care; inadequate scale width for people whose limitations are either too severe or relatively modest. Administered by clinical staff. Validated: Yes. Identified for use with these patient populations: stoke, spinal injuries, Parkinson’s disease, osteoarthritis, Alzheimer’s, vestibular disorders. [Soubra 2019] |
| 1987 *Functional Independence Measure |
Three main categories: Independent: 7. Complete Independence 6. Modified Independence; Dependent: 5. Supervision or set up 4.Minimal Assistance 3. Moderate Assistance; Complete: 2. Maximal Assistance 1. Total Assistance. Widely used tool that classifies a patient’s function; criterion-referenced and administered by trained and tested clinicians in order for assessments of functioning to be uniform across different certified raters. Administered by PTs/OTs/Nurses. Validated: UTD * Uniform Data System for Medical Rehabilitation: Functional Independence Measure (FIM) [Chumney 2010 and Uniform Data System for Medical Rehabilitation, The FIM Instrument] 1987 |
| 1988 Braden Scale for Predicting Pressure Sore Risk |
Six categories: Sensory, Moisture, Activity (degree of physical activity), Mobility (ability to change and control body position), Nutrition, Friction and Shear scored by RN. For Activity: bedfast/confined to bed = 1, chairfast: ability to walk severely limited or non-existent; cannot bear own weight and/or must be assisted into chair or wheelchair = 2; walks occasionally = 3; walks frequently = 4. For Mobility: completely immobile/does not make even slight changes in body or extremity position without assistance = 1; very limited/makes occasional slight changes in body or extremity position but unable to make frequent or significant changes independently = 2; slightly limited/makes frequent though slight changes in body extremity position independently = 3; no limitations/makes frequent major changes in position without assistance = 4. For Friction and Shear: problem/requires moderate to maximum assistance in moving/complete lifting without sliding against sheets in impossible; frequently slides down in bed or chair, requiring frequent repositioning with maximum assistance; spasticity, contractures or agitation leads to almost constant friction = 1; potential problem/moves freely or requires minimum assistance; during a move, skin probably slides to some extent against sheets, chair, restraints or other devices; maintains relatively good position in chair or bed most of the time but occasionally slides down = 2; no apparent problem/moves in bed and in chair independently and has sufficient muscle strength to lift up completely during move; maintains good position in bed or chair at all times = 3 Validated: UTD |
| 1994 Physical Performance Mobility Examination (PPME) | Six mobility tasks: bed mobility, transfer skills, multiple stands from chair, standing balance, step-up, and ambulation. Pass/Fail and 3-level scoring system; performance-based instrument measuring physical functioning and mobility in hospitalized and frail elderly; validated; “observer-administered.” Administered by clinical staff. Validated: Yes |
| 1997 St. Thomas Risk Assessment Tool (STRATIFY) Fall Risk Tool |
Five subscales: transfer and mobility, history of falls, vision, agitation, and toileting Asks if the patient has a combined transfer and mobility score of 3 or 4 based on which of the following best describes the patient’s level of capability when transferring from a bed to a chair with 0 = unable, 1 = needs major help, 2 = needs minor help, 3 = independent AND For the mobility score choose the following option which best describes the patient’s level of mobility with 0 = immobile, 1 = independent with the aid of a wheelchair, 2 = uses walking aid or help of one person, 3 = independent. Validated: Yes |
|
1994 Elderly Mobility Scale (EMS) [Elderly Mobility Scale. Ver 2]; updated 2012 |
Seven components each scored from 0 to 2, 0–3 or 0–4: Lying to Sitting; Sitting to Lying; Sitting to Standing; Standing; Gait; Timed Walk (6 m); Functional Reach. Totaled up to 20/20 with: Scores under 10 = dependent in mobility: require help with basic ADLs; Scores between 10–13 = borderline: requires some help Scores over 14 = independent: able to perform mobility maneuvers alone and independent in basic ADLs; appropriate for elderly patients in a hospital setting. Administered by clinical staff/Nurses/PT/OT/aides. Validated: Yes |
| 1995 4-Stage Balance Test | One timed sequence: For each position say, “Ready, begin” and start timing. After 10 s, stay, “Stop” for: (1) Stand with your feet side-by-side; (2) Place the instep of one foot so it is touching the big toe of the other foot; (3) Tandem stand (4) Stand on one foot. Tool to assess mobility and risk of falls, based on ability to hold four progressively more challenging positions; appears to have acceptable reliability, validity, and discriminant ability. Administered by clinical staff. Validated: UTD |
