Abstract
Elevated levels of Neuroticism/Negative Emotionality (N/NE) and, less consistently, lower levels of Extraversion/Positive Emotionality (E/PE) confer risk for pathological depression and anxiety. To date, most prospective-longitudinal research has narrowly focused on traditional diagnostic categories, creating uncertainty about the precise nature of these prospective associations. Adopting an explicitly hierarchical-dimensional approach, we examined the association between baseline variation in personality and longitudinal changes in broad and narrow internalizing-symptom dimensions in 234 emerging adults followed for 2.5 years, during the transition from older adolescence to early adulthood. N/NE was uniquely associated with increases in broadband internalizing—the core cognitive and affective symptoms that cut across the emotional disorders—and unrelated to the narrower dimensions of positive affect and anxious arousal that differentiate specific internalizing presentations. Variation in E/PE and several other Big Five traits was cross-sectionally, but not prospectively, related to longitudinal changes in specific internalizing symptoms. Exploratory personality-facet-level analyses provided preliminary evidence of more granular associations between personality and longitudinal changes in internalizing symptoms. These observations enhance the precision of models linking personality to internalizing illness; highlight the centrality of N/NE to increases in transdiagnostic internalizing symptoms during a key developmental chapter; and set the stage for developing more effective prevention and treatment strategies.
Keywords: anxiety, Big Five, depression, emerging adulthood, emotional disorders, Hierarchical Taxonomy of Psychopathology (HiTOP), internalizing illness, personality and temperament
Introduction
Anxiety, depression, and other internalizing (‘emotional’) disorders are the most common family of psychiatric illnesses (Kessler et al., 2012). They consistently rank among the top causes of global disability, particularly among young people, and exact a tremendous social and economic toll (Dieleman et al., 2020; Olfson et al., 2019; Vos et al., 2020). Existing treatments are far from consistently curative, underscoring the urgency of developing a better understanding of the factors that promote the development, maintenance, and recurrence of these often-debilitating illnesses (Craske et al., 2017; Cuijpers et al., 2020; Singewald et al., 2023).
N/NE, E/PE, and Depression
Trait-like variation in temperament and personality is central to most etiological models of internalizing psychopathology (Clark, 2005; Fanous et al., 2002; Klein et al., 2011; Ormel et al., 2013; Shackman et al., 2016). Two major axes of personality—Neuroticism/Negative Emotionality (N/NE) and Extraversion/Positive Emotionality (E/PE)—have attracted the most theoretical attention and show the most robust empirical links in cross-sectional and longitudinal studies with internalizing symptoms (Clark, 2005; Kotov et al., 2010; Naragon-Gainey et al., 2018). Individuals with high levels of N/NE are predisposed to negative emotions, tend to perceive life as a series of punishments or threats (i.e., pessimistic), and are prone to avoidance (Shackman et al., 2016). In contrast, those with high levels of E/PE are susceptible to positive emotions; tend to experience the world as a series of opportunities for reward, particularly social reward (i.e., optimistic); and are prone to vigorous approach and engagement with potential rewards (Caspi, Roberts & Shiner; 2005).
N/NE.
Longitudinal research demonstrates that high-N/NE adolescents and adults are more likely to experience future depressive symptoms and diagnoses (e.g., Hur, Stockbridge et al., 2019). During early adulthood and beyond, N/NE predicts both the first onset and recurrence of MDD, suggesting that it is a precursor—and not simply a scar or correlate—of depressive episodes (Hayden & Klein, 2001; Kendler et al., 1993; Klein et al., 2011; Spinhoven et al., 2011). A large-scale meta-analysis confirmed that the longitudinal association between N/NE and with depression is consistent and substantial (d = 0.50–0.74), endures across the lifespan, and remains significant after adjusting for baseline symptoms (d = 0.33; Jeronimus et al., 2016).
E/PE.
When compared to N/NE, there is greater uncertainty about prospective associations between (low) E/PE and depression. A comprehensive meta-analysis documented a substantial association between E/PE and future depression (d = −0.54), but this prospective association was markedly diminished when adjusting for baseline symptoms (d = −0.16), suggesting that E/PE is a comparatively weak predictor of longitudinal changes in depression (Khazanov & Ruscio, 2016).
N/NE, E/PE, and Anxiety
Relative to depression, less empirical attention has been devoted to understanding the consequences of N/NE and E/PE for longitudinal changes in anxiety. Nevertheless, the Jeronimus et al. (2016) meta-analysis noted above documented robust prospective associations between N/NE and anxiety symptoms (d = 0.68) and disorders (d = 0.48), even after controlling for baseline symptoms (d = 0.38 and 0.18, respectively; Jeronimus et al., 2016). On the other hand, the Khazanov-Ruscio meta-analysis indicated that longitudinal associations between E/PE and anxiety (d = −0.39) are notably weaker after controlling for baseline variation in symptom severity (d = −0.18; Khazanov & Ruscio, 2016).
DSM-Centered Research Limits Conceptual Precision
There is compelling evidence that high levels of N/NE, and potentially low levels of E/PE, prospectively predict longitudinal changes in internalizing problems. Yet our understanding is limited by the field’s heavy empirical and conceptual emphasis on traditional categorical diagnoses. Because they are defined by polythetic criteria, patients diagnosed with MDD and other DSM-5 internalizing disorders show marked variability in symptom presentations (Olbert, Gala, & Tupler, 2014). In fact, any two patients diagnosed with MDD typically have little overlap in their symptom profiles (Fried & Nesse, 2015). This heterogeneity makes it impossible to determine which facets of pathological depression and anxiety account for their well-documented longitudinal associations with N/NE and, somewhat less consistently, E/PE (Conway, Forbes et al., 2019). Furthermore, structural research has established that many internalizing symptoms cut across diagnoses—consistent with rampant comorbidity, overlapping treatment effects, and shared genetic substrates—whereas other symptoms are more specific (Barlow et al., 2014; Forbes, 2023; Hur et al., 2019; Watson et al., 2022). Traditional DSM-centered research cannot resolve whether N/NE is primarily related to the symptoms that bind depression and anxiety together or those that distinguish specific syndromes or syndrome clusters. In sum, evidence linking personality traits to MDD and other isolated diagnoses cannot shed light on the particular features of internalizing psychopathology that underlie such prospective associations, and therefore existing theoretical models remain underspecified (e.g., Klein et al., 2011).
Building on decades of success in developmental psychopathology research, hierarchical-dimensional models of internalizing psychopathology set the stage for overcoming this key barrier (Achenbach, 1966, 2020; Kotov et al., 2017, 2021, 2022). The tripartite model of anxiety and depression was the point of departure for much of the psychometric research into the architecture of internalizing symptoms (Mineka et al., 1998). This model posits that a broad (‘higher-order’) general distress symptom dimension characterizes all internalizing problems, whereas narrower (‘lower-order’) anxious arousal and positive affect (PA) dimensions account for differences in presentation across different internalizing problems. Anxious arousal was conceptualized as primarily related to panic, whereas blunted PA1 was specifically linked to depression and social anxiety (Watson et al., 2012). Ample research in adolescents and adults supports the convergent and discriminant validity of these three dimensions with respect to interviewer-rated diagnoses and self-reported symptoms (Mineka et al., 1998). This work also documented substantial individual differences in the sign and magnitude of longitudinal changes in the three symptom dimensions across the transition from late adolescence to early adulthood (Conway et al., 2017).
Efforts to understand the dimensional architecture of depression and anxiety have continued to evolve over the past two decades. The Hierarchical Taxonomy of Psychopathology (HiTOP) consortium synthesized these observations into a unified structural model of psychopathology (Kotov et al., 2017, 2021, 2022). Two features of the HiTOP model differentiate it from the kinds of categorical nosologies that have served as the conceptual foundation for the vast majority of work focused on dispositional risk for internalizing disorders. First, HiTOP constructs are continuous and dimensional, reflecting ample evidence that psychopathology constructs differ in degree, not kind (Haslam et al., 2020). Second, HiTOP is hierarchical. This means that internalizing disorders can be conceptualized and quantified at varying levels of breadth. At the base of the HiTOP framework, specific symptoms form circumscribed symptom components. Anxious arousal, for example, is defined by dizziness, shortness of breath, and faintness (Clark et al., 2014; Forbes et al., 2021; Waszczuk et al., 2017; Watson et al., 2007; Watson et al., 2012; Waszczuk et al., 2017). These components represent the most granular building blocks of the HiTOP framework and encompass the same symptoms and signs embodied in categorical diagnoses. Symptom components, in turn, covary in predictable ways to form syndromes. Insomnia, for instance, clusters with appetite loss, psychomotor retardation, and anergia to form a ‘vegetative depression’ syndrome (Waszczuk et al., 2017; Watson et al., 2007). Syndromes then coalesce into broader subfactors, such as distress (which accounts for symptoms shared by depression, generalized anxiety, and posttraumatic distress) and fear (which accounts for symptoms shared by panic, social anxiety, and phobias; Watson et al., 2022). At the top of the hierarchy, these subfactors form an overarching internalizing spectrum—akin to the tripartite model’s broadband general distress factor—that represent the symptoms (e.g., distress, perseverative thinking, indecision) that cut across many cases of pathological anxiety and depression.
Viewed from the perspective of HiTOP, prior efforts to document prospective associations between personality and isolated DSM diagnoses yield indeterminate inferences. The conventional interpretation is that prospective associations between N/NE and MDD reflect syndrome-specific links (“N/NE confers heightened risk for MDD”), but in fact such observations could reflect associations with the broader internalizing dimension, the narrower dimensions highlighted by the tripartite model, such as diminished PA, or some combination (Conway et al., 2019). Adopting an explicitly hierarchical-dimensional approach opens the door to resolving these fundamental questions.
