Abstract
Objective.
To examine telemedicine use among nursing home (NH) residents with Alzheimer’s disease and related dementias (ADRD) and the associations with NH characteristics.
Design.
Observational study.
Setting and Participants.
2020–2021 Minimum Data Set 3.0, Medicare datasets, and Nursing Home Compare data were linked. 10,810 NHs were identified.
Methods.
The outcome variable was the percentage of ADRD residents who used telemedicine in a NH in a quarter. The main independent variables were NH racial and ethnic compositions (i.e., percentages of Black and Hispanic residents) and NH rurality. A set of linear models with NH random effects were estimated. The analysis was stratified by COVID-19 pandemic stages, including the beginning of the pandemic (2nd quarter of 2020 [2020 Q2]), before and after the widespread of the COVID-19 vaccine (i.e., 2020 Q3 – 2021 Q1 & 2021 Q2 – 2021 Q4).
Results.
The proportion of ADRD residents in NHs who had telemedicine use declined from 35.0% in 2020 Q2 to 9.3% in 2021 Q4. After adjusting for other NH characteristics, NHs with a high proportion of Hispanic residents were 2.7 percentage-points more likely to use telemedicine for ADRD residents than those with a low proportion during 2021 Q2 – 2021 Q4 (P<0.001), while NHs with a high proportion of Black residents were 1.5 percentage-points less likely to use telemedicine than those with a low proportion (P<0.01). Additionally, compared with metropolitan NHs, rural NHs were 6.4 percentage-points less likely to use telemedicine in 2020 Q2 (P<0.001), but 5.9 percentage-points more likely to use telemedicine during 2021 Q2 – 2021 Q4 (P<0.001). We also detected the relationship between telemedicine use and other NH characteristics, such as NH quality, staffing level, and Medicaid-pay days.
Conclusions and Implications.
The proportion of ADRD residents in NHs who had telemedicine use decreased during the pandemic. Telemedicine could improve healthcare access for NHs with a high proportion of Hispanic residents and NHs in remote areas. Future studies should investigate how telemedicine use affects the health outcomes of NH residents with ADRD.
Keywords: Alzheimer’s Disease and Related Dementia, Nursing Home, Telemedicine, COVID-19
Introduction
Over half of nursing home (NH) residents are diagnosed with Alzheimer’s disease and related dementias (ADRD).1 NH residents with ADRD are particularly vulnerable, often with multiple comorbidities and at a high risk of psychological issues and behavioral problems.2,3 Routine medical services, such as evaluation and management, primary care, and metal health care, are important for managing their health conditions and avoiding adverse health outcomes (e.g., avoidable hospitalizations).4,5 NH residents with ADRD often rely on health professionals, such as physicians, psychiatrists, and registered nurses (RNs), Íto manage their health conditions.6–10 However, many NH residents face challenges in adequately addressing their healthcare needs, especially the need of mental health care, attributed to factors such as impaired cognitive function, mobility issue, lack of access to mental healthcare providers, and NH staff trained in mental health.11,12
The Centers for Medicare and Medicaid Services (CMS) significantly expanded telemedicine coverage for all Medicare beneficiaries at the beginning of the pandemic, lifting the location restrictions and reimbursing healthcare providers for telemedicine at the same rate as in-person services. 13 Before the pandemic, telemedicine services were only reimbursed in remote areas with restrictions.14 The expansion of telemedicine may have provided an opportunity to improve medical services in NHs by connecting to providers remotely and offering more provider options in a broader geographic area.15 Indeed, there was a quick uptake of telemedicine in various sectors of the U.S. healthcare system after the telemedicine expansion policy. For instance, previous research showed that telemedicine visits increased more than ten times in skilled nursing facilities (SNF) from 2019 to 2020.16
Despite the growing use of telemedicine use, its adoption in NHs for residents with ADRD remains unclear. It is also unknown whether disparities exist in telemedicine use across NHs, a concern compounded by the longstanding issues of disparities in NH care quality.17–19 Factors associated with these disparities may also influence telemedicine use. For instance, NHs serving higher proportions of racial and ethnic minorities (e.g., Black and Hispanic residents) often have lower staffing levels and greater financial constraints,17,19 which may hinder the adoption of telemedicine in NHs. This is particularly relevant for residents with ADRD, who often have additional hearing and vision impairments and would require assistance from NH staff to communicate with providers during telemedicine encounters.20,21 Furthermore, the availability of resources in NHs can impact their infrastructure’s readiness, such as stable internet connectivity and access to technological devices, to adopt telemedicine.22 Prior research has shown that SNFs with a higher proportion of Black residents were less likely to use telemedicine during the pandemic compared to those with a lower proportion. 16 However, no study has yet examined the racial and ethnic differences in the telemedicine utilization in NHs among ADRD residents.
The adoption of telemedicine may also vary by NH rurality. Although rural NHs may have greater needs for telemedicine due to significant provider shortages and limited healthcare resources,15,23,24 these NHs often have inadequate infrastructure (e.g., limited broadband access) and experienced greater workforce shortages during the pandemic than their urban counterparts,25 potentially impacting telemedicine adoption. The current research presents mixed findings on the rural-urban difference in telemedicine use in NHs. For instance, a study indicated that NHs in rural areas were less likely to use telemedicine during the early stage of the pandemic.26 In contrast, another study using a longer period suggested that residents in SNFs in non-metropolitan areas were more likely to use telemedicine than those in metropolitan SNFs.16
To date, the extent of telemedicine utilization among NH residents with ADRD, influenced by NH characteristics such as racial and ethnic composition and rurality, remains unclear. Therefore, this study aims to examine telemedicine use among NH residents with ADRD from 2020 to 2021, exploring how NH characteristics, especially NH racial and ethnic compositions and rurality, were associated with telemedicine use in NHs. We hypothesize that NHs with higher levels of racial and ethnic compositions and those in rural areas were less likely to use telemedicine. Additionally, there could be changes in telemedicine adoption across different pandemic phases, especially with the widespread adoption of the COVID-19 vaccine leading to reduced COVID-19-related infections and mortality in NHs.27 Thus, this study also examines the shifts in telemedicine during the later stage of the pandemic.
