Abstract
STUDY QUESTION
What is the prevalence of occupational stress, somatization, and burnout reported by UK and US, embryologists and the impact of work conditions on these well-being outcomes?
SUMMARY ANSWER
Surveyed UK and US embryologists reported moderate perceived stress, low somatic symptom severity, high levels of burnout, and overall stressful work conditions, but with differences that could be due to country-specific occupational and employment characteristics.
WHAT IS KNOWN ALREADY?
Spanish, UK, US, and international surveys have identified high levels of occupational stress, somatization, burnout, and occupational health issues among embryologists. These issues have been attributed to embryologists’ occupational challenges and work conditions.
STUDY DESIGN, SIZE, DURATION
A cross-sectional web-based survey was sent to 253 embryologists working in UK ART/IVF clinics and 487 embryologists working in US ART/IVF clinics.
PARTICIPANTS/MATERIALS, SETTING, METHODS
Participants self-reported their stress levels, somatization, burnout, and work conditions. Proportions across the Perceived Stress Scale (PSS), Patient Health Questionnaire (PHQ-15), Maslach Burnout Inventory-General Survey (MBI-GS), a single-item work unit grade (A–F), and customized occupational and sociodemographic questionnaires were calculated using descriptive statistics. Welch’s t-test was utilized to compare PSS and PHQ-15 scores between groups. Risk ratios were calculated using log-binomial regression for all models except for levels of anxiety related to performing cryostorage tasks, for which Poisson models were used.
MAIN RESULTS AND THE ROLE OF CHANCE
In total, 50.6% (128) of the embryologists in the UK and 50.1% (244) in the US completed the survey. Both groups self-reported moderate PSS and low PHQ-15 scores, although fewer UK embryologists scored high on the MBI cynicism dimension than their US colleagues (43% UK vs 60% US embryologists, P < 0.05). The UK and US embryologists did not differ on the MBI exhaustion dimension with both scoring high for exhaustion (59% UK vs 62% US). Although 81% and 80% of UK and US embryologists, respectively, reported working overtime, more embryologists in the UK reported being adequately compensated. Increasing levels of anxiety-related to cryostorage showed a dose-dependent increased risk of burnout on at least two MBI-GS dimensions only in the UK group, and, a dose-dependent likelihood of higher PSS and PHQ-15 scores in both groups.
LIMITATIONS, REASONS FOR CAUTION
Since the two groups were surveyed 9 months apart and were self-reporting, the study is limited by the differences in responsibilities, scheduling, and workload specific to the time of year.
WIDER IMPLICATIONS OF THE FINDINGS
Work-related health issues and occupational challenges shared by UK and US embryologists could be addressed by organizational enhancements and technology. Lower levels of stress and burnout among UK embryologists might be due to the HFEA-provided structure/certainty.
STUDY FUNDING/COMPETING INTEREST(S)
This study was supported without any external funding by TMRW Life Sciences Inc., which is developing and commercializing an automated platform for embryology. M.G.C. and M.S.L. are full-time employees and stockholders/shareholders with TMRW Life Sciences, and A.M. of Novavax, Inc. was an employee of TMRW Life Sciences. G.P. is a consultant for TMRW Life Sciences. The remaining authors declare no conflict of interest.
TRIAL REGISTRATION NUMBER
Keywords: stress, somatization, burnout, anxiety, ART/IVF, work conditions
Introduction
Clinical embryologists are exacting, highly trained members of ART/IVF clinics who carry out the diagnosis and treatment of infertility by manipulating and preserving fresh and frozen reproductive specimens, testing them for genetic and infectious diseases, maintaining and managing embryology laboratories and cryostorage facilities, and, ultimately, helping patients fulfill their family-building goals (Practice Committee of the American Society for Reproductive Medicine, Practice Committee of the Society for Assisted Reproductive Technology, and Practice Committee of the Society of Reproductive Biologists and Technologists, 2014, 2021). Work-related stress, burnout, and anxiety are known to decrease work performance (Ruotsalainen et al., 2014). The negative effects of work conditions and work-related problems on the emotional and physical well-being of workers became a subject of scientific interest in the mid-1970s (Freudenberger, 1974; Punnett and Wegman, 2004), culminating in the development of the Maslach Burnout Inventory (MBI; Maslach and Jackson, 1981). Combined with other reliable tools measuring work-related stress, somatization, fatigue, and other psychological and physical disorders among workers employed in various fields, the MBI has become a gold standard for measuring burnout. However, more work needs to be done to define burnout (Maslach et al., 2001; Guseva Canu et al., 2021; Schaufeli, 2021, 2023), and each field needs a customized toolkit to assess occupational challenges and health issues specific to its workers (Frone and Tidwell, 2015).
The first study of occupational health issues among embryologists was conducted in Spain via an online health questionnaire distributed among members of the Spanish Association of Clinical Embryologists (López-Lería et al., 2014). Several other groups have studied occupational health issues among embryologists in the UK (Priddle et al., 2022; Murphy et al., 2023a, 2023d), the US (Murphy et al., 2022a, 2023a, 2023b, 2023c), and an international cohort of embryologists from 85 countries (Palmer et al., 2022) using different survey toolkits.
High levels of occupational stress, somatization, and burnout in addition to other occupational health issues among embryologists have been reported in several studies (López-Lería et al., 2014; Collins et al., 2022; Murphy et al., 2022a, 2023a, 2023b, 2023c, 2023d; Palmer et al., 2022; Priddle et al., 2022) and attributed to stressful work conditions in the embryology laboratory. Stressors include the lack of room for error since mishandling reproductive specimens can lead to devastating consequences for the patient(s) and legal implications for the providers (Letterie, 2017; Moutos et al., 2019; Letterie and Fox, 2020; Murphy et al., 2022b; Applebaum et al., 2023; Klipstein and Daar, 2023). Additionally, embryologists face a heavy workload with long hours and frequent holiday/weekend work (Murphy et al., 2022a, 2023a), performing repetitive and fatiguing tasks using manual procedures (López-Lería et al., 2014; Collins et al., 2022; Priddle et al., 2022), and an overwhelming amount of paperwork (López-Lería et al., 2014; Go, 2015; Murphy et al., 2022a, 2023a, 2023b, 2023c, 2023d).
