Abstract
This single‐arm confirmatory study (JCOG1305) aimed to evaluate the utility of interim positron emission tomography (iPET)‐guided therapy for newly diagnosed advanced‐stage classic Hodgkin lymphoma (cHL). Patients aged 16–60 years with cHL received two cycles of doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) and then underwent an iPET scan (PET2), which was centrally reviewed using a five‐point Deauville scale. PET2‐negative patients continued an additional four cycles of ABVD, whereas PET2‐positive patients switched to six cycles of escalated bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone (eBEACOPP). The co‐primary endpoints were 2‐year progression‐free survival (PFS) among all eligible and PET2‐positive patients. Ninety‐three patients were enrolled between January 2016 and December 2019. One patient was ineligible because of a diagnostic error. The median age of the 92 eligible patients was 35 (interquartile range, 28–48) years. Forty (43%) patients had stage III disease, and 43 (47%) had stage IV disease. The remaining nine (10%) patients had stage IIB disease with risk factors. Nineteen PET2‐positive (21%) patients received eBEACOPP, 18 completed six cycles of eBEACOPP, 73 PET2‐negative (79%) patients continued ABVD, and 70 completed an additional four cycles of ABVD. With a median follow‐up period of 41.1 months, the 2‐year PFS of 92 eligible patients and 19 PET2‐positive patients were 84.8% (80% confidence interval [CI], 79.2–88.9) and 84.2% (80% CI, 69.7–92.1), respectively. Both primary endpoints were met at the prespecified threshold. This study demonstrates that iPET‐guided therapy is a useful treatment option for younger patients with newly diagnosed advanced‐stage cHL. Registration number: jRCTs031180218.
Keywords: ABVD, advanced‐stage, cHL, escalated BEACOPP, interim PET‐guided
JCOG1305 demonstrated that interim PET‐guided therapy was useful for younger patients with newly diagnosed advanced‐stage cHL.
1. Introduction
Combination chemotherapy with doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) has been the preferred therapy for newly diagnosed advanced‐stage classic Hodgkin lymphoma (cHL). 1 , 2
Escalated bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone (eBEACOPP) have been developed to achieve a progression‐free survival (PFS) significantly superior to that of the ABVD regimen. 3 , 4 However, there was no difference in overall survival (OS) between the two regimens in the salvage setting of autologous hematopoietic stem cell transplantation (auto‐HSCT). 5 A previous meta‐analysis demonstrated that eBEACOPP had a 5%–10% 5‐year OS benefit compared with ABVD. 6 Although the acute and late toxicities of the eBEACOPP regimen are higher than those of ABVD, eBEACOPP is considered to be one of the most promising regimens for younger patients with high‐risk features. 7
Interim positron emission tomography (iPET) can predict clinical outcomes in patients with cHL. A prior retrospective study demonstrated that 18F‐fluorodeoxyglucose (FDG) PET findings after two cycles of ABVD (PET2) were good predictive markers for the efficacy of the ABVD regimen. Patients with PET2‐negative findings had a 2‐year PFS of 95%, whereas those with PET2‐positive findings had a 2‐year PFS of 13%. 8 Therefore, several clinical trials have been conducted to evaluate the efficacy of iPET‐guided therapy for advanced‐stage cHL, in which FDG‐PET scans have been performed in patients after two cycles of ABVD to modify subsequent treatment depending on the results (SWOG S0816, 9 RATHL, 10 HD0607 11 ). In these three trials, eBEACOPP or BEACOPP 14 was adapted to patients with PET2‐positive findings who were likely to be at a high risk of refractory or relapsing lymphoma, whereas those with less toxic treatments were adapted to patients with PET2‐negative findings (RATHL, 10 HD0607 11 ).
We conducted a multicenter prospective trial to evaluate the utility of an iPET‐guided treatment strategy for newly diagnosed advanced‐stage cHL.
2. Methods
2.1. Study design
This was a multicenter, single‐arm confirmatory study (JCOG1305, INNOVATE‐HL). Eligible patients with cHL received two cycles of ABVD as induction chemotherapy and then underwent an interim PET scan. Images were centrally reviewed using a five‐point Deauville scale (DS) 12 for PET findings for further response‐guided treatments.
Patients with negative interim PET findings (defined as DS scores 1–3) continued an additional four cycles of ABVD, whereas those with positive interim PET findings (DS score 4 or 5) switched to six cycles of eBEACOPP. Involved site radiation therapy (ISRT) was set as the treatment protocol if patients with a partial response had a single residual lesion after completion of chemotherapy (Figure S1).
