Abstract
Background: Various methods are used to treat patients with coronavirus, including drug therapy and alternative and non-invasive therapies Research has been done on the effects of body position on cardiac function in patients with COVID-19 diagnosis. Methods: This study was performed on patients admitted with COVID-19 diagnosis. Patients with inclusion criteria were selected based on purpose and entered into the study. They were divided into three groups: Group A patients were placed in a semi-sitting position, group B patients were placed in a tripod position, and group C patients were placed in a prone position. After being placed in the relevant positions at 15 and 60 minutes were measured in terms of heart rate and blood pressure at the mentioned times in the relevant checklist. Results: The results showed that there was no statistically significant difference in heart rate between the three groups before the intervention (P>0.05). In other words, changes in heart rate over time between the three groups (in several measurements) were statistically significant (P<0.05). Regarding Systolic Blood Pressure (SBP) and Diastolic Blood pressure patterns, the results showed that the three position groups was not statistically different before and 15 and 60 minutes after the intervention (P>0.05). Conclusion: According to the results, it can be concluded that placing the patient in all three positions of the tripod, prone and semi-sitting can be effective in improving the patient's heart rate pattern and lead to improving the patient's clinical condition.
Keywords: COVID-19 , change position , cardiac function
Introduction
COVID-19 is an emerging disease that led to widespread epidemics worldwide with the detection of coronavirus in December 2019 in Wuhan, China [1, 2, 3, 4].
Patients with COVID-19 diagnosis usually show a decrease in the number of lymphocytes and eosinophils, lower mean hemoglobin levels, as well as an increase in WBC, neutrophil count, and serum levels of CRP, LDH, AST, and ALT. In addition, early serum CRP levels have been reported as an independent predictor of severe COVID-19 infection [5].
The incubation period of this disease is between 1-14 days and the infected person in this period can also be a carrier of the disease.
95% of the infected people show symptoms 12.5 days after contact with the virus. Oral secreted droplets are the most common mode of transmission of the virus to another person. Also, it enters the body through the mouth, nose, and conjunctiva [6, 7, 8].
The other symptoms of COVID-19 include fever, cough, dizziness, hemoptysis, hypoxia, dyspnea, lymphopenia, sore throat, rhinorrhea, dry cough, myalgia, anosmia, chest pain, diarrhea, ARDS, and even heart damage [8, 9, 10, 11, 12].
Although the main target of coronavirus infection is an invasion of the lungs, the widespread distribution of ACE2 receptors in the organs may lead to gastrointestinal, renal, liver, central nervous system, ocular, and cardiovascular damage that should be screened for in patients with coronavirus. Clinically closely monitored [5].
Reports suggest that heart problems can also occur in COVID-19 patients when the cardiovascular system is affected by a coronavirus, the patient may develop complications such as myocarditis, myocardial infarction, myocardial injury, cardiac arrhythmias, heart failure, as well as vascular problems such as venous thromboembolism [5, 13].
Therefore, knowing the cardiovascular system and taking the necessary care in this regard for patients with COVID-19 can be considered as a turning point in treatment and complementary care [14].
Treatments often seek to reduce inflammation. However, the treatment of the symptoms and complications of this disease requires a comprehensive approach, including the work of a physician, physiotherapist, radiograph, etc. [15].
In some cases, the use of antibiotics, antivirals, and corticosteroids have also been considered in treatment lines [7, 16].
One of the non-invasive treatments that can be considered for patients along with receiving other treatments is positioning the patient [17].
Positioning when treating patients with various problems is very important in maximizing physical function. It is important to know the consequences of each position on the respiratory system of a particular disease. Understanding the effect of position can give health care professionals a better understanding of the optimal position of patients with various diseases [18].
In general, the body change of the patient can improve the pattern of cardiac function and lead to the proper functioning of the cardiac autonomic system [19].
One of the positions that can be used for such patients is the semi-sitting position. According to research on the function of this position, it has been concluded that when the patient is in this position, it improves the patient's hemodynamic pattern [20, 21].
A semi-sitting position can also lead to a decrease in systolic blood pressure as well as an increase in diastolic blood pressure [22].
Another position is the tripod position, which can be used for the patient by bending the patient forward with his hands on his knees. Several researchers have hypothesized that the tripod position improves the function of the respiratory sub-muscles and also facilitates breathing by releasing the auxiliary respiratory muscles as a result of stabilizing the arms and reducing the will be the use of the upper chest muscles and freeing the diaphragm from abdominal visceral pressure [23].
Another position that can be used as a non-invasive measure to solve patients' problems is the prone position. This position has been used for many years and is also recommended for patients with severe or moderate to severe acute respiratory distress syndrome (ARDS) who receive invasive mechanical ventilation with sedation and paralysis [24].