However, there is still a significant knowledge gap among clinical laboratory professionals (Thompson et al., 2003; Lorusso et al., 2007; Fritzsche et al., 2012). This includes embryologists, and the occupational challenges and health issues arising from their work (López-Lería et al., 2014; Campbell et al., 2022; Collins et al., 2022; Murphy et al., 2022a, 2023a, 2023b, 2023c, 2023d; Palmer et al., 2022; Priddle et al., 2022), while the same issues among other healthcare professionals have been the subject of numerous studies (Boivin et al., 2017; Dyrbye et al., 2018, 2019; Tawfik et al., 2018; West et al., 2018; Caruso et al., 2019; Trockel et al., 2020; Brady et al., 2021, 2022; Shanafelt, 2021; Rowe et al., 2022; Shanafelt et al., 2022, 2023b, 2023c; Longo et al., 2023; Makowski et al., 2023; Marchalik and Shanafelt, 2023; Sinsky et al., 2023). Moreover, despite their indispensable role in fertility treatments and patient outcomes, embryologists are not generally considered healthcare professionals by regulatory bodies, and their occupational concerns and needs are often overlooked by their employers (Kovačič et al., 2015; ESHRE Working Group on Embryologist Training Analysis et al., 2023). The scarcity of real-life evidence and the lack of understanding about embryologists’ occupational challenges by their employers may contribute to stress, somatization, and burnout, which can have short- and long-term negative consequences for embryologists, their work, and the clinics (Maslach et al., 2001; Guseva Canu et al., 2021; Schaufeli, 2021, 2023).
Compounding this issue, embryologists in different countries and different states within the US may operate under different legal and regulatory conditions, which may result in varied access to resources and can either alleviate or exacerbate their occupational challenges and health issues. Therefore, studies carried out in a single country might be highly specific to that country, and international studies that cover multiple countries might not account for the local characteristics of each participant’s work conditions.
The present study seeks to compare stress, somatization, and burnout among embryologists in the UK and the US. Recently, cryostorage expansion has increased the demands on embryologists (Alikani et al., 2014; Go, 2015, 2019; Alikani, 2018; Alikani and Parmegiani, 2018). The current workflow and organizational characteristics of the embryology laboratories are investigated to determine if there is an association with embryologists’ physical and psychological health. Additionally, the relationship between anxiety associated with specific workflows, such as cryostorage, on embryologists’ stress, somatization, and burnout is determined. The results of this study will identify necessary areas of improvement in the embryology laboratory that could increase patient care by alleviating embryologist stress, somatization, and burnout.
Materials and methods
Study design and participants
This study used data from the Embryologist Fatigue Study (EFS), carried out as a cross-sectional web-based survey emailed to 253 embryologists working at HFEA-licensed UK (Murphy et al., 2023d) ART/IVF public and private clinics and 487 embryologists working at College of American Pathologists (CAP) accredited and/or The Joint Commission (TJC) certified or non-accredited US clinics (Murphy et al., 2022a). Responses were collected for two weeks in January 2023 and April 2022, respectively. This data was collected using a customized survey toolkit where respondents were asked to self-report their stress levels, physical health status, burnout, and work conditions that they perceived as related to their occupation as an embryologist. The survey toolkit used validated standardized psychological and somatic symptom assessment tools and customized sociodemographic and occupational questionnaires. The email list(s) were compiled from the authors’ known contacts in the field of Reproductive Health, and by actively gathering contacts in the years preceding the study by other members of the authors’ organizations. The list is periodically updated to maintain as accurate contact information as possible.
All survey participants were required to be practicing embryologists at different stages of their careers and to complete all parts of the survey. No other exclusion/inclusion criteria were applied to the study groups.
The studies were registered on ClinicalTrials.gov (US EFS: NCT05326802; and UK EFS: NCT05708963).
Sample characteristics
Sociodemographic information regarding age, gender, education, years of experience, and other key descriptive characteristics of the survey participants was collected using a customized sociodemographic questionnaire.
Symptoms of stress, somatization, and burnout
Embryologists self-reported perceived stress using the standardized validated Perceived Stress Scale (PSS)-10 (Cohen et al., 1983). Items are scored on a 5-point scale from 0 (‘never’) to 4 (‘often’), with some inversion. Total scores of 0–13 are considered low perceived stress, 14–26 are moderate stress, and 27–40 are high stress.
Somatic symptom severity was measured using the standardized validated 15-question Patient Health Questionnaire (PHQ-15) (Kroenke et al., 2002). Items are scored on a 3-point scale of 0 (‘not bothered at all’), 1 (‘bothered a little’), and 2 (‘bothered a lot’). Somatization is categorized from total scores as minimal (0–4), low (5–9), medium (10–14), and high (15–30).
Burnout was assessed using the MBI-GS (Mind Garden™, Menlo Park, CA), and responses were scored according to the MBI Manual 3rd edition (Maslach et al., 1996), as described in López-Lería et al. (2014). The MBI-GS assesses burnout on three dimensions: Exhaustion, Cynicism, and Professional Efficacy. Results on these dimensions are categorized as low, medium, or high burnout (Schaufeli et al., 1996; López-Lería et al., 2014; see Results below and Corresponding Supplementary Figures). High burnout was defined as having burnout scores in the third tertile in at least two of the three burnout dimensions.
Working conditions
Embryologists self-reported their satisfaction with their workplace culture, careers and future career outlook, job fulfillment, scheduling and overtime concerns, and burdens associated with technical tasks specific to their occupation in a customized occupational questionnaire. A ‘Technology & The Lab’ section consisted of five items (e.g. ‘Do any of the current cryostorage processes cause you anxiety?’), ‘Career Outlook’ eight items (e.g. ‘How likely are you to recommend a career in embryology to a new college graduate or a person looking to change career paths?’), ‘Physical and Mental Stress Levels’ eight items (e.g. ‘How often do you experience stress when depositing and retrieving oocytes and embryos from cryostorage?’), and the ‘Scheduling/Staffing & Time Off’ nine items (e.g. ‘How many hours of overtime do you typically work per week? Is overtime voluntary or mandatory?’). Several items included questions that required ‘Yes/No’, ‘Yes/No/Maybe/I don’t know’, or ‘Very Often/Often/Rarely/Never’ pre-formulated multiple choice, and open-ended answers. Items that asked respondents to score their career satisfaction and outlook, job fulfillment, and stress levels associated with performing cryopreservation tasks, such as freezing/thawing reproductive specimens and handling tanks, were scored on a 10-point Likert-type scale ranging from 1 (‘lowest/never/least’) to 10 (‘highest/always/most’). Respondents were asked to rank their levels of anxiety related to performing cryostorage tasks, from freezing/thawing reproductive specimens to handling cryotanks and managing cryoinventory, on a 5-point Likert-type scale ranging from 1 (‘No Anxiety) to 5 (‘Constant Anxiety’).