2.2. Eligibility
The key eligibility criteria were as follows:
(1) newly diagnosed cHL (World Health Organization classification 2008);
(2) clinical stage III, IV, or IIB (Ann Arbor classification) with a bulky mediastinal or continuously invasive lesion to extranodal tissues;
(3) aged 16–60 years at enrollment;
(4) Eastern Cooperative Oncology Group performance status of 0–2;
(5) having a measurable lesion;
(6) no previous chemotherapy or radiotherapy;
(7) preserved organ function;
(8) provision of written informed consent by the patient.
The full inclusion and exclusion criteria are listed in Supplementary Document S1: Appendix S1.
Written informed consent was obtained from all patients before enrollment, and the study protocol was approved by the Protocol Review Committee of Japan Clinical Oncology Group (JCOG) and the institutional review board of each participating center.
2.3. Interim positron emission tomography (PET) and central judgment
Interim PET was performed between days 22 and 27 of the second cycle of induction ABVD chemotherapy. Each scan of the pretreatment and interim PET images was electronically transmitted as Digital Imaging and Communication in Medicine data to the diagnostic imaging consultation system at the National Cancer Center (Tokyo) for on‐demand centralized imaging judgment by an independent central committee consisting of expert diagnostic radiologists (Supplementary Document S2: Appendix S1 for PET imaging standardization/quality assurance and interim PET central judgment).
2.4. Chemotherapy
Induction ABVD therapy was administered on days 1 and 15 with cycles repeated once every 28 days. Primary prophylactic administration of granulocyte colony‐stimulating factor (G‐CSF) was not recommended in patients who received ABVD. If febrile neutropenia or infection with neutropenia occurred, G‐CSF and antibiotics were administered, followed by the prophylactic administration of both G‐CSF and antibiotics.
Post‐interim PET ABVD therapy was initiated on days 29–32 of the second cycle of induction ABVD therapy and was subsequently administered for an additional four cycles unless the protocol treatment discontinuation criteria were met.
eBEACOPP therapy was initiated on days 29–42 on the second cycle of induction ABVD therapy and was subsequently administered for six cycles. Primary prophylactic administration of G‐CSF from day 4 was set as the protocol treatment in patients who received eBEACOPP (Table S1).
2.5. Radiotherapy
ISRT was initiated within 14 weeks after the final chemotherapy dose. The total dose of ISRT was set at 36 Gy, with a 1.8 Gy per dose, administered once a day in fractions, over 4 weeks.
2.6. Endpoints and efficacy assessment
The objective disease response was assessed at each evaluation time point according to the revised criteria based on the 2007 Cheson criteria using PET. 13 The primary endpoint was a 2‐year PFS among all eligible patients and interim PET‐positive patients (co‐primary endpoints). PFS was defined as the time from the date of registration to the date of disease progression or death, whichever occurred first.
Secondary endpoints included the complete response (CR) rate, event‐free survival (EFS), OS, incidence of adverse events and secondary malignancy, and incidence of per‐protocol interim PET. EFS was defined as the time from the date of registration to the date of failure to achieve a CR at the end of the treatment protocol, disease progression, or death, whichever occurred first. OS was defined as the time from the date of registration to the date of death due to any cause. Adverse events were evaluated using Common Terminology Criteria for Adverse Events version 4.0. Bleomycin lung toxicity (BLT) was defined as a noninfectious pulmonary inflammation clinically diagnosed by each investigator following bleomycin administration.
2.7. Central pathology review
A central pathology review was performed by three hematopathologists according to the WHO classification system. Cases not diagnosed as classic Hodgkin lymphoma by the central pathology review were not excluded from the analysis the co‐primary endpoints.
2.8. Statistical analyses
This study confirmed the following two hypotheses: (1) the 2‐year PFS of eligible patients exceeds the threshold of 75%, and (2) the 2‐year PFS of interim PET‐positive patients exceeds the threshold of 35%. These thresholds were set based on the JCOG9305 14 and international validation studies. 15 To maintain a study‐wise alpha of 10%, a closed method was used; that is, hypothesis (2) would be examined only when hypothesis (1) was confirmed. If the lower limits of 80% confidence intervals (CIs) of the 2‐year PFS in eligible and interim PET‐positive patients exceeded each threshold, we would conclude that the co‐primary endpoints were met. The planned sample size was 105 to achieve a study‐wise power of 80%, assuming that the expected 2‐year PFS were 85% for eligible patients and 65% for interim PET‐positive patients.
PFS, EFS, and OS and their CIs were estimated using the Kaplan–Meier method and Greenwood formula. Data as of February 2, 2022, were included in the analysis. All statistical analyses were performed using SAS version 9.4. This study was registered with jRCTs031180218.