| 1999 30-Second Chair Stand Test | One timed sequence: Instruct patient to: (1) Sit in the middle of the chair; Place hands on opposite shoulder crossed, at the wrists; Keep fee flat on the floor; Keep back straight, and arms against chest; On “Go” rise to a full standing position, then sit back down again; Repeat for 30 s. (2) On the word “Go,” begin timing. If uses arms to stand, stop the test. (3) Count times patient comes to full standing position in 30 s. (4) Record the number of times the patient stands in 30 s. Use chart based on age and gender to score; below average score indicates a risk for falls. Designed for use with community dwelling elders. Administered by staff. Validated: UTD |
|
2000 Hierarchical Assessment of Balance and Mobility (HABAM) |
Three domains: Balance: scored from 0–21 (0 = impaired static sitting up to 21 = stable ambulation); Transfers: scored from 0–18 (0 = total lift; 3 = 2 person assist up to 18 = independent); Mobility: scored from 0–26 (0 = needs positioning in bed; 4 = positions self in bed up to 25 = limited > 50 m; 26 = unlimited); designed for use with hospitalized patients; validated against the Barthel Index; studies have noted an inability to discriminate among higher-performing participants. Administered by Nurses/PTs/OTs. Validated: Yes |
| 2003 Hendrich II Fall Scale |
Score based on gender, mental and emotional status, symptoms of dizziness, and use of specific categories of medications (i.e., antiepileptics, benzodiazepines)4 Inclusion of the “Get Up and Go test” was the major change between version I and II Validated: Yes |
|
2004 AM-PAC Activity Measure for Post Acute Care (AM-PAC) 2004 AM-PAC Inpatient Mobility Short Form (AM-PAC IMSF) 2007 AM-PAC “6-Clicks” |
Three Domains: Basic Mobility Domain/Movement and Physical including Ambulation and Transfers (131 items); Daily Activity Domain; Applied Cognitive Domain. AM-PAC Generic Outpatient Basic Mobility Short Form: 18 items scored on “difficulty do you currently have…” (e.g., standing up from a low, soft couch; taking a 1-mile brisk walk without stopping to rest) scored from 1 -Unable to 4 -None. Designed to be used during post-acute care rehabilitation. 6-Clicks: Physical Therapist evaluates patient’s abilities for: (1) Turning over in bed; (2) Supine to sit; (3) Bed to chair; (4) Sit to stand; (5) Walk in room; (6) 3–5 steps with a rail. Occupational Therapist evaluates patient’s abilities for: (1) Feeding; (2) O/F hygiene; (3) Dressing Uppers; (4) Dressing Lowers; (5) Toilet (toilet, urinal, bedpan); (6) Bathing (wash/rinse/dry). Score using scale: 1 = Unable (Total Assist); 2 = A Lot (Mod/Max Assist); 3 = A Little (Min Assist/Supervision); 4 = None (Independent). Purpose: Improve mobility, guide discharge recommendations and therapist utilization - therapists seeing the right patient at the right time for the right reason. validated in a single-center stud; licensed from Mediware.com. Administered by PTs/OTs/Nurses. Validated: Yes |
| 2005 Liko Quick 5 Bedside Guide | Five Maneuvers/Tests: evaluate functional competence and score “Fail” or “Pass:” Roll; Bridge; Sit and Shake; March; Stand. Assists with choosing safe patient handling device based on demonstrated functional competence and limitations; not validated; revised to the Liko Quick 3. Administered by PTs/OTs/Nurses. Validated: No |
| 2005 Egress Test | Three Phases/Components: Three Reps of Sit-to-Stand; Three Steps of Marching in Place – each leg; Advance Step and Return Each Foot. If patient requires assistance greater than cues and guarding techniques, indicated for mechanical lift until demonstrates consistent performance. Purpose: safe progression and “defensible” patient transfer. Administered by PTs. Validated: UTD |
| 2005 Johns Hopkins Fall Risk Assessment Tool (JH-FRA) |
Six subscales: history of falls, toileting, medications, patient care equipment, mobility, and cognition. For mobility choose all that apply and add points together: requires assistance or supervision for mobility, transfer or ambulation = 2 points; unsteady gait = 2 points; visual or auditory impairment affecting mobility = 2 points. Validated: UTD |
| 2007 Liko Quick 3 |
Three Tests/Assessment Levels: evaluate functional competence and score “Fail” or “Pass:” Sit and Shake, Kick and Point, Stand. Assists with choosing appropriate Liko lift and sling/safe patient handling device(s) based on demonstrated functional competence and limitations. Includes THERAPY REFERENCE GUIDE: Patient Progression with Patient Handling Equipment that covers FIM scores and choosing sling and lift options. Based on Liko Quick 5 Bedside Guide. Liko Quick 3 is the foundation for the Bedside Mobility Assessment Tool for Nurses (BMAT; aka the Banner Mobility Assessment Tool for Nurses), which is validated. Administered by PTs/OTs/Nurses. Validated: No |