Methods
Data and cohort:
We linked the 2020–2021 Minimum Data Set (MDS) 3.0, Medicare claims data, and Medicare beneficiary summary (MBSF) to identify NH residents, telemedicine use, and individual characteristics. Nursing Home Compare (NHC) data,28 Payroll-Based Journal (PBJ) data,20, and rural-urban commuting area data (RUCA) for the same study period 30 were linked to obtain NH characteristics. Lastly, we used CMS NH COVID-19 infection data to account for the COVID-19 pandemic impact on NHs.31
We identified 817,821 NH residents with ADRD who are Medicare fee-for-service (FFS) beneficiaries during the pandemic (i.e., from 2020 2nd quarter to 2021 4th quarter). ADRD diagnosis was based on the 2019 MBSF chronic condition file. We then aggregated the data at the NH-quarter level. NHs with less than 20 ADRD residents (i.e., bottom quartile based on NH ADRD residents distribution) in all quarters during the study period were excluded. Our final analytic cohort included 10,810 NHs in the U.S. (around 4,000 NHs were excluded).
Variables
The outcome variable was the proportion of NH residents with ADRD who had at least one telemedicine visit in a NH in a quarter. Telemedicine use was identified based on HCPCS codes and modifiers in the carrier file.32
The main independent variables were quarters, NH racial and ethnic compositions, and NH rurality. We included quarters as a continuous variable to represent the trend of telemedicine use during each study period. NH racial and ethnic compositions were calculated as the percentage of Black residents and the percentage of Hispanic residents in a NH in a year, based on the MDS data. According to the distribution, we categorized NHs as high (above 14.1%, 75th percentile) versus low proportion of Black residents and high (above 17.7%, 90th percentile) versus low proportion of Hispanic residents. We used the 90th percentile to dichotomize the percentage of Hispanic residents due to the low prevalence in general (i.e., the average proportion of Hispanic residents is 4.5%). NH rurality includes four levels: metropolitan, micropolitan, small town, and rural, which were defined based on the NH zip codes using RUCA data.
We also included a set of NH characteristics that may affect the adoption of telemedicine, including the number of beds, ownership, and occupancy level at the study baseline, and quality rating (1–2 as low, 3 as medium, and 4–5 as high quality) in each quarter from NHC. Based on PBJ data, we calculated quarterly average NH staff (i.e., including registered nurse[RN] and nursing home aids[NA]) hours per resident per day. We constructed the quarterly average percentage of Medicaid-paid and Medicare-paid NH days for each NH using MDS data, MBSF, and Medicare skilled nursing facility claims. We additionally included the quarterly average NH COVID-19 infection rate from CMS NH COVID-19 infection data. We classified NHs into geographical regions, including northeast, southeast, midwest, southwest, and west. We categorized the continuous NH characteristics variables (e.g., quarterly average NH staff hours) into three categories based on tertiles to allow for the potential non-linear relationships between these variables and the outcome.
Furthermore, to account for individual care needs among ADRD residents, we included residents’ age, sex, the number of chronic conditions, physical functioning status (activity daily living [ADL] score),25, and cognitive impairment status (cognitive function scale[CFS]) prior to each study quarter, based on MBSF and MDS data.35 Individual characteristics were then aggregated at the NH level.
Statistical analysis
The unit of our analysis is NH-quarters. We first compared NH characteristics by different levels of telemedicine use at the beginning of the pandemic (i.e., 2nd quarter of 2020 [2020 Q2]), categorized into four quartiles. We then used linear regression models with NH random effects to examine the relationship between NH characteristics and the proportion of ADRD residents with telemedicine use. To understand how the relationship between NH characteristics and telemedicine use varied by stages of the pandemic, we stratified the analyses by three time periods: the beginning of the pandemic (2020 Q2), 36 the period before the widespread availability of COVID-19 vaccines (2020 Q3 to 2021 Q1), and the period after the widespread of COVID-19 vaccines (2021 Q2 to 2021 Q4).37 We separated 2020 Q2 due to the uncertainties at the beginning of the public crisis. To be consistent with the literature, we used 2021 Q1 as the dividing point to separate the periods before and after the widespread availability of vaccines.33,34
The study has been approved by the Institutional Review Board of the investigator’s institution. All statistical analyses were performed in SAS 9.4 (SAS Institute Inc, Cary, NC) and Stata 16.0 (StataCorp LLC, College Station, TX).
Results
Figure 1 illustrates the overall quarterly telemedicine use in NHs during the study period, by NH racial and ethnic compositions and rurality. As shown in Figure 1, there was a decreasing trend in the proportion of NH ADRD residents with telemedicine use over time, ranging from 35.0% at the beginning of the pandemic (2020 Q2) to 9.3% in 2021 Q4. Figure 1 also suggests variations in telemedicine use by NH racial and ethnic compositions and rurality. For instance, during the study period, the prevalence of telemedicine use varied from 1.6 – 5.1 percentage points lower in NHs with a high proportion of Black residents compared to those with a low proportion of Black residents (Figure 1b). However, NHs with high percentages of Hispanic residents appeared to have similar telemedicine use as those with low percentages of Hispanics (Figure 1c). Additionally, NHs in rural areas were less likely to use telemedicine compared to NHs in metropolitan or micropolitan areas at the beginning of the pandemic (e.g., 4.3 percentage-points less compared to NHs in metropolitan areas) but had a smaller decreasing trend during the later stages compared to NHs in non-rural areas.
