Abstract
Context
Musculoskeletal disorders (MSKD) are currently the leading contributor to disability worldwide. Unlike other prevalent and disabling healthcare conditions such as CVD, risk factors associated with MSKD are not commonly discussed or integrated into current medical practice, rehabilitation practice or wellness programs. The primary purpose of this review is to describe the known risk factors most closely associated with MSKD. The secondary purpose is to propose a clinical model to manage MSK health aimed at maximizing the healthy pursuit of a physically active and healthy lifestyle.
Evidence acquisition
In this review the most common MSKD risk factors, with a focus on those that can be easily screened in clinical practice are presented. The importance of understanding the magnitude and number of risk factors present as well as the multidimensional nature of MSKD risk is discussed.
Results
A total of 11 MSKD risk factors were identified. Most of the risk factors are modifiable, and the evidence associated with modifiability for the most prominent risk factors is reviewed.
Researchers have found that often patients are discharged from care with several known MSKD risk factors. In such instances, local pain and dysfunction are managed well, but expanding our rehabilitation care to include comprehensive risk factor management would ultimately benefit the patient and reduce healthcare costs.
Conclusion
The most common MSKD risk factors are discussed and a clinical framework to individualize intervention is proposed. Addressing key risk factors within rehabilitation may be an important step to reduce the enormous and growing burden these disorders are having on society.
Level of Evidence
5
Keywords: Movement systems, musculoskeletal disorder, prevention, risk factor
INTRODUCTION
Musculoskeletal disorders (MSKD) include more than 150 diagnoses that affect the locomotor system of individuals. MSKD are initially recognized by musculoskeletal (MSK) pain, and then secondarily, by limitations in mobility, motor control, dexterity, and general function. They range from disorders that arise suddenly, such as fractures, sprains, and strains, to chronic conditions contributing to functional limitations and disability.1 Often the muscle, bone, or joint condition is mechanical in nature as is the case in osteoarthritis. Additionally, disorders affecting the body’s inflammatory process are included, such as rheumatoid arthritis, psoriatic arthritis, gout, and ankylosing spondylitis. World-wide, the most common MSKD reported are low back pain and osteoarthritis.2 MSKD are on the rise around the world.3 The total number of MSK-related disability-adjusted life years have increased by 25% from 2000 to 2015 with MSK diseases being the second cause of years lived with disability worldwide. MSKD are known to contribute to significant mental health decline, cluster around common chronic diseases and increase all-cause mortality.3
MSKD are the highest contributor to the need for rehabilitation across the globe with two-thirds of all adults in need of rehabilitation.4 More than one in two adults in the United States (US), 124 million over the age of 18, report a musculoskeletal medical condition. That exceeds the next two most common health conditions including circulatory conditions (such as heart disease, stroke, and hypertension) and respiratory conditions.5 Across all adult age categories, MSKD are either the most reported medical conditions (among those < 65 years old) or second most reported (among those 65 years and older). In 2015, 36% of the US adult population reported difficulties performing routine activities of daily living (ADLs) due to a medical condition. Of those adults reporting ADL limitations, 64 million had a concomitant musculoskeletal condition. Individuals in the US population with an MSKD are likely to have other associated conditions and comorbidities, affecting health overall and complicating the MSKD diagnosis and treatment process.6
A recent survey conducted in Australia7 focused on the impact of MSKD on the population and described similar results with an estimated seven million adults affected by chronic and painful MSKD. Of those affected, 57% report two or more MSKD, 66% indicated their condition had an adverse effect on their family and personal relationships, 72% report adverse effects on sleep, and 50% report a negative impact on their mental health. Additionally, MSKD can severely disrupt work for adults since 58% affected are in their prime working years between 25-64 years of age. In the United States, low back and neck pain are the most expensive health conditions, estimated at $134.5 billion. As this condition often occurs in the working-age population, the indirect costs, including disability benefits and days of work missed, are estimated to be as high as $624.8 billion.8
Considering millions of people seek rehabilitation currently, aligning rehabilitation professionals to focus on identifying the most prominent MSK risk factors for everyone under their care through a standardized operating procedure could be helpful. While prevention and physical activity promotion are clearly within the scope of the rehabilitation provider, efforts in these domains are falling short.9 Most patients conclude their rehabilitation program with little knowledge of the value of physical activity, without the awareness of their most prominent risk factors for MSK health and prevention.