Statistics
Descriptive statistics for stress, somatization, burnout, and sociodemographic characteristics were presented as the mean ± SD or as count and proportion. Mean differences between groups within each study population were compared using Welch’s t-test. Two independent population proportions were compared using the Z-test.
Log-binomial models were used to estimate the unadjusted and adjusted risk ratio (RR) and 95% CI of having high levels of burnout associated with various characteristics of the work environment. Linear models were used to estimate the adjusted change and 95% CI in PSS and PHQ-15 scores associated with various characteristics of the work environment. All models were adjusted for years of experience as an embryologist, full vs part-time work, and having vs not having a doctoral degree, as covariates. All analyses were conducted with SAS® 9.4 Software (SAS Institute, Cary, NC).
Ethics
The US survey was reviewed by an IRB (Pro00062375, Center for IRB Intelligence (CIRBI) Platform, Advarra, Columbia, MD). The determination was that the study did not require IRB oversight. The UK survey was determined to be exempt from an NHS Research Ethics Committee (REC) review by using the ‘Do I need NHS REC review?’ tool (NHS Health Research Authority, https://www.hra-decisiontools.org.uk/ethics/index.html).
The participants in both groups provided their informed consent prior to completing the survey. Participants in the US and the UK received an Amazon gift card with a value of $25 and £25, respectively, upon completion of the entire survey.
Results
Sample description
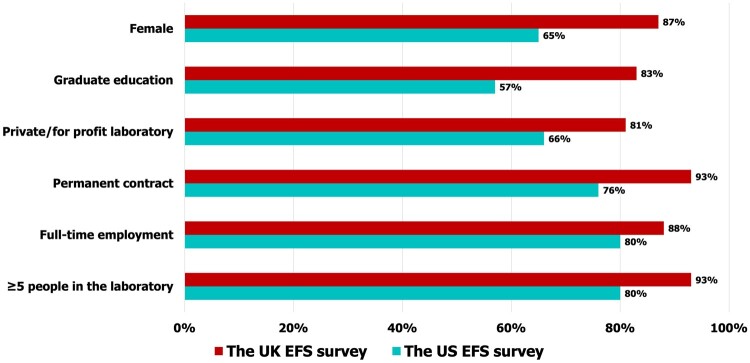
In total, 50.6% (128) of the embryologists in the UK and 50.1% (244) in the US completed the survey. The UK survey participants were, on average, 34.4 years old compared to their US colleagues whose mean age was 40.4 years, and although not statistically significant, more UK participants were female (87% UK and 65% US). Figure 1 compares the education and key employment characteristics of UK and US participants. (For sociodemographic data, see Supplementary Fig. S1; for PSS and PHQ-15 values, see Supplementary Figs S2 (UK) and S3 (US)).
Figure 1.
Sociodemographic characteristics and employment characteristics of embryologists working in the HFEA-licensed UK clinics and CAP-accredited and/or TJC-certified or non-accredited US public and private ART/IVF clinics. ART/IVF, assisted reproductive technology/in vitro fertilization; CAP, College of American Pathologists; HFEA, Human Fertilisation & Embryology Authority; TJC, The Joint Commission.
Self-reported stress, somatization, and burnout
There was no difference between the two countries for the self-reported moderate PSS stress scores, but embryologists in the UK scored slightly lower on PHQ-15 than their colleagues in the US (P = 0.04). For a detailed comparison of responses to each question in PSS-10, see Supplementary Figs S4 (UK vs US), S5 (UK), and S6 (US), and in PHQ-15, Supplementary Figs S7 (UK vs US), S8 (UK), and S9 (US).
The MBI showed high levels of burnout on the exhaustion dimension in both groups (59% UK vs 62% US embryologists, P = 0.27). Fewer UK embryologists scored high on the cynicism (43% UK vs 60% US embryologists, P ≤ 0.05) and professional efficacy (15% UK vs 28% US embryologists, P ≤ 0.05) MBI dimensions than their US colleagues (Supplementary Figs S10 (UK vs US), S11 (UK), and S12 (US) and Supplementary Data File S1).
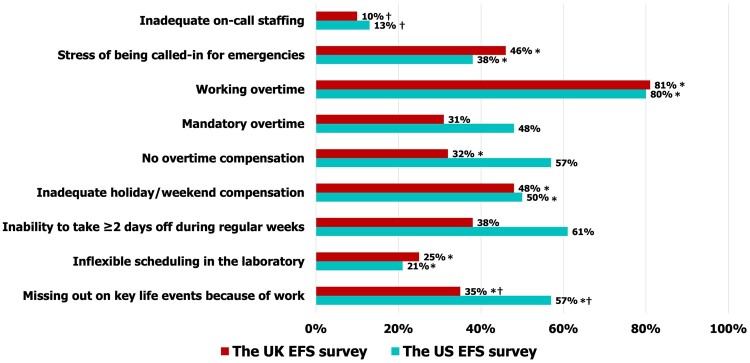
Work conditions
Of embryologists in the UK survey, 83% had a graduate degree compared to 57% of their colleagues in the US survey, and 93% of UK embryologists worked on a permanent contract basis compared with 76% of their colleagues in the US. Of the embryologists in the UK survey, 88% were employed on a full-time basis compared to 80% of their US colleagues, and 6% of the UK embryologists worked for corporate employers vs 14% of their US colleagues. Furthermore, 93% of the surveyed UK embryologists worked in laboratories with ≥5 persons (considered as adequately staffed; Alikani et al., 2014; Veiga et al., 2022) compared to 80% of the US embryologists (Fig. 1). When comparing organizational characteristics, although a similar number of participants in both groups reported working overtime (81% of UK and 80% of US embryologists, P = 0.63), a smaller proportion of UK embryologists reported being not compensated for overtime (P ≤ 0.05), not being able to take off 2 or more consecutive days during regular weeks (P ≤ 0.05), and missing out on key life events due to work (P ≤ 0.05) compared to their US colleagues (Fig. 2; Supplementary Figs S13 and S14 (UK) and S15 and S16 (US)).