Figure 1.
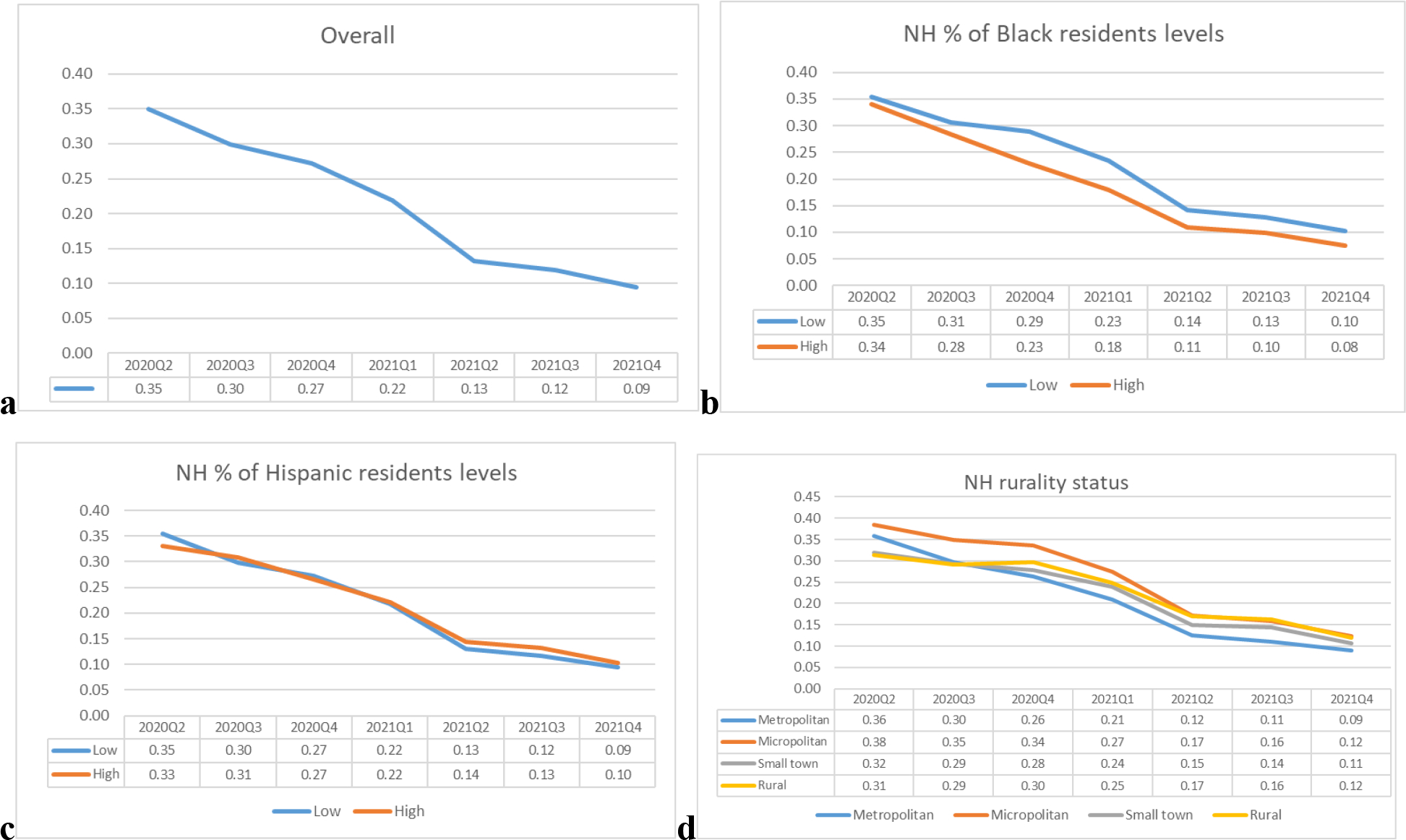
The trends of average percentage of telemedicine use in NHs: overall and by racial and ethnic compositions and rural status.
Table 1 presents the summary statistics of various NH characteristics by quartiles of telemedicine use among ADRD residents at the beginning of the pandemic (i.e.,2020Q2). For example, 61.0% of NHs in the lowest quartile of telemedicine use had a high-quality rating (i.e., 4 – 5 quality stars), compared to 55.3% of NHs in the highest quartile of telemedicine use (p <0.001). Also, NHs with a high prevalence of telemedicine use tended to have a high proportion of Medicaid residents compared to those with a low prevalence of telemedicine use (i.e., 74.5% vs. 78.2% of NHs in the lowest quartile vs. highest quartile of telemedicine use had a high proportion of Medicaid residents, p<0.001). In addition, NHs in the highest quartile of telemedicine use were more likely to be in the Midwest region (33.7%) compared to other regions (P<0.001).
Table 1.