| 2008 de Morton Mobility Index (DEMMI) | Five Main Categories/Fifteen Items assigned Raw Score from 0–19 and DEMMI Score from 0-100: Bed: (1) Bridge; (2) Roll on to side; (3) Lying to sitting; Chair: (4) Sit unsupported in chair; (5) Sit to stand from chair; (6) Sit to stand without using arms; Static balance (no gait aid) (7) Stand unsupported; (8) Stand feet together; (9) Stand on toes; (10) Tandem stand with eyes closed; Walking: 11. Walking distance +/-gait aid; 12. Walking independence; Dynamic balance: 13. Pick up pen from floor; 14. Walks 4 steps backwards; 15. Jump. Measures mobility across the spectrum from bed bound to independent mobility. Developed for use among hospitalized older adults; validated; can identify meaningful changes in mobility between admission and discharge. Administered by staff. Validated: Yes |
| 2009 Morse Fall Scale |
Six subscales used as a screening tool: history of falls, secondary diagnosis, ambulatory aid, IV/heparin lock, gait (normal/bedrest/wheelchair = 0 points, weak gait = 10 points, impaired gait = 20 points) and mental status; completed as a screening tool used to determine when a more comprehensive fall assessment is needed; includes suggested interventions to prevent falls including preventative and protective strategies Validated: Yes |
| 2014 Perme Intensive Care Unit Mobility Score | Seven Components and Fifteen Items: Mental Status; Potential Mobility Barriers; Functional Strength; Bed Mobility; Transfers: Gait; Endurance. ICU-specific tool to measure mobility status of patients with limited independent activities, indicative of functional performance, and particularly the patient’s walking capability. Administered by clinical staff. Validated: Yes |
| 2009 I-MOVE |
Twelve-point scale: (1) Turns in bed with assistance; (2) Turns in bed independently; (3) Sits on bed with assistance; (4) Sits on bed independently; 5. Stands with assistance; 6. Stands independently; 7. Sits in chair with assistance; 8. Sits in chair independently; b Walks in room with assistance 10. Walks in room independently; 11. Walks in hallway with assistance; 12. Walks in hallway independently. Identify patients early to get therapy; measurement of functional outcome; “could help hospitalists assess their patients’ mobility.” Administered by clinical staff. Validated: UTD |
| 2013 Hester Davis Scale for Fall Risk | Nine sub-categories: Age, Last Known Fall, Mobility, Medications, Mental Status/LOC/Awareness, Toileting Needs, Volume/Electrolyte Status, Communication/Sensory, Behavioral Status. RNs score mobility as follows (select all that apply): no limitations = 0, dizziness/generalized weakness = 1, immobilized/requires assist of one person = 2, use of assistive device/requires assist of two people = 3, hemiplegic, paraplegia, quadriplegia = 4; higher the sub-category score and total score, higher the fall risk. Validated: UTD |
|
2014 Banner Bedside Mobility Assessment Tool (BMAT) 2020 Bedside Mobility Assessment Tool 2.0 (BMAT 2.0) |
Four maneuvers/assessment levels: The Bedside Mobility Assessment Tool (BMAT/BMAT 1.0/BMAT 2.0) is a structured test of patient mobility developed for use by nurses and by unlicensed aids, assistants and technicians (UAP) as a recheck or exercise following set protocols within state practice acts and delegation guidelines. Based on the Liko 2007 Quick 3 and 2005 Egress Test. Patients are assessed for their ability to independently perform a series of maneuvers: sit and shake, stretch and point, stand and step: march-/step-in-place; forward step and return. The tool contains recommendations for safe patient-handling techniques based on the patient’s real-time observed level of mobility. A validation study by the developers of BMAT demonstrated good inter-rater reliability with hospitalized patients in a medical-surgical unit and an intensive care unit using random checks of 20 patients on each unit. Additionally a 30 patient sample was evaluated using the BMAT in ICU, medical-surgical and neurology units with good agreement on mobility level as independently assessed by a physical therapist and a SPHM Specialist, who was also a nurse. Construct validity was assessed through a contrasted groups approach with expert agreement. Prior to the 2013 IRB validation project, a clinical utility research approach with feedback and data collection from nurses and CNAs using the BMAT over a three-year period with patients at 11 hospitals was completed, and support tools including flowcharts and algorithms were created to support the IRB project and system-wide implementation including training tools and competency checklists for licensed professionals and UAP. A 2014 Banner system-wide strategic initiative further validated inter-rater reliability of BMAT used with patients in acute care settings. BMAT 2.0 contains the same validated maneuvers and components as BMAT 1.0 but also focuses on safe mode for testing, completing patient care tasks, progressing and strengthening, and on optimal discharge planning and placement. In acute care settings, BMAT is linked to the fall risk and skin assessments, task list and patient care plan in the EMR. Validated: Yes |
|
2016 Johns Hopkins Highest Level of Mobility (JH-HML) |
Four Main Categories scored from 1 to 8: Bed: Lying = 1; Turn Self/Activity = 2; Sit at Edge = 3; Chair: Transfer = 4; Stand: 1 min = 5; Walk: 10 + Steps = 6; 25 + Feet = 7; 250 + Feet = 8. Track patient’s function longitudinally through acute-care and post-acute care services; fulfill CMS regulatory requirements - address Core Measure that requires inclusion of functional status; CMS meaningful use and conditions of participation. Designed for in-hospital use. Validated: Yes |