3. RESULTS
3.1. Patient characteristics
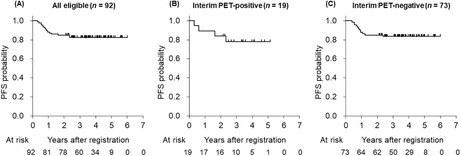
In total, 93 patients were enrolled from 35 institutions between January 2016 and December 2019 (Figure 1 and Table S2). Unfortunately, patient accrual was closed without achieving the target sample size (105 patients) owing to the termination of our diagnostic imaging consultation system. One patient was ineligible because of a diagnostic error. The baseline characteristics of the 92 eligible patients who received induction ABVD therapy and underwent an interim PET scan were as follows (Figure 1 and Table 1): the median age of the patients was 35 (interquartile range [IQR], 28–48) years; 58% were male; most of the patients (87 [95%]) had performance status of 0 or 1; 40 (43%) and 43 (47%) patients had been diagnosed as Ann Arbor stages III and IV, respectively; nine (10%) patients had stage IIB disease with bulky (≥10 cm) mediastinal or nodal lesion involving directly to extranodal lesion; and 51 (55%) and 14 (15%) patients had B symptoms and bulky lesions, respectively.
FIGURE 1.
Patient flow diagram. Flow diagram of patients with newly diagnosed classic Hodgkin lymphoma enrolled in the JCOG1305 study using interim PET‐guided ABVD or ABVD/escalated BEACOPP therapy. ABVD, doxorubicin, bleomycin, vinblastine, and dacarbazine; eBEACOPP, escalated bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone; ISRT, involved site radiation therapy; PET, positron emission tomography.
TABLE 1.
Baseline characteristics of 92 patients with interim PET‐guided therapy.
| All eligible n = 92 | Interim PET‐positive n = 19 | Interim PET‐negative n = 73 | |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Median age, years (IQR) | 35 (28–48) | 27 (24–44) | 35 (30–49) |
| Gender male | 53 (58) | 8 (42) | 45 (62) |
| ECOG‐PS | |||
| 0/1 | 87 (95) | 17 (89) | 70 (96) |
| 2 | 5 (5) | 2 (11) | 3 (4) |
| Ann Arbor stage | |||
| III/IV | 83 (90) | 17 (89) | 66 (90) |
| IIB | 9 (10) | 2 (11) | 7 (10) |
| B symptom (+) | 51 (55) | 11 (58) | 40 (55) |
| Maximum tumor diameter | |||
| Less than 5 cm | 49 (53) | 5 (26) | 44 (60) |
| 5 cm or more, but less than 10 cm | 28 (30) | 8 (42) | 20 (27) |
| 10 cm or more | 15 (16) | 6 (32) | 9 (12) |
| Bulky mediastinal lesion (+) | 14 (15) | 6 (32) | 8 (11) |
| International prognostic score | |||
| 0–3 | 63 (68) | 12 (63) | 51 (70) |
| 4–7 | 29 (32) | 7 (37) | 22 (30) |
| Eligible by pathological central review | 89 (97) | 19 (100) | 70 (96) |
Among the 92 eligible patients, 89 were diagnosed with cHL via central pathological review, but the remaining three were diagnosed as the following: T‐cell lymphoma (n = 1), diffuse large B‐cell lymphoma (n = 1), and fibrosis (n = 1).
3.2. Centralized 18F‐fluorodeoxyglucose‐PET/computed tomography review
Baseline and interim (PET2) scans of all 92 eligible patients were submitted for centralized review. Eighty‐eight patients (96%) underwent PET2 per‐protocol, the remaining four had delayed PET2 imaging. The central PET2 review was completed in <2 days in 84% of the patients and <4 days in 97% of the patients (Figure S2).
A PET2 scan showed 19 (21%) patients with positive findings. All of these patients received eBEACOPP: 18 completed six cycles of eBEACOPP, including one who received ISRT, and then 15 patients completed protocol treatment including ISRT; one patient discontinued eBEACOPP due to disease progression before two cycles of eBEACOPP and three patients did not receive ISRT due to patient refusal (n = 1) and physician's decision (n = 2). In contrast, the remaining 73 (79%) patients who had interim PET‐negative findings continued ABVD: 70 completed an additional four cycles of ABVD, including two who received ISRT, and then 69 patients completed protocol treatment including ISRT; three patients discontinued ABVD due to adverse events (n = 2; Aspergillus infection, alcoholic liver injury) and disease progression (n = 1), and one patient did not receive ISRT due to disease progression (n = 1) (Figure 1). In total, three patients received ISRT (8.9, 10.6, and 11.7 weeks) after the last dose of chemotherapy.