The function of this position can be considered in the fact that by redistributing blood flow, they improve perfusion ventilation, which can affect the cardiopulmonary function and improve the patient's hemodynamic condition and when placing the patient in a prone position also leads to an improvement in the perfusion pattern [25, 26].
Peron position can also be effective in improving blood pressure patterns, especially systolic blood pressure [27].
COVID-19 is widely accepted by physicians and is used even before intubation in patients who breathe spontaneously so that if this position is used for a long time Improves right ventricular function and improves hemodynamic pattern, reduces the rate of hypoxia and hypercapnia, improves the process of lung involvement caused by the virus [24].
Various mechanisms explain the potential benefits of this position, including homogenization of ventilation-perfusion mismatch, redistribution of pleural pressure gradient, pure alveolar uptake, and more coordinated alveolar swelling, and prevention and reduction of lung injury from the respiratory tract [28].
Based on previous research and available evidence, it can be seen that the position of the body has such a significant effect on the function of various organs, especially the heart and lungs that cannot be ignored. Research has been done on the effects of body position on heart function in patients with COVID-19 disease, but there has been no comprehensive study on the comparison and comparison of these three positions on blood pressure pattern and heart rate. Therefore, this study aimed based on the nursing intervention to investigate the effect of semi-sitting, tripod, and prone positions on cardiac function in patients with COVID-19 diagnosis.
Materials and Methods
Design
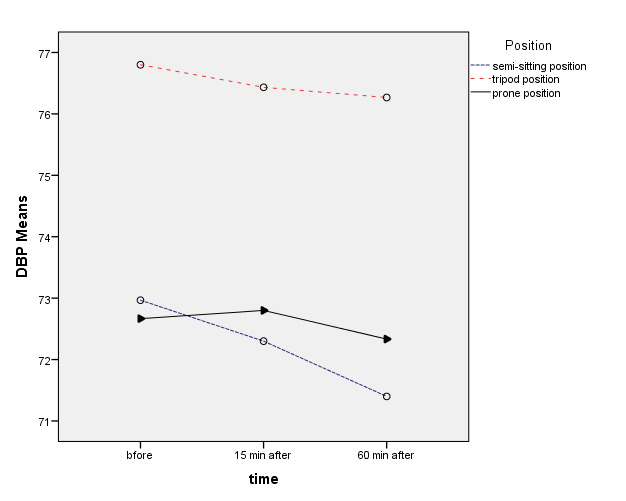
This research is a clinical trial that was performed on patients admitted with COVID-19 diagnosis to Amir Al-Momenin Hospital in Arak city, Iran. First, 90 eligible patients with inclusion criteria were selected based on purpose and entered into the study. According to the bellow formula for comparing the means and previous studies with 0.05 confidence and test power of 90% of the sample size, with the help of G. power software, the comparison of the average of two communities of 18 people for each group is calculated [29].
The ethics committee of Khomein University of Medical Sciences, Khomein, Iran, approved this study (Ethical code: IR.KHOMEIN.REC.1400.001). ID of the Iranian Registry of Clinical Trials (IRCT) of this study is IRCT20171203037733N3. All patients have signed a written informed consent regarding their participation in this study.
Participants and Intervention
According to the probability of falling samples in each group, 30 people were determined (Total: 90 patients).
Then by the rand function in excel software randomization was performed and they were divided into three groups: A, B, and C.
Group A patients were placed in a semi-sitting position, group B patients were placed in a tripod position, and group C patients were placed in a prone position. Before the intervention, patients' cardiac function, which included blood pressure pattern and heart rate, was measured and recorded in the relevant checklist for all three groups. Then the patients of all three groups were placed in their respective positions.
Data Collection Tools
Patients after being placed in the relevant positions at 15 and 60 minutes were measured in terms of heart rate and blood pressure at the mentioned times and the extracted information was accurately entered in the relevant checklist.
In this study, a researcher-made checklist was used. The first part included demographic information (name, surname, medical history, surgical history, history of infection, date of hospitalization, length of hospitalization, level of education, gender, age, and the second part was related information). According to the type of positions (semi-sitting, tripod, and prone), their heart function, which included heart rate and blood pressure, was recorded separately for each patient [29, 30].
Blinding
The method of blinding in this study was that the data analyzer and the main researcher were unaware of how to blind the samples.
Statistical tests used in this study include ANOVA, Chi-square, repeated measure test as well as the results of Greenhouse-Geisser and Sphericity Assumed tests, and SPSS version 21 was used for statistical analysis.