| Minimum Data Set 3.0 v1.14 | Two Measures of Mobility Function: The Minimum Data Set 3.0 v1.14, which is used to assess nursing home residents, contains two measures of mobility function. In section G, the patient’s ability to lie down, sit, stand, transfer, and walk is rated on a five-level scale from independent to fully dependent. This measure has been validated and is used to assign Resource Utilization Group codes for payment. In Section GG, which was developed for the Post-Acute Care Payment Reform Demonstration (PAC-PRD) project, the patients’ ability in each of five domains (sit, stand, transfer, walk 50 feet, and walk 150 feet) is rated on a six-level scale from independent to fully dependent. Section G will eventually be phased out in favor of Section GG. Neither of these measures has been tested in hospitalized populations. Validated: Yes – nursing home residents; No – hospitalized patients |
| 2022 The Veterans Administration (VA) Mobility Screening and Solutions Tool (MSST) with embedded BMAT | Seven Screening Questions/Four BMAT maneuvers: The VA MSST flowchart is a derivation tool of the BMAT, which the VA considers a screening tool that can be completed by any healthcare worker, including unlicensed assistive personnel (UAP) trained to test a patient’s mobility status and consider fall risk. It starts by having HCW ask two questions: (1) Is the patient currently walking independently without assistance or support and with good safety awareness? (2) Was the patient available for screening? It uses the same maneuvers as the BMAT but is separated into 7 Mobility Levels including Mobility Level 0 for patients who are unavailable for screening; screeners may go back and forth between Mobility Level 0 and Mobility Level 1 (i.e. these are interchangeable with no SPHM equipment suggested for Mobility Level 0 patients). For Mobility Level 2 Patients (unable to pass “Stretch and Point”), HCW are instructed to use powered equipment; for Mobility Level 3P (Powered) patients, HCW are instructed to use powered equipment; for Mobility Level 3 N (Non-powered) patients, HCW are instructed to consider a non-powered stand aid or full body lift with ambulation harness (which is typically a powered device). For Mobility Level 1 (patients unable to pass “Sit and Shake”) through Mobility Level 3 N (Non-powered), suggested equipment includes use of a multifunction vertical tilt bed. The BMAT embedded in the VA MSST flowchart is designated as a screening tool (versus part of a comprehensive nurse-driven mobility and physical assessment) for use by any HCW at any time to accurately measure and communicate mobility and transfer equipment needs across disciplines and settings. For Mobility Level 4 no SPHM equipment is suggested but the HCW is instructed to consider if the patient has high fall risk, and, if “yes,” the HCW is instructed to consider supervision. Similar to BMAT, the VA MSST flowchart instructs HCW to always default to the safest choice of SPHM equipment. Reliability and validity based on viewing and screening 18 filmed scenarios is good. VA MSST instructions (which are very similar to BMAT instructions) were found by VA raters to be clear or very clear compared to BMAT instructions which were rated uncomfortable to use. Although labeled a screening tool, the VA MSST flowchart functions as an assessment. Validated: Yes. Limitation: Not validated with patients |
Many therapy-focused mobility assessments (including Barthel Index, Hierarchical Assessment of Balance and Mobility, and Activity Measure for Post Acute Care) are designed to determine mobility limitations, establish baselines, assist with care planning and rehabilitation goals, and enhance discharge planning. Compared to BMAT, these other tools include more components and are more like functional activities of daily living (ADL) assessments. They may be part of a comprehensive assessment, but unlike BMAT, they are not linked to safe patient handling and mobility interventions and technology based on real-time mobility status and safety needs, nurse-driven and used as a recheck, verification or exercise when delegated to UAP. BMAT is used with both adult and pediatric populations
Other mobility tools like the Rivermead Mobility Index, the Canadian Neurological Scale, the Expanded Disability Status Scale, the Hauser Ambulatory Index, the Functional Mobility Assessment Tool, the Mobility Scale, the Physiotherapy Functional Mobility Profile, Katz Activities of Daily Living Scale, Minimum Data Set, 2018 HELP Mobility Change Package and Toolkit with Baseline Mobility Assessment Tracking Health Recovery in Veterans (THRIVe) and 20 s Just in Time Assessment (JITA) of patient’s mobility, are not included in this review. Additionally the following mobility assessments identified for use with specific patient populations (e.g. stroke, spinal injuries, Parkinson’s disease, osteoarthritis, Alzheimer’s, vestibular disorders, multiple sclerosis, arthritis, back pain, neuromuscular disease) are not covered: 5-Time Sit-to-Stand, Tinetti Performance Oriented Mobility Assessment, Physical Performance Test. Balance Evaluation Systems Test, Dynamic Gait Index, Functional Gait Assessment, 6-minute Walk Test, Usual/Habitual Gait Speed, Life Space Mobility Assessment, Turn 180, Backward Walking are not included. Within the scope of this Matters Arising article and table, the author is unable to provide a discussion of the pros and cons of each tool