3.3. Therapy outcomes
3.3.1. Progression‐free survival
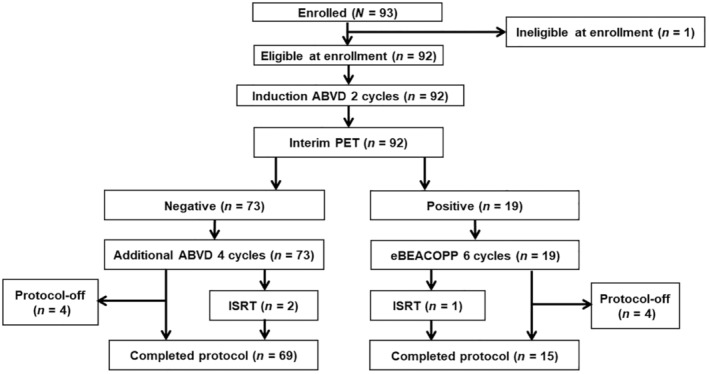
With a median follow‐up period of 41.1 (IQR, 29.7–53.1) months, the 2‐year PFS were 84.8% (80% CI, 79.2–88.9) and 84.2% (80% CI, 69.7–92.1) among all 92 eligible patients and 19 interim PET‐positive patients, respectively (co‐primary endpoints, Figure 2A,B). The 2‐year PFS was 84.9% in the 73 interim PET‐negative patients (Figure 2C).
FIGURE 2.
Progression‐free survival. (A) Progression‐free survival (PFS) for all 92 eligible patients. The 2‐year PFS was 84.8% (80% CI, 79.2–88.9) in all 92 eligible patients. (B) PFS for 19 interim PET‐positive patients. The 2‐year PFS was 84.2% (80% CI, 69.7–92.1) in the 19 interim PET‐positive patients. (C) PFS for 73 interim PET‐negative patients. The 2‐year PFS was 84.9% in the 73 interim PET‐negative patients.
The 2‐year PFS for the 92 eligible patients stratified by clinical stages II, III, and IV were 88.9%, 85.0%, and 83.7%, respectively (Figure S3). The 2‐year PFS for 19 interim PET‐positive patients stratified by DS scores 4 and 5 were 86.7% and 75.0%, respectively, whereas the 2‐year PFS for 73 interim PET‐negative patients stratified by DS scores 1/2 and 3 were 88.4% and 80.0%, respectively (Figure S4A,B).
Among the 89 eligible patients with a confirmed cHL diagnosis by the central review, the 2‐year PFS were 84.2% and 85.7% for 19 interim PET‐positive patients and 70 interim PET‐negative patients, respectively (Figure S5A,B).
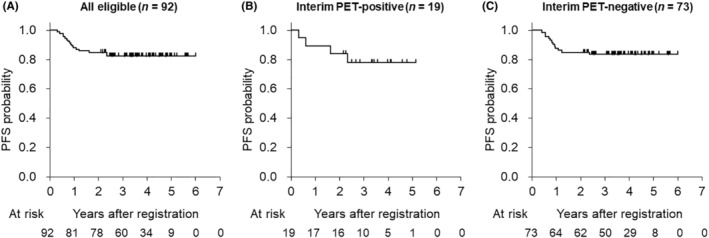
3.3.2. Event‐free survival
The 2‐year EFS was 76.1% among the 92 eligible patients. The 2‐year EFS were 68.4% and 78.1% for the 19 interim PET‐positive and 72 interim PET‐negative patients, respectively (Figure 3A–C). Of the 92 eligible patients, 24 events were observed during follow‐up as follows: death without lymphoma progression (n = 1), lymphoma progression (n = 13), and non‐CR at the end of protocol treatment (n = 10).
FIGURE 3.
Event‐free survival. (A) Event‐free survival (EFS) for all 92 eligible patients. The 2‐year EFS was 76.1% in the 92 eligible patients. (B) EFS for 19 interim PET‐positive patients. The 2‐year EFS was 68.4% in the 19 interim PET‐positive patients. (C) EFS for 73 interim PET‐negative patients. The 2‐year EFS was 78.1% in 72 interim PET‐negative patients.
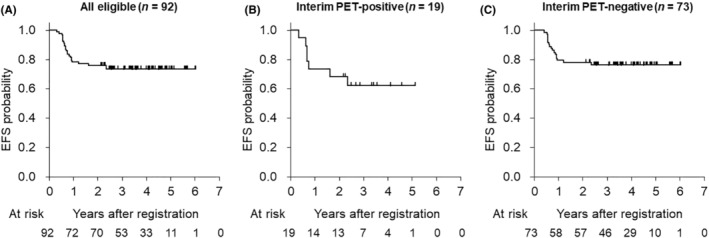
3.3.3. Overall survival
The 2‐year OS was 98.9%; two patients died due to interstitial pneumonia after autologous HSCT and brain hemorrhage without relapsing cHL among the interim PET‐positive patients, whereas no patients died among the interim PET‐negative patients (Figure 4A–C).