Summary statistics of NH characteristics by telemedicine use level in 2nd quarter of 2020.
| Telemedicine use < 10% | Telemedicine use 10% – 27% | Telemedicine use 27% – 56% | Telemedicine use >=56% | |
|---|---|---|---|---|
| NH percent of Hispanic residents | ||||
| Low (under 90 percentile) | 2,516 (92.1) | 2,319 (90.8) | 2,328 (87.5) | 2,570 (89.8) |
| High (on and over 90 percentile) | 215 (7.9) | 236 (9.2) | 333 (12.5) | 293 (10.2) |
| NH percent of Black residents | ||||
| Low (under 75 percentile) | 2,034 (74.5) | 1,986 (77.7) | 1,985 (74.6) | 2,125 (74.2) |
| High (on and over 75 percentile) | 697 (25.5) | 569 (22.3) | 676 (25.4) | 738 (25.8) |
| Rural-urban status | ||||
| Metropolitan | 1,785 (65.4) | 1,905 (74.6) | 1,966 (73.9) | 2,008 (70.1) |
| Micropolitan | 385 (14.1) | 342 (13.4) | 362 (13.6) | 480 (16.8) |
| Small town | 383 (14) | 199 (7.8) | 234 (8.8) | 256 (8.9) |
| Rural | 178 (6.5) | 109 (4.3) | 99 (3.7) | 119 (4.2) |
| Quality rating | ||||
| Low (1–2 stars) | 521 (19.1) | 459 (18) | 514 (19.3) | 655 (22.9) |
| Medium (3 stars) | 544 (19.9) | 494 (19.3) | 585 (22) | 626 (21.9) |
| High (4– 5 stars) | 1,666 (61) | 1,602 (62.7) | 1,562 (58.7) | 1,582 (55.3) |
| Averaged registered nurse hours per resident per day | ||||
| Low (< 0.47) | 991 (36.3) | 863 (33.8) | 1,084 (40.7) | 1,224 (42.8) |
| Medium [0.47–0.72) | 963 (35.3) | 876 (34.3) | 870 (32.7) | 920 (32.1) |
| High (>= 0.72) | 777 (28.5) | 816 (31.9) | 707 (26.6) | 719 (25.1) |
| Averaged nurse aids hours per resident per day | ||||
| Low (<2.0) | 813 (29.8) | 677 (26.5) | 867 (32.6) | 1,010 (35.3) |
| Medium [2.0 – 2.45) | 949 (34.7) | 987 (38.6) | 1,002 (37.7) | 1,049 (36.6) |
| High (>=2.45) | 969 (35.5) | 891 (34.9) | 792 (29.8) | 804 (28.1) |
| Averaged percent of NH days paid by Medicaid | ||||
| Low (<26.72%) | 282 (10.3) | 315 (12.3) | 254 (9.5) | 211 (7.4) |
| Medium [26.72 – 38.96%) | 415 (15.2) | 429 (16.8) | 432 (16.2) | 413 (14.4) |
| High (>=38.96%) | 2,034 (74.5) | 1,811 (70.9) | 1,975 (74.2) | 2,239 (78.2) |
| Averaged percent of NH days paid by Medicare | ||||
| Low (<10.84%) | 1,000 (36.6) | 830 (32.5) | 813 (30.6) | 1,021 (35.7) |
| Medium [10.84 – 19.25%) | 965 (35.3) | 850 (33.3) | 944 (35.5) | 1,045 (36.5) |
| High (>=19.25%) | 766 (28) | 875 (34.2) | 904 (34) | 797 (27.8) |
| NH region | ||||
| Midwest | 608 (22.4) | 630 (24.8) | 735 (27.6) | 963 (33.7) |
| Northeast | 650 (23.7) | 674 (26.5) | 560 (21.1) | 400 (14.0) |
| Southeast | 1012 (37.0) | 643 (25.3) | 664 (25.0) | 707 (24.7) |
| Southwest | 178 (6.5) | 242 (9.3) | 355 (13.2) | 474 (16.5) |
| West | 283 (10.4) | 366 (14.2) | 348 (13.1) | 319 (11.2) |
| NH average number of COVID-19 cases per 1000 residents (Mean [SD]) | 16.39 (38.6) | 19.89 (41.77) | 23.64 (47.00) | 21.15 (46.44) |
| Individual characteristics among ADRD residents aggregated at NH level | ||||
| NH percent of females (Mean [SD]) | 0.67 (0.14) | 0.68 (0.12) | 0.67 (0.12) | 0.66 (0.13) |
| NH percent of moderate cognitive impairment (Mean [SD]) | 0.21 (0.09) | 0.21 (0.09) | 0.22 (0.1) | 0.22 (0.1) |
| NH percent of severe cognitive impairment (Mean [SD]) | 0.58 (0.13) | 0.57 (0.14) | 0.56 (0.14) | 0.56 (0.14) |
| NH average ADL score (Mean [SD]) | 16.79 (2.31) | 16.92 (2.27) | 17.03 (2.33) | 16.68 (2.52) |
| NH average number of chronic conditions per residents (Mean [SD]) | 6.84 (1.1) | 6.97 (1.07) | 7.02 (1.04) | 7 (1.1) |
| NH averaged age (Mean [SD]) | 82.34 (4.61) | 82.48 (4.59) | 81.68 (4.62) | 81.05 (5.01) |
Note:
Chi-square test was used to test differences between groups for categorical variables. The test results were statistically significant for all variables (P<0.001).
Table 2 presents the findings from the regression models, stratified by three time periods(i.e., Model 1–3 [M1–3]). NH telemedicine use was associated with racial and ethnic compositions in NHs. NHs with a high proportion of Hispanic residents had a 2.7 percentage-points higher prevalence of telemedicine use among ADRD residents during the later stage of the pandemic (i.e., 2021 Q2 – 2021 Q4) compared to those with a low proportion (P<0.001). In comparison, NHs with a high proportion of Black residents were less likely to use telemedicine than those with a low proportion after the beginning of the pandemic. For example, between 2021 Q2 and 2021 Q4 (M3), the prevalence of telemedicine use was 1.5 percentage-points lower in NHs with a high proportion of Black residents than those with a low proportion (P<0.001).
Table 2.