*UTD Unable to determine
Aim of BMAT
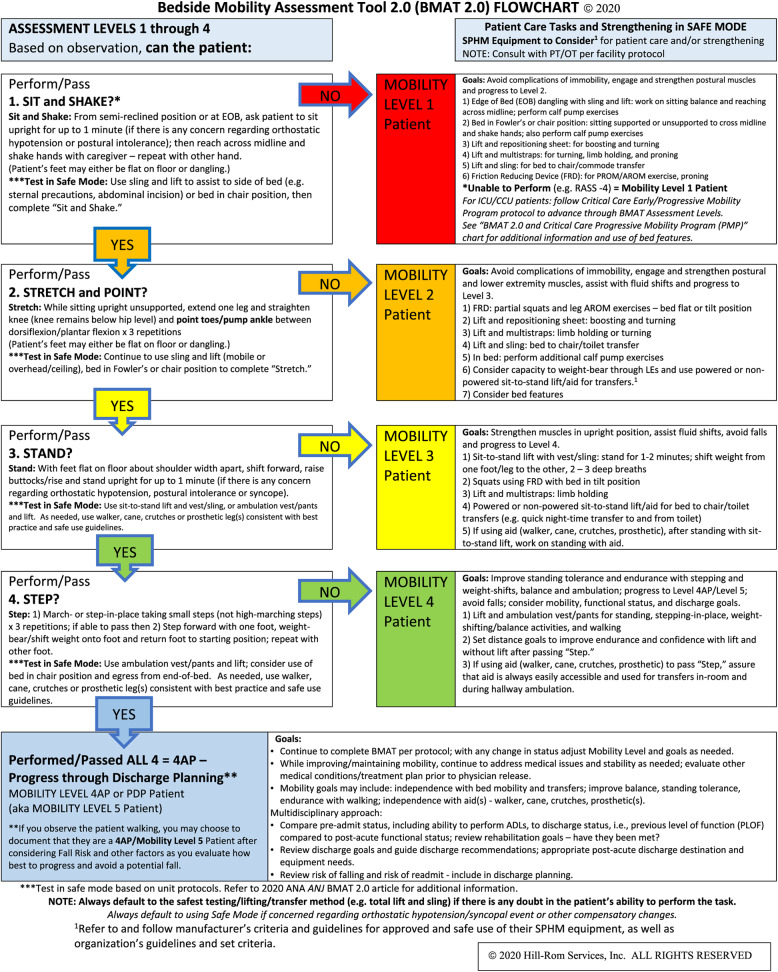
The aim of BMAT is to determine a patient’s current mobility status (based on completing four maneuvers: sit and shake, stretch and point, stand, step: march-in-place, advance step and return), assign a mobility level and choose equipment to complete a task [4–6]. This makes BMAT different compared to mobility tools not designed to assist in choosing SPHM equipment. See Fig. 1.
Fig. 1.
Example of support tool for acute care settings - Link to bedrest orders, weight-bearing limitations, cognition, fall risk
Melillo et al. state that the “VA MSST was developed to screen a patient’s safe mobility level ‘in the moment’ and provide clinical decision support related to the use of safe patient handling and mobility (SPHM) equipment,” which is the same reason the BMAT was developed. The use of BMAT by UAP is not unique to the MSST but has been the practice in acute care settings following National Council of State Boards of Nursing (NCSBN) practice guidelines [13] for over 10 years. While empowering nurses to take responsibility for safely mobilizing patients was a primary reason for creating BMAT, this was not the only reason [4–6, 8–11].
Goals for BMAT were: (1) standardizing use of SPHM equipment across the continuum of care, (2) decreasing caregiver injuries associated with manual handling, transfers and controlled descents [14], (3) addressing the need for a mobility tool linked to falls, progressive mobility and delirium prevention. Other goals focused on applying “Just Culture” to SPHM practices, allowing UAP to use BMAT following delegation guidelines, promoting appropriate referrals to rehabilitation, increasing awareness that mobility can change during a shift, and avoiding day of discharge surprises.
Psychometrics, education and training
This article is not a critique of the authors’ psychometrics but is focused on confusing items and questioning the authors’ definition of a screening tool intended to be used by any HCW, including UAP, at any time across all settings.
The psychometrics testing of the MSST derivative tool and methods are reasonable - they further validate the BMAT as a reliable tool. The video scenarios appear to be good training tools; however, it is still recommended that inter-rater reliability and validity be determined with patients.
The validity and reliability of MSST could be further examined by reviewing patient initiatives the VA wanted to address. A review of how BMAT was modified for use in settings like emergency departments (EDs) and outpatient settings compared to why Melillo et al. created MSST to be valid for use in any setting would be helpful. A discussion of reliability of MSST related to scope of practice for professionals and how the VA handles delegation to UAP is recommended. Further, it would help to compare BMAT 2.0 instructions to MSST instructions for clarity and understanding and compare BMAT 2.0 four assessment levels to MSST’s seven levels when evaluating “comfortable to use.” Revisions made to BMAT 1.0 support tools after 2013 and the BMAT 2.0 article and support tools address gaps and revision of items identified in the MSST article and flowchart. Since Melillo et al. did not recognize these revisions and did not indicate which BMAT instructions were used, it is reasonable to question if the authors used more current BMAT instructions for their comparisons.
During its evolution, in addition to developing clear BMAT instructions on how to complete each level, standardization of education and creating training tools was critical with competencies collaboratively identified by educators, frontline staff, managers and multidisciplinary program improvement leaders. (See Tables S1 and S2).
Although Melillo et al. do not specify which BMAT instructions they used, they compared BMAT instructions with the instructions they created for the MSST flowchart with 56% of raters endorsing MSST instructions as clear or very clear compared to 39% of raters endorsing BMAT instructions as Not-or Somewhat- or Moderately-comfortable to use. Mobility Level 0 and the first two questions of the MSST were not included by the authors when rating clarity; however, 82% of MSST instructions were rated clear/very clear with more than three quarters rating every level of MSST instructions as clear/very clear and understandable. It would be helpful to know why Level 0 and the first two questions were not included.