FIGURE 4.
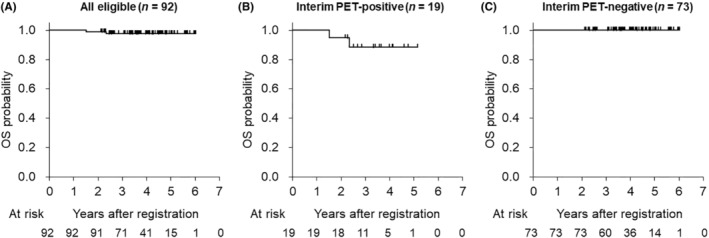
Overall survival. (A) Overall survival (OS) for all 92 eligible patients. The 2‐year OS was 98.9% in the 92 eligible patients. (B) OS for 19 interim PET‐positive patients. The 2‐year OS was 94.7% in the 19 interim PET‐positive patients. (C) OS for 73 interim PET‐negative patients. The 2‐year OS was 100% in 72 interim PET‐negative patients.
3.3.4. Complete response rate
The CR rates were 81.5%, 73.7%, and 83.6% in the 92 eligible patients, 19 interim PET‐positive patients, and 73 interim PET‐negative patients, respectively. Seven patients were determined to have progressive disease at the end of the protocol treatment; two and five were interim PET‐positive and interim PET‐negative patients, respectively.
3.3.5. Relative dose intensity
The average relative dose intensities (ARDIs) of induction ABVD (n = 92), additional ABVD (n = 73), and eBEACOPP (n = 19) were 98.6% (±4.0), 96.7% (±5.7), and 82.2% (±9.3%), respectively. Among the 19 patients who received eBEACOPP, 15 (78.9%) required dose reduction owing to treatment toxicities.
3.3.6. Toxicity
The toxicities observed during the induction of ABVD, additional ABVD, and eBEACOPP are summarized in Table 2. Grade 3 or greater neutropenia and thrombocytopenia were more frequent in eBEACOPP (100% and 94.7%, respectively) compared with additional ABVD (68.5% and 1.4%, respectively). BLT occurred in nine patients: two (2.2%) during induction ABVD (n = 92), four (5.5%) during additional ABVD (n = 73), and three (15.8%) patients experienced BLT during eBEACOPP (n = 19) chemotherapy. Six patients who developed BLT during chemotherapy were discontinued from further bleomycin administration. None of the patients experienced BLT‐related death during follow‐up.
TABLE 2.
Adverse events in induction ABVD, additional ABVD, escalated BEACOPP.
| NCI‐CTCAE ver.4.0 | Induction ABVD (n = 92) | Additional ABVD (n = 73) | Escalated BEACOPP (n = 19) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Any grade % | G3/4% | G3 | G4 | Any grade % | G3/4% | G3 | G4 | Any grade % | G3/4% | G3 | G4 | |
| Leukopenia | 83.7 | 46.7 | 33 | 10 | 83.6 | 47.9 | 26 | 9 | 100.0 | 100.0 | 0 | 19 |
| Neutropenia | 98.9 | 75.0 | 27 | 42 | 95.9 | 68.5 | 23 | 27 | 100.0 | 100.0 | 0 | 19 |
| Lymphocytopenia | 83.7 | 37.0 | 27 | 7 | 84.9 | 34.2 | 24 | 1 | 100.0 | 100.0 | 0 | 19 |
| Anemia | 43.5 | 2.2 | 2 | 0 | 45.2 | 2.7 | 2 | 0 | 68.4 | 57.9 | 10 | 1 |
| Thrombocytopenia | 23.9 | 1.1 | 1 | 0 | 9.6 | 1.4 | 0 | 1 | 100.0 | 94.7 | 7 | 11 |
| Bilirubin increased | 6.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| AST increased | 50.0 | 0 | 0 | 0 | 45.2 | 1.4 | 0 | 1 | 78.9 | 0.0 | 0 | 0 |
| ALT increased | 67.4 | 3.3 | 3 | 0 | 53.4 | 1.4 | 1 | 0 | 94.7 | 5.3 | 1 | 0 |
| Creatinine increased | 6.5 | 0 | 0 | 0 | 5.5 | 0 | 0 | 0 | 5.3 | 0 | 0 | 0 |
| Hyperglycemia | 16.3 | 0 | 0 | 0 | 20.5 | 1.4 | 1 | 0 | 21.1 | 0 | 0 | 0 |
| Hyponatremia | 23.9 | 0 | 0 | 0 | 13.7 | 1.4 | 1 | 0 | 21.1 | 5.3 | 1 | 0 |