Present Study
Leveraging an explicitly hierarchical-dimensional approach, the overarching goal of the present study was to understand the relevance of individual differences in personality—with a theory-driven emphasis on high-N/NE and low-E/PE—to longitudinal changes in broad (general distress) and narrow (anxious arousal and high-PA) internalizing-symptom dimensions in a racially diverse sample of 234 emerging adults followed for 2.5 years, across the transition from late adolescence to early adulthood. To ensure a broad spectrum of dispositional risk, participants were selectively recruited from a pool of 6,594 emerging adults screened for individual differences in N/NE, similar to other prospective-longitudinal studies focused on the emergence of internalizing symptoms (e.g., Alloy & Abramson, 1999; Young et al., 2021; Zinbarg et al., 2010). We focused on ‘emerging adulthood’ (~18 to 30 years) because it is a time of profound, often stressful transitions, with more than half of undergraduate students reporting moderate-to-severe levels of anxiety and depression, and many experiencing the emergence of clinically significant internalizing symptoms during this often-turbulent developmental chapter (Arnett, 2000; NASEM, 2021; Shackman et al., 2018; Vos et al., 2020).
Building on the tripartite model and its recent extensions, our primary focus was on prospective associations between baseline levels of N/NE and E/PE and longitudinal changes in general distress—the core cognitive (e.g., difficulty concentrating) and affective (e.g., worry) symptoms that cut across the emotional disorders—and the narrower dimensions of high-PA2 and anxious arousal thought to differentiate specific internalizing presentations across the transition to adulthood (Watson et al., 2008, 2012). From a developmental perspective, we conceptualize this transition as spanning a period of years, not weeks or months (Arnett, 2000). Likewise, from the perspective of personality traits, we anticipated that the moderating effects of N/NE and E/PE on the course of internalizing symptoms would accrue gradually and primarily be discernible at the scale of years. On an exploratory basis, we examined the predictive value of other Big 5 traits (e.g., Conscientiousness), more granular facets of N/NE and E/PE (e.g., sociability), as well as longitudinal changes and dispositional predictors of other narrow-band internalizing symptom components (e.g., social anxiety). We anticipated that higher levels of N/NE at baseline would be associated with larger increases or smaller decreases in all internalizing dimensions across the 30-month longitudinal follow-up when controlling for baseline symptoms. In contrast, we hypothesized that lower levels of E/PE at baseline would be more narrowly associated with longitudinal decreases in high-PA (i.e., wellbeing). Given the dearth of published longitudinal data, we made no specific predictions regarding longitudinal changes in other narrow-band symptom components.
Adopting a hierarchical-dimensional perspective on the longitudinal course of depression and anxiety is important because of the potential gains in precision for both etiological models and risk assessment. It could be that (elevated) N/NE shows consistent, robust, and relatively nonspecific associations with future internalizing symptoms because it represents a common root cause or vulnerability (‘diathesis’) for the pervasively elevated distress and dysphoria that defines the internalizing spectrum (Ormel et al., 2013; Barlow et al., 2014; Hur et al., 2019). Typically, this inference is assumed, but not explicitly tested. Likewise, it could be that (attenuated) E/PE shows comparatively inconsistent and weak associations with longitudinal changes in internalizing symptoms because it narrowly confers risk for deficits in high-PA—a possibility that has not previously been tested. In short, the present study has the potential to inform the development of more precise models of how emotional traits promote the development of internalizing symptoms in emerging adulthood, with implications for the design of more effective transdiagnostic intervention strategies for older adolescents and young adults (Gruber et al., 2023; Sauer-Zavala & Barlow, 2021).
Transparency and Openness
Processed data, analysis code, and supplemental material are freely available at https://osf.io/xvgr5/. We report below how we determined our sample size, all data exclusions, and all measures involved in this study. We report how we determined our sample size, all data exclusions, and all measures in the study. This study was not preregistered. All procedures were approved by the University of Maryland Institutional Review Board (protocol # 659385-28).
Method
Overview and General Procedures
The present study leverages previously unpublished data collected as part of a larger 30-month prospective-longitudinal study focused on the development of internalizing illness in emerging adults. The general study design was inspired by Alloy and Abramson’s seminal 30-month Temple-Wisconsin study of depression in university students (Alloy & Abramson, 1999) and reflected a compromise between the scientific goal of tracking the participants for as long as possible—to enable greater opportunity for meaningful change in the severity of internalizing symptoms—and practical considerations, including the need to screen, enroll, and perform multiple waves of follow-up assessments within the constraints of a 5-year grant and 4-year baccalaureate degree program.
We used well-established measures of N/NE to screen 6,594 young adults (57.1% female, 42.9% male; 59.0% White, 19.0% Asian, 9.9% African American, 6.3% Hispanic, 5.8% Multiracial/Other; M = 19.2 years, SD = 1.1 years) (Hur et al., 2020a; Shackman et al., 2018). Screening data were stratified into quartiles (top quartile, middle quartiles, bottom quartile) separately for men and women. Individuals who met preliminary inclusion criteria were independently and randomly recruited from each of the resulting six strata. Given the focus of the larger study, approximately half the participants were recruited from the top quartile, with the remainder split between the middle and bottom quartiles (i.e., 50% high, 25% medium, and 25% low). This enabled us to sample a wide range of internalizing risk without gaps or discontinuities, while balancing the inclusion of men and women. Simulation work suggests that this oversampling (‘enrichment’) approach does not bias statistical tests to a degree that would compromise their validity (Hauner, Zinbarg, & Revelle, 2014).
At enrollment, all participants were first-year university students in good physical health with normal or corrected-to-normal color vision and access to a personal smartphone. All reported the absence of lifetime neurological or pervasive developmental disorders, MRI contraindications, or prior experience with aversive electrical stimulation. All were free from lifetime psychotic and bipolar disorders; a current DSM-5 ‘blue ribbon’ mood, anxiety, or trauma disorder (past 2 months); severe substance abuse (i.e., associated with physical disability, hospitalization, or inpatient treatment); active suicidality; and ongoing psychiatric treatment as determined by an experienced masters-level diagnostician using the Structured Clinical Interview for DSM-5 (First, Williams, Karg, & Spitzer, 2015). To maximize the range of risk, participants with a current Other Specified internalizing diagnosis and/or a lifetime history of internalizing disorders were not excluded, consistent with prior studies of this kind (Alloy & Abramson, 1999). At the initial laboratory session (0 months), participants provided informed written consent and completed self-report measures of personality and internalizing symptoms. Symptoms were re-assessed 6, 24, and 30 months later. Big Five domains were re-assessed 6 months after the initial visit. Follow-up assessments were conducted in the laboratory or online based on participant preference.
We created composite personality and internalizing measures that were aggregated across adjacent assessments, minimizing error and occasion-specific (‘state’) fluctuations in responding (Chmielewski & Watson, 2009; Gell et al., 2023; Nikolaidis et al., 2022). We averaged the 0- and 6-month personality assessments to form ‘baseline’ composites for the Big Five domains. A parallel approach was used for the internalizing symptoms, which were separately averaged across the 0- and 6-month (‘baseline’) and the 24- and 30-month assessments (‘follow-up’). The decision to focus our analyses on aggregate measures was motivated by a combination of conceptual and methodological considerations. From a conceptual perspective, we aimed to understand the prospective relevance of dispositional risk to change in internalizing symptoms across the transition from late adolescence to early adulthood—a transition that spans years, not weeks or months (Arnett, 2000). Shorter-term fluctuations (e.g., 0 to 6 months) in internalizing are not central to our aims. In light of this goal, it was methodologically appealing to aggregate the two natural pairs of assessments—’baseline’ (0–6 months) and ‘follow-up’ (24–30 months)—enhancing reliability and statistical power (Tiego et al., in press).
All procedures were approved by the University of Maryland Institutional Review Board (protocol # 659385-28). The present sample overlaps with that featured in prior work focused on social anxiety and momentary affect (Hur et al., 2020a), the basic neurobiology of threat processing (Hur et al., 2020b), relations between neural reactivity to threat and momentary affect (Hur et al., 2022), and the neuroanatomical correlates of early-life shyness and behavioral inhibition (Bas-Hoogendam et al., 2022), but it has never been used to understand the factors associated with longitudinal changes in internalizing symptoms.
Participants
A total of 258 participants met preliminary inclusion criteria and provided informed written consent. Of these, 234 successfully completed all aspects of the baseline assessment—including a diagnostic interview, self-report measures, and MRI assessment—and were deemed eligible for longitudinal follow-up (50.0% female; 61.1% White, 17.9% Asian, 9.0% African American, 4.7% Hispanic, 0.4% Native Hawaiian or Other Pacific Islander, 6.8% Multiracial/Other; M = 18.8 years, SD = 0.4 years). The remaining 24 were deemed ineligible based on the baseline diagnostic interview (e.g., current or recent internalizing illness) or withdrew from the study.
Power Analysis
Sample size was determined a priori as part of the award that supported data collection (R01-MH107444) on the basis of benchmark (i.e., analysis independent) effect sizes. The target sample size (N = 240) was chosen to afford acceptable power and precision given available resources (Schönbrodt & Perugini, 2013). At the time of study design, G-power 3.1.9.2 (Faul et al., 2007) indicated >99% power to detect a generic medium-sized effect (r = 0.30) with up to 20% planned attrition (N = 192 usable datasets) using α = 0.05 (two-tailed).