Results of linear regression with NH random effect, stratified by pandemic stages.
| Model 1: 2020 Q2 | Model 2: 2020 Q3 - 2021Q1 | Model3: 2021 Q2 - 2021 Q4 | |
|---|---|---|---|
| Quarter | −0.0368*** | −0.0201*** | |
| NH percent of Blacks | |||
| Low (under 75 percentile) | Ref | Ref | Ref |
| High (on and over 75 percentile) | −0.0047 | −0.0227*** | −0.0153*** |
| NH percent of Hispanic | |||
| Low (under 90 percentile) | Ref | Ref | Ref |
| High (on and over 90 percentile) | −0.0070 | 0.0090 | 0.0271*** |
| Rural-urban status | |||
| Metropolitan | Ref | Ref | Ref |
| Micropolitan | 0.0066 | 0.0457*** | 0.0493*** |
| Small town | −0.0605*** | −0.0034 | 0.0375*** |
| Rural | −0.0635*** | 0.0089 | 0.0594*** |
| Quality rating | |||
| Low (1–2 stars) | Ref | Ref | Ref |
| Medium (3 stars) | −0.0006 | −0.0040 | −0.0033 |
| High (4– 5 stars) | −0.0145 | −0.0156** | −0.0124*** |
| Averaged registered nurse hours per resident per day | |||
| Low (< 0.47) | Ref | Ref | Ref |
| Medium [0.47– 0.72) | −0.0033 | −0.0048 | 0.0012 |
| High (>= 0.72) | 0.0063 | −0.0109* | 0.0010 |
| Averaged nurse aids hours per resident per day | |||
| Low (<2.0) | Ref | Ref | Ref |
| Medium [2.0 – 2.45) | −0.0050 | −0.0011 | −0.0015 |
| High (>=2.45) | −0.0164* | −0.0007 | −0.0012 |
| Averaged percent of NH days paid by Medicaid | |||
| Low (<26.72) | Ref | Ref | Ref |
| Medium [26.72 – 38.96) | 0.0174 | 0.0035 | 0.0057 |
| High (>=38.96%) | 0.0144 | 0.0148*** | 0.0172 |
| Averaged percent of NH days paid by Medicare | |||
| Low (<10.84) | Ref | Ref | Ref |
| Medium [10.84 – 19.25) | −0.0147* | 0.0062 | 0.0123** |
| High (>=19.25) | −0.0317*** | −0.0032 | 0.0105** |
| NH region | |||
| Midwest | Ref | Ref | Ref |
| Northeast | −0.1172*** | −0.0700*** | 0.0159*** |
| Southeast | −0.1035*** | −0.0651*** | −0.0265*** |
| Southwest | 0.0296** | 0.0632*** | 0.0102 |
| West | −0.0564*** | 0.0181* | 0.0600*** |
| NH average number of COVID-19 cases per 1000 residents | 0.0004*** | 0.0010*** | 0.0010*** |
| Individual characteristics among ADRD residents aggregated at NH level | |||
| NH percent of females | 0.0779** | 0.0212 | −0.0230** |
| NH percent of moderate cognitive impairment | 0.0263 | 0.0346* | −0.0170 |
| NH percent of severe cognitive impairment | 0.0020 | 0.0180 | −0.0260** |
| NH average ADL score | 0.0014 | 0.0015* | 0.0006 |
| NH average number of chronic conditions per residents | 0.0178*** | 0.0059*** | 0.0027* |
| NH averaged age | −0.0074*** | −0.0045*** | −0.0023*** |
Note:
The estimates of variables are shown in the table. The numbers * 100 can be interpreted as percentage-points.
P<0.05
P<0.01
p<0.001
The relationship between NH rurality status and telemedicine use among ADRD residents varied across pandemic periods. In 2020 Q2, rural NHs were 6.4 percentage-points less likely to use telemedicine for ADRD residents than Metropolitan NHs (P<0.001, M1). However, between 2021 Q2 and 2021 Q4, rural NHs were 5.9 percentage-points more likely to use telemedicine than metropolitan NHs (P<0.001, M3).
Other NH characteristics were also associated with NH telemedicine use. For instance, NHs with a high-quality rating (i.e., 4 – 5 stars) were 1.6 and 1.2 percentage-points less likely to use telemedicine for ADRD residents compared to low-quality NHs (i.e., 1–2 stars) during 2020 Q3 – 2021 Q1 (P<0.01) and 2021 Q2–2021 Q4, respectively (P<0.001). Additionally, NHs with a high level of RN staffing (i.e., >=0.72 RN hours per resident per day) were 1.1 percentage-points less likely to use telemedicine than NHs with a low RN staffing level (<0.47 RN hours per resident per day) during 2020 Q3–2021 Q1 (P <0.05), but not during 2021 Q2 – 2021 Q4. Furthermore, NHs with a high percentage of Medicaid-paid days were 1.5 percentage-points more likely to use telemedicine than those with a low percentage during 2020 Q3– 2021 Q1 (P<0.01), but not during 2021 Q2 – 2021 Q4. NHs with a high percentage of Medicare-paid days were 3.2 percentage-points less likely to use thelemedicine at the beginning of the pandemic (P<0.01) but 1.1 percentage-points more likely to use telemedicine during the later stage of the pandemic (P<0.01), compared to those with a low percentage.
Discussion
This study examined the associations between NH characteristics and telemedicine use among residents with ADRD and their variations across pandemic stages. We observed a decreasing trend in telemedicine use during the pandemic. We found that telemedicine use varied by NH racial and ethnic compositions, rurality, and other NH characteristics, such as staffing level, financial status, and quality level. These variations shifted across different pandemic stages of the pandemic.
Consistent with a prior study,16 we observed that NHs with a high proportion of Black residents were less likely to use telemedicine after the beginning of the pandemic compared to those with a low proportion of Black residents. As we have accounted for other NH characteristics, such as staffing level and percentage of Medicaid-paid NH days, it is likely that there are some other uncaptured differences, such as infrastructure, health literacy of NH staff, or cultural background, contributing to the different level of telemedicine use between these NHs and NHs with a low percentage of Black residents.