Inclusion and exclusion criteria included the following:
Inclusion criteria:
COVID-19 diagnosis (positive PCR test)
Age 20 to 70 years
Willingness to participate in research
Lack of connection to a mechanical ventilator (no intubation)
Ability to communicate
No underlying respiratory disease
No pregnancy
No history of abdominal surgery during the last 6 months (for placement in the lumbar position)
Having lung involvement at least 10%
Exclusion criteria:
Patient death
Unwillingness to participate in further research
Patient intubation during research
Abdominal obesity
Abdominal surgery recently (during the last 6 months)
Results
The results show that the examined groups were not significantly different in the variables of height, weight, number of hospitalized days, gender, and hospitalization history (P>0.05).
However, they were significantly different in their ages, educational levels, and marital status (P<0.05) (Table 1).
Table 1.
Frequency distribution of examined units according to quantitative demographic variables in studied groups
|
Variables Group |
Semi-sitting position |
Tripod position |
Prone position |
P-value |
|
|
Age (years) |
Mean±SD |
55.40±14.67 |
49.23±12.17 |
45.38±14.33 |
P=0.028 F=3.719 |
|
Size (cm) |
Mean±SD |
168.40±8.73 |
168.93±8.45 |
170.17±9.78 |
P=0.733 F=0.311 |
|
Weight (kg) |
Mean ±SD |
77.40±13.08 |
79.76±11.18 |
75.56±12.91 |
P=0.426 F=0.862 |
|
Duration of hospitalization (days) |
Mean±SD |
1.43±0.50 |
1.47±0.50 |
1.33±0.47 |
P=0.560 F=0.584 |
|
Sex |
Man |
15(50) |
16 (53.3) |
17 (56.7) |
P=0.974 |
|
Female |
15(50) |
14 (46.7) |
13 (43.3) |
||
|
Level of Education |
Primary education and guidance |
5(16.7) |
7 (23.3) |
0(0) |
P=0.037 |
|
High school education |
9 (30) |
7 (23.3) |
6 (20) |
||
|
Diploma |
12(40) |
6 (20) |
14 (46.7) |
||
|
University education |
4 (13.3) |
10 (33.3) |
10 (33.3) |
||
|
History of hospitalization |
10 (33.3) |
17 (56.7) |
15 (50) |
P=0.058 |
|
|
No |
20 (66.7) |
13 (43.3) |
15 (50) |
||
|
Marital status |
Single |
0 (0) |
4 (13.3) |
6 (20) |
P=0.043 |
|
Married |
30 (100) |
26 (86.7) |
24 (80) |
||
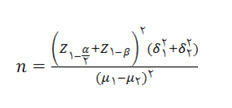
The results showed that there was no statistically significant difference in heart rate between the three groups before the intervention (P>0.05).
However, group differences became statistically significant after the study (P<0.05); so that the heart rate of the tripod group was significantly higher than the semi-sitting and prone groups.
Also, the results of repeated measurements of the Sphericity Assumed test showed that the effect of time effect and group effect was significant (P<0.05).
In other words, changes in heart rate over time between the three groups (in several measurements) were statistically significant (Table 2).
Table 2.
Comparing the number of heart rate in examined groups
|
Variables Group |
Semi-sitting position |
Tripod position |
Prone position |
p-value |
|
|
Heart Rate |
Before |
74.37 ±12.85 |
82.37 ±10.98 |
76.17 ±16.49 |
P=0.064 F=2.84 |
|
After 15 min |
73.03 ±13.29 |
81.83 ±11.77 |
70.10 ±14.00 |
P=0.002 F=6.56 |
|
|
After 60 min |
71.67 ±15.06 |
82.93 ±11.32 |
71.50 ±14.46 |
P=0.002 F=6.85 |
|
|
Time effect |
F=3.24 |
P=0.041 |
|||
|
Time * group interaction |
F=1.60 |
P=0.175 |
|||
|
Group effect |
F=6.39 |
P=0.003 |
|||
Also Figure 1 shows the mean Heart Rate before the intervention, 15 minutes and 60 minutes after the intervention in three groups (Figure 1).
Figure 1.
Mean Heart Rate before, 15, and 60 minutes after the intervention in three groups
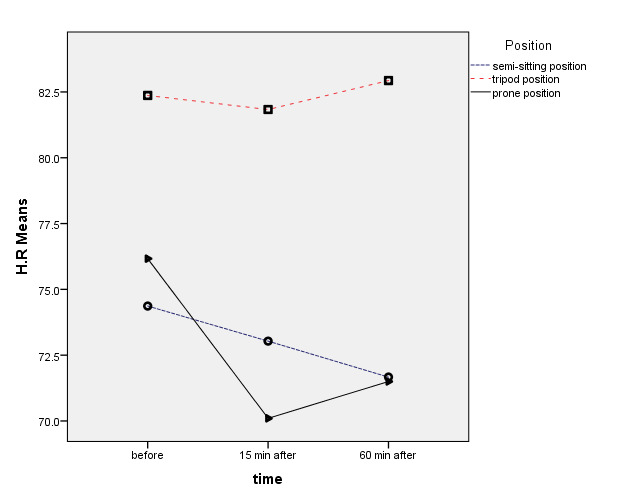
Regarding Systolic Blood Pressure (SBP) patterns, the results showed that the Systolic Blood Pressure (SBP) of the three-positions groups was not statistically different before and 15 and 60 minutes after the intervention (P>0.05).