Known strategies to prevent and treat MSKD are generally described around increasing physical activity levels. Good MSK health habits, like smart exercise, have an abundance of positive effects from decreased obesity to improved mental health and reduced pain.10 But, simply suggesting an individual with a MSKD become more active may not be an adequate solution. While most individuals are aware of the benefits of physical activity and exercise, many are unable to engage in routine physical activity because of existing MSKD pain. Approximately 76% of adults with an MSKD report that it directly limits their physical activity.7 Although increased physical activity is a proven way to decrease the prevalence of all-cause mortality risk factors and improve overall health, physical inactivity seems to be on the rise,11 and trends suggest MSKD are a contributing factor. While efforts focused on behavioral change can be helpful to increase activity level for some individuals12 a concurrent consideration for current MSK health status and risk should be considered as well.
There is a tremendous burden associated with MSKD directly and, because of their attenuating effect on physical activity levels, MSKD are also a silent contributing factor to the well-established chronic diseases that make up metabolic syndrome.13 In 2015, Carlson et al. noted that 11.1% of all health care costs were associated with “inadequate” physical activity and that this is on the rise.14 Theoretically, addressing MSKD by identification and management of common risk factors could result in improved physical activity levels, decreased injury rates, and less overall financial burden. Therefore, the primary purpose of this review is to describe the known risk factors most closely associated with MSKD. The secondary purpose is to propose a clinical model to manage MSK health aimed at maximizing the healthy pursuit of a physically active and healthy lifestyle.
WHAT ARE RISK FACTORS?
A health risk factor is anything that increases a person’s chances of getting a disease or other health-related condition.15 Risk factors are well established for many life-threatening conditions present in adults such as cardiovascular disease. But there is little public health focus on risk factors associated with MSKD, which is surprising given the massive burden MSKD have on our society.1,2,5 In this commentary the authors discuss risk factors that have been associated with the development of MSKD overall and discuss strategies that may help to manage these risk factors more effectively. Perhaps, if risk factors for MSKD are managed more effectively, the burden associated with MSKD will be reduced.
MSKD are multifactorial and a good understanding of the key risk factors and conditions associated with MSKD is important. While most MSK risk factor research has focused on MSK function or a singular injury, researchers now have demonstrated the multifactorial nature of MSKD and the specific risk factors associated with the overall development of MSKD in adults.16 For example, individuals with behavioral health needs are at greater risk for MSKD17,18 as are those who have had a recent MSK injury.16,19,20 A previous injury within the prior 12 months is a known strong risk factor,19 but also the magnitude of that injury16 as well as the self-perception of recovery16,20 from that injury are also independent risk factors that deserve consideration in an individual’s overall risk profile.
Recent research has shown that individuals with multiple risk factors are at increased risk for MSK injury16,21,22 and have reduced physical performance.21 Not surprisingly, there is a linear relationship between the number of risk factors and injury risk.16 The more risk factors that an individual has, the more likely they are to ultimately develop an MSKD. Therefore, it may be important to screen for MSKD risk factors, to consider the presence of multiple risk factors, and the combinations of these factors to establish everyone’s overall risk level. Screening can help to determine the most important domain of MSK health which should be prioritized and provide rationale and guidance for direct intervention for those at greatest risk. For example, it is well known that individuals with higher BMI are at greater risk for OA. But, simply sharing this with a patient and expecting changes in exercise and diet to address high BMI is not likely to be an effective strategy.23 Perhaps employing a screening process that prioritizes risk factors for MSK health, with a focus on the most prominent and modifiable areas could be helpful. When key risk factors are screened for and considered together, an appropriate migration strategy can be developed, in conjunction with the patient’s current rehabilitation program to enhance and promote overall MSK health.
RISK FACTORS ASSOCIATED WITH COMMON MSKD
Comprehensive review of the literature has resulted in the summation of the risk factors most closely associated with overall MSK health. These risk factors can be identified through the MSK screening process in clinical practice as routine annual wellness check-ups or throughout the course of rehabilitation. Like cardiovascular risk factors, MSK risk factors are interrelated suggesting that healthcare professionals must systematically evaluate the entire profile of an individual. For example, a previous ankle sprain injury where the ankle dorsiflexion ROM was not fully restored could potentially result in another ankle sprain or possibly an injury to the knee. Furthermore, reduced ankle mobility will have negative effects on functional movement (i.e. squatting, stepping, lunging) and dynamic balance which could limit the individual’s ability to be physically active, resulting in poor cardiovascular fitness, increased BMI, and suboptimal psychological status. Restricted ankle dorsiflexion does respond favorably to direct intervention and/or education when appropriately identified and administered. The following are key MSK risk factors, presented alphabetically.