On the other hand, we found that residents with ADRD in NHs with a higher proportion of Hispanic residents were more likely to use telemedicine during the later stage of the pandemic. It is possible that these NHs have limited availability of healthcare services and lower quality of care.19,40,41Telemedicine, which may offer a unique opportunity to improve their access to care and facilitate access to providers who can better accommodate residents’ needs with appropriate services.
We also detected significant relationships between NH rurality and telemedicine use. However, the relationships varied during the pandemic. At the beginning of the pandemic, NHs in rural and small-town areas were less likely to use telemedicine compared to NHs in metropolitan areas. However, during the later stage, those NHs were more likely to use telemedicine. The findings suggest that, although telemedicine could offer greater benefits to NHs in remote areas, these NHs might have a slower adoption of telemedicine initially due to constraints such as insufficient technology devices or inadequate broadband capacity at the beginning of the pandemic. Delayed access to telemedicine adoption, especially during a public health crisis, may lead to worse health outcomes for the vulnerable residents in NHs.
In addition, we found relationships between other NH characteristics and telemedicine utilization. For instance, NHs with high-quality ratings were less likely to use telemedicine during the later stages of the pandemic. High-quality NHs tend to have more healthcare resources and probably better access to care,42 reducing the need for telemedicine to improve care access. On the other hand, NHs with a low level of RN staffing were more likely to use telemedicine during the pandemic’s early stages than those with high RN levels. The pandemic may have exacerbated the staffing shortages in these NHs, expecially before the widespread availability of COVID-19 vaccines, prompting them ot use telemedicine for healthcare services.
Similarly, NHs with a high percentage of Medicaid-paid days were more likely to use telemedicine after the initial outbreak of the pandemic but before the vaccine was widely available. NHs with a high percentage of Medicaid-days tend to have financial vulnerability, poor resources, and they have been disproportionally affected by the pandemic, especially before the widespread availability of the COVID-19 vaccine, which could lead to greater challenges in accessing medical care services and providers.43–45 In contrast, NHs with a higher percentage of Medicare-paid were initially less likely to use telemedicine but became more likely to use telemedicine later on. These NHs are likely to be equipped with more medical providers as Medicare-paid residents generally require post-acute services.46 Thus, they may not have needed remote care access at the beginning of the pandemic, but later used telemedicine to facilitate residents’ access to medical services, considering the high need for medical services for post-acute residents.
Lastly, we observed a decreasing trend in telemedicine use during the pandemic. NH residents may have chosen to return to in-person care after the wide availability of the COVID-19 vaccines and the significant decrease in COVID-19-related mortality and hospitalizations.47 We also found regional differences in NH telemedicine use. This result is consistent with a previous study.48 One potential reason is the differences in telemedicine infrastructure, system support, and cultural backgrounds across various regions.
Our study has several limitations. First, we only included Medicare FFS NH residents with ADRD in the study. Thus, the findings may not be generalized to Medicare-managed care enrollees or those without ADRD. Secondly, the study period is between 2020 and 2021. There may be further changes in telemedicine use in the later phases. Thirdly, the ADRD population may be underestimated using claims data.49 However, considering the large number of ADRD residents we included in the study, our findings could provide meaningful insights about telemedicine use among ADRD residents. Lastly, this study focused on the variation of telemedicine utilization across NHs with different characteristics, following the expansion of the telemedicine policies. Future research is needed to determine whether telemedicine was used as a replacement for in-person visits or if it increased overall access to healthcare services.
Conclusion
NH racial and ethnic compositions were associated with telemedicine use during the pandemic. NHs with a higher proportion of Hispanic residents were more likely to use telemedicine during the later stage of the pandemic, but NHs with a higher proportion of Black residents were less likely to use telemedicine during the pandemic. NHs in remote areas could potentially improve their access to care through the use of telemedicine, but those NHs may have delayed the adoption of telemedicine at the beginning of the pandemic. Other NH characteristics, such as quality rating, staffing, and financial status were also associated with telemedicine utilization among residents with ADRD. Future studies may be warranted to explore telemedicine use in NHs and overall access to care using more up-to-date data and to examine the impact of telemedicine on the health outcomes of NH residents with ADRD.
Footnotes
Conflict of interest:
There are no known conflicts of interest associated with this publication for all authors who were included in the manuscript.