| Hypokalemia | 2.2 | 0 | 0 | 0 | 2.7 | 0 | 0 | 0 | 36.8 | 10.5 | 2 | 0 |
| PN: sensory | 31.5 | 0 | 0 | 0 | 38.4 | 0 | 0 | 0 | 47.4 | 5.3 | 1 | 0 |
| PN: motor | 5.4 | 0 | 0 | 0 | 5.5 | 0 | 0 | 0 | 5.3 | 0 | 0 | 0 |
| Constipation | 8.7 | 0 | 0 | 0 | 32.9 | 0 | 0 | 0 | 31.6 | 0 | 0 | 0 |
| Diarrhea | 7.6 | 0 | 0 | 0 | 6.8 | 0 | 0 | 0 | 10.5 | 0 | 0 | 0 |
| Nausea | 72.8 | 1.1 | 1 | – | 65.8 | 2.7 | 2 | ‐ | 63.2 | 5.3 | 1 | – |
| Oral mucositis | 22.8 | 1.1 | 1 | 0 | 16.4 | 2.7 | 2 | 0 | 15.8 | 0 | 0 | 0 |
| Ileus | 1.1 | 1.1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Anorexia | 44.6 | 1.1 | 1 | 0 | 38.4 | 0 | 0 | 0 | 47.4 | 0 | 0 | 0 |
| Fever | 8.7 | 1.1 | 1 | 0 | 17.8 | 0 | 0 | 0 | 36.8 | 0 | 0 | 0 |
| Febrile neutropenia | 5.4 | 5.4 | 5 | 0 | 8.2 | 8.2 | 6 | 0 | 26.3 | 26.3 | 5 | 0 |
| Coughing | 4.3 | 0 | 0 | – | 6.8 | 1.4 | 1 | – | 10.5 | 0 | 0 | – |
| Dyspnea | 1.1 | 0 | 0 | 0 | 2.7 | 1.4 | 1 | 0 | 5.3 | 5.3 | 1 | 0 |
| Hypoxemia | 1.1 | 0 | 0 | 0 | 1.4 | 1.4 | 1 | 0 | 5.3 | 5.3 | 1 | 0 |
| Pneumonia | 1.1 | 0 | 0 | 0 | 5.5 | 1.4 | 1 | 0 | 0 | 0 | 0 | 0 |
| Any infections | 10.9 | 4.3 | 4 | 0 | 24.7 | 2.7 | 2 | 0 | 26.3 | 0 | 0 | 0 |
Grade 4 non‐hematologic toxicity was observed in three patients, which included hypertriglyceridemia, liver damage (elevated aspartate aminotransferase), and pericardial tamponade with pericardial effusion, which was considered not to be causally related to the protocol treatment. No protocol for treatment‐related deaths was reported.
Diffuse large B‐cell lymphoma developed as a secondary malignancy in one patient with interim PET‐negative findings as a secondary malignancy 4.6 years after enrollment.
3.3.7. Salvage treatment
In total, 14 patients received salvage treatments during follow‐up: 13 received salvage treatments after confirmed disease progression, but the remaining patient received autologous HSCT without lymphoma progression (owing to non‐CR at the completion of eBEACOPP chemotherapy). Thirteen patients received systemic chemotherapy, and the remaining patient received radiotherapy as the first salvage treatment. Twelve and three patients underwent autologous and allogeneic HSCT, respectively, including one who underwent allogeneic HSCT for relapse after autologous HSCT.
4. DISCUSSION
This single‐arm confirmatory study (JCOG1305, INNOVATE‐HL) of newly diagnosed advanced‐stage cHL showed 2‐year PFS of 84.8% and 84.2% in 92 eligible and 19 PET2‐positive patients, respectively. The co‐primary endpoints were met because these results were significantly better than the prespecified threshold 2‐year PFS of 75% and 35% among all eligible and PET2‐positive patients, respectively. In particular, the results of patients with PET2‐positive findings in JCOG1305 seemed to be superior to those in previous trials (60%–68% in 2‐ or 3‐year PFS, in SWOG S0816, 9 RATHL, 10 HD0607 11 ). Consistent with the three previous trials, the proportion of patients with PET2‐positive findings was approximately 20% in JCOG1305.