Figure 2.
Employment characteristics and work conditions in the embryology laboratory reported by participants of the UK and US surveys. *, a statistically significant increased risk of burnout in at least two MBI domains associated with employment characteristics/work conditions; †, a statistically significant increase in PSS and PHQ-15 associated with employment characteristics/work conditions. MBI, Maslach Burnout Inventory; PHQ-15, a 15-question Patient Health Questionnaire; PSS, Perceived Stress Scale.
Association of work conditions and anxiety with stress, somatization, and burnout
In both the UK and the US results/studies, there were significantly greater PSS stress scores associated with inadequate staffing (4.66, 95% CI: 2.42–6.90 and 3.09, 95% CI: 1.47–4.72, respectively) and ever-missing life events due to work (4.08, 95% CI: 1.79–6.38, and 3.71, 95% CI: 2.02–5.41, respectively). In the US results, higher PSS scores were also significantly associated with anxiety related to being on-call (2.51, 95% CI: 1.06–3.95) and having inflexible scheduling (2.93, 95% CI: 1.55–4.30) (Supplementary Table S1). Regarding PHQ-15 scores, in both groups, significantly higher PHQ-15 scores were associated with inadequate staffing (1.96, 95% CI: 0.17–3.76, and 2.34, 95% CI: 0.83–3.85, respectively) and missing out on key life events due to work (2.85, 95% CI: 1.08–4.61, and 3.36, 95% CI: 1.80–4.92, respectively). In the US, inflexible scheduling was also associated with higher PHQ-15 scores (1.59, 95% CI: 0.30–2.88) (Supplementary Table S1).
In both the UK and the US studies, the risk of having high levels of burnout in at least two dimensions was significantly associated with anxiety related to being on-call (aRR: 1.62, 95% CI: 1.13–2.31, and aRR: 1.32, 95% CI: 1.13–1.54, respectively), inflexible scheduling (aRR: 1.49, 95% CI: 1.09–2.04, and aRR: 1.21, 95% CI: 1.02–1.43, respectively), and missing out on key life events due to work (aRR: 1.97, 95% CI: 1.36–2.85, and aRR: 1.58, 95% CI: 1.17–2.14, respectively). In the UK results, the risk of burnout was significantly associated with working overtime (aRR: 1.82, 95% CI: 1.01–3.29) and inadequate evening and weekend compensation (aRR: 1.64, 95% CI: 1.04–2.61). In the US results, the risk of burnout was significantly associated with inadequate on-call staffing (aRR: 1.63, 95% CI: 1.22–2.17) and mandatory overtime (aRR: 1.22, 95% CI: 1.02–1.47) (Supplementary Table S2).
Effects of specific cryostorage-related anxiety levels on perceived stress, somatization, and burnout
Half of the respondents in both study groups reported anxiety related to cryostorage (data not shown). While there was a difference in the proportions of UK and US embryologists reporting constant, high, and moderate levels of cryostorage-related anxiety, only the difference in the proportions of those reporting constant anxiety was statistically significant (P ≤ 0.05; Supplementary Figs S17 (UK) and S18 (US) and Supplementary Data File S1). Only the UK survey respondents self-reported a dose-dependent anxiety-related clinically significant increased risk of burnout on at least two MBI-GS dimensions (Table 1).
Table 1.
Effects of cryostorage-related anxiety levels on burnout.
| Cryostorage-related anxiety levels | The UK survey |
The US survey |
||
|---|---|---|---|---|
| Unadjusted RR (95% CI) | Adjusted* aRR (95% CI) | Unadjusted RR (95% CI) | Adjusted* aRR (95% CI) | |
| None | Ref | Ref | Ref | Ref |
| Mild | 1.23 (0.53–2.86) | 1.19 (0.51–2.82) | 1.69 (0.99–2.89) | 1.70 (1.02–2.83) |
| Moderate | 1.51 (0.64–3.58) | 1.38 (0.56–3.38) | 2.10 (1.24–3.54) | 2.09 (1.26–3.46) |
| High | 2.22 (0.93–5.28) | 2.13 (0.87–5.22) | 1.33 (0.75–2.36) | 1.57 (0.90–2.75) |
| Constant | 2.57 (0.67–9.94) | 2.64 (0.68–10.3) | 1.51 (0.81–2.80) | 1.69 (0.95–3.02) |
Cryostorage-related anxiety levels showed a clinically significant dose-dependent increased risk of burnout on at least two MBI-GS dimensions in the UK survey participants.
Adjusted for years as an embryologist, full-time vs part-time/per-diem working status, and doctorate-level education. Bold denotes a statistically significant dose-dependent effect of cryostorage-related anxiety on burnout.
PSS scores also significantly increased with the amount of anxiety related to cryostorage; larger increases in scores were observed in the UK results (range: 3.89 [95% CI: 0.85–6.94] for mild anxiety to 18.9 [95% CI: 12.2–25.7] for constant anxiety) compared to the US results (range: 2.49 [95% CI: 0.02–4.97] for mild anxiety to 6.44 [95% CI: 3.28–9.60] for constant anxiety). In both the UK and US groups, cryostorage-related anxiety was associated with higher PHQ-15 scores (UK range: 3.25 [95% CI: 0.57–5.92] for mild anxiety to 7.76 [95% CI: 1.83–13.7] for constant anxiety; US range: 1.96 [95% CI: −0.34 to 4.25] for mild anxiety to 5.17 [95% CI: 2.24–8.11] for constant anxiety, respectively). However, the association with mild anxiety did not reach statistical significance for the US respondents (Table 2).
Table 2.