Assessment tools compared to screening tools
Screenings and assessments are performed in many disciplines for a variety of reasons. Frequently, screenings and assessments are discussed as if they are interchangeable tools that are used the same way for the same purpose. However, there are critical distinctions [15–17]. Screenings are used to evaluate the possible presence of a particular problem. Outcomes are normally a simple yes or no or score with no intervention recommended. If a screening shows positive findings, instructions often include a follow-up assessment. Assessments are a process for defining the problem and developing interventions to address the problem. In the case of mobility-related challenges, the intervention may include use of SPHM equipment.
The fact that the BMAT is a nurse-driven assessment designed to be used by UAP as a recheck or exercise is not a gap in the BMAT that needed to be revised or enhanced. Original use of the BMAT by UAP considered delegation guidelines for licensed professionals supervising UAP and other factors [8–11, 15]. Assigning a mobility level and choosing safe interventions should not be done based only on use of a screening tool completed by a UAP.
Although labeled a screening tool, the MSST functions as an assessment tool with respect to requiring the HCW to: (1) consider if a Level 4 patient is a high fall risk who needs supervision but does not need ambulation equipment to avoid a fall, (2) evaluate if a patient is “currently walking independently without assistance or support and with good safety awareness,” (3) understand criteria for use of equipment like specialty beds and ceiling lifts, (4) have knowledge of manufacturer’s patient criteria and guidelines to choose options from the list of suggested equipment, (5) differentiate between critical care Mobility Level 0 and Level 1 patients.
Whether screening or assessment, regulatory bodies, liability and scope of practice need to be considered when determining who is qualified, responsible for and permitted to complete a test. Labeling the MSST a screening tool does not automatically allow any HCW at any time to measure, communicate, choose and use transfer equipment across disciplines and settings without considering type of unit, findings from comprehensive assessments, and addressing how a UAP potentially contradicting a supervising professional will be handled. (See Table S3.)
Rehabilitation specialty units
The authors indicate that mobility is within the scope of practice for all HCW. However, they acknowledge there are exceptions as the “VA MSST does not replace other mobility assessments, especially those used by occupational or physical therapists in rehabilitation specialties.” This leads to another observed inaccuracy and reason the BMAT was created: to improve communication between nursing and rehabilitation staff acknowledging that nursing staff are with the patient 24/7. Also that (1) a patient’s mobility status can change during a shift (i.e. what PT evaluated and recommended in the morning may no longer be appropriate in the afternoon if the patient has declined), (2) not all patients have a new functional deficit related to the current hospitalization that needs PT/OT input, (3) not all patients will see a PT/OT during their stay or will only see rehabilitation day of discharge, (4) that referrals to rehabilitation become more timely when nursing staff use BMAT on admission, at least once per shift and with any change in status, and (5) mobility practices (even in rehabilitation specialty settings) require nursing to be responsible for meeting mobility goals. While nurses working in rehabilitation specialty units are expected to coordinate with rehabilitation staff, they are still expected to address mobility goals – they should not just delegate mobility to the treating PT nor should they only rely on the mobility assessment and guidelines previously given by PT/OT, especially if the RN has determined that the patient declined.
Education and support tools
In addition to developing clear BMAT instructions on how to complete each level (sit and shake, stretch and point, stand and step), standardization of education and creating support tools like flowcharts was critical with competencies collaboratively identified by educators, frontline staff, managers and quality improvement/program improvement leaders. (See Table S2).
Examples of confusing items and increased complexity
Following are three examples of confusing items or items that add complexity found in the MSST flowchart.
Mobility Level 0 versus Mobility Level 1: Melillo et al. added Mobility Level 0 defined as answering “No” to the question “Was patient available for screening?” with no SPHM equipment suggested for Mobility Level 0 patients. Melillo et al. also state that HCW may alternate between Level 0 and Level 1 and indicate they need to define what this means - what action should be taken when a patient is “unavailable for screening” and labeled Mobility Level 0 patient who may be a critically ill patient but with no suggested SPHM practices listed.
Unclear screening questions: The first MSST question asked by the HCW is: “Is the patient currently walking independently without assistance or support and with good safety awareness?” If the answer is “Yes,” the patient is Mobility Level 4 and no SPHM equipment is needed. If the patient is determined to be a Level 4 patient after completing “March and Step without Support,” the HCW should “Consider supervision if the patient has high fall risk.” If the answer to the first question is “No” - the patient was either not observed walking or was observed walking independently but with assistance or support or with poor safety awareness, the HCW determines “Was the patient available for screening?” If the answer is “Yes,” the HCW is instructed to “Begin Screening. What can the patient do?” and evaluate the patient’s ability to perform “sit and shake.” If the patient is walking but is not available for screening, the screener is instructed to rate them a Mobility Level 0. This is confusing. It would be helpful if the authors identified under what circumstances a HCW screener would make this determination, where and how the HCW is expected to communicate and document their findings that the patient was observed walking with poor safety awareness but was unavailable for screening.
Overly prescriptive equipment recommendations: Because of its increased complexity, seven distinct evaluation questions (with the first question containing three sub-questions) and seven mobility levels, use of MSST may encourage unnecessary equipment purchase and delays in implementing SPHM practices. Suggested use of multi-function vertical tilt beds, for Mobility Level 1 through Mobility Level 3P (Powered) patients may be unnecessarily restrictive for higher functioning patients - those who are encouraged and supported in being out-of-bed.