Furthermore, the results of the repeated measures of the Greenhouse-Geisser test disclosed that the effects of time and time-group interaction were not significant (P>0.05) (Table 3).
Table 3.
Comparing the average systolic blood pressure of examined groups
|
Variables Group |
Semi-sitting position |
Tripod position |
Prone position |
p-value |
|
|
Systolic Blood Pressure (SBP) |
Before |
113.00±17.91 |
117.53±16.57 |
108.67±13.57 |
P=0.110 F=2.26 |
|
15 min After |
112.00±13.57 |
115.60±18.04 |
108.37±12.70 |
P=0.181 F=1.74 |
|
|
60 min After |
110.17±12.85 |
114.53±16.88 |
109.33±10.14 |
P=0.286 F=1.26 |
|
|
Time effect |
F=1.12 |
P=0.325 |
|||
|
Time * group interaction |
F=0.580 |
P=0.664 |
|||
|
Group effect |
F=2.090 |
P=0.130 |
|||
Also Figure 2 shows the mean Systolic Blood Pressure (SBP) before the intervention, 15 minutes and 60 minutes after the intervention in three groups (Figure 2).
Figure 2.
Mean Systolic Blood Pressure before, 15, and 60 minutes after the intervention in three groups
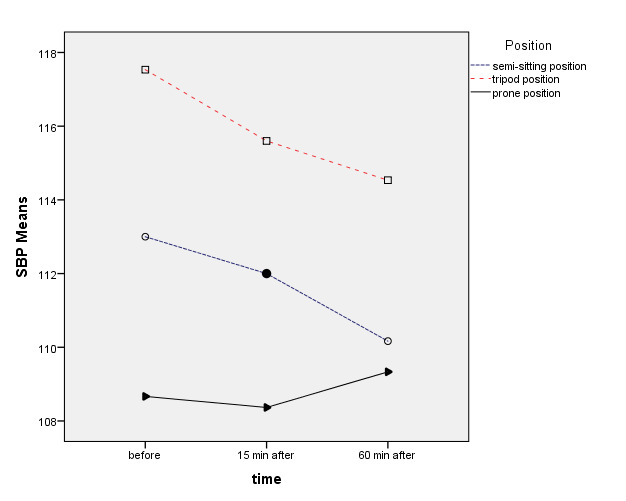
Regarding Diastolic Blood Pressure (DBP) patterns, the results showed that the Diastolic Blood Pressure (DBP) of the three-positions groups was not statistically different before and 15 and 60 minutes after the intervention (P>0.05).
Furthermore, the results of the repeated measures of the Sphericity Assumed test showed that the effects of time and time-group interaction were not significant (P>0.05) (Table 4).
Table 4.
Comparing the average diastolic blood pressure of examined groups
|
Variables Group |
Semi-sitting position |
Tripod position |
Prone position |
p-value |
|
|
Diastolic Blood Pressure (DBP) |
Before |
72.97±11.06 |
76.80±11.43 |
72.67±7.84 |
P=0.225 F=1.51 |
|
15 min After |
72.30±8.52 |
78.43±12.65 |
72.80±7.38 |
P=0.209 F=1.59 |
|
|
60 min After |
71.40±8.93 |
76.27±12.18 |
72.33±7.73 |
P=0.131 F=2.08 |
|
|
Time effect |
F=0.761 |
P=0.469 |
|||
|
Time * group interaction |
F=0.185 |
P=0.946 |
|||
|
Group effect |
F=1.96 |
P=0.146 |
|||
Figure 3 shows the mean Diastolic Blood Pressure (DBP) before the intervention, 15 minutes and 60 minutes after the intervention in three groups (Figure 3).
Figure 3.
Mean DBP before and 15 and 60 minutes after the intervention in three groups
Discussion
The results of this study showed that the mean heart rate of patients with COVID-19 disease increased significantly in the tripod, semi-sitting, and then prone positions, respectively. This means that the HR of the patient with COVID-19 has increased in the tripod position more than the semi-sitting position, in the semi-sitting position more than the prone position, and the tripod position more than the prone position.
In the study of Cruz et al., which performed on the effects of different positions on the HR of healthy men the results showed that the amount of HR in the two positions of standing and supine was not statistically significant. As can be seen, although Cruz et al., Examined different positions on HR, standing was not considered in this study.