Effects of cryostorage-related anxiety on perceived stress and somatic symptom severity.
| Cryostorage-related anxiety levels | The UK survey |
The US survey |
||
|---|---|---|---|---|
| PSS change (95% CI) | PHQ-15 change (95% CI) | PSS change (95% CI) | PHQ-15 change (95% CI) | |
| None | Ref | Ref | Ref | Ref |
| Mild | 3.89 (0.85–6.94) | 3.25 (0.57–5.92) | 2.49 (0.02–4.97) | 1.96 (−0.34 to 4.25) |
| Moderate | 7.60 (4.29–10.9) | 5.25 (2.35–8.16) | 5.73 (3.23–8.26) | 4.02 (1.70–6.34) |
| High | 10.7 (7.15–14.2) | 5.48 (2.37–8.59) | 5.24 (2.57–7.91) | 5.43 (2.96–7.91) |
| Constant | 18.9 (12.2–25.7) | 7.76 (1.83–13.7) | 6.44 (3.28–9.60) | 5.17 (2.24–8.11) |
Change and 95% CI in Perceived Stress Scale (PSS) and Patient Health Questionnaire (PHQ)-15 scores adjusted for the following variables: years as an embryologist, full-time vs part-time/per-diem working status, and doctorate-level education. Bold denotes a statistically significant dose-dependent effect of cryostorage-related anxiety on PSS and PHQ-15 changes.
Discussion
Interpretation of the survey results
Findings from this study confirm that embryologists are vulnerable to stress and burnout when working in HFEA-licensed UK ART/IVF and US private and public ART/IVF clinics. There are specific working conditions that seem to contribute to the risk of burnout and worse well-being.
By combining validated, standardized psychological and somatic symptom assessment tools and customized occupational and sociodemographic questionnaires, and asking embryologists about work conditions, job fulfillment and career satisfaction, stress, somatization, anxiety, burnout factors, and other occupational aspects that are exclusive to embryologists, it was possible to narrow down their emotional and physical health issues.
The standardized questionnaires showed that embryologists in both groups experienced moderate levels of self-perceived stress and low somatic symptom severity. Working at the bench and computer stations and performing manual cryopreservation and cryostorage procedures involve prolonged periods of sitting, standing, reaching out, bending, and lifting heavy objects, which, in combination with the scheduling specifics in ART/IVF laboratories that require overtime and weekend/holiday work, create a stressful and fatiguing working environment (Collins et al., 2022; Murphy et al., 2022a, 2023a, 2023b, 2023c, 2023d; Palmer et al., 2022; Priddle et al., 2022) for all embryologists, regardless of the country of their employment. There were differences in responses to individual questions in PSS and PHQ-15 questionnaires between the two groups, which could be due to differences in both work and national cultures, lifestyles, overall health, diets, and other factors specific to each country. However, the most prevalent somatic symptoms in both groups were back pain, feeling tired or low energy, and trouble sleeping, consistent with other studies on embryologists’ physical well-being (Priddle et al., 2022) and fatiguing working conditions (Collins et al., 2022).
When comparing MBI dimensions, both groups reported similar levels of burnout on the exhaustion dimension. However, embryologists working in UK clinics reported lower levels of burnout on cynicism and professional efficacy dimensions than their colleagues in the US, which could also be due to cultural differences between the two groups and strict HFEA oversight, and, therefore, embryologists working in UK clinics may feel they have more accountability and security in their jobs.
Stressful employment conditions in both groups, such as working overtime, lack of compensation for overtime and weekend/holiday work, inadequate staffing, being called in for emergencies, and missing out on key life events due to work, are more likely to be reflected in high levels of burnout. Additionally, inadequate staffing and missing out on key life events due to work are more likely to trigger higher levels of stress and somatization. These findings demonstrate the equal importance of a balanced and well-compensated work environment and life-work balance for embryologists working in both UK and US ART/IVF clinics.
The stronger dose dependence between burnout, perceived stress and somatic symptom severity, and the levels of cryostorage-related anxiety in embryologists working in UK clinics may be due to a structured regulatory environment and rigid reporting requirements implemented by HFEA, the statutory public body. Specifically, all UK ART/IVF clinics are licensed and regulated by HFEA, and they are legally required to report data on all aspects of their operations, including incident rates ranked by severity levels. Meanwhile, US ART/IVF clinics only report success rates and percentages of individual procedures to the CDC and SART, and laws pertaining to fertility procedures, specimen safety, and patient rights vary by state. Hence, handling frozen reproductive specimens and liquid nitrogen tanks may be more emotionally and physically straining to embryologists working in UK clinics because higher rates of IVF incidents may negatively impact their standing with HFEA. US colleagues do not carry the same legal responsibilities. In the US, most IVF incidents are handled at the clinic level according to the local state laws and are often settled out of court. Medicolegal experts can only estimate the rates of IVF incidents in the US based on the sparsely available public information, and their actual number is unknown (Moutos et al., 2019; Letterie and Fox, 2020; Murphy et al., 2022b; Applebaum et al., 2023).
Regardless of embryologists’ country-specific organizational and employment characteristics, the stressful work conditions and occupational challenges reported by both study groups can have a similar negative impact on embryologists’ well-being, by increasing levels of occupational stress, somatization, and burnout. Those issues, in turn, may adversely affect the quality of embryologists’ work but can be addressed by organizational enhancements and common technology improvements.
Strengths and limitations
This study is the first to compare the prevalence of stress, somatization, and burnout among embryologists in the UK and the US, the current workflow and organizational characteristics specific to each country, and how these differences affect embryologists’ physical and emotional health. The main limitation of this study is the self-reporting nature of the data collection via online surveys of a contact list of embryologists. The survey responses were collected from the two groups 9 months apart, which may affect their responses due to differences in the responsibilities, scheduling, and workload specific to the time of the year. The US survey was sent out in April 2022, shortly after 2 years of lockdowns, restrictions on elective medical procedures, and resulting scheduling uncertainties of the COVID-19 pandemic, all of which may have contributed to higher levels of stress, somatization, and burnout than in the UK where the participants completed the survey when those restrictions had been substantially lifted. Since the survey did not ask embryologists questions about the effects of the COVID-19 pandemic on their well-being during and after lockdowns, one can only speculate about this shortcoming. Therefore, it merits further studies similar to Shanafelt et al. (2023a) and Sinsky et al. (2023) that evaluated how the COVID-19 pandemic affected physicians’ well-being and desire to continue practicing medicine.
The average age of respondents in the UK survey was lower than in the US survey, suggesting that the US respondents were more likely to hold higher-level supervisory/managerial positions in their laboratories, and, therefore, their daily routine may involve more managerial and administrative tasks, as opposed to benchwork and cryopreservation/cryostorage tasks performed by younger colleagues.