References
- 1.Wang S, Temkin-Greener H, Conwell Y, Cai S. Policy to reduce antipsychotic use and hospitalization of nursing home residents with dementia. J Am Med Dir Assoc. 2020;21(11):1617–1622.e3. doi: 10.1016/j.jamda.2020.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lyketsos CG, Carrillo MC, Ryan JM, et al. Neuropsychiatric symptoms in Alzheimer’s disease. Alzheimers Dement J Alzheimers Assoc. 2011;7(5):532–539. doi: 10.1016/j.jalz.2011.05.2410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Santiago JA, Potashkin JA. The Impact of Disease Comorbidities in Alzheimer’s Disease. Front Aging Neurosci. 2021;13:631770. doi: 10.3389/fnagi.2021.631770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Temkin-Greener H, Cen X, Hasselberg MJ, Li Y. Preventable Hospitalizations Among Nursing Home Residents With Dementia and Behavioral Health Disorders. J Am Med Dir Assoc. 2019;20(10):1280–1286.e1. doi: 10.1016/j.jamda.2019.03.006 [DOI] [PubMed] [Google Scholar]
- 5.LaMantia MA, Stump TE, Messina FC, Miller DK, Callahan CM. Emergency Department Use Among Older Adults With Dementia. Alzheimer Dis Assoc Disord. 2016;30(1):35–40. doi: 10.1097/WAD.0000000000000118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yan D, Wang S, Temkin-Greener H, Cai S. Quality of Nursing Homes and Admission of Residents With Alzheimer’s Disease and Related Dementias: The Potential Influence of Market Factors and State Policies. J Am Med Dir Assoc. 2020;21(11):1671–1676.e1. doi: 10.1016/j.jamda.2020.04.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bartels SJ, Moak GS, Dums AR. Mental Health Services in Nursing Homes: Models of Mental Health Services in Nursing Homes: A Review of the Literature. Psychiatr Serv. 2002;53(11):1390–1396. doi: 10.1176/appi.ps.53.11.1390 [DOI] [PubMed] [Google Scholar]
- 8.Katz PR, Karuza J, Intrator O, et al. Medical Staff Organization in Nursing Homes: Scale Development and Validation. J Am Med Dir Assoc. 2009;10(7):498–504. doi: 10.1016/j.jamda.2009.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams ME. The physician’s role in nursing home care: an overview. Geriatrics. 1990;45(1):47–49. [PubMed] [Google Scholar]
- 10.Barker RO, Craig D, Spiers G, Kunonga P, Hanratty B. Who Should Deliver Primary Care in Long-term Care Facilities to Optimize Resident Outcomes? A Systematic Review. J Am Med Dir Assoc. 2018;19(12):1069–1079. doi: 10.1016/j.jamda.2018.07.006 [DOI] [PubMed] [Google Scholar]
- 11.Orth J, Li Y, Simning A, Temkin-Greener H. Providing Behavioral Health Services in Nursing Homes is Difficult: Findings from a National Survey. J Am Geriatr Soc. 2019;67(8):1713–1717. doi: 10.1111/jgs.16017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kalánková D, Stolt M, Scott PA, Papastavrou E, Suhonen R. Unmet care needs of older people: A scoping review. Nurs Ethics. 2021;28(2):149–178. doi: 10.1177/0969733020948112 [DOI] [PubMed] [Google Scholar]
- 13.MEDICARE TELEMEDICINE HEALTH CARE PROVIDER FACT SHEET | CMS. Accessed October 14, 2020. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet [Google Scholar]
- 14.Shaver J. The State of Telehealth Before and After the COVID-19 Pandemic. Prim Care. 2022;49(4):517–530. doi: 10.1016/j.pop.2022.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barnett ML, Huskamp HA. Telemedicine for Mental Health in the United States: Making Progress, Still a Long Way to Go. Psychiatr Serv Wash DC. 2020;71(2):197–198. doi: 10.1176/appi.ps.201900555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ulyte A, Mehrotra A, Wilcock AD, SteelFisher GK, Grabowski DC, Barnett ML. Telemedicine Visits in US Skilled Nursing Facilities. JAMA Netw Open. 2023;6(8):e2329895. doi: 10.1001/jamanetworkopen.2023.29895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Campbell LJ, Cai X, Gao S, Li Y. Racial/Ethnic Disparities in Nursing Home Quality of Life Deficiencies, 2001 to 2011. Gerontol Geriatr Med. 2016;2:2333721416653561. doi: 10.1177/2333721416653561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bowblis JR, Ng W, Akosionu O, Shippee TP. Decomposing Racial and Ethnic Disparities in Nursing Home Quality of Life. J Appl Gerontol. 2021;40(9):1051–1061. doi: 10.1177/0733464820946659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fennell ML, Feng Z, Clark MA, Mor V. Elderly Hispanics More Likely To Reside In Poor-Quality Nursing Homes. Health Aff Proj Hope. 2010;29(1). doi: 10.1377/hlthaff.2009.0003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ford JH, Jolles SA, Heller D, Langenstroer M, Crnich C. There and back again: the shape of telemedicine in U.S. nursing homes following COVID-19. BMC Geriatr. 2022;22(1):337. doi: 10.1186/s12877-022-03046-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Angelopoulou E, Papachristou N, Bougea A, et al. How Telemedicine Can Improve the Quality of Care for Patients with Alzheimer’s Disease and Related Dementias? A Narrative Review. Medicina (Mex). 2022;58(12):1705. doi: 10.3390/medicina58121705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lin CCC, Dievler A, Robbins C, Sripipatana A, Quinn M, Nair S. Telehealth In Health Centers: Key Adoption Factors, Barriers, And Opportunities. Health Aff (Millwood). 2018;37(12):1967–1974. doi: 10.1377/hlthaff.2018.05125 [DOI] [PubMed] [Google Scholar]
- 23.Rural Long-Term Care Facilities Overview - Rural Health Information Hub. Accessed April 14, 2022. https://www.ruralhealthinfo.org/topics/long-term-care [Google Scholar]
- 24.Rabinowitz T, Murphy KM, Amour JL, Ricci MA, Caputo MP, Newhouse PA. Benefits of a Telepsychiatry Consultation Service for Rural Nursing Home Residents. Telemed E-Health. 2010;16(1):34–40. doi: 10.1089/tmj.2009.0088 [DOI] [PubMed] [Google Scholar]