Therefore, this discrepancy can be explained by the samples under study, the difference in the type of positions, and the difference in the duration of placement in each of the mentioned positions. For example, in our study, the samples were male and female patients with COVID-19, while in the study of Cruz et al., Only healthy men made up the specimens under study [31].
However, in this section, it should be noted that in the study of Bourdillon et al., which examined the effect of supine and standing positions in patients with COVID-19, despite the complete similarity in all stages of the intervention and the type of positions with the study of Cruz et al., they are completely inconsistent with each other in the results. In the study by Bourdillon et al., it was shown that the amount of HR in the supine position would increase compared to the standing position due to more sympathetic stimulation, while in the study of Cruz et al., the opposite was shown. Perhaps this obvious discrepancy, despite the fundamental similarities, can be explained by the differences in the samples under study, because in the study of Bourdillon et al., patients with COVID-19 were examined, but in the Cruz study, healthy individuals were examined and this paradox can be related to the malignant coronavirus and its widespread and sometimes unknown effects, which have led to changes in the heart or arteries of these patients, which, following a change in position, undergo changes to increase or decrease HR [31, 32].
In other studies such as the study of Hnatkova et al., the amount of HR in other positions such as supine, sitting and semi-sitting positions has been studied and the results of their study showed that the amount of HR in the supine position was higher than sitting and semi-sitting positions [33].
Concerning this study, it is not possible to make an accurate and clear judgment or comparison with our study, because in the study of Hnatkova et al., different positions were used and the only common denominator between this study and our study is in the semi-sitting position, which is not enough for a wise and logical comparison, but according to the results, the superiority of the supine position over the semi-sitting position to increase HR can be acknowledged.
Regarding tripod position and changes in HR, we can refer to the study of Rauseo et al., in patients with pneumonia following SARS that which the results of their study showed that there was no statistically significant difference between the patient's position in the supine and the tripod positions, in other words, the patients' HR did not change. As can be seen, the results of their study are in complete contradiction with our study; because in our study, the results showed that we have the most changes in the direction of increasing HR in the tripod position, which may be the difference on patients with pneumonia were in the Rauseo study and patients with COVIID-19 disease were in our study, as well as the widespread and sometimes unknown effects of the coronavirus [34].
Regarding the prone position and changes in HR, we can refer to the study of Özçelik et al., whose results showed an increase in HR by changing the position of patients with Obstructive Sleep Apnea (OSA) to sleep. Although Özçelik et al., conducted their research in samples with OSA and not in COVID-19 patients, they considered the main variables of the study, including lumbar position and HR, and similar results with our study, it can be stated that the results of their study, despite minor differences, were consistent with our study [35].
Regarding the tripod position and heart rate changes, a study conducted by Kocatepe and et al. shows that the patients admitted to the ICU experience a decrease in heart rate after the onset of the tripod position, which contradicts the results of the present study.
In our study, patients did not have a statistically significant difference in heart rate after being placed in the tripod position. In the present study, there was a significant difference between the tripod group and the peroneal and semi-sitting position between the patients' heart rates. In the field of selecting the appropriate position for automatic adjustment of cardiac function [19].
Also, the results of our study showed that the mean of Systolic Blood Pressure (SBP) and Diastolic Blood Pressure (DBP) in three semi-sitting positions, tripod and prone positions, before, 15 minutes, and 60 minutes after being in the mentioned positions, were not statistically significant. This means that the mentioned positions cannot lead to changes in the direction of increasing or decreasing SBP and DBP in patients with COVID-19 disease, and in other words, it can be said that semi-sitting, tripod, and prone positions don't affect SBP and DBP in patients with COVID-19 disease.
The changes of SBP and DBP in our study were similar and different from the study of Sahraie et al., in such a way that, as mentioned, in our study, there was no statistically significant difference between the SBP and DBP in each of the position groups separately and also between the three groups, but in the study of Sahraie et al., there was a statistically significant difference in SBP and DBP in the prone position compared to the supine position, only in the "post-recovery time", so that the rate SBP was higher and DBP was higher in the supine position compared to the prone position. But in this study, as in our study, in general, there was no statistically significant difference between the two positions. The general differences between Sahraie et al. and our study can be explained by the differences in the samples of the study. For example, in the study of Sahraie et al., the samples were patients undergoing kidney stone surgery, and in our study, the samples were patients with COVID-19 diagnosis, or these differences can even be explained by the type of positions and the duration of placement in each position were also justified. Because in the study of Sahraie et al., the supine and prone positions were used, which in our study, the tripod, semi-sitting, and prone positions were used instead, and also in terms of the duration of being in each of the positions in the study of Sahraie et al., previous, 10 minutes, 15 minutes and 6 hours after surgery [36] and our study, before, 15 and 60 minutes after placement in each position that all the minor differences mentioned may eventually be a whole and a large unit that in the general differences in the results of the above studies and justify.