Future studies
Differences between their occupational challenges merit future studies targeting early- to mid-career embryologists in non-supervisory positions to identify and address occupational challenges and health issues specific to them. We could also directly compare work conditions and occupational health issues among embryologists with doctors and nurses working in ART/IVF clinics to identify challenges common to the ART/IVF field and those specific to working in the embryology laboratory.
Supplementary Material
Acknowledgements
We thank Dr Elaine Meyer, an Associate Professor of Psychology, Harvard Medical School, for her contributions to the development of the psychological toolkit used to measure embryologist stress, somatization, and burnout in our study, for critical review of study protocols, reports, and conference abstracts, and for editing abstracts and presentations, and Dr Laura Dodge, a Senior Epidemiologist at Optum, for the high-level statistical analysis and interpretation of study results and writing corresponding parts in this study. We also want to acknowledge the work of Ms Julia Stork, an undergraduate intern with TMRW Life Science and a senior at Northwestern University, for her help in coordinating the manuscript outline, author correspondence, and other administrative tasks associated with this article.
Contributor Information
Anar Murphy, Department of Scientific Affairs, TMRW Life Sciences, New York, NY, USA.
Mark S Lapczynski, Department of Scientific Affairs, TMRW Life Sciences, New York, NY, USA.
Glenn Proctor, Jr., Conceptions Reproductive Associates of Colorado—IVI RMA, Littleton, CO, USA
Timothy R Glynn, Dudley Associates Healthcare Marketing and Communications, Maplewood, NJ, USA.
Alice D Domar, Inception Fertility, Houston, TX, USA.
Sofia Gameiro, School of Psychology, Cardiff University, Cardiff, UK.
Giles A Palmer, International IVF Initiative, New York, NY, USA; Institute of Life, Athens, Greece; IVF 2.0 Ltd, London, UK.
Michael G Collins, Department of Scientific Affairs, TMRW Life Sciences, New York, NY, USA.
Data availability
The data contain personally identifiable information of the survey participants in the US and the UK and therefore cannot be made public. The anonymity of the survey participants is guaranteed and restricted by the informed consent and the IRB. For further requests, please contact the corresponding author.
Authors’ roles
A.M. wrote the study plans, protocols, and reports for the US and UK surveys and the manuscript with input from all authors and conducted the descriptive statistical analyses. A.M. and M.G.C. conducted a literature review and read and reviewed the manuscript. All authors (including M.S.L., G.P., T.R.G., A.D.D., S.G., and G.A.P.) were involved with the design and implementation of the study, assisted with the data interpretation, and reviewed and edited the manuscript.
Funding
TMRW Life Sciences Inc., which is developing and commercializing an automated platform for embryology.
Conflict of interest
M.G.C. and M.S.L. are full-time employees and stockholders/shareholders with TMRW Life Sciences, and A.M. of Novavax, Inc. was an employee of TMRW Life Sciences. G.P. is a consultant for TMRW Life Sciences. The remaining authors declare no conflict of interest.
References
- Alikani M. Cryostorage of human gametes and embryos: a reckoning. Reprod Biomed Online 2018;37:1–3. [DOI] [PubMed] [Google Scholar]
- Alikani M, Go KJ, McCaffrey C, McCulloh DH. Comprehensive evaluation of contemporary assisted reproduction technology laboratory operations to determine staffing levels that promote patient safety and quality care. Fertil Steril 2014;102:1350–1356. [DOI] [PubMed] [Google Scholar]
- Alikani M, Parmegiani L. Human reproductive cell cryopreservation, storage, handling, and transport: risks and risk management. Semin Reprod Med 2018;36:265–272. [DOI] [PubMed] [Google Scholar]
- Applebaum J, Humphries LA, Nepps ME, Berger DS, O’Neill K. Malpractice litigation surrounding in vitro fertilization in the United States: a legal literature review. Fertil Steril 2023;119:572–580. [DOI] [PubMed] [Google Scholar]
- Boivin J, Bunting L, Koert E, Ieng U C, Verhaak C. Perceived challenges of working in a fertility clinic: a qualitative analysis of work stressors and difficulties working with patients. Hum Reprod 2017;32:403–408. [DOI] [PubMed] [Google Scholar]
- Brady KJS, Sheldrick RC, Ni P, Trockel MT, Shanafelt TD, Rowe SG, Kazis LE. Examining the measurement equivalence of the Maslach Burnout Inventory across age, gender, and specialty groups in US physicians. J Patient Rep Outcomes 2021;5:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady KJS, Ni P, Carlasare L, Shanafelt TD, Sinsky CA, Linzer M, Stillman M, Trockel MT. Establishing Crosswalks Between Common Measures of Burnout in US Physicians. J Gen Intern Med 2022;37:777–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell A, Cohen J, Ivani K, Morbeck D, Palmer G, Mortimer S. The in vitro fertilization laboratory: teamwork and teaming. Fertil Steril 2022;117:27–32. [DOI] [PubMed] [Google Scholar]
- Caruso CC, Baldwin CM, Berger A, Chasens ER, Edmonson JC, Gobel BH, Landis CA, Patrician PA, Redeker NS, Scott LD et al. Policy brief: Nurse fatigue, sleep, and health, and ensuring patient and public safety. Nurs Outlook 2019;67:615–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983;24:385–396. [PubMed] [Google Scholar]
- Collins MG, Venier W, Salhia A, Beltsos A, Lee JA, Copperman AB, Bailey J, Sakkas D, Broussard A. Working with fatigue: assessment of cryomanagement conditions in IVF biorepositories. Fertil Steril 2022;118:E124. [Google Scholar]
- Dyrbye LN, Meyers D, Ripp J, Dalal N, Bird SB, Sen S. A Pragmatic Approach for Organizations to Measure Health Care Professional Well-Being. Discussion Paper. Washington, DC: NAM Perspectives, National Academy of Medicine, 2018.