Measures
Internalizing Symptoms
Internalizing symptoms were assessed using the Inventory of Depression and Anxiety Symptoms (IDAS) (version 1; Watson et al., 2007). The IDAS includes 11 specific symptom scales: Appetite Gain, Appetite Loss, Dysphoria, Ill Temper, Insomnia, Lassitude, Panic, Social Anxiety, Suicidality, Traumatic Intrusions, and Well-Being). The Panic and Well-being scales map onto the narrow tripartite dimensions of anxious arousal and high-PA, respectively (Watson et al., 2007). The IDAS also includes two broader scales: General Depression (which contains items drawn from several specific IDAS scales) and Dysphoria (which does not). To maximize independence of measures, we used the latter scale to index the broadband internalizing dimension (Watson et al., 2007, 2012). The IDAS developers suggested that the Dysphoria scale captures “a large, nonspecific factor representing the core affective and cognitive symptoms of depression and anxiety” (Watson et al., 2012, p. 399), making it a strong marker of the tripartite model’s general distress construct. Variation in Dysphoria is a sensitive and specific marker of DSM internalizing diagnoses (Stasik-O’Brien et al., 2019). Participants used a 1 (not at all) to 5 (extremely) scale to rate themselves on a total of 64 items; item responses were averaged to compute mean scale scores. For the present study, the IDAS timeframe was modified to cover past-month symptoms. As noted earlier, IDAS dimensions were separately averaged across the two early assessments (0 and 6 months) to form ‘baseline’ composites, and across the two late assessments (24 and 30 months) to form ‘follow-up’ composites. Cronbach’s alpha and omega internal-consistency reliability was 0.91/0.93, 0.94/0.96, and 0.89/0.91 at baseline and 0.93/0.95, 0.95/0.96, and 0.90/0.93 at follow-up for the Dysphoria, Well-Being, and Panic composites, respectively.
Personality
Trait-like individual differences in personality were assessed using the Big Five Inventory-2 (BFI-2; Soto & John, 2017). Participants used a 1 (disagree strongly) to 5 (agree strongly) scale to rate themselves on 60 items that tap into the five major axes of normal-range personality: N/NE, E/PE, Open-mindedness, Agreeableness, and Conscientiousness. Scale scores were computed by computing the mean of relevant items. Paralleling the approach used for the internalizing symptom dimensions, personality traits were averaged across months 0 and 6 to create ‘baseline’ personality composites. At baseline, Cronbach’s alpha and omega reliability was 0.94/0.96, 0.90/0.93, 0.86/0.89, 0.89/0.92, and 0.86/0.91 for the N/NE, E/PE, Agreeableness, Conscientiousness, and Open-Mindedness composites, respectively. Each Big Five domain encompassed three 4-item facets, which we examined in exploratory analyses.
Analytic Strategy
The central aim of the present study was to understand the degree to which variation in N/NE and E/PE is associated with longitudinal changes in broadband (general distress) and narrow-band (anxious arousal and high-PA) internalizing symptoms across the transition from late adolescence (‘baseline’) to early adulthood (‘follow-up’). To that end, we used Latent Change Score (LCS) models, a form of structural equation modeling (McArdle, 2001; McArdle & Nesselroade, 1994; Klopack & Wickrama, 2020; Kievit et al., 2018). LCS models were implemented using the lavaan package for R and robust maximum likelihood estimation, which accounts for potential non-normality (Rosseel, 2012; R core team, 2020). Data missingness was addressed using full information maximum likelihood estimation (Allison, 2003). Personality data (BFI-2) were unavailable for a single participant at month 6. Symptom data (IDAS) were unavailable for 1, 5, and 6 participants at months 6, 24, and 30, respectively.
To examine patterns of symptom change, we specified a univariate LCS model that accounted for variation in follow-up internalizing symptoms as a function of baseline internalizing symptoms and a LCS factor. The LCS factor accounts for deviations between baseline and follow-up symptom scores, with the intercept representing the average change in symptoms and the variance indicating the degree of between-person variability in change. The model also included an association between baseline internalizing and the LCS factor, representing the degree to which change-over-time is associated with the severity of initial internalizing symptoms.
To examine prospective associations between baseline variation in personality and longitudinal change in internalizing symptoms, we specified conditional LCS models—separately for each symptom dimension—in which baseline internalizing and the change factor were regressed on all Big Five domains simultaneously. This approach has the advantage of estimating the degree to which each personality domain is uniquely associated with both baseline levels (cross-sectional) and changes (longitudinal) in internalizing outcomes, over and above the variance shared with the remaining Big Five domains.
Results
Descriptive Statistics
Table 1 provides descriptive statistics for the three primary internalizing outcomes. Baseline levels of Dysphoria (i.e., general distress), Well-being (i.e., high-PA), and Panic (i.e., anxious arousal) were well aligned with normative levels in university and nationally representative samples (Nelson, O’Hara, & Watson, 2018; Watson et al., 2012). At baseline, 46%, 19%, and 12% of the sample exceeded liberal, moderate, and conservative empirically based thresholds, respectively, for a probable internalizing disorder diagnosis (Stasik-O’Brien et al., 2019). Although none of the participants met DSM-5 criteria for depression or anxiety disorders at enrollment, these observations suggest a relatively high prevalence of subclinical internalizing symptoms or ‘other-specified’ presentations that do not fit neatly into the (somewhat arbitrary) boundaries of categorical DSM-5 diagnoses.
Table 1.
Descriptive statistics for primary internalizing outcomes and personality dimensions.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | M (SD) | N | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Dysphoria, Baseline | . | . | . | . | . | . | . | . | . | . | 2.03 (0.68) | 234 |
| 2 | Dysphoria, Follow-up | 0.62 | . | . | . | . | . | . | . | . | . | 2.08 (0.77) | 230 |
| 3 | Well-beinga, Baseline | −0.46 | −0.38 | . | . | . | . | . | . | . | . | 3.06 (0.43) | 234 |
| 4 | Well-beinga, Follow-up | −0.22 | −0.47 | 0.60 | . | . | . | . | . | . | . | 3.05 (0.46) | 230 |
| 5 | Panicb, Baseline | 0.70 | 0.46 | −0.23 | −0.06 | . | . | . | . | . | . | 1.30 (0.40) | 234 |
| 6 | Panicb, Follow-up | 0.54 | 0.64 | −0.18 | −0.13 | 0.65 | . | . | . | . | . | 1.29 (0.43) | 230 |
| 7 | N/NE, Baseline | 0.75 | 0.56 | −0.50 | −0.26 | 0.46 | 0.35 | . | . | . | . | 33.24 (10.19) | 234 |
| 8 | E/PE, Baseline | −0.42 | −0.27 | 0.49 | 0.31 | −0.30 | −0.20 | −0.42 | . | . | . | 38.88 (9.95) | 234 |
| 9 | Conscientiousness, Baseline | −0.40 | −0.36 | 0.36 | 0.24 | −0.28 | −0.29 | −0.35 | 0.25 | . | . | 41.41 (8.17) | 234 |
| 10 | Agreeableness, Baseline | −0.37 | −0.33 | 0.38 | 0.28 | −0.26 | −0.23 | −0.44 | 0.25 | 0.30 | . | 44.33 (7.19) | 234 |
| 11 | Open-mindedness, Baseline | 0.07 | 0.03 | 0.17 | 0.20 | −0.01 | 0.05 | 0.04 | 0.18 | 0.06 | 0.18 | 45.63 (7.23) | 234 |
The IDAS ‘Well-being’ scale is conceptualized as an indicator of high positive affect.
IDAS ‘Panic’ is conceptualized as an indicator of anxious arousal symptoms.
Note. Correlations were computed using pairwise deletion. Abbreviations—E/PE = Extraversion/Positive Emotionality; N = sample size; N/NE = Neuroticism/Negative Emotionality; SD = standard deviation
Table 1 suggests that the average observed levels of internalizing symptoms were relatively stable from baseline to follow-up. The Cohen’s d effect sizes (based on standard deviations of baseline scores) were 0.08, −0.03, and −0.03 for Dysphoria, Well-being, and Panic, respectively. Nevertheless, Figure 1 makes it clear that there were marked individual differences in the sign and slope of longitudinal change.
Figure 1. Change in observed internalizing symptoms across the transition from late adolescence to early adulthood.
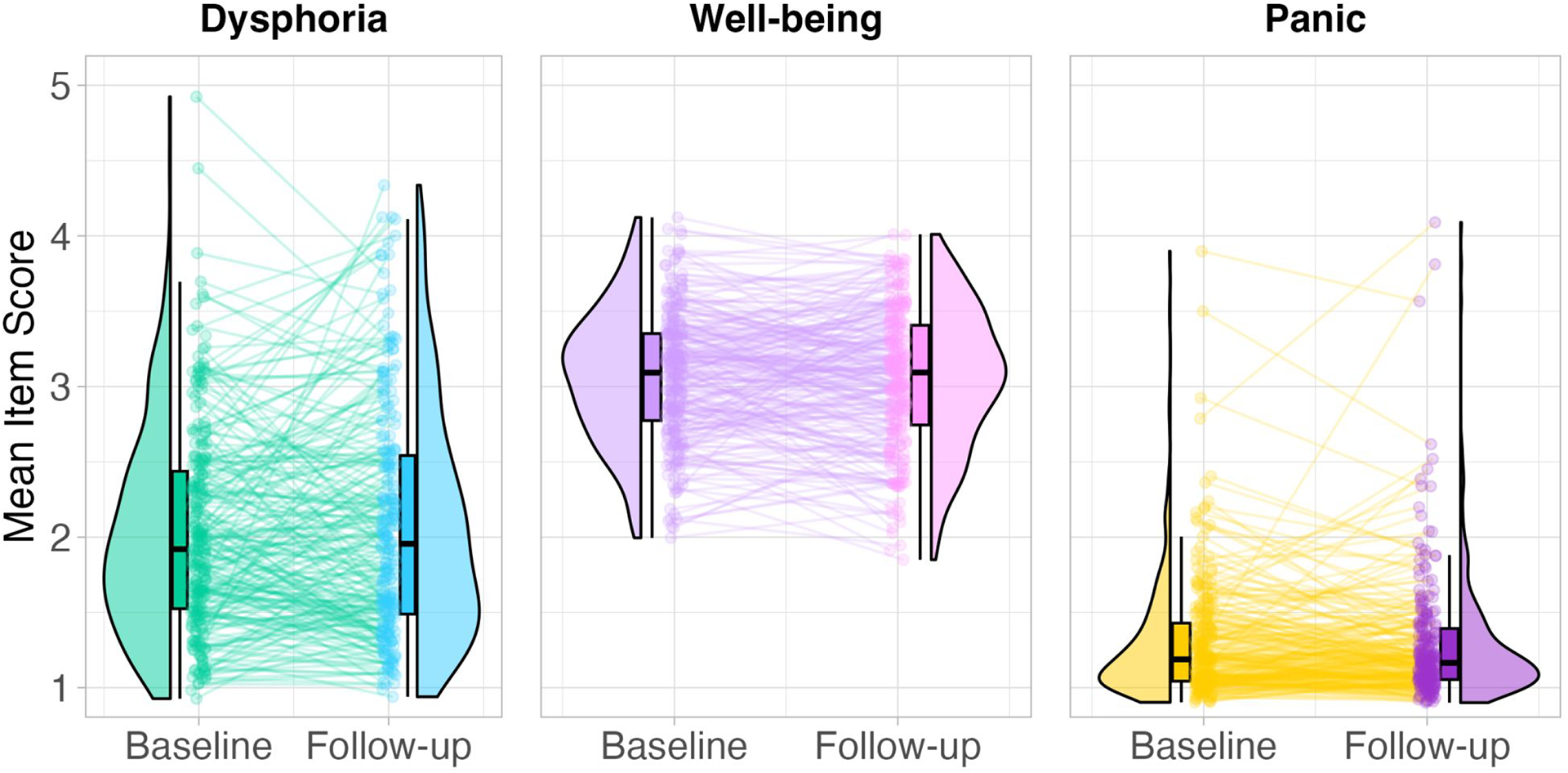
Individual internalizing symptoms were rated using a 5-point Likert scale. Dots depict mean scale scores at baseline or follow-up for individual participants. Gray lines depict the sign and magnitude of intra-individual longitudinal changes. Boxplots indicate the median and inter-quartile range. Half-violin (‘bean’) plots show the corresponding smoothed distributions. Note: ‘Baseline’ measures represent the average of the 0- and 6-month assessments. ‘Follow-up’ measures represent the average of the 24- and 30-month assessments.