The comparison of the baseline characteristics and outcomes of JCOG1305 and SWOG S0816 are summarized in Table S3. 9 , 16 In SWOG S0816, 331 eligible patients with a median age of 32 years were limited to clinical stage III or IV. The proportion of patients with PET2‐positive findings was 18%; subsequently, all PET2‐positive patients were scheduled to switch to eBEACOPP. However, only 80% of the patients received eBEACOPP because of patient refusal. The ARDIs in additional ABVD and eBEACOPP were 93% and 75%, respectively, and ISRT was not permitted in SWOG S0816. 9 The 2‐year PFS were 79% and 64% for all eligible and PET‐2 positive patients, respectively. Compared with the results of SWOG S0816, 9 , 16 our current study is thought to have better PFS, partly because patients with clinical stage II disease with risk factors were enrolled (0% vs. 10%), all patients with PET‐2 positive findings received eBEACOPP (80% vs. 100%), and the patients received ABVD and eBEACOPP while maintaining a high ARDI (ABVD, 93% vs. 97%; eBEACOPP, 75% vs. 82%). Dose‐intensity chemotherapy is essential for improving the outcomes of patients with cHL. ABVD was safely and effectively administered at >99% dose intensity without G‐CSF in a retrospective study. 17 Furthermore, dose‐intensified BEACOPP (eBEACOPP or BEACOPP‐14) is the preferred regimen for younger patients with advanced‐stage cHL in Europe, suggesting that maintaining the dose intensity of BEACOPP can lead to improved outcomes in these patients.
In the current study, BLT occurred in nine (9.8%) patients: two, four, and three patients experienced BLT during induction ABVD, additional ABVD, and eBEACOPP, respectively, but no patients experienced BLT‐related death. In the RATHL study, patients with PET2‐negative findings were randomly assigned to continue ABVD (ABVD group) or to omit bleomycin (AVD group) in cycles 3–6, whereas those with PET2‐positive findings received BEACOPP‐14 or eBEACOPP. 10 In the initial presentation of RATHL, the 3‐year PFS in the AVD group was slightly below the prespecified non‐inferiority margin compared with the PFS in the ABVD group. Recently, a long‐term follow‐up study of RATHL with a median follow‐up period of 7.3 years showed that there was no statistically significant difference in the 7‐year PFS (81.0% and 79.2% in the ABVD and AVD groups, respectively) among PET2‐negative randomized eligible patients, which concluded that bleomycin could be safely omitted in the subsequent treatment of PET2‐negative patients. 18 iPET‐guided therapy, which allows switching to AVD in PET2‐negative patients, may be important, especially in elderly patients with cHL who are at high risk of BLT.
The 2‐year EFS of 92 eligible patients in our study was 76.1%, and there were 24 events, including one death without disease progression, 13 disease progression, and 10 non‐CR at the end of protocol treatment in JCOG1305. All 13 patients with disease progression received salvage treatment, whereas only one of the 10 patients who were non‐CR at the end of the protocol treatment received salvage treatment during follow‐up. Nine of the 10 patients who were in non‐CR at the end of the protocol treatment were still undergoing follow‐up without salvage treatment or disease progression. Although confirmation of cHL‐related events with long‐term follow‐up is required, a subset of patients with non‐CR after initial treatment for cHL may not require salvage chemotherapy, including HSCT.
The current study has some limitations. First, JCOG1305 was a single‐arm study with a relatively small sample size. We planned from the beginning to consider the results of previous trials (SWOG S0816, RATHL) with JCOG1305 to determine the significance of iPET‐guided therapy in advanced‐stage cHL. Second, as already mentioned, the follow‐up period was short, and long‐term follow‐up is necessary to observe events, such as late relapse of lymphoma and secondary malignancies. Third, patient accrual in the current study was closed without achieving the prespecified target number of patients because of the termination of our diagnostic imaging consultation system. However, the co‐primary endpoints were met.
In conclusion, this JCOG1305 (INNOVATE‐HL) study demonstrated that the iPET‐guided treatment strategy was useful for younger patients with newly diagnosed advanced‐stage cHL. Notably, six cycles of eBEACOPP is a feasible and effective regimen for patients with PET2‐positive cHL.
AUTHOR CONTRIBUTIONS
Shigeru Kusumoto: Conceptualization; investigation; writing – original draft; writing – review and editing. Wataru Munakata: Investigation; writing – review and editing. Ryunosuke Machida: Conceptualization; formal analysis; writing – original draft; writing – review and editing. Takashi Terauchi: Investigation; writing – review and editing. Hiroaki Onaya: Investigation; writing – review and editing. Masahiko Oguchi: Investigation; writing – review and editing. Shinsuke Iida: Investigation; writing – review and editing. Kisato Nosaka: Investigation; writing – review and editing. Yasuhiro Suzuki: Investigation; writing – review and editing. Yasuhiko Harada: Investigation; writing – review and editing. Kana Miyazaki: Investigation; writing – review and editing. Masaki Maruta: Investigation; writing – review and editing. Noriko Fukuhara: Investigation; writing – review and editing. Tomomi Toubai: Investigation; writing – review and editing. Nobuko Kubota: Investigation; writing – review and editing. Ken Ohmachi: Investigation; writing – review and editing. Toko Saito: Investigation; writing – review and editing. Shinya Rai: Investigation; writing – review and editing. Ishikazu Mizuno: Investigation; writing – review and editing. Suguru Fukuhara: Investigation; writing – review and editing. Mai Takeuchi: Investigation; writing – review and editing. Ukihide Tateishi: Investigation; writing – review and editing. Dai Maruyama: Investigation; writing – review and editing. Kunihiro Tsukasaki: Funding acquisition; investigation; writing – review and editing. Hirokazu Nagai: Conceptualization; funding acquisition; investigation; writing – original draft; writing – review and editing.