The study of Cicolini and et al. evaluated the difference between patients' blood pressure in sitting, semi-sitting, and supine positions, which showed that DBP was at the highest level in the sitting position, moderate in the semi-sitting position, and at its lowest level in the supine position. In contrast, the SBP in the sitting and semi-sitting positions was lower than in the supine position.
Cicolini and et al., in comparison with the group of patients in the semi-sitting position, achieved results following the results of our present study. In our study, patients in the semi-sitting position after 15 and 60 minutes did not have a statistically significant difference in systolic and diastolic blood pressure that in the study of Cicolini and et al., patients after being placed in a semi-sitting position did not have a significant difference in systolic and diastolic blood pressure, and this indicates that the semi-sitting position has more credibility in measuring patients' blood pressure and can be used more in care.
The reason for the significant difference between the different positions in the Cicolini study, which contradicts the present study, maybe the time difference in the patients' blood pressure measurements. The measurement time of 15 and 60 minutes in patients makes it possible that the automatic regulation system of cardiovascular function adapts to the change of body position over time. Also, the tripod and prone positions were considered in our study that in the Cicolini and et al., study, the semi-sitting position was compared with the full and lying sitting position [22].
Regarding prone position and blood pressure changes, Watanabe et al. showed that the SBP and DBP are higher than from full sitting position in healthy individuals in the prone position, which is contrary to the results of our study. The patients in our study did not have a significant difference in systolic and diastolic blood pressure compared to other positions in the prone position. The reason for this discrepancy may be the difference in positions compared to the prone position, and another reason is that in the present study, patients with COVID-19 were present, but in the Watanabe et al., study, healthy individuals were examined [19].
Also in the study of Dennis et al., there was no statistically significant difference between SBP and DBP of patients lying on their sides in different positions, which is consistent with the results of the present study [27].
Also, regarding tripod position and changes in blood pressure, the study of Kocatepe et al. examines the changes of SBP and DBP of patients in tripod and lotus positions, which has obtained results that are contrary to and agree with the results of our study. In Kocatepe et al., study, systolic blood pressure in tripod position there was no statistically significant that agreement with the results of our study, but in diastolic blood pressure, patients in the tripod position experienced a decrease in DBP, which is not consistent with the results of our study. The difference between these two studies is in the types of positions. In Kocatepe et al., study, the tripod position was compared with the lotus position [37].
Due to the changes in cardiac function observed in the Kocatepe et al., study and the differences with the results of the present study and due to the very limited research on the effect of tripod position on heart function of patients, more research is needed in this field.
Acknowledgments
The authors of this article would like to express their gratitude to the officials of Khomein University of Medical Sciences and Arak University of Medical Sciences and Amir-Al-Momenin hospital of Arak city.
Conclusion
According to the results of the study, the patient was placed in a tripod position relative to the supine and semi-sitting positions can improve the heart rate of patients with COVID-19, which can be considered as a provided complementary therapy along with other medical care the patient receives. But in general, it can be concluded that placing the patient in all three positions of the tripod, prone and semi-sitting can be effective in improving the patient's heart rate pattern and lead to improving the patient's clinical condition.
Regarding the patient's placement in the mentioned positions and repeated measurements of blood pressure, it is not possible to consider superiority between any of the tripod, semi-sitting, and prone positions, and the patient's placement in the mentioned positions does not affect increasing or decreasing the systolic and diastolic blood pressure pattern.
In general, it can be concluded that in addition to the invasive medical care that patients receive to improve their clinical condition, alternative therapies can also be used to improve the clinical condition of patients with COVID-19.
Funding
This study was supported by Khomein University of Medical Sciences, Khomein, Iran (No: 99000009).
Conflict of interests
The authors have no conflict of interest to declare.