Ankle Dorsiflexion ROM
Asymmetrical ankle dorsiflexion of at least 4 degrees has been identified as a significant risk factor for time loss injury in military and sport populations. Asymmetrical ankle dorsiflexion has been identified as a risk factor for future falls in elderly populations.16,24,25
Body Mass Index
High body mass index has been associated with increased risk of sustaining an injury in military and sport populations. High body mass index has also been identified as a significant risk factor in future osteoarthritis and total joint replacement.26–30
Cardiovascular Fitness
Decreased cardiovascular fitness has been identified as an independent risk factor for future time loss injury in military, sport populations, and elderly populations.16,30
Dynamic Balance
Impaired dynamic balance has been identified as a significant risk factor in future time loss injury for military and sport populations.16,24,31
Functional Movement Competency
Impaired functional movement (measured by the Functional Movement Screen and the Selective Functional Movement Assessment) has been identified as a significant risk factor in future time loss injury for military and sport populations.30,32–36
Muscle Strength
Decreased muscle strength has been identified as an independent risk factor to sustain a future injury in sport and elderly populations.10
Pain with Movement
Pain with movement was identified in three separate military populations as a significant risk factor in future time loss injury.16,24,30
Perceived Recovery
Perceived recovery as measured by the Single Assessment Numeric Evaluation (SANE) score following an injury was identified as an independent prospective risk factor for future injury. Individuals who report their SANE score following an injury at <92% were shown to be more likely to sustain a future time loss injury.16
Physical Activity
Low physical activity has been identified as a significant risk factor for the development of osteoarthritis and sustaining a fall in elderly populations.27
Previous Loss Time Injury
The presence of a previous time loss injury has been identified in multiple studies as an independent and robust risk factor. Additionally, the magnitude of the injury, as measured by the number of days missed, has also been identified as a risk factor for future injury.16,19,24,37
Psychological Status
Diagnosis of anxiety and/or depression has been identified as an independent significant risk factor in musculoskeletal pain or injury.17,18,38
CLINICAL MODEL
There is a need for a modern and innovative model to approach MSKD. The MSKD health problem is extremely complex requiring management with more than one tactic. However, the first step in addressing this large-scale problem is identifying known risk factors and providing individuals with awareness of the biggest limiting factors impacting their own MSK health.
Consideration of the number of risk factors present and the magnitude of each factor is contemplated in the overall care of the patient. With a good understanding of a patient’s current risk, a comprehensive rehabilitation plan can be executed to mitigate the impact that risk factors have on overall physical activity and function. This approach is a more systematic and comprehensive model to evaluate MSK health, rather than a purely pathoanatomical approach where treatment is dictated simply by current symptoms or medical diagnoses. In a recent study conducted in 18–45 year-old adults, the researchers captured multiple physical performance measures and known MSKD risk factors at time of discharge from rehabilitation for lower extremity or spine dysfunction.39 This entire sample of 469 subjects had been cleared to return to full activity by their healthcare professional. The researchers found that over 70% of the sample had at least five known MSKD risk factors at time of discharge and 44% had pain with global movements. This does not include the obvious previous injury that was an inclusion criterion for the study. In this case, local pain was managed well, but these data demonstrate the need to expand conventional rehabilitative care to include comprehensive risk factor management.39
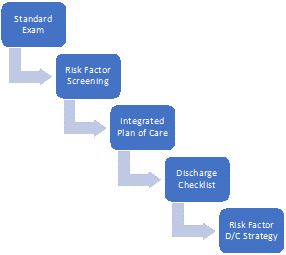
There are a variety of evidence-based approaches that are utilized by rehabilitation providers to directly address the pain and disability associated with a given MSK condition. It may seem overwhelming to add MSKD risk factor management to current models, but a commonsense approach that optimizes a standardized process is the key to establishing MSKD risk factor management into current rehabilitation practice. When the most prominent and modifiable risk factors are considered rather than each one individually, the process becomes attainable. It can be as simple as screening for functional movement40,41 (including presence of pain), ankle mobility42,43 and balance44,45 which is approximately a 15-minute investment. Risk factor screening can occur as part of the standard physical therapy examination or can be executed in the early phases of the rehab process. The timing of screening will be somewhat dependent on the acuity and nature of the primary condition the patient is being seen for. Ultimately, the plan of care should include intervention targeted at the most prominent risk factors as well as a discharge plan that addresses ongoing risk factor management. (Figure 1).