- 25.Yang BK, Carter MW, Nelson HW. Trends in COVID-19 cases, deaths, and staffing shortages in US nursing homes by rural and urban status. Geriatr Nurs N Y N. 2021;42(6):1356–1361. doi: 10.1016/j.gerinurse.2021.08.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alexander GL, Powell KR, Deroche CB. An evaluation of telehealth expansion in U.S. nursing homes. J Am Med Inform Assoc. 2021;28(2):342–348. doi: 10.1093/jamia/ocaa253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wouters F, van Loon AM, Rutten JJS, Smalbrugge M, Hertogh CMPM, Joling KJ. Risk of Death in Nursing Home Residents After COVID-19 Vaccination. J Am Med Dir Assoc. 2022;23(10):1750–1753.e2. doi: 10.1016/j.jamda.2022.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Find Healthcare Providers: Compare Care Near You | Medicare. Accessed December 2, 2020. https://www.medicare.gov/care-compare/?providerType=NursingHome&redirect=true [Google Scholar]
- 29.Payroll Based Journal Methodology - Centers for Medicare & Medicaid Services Data. Accessed October 19, 2022. https://data.cms.gov/resources/payroll-based-journal-methodology [Google Scholar]
- 30.USDA ERS - Documentation. Accessed October 21, 2022. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/documentation/
- 31.Centers for Medicare & Medicaid Services Data. Accessed October 4, 2023. https://data.cms.gov/covid-19/covid-19-nursing-home-data
- 32.List of Telehealth Services | CMS. Accessed December 2, 2020. https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes [Google Scholar]
- 33.Telemedicine CPT & HCPCS Level II Codes & Modifiers | AASM. American Academy of Sleep Medicine – Association for Sleep Clinicians and Researchers. Accessed August 14, 2022. https://aasm.org/clinical-resources/coding-reimbursement/telemedicine-codes/ [Google Scholar]
- 34.Carpenter GI, Hastie CL, Morris JN, Fries BE, Ankri J. Measuring change in activities of daily living in nursing home residents with moderate to severe cognitive impairment. BMC Geriatr. 2006;6:7. doi: 10.1186/1471-2318-6-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.MDS 3.0 Quality Measures User’s Manual - v12.1, Effective October 1, 2019. Published online 2019:110. [Google Scholar]
- 36.A Timeline of COVID-19 Vaccine Developments in 2021. AJMC. Published June 3, 2021. Accessed October 4, 2023. https://www.ajmc.com/view/a-timeline-of-covid-19-vaccine-developments-in-2021 [Google Scholar]
- 37.Singh J, Albertson A, Sillerud B. Telemedicine during COVID-19 Crisis and in Post-Pandemic/Post-Vaccine World—Historical Overview, Current Utilization, and Innovative Practices to Increase Utilization. Healthcare. 2022;10(6):1041. doi: 10.3390/healthcare10061041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Geller AI, Budnitz DS, Dubendris H, et al. Surveillance of COVID-19 Vaccination in Nursing Homes, United States, December 2020–July 2021. Public Health Rep. 2022;137(2):239–243. doi: 10.1177/00333549211066168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Diesel J. COVID-19 Vaccination Coverage Among Adults — United States, December 14, 2020–May 22, 2021. MMWR Morb Mortal Wkly Rep. 2021;70. doi: 10.15585/mmwr.mm7025e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rivera-Hernandez M, Kumar A, Epstein-Lubow G, Thomas KS. Disparities in Nursing Home Use and Quality Among African American, Hispanic, and White Medicare Residents With Alzheimer’s Disease and Related Dementias. J Aging Health. 2019;31(7):1259. doi: 10.1177/0898264318767778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rivera-Hernandez M, Fabius C, Fashaw S, et al. Quality of Post-acute care in Skilled Nursing Facilities That Disproportionally Serve Hispanics With Dementia. J Am Med Dir Assoc. 2020;21(11):1705–1711.e3. doi: 10.1016/j.jamda.2020.06.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Boccuti C, Casillas G, Published TN. Reading the Stars: Nursing Home Quality Star Ratings, Nationally and by State - Issue Brief - 8726. KFF. Published May 14, 2015. Accessed May 27, 2024. https://www.kff.org/report-section/reading-the-stars-nursing-home-quality-star-ratings-nationally-and-by-state-issue-brief/ [Google Scholar]
- 43.Grabowski DC, Angelelli JJ, Mor V. Medicaid Payment And Risk-Adjusted Nursing Home Quality Measures. Health Aff (Millwood). 2004;23(5):243–252. doi: 10.1377/hlthaff.23.5.243 [DOI] [PubMed] [Google Scholar]
- 44.Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to Tiers: Socioeconomic and Racial Disparities in the Quality of Nursing Home Care. Milbank Q. 2004;82(2):227–256. doi: 10.1111/j.0887-378X.2004.00309.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li Y, Cai X, Mao Y, Cheng Z, Temkin-Greener H. Trends in racial and ethnic disparities in coronavirus disease 2019 (COVID-19) outcomes among nursing home residents. Infect Control Hosp Epidemiol. 2022;43(8):997–1003. doi: 10.1017/ice.2021.246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lepore M, Leland NE. Nursing Homes That Increased The Proportion Of Medicare Days Achieved Gains In Quality. Health Aff Proj Hope. 2015;34(12):2121–2128. doi: 10.1377/hlthaff.2015.0303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Watson OJ, Barnsley G, Toor J, Hogan AB, Winskill P, Ghani AC. Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. Lancet Infect Dis. 2022;22(9):1293–1302. doi: 10.1016/S1473-3099(22)00320-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Park JH, Lee MJ, Tsai MH, Shih HJ, Chang J. Rural, Regional, Racial Disparities in Telemedicine Use During the COVID-19 Pandemic Among US Adults: 2021 National Health Interview Survey (NHIS). Patient Prefer Adherence. 2023;17:3477–3487. doi: 10.2147/PPA.S439437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yuan J, Lu K. Is the prevalence of alzheimer’s disease underestimated? Comparisons and contrasts of different approaches in estimating alzheimer’s disease. Value Health. 2015;18(3):A17. doi: 10.1016/j.jval.2015.03.105 [DOI] [Google Scholar]