References
- 1.Akbari M, Fayazi N, Kazemzadeh Y, Didehdar M, Momeni H, Abedi B, Orouji M. Evaluate the case fatality rate (CFR) and basic reproductive rate (R-naught) of COVID-19. Curr. Health Sci. J. 2021;47(2):270–274. doi: 10.12865/CHSJ.47.02.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akbari M, Kazemzadehy undefined, Fayazi N, Sadeghi K, Orouji M, Momeni H, Abedi B. Investigation of the Epidemiological Situation and the Incidence of Covid 19 Disease in an Area of Markazi Province in Iran Country. Curr. Health Sci. J. 2021;47(1):16–22. doi: 10.12865/CHSJ.47.01.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Akbari M, Didehdar M, Nazari M, Azadi D. Pediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 symptoms in Iran. Future Virol. 2022;17(1):13–18. doi: 10.2217/fvl-2021-0156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baloch S, Baloch MA, Zheng T, Pei X. The coronavirus disease 2019 (COVID-19) pandemic. Tohoku J Exp Med. 2020;250(4):271–278. doi: 10.1620/tjem.250.271. [DOI] [PubMed] [Google Scholar]
- 5.Ciotti M, Ciccozzi M, Terrinoni A, Jiang W-C, Wang C-B, Bernardini S. The COVID-19 pandemic. Crit Rev Clin Lab Sci. 2020;57(6):365–388. doi: 10.1080/10408363.2020.1783198. [DOI] [PubMed] [Google Scholar]
- 6.Liang H, Acharya G. Novel corona virus disease (COVID‐19) in pregnancy: What clinical recommendations to follow. Acta Obstet Gynecol Scand. 2020;99(4):439–442. doi: 10.1111/aogs.13836. [DOI] [PubMed] [Google Scholar]
- 7.Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. Jama. 2020;324(8):782–793. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- 8.He F, Deng Y, Li W. Coronavirus disease 2019: What we know. J Med Virol. 2020;92(7):719–725. doi: 10.1002/jmv.25766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Viner RM, Ward JL, Hudson LD, Ashe M, Patel SV, Hargreaves D, Whittaker E. Systematic review of reviews of symptoms and signs of COVID-19 in children and adolescents. Arch Dis Child. 2021;106(8):802–807. doi: 10.1136/archdischild-2020-320972. [DOI] [PubMed] [Google Scholar]
- 10.Kaye R, Chang CWD, Kazahaya K, Brereton J, Denneny JC. COVID-19 anosmia reporting tool: initial findings. Otolaryngol Head Neck Surg. 2020;163(1):132–134. doi: 10.1177/0194599820922992. [DOI] [PubMed] [Google Scholar]
- 11.Alimohamadi Y, Sepandi M, Taghdir M, Hosamirudsari H. Determine the most common clinical symptoms in COVID-19 patients: a systematic review and meta-analysis. J Prev Med Hyg. 2020;61(3):304–304. doi: 10.15167/2421-4248/jpmh2020.61.3.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zheng Y-Y, Ma Y-T, Zhang J-Y, Xie X. COVID-19 and the cardiovascular system. Nature reviews cardiology. 2020;17(5):259–260. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aghagoli G, Gallo Marin, Soliman LB, Sellke FW. Cardiac involvement in COVID‐19 patients: Risk factors, predictors, and complications: A review. J Card Surg. 2020;35(6):1302–1305. doi: 10.1111/jocs.14538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Long B, Brady WJ, Koyfman A, Gottlieb M. Cardiovascular complications in COVID-19. AJEM. 2020;38(7):1504–1507. doi: 10.1016/j.ajem.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fraser E. Long term respiratory complications of covid-19. BMJ. 2020;370:3001–3001. doi: 10.1136/bmj.m3001. [DOI] [PubMed] [Google Scholar]
- 16.Liu W, Tao Z-W, Wang L, Yuan M-L, Liu K, Zhou L, Wei S, Deng Y, Liu J, Liu HG, Yang M, Hu Y. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin Med J. 2020;133(09):1032–1038. doi: 10.1097/CM9.0000000000000775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Safari M, Cheraghi M, Ansari M, Amini M. Semi-fowler’s Position and Its Duration Effect on The Arterial Blood Gases (ABGs) Journal of Guilan University of Medical Sciences. 2002;11(42):54–62. [Google Scholar]
- 18.Katz S, Arish N, Rokach A, Zaltzman Y, Marcus E-L. The effect of body position on pulmonary function: a systematic review. BMC Pulm. Med. 2018;18(1):1–16. doi: 10.1186/s12890-018-0723-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Watanabe N, Reece J, Polus BI. Effects of body position on autonomic regulation of cardiovascular function in young, healthy adults. Chiropr Man Therap. 2007;15(1):1–8. doi: 10.1186/1746-1340-15-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chanif C, Prastika D. Position of Fowler and Semi-fowler to Reduce of Shortness of Breath (Dyspnea) Level While Undergoing Nebulizer Therapy. South East Asian Nurs Res. 2019;1(1):14–19. [Google Scholar]
- 21.Sabeti F, Soltanzadeh M, Mali S, Akbari-Nassaji N, Mahvar T. The effect of semi sitting, supine and lateral positions on results of arterial blood gases and vital signs in patients undergoing coronary artery bypass graft surgery. Life Sci J. 2012;9(3):1432–1437. [Google Scholar]
- 22.Cicolini G, Pizzi C, Palma E, Bucci M, Schioppa F, Mezzetti A, Manzoli L. Differences in blood pressure by body position (supine, Fowler's, and sitting) in hypertensive subjects. Am. J. Hypertens. 2011;24(10):1073–1079. doi: 10.1038/ajh.2011.106. [DOI] [PubMed] [Google Scholar]
- 23.Bhatt S, Guleria R, Luqman-Arafath T, Gupta A, Mohan A, Nanda S, et al. Effect of tripod position on objective parameters of respiratory function in stable chronic obstructive pulmonary disease. Indian J Chest Dis Allied Sci. 2009;51(2):83–83. [PubMed] [Google Scholar]
- 24.Guérin C, Albert RK, Beitler J, Gattinoni L, Jaber S, Marini JJ, et al. Prone position in ARDS patients: why, when, how and for whom. Intensive Care Med. 2020;46:2385–2396. doi: 10.1007/s00134-020-06306-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zang X, Wang Q, Zhou H, Liu S, Xue X. Efficacy of early prone position for COVID-19 patients with severe hypoxia: a single-center prospective cohort study. Intensive Care Med. 2020;46(10):1927–1929. doi: 10.1007/s00134-020-06182-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Albert RK, Hubmayr RD. The prone position eliminates compression of the lungs by the heart. Am. J. Respir. Crit. 2000;161(5):1660–1665. doi: 10.1164/ajrccm.161.5.9901037. [DOI] [PubMed] [Google Scholar]
- 27.Dennis AT, Hardy L, Leeton L. The prone position in healthy pregnant women and in women with preeclampsia-a pilot study. BMC pregnancy and childbirth. 2018;18(1):1–10. doi: 10.1186/s12884-018-2073-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gaudry S, Tuffet S, Lukaszewicz A-C, Laplace C, Zucman N, Pocard M, Costaglioli B, Msika S, Durenteau J, Payen D, Dreyfuss D, Hajage D, Richard JD. Prone positioning in acute respiratory distress syndrome after abdominal surgery: a multicenter retrospective study. Ann. Intensive Care. 2017;7(1):21–21. doi: 10.1186/s13613-017-0235-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sadeghi R, Safari M, Karimlou M, Baghery nesami, Esmaily douky. Study of Position effect on Results of ABG of Hospitalized Patients in ICU of Open Heart Surgery Center of Mazandaran. Armaghane danesh. 2008;13(3):65–71. [Google Scholar]
- 30.Eşer İ, Khorshid L, Yapucu Güneş, Demir Y. The effect of different body positions on blood pressure. J Clin Nurs. 2007;16(1):137–140. doi: 10.1111/j.1365-2702.2005.01494.x. [DOI] [PubMed] [Google Scholar]
- 31.da Cruz, Porto LGG, da Silva, de Souza, Garcia GL, Molina GE. Impact of heart rate on reproducibility of heart rate variability analysis in the supine and standing positions in healthy men. Clinics. 2019;74:806–806. doi: 10.6061/clinics/2019/e806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bourdillon N, Yazdani S, Schmitt L, Millet GP. Effects of COVID-19 lockdown on heart rate variability. PloS one. 2020;15(11):1–1. doi: 10.1371/journal.pone.0242303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hnatkova K, Šišáková M, Smetana P, Toman O, Huster KM, Novotný T, Schmidt G, Malik M. Sex differences in heart rate responses to postural provocations. Int. J. Cardiol. 2019;297:126–134. doi: 10.1016/j.ijcard.2019.09.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rauseo undefined, M undefined, Mirabella L, Caporusso R, Cantatore L, Perrini M, Vetuschi P, Cinnella G. SARS-CoV-2 pneumonia succesfully treated with cpap and cycles of tripod position. BMC Anesthesiol. 2021;21(1):1–4. doi: 10.1186/s12871-020-01221-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.zçelik HK, Bayram M, Doganay E, Kart L, Sezer M, Akkoyunlu ME, Karaköse F, Yakar F. Effects of body position on sleep architecture and quality in subsyndromal adults without apparent obstructive sleep apnea. Sleep Biol Rhythms. 2015;13(3):279–286. [Google Scholar]
- 36.Sahraie R, Eftekharian F, Damshenas MH, Kalani N, Rastgarian A. Comparison of Postoperative Nausea and Vomiting in Percutaneous Nephrolithotomy (PCNL) through Two Supine and Prone Methods: A Clinical Trial Study. medical journal of mashhad university of medical sciences. 2020;63(1):2230–2237. [Google Scholar]
- 37.Kocatepe V, Yildirim D, Can G, Bahceci E. The Effect of Lotus Position on Dyspnoea Management in Intensive Care Unit. JPMA. 2020;70(5):820–824. doi: 10.5455/JPMA.302643210. [DOI] [PubMed] [Google Scholar]