Figure 1. Risk Factor Management Flow Chart.
ADDRESSING RISK FACTORS
Evidence-based interventions, prescribed to address identified risk factors, can be integrated into the locally focused rehabilitation program, and built into the program progression. In a study by Schwarzkoph-Phifer et al46 that measured risk factor management during rehabilitation, it was demonstrated that with traditional interventions focused on manual therapy and therapeutic exercise, the number of risk factors present following the intervention period was significantly reduced with an average reduction of three risk factors. In another study by Huebner et. al. it was demonstrated that overall MSK risk category can change significantly from higher risk to lower risk with individualized interventions.47 A combination of manual therapies and therapeutic exercise has been shown to improved ROM and dynamic balance in subject with ankle dorsi-flexion restrictions.48–50 Individualized therapeutic exercise programs have been shown to significantly improve functional movement abilities when compared to control subjects,51,52 and dynamic and static balance has been shown to improve in multiple studies with a variety of interventions across different age groups.53,54
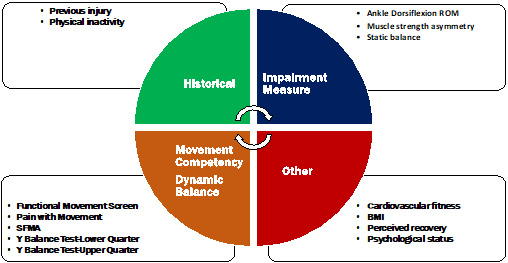
Awareness of the number of risk factors is also considered. Some individual factors are in and of themselves nonmodifiable, making it even more important to address the factors that are amenable to intervention, to reduce overall risk. Additionally, some patients may benefit from referral for professional help with areas such as behavioral health or to a training specialist for help with cardiovascular fitness and/or strength training. Organizing risk factors by category can help the clinician clarify which risk factors to intervene on and provides a risk factor profile to help understand each patient’s prognosis. (Figure 2).
Figure 2. Musculoskeletal Risk Factors by Category.
A thorough understanding of each patient’s individual risk profile at discharge time can help to instill confidence in the therapeutic relationship and serve to provide clear guidance to the patient of what they should be working on to maximize their MSK health and benefits gained from a physically active lifestyle. As clinicians become more comfortable with this full body, risk factor approach, it simply becomes how they practice rather than a disconnected portion of the program that is added on near the end.
CONCLUSION
MSKD are the leading contributors to disability worldwide and present a substantial burden to healthcare systems. Unlike other prevalent and disabling healthcare conditions, risk factors associated with MSKD are not commonly discussed or integrated into current medical practice or wellness programs. In this review the authors describe the most common MSKD risk factors, and it is suggested that addressing known risk factors for MSKD in rehabilitation may be an important factor moving forward to reduce the enormous and growing burden these disorders are having on society.
Conflicts of interest
Dr. Kiesel and Dr. Plisky report a relationship with Functional Movement Systems where they own stock. Dr. Arnold is a compensated instructor for Functional Movement Systems. The other authors report no potential conflicts of interest.
References
- Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Murray C. J., Vos T., Lozano R.., et al. 2012Lancet. 380:2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- What low back pain is and why we need to pay attention. Hartvigsen J., Hancock M. J., Kongsted A.., et al. 2018Lancet. 391:2356–2367. doi: 10.1016/S0140-6736(18)30480-X. [DOI] [PubMed] [Google Scholar]
- Musculoskeletal health conditions represent a global threat to healthy aging: a report for the 2015 world health organization world report on ageing and health. Briggs A. M., Cross M. J., Hoy D. G.., et al. 2016Gerontologist. 56 Suppl 2:S243–55. doi: 10.1093/geront/gnw002. [DOI] [PubMed] [Google Scholar]
- Global estimates of the need for rehabilitation based on the global burden of disease study 2019: a systematic analysis for the global burden of disease. Cieza A., Causey K., Kamenov K.., et al. 2021Lancet. 396:2006–2017. doi: 10.1016/S0140-6736(20)32340-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United states bone and joint initiative . The burden of musculoskeletal diseases in the United States (BMUS) Rosemont, IL; [Google Scholar]
- The burden of musculoskeletal diseases in the United States. Yelin E., Weinstein S., King T. 2016Sem Arthritis Rheumatism. 46:259–260. doi: 10.1016/j.semarthrit.2016.07.013. [DOI] [PubMed] [Google Scholar]
- Musculoskeletal Australia . Making the invisible visible; Australians share the impact of musculoskeletal conditions on their lives. Baseline survey report; [Google Scholar]
- Systematic review of low back pain cost of illness studies in the United States and internationally. Dagenais S., Caro J., Haldeman S. A. 2008Spine J. 8:8–20. doi: 10.1016/j.spinee.2007.10.005. [DOI] [PubMed] [Google Scholar]
- Understanding physical activity promotion in physiotherapy practice: A qualitative study. Lowe A., Littlewood C., McLean S. 2018Musculoskel Sci Pract. 35:1–7. doi: 10.1016/j.msksp.2018.01.009. [DOI] [PubMed] [Google Scholar]
- World health organization 2020 guidelines on physical activity and sedentary behavior. Bull F. C., Al-Ansari S. S., Biddle S.., et al. 2020Br J Sports Med. 54:1451–1462. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Role of inactivity in chronic diseases: evolutionary insight and pathophysiological mechanisms. Booth F. W., Roberts C. K., Thyfault J. P.., et al. 2017Physiol. Rev. 97:1351–1402. doi: 10.1152/physrev.00019.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Physical activity promotion: moving from talking the talk to walking the walk. Rethorn Z. D., Covington J. K., Cook C. E.., et al. 2022J Orthop Sports Phys Ther. 52:236–242. doi: 10.2519/jospt.2022.10859. [DOI] [PubMed] [Google Scholar]
- Metabolic syndrome. Samson S. L., Garber A. J. 2014Endocrinol Metab Clin North Am. 43:1–23. doi: 10.1016/j.ecl.2013.09.009. [DOI] [PubMed] [Google Scholar]
- Inadequate physical activity and health care expenditures in the United States. Carlson S. A., Fulton J. E., Pratt M.., et al. 2015Prog Cardiovasc Dis. 57:315–323. doi: 10.1016/j.pcad.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The role of health risk factors and disease on worker productivity. Burton W. N., Conti D. J., Chen C. Y.., et al. 1999J Occup Environ Med. 41:863–877. doi: 10.1097/00043764-199910000-00007. [DOI] [PubMed] [Google Scholar]
- identification of risk factors prospectively associated with musculoskeletal injury in a warrior athlete population. Teyhen D. S., Shaffer S. W., Butler R. J.., et al. 2020Sports Health. 12:564–572. doi: 10.1177/1941738120902991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association of depression and anxiety alone and in combination with chronic musculoskeletal pain in primary care patients. Bair M. J., Wu J., Damush T. M.., et al. 2008Psychosom Med. 70:890–897. doi: 10.1097/PSY.0b013e318185c510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reciprocal relationship between pain and depression: a 12-month longitudinal analysis in primary care. Kroenke K., Wu J., Bair M. J.., et al. 2011J Pain. 12:964–973. doi: 10.1016/j.jpain.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Is subsequent lower limb injury associated with previous injury? A systematic review and meta-analysis. Toohey L. A., Drew M. K., Cook J. L.., et al. 2017Br J Sports Med. 51:1670–1678. doi: 10.1136/bjsports-2017-097500. [DOI] [PubMed] [Google Scholar]
- injury risk is increased by changes in perceived recovery of team sport players. Does H.T., van der D., Brink M.S.., et al. 2017Clin J Sport Med. 27:46–51. doi: 10.1097/JSM.0000000000000306. [DOI] [PubMed] [Google Scholar]
- Association of physical inactivity, weight, smoking, and prior injury on physical performance in a military setting. Teyhen D. S., Shaffer S. W., Butler R. J.., et al. 2016J Athl Train. 51:866–875. doi: 10.4085/1062-6050-51.6.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field-expedient screening and injury risk algorithm categories as predictors of noncontact lower extremity injury. Lehr M. E., Plisky P. J., Butler R. J.., et al. 2013Scand J Med Sci Sports. 23:e225–232. doi: 10.1111/sms.12062. [DOI] [PubMed] [Google Scholar]
- Determinants of adherence to lifestyle intervention in adults with obesity: a systematic review. Burgess E., Hassmén P., Pumpa K. 2017Clin Obes. 7:123–135. doi: 10.1111/cob.12183. [DOI] [PubMed] [Google Scholar]
- What risk factors are associated with musculoskeletal injury in us army rangers? a prospective prognostic study. Teyhen D. S., Shaffer S. W., Butler R. J.., et al. 2015Clin Ortho Relat Res. 473:2948–2958. doi: 10.1007/s11999-015-4342-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ankle dorsiflexion delay can predict falls in the elderly. Kemoun G., Thoumie P., Boisson D.., et al. 2002J Rehabil Med. 34:278–283. doi: 10.1080/165019702760390374. [DOI] [PubMed] [Google Scholar]
- Prognostic factors for progression of clinical osteoarthritis of the knee: a systematic review of observational studies. Bastick A. N., Runhaar J., Belo J. N.., et al. 2015Arthritis Res Ther. 17:152. doi: 10.1186/s13075-015-0670-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patient characteristics that predict progression of knee osteoarthritis: a systematic review of prognostic studies. Chapple C. M., Nicholson H., Baxter G. D.., et al. 2011Arthritis Care Res. 63:1115–1125. doi: 10.1002/acr.20492. [DOI] [PubMed] [Google Scholar]
- Change in body mass index during middle age affects risk of total knee arthoplasty due to osteoarthritis: a 19-year prospective study of 1003 women. Nicholls A. S., Kiran A., Javaid M. K.., et al. 2012Knee. 19:316–319. doi: 10.1016/j.knee.2011.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association between overweight and obesity and risk of clinically diagnosed knee, hip, and hand osteoarthritis: a population-based cohort study. Reyes C., Leyland K. M., Peat G.., et al. 2016Arthritis. 68:1869–1875. doi: 10.1002/art.39707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Much work remains to reach consensus on musculoskeletal injury risk in military service members: A systematic review with meta-analysis. Rhon D. I., Molloy J. M., Monnier A.., et al. 2022Eur J Sport Sci. 1:16–34. doi: 10.1080/17461391.2021.1931464. [DOI] [PubMed] [Google Scholar]
- Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. Plisky P. J., Rauh M. J., Kaminski T. W.., et al. 2006J. Orthop Sports Phys Ther. 36:911–919. doi: 10.2519/jospt.2006.2244. [DOI] [PubMed] [Google Scholar]
- Relationship of movement screens with past shoulder or elbow surgeries in collegiate baseball players. Busch A. M., Clifton D. R., Onate J. A. 2018Int J Sports Phys Ther. 13:1008–1014. doi: 10.26603/ijspt20181008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prediction of injury by limited and asymmetrical fundamental movement patterns in american football players. Kiesel K. B., Butler R. J., Plisky P. J. 2014J Sport Rehabil. 23:88–94. doi: 10.1123/JSR.2012-0130. [DOI] [PubMed] [Google Scholar]
- The association between the functional movement screen outcome and the incidence of musculoskeletal injuries: A systematic review with meta-analysis. Bunn P., Rodrigues A.I., da Silva E.B. 2019Phys Ther Sport. 35:146–158. doi: 10.1016/j.ptsp.2018.11.011. [DOI] [PubMed] [Google Scholar]
- Regional interdependence: a musculoskeletal examination model whose time has come. Wainner R. S., Whitman J. M., Cleland J. A.., et al. 2007J. Orthop Sports Phys Ther. 37:658–660. doi: 10.2519/jospt.2007.0110. [DOI] [PubMed] [Google Scholar]
- A regional interdependence model of musculoskeletal dysfunction: research, mechanisms, and clinical implications. Sueki D. G., Cleland J. A., Wainner R. S. 2013J Man Manip Ther. 21:90–102. doi: 10.1179/2042618612Y.0000000027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Which determinants predict tibiofemoral and patellofemoral osteoarthritis after anterior cruciate ligament injury? A systematic review. van Meer B. L., Meuffels D. E., van Eijsden W. A.., et al. 2015Br J Sports Med. 49:975–983. doi: 10.1136/bjsports-2013-093258. [DOI] [PubMed] [Google Scholar]