FUNDING INFORMATION
This study was supported in part by the National Cancer Center Research and Development Funds (25‐A‐13, 26‐A‐4, 29‐A‐3, 2020‐J‐3, 2023‐J‐03) and AMED (grant numbers JP16ck0106220 and 19ck0106509).
CONFLICT OF INTEREST STATEMENT
S.K. reports research funding from Bristol‐Myers Squibb, Meiji Seika Pharma Co. and AbbVie; and honoraria from Janssen, Chugai, Ono, and Daiichi Sankyo. W.M. reports research funding from Janssen, Ono, Genmab, Nippon Shinyaku; and honoraria from Takeda, Ono, Eisai, Chugai, Bristol‐Myers Squibb, Astra Zeneca, Nippon Shinyaku, SymBio, Gilead Sciences, Nippon Kayaku, MSD, Mundi pharma, and Janssen. R.M. has nothing to disclose. T.T. has nothing to disclose. H.O. has nothing to disclose. M.O. has nothing to disclose. S.I. reports consultancies from Janssen, Bristol‐Myers Squibb, Sanofi, Takeda, Pfizer, Glaxo Smith Klein, AbbVie, Novartis, Regeneron; research funding from Janssen, Bristol‐Myers Squibb, Sanofi, Ono, Takeda, Pfizer, Daiichi Sankyo, Amgen, Kyowa Kirin, GlaxoSmithKline, Chugai, AbbVie, Alexion, Novartis, and Shionogi; and honoraria from Janssen, Bristol‐Myers Squibb, Sanofi, Ono, Takeda, and Pfizer. K.N. has nothing to disclose. Y.S. has nothing to disclose. Y.H. has nothing to disclose. K.M. reports research funding from Kyowa Kirin and Zenyaku; and honoraria from Janssen. M.M. has nothing to disclose. N.F. reports research funding from AbbVie, Chugai, Chordia Therapeutics, Genmab, Incyte, Kyowa Kirin, Loxo Oncology and Takeda; and honoraria from BMS, Chugai, and SymBio. T.T. reports research funding from AbbVie, IQVIA, Incyte, Pfizer, Novartis, Amgen, and Zenyaku. N.K. has nothing to disclose. K.O. reports honoraria from Chugai. T.S. reports research funding from Meiji Seika Pharma Co. and AbbVie. S.R. has nothing to disclose. I.M. has nothing to disclose. S.F. reports a consultancy from Otsuka; research funding from Chugai, LOXO oncology, and Mitsubishi Tanabe; and honoraria from Janssen, Ono, Takeda, Amgen, Chugai, AbbVie, and Astra Zeneca. M.T. has nothing to disclose. U.T. has nothing to disclose. D.M. reports research funding from Amgen Astellas Biopharma, Janssen, Takeda, Eisai, Chugai, Ono, MSD, Astellas, Otsuka, Novartis, Kyowa Kirin, Sanofi, Bristol‐Myers Squibb, Taiho, Eli Lilly, AbbVie, Astra Zeneca, and Genmab; and honoraria from Janssen, Takeda, Eisai, Chugai, Ono, Kyowa Kirin, MSD, Zenyaku Kogyo, Bristol‐Myers Squibb, Astra Zeneca, Mundi pharma, Nippon Shinyaku, SymBio, AbbVie, Sanofi, and Genmab. K.T. reports consultancies from Meiji Seika, Daiichi Sankyo, HUYABIO, Ono, Solasia, Yakuruto; research funding from Kyowa Kirin, Meiji Seika, Bristol‐Myers Squibb, Byer, Daiichi Sankyo, HUYABIO, Regeneron, and Mitsubishi Tanabe; and honoraria from Chugai, Eisai, Takeda, Meiji Seika, Solasia, and Daiichi Sankyo. H.N. reports research funding from AbbVie, Astra Zene, Beigene, Genmab, HUYA, Janssen, Eli Lilly, Takeda, Kyowa Kirin, MSD, Mitsubishi Tanabe, Chugai, Daiichi Sankyo, Celgene, Zenyaku Kogyo, Solasia, Ono, Chugai, Takeda, and Nippon Shinyaku; and honoraria from AbbVie, Astra Zene, Genmab, Janssen