Adding more equipment does not necessarily improve SPHM programs; being overly prescriptive and setting criteria for use of one type of equipment over another type does not eliminate the need for critical thinking when determining the best SPHM options. Due to limited storage, budgetary constraints, small rooms and other factors, limiting SPHM practices to a few well-chosen versatile lifts is the more sustainable option. Melillo et al. acknowledge that “One respondent wrote the recommended equipment for each VA MSST level may not be available in some settings. They reported this may cause confusion or frustration for staff.” A lack of unit specific SPHM equipment or difficulty in obtaining types and amounts of equipment typically leads to confusion, frustration and lack of standardized care.
Conclusions
The BMAT linked to SPHM programs is gaining recognition as a tool that can impact mobility in inpatient and other settings. BMAT linked to SPHM practices has been in use for over 13 years as a nurse-driven assessment but also as a validated and accepted tool for use by delegated UAP. BMAT is used in the United States and internationally. While confusing elements regarding BMAT observed in the Melillo et al. article and flowchart are concerning, these should not impede use of the BMAT linked to physical assessments and SPHM practices. The fact that Melillo et al. further validated the BMAT and created videos for training purposes should be beneficial. Further research around use of mobility tools and SPHM practices in AC/OP settings would be valuable and should include collaborating with SPHM equipment manufacturers on how they currently support mobility and fall prevention in these types of settings.
When considering potential complications associated with immobility and the negative effects of bedrest, monitoring mobility and implementing meaningful assessments and interventions across the continuum of care is essential. SPHM practices are critical for patient, resident and caregiver safety and injury prevention. Further evaluation of the feasibility of developing a quality measure to assess mobility outcomes and the success of mobility interventions are needed, as well as research directly linking SPHM practices to improved mobility practices.
Supplementary Information
Acknowledgements
The author reviewed the VA MSST article and flowchart and wrote this Matters Arising manuscript following the BMC Health Services Research guidelines and format for this type of response. This present article is based on inaccurate statements regarding the BMAT observed in the Melillo et al. article and in the VA MSST flowchart, a derivative tool of the BMAT. BMAT was created and developed by the author and the Banner Health SPHM team, including Merl Miller, Chris Trudgen, Amber Perez, Young An, Kathleen Werner, Lesly Kelly, Robbin Taggart, Gena Edmiston, Julie Roth-Carter, Kimberly Pepmiller, Cara Bruntz and Didi Hartling.
The author would like to acknowledge all of the nurses, nursing aids, PTs, OTs and SPHM team members who contributed to the BMAT in its evolution over 20 years, and its use as an effective assessment by RNs and a recheck tool used by CNAs, Transporters, Radiology Technicians and other ancillary staff, and their contributions in building standardized SPHM practices focused on preventing complications associated with immobility and the negative effects of bedrest, as well as safer practices for patients and their caregivers. Dee Kumpar, a creative and insightful RN, not only gave great feedback and support during creation of BMAT 1.0 but did the same during creation of BMAT 2.0. The author wants to acknowledge Julie Roth-Carter, a creative and caring Clinical Nurse Specialist who recognized the potential of the BMAT and the impact it could have on preventing patient falls and staff injuries with consistent use of SPHM equipment. She and her care team agreed to let the author complete an early pilot of the BMAT with patients on their medical telemetry unit; they gave critical feedback that led to critical modifications. Julie and her team went on to present their findings at nursing research conferences. Their initial use and support of the BMAT over an extended period of time was invaluable. Feedback from VA SPHM leaders (who were early adopters of BMAT) was instrumental in developing and creating BMAT 2.0. The author also wants to acknowledge Lynn Runyan, Director of Risk Management for Banner Health for the Western Region, who had the foresight to pilot SPHM practices at four Colorado hospitals in 2001 with a focus on preventing caregiver injuries and improving care for patients. My Administrative Assistant, Stacey Coffman went above and beyond when it came to assisting with data analysis and helping to move SPHM practices forward.
Abbreviations
- VA MSST
Veteran Administration Mobility Screening and Solutions Tool
- BMAT
Bedside Mobility Assessment Tool
- SPHM
Safe Patient Handling and Mobility
- EHR
Electronic Health Record
- NCSBN
National Council of State Boards of Nursing
- NPA
Nurse Practice Act
- UAP
Unlicensed Assistive Personnel
- HCW
Healthcare Worker(s)
- RN
Registered Nurse
- CNA
Certified Nursing Assistant
- PT
Physical Therapist
- OT
Occupational Therapist
- ICU/CCU
Intensive Care Unit/Critical Care Unit
- ED
Emergency Department
- MI
Medical Imaging
- OP
Outpatient
- AC
Ambulatory Care
Author’s contributions
T.B. is the sole author who conceptualized, developed and wrote this manuscript in response to the Melillo et al. article on the VA MSST.
Funding
Not applicable.