- Investigating the prevalence of anxiety and depression in people living with patellofemoral pain in the UK: the Dep-Pf Study. Wride J., Bannigan K. 2019Scand J Pain. 19:375–382. doi: 10.1515/sjpain-2018-0347. [DOI] [PubMed] [Google Scholar]
- Recovery, rehabilitation, and return to full duty in a military population after a recent injury: differences between lower-extremity and spine injuries. Rhon D. I., Teyhen D. S., Kiesel K. B.., et al. 2022Arthrosc Sports Med Rehabil. 4:e17–e27. doi: 10.1016/j.asmr.2021.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Intra- and inter-rater reliability of the Selective Functional Movement Assessment (SFMA) Glaws K. R., Juneau C. M., Becker L. C.., et al. 2014Int J Sports Phys Ther. 9:195–207. [PMC free article] [PubMed] [Google Scholar]
- Predicting subsequent injury after being cleared to return to work from initial lumbar or lower extremity injury. Rhon D. I., Plisky P. J., Kiesel K. B.., et al. 2023Med Sci Sports Exerc. 55:2115–2122. doi: 10.1249/MSS.0000000000003257. [DOI] [PubMed] [Google Scholar]
- The reliability and criterion validity of a novel dorsiflexion range of motion screen. Gourlay J., Bullock G., Weaver A.., et al. 2020Athl Train Sports Health Care. 12:40–44. doi: 10.3928/19425864-20190214-02. [DOI] [Google Scholar]
- The dorsiflexion range of motion screen: a validation study. Plisky P. J., Bulluck G., Garner M. B.., et al. 2021Int J Sports Phys Ther. 16:306–311. doi: 10.26603/001c.21253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Self-movement screening using the symmio application is reliable and valid for identifying musculoskeletal risk factors. Matsel K., Kirsch J., Netelbeek T.., et al. 2023Int J Sports Phys Ther. 18:439–449. doi: 10.26603/001c.73319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Systematic review and meta-analysis of the y-balance test lower quarter: reliability, discriminant validity, and predictive validity. Plisky P. J., Schwartkopf-Phifer K., Huebner B.., et al. 2021Int J Sports Phys Ther. 16:1190–1209. doi: 10.26603/001c.27634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The effect of one-on-one intervention in athletes with multiple risk factors for injury. Schwartzkopf-Phifer K., English R. A., Mattacola C. G.., et al. 2019Int J Sports Phys Ther. 14:384–402. doi: 10.26603/ijspt20190384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Can injury risk category be changed in athletes? an analysis of an injury prevention system. Huebner B. J., Plisky P. J., Kiesel K. B.., et al. 2019Int J Sports Phys Ther. 14:127–134. doi: 10.26603/ijspt20190127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ankle dorsiflexion range of motion influences dynamic balance in individuals with chronic ankle instability. Basnett C. R., Hanish M. J., Wheeler T. J.., et al. 2013Int J Sports Phys Ther. 8:121–128. [PMC free article] [PubMed] [Google Scholar]
- Comparison of compressive myofascial release and the graston technique for improving ankle-dorsiflexion range of motion. Stanek J., Sullivan T., Davis S. 2018J Athl Train. 53:160–167. doi: 10.4085/1062-6050-386-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Effects of joint mobilization on chronic ankle instability: a randomized controlled trial. Cruz-Díaz D., Vega L. R., Osuna-Pérez M. C.., et al. 2015Disabil Rehabil. 37:601–610. doi: 10.3109/09638288.2014.935877. [DOI] [PubMed] [Google Scholar]
- Functional movement test scores improve following a standardized off-season intervention program in professional football players. Kiesel K. B., Plisky P. J., Butler R. J. 2011Scand J Med Sci Sports. 21:287–292. doi: 10.1111/j.1600-0838.2009.01038.x. [DOI] [PubMed] [Google Scholar]
- The effect of an intervention program on functional movement screen test scores in mixed martial arts athletes. Bodden J. G., Needham R. A., Chockalingam N. 2015J Strength Cond Res. 29:219–225. doi: 10.1519/JSC.0b013e3182a480bf. [DOI] [PubMed] [Google Scholar]
- Resistance training and executive functions: a 12-month randomized controlled trial. Liu-Ambrose T., Nagamatsu L. S., Graf P.., et al. 2010Arch Intern Med. 170:170–178. doi: 10.1001/archinternmed.2009.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Using the star excursion balance test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. Gribble P. A., Hertel J., Plisky P. J. 2012J Athl Train. 47:339–357. doi: 10.4085/1062-6050-47.3.08. [DOI] [PMC free article] [PubMed] [Google Scholar]


