Abstract
Acute limb ischemia, or ALI, is a rapid decrease in limb perfusion due to an occlusion of an artery or a bypass graft. Most cases result from in situ thrombosis or embolism in patients with antecedent peripheral arterial disease. Potential sources of arterial embolism as a cause of this condition include cardiogenic, aortic, peripheral aneurysms with an associated mural thrombus or, less commonly, a paradoxical embolism through a septal defect. We present a rare case of ALI due to an underlying patent foramen ovale that was successfully treated following revascularization. This article emphasizes one of the more unusual mechanisms of ALI. Despite the rarity, physicians should maintain a high index of clinical suspicion for a paradoxical embolism across a patent foramen ovale in unexplained arterial occlusion. Correct mechanism identification ensures adequate referral and prompt treatment that may reduce complications.
Keywords: Patent foramen ovale , peripheral arterial disease , acute limb ischemia , deep vein thrombosis , right-to-left shunt
Introduction
Acute limb ischemia (ALI) is an acute onset loss of limb perfusion [1].
The etiology of this disease includes a cardiac or arterial embolus (such as atrial fibrillation, left ventricular thrombus, or infective endocarditis), arterial thrombosis from peripheral arterial disease, or trauma [1, 2].
The classic presentation of arterial occlusion leading to ALI in these patients includes the 6 P’s: pain, pallor, pulselessness, paresthesia, poikilothermia, and paralysis [3].
The absence of pulse and paralysis are the most indicative signs of late-stage disease and are associated with poorer clinical outcomes [1, 2, 3, 4].
Complications of late-stage disease include gangrene, compartment syndrome, muscle cell liquefactive necrosis, and the accumulation of potassium ion, creatine kinase, myoglobin, superoxide, and lactic acid in the affected limb, termed myonephropathic metabolic syndrome [5].
Although little information is known regarding the incidence of ALI in the general population, it is estimated to comprise 10 to 16% of vascular workload [1, 2].
A patent foramen ovale (PFO) as a mechanism of ALI is rare despite its prevalence of up to 25% in adults [6].
We present a unique case of a PFO-induced embolism leading to acute limb ischemia and a literature review regarding its epidemiology, mechanism, and treatment.
Case Report
A 66-year-old man presented to the emergency department (ED) with a 4-day history of left foot pain, tingling, and numbness.
He stated that his foot appeared discolored at the onset of his symptoms.
Medical history included type 2 diabetes, dyslipidemia, and hypertension.
The patient also reported intermittent pain in his bilateral lower extremities, worse on ambulation and better with rest, associated with edema from the mid-shin distally to his toes.
He went to an urgent care center twice over the past month due to bilateral foot pain, for which he was prescribed ibuprofen.
The medication did not alleviate his symptoms. Social history was insignificant; the patient did not smoke.
On physical examination, he was tachycardic, in mild distress; all other vital signs, such as temperature, respirations, and oxygen saturation, were within normal limits.
The legs were swollen bilaterally, predominantly on the left, with a bluish discoloration (Figure 1a).
Figure 1.
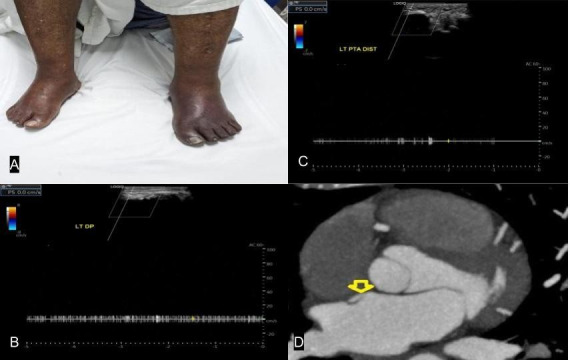
Bluish discoloration of the left lower extremity on physical examination (A).
Arterial duplex US showed no color or spectral Doppler signals identifiable in the left DP (B) and distal PT artery (C). CT angiography demonstrated an influx of contrast jet (arrow) to the inferior vena cava (D).
Additionally, the left lower extremity was cool to touch with non-existent dorsalis pedis (DP) and distal posterior tibial (PT) pulses; the limb lacked sensation, but motor function remained intact.
Laboratory values (Table 1) in the ED revealed anemia (6.3g/dL), leukopenia (4,200/mm3), hyponatremia (134 mEq/L,) and an international normalized ratio of 1.1.