Availability of data and materials
Contact the author, T.B., for data or additional materials supporting use of the Bedside Mobility Assessment Tool and for pdf copies of slide decks used at conference presentations and webinars listed under References.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Starting in 2003, the author, T.B. (Banner Health Ergonomics and Injury Preventions Specialist and SPHM Coordinator) along with Banner Health and Liko/Hill-Rom colleagues, created and developed what became the Bedside Mobility Assessment Tool; led pilot projects using the BMAT to improve SPHM practices in 11 hospitals; was a member of the Banner Health validation and system-wide BMAT SPHM implementation team and falls prevention teams; built BMAT in the EMR and updated the falls risk tool in the EMR; shared findings with colleagues including through VA SPHM conferences and discussions with VA SPHM leaders; was the lead author of two articles on the BMAT validation project and initial findings; created numerous BMAT flowcharts, algorithms and other support tools; compiled feedback from BMAT 1.0 users; assisted in building BMAT in numerous EMRs; improved cause of injury coding, tracking and trending of workers’ compensation claims and injury data – specifically data related to patient handling injuries. As a clinical consultant for Hill-Rom, T.B. worked with Hill-Rom colleagues including Dee Kumpar and Cathy VanGilder on the upgraded BMAT 2.0 project; was the lead author on a 2020 article introducing BMAT 2.0 and its support tools; presented on BMAT 2.0 and its support tools during VA and other SPHM conferences and webinar; and continues to consult on implementing mobility assessments and standardized SPHM practices. T.B. worked for Banner Health from 1989 to October 2015 and then for Hill-Rom from October 2015 through December 2018, and helped to facilitate clarifying copyright and intellectual property rights for BMAT and establishing the license and sub-license allowing hospitals and healthcare organizations to obtain a no-charge license giving formal permission to use and build the BMAT in their EMRs, and with establishing the Hill-Rom license for BMAT 2.0 that addresses copyright, intellectual property and permission to use.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dickinson S, Taylor S, Anton P. Integrating a standardized mobility program and safe patient handling. Crit Care Nurs. 2018;3:240–52. [DOI] [PubMed] [Google Scholar]
- 2.Matz M. Patient handling and mobility assessments: a white paper. 2nd ed. The Facilities Guidelines Institute; 2019. [Google Scholar]
- 3.Fulmer T, Pelton L. Age-Friendly Health Systems – A guide to using the 4Ms while caring for older adults, Institute for Healthcare Improvement. 2022. [Google Scholar]
- 4.Boynton T, Kelly L, Perez A. Implementing a mobility assessment tool for nurses. Am Nurse Today. 2014;9:15–8. [Google Scholar]
- 5.Boynton T, Kelly L, Perez A, et al. Banner mobility Assessment Tool for nurses: instrument validation. Am J SPHM. 2014;4:86–92. [Google Scholar]
- 6.Boynton T, Kumpar D, VanGilder C. Bedside mobility Assessment Tool 2.0. Am Nurse J. 2020;15:18–22. [Google Scholar]
- 7.Melillo C, Rugs D, Toyinbo P, et al. Reliability and validity of the Veterans Administration Mobility Screening and Solutions Tool. BMC Health Serv Res. 2022;22:1323. 10.1186/s12913-022-08745-1.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boynton T. Assessing mobility: A review of mobility screenings and assessments. Veterans Administration Safe Patient Handling and Mobility Virtual Conference; webinar. 2021.
- 9.Boynton T, Kielich R. Why mobilizing patients is critical. Veterans Administration Safe Patient Handling and Mobility Conference: A vision to the future; podium presentation. 2020.
- 10.Boynton T. Effectively assessing and improving patient mobility -improving patient and caregiver safety: the Bedside mobility Assessment Tool 2.0. American Hospital Association webinar; 2020.
- 11.Boynton T, Kumpar D, Trudgen C. Implementing a bedside mobility assessment tool for nurses: linking SPHM and falls prevention. Veterans Administration Safe Patient Handling and Mobility Conference: Transforming care; podium presentation. 2015.
- 12.Wald H, Ramaswamy R, Perskin M et al. The case for mobility assessment in hospitalized older adults: American Geriatrics Society white paper executive summary. 2018 https://agsjournals.onlinelibrary.wiley.com/doi/10.1111/jgs.15595 [DOI] [PubMed]
- 13.National Council of State Boards of Nursing (2016). National Guidelines for Nursing Delegation. 2016;7:1.
- 14.Boynton T. Coding and applying injury claims data to implement and sustain effective safe patient handling and mobility solutions. Int J Ind Ergon. 2022. 10.1016/j.ergon.2022.103397. [Google Scholar]
- 15.Boynton T. Evaluating mobility: assessments versus screenings – competency and scope of practice. The Association of Safe Patient Handling Professionals webinar. 2023.
- 16.National Council of Juvenile and Family Court Judges, Linking Systems of Care for Children and Youth Project, Differences Between Screening and Assessment. 2021. https://www.ncjfcj.org/wp-content/uploads/2021/11/Differences-between-screening-and-assessment.pdf.
- 17.University of Maryland, Baltimore County Center for Community Collaboration. Screening versus assessment, understanding screening and assessment. 2022. https://communitycollaboration.umbc.edu/screening-versus-assessment.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Contact the author, T.B., for data or additional materials supporting use of the Bedside Mobility Assessment Tool and for pdf copies of slide decks used at conference presentations and webinars listed under References.