- Dyrbye LN, Shanafelt TD, Johnson PO, Johnson LA, Satele D, West CP. A cross-sectional study exploring the relationship between burnout, absenteeism, and job performance among American nurses. BMC Nurs 2019;18:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ESHRE Working Group on Embryologist Training Analysis; Scarica C, Woodward BJ, De Santis L, Kovačič B. Training and competency assessment of clinical embryologists and licensing of the profession in European countries. Hum Reprod Open 2023;2023:hoad001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freudenberger HJ. Staff burn-out. J Soc Iss 1974;30:159–165. [Google Scholar]
- Fritzsche FR, Ramach C, Soldini D, Caduff R, Tinguely M, Cassoly E, Moch H, Stewart A. Occupational health risks of pathologists–results from a nationwide online questionnaire in Switzerland. BMC Public Health 2012;12:1054–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frone MR, Tidwell MO. The meaning and measurement of work fatigue: Development and evaluation of the Three-Dimensional Work Fatigue Inventory (3D-WFI). J Occup Health Psychol 2015;20:273–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guseva Canu I, Marca SC, Dell’Oro F, Balázs Á, Bergamaschi E, Besse C, Bianchi R, Bislimovska J, Koscec Bjelajac A, Bugge M et al. Harmonized definition of occupational burnout: A systematic review, semantic analysis, and Delphi consensus in 29 countries. Scand J Work Environ Health 2021;47:95–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Go KJ. ‘By the work, one knows the workman’: the practice and profession of the embryologist and its translation to quality in the embryology laboratory. Reprod Biomed Online 2015;31:449–458. [DOI] [PubMed] [Google Scholar]
- Go KJ. A subspecialty of the assisted reproductive technologies: cryogenic inventory maintenance. J Assist Reprod Genet 2019;36:15–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klipstein S, Daar J. Impact of shifting legal and scientific landscapes on in vitro fertilization litigation. Fertil Steril 2023;119:581–582. [DOI] [PubMed] [Google Scholar]
- Kovačič B, Plas C, Woodward BJ, Verheyen G, Prados FJ, Hreinsson J, De los Santos MJ, Magli MC, Lundin K, Plancha CE. The educational and professional status of clinical embryology and clinical embryologists in Europe. Hum Reprod 2015;30:1755–1762. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med 2002;64:258–266. [DOI] [PubMed] [Google Scholar]
- Letterie G. Outcomes of medical malpractice claims in assisted reproductive technology over a 10-year period from a single carrier. J Assist Reprod Genet 2017;34:459–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letterie G, Fox D. Lawsuit frequency and claims basis over lost, damaged, and destroyed frozen embryos over a 10-year period. F S Rep 2020;1:78–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longo BA, Schmaltz SP, Williams SC, Shanafelt TD, Sinsky CA, Baker DW. Clinician well-being assessment and interventions in Joint Commission-accredited hospitals and federally qualified health centers. Jt Comm J Qual Patient Saf 2023;49:511–520. [DOI] [PubMed] [Google Scholar]
- López-Lería B, Jimena P, Clavero A, Gonzalvo MC, Carrillo S, Serrano M, López-Regalado ML, Olvera C, Martínez L, Castilla JA. Embryologists’ health: a nationwide online questionnaire. J Assist Reprod Genet 2014;31:1587–1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorusso A, Bruno S, Caputo F, L’Abbate N. Risk factors for musculoskeletal complaints among microscope workers. G Ital Med Lav Ergon 2007;29:932–937. [PubMed] [Google Scholar]
- Makowski MS, Trockel M, Paganoni S, Weinstein S, Verduzco-Gutierrez M, Kinney C, Kennedy DJ, Sliwa J, Wang H, Knowlton T et al. Occupational characteristics associated with professional fulfillment and burnout among U.S. physiatrists. PM R 2023;15:541–551. [DOI] [PubMed] [Google Scholar]
- Marchalik D, Shanafelt TD. Surgeon wellbeing in the 21st century. Br J Surg 2023;110:1021–1022. [DOI] [PubMed] [Google Scholar]
- Maslach C, Jackson SE. The measurement of experienced burnout. J Organ Behavior 1981;2:99–113. [Google Scholar]
- Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual, 3rd edn. Palo Alto, CA: Consulting Psychologists Press, 1996. [Google Scholar]
- Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol 2001;52:397–422. [DOI] [PubMed] [Google Scholar]
- Moutos CP, Lahham R, Phelps JY. Cryostorage failures: a medicolegal review. J Assist Reprod Genet 2019;36:1041–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy A, Baltimore H, Lapczynski M, Proctor G, Meyer EC, Glynn T, Domar A, Collins MG. Embryologist burnout: physical and psychological symptoms and occupational challenges currently reported by U.S. embryologists. Fertil Steril 2022a;118:e66. [Google Scholar]
- Murphy A, Gollapudi S, Collins MG. Legal case study of severe IVF incidents worldwide: causes, consequences, and high emotional, financial, and reputational costs to patients and providers. N Am Proc Gynecol Obstet 2022b;2:22. [Google Scholar]
- Murphy A, Lapczynski M, Proctor G, Glynn T, Domar A, Gameiro S, Palmer G, Collins MG. Comparison of embryologist stress, fatigue, and burnout currently reported by U.K. and U.S embryologists. Fertil Steril 2023a;120:e265. [Google Scholar]
- Murphy A, Lapczynski M, Proctor G, Meyer EC, Glynn T, Domar A, Collins MG. Fulfillment, career satisfaction, and professional outlook: physical and psychological symptoms reported by U.S. embryologists. Hum Fertil 2023b;26:188–213. [Google Scholar]
- Murphy A, Lapczynski M, Proctor G, Meyer EC, Glynn T, Domar A, Collins MG. The role of gender in fulfillment, career satisfaction, and professional outlook reported by U.S. embryologists. Fertil Steril 2023c;120:e12–e13. [Google Scholar]
- Murphy A, Lapczynski M, Proctor G, Meyer EC, Glynn T, Domar A, Gameiro S, Palmer G, Collins M. The occupational challenges reported by UK embryologists: stress, fatigue, and burnout. Hum Reprod 2023d;38:dead093.906. [Google Scholar]