Unconditional LCS Models
A series of univariate LCS models was used to estimate average symptom changes from baseline to follow-up, individual differences in longitudinal change, and the degree to which change was associated with baseline symptoms. Table 2 presents the resulting parameter estimates. None of the LCS factor intercepts significantly differed from 0, indicating negligible mean changes. Consistent with the results depicted in Figure 1, LCS factor variance was substantial and statistically significant (p < .001) for all of the primary internalizing outcomes, indicating meaningful individual differences in the sign and degree of longitudinal symptom change3,4. For 3 internalizing dimensions, there were moderate negative associations between baseline symptoms and the degree of longitudinal change (r = −0.21 to −0.39), indicating that emerging adults with more severe symptoms at baseline tended to show smaller increases (or larger decreases), consistent with regression to the mean.
Table 2.
Parameter estimates from univariate unconditional latent change score models of primary internalizing outcomes.
| Parameter (SE) | Dysphoria | Well-beinga | Panicb |
|---|---|---|---|
| Covariance of change factor with baseline symptoms | −0.135 (0.033)*** | −0.067 (0.011)*** | −0.048 (0.015)*** |
| Correlation of change factor with baseline symptoms | −0.21*** | −0.39*** | −0.34*** |
| Change factor intercept | 0.050 (0.042) | −0.010 (0.026) | −0.011 (0.023) |
| Standardized change factor intercept | 0.08 | −0.03 | −0.03 |
| Baseline symptom mean | 2.031 (0.044)*** | 3.063 (0.028)*** | 1.304 (0.026)*** |
| Change factor variance | 0.402 (0.057)*** | 0.157 (0.017)*** | 0.124 (0.031)*** |
| Baseline symptom variance | 0.455 (0.054)*** | 0.185 (0.015)*** | 0.160 (0.037)*** |
The IDAS ‘Well-being’ scale is conceptualized as an indicator of high positive affect.
IDAS ‘Panic’ is conceptualized as an indicator of anxious arousal symptoms.
Notes.
p < .001.
Except where noted otherwise, parameter estimates are unstandardized. Abbreviations—SE = standard error
On an exploratory basis, we examined to what extent change in one symptom dimension over time was correlated with change in the others over the same span. We fit a series of bivariate LCS models to the data and examined the correlations across LCS factors. Results indicated that longitudinal changes in broadband Dysphoria were robustly associated with changes in the narrower Well-being (r = −0.40, p < 0.001) and Panic facets (r = 0.46, p < 0.001) in the expected directions. In contrast, the correlation among Well-being and Panic change factors was notably smaller, indicating weaker coupling (r = −0.14, p = 0.04). This pattern of results affirms how longitudinally independent these symptom dimensions can be, and underscores the importance of taking a multidimensional perspective that goes beyond monolithic DSM diagnoses. It also closely mirrors a prior longitudinal study of young adults that reported moderate co-development of broadband general distress and PA (r = 0.27) and general distress and anxious arousal (r = 0.59), but virtually no co-development of the narrow-band PA and anxious arousal dimensions (r = −0.02; Conway et al., 2017).
Conditional LCS Models
We used a series of conditional LCS models to quantify cross-sectional (‘baseline’) and prospective-longitudinal associations between personality and internalizing symptoms. Here, baseline symptoms and the LCS factor were simultaneously regressed on all Big Five personality domains. Table 3 shows that N/NE had statistically significant and robust cross-sectional associations with the 3 internalizing dimensions, particularly broadband Dysphoria (standardized effect = 0.64). E/PE showed a moderate cross-sectional association with Well-being (i.e., high-PA; standardized effect = 0.29), and modest cross-sectional links with Dysphoria and Panic (i.e., anxious arousal) (standardized effects = −0.12 and −0.11, respectively). Conscientiousness showed statistically significant cross-sectional associations with all 3 internalizing dimensions in the expected direction, albeit to a much smaller degree than N/NE (standardized effects: −0.14 to 0.15). Agreeableness and Open-mindedness were generally unrelated to the severity of baseline internalizing symptoms. The total variance in baseline symptoms collectively explained by the Big Five traits was 60%, 39%, and 24% for Dysphoria, Well-being, and Panic, respectively.
Table 3.
Regressions of primary outcomes on baseline personality domains in the latent change score model.
| Baseline Symptoms | LCS Factor (Representing Symptom Change) | |||||||
|---|---|---|---|---|---|---|---|---|
| b | SE | p | β | b | SE | p | β | |
| Dysphoria | ||||||||
| N/NE | 0.042 | 0.004 | < .001 | .64 | 0.015 | 0.006 | .018 | .24 |
| E/PE | −0.009 | 0.004 | .025 | −.12 | 0.002 | 0.005 | .729 | .02 |
| Conscientiousness | −0.012 | 0.003 | .001 | −.14 | −0.010 | 0.006 | .088 | −.13 |
| Agreeableness | −0.003 | 0.004 | .523 | −.03 | −0.008 | 0.007 | .261 | −.09 |
| Open-mindedness | 0.007 | 0.004 | .082 | .08 | 0.001 | 0.005 | .869 | .01 |
| Well-being a | ||||||||
| N/NE | −0.012 | 0.003 | < .001 | −.28 | 0.002 | 0.003 | .434 | .06 |
| E/PE | 0.014 | 0.003 | < .001 | .29 | 0.001 | 0.003 | .777 | .02 |
| Conscientiousness | 0.008 | 0.003 | .013 | .15 | 0.002 | 0.003 | .595 | .04 |
| Agreeableness | 0.007 | 0.004 | .063 | .12 | 0.004 | 0.004 | .320 | .07 |
| Open-mindedness | 0.006 | 0.003 | .073 | .10 | 0.006 | 0.003 | .082 | .11 |
| Panic b | ||||||||
| N/NE | 0.014 | 0.003 | < .001 | .35 | 0.001 | 0.002 | .748 | .02 |
| E/PE | −0.005 | 0.003 | .052 | −.11 | 0.000 | 0.002 | .907 | .01 |
| Conscientiousness | −0.006 | 0.003 | .035 | −.11 | −0.005 | 0.003 | .100 | −.12 |
| Agreeableness | −0.003 | 0.004 | .495 | −.05 | −0.003 | 0.004 | .424 | −.06 |
| Open-mindedness | 0.001 | 0.004 | .872 | .01 | 0.004 | 0.003 | .274 | .07 |
The IDAS ‘Well-being’ scale is conceptualized as an indicator of high positive affect.
IDAS ‘Panic’ is conceptualized as an indicator of anxious arousal symptoms.
Note. Bolded parameter estimates are statistically significant (p < 0.05). Abbreviations— E/PE = extraversion/positive emotionality; N/NE = neuroticism/negative emotionality.
Regarding the longitudinal change in symptoms over the 30-month follow-up period, baseline levels of N/NE were significantly associated with longitudinal increases in broadband Dysphoria (standardized effect = 0.24)—but not the narrow-band Well-being (0.06) or Panic (0.02) symptom dimensions—after adjusting for the other four personality domains (Table 3). In contrast, E/PE (standardized effects: 0.01 to 0.02) and the other Big Five personality traits had negligible associations with longitudinal changes in Dysphoria, Well-being, and Panic. The variance explained in change factors by the Big Five explained 6%, 2%, and 3% of the variance in Dysphoria, Well-being, and Panic changes, respectively.
Exploratory Analyses of N/NE and E/PE Personality Facets
We used a series of conditional LCS models to explore the relevance of narrower personality facets. For N/NE, we simultaneously regressed the Dysphoria LCS factor on the three facets captured by the BFI-2: Depression, Anxiety, and Emotional Volatility (Table 4). Results indicated that the Depression and Emotional Volatility facets (standardized effects ~= 0.18), but not the Anxiety facet (−0.02), have moderate longitudinal associations with Dysphoria. These facets may be primarily responsible for the prospective link between broadband N/NE and Dysphoria.
Table 4:
Regressions of symptom outcomes on baseline Neuroticism/Negative Emotionality facets
| Baseline Symptoms | LCS Factor (Representing Symptom Change) | |||||||
|---|---|---|---|---|---|---|---|---|
| b | SE | p | β | b | SE | p | β | |
| Dysphoria | ||||||||
| Depression | 0.097 | 0.012 | < 0.001 | 0.551 | 0.029 | 0.017 | 0.090 | 0.175 |
| Anxiety | 0.024 | 0.010 | 0.017 | 0.131 | −0.003 | 0.015 | 0.841 | −0.018 |
| Emotional Volatility | 0.029 | 0.010 | 0.004 | 0.167 | 0.029 | 0.014 | 0.042 | 0.178 |
| Well-being | ||||||||
| Depression | −0.074 | 0.008 | < 0.001 | −0.657 | −0.019 | 0.010 | 0.055 | −0.180 |
| Anxiety | 0.005 | 0.010 | 0.653 | 0.040 | 0.008 | 0.008 | 0.290 | 0.080 |
| Emotional Volatility | 0.006 | 0.009 | 0.497 | 0.055 | 0.012 | 0.008 | 0.162 | 0.115 |
| Panic | ||||||||
| Depression | 0.034 | 0.009 | < 0.001 | 0.322 | 0.014 | 0.009 | 0.092 | 0.158 |
| Anxiety | 0.009 | 0.007 | 0.179 | 0.084 | −0.011 | 0.008 | 0.172 | −0.113 |
| Emotional Volatility | 0.012 | 0.008 | 0.122 | 0.113 | 0.005 | 0.007 | 0.473 | 0.057 |
Note. Bolded parameter estimates are statistically significant (p < 0.05).
We detected significant prospective associations between two of the three E/PE facets—Sociability (0.21) and Energy Level (−0.23)—and longitudinal changes in Dysphoria (Table 5). Energy Level also showed a significant association with changes in Well-being (i.e., high-PA; 0.17). These observations are broadly consistent with prior cross-sectional work (e.g., Watson, Stanton et al., 2019) and a prior longitudinal study in community-dwelling adults (Khoo et al., 2020). They provide preliminary evidence that specific facets of E/PE have predictive validity for the longitudinal development of broadband internalizing symptoms, prospective associations that are not evident at the broader domain level (E/PE).
Table 5:
Regressions of symptom outcomes on baseline Extraversion/Positive Emotionality facets
| Baseline Symptoms | LCS Factor (Representing Symptom Change) | |||||||
|---|---|---|---|---|---|---|---|---|
| b | SE | p | β | B | SE | p | β | |
| Dysphoria | ||||||||
| Sociability | 0.014 | 0.013 | 0.275 | 0.087 | 0.033 | 0.015 | 0.026 | 0.210 |
| Assertiveness | −0.037 | 0.013 | 0.004 | −0.192 | −0.015 | 0.017 | 0.395 | −0.080 |
| Energy Level | −0.094 | 0.017 | < 0.001 | −0.441 | −0.047 | 0.019 | 0.013 | −0.234 |
| Well-being | ||||||||
| Sociability | −0.003 | 0.008 | 0.766 | −0.024 | −0.010 | 0.008 | 0.224 | −0.102 |
| Assertiveness | 0.015 | 0.009 | 0.079 | 0.122 | 0.002 | 0.010 | 0.828 | 0.020 |
| Energy Level | 0.073 | 0.009 | < 0.001 | 0.536 | 0.022 | 0.010 | 0.028 | 0.174 |
| Panic | ||||||||
| Sociability | −0.001 | 0.009 | 0.937 | −0.007 | 0.012 | 0.008 | 0.151 | 0.135 |
| Assertiveness | −0.009 | 0.009 | 0.279 | −0.080 | −0.008 | 0.011 | 0.464 | −0.079 |
| Energy Level | −0.037 | 0.010 | < 0.001 | −0.297 | −0.012 | 0.008 | 0.133 | −0.109 |
Note. Bolded parameter estimates are statistically significant (p < 0.05).
Supplementary Tables S5.1–S5.5 provide comparable results for the other Big Five facets and for secondary symptom outcomes.
Exploratory Analyses of Secondary Internalizing Outcomes
Supplementary Table S6 shows the results from exploratory analyses of the eight other narrow-bandwidth internalizing dimensions captured by the IDAS. We regressed each of the eight IDAS symptom dimensions on all five personality domains simultaneously. Higher N/NE was associated with significant longitudinal increases in Appetite Gain and Lassitude (i.e., weariness and fatigue), higher E/PE was associated with significant longitudinal increases in Appetite Gain and decreases in Social Anxiety and Suicidality, and higher Conscientiousness significantly predicted decreases in Ill-temper (i.e., anger, hostility).
Discussion
Meta-analyses show that elevated levels of N/NE and, somewhat less consistently, lower levels of E/PE confer risk for future pathological depression and anxiety. Yet the vast majority of prospective-longitudinal research has narrowly focused on traditional diagnostic categories, creating uncertainty about the precise nature of these prospective associations. Here we leveraged an explicitly hierarchical-dimensional approach to understand the relevance of individual differences in N/NE and E/PE to longitudinal changes in broad and narrow internalizing symptoms in a racially diverse sample followed across the transition from late adolescence to early adulthood.
Nature of Internalizing Change in Emerging Adulthood
We found negligible changes—less than one-tenth of a SD—in average levels of broadband general distress, high-PA, and anxious arousal symptoms over the 2.5-year follow-up period. These observations indicate that most internalizing symptoms do not rise or fall much on average among emerging adults. This result is generally consistent with prior epidemiologic research showing increases in some internalizing indicators (e.g., depression diagnoses) but not others (e.g., social anxiety, specific phobias) during this developmental chapter (e.g., Copeland et al., 2014; Costello et al., 2011; Kessler et al., 2005; Rohde et al., 2013). Nevertheless, we observed marked individual differences in the degree and direction of change across all 3 primary symptom outcomes (Figure 1).
N/NE Uniquely Predicts Increases in Broadband Internalizing Symptoms in Emerging Adults
Prior studies have linked elevated levels of N/NE to the future development, chronicity, and recurrence of DSM-diagnosed depression and anxiety disorders (Hur et al., 2019). The present findings extend and refine these observations. N/NE was prospectively associated with longitudinal increases in the general distress (standardized effect = 0.24)—the core cognitive and affective symptoms that cut across the emotional disorders and best define HiTOP’s internalizing spectrum—even after adjusting for other Big Five domains and baseline symptoms. The magnitude of this association is consistent with prior work in young and middle-aged adults, underscoring N/NE’s unique prognostic value for internalizing psychopathology (Goldstein, Perlstein et al., 2020; Hayden & Klein, 2001; Newton-Howes et al., 2015; Wilson et al., 2014). In contrast, N/NE showed negligible associations with longitudinal changes in narrow-band anxious arousal and high-PA symptoms. Nevertheless, exploratory analyses did demonstrate that baseline variation in N/NE is associated with longitudinal increases in lassitude (i.e., weariness and fatigue) and appetite gain, narrow symptom dimensions that have received comparatively little conceptual and empirical attention (Supplementary Table S6).
On balance, this general pattern of results reinforces the hypothesis that N/NE represents a common root cause or shared vulnerability (‘diathesis’) for the chronically elevated distress and dysphoria that cuts across the internalizing spectrum of disorders (Barlow et al., 2014; Hur et al., 2019; Ormel et al., 2013). This conclusion is consistent with work demonstrating the clinical efficacy of the Unified Protocol for the Transdiagnostic Treatment of Emotional Disorders and other emerging ‘broad-spectrum’ interventions that target N/NE (Barlow et al., 2017; Dalgleish et al., 2020; Sauer-Zavala & Barlow, 2021).
E/PE is Unrelated to Longitudinal Changes in Primary Internalizing Outcomes
E/PE was positively associated with high-PA at baseline, over and above other Big 5 domains (standardized effect = 0.29), but, contrary to expectations, was not associated with longitudinal changes in high-PA (0.02). E/PE was also unrelated to changes in anxious arousal (0.01) or general distress symptoms (0.02). These observations run counter to claims that low levels of E/PE confer heightened risk for the future development and maintenance of depression (Klein et al., 2011). Previous longitudinal research on E/PE and internalizing outcomes has been mixed. Our study joins a number of others in finding an effect size close to 0 (Khazanov & Ruscio, 2016). The present results extend this work by clarifying E/PE’s associations with symptom dimensions at various levels of the internalizing domain.
Inconsistent E/PE associations across longitudinal studies undoubtedly reflect a variety of substantive differences, including variation in sample demographics, assessment instruments, follow-up duration, and analytic strategy. While different questionnaire assessments of E/PE are robustly correlated at the domain level, they show notable differences in their coverage of specific facets of E/PE (Soto & John, 2017; Watson, Nus & Wu, 2019). The results of our exploratory analyses demonstrate that variation in Energy Level and other facets of E/PE captured by the BFI-2 questionnaire are significant predictors of change in broadband internalizing symptoms and high-PA in emerging adulthood (Table 5), consistent with cross-sectional evidence (Watson, Stanton et al., 2019). In fact, the magnitude of these prospective associations was numerically greater than those found for N/NE facets (Table 4). These preliminary observations reinforce the possibility that seemingly subtle differences in the choice of personality assessment can have important consequences for understanding dispositional risk, a point previously made by Watson and colleagues (Watson, Stanton et al., 2019). A key challenge for the future will be to determine the reproducibility of these associations in other populations. More broadly, these observations highlight the potential value—for prediction, for etiological understanding, and for intervention—of going beyond the Big 5 domains and systematically examining more granular measures of dispositional risk (Goldstein, Kotov et al., 2020; Goldstein, Perlstein et al., 2020; Mõttus et al., 2020; Watson, Stanton et al., 2019).
Exploratory Analyses Raise the Possibility That Low E/PE Confers Risk for Social Anxiety
Exploratory analyses of the eight other narrow-band symptom dimensions captured by the IDAS provide preliminary evidence that diminished levels of E/PE at baseline are uniquely associated with longitudinal increases in social anxiety symptoms in emerging adulthood (Supplementary Table S6). N/NE showed a trend-level association (p = .06). Taken with ample cross-sectional evidence that social anxiety is marked by diminished reactivity to positive experiences (e.g., Kashdan, 2007; Watson, Stanton et al., 2019), this prospective observation motivates the hypothesis that lower levels of E (social engagement and motivation) and PE (emotional reactivity to social and nonsocial reward) causally contribute to the development of social anxiety, and suggests the potential therapeutic value of targeting E/PE in individuals at-risk for developing with pathological social anxiety, for example, using emerging digital coaching approaches (Stieger et al., 2021).
Other Big 5 Traits Are Unrelated to Longitudinal Changes in Primary Internalizing Outcomes
Like E/PE, higher levels of Conscientiousness were associated with lower levels of internalizing symptoms at baseline (standardized effects = −0.14, −0.29, and −0.11 for general distress, high-PA, and anxious arousal, respectively). These findings are consistent with a prior cross-sectional work (Kotov et al., 2010). Agreeableness and Open-mindedness evinced no meaningful associations with baseline internalizing symptoms, which is also consistent with prior meta-analytic findings. Individual differences in Conscientiousness, Agreeableness, and Openness were all unrelated to longitudinal changes in internalizing symptoms.
Future Challenges
Despite a number of strengths, the present study was not without limitations. First, we focused on an ethnoracially diverse sample of emerging adults. A key challenge for future research will be to expand prospective-longitudinal work to include samples that better represent the full demographic diversity of the population, including other developmental periods and people who are in treatment, at high risk for suicide, and/or have a history of psychosis and bipolar disorder. Second, because the sample was part of larger study focused on risk for the development or recurrence of internalizing illness, individuals with a current internalizing diagnosis were excluded. This design choice undoubtedly restricted the range of baseline symptoms and might have led to attenuated estimates of symptom change across emerging adulthood, relative to what one would expect to see in the general population. From this perspective, it is possible that we underestimated the association between N/NE and increases in general distress and other internalizing symptoms. Third, as is typical of many studies in this area, the assessments of internalizing and personality both relied on self-report, leading to shared measurement variance, and potentially inflated association estimates. An important avenue for future research will be to extend this work to encompass other informants. Fourth, the IDAS covers only a subset of the internalizing domain’s narrow symptom components. We look forward to future work, perhaps based on the HiTOP consortium’s forthcoming omnibus measurement system (Watson, Forbes et al., 2022), that can more comprehensively map longitudinal personality-symptom associations.
Conclusions
In sum, the present results demonstrate that baseline variation in N/NE is uniquely associated with 30-month changes in general distress (i.e., broadband internalizing symptoms), but not anxious arousal or high-PA during the transition from late adolescence to early adulthood. E/PE and other Big Five traits were unrelated to change in our primary internalizing outcomes. The results of our exploratory analyses raise the possibility that prospective effects of E/PE on general distress are more evident at the facet level, and support the hypothesis that low levels of E/PE prospectively predict increases in social anxiety symptoms. Collectively, these observations highlight the centrality of N/NE to the longitudinal development of core components of internalizing psychopathology in emerging adulthood, provide new clues about the specific pathways linking dispositional risk to internalizing symptoms, set the stage for more precise etiologic and prognostic models of personality-psychopathology relations, and showcase the enhanced precision afforded by adopting hierarchical-dimensional models.
Supplementary Material
Acknowledgments
Authors acknowledge assistance and critical feedback from A. Antonacci, L. Friedman, J. Furcolo, C. Grubb, R. Hum, C. Kaplan, T. Kashdan, J. Kuang, C. Lejuez, D. Limon, S. Rose, J. Smith, J. Swayambunathan, A. Vogel, members of the Affective and Translational Neuroscience laboratory, the staff of the Maryland Neuroimaging Center, the Office of the Registrar at the University of Maryland, and 3 peer reviewers. This work was partially supported by the National Institutes of Health (AA030042, MH131264, MH121409, MH125370, MH132280); National Research Foundation of Korea (2021R1F1A1063385 and 2021S1A5A2A03070229); University of Maryland; and Yonsei Signature Research Cluster Program (2021-22-0005). Authors declare no conflicts of interest.
Footnotes
Earlier formulations of the tripartite model suggested that measures of low-PA (e.g., diminished motivation, interest, and enjoyment of rewards; often termed ‘anhedonia’) distinguish pathological depression from anxiety (Clark & Watson, 1991). While continuing to emphasize the importance of PA, more recent work indicates that high-PA (e.g., happy, excited, and enthusiastic; sometimes collectively termed ‘wellbeing’) demonstrates superior discriminant validity relative to measures of low-PA (Watson et al., 2008, 2012).
High-PA is an interstitial dimension in the HiTOP framework, a key component of both the Internalizing and Detachment domains (Clark & Watson, 2022; Kotov et al., 2017).
Supplementary Tables S1–S2 provide Cohen’s d and LCS-derived change estimates for the other eight internalizing dimensions captured by the IDAS scale. With the exception of Social Anxiety, the mean |d| value was 0.06, consistent with the effect sizes for Dysphoria, Well-being, and Panic. The effect for Social Anxiety was −0.36, more than three times as large as the next strongest effect. The LCS factor’s variance estimate was statistically significant (p<0.001) for all 8 dimensions, indicating meaningful individual differences in the sign and degree of symptom change.
To examine potential gender differences in longitudinal symptom change, we created a multiple-group version of the unconditional LCS models. As shown in Supplementary Table S3, neither the intercept nor the variance of the LCS factors varied significantly across gender, with one exception. Change in Dysphoria differed across genders. Men’s Dysphoria decreased by approximately one-tenth of a SD from baseline to follow-up, whereas women’s Dysphoria increased by approximately one-quarter of a SD. Supplementary Table S4 presents the corresponding parameter estimates for conditional LCS models separately for each gender. Results indicated that prospective associations between baseline differences in personality and symptom change showed negligible gender differences.
Resource Sharing
Raw data and select materials are publicly available at the National Institute of Mental Health Data Archive (https://nda.nih.gov/edit_collection.html?id=2447). Processed data and analysis code for this project are available at the Open Science Framework (https://osf.io/xvgr5/).
References
- Achenbach TM (1966). The classification of children’s psychiatric symptoms: A factor-analytic study. Psychological Monographs: General and Applied, 80(7), 1–37. 10.1037/h0093906 [DOI] [PubMed] [Google Scholar]
- Achenbach TM (2020). Bottom-up and top-down paradigms for psychopathology: A half-century odyssey. Annual Review of Clinical Psychology, 16, 1–24. 10.1146/annurev-clinpsy-071119-115831 [DOI] [PubMed] [Google Scholar]
- Allison PD (2003). Missing data techniques for structural equation modeling. Journal of Abnormal Psychology, 112(4), 545–557. 10.1037/0021-843X.112.4.545 [DOI] [PubMed] [Google Scholar]
- Alloy LB, & Abramson LY (1999). The Temple-Wisconsin Cognitive Vulnerability to Depression Project: Conceptual background, design, and methods. Journal of Cognitive Psychotherapy, 13(3), 227–262. [Google Scholar]
- Arnett JJ (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist, 55(5), 469–480. 10.1037/0003-066X.55.5.469 [DOI] [PubMed] [Google Scholar]
- Bas-Hoogendam JM, Bernstein R, Benson BE, Buss KA, Gunther KE, Pérez-Edgar K, Salum GA, Jackowski AP, Bressan RA, Zugman A, Degnan KA, Filippi CA, Fox NA, Henderson HA, Tang A, Zeytinoglu S, Harrewijn A, Hillegers M, White T, van IJzendoorn MH, … ENIGMA-Anxiety Working Group (2022). Structural Brain Correlates of Childhood Inhibited Temperament: An ENIGMA-Anxiety Mega-analysis. Journal of the American Academy of Child and Adolescent Psychiatry, 61(9), 1182–1188. 10.1016/j.jaac.2022.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow DH, Farchione TJ, Bullis JR, Gallagher MW, Murray-Latin H, Sauer-Zavala S, … & Cassiello-Robbins C (2017). The unified protocol for transdiagnostic treatment of emotional disorders compared with diagnosis-specific protocols for anxiety disorders: A randomized clinical trial. JAMA Psychiatry, 74(9), 875–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow DH, Sauer-Zavala S, Carl JR, Bullis JR, & Ellard KK (2014). The nature, diagnosis, and treatment of neuroticism: Back to the future. Clinical Psychological Science, 2(3), 344–365. [Google Scholar]
- Caspi A, Roberts BW, & Shiner RL (2005). Personality development: Stability and change. Annual Review of Psychology, 56, 453–484. [DOI] [PubMed] [Google Scholar]
- Clark LA (2005). Temperament as a unifying basis for personality and psychopathology. Journal of Abnormal Psychology, 114(4), 505. 10.1037/0021-843X.114.4.505 [DOI] [PubMed] [Google Scholar]
- Clark LA, & Watson D (1991). Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology, 100, 316–336. 10.1037//0021-843x.100.3.316 [DOI] [PubMed] [Google Scholar]
- Conway CC, Forbes MK, Forbush KT, Fried EI, Hallquist MN, Kotov R, Mullins-Sweatt SN, Shackman AJ, Skodol AE, South SC, Sunderland M, Waszczuk MA, Zald DH, Afzali MH, Bornovalova MA, Carragher N, Docherty AR, Jonas KG, Krueger RF, Patalay P, … Eaton NR (2019). A Hierarchical Taxonomy of Psychopathology Can Transform Mental Health Research. Perspectives on Psychological Science, 14(3), 419–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway CC, Zinbarg RE, Mineka S, & Craske MG (2017). Core dimensions of anxiety and depression change independently during adolescence. Journal of Abnormal Psychology, 126(2), 160–172. 10.1037/abn0000222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Angold A, Shanahan L, & Costello EJ (2014). Longitudinal patterns of anxiety from childhood to adulthood: the Great Smoky Mountains Study. Journal of the American Academy of Child & Adolescent Psychiatry, 53(1), 21–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Copeland W, & Angold A (2011). Trends in psychopathology across the adolescent years: what changes when children become adolescents, and when adolescents become adults? Journal of Child Psychology and Psychiatry, 52(10), 1015–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craske MG, Stein MB, Eley TC, Milad MR, Holmes A, Rapee RM, & Wittchen HU (2017). Anxiety disorders. Nature Reviews Disease Primers, 3, 17024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Stringaris A, & Wolpert M (2020). Treatment outcomes for depression: challenges and opportunities. The Lancet Psychiatry, 7(11), 925–927. 10.1016/S2215-0366(20)30036-5 [DOI] [PubMed] [Google Scholar]
- Dalgleish T, Black M, Johnston D, & Bevan A (2020). Transdiagnostic approaches to mental health problems: Current status and future directions. Journal of Consulting and Clinical Psychology, 88(3), 179–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dieleman JL, Cao J, Chapin A, Chen C, Li Z, Liu A, … & Murray CJ (2020). US health care spending by payer and health condition, 1996–2016. JAMA, 323(9), 863–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fanous A, Gardner CO, Prescott CA, Cancro R, & Kendler KS (2002). Neuroticism, major depression and gender: a population-based twin study. Psychological Medicine, 32(4), 719–728. 10.1017/s003329170200541x [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang A-G, & Buchner A (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39, 175–191. [DOI] [PubMed] [Google Scholar]
- First MB, Williams JB, Karg RS, & Spitzer RL (2015). Structured clinical interview for DSM-5—Research version (SCID-5 for DSM-5, research version; SCID-5-RV). Arlington, VA: American Psychiatric Association, 1–94. [Google Scholar]
- Forbes MK (2023). Implications of the symptom-level overlap among DSM diagnoses for dimensions of psychopathology. Journal of Emotion and Psychopathology, 1(1), 104–112. 10.55913/joep.v1i1.6 [DOI] [Google Scholar]
- Forbes MK, Sunderland M, Rapee RM, Batterham PJ, Calear AL, Carragher N, … & Krueger RF (2021). A detailed hierarchical model of psychopathology: From individual symptoms up to the general factor of psychopathology. Clinical Psychological Science, 9(2), 139–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried EI, & Nesse RM (2015). Depression is not a consistent syndrome: An investigation of unique symptom patterns in the STAR*D study. J Affect Disord, 172, 96–102. doi: 10.1016/j.jad.2014.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gell M, Eickhoff SB, Omidvarnia A, Küppers V, Patil KR, Satterthwaite TD, Müller VI, & Langner R (2023). The burden of reliability: How measurement noise limits brain-behaviour predictions. bioRxiv, 2023.2002.2009.527898. [Google Scholar]
- Gershuny BS, & Sher KJ (1998). The relation between personality and anxiety: findings from a 3-year prospective study. Journal of Abnormal Psychology, 107(2), 252. [DOI] [PubMed] [Google Scholar]
- Goldstein BL, Perlman G, Eaton NR, Kotov R, & Klein DN (2020). Testing explanatory models of the interplay between depression, neuroticism, and stressful life events: a dynamic trait-stress generation approach. Psychological Medicine, 50(16), 2780–2789. 10.1017/S0033291719002927 [DOI] [PubMed] [Google Scholar]
- Goldstein BL, Kotov R, Perlman G, Watson D, & Klein DN (2018). Trait and facet-level predictors of first-onset depressive and anxiety disorders in a community sample of adolescent girls. Psychological Medicine, 48, 1282–1290. [DOI] [PubMed] [Google Scholar]
- Gruber J, Hinshaw SP, Clark LA, Rottenberg J, & Prinstein MJ (2023). Young adult mental health beyond the COVID-19 era: Can enlightened policy promote long-term change? Policy Insights from the Behavioral and Brain Sciences, 10, 75–82. 10.1177/23727322221150199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslam N, McGrath MJ, Viechtbauer W, & Kuppens P (2020). Dimensions over categories: A meta-analysis of taxometric research. Psychological Medicine, 50(9), 1418–1432. 10.1017/S003329172000183X [DOI] [PubMed] [Google Scholar]
- Hauner KK, Zinbarg RE, & Revelle W (2014). A latent variable model approach to estimating systematic bias in the oversampling method. Behavior Research Methods, 46(3), 786–797. 10.3758/s13428-013-0402-6 [DOI] [PubMed] [Google Scholar]
- Hayden EP, & Klein DN (2001). Outcome of dysthymic disorder at 5-year follow-up: the effect of familial psychopathology, early adversity, personality, comorbidity, and chronic stress. American Journal of Psychiatry, 158(11), 1864–1870. 10.1176/appi.ajp.158.11.1864 [DOI] [PubMed] [Google Scholar]
- Hur J, DeYoung KA, Islam S, Anderson AS, Barstead MG, & Shackman AJ (2020a). Social context and the real-world consequences of social anxiety. Psychological Medicine, 50(12), 1989–2000. 10.1017/S0033291719002022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hur J, Kuhn M, Grogans SE, Anderson AS, Islam S, Kim HC, Tillman RM, Fox AS, Smith JF, DeYoung KA, & Shackman AJ (2022). Anxiety-related frontocortical activity is associated with dampened stressor reactivity in the real world. Psychological Science, 33(6), 906–924. 10.1177/09567976211056635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hur J, Smith JF, DeYoung KA, Anderson AS, Kuang J, Kim HC, Tillman RM, Manuel K, Fox AS, & Shackman AJ (2020b). Anxiety and the neurobiology of temporally uncertain threat anticipation. Journal of Neuroscience, 40, 7949–7964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hur J, Stockbridge MD, Fox AS, & Shackman AJ (2019). Dispositional negativity, cognition, and anxiety disorders: An integrative translational neuroscience framework. Progress in Brain Research, 247, 375–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeronimus BF, Kotov R, Riese H, & Ormel J (2016). Neuroticism’s prospective association with mental disorders halves after adjustment for baseline symptoms and psychiatric history, but the adjusted association hardly decays with time: a meta-analysis on 59 longitudinal/prospective studies with 443 313 participants. Psychological Medicine, 46(14), 2883–2906. 10.1017/S0033291716001653 [DOI] [PubMed] [Google Scholar]
- Kashdan TB (2007). Social anxiety spectrum and diminished positive experiences: theoretical synthesis and meta-analysis. Clinical Psychology Review, 27, 348–365. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Kessler RC, Heath AC, & Eaves LJ (1993). A longitudinal twin study of personality and major depression in women. Archives of General Psychiatry, 50(11), 853–862. 10.1001/archpsyc.1993.01820230023002 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, & Wittchen HU (2012). Twelve month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research, 21(3), 169–184. 10.1002/mpr.1359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Khazanov GK, & Ruscio AM (2016). Is low positive emotionality a specific risk factor for depression? A meta-analysis of longitudinal studies. Psychological Bulletin, 142(9), 99. 10.1037/bul0000059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoo S, Stanton K, Clark LA, & Watson D (2020). Facet-level personality relations of the symptom dimensions of the tripartite model. Journal of Psychopathology and Behavioral Assessment, 42, 160–177. [Google Scholar]
- Kievit RA, Brandmaier AM, Ziegler G, van Harmelen AL, de Mooij SM, Moutoussis M, … & NSPN Consortium. (2018). Developmental cognitive neuroscience using latent change score models: A tutorial and applications. Developmental Cognitive Neuroscience, 33, 99–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DN, Kotov R, & Bufferd SJ (2011). Personality and depression: explanatory models and review of the evidence. Annual Review of Clinical Psychology, 7, 269–295. 10.1146/annurev-clinpsy-032210-104540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klopack ET, & Wickrama K (2020). Modeling latent change score analysis and extensions in Mplus: A practical guide for researchers. Structural Equation Modeling: A Multidisciplinary Journal, 27(1), 97–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Cicero DC, Conway CC, DeYoung CG, Dombrovski A, Eaton NR, First MB, Forbes MK, Hyman SE, Jonas KG, Krueger RF, Latzman RD, Li JJ, Nelson BD, Regier DA, Rodriguez-Seijas C, Ruggero CJ, Simms LJ, Skodol AE, Waldman ID, … Wright A (2022). The Hierarchical Taxonomy of Psychopathology (HiTOP) in psychiatric practice and research. Psychological Medicine, 52(9), 1666–1678. 10.1017/S0033291722001301 [DOI] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Cicero DC, Conway CC, DeYoung CG, Eaton NR, Forbes MK, Hallquist MN, Latzman RD, Mullins-Sweatt SN, Ruggero CJ, Simms LJ, Waldman ID, Waszczuk MA, & Wright A (2021). The Hierarchical Taxonomy of Psychopathology (HiTOP): A Quantitative Nosology Based on Consensus of Evidence. Annual Review of Clinical Psychology, 17, 83–108. 10.1146/annurev-clinpsy-081219-093304 [DOI] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, Brown TA, Carpenter WT, Caspi A, Clark LA, Eaton NR, Forbes MK, Forbush KT, Goldberg D, Hasin D, Hyman SE, Ivanova MY, Lynam DR, Markon K, Miller JD, … Zimmerman M (2017). The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126(4), 454–477. 10.1037/abn0000258 [DOI] [PubMed] [Google Scholar]
- Kotov R, Perlman G, Gámez W, & Watson D (2015). The structure and short-term stability of the emotional disorders: a dimensional approach. Psychological Medicine, 45(8), 1687–1698. 10.1017/S0033291714002815 [DOI] [PubMed] [Google Scholar]
- Kotov R, Gamez W, Schmidt F, & Watson D (2010). Linking “big” personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychological Bulletin, 136(5), 768. 10.1037/a0020327 [DOI] [PubMed] [Google Scholar]
- McArdl JJ. (2001). A latent difference score approach to longitudinal dynamic structural analyses. In Cudeck R, du Toit S & Sörbom D (Eds.), Structural Equation Modeling: Present and Future (pp. 342–380). Lincolnwood, IL: Scientific Software International. [Google Scholar]
- McArdle JJ, & Nesselroade JR (1994). Using multivariate data to structure developmental change In Cohen SH & Reese HW (Eds.), Life Span Developmental Psychology: Methodological Contributions (pp. 223–267). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Mineka S, Watson D, & Clark LA (1998). Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology, 49(1), 377–412. 10.1146/annurev.psych.49.1.377 [DOI] [PubMed] [Google Scholar]
- Mõttus R, Wood D, Condon DM, Back MD, Baumert A, Costantini G, Epskamp S, Greiff S, Johnson W, Lukaszewski A, Murray A, Revelle W, Wright AGC, Yarkoni T, Ziegler M, & Zimmermann J (2020). Descriptive, predictive and explanatory personality research: Different goals, different approaches, but a shared need to move beyond the Big Few traits. European Journal of Personality, 34, 1175–1201. [Google Scholar]
- Naragon-Gainey K, McMahon TP, & Park J (2018). The contributions of affective traits and emotion regulation to internalizing disorders: Current state of the literature and measurement challenges. American Psychologist, 73, 1175–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NASEM. (2021). Mental health, substance use, and wellbeing in higher education: Supporting the whole student. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Nelson GH, O’Hara MW, & Watson D (2018). National norms for the expanded version of the Inventory of Depression and Anxiety Symptoms (IDAS-II). Journal of Clinical Psychology, 74(6), 953–968. 10.1002/jclp.22560 [DOI] [PubMed] [Google Scholar]
- Newton-Howes G, Horwood J, & Mulder R (2015). Personality characteristics in childhood and outcomes in adulthood: findings from a 30 year longitudinal study. The Australian and New Zealand Journal of Psychiatry, 49(4), 377–386. 10.1177/0004867415569796 [DOI] [PubMed] [Google Scholar]
- Nikolaidis A, Chen AA, He X, Shinohara RT, Vogelstein J, Milham M, & Shou H (2022). Suboptimal phenotypic reliability impedes reproducible human neuroscience. bioRxiv. [Google Scholar]
- Olbert CM, Gala GJ, & Tupler LA (2014). Quantifying heterogeneity attributable to polythetic diagnostic criteria: theoretical framework and empirical application. Journal of Abnormal Psychology, 123, 452–462. doi: 10.1037/a0036068 [DOI] [PubMed] [Google Scholar]
- Olfson M, Blanco C, Wall MM, Liu SM, & Grant BF (2019). Treatment of common mental disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions-III. The Journal of Clinical Psychiatry, 80(3), 21534. [DOI] [PubMed] [Google Scholar]
- Ormel J, Jeronimus BF, Kotov R, Riese H, Bos EH, Hankin B, Rosmalen J, & Oldehinkel AJ (2013). Neuroticism and common mental disorders: meaning and utility of a complex relationship. Clinical Psychology Review, 33(5), 686–697. 10.1016/j.cpr.2013.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team (2013). R: A language and environment for statistical computing.
- Rohde P, Lewinsohn PM, Klein DN, Seeley JR, & Gau JM (2013). Key characteristics of major depressive disorder occurring in childhood, adolescence, emerging adulthood, and adulthood. Clinical Psychological Science, 1(1), 41–53. 10.1177/2167702612457599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosseel Y (2012). lavaan: An R Package for Structural Equation Modeling. Journal of Statistical Software, 48(2), 1–36. [Google Scholar]
- Sauer-Zavala SE, & Barlow DH (2021). Neuroticism. A new framework for emotional disorders and their treatment. New York, NY: Guilford Press. [Google Scholar]
- Schönbrodt FD, & Perugini M (2013). At what sample size do correlations stabilize?. Journal of Research in Personality, 47(5), 609–612. 10.1016/j.jrp.2013.05.009 [DOI] [Google Scholar]
- Shackman AJ, Weinstein JS, Hudja SN, Bloomer CD, Barstead MG, Fox AS, & Lemay EP (2018). Dispositional negativity in the wild: Social environment governs momentary emotional experience. Emotion, 18(5), 707–724. 10.1037/emo0000339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singewald N, Sartori SB, Reif A, & Holmes A (2023). Alleviating anxiety and taming trauma: Novel pharmacotherapeutics for anxiety disorders and posttraumatic stress disorder. Neuropharmacology, 226, 109418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soto CJ, & John OP (2017). The next Big Five Inventory (BFI-2): Developing and assessing a hierarchical model with 15 Facets to enhance bandwidth, fidelity, and predictive power. Journal of Personality and Social Psychology, 113(1), 117–143. 10.1037/pspp0000096 [DOI] [PubMed] [Google Scholar]
- Spinhoven P, Elzinga BM, Hovens JGFM, Roelofs K, Van Oppen P, Zitman FG, & Penninx BWJH (2011). Positive and negative life events and personality traits in predicting course of depression and anxiety. Acta Psychiatrica Scandinavica, 124(6), 462–473. 10.1111/j.1600-0447.2011.01753.x [DOI] [PubMed] [Google Scholar]
- Stasik-O’Brien SM, Brock RL, Chmielewski M, Naragon-Gainey K, Koffel E, McDade-Montez E, O’Hara MW, & Watson D (2019). Clinical Utility of the Inventory of Depression and Anxiety Symptoms (IDAS). Assessment, 26(5), 944–960. 10.1177/1073191118790036 [DOI] [PubMed] [Google Scholar]
- Stieger M, Flückiger C, Rüegger D, Kowatsch T, Roberts BW, & Allemand M (2021). Changing personality traits with the help of a digital personality change intervention. PNAS, 118, e2017548118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiego J, Martin E, DeYoung CG, Hagan K, Cooper SE, Pasion R, Satchell L, Shackman AJ, Bellgrove MA, Fornito A, & The HiTOP Neurobiological Foundations Work Group. (in press). Precision behavioral phenotyping as a strategy for uncovering the biological correlates of psychopathology. Nature Mental Health. https://osf.io/geh6q/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, … & Bhutta ZA (2020). Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet, 396(10258), 1204–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Forbes MK, Levin-Aspenson HF, Ruggero CJ, Kotelnikova Y, Khoo S, Bagby RM, Sunderland M, Patalay P, & Kotov R (2022). The development of preliminary HiTOP internalizing spectrum scales. Assessment, 29(1), 17–33. [DOI] [PubMed] [Google Scholar]
- Watson D, Levin-Aspenson HF, Waszczuk MA, Conway CC, Dalgleish T, Dretsch MN, Eaton NR, Forbes MK, Forbush KT, Hobbs KA, Michelini G, Nelson BD, Sellbom M, Slade T, South SC, Sunderland M, Waldman I, Witthöft M, Wright A, Kotov R, … HiTOP Utility Workgroup (2022). Validity and utility of Hierarchical Taxonomy of Psychopathology (HiTOP): III. Emotional dysfunction superspectrum. World Psychiatry, 21(1), 26–54. 10.1002/wps.20943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Nus E, & Wu KD (2019). Development and validation of the faceted inventory of the five-factor model (FI-FFM). Assessment, 26, 17–44. [DOI] [PubMed] [Google Scholar]
- Watson D, O’Hara MW, Naragon-Gainey K, Koffel E, Chmielewski M, Kotov R, Stasik SM, & Ruggero CJ (2012). Development and validation of new anxiety and bipolar symptom scales for an expanded version of the IDAS (the IDAS-II). Assessment, 19(4), 399–420. 10.1177/1073191112449857 [DOI] [PubMed] [Google Scholar]
- Watson D, O’Hara MW, Chmielewski M, McDade-Montez EA, Koffel E, Naragon K, & Stuart S (2008). Further validation of the IDAS: evidence of convergent, discriminant, criterion, and incremental validity. Psychological Assessment, 20(3), 248–259. 10.1037/a0012570 [DOI] [PubMed] [Google Scholar]
- Watson D, O’Hara MW, Simms LJ, Kotov R, Chmielewski M, McDade-Montez EA, Gamez W, & Stuart S (2007). Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS). Psychological Assessment, 19(3), 253–268. 10.1037/1040-3590.19.3.253 [DOI] [PubMed] [Google Scholar]
- Watson D, Stanton K, Khoo S, Ellickson-Larew S, & Stasik-O’Brien SM (2019). Extraversion and psychopathology: A multilevel hierarchical review. Journal of Research in Personality, 81, 1–10. [Google Scholar]
- Waszczuk MA, Kotov R, Ruggero C, Gamez W, & Watson D (2017). Hierarchical structure of emotional disorders: From individual symptoms to the spectrum. Journal of Abnormal Psychology, 126(5), 613–634. 10.1037/abn0000264 [DOI] [PubMed] [Google Scholar]
- Wilson S, DiRago AC, & Iacono WG (2014). Prospective inter-relationships between late adolescent personality and major depressive disorder in early adulthood. Psychological Medicine, 44(3), 567–577. 10.1017/S0033291713001104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinbarg RE, & Barlow DH (1996). Structure of anxiety and the anxiety disorders: A hierarchical model. Journal of Abnormal Psychology, 105(2), 181–193. 10.1037//0021-843x.105.2.181 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