Table 1.
Laboratory values on presentation at the emergency department
|
Variable |
Patient values |
Normal range |
|
Leukocyte count (White blood cell) |
4200/mm3 |
4500-11,000/mm3 |
|
Hemoglobin |
6.3g/dL |
12-16g/dL |
|
Platelets |
250,023/mm3 |
150,000-400,000/mm3 |
|
Absolute neutrophil count |
4.5 |
1.5-8.0 |
|
Urea nitrogen |
10mg/dL |
7-18mg/dL |
|
Creatinine |
0.8mg/dL |
0.6-1.2mg/dL |
|
Sodium (Na+) |
134mEq/L |
136-146mEq/L |
|
Potassium (K+) |
4.2mEq/L |
3.5-5.0mEq/L |
|
Calcium |
9.4mg/dL |
8.4-10.2mg/dL |
|
Magnesium (Mg2+) |
1.6mEq/L |
1.5-2.0mEq/L |
|
Prothrombin time (PT) |
12 seconds |
11-15 seconds |
|
Partial thromboplastin time (PTT)(activated) |
32 seconds |
25-40 seconds |
|
International normalized ratio (INR) |
1.1 |
0.8-1.2 |
|
Aspartate aminotransferase (AST) |
28U/L |
12-38U/L |
|
Alanine aminotransferase (ALT) |
25U/L |
10-40U/L |
|
Erythrocyte sedimentation rate (ESR) |
5.1 million/mm3 |
4.3-5.9 million/mm3 |
|
C-reactive protein |
0.2mg/dL |
<0.5mg/dL |
|
Vitamin B12 |
525pg/mL |
200-800pg/mL |
|
Folate |
7ng/mL |
2-10ng/mL |
|
Low density lipoprotein (LDL) |
124mg/dL |
<130mg/dL |
|
Thyroid stimulating hormone (TSH) |
2.1µU/mL |
0.4-4.0µU/mL |
Ankle-brachial index of the bilateral lower extremities was measured to be 0.8.
Duplex arterial ultrasound (US) confirmed occlusions of the left DP (Figure 1b) and distal PT (Figure 1c) arteries, while venous US was done simultaneously and demonstrated bilateral popliteal deep vein thrombosis (DVT).
Subsequently, a computed tomographic angiogram (CTA) of the chest showed a pulmonary embolus in the posterior basal segmental branch of the right lobe and incidentally revealed a saline-chaser contrast jet into the right atrium (Figure 1d), confirming the presence of a PFO.
An electrocardiogram done on work-up showed sinus rhythm, heart rate at 85/min, negative T-wave inversions on precordial leads V1-4, and evidence of right heart strain.
He was diagnosed with Rutherford IIb ALI of the left leg.
The patient was transferred to the general medicine ward and subsequently started intravenous heparin and a nothing-by-mouth diet.
Two hours after therapeutic anticoagulation, he underwent cardiac catheterization for PFO closure and surgical embolectomy.
He was discharged after 13 days of hospitalization with ambulatory anticoagulation.
At the 2-week follow-up, the patient reported improvement in his symptoms, expressing decreased pain and tingling of the left foot with numbness resolution.
Upon examination of the foot, pulses were palpable, and mild redness was noted on the plantar surface, indicating adequate reperfusion.
He was prescribed dual-antiplatelet therapy (aspirin and clopidogrel) and advised to follow up at the vascular surgery clinic in three months.
Written informed consent was obtained from the patient for the publication of this article and its associated image.
Discussion
One of the less common causes of ALI is a paradoxical embolism through a septal defect, as presented in this patient [4, 6, 7, 8].
A paradoxical embolism refers to the migration of a thrombus arising in the venous circulation into systemic arterial circulation via an arteriovenous shunt [2, 9].
Upon further workup with a CTA of the chest, this patient was found to have a PFO, described as an opening at the joining sections of the atrial septa primum and secundum, located by fossa ovalis that persists after birth [10].
PFOs exist in approximately 15 to 35% of the general population [6, 11].
The most common consequence as a result of the flaplike opening is a cerebrovascular accident; the incidence of ALI is more sporadic [12].
In fact, a paradoxical embolus through a PFO accounts for less than 2% of all arterial emboli, signifying its rare occurrence [13].
A previously reported case in a patient with several risk factors for hypercoagulability showed a grade IIb ischemia of the left lower limb secondary to an embolus through a previously silent PFO [11].
It is also important to note the pattern of presentation in patients with ALI due to a PFO-mediated paradoxical embolism.
In a systematic review of the literature aimed at identifying the patient populations most commonly affected as well as the anatomic distribution of emboli and treatment protocol, found that, in 51 patients with a PFO-mediated paradoxical embolism, 51% were men with an average age of presentation at 54 years [11, 13].
The study found a proclivity for the lower limbs at 72% and left-sided circulation at 82%; DVT was found in 36 patients (71%), and immediate anticoagulation was initiated in 60% of patients.
Lastly, fibrinolysis and embolectomy were done in 45 patients (88%).
In our case, this patient presented similarly to the overall findings mentioned in the systematic review, including the location of the embolus and the concurrent deep vein thromboembolism.
Most patients with a PFO appear asymptomatic because of the low pressure in both atria and anatomical position of the septum secundum; as a result, left-to-right shunting is insignificant [14, 15].
In physiologic conditions that increase the right atrial pressure, such as pulmonary embolism, as identified in this patient on initial presentation, the slit-like flap separates and allows right-to-left shunting as most PFOs are not clinically significant in size to facilitate embolism at resting physiologic pressures [15, 16, 17].
This patient presented with an occlusive DVT, likely serving as the source of the embolus.
In addition to therapeutic anticoagulation, he underwent operative embolectomy.
Urgent surgical revascularization was chosen as the treatment of choice in this scenario due to a Rutherford IIb classification of ALI, which highlights various sensory loss, motor function, doppler signals, and prognosis of the condition [7].
Patients with grade IIb require urgent revascularization [7, 18].
Stage III treatment options include amputation [7, 18].
In this patient, findings were significant for sensory loss in the limb with inaudible arterial doppler signals.
Catheter-directed thrombolysis is a relatively new and non-invasive method to treat ALI [19].
It is now accepted as the first-line treatment for selected patients with mild to moderate ALI (Rutherford I, II, and IIa).
The time frame from the onset of the symptoms to thrombolysis is crucial in attaining better outcomes, and ambulatory anticoagulation on discharge is essential for preventing recurrence.
Conclusion
Clinicians should have a high index of suspicion for unexplained arterial occlusion, such as ALI.
A paradoxical embolism, although infrequent, can involve any artery in the body [20].
A combination of DVT suspicion with symptoms of ALI should prompt a complete cardiac work-up.
Recurrent episodes of unexplained arterial occlusion should also raise an index of suspicion for a PFO-mediated embolism.
Awareness of this mechanism of occlusion with prompt recognition may limit disabilities and concurrent deaths from cerebrovascular accidents and pulmonary thromboembolism.
Funding
This article received no specific grant of support from any public or private agencies.
Conflict of interests
The authors have no conflict of interest to declare.
References
- 1.Obara H, Matsubara K, Kitagawa Y. Acute Limb Ischemia. Ann Vasc Dis. 2018;11(4):443–448. doi: 10.3400/avd.ra.18-00074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lyaker MR, Tulman DB, Dimitrova GT, Pin RH, Papadimos TJ. Arterial embolism. Int J Crit Illn Inj Sci. 2013;3(1):77–87. doi: 10.4103/2229-5151.109429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Santistevan JR. Acute Limb Ischemia: An Emergency Medicine Approach. Emerg Med Clin North Am. 2017;35(4):889–909. doi: 10.1016/j.emc.2017.07.006. [DOI] [PubMed] [Google Scholar]
- 4.Dilawari TH, Farooqui F, Aimon S, Jehan M, Latif S. Late Presentation of Acute Limb Ischemia: Causes and Outcomes. J Coll Physicians Surg Pak. 2023;33(1):103–106. doi: 10.29271/jcpsp.2023.01.103. [DOI] [PubMed] [Google Scholar]
- 5.Tsuji Y, Kambayashi J, Shiba E, Sakon M, Kawasaki T, Mori T. Involvement of calpain in myonephropathic metabolic syndrome (MNMS) Eur J Vasc Surg. 1994;8(4):482–488. doi: 10.1016/s0950-821x(05)80969-7. [DOI] [PubMed] [Google Scholar]
- 6.Kimberly Atianzar, Peter Casterella, Ming Zhang, Sameer Gafoor. Update on the Management of Patent Foramen Ovale in 2017: Indication for Closure and Literature Review. US Cardiology Review. 2017;11(2):75–79. [Google Scholar]
- 7.Hardman RL, Jazaeri O, Yi J, Smith M, Gupta R. Overview of classification systems in peripheral artery disease. Semin Intervent Radiol. 2014;31(4):378–388. doi: 10.1055/s-0034-1393976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Natarajan B, Patel P, Mukherjee A. Acute Lower Limb Ischemia-Etiology, Pathology, and Management. Int J Angiol. 2020;29(3):168–174. doi: 10.1055/s-0040-1713769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Geng J, Tian HY, Zhang YM, He S, Ma Q, Zhang JB, Liu Y, Tian H, Zhang D, Meng Y. Paradoxical embolism: A report of 2 cases. Medicine (Baltimore) 2017;96(26):e7332–e7332. doi: 10.1097/MD.0000000000007332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ravi D, Parikh RV, Aboulhosn J, Tobis JM. A New Syndrome of Patent Foramen Ovale Inducing Vasospastic Angina and Migraine. JACC Case Rep. 2023;28:102132–102132. doi: 10.1016/j.jaccas.2023.102132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Greenberg JW, Goff ZD, Mooser AC, Wittgen CM, Smeds MR. Acute Limb Ischemia Secondary to Patent Foramen Ovale-Mediated Paradoxical Embolism: A Case Report and Systematic Review of the Literature. Ann Vasc Surg. 2020;66(668):5–100. doi: 10.1016/j.avsg.2019.12.022. [DOI] [PubMed] [Google Scholar]
- 12.Homma S, Messé SR, Rundek T, Sun YP, Franke J, Davidson K, Sievert H, Sacco RL, Di Tullio. Patent foramen ovale. Nat Rev Dis Primers. 2016;2:15086–15086. doi: 10.1038/nrdp.2015.86. [DOI] [PubMed] [Google Scholar]
- 13.Kallel O, Charmake D, Chergui I, El Ouafi, Ismaili N. Patent foramen oval: A rare case of acute ischemia of the upper limb: A case with 2 year follow-up. Ann Med Surg (Lond) 2021;63:102188–102188. doi: 10.1016/j.amsu.2021.102188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moses KL, Beshish AG, Heinowski N, Baker KR, Pegelow DF, Eldridge MW, Bates ML. Effect of body position and oxygen tension on foramen ovale recruitment. Am J Physiol Regul Integr Comp Physiol. 2015;308(1):28–33. doi: 10.1152/ajpregu.00263.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alakbarzade V, Keteepe-Arachi T, Karsan N, Ray R, Pereira AC. Patent foramen ovale. Pract Neurol. 2020;20(3):225–233. doi: 10.1136/practneurol-2019-002450. [DOI] [PubMed] [Google Scholar]
- 16.Kerut EK, Norfleet WT, Plotnick GD, Giles TD. Patent foramen ovale: a review of associated conditions and the impact of physiological size. J Am Coll Cardiol. 2001;38(3):613–623. doi: 10.1016/s0735-1097(01)01427-9. [DOI] [PubMed] [Google Scholar]
- 17.Hara H, Virmani R, Ladich E, Mackey-Bojack S, Titus J, Reisman M, Gray W, Nakamura M, Mooney M, Poulose A, Schwartz RS. Patent foramen ovale: current pathology, pathophysiology, and clinical status. J Am Coll Cardiol. 2005;46(9):1768–76. doi: 10.1016/j.jacc.2005.08.038. [DOI] [PubMed] [Google Scholar]
- 18.Khan S, Hawkins BM. Acute Limb Ischemia Interventions. Interv Cardiol Clin. 2020;9(2):221–228. doi: 10.1016/j.iccl.2019.12.002. [DOI] [PubMed] [Google Scholar]
- 19.Morrison HL. Catheter-directed thrombolysis for acute limb ischemia. Semin Intervent Radiol. 2006;23(3):258–269. doi: 10.1055/s-2006-948765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lu J, Morton C, Hall M, Nagarsheth K. Paradoxical Embolism Is an Unusual Etiology of Acute Limb Ischemia in Patients Suffering from COVID-19 Infection. Vasc Endovascular Surg. 2024;58(1):13–19. doi: 10.1177/15385744231185641. [DOI] [PubMed] [Google Scholar]