- Palmer G, Tully B, Angle M, Sadruddin S, Howles C, Elliott T, Szvetecz S, Nagy ZP, Cohen J. Occupational demands and resultant stress of reproductive scientists: outcomes from an international survey. Fertility 2022. January 5–8, 2022, ACC Liverpool, UK. https://scholar.google.com/scholar?hl=en&as_sdt=0%2C5&q=Palmer+G%2C+Tully+B%2C+Angle+M%2C+Sadruddin++demands+and+resultant+stress+of+reproductive+scientists%3A+outcomes+from+an+international+survey.+Fertility+2022&btnG= (1 August 2024, date last accessed). [Google Scholar]
- Practice Committee of the American Society for Reproductive Medicine, Practice Committee of the Society for Assisted Reproductive Technology, and Practice Committee of the Society of Reproductive Biologists and Technologists. Minimum standards for practices offering assisted reproductive technologies: a committee opinion. Fertil Steril 2021;115:578–582. asrm@asrm.org. [DOI] [PubMed] [Google Scholar]
- Practice Committee of the American Society for Reproductive Medicine; Practice Committee of the Society for Assisted Reproductive Technology; Practice Committee of the Society of Reproductive Biologists and Technologists. Recommended practices for the management of embryology, andrology, and endocrinology laboratories: a committee opinion. Fertil Steril 2014;102:961–963. [DOI] [PubMed] [Google Scholar]
- Priddle H, Pickup S, Hayes C; Association of Reproductive and Clinical Scientists (ARCS). Occupational health issues experienced by UK embryologists: informing improvements in clinical reproductive science practice. Hum Fertil (Camb) 2022;25:608–617. [DOI] [PubMed] [Google Scholar]
- Punnett L, Wegman DH. Work-related musculoskeletal disorders: the epidemiologic evidence and the debate. J Electromyogr Kinesiol 2004;14:13–23. [DOI] [PubMed] [Google Scholar]
- Rowe SG, Stewart MT, Van Horne S, Pierre C, Wang H, Manukyan M, Bair-Merritt M, Lee-Parritz A, Rowe MP, Shanafelt T et al. Mistreatment experiences, protective workplace systems, and occupational distress in physicians. JAMA Netw Open 2022;5:e2210768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruotsalainen JH, Verbeek JH, Mariné A, Serra C. Preventing occupational stress in healthcare workers. Cochr Library 2014;12:CD002892. [DOI] [PubMed] [Google Scholar]
- Schaufeli W. The burnout enigma solved? Scand J Work Environ Health 2021;47:169–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaufeli WB. Burnout: a critical overview. In: Lapierre LM, Cooper C (eds). Cambridge Companion to Organizational Stress and Well-Being. Cambridge, UK: Cambridge University Press, 2023, 214–259. [Google Scholar]
- Schaufeli WB, Leiter MP, Maslach C, Jackson SE. The Maslach Burnout Inventory – general survey. In: Maslach C, Jackson SE, Leiter MP (eds). Maslach Burnout Inventory Manual. Palo Alto, CA: Consulting Psychologists Press, 1996, 19–26. [Google Scholar]
- Shanafelt TD. Physician well-being 2.0: Where are we and where are we going? Mayo Clin Proc 2021;96:2682–2693. 10.1016/j.mayocp.2021.06.005. [DOI] [PubMed] [Google Scholar]
- Shanafelt TD, Dyrbye LN, West CP, Trockel M, Tutty M, Wang H, Carlasare LE, Sinsky CA. Career plans of US physicians after the first 2 years of the COVID-19 pandemic. Mayo Clin Proc 2023a;98:1629–1640. 10.1016/j.mayocp.2023.07.006. [DOI] [PubMed] [Google Scholar]
- Shanafelt TD, Larson D, Bohman B, Roberts R, Trockel M, Weinlander E, Springer J, Wang H, Stolz S, Murphy D. Organization-wide approaches to foster effective unit-level efforts to improve clinician well-being. Mayo Clin Proc 2023b;98:163–180. 10.1016/j.mayocp.2022.10.031. [DOI] [PubMed] [Google Scholar]
- Shanafelt TD, West CP, Sinsky C, Trockel M, Tutty M, Wang H, Carlasare LE, Dyrbye LN. Changes in burnout and satisfaction with work-life integration in physicians and the general us working population between 2011 and 2020. Mayo Clin Proc 2022;97:491–506. 10.1016/j.mayocp.2018.10.023. [DOI] [PubMed] [Google Scholar]
- Shanafelt TD, West CP, Sinsky CA, Trockel MT, Tutty MA, Wang H, Carlasare LE, Dyrbye LN. At-risk work hours among U.S. Physicians and other U.S. Workers. Am J Prev Med 2023c;65:568–578. 10.1016/j.amepre.2023.03.020. [DOI] [PubMed] [Google Scholar]
- Sinsky CA, Trockel M, Carlasare LE, West CP, Wang H, Tutty M, Dyrbye LN, Shanafelt TD. Politicization of medical care, burnout, and professionally conflicting emotions among physicians during COVID-19. Mayo Clin Proc 2023;98:1613–1628. 10.1016/j.mayocp.2023.07.007. [DOI] [PubMed] [Google Scholar]
- Tawfik DS, Profit J, Morgenthaler TI, Satele DV, Sinsky CA, Dyrbye LN, Tutty MA, West CP, Shanafelt TD. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. Mayo Clin Proc 2018;93:1571–1580. https://www.mayoclinicproceedings.org/article/S0025-6196(18)30372-0/fulltext. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson SK, Mason E, Dukes S. Ergonomics and cytotechnologists: reported musculoskeletal discomfort. Diagn Cytopathol 2003;29:364–367. [DOI] [PubMed] [Google Scholar]
- Trockel MT, Menon NK, Rowe SG, Stewart MT, Smith R, Lu M, Kim PK, Quinn MA, Lawrence E, Marchalik D et al. Assessment of physician sleep and wellness, burnout, and clinically significant medical errors. JAMA Netw Open 2020;3:e2028111. [DOI] [PubMed] [Google Scholar]
- Veiga E, Olmedo C, Sánchez L, Fernández M, Mauri A, Ferrer E, Ortiz N. Recalculating the staff required to run a modern assisted reproductive technology laboratory. Hum Reprod 2022;37:1774–1785. [DOI] [PubMed] [Google Scholar]
- West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med 2018;283:516–529. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data contain personally identifiable information of the survey participants in the US and the UK and therefore cannot be made public. The anonymity of the survey participants is guaranteed and restricted by the informed consent and the IRB. For further requests, please contact the corresponding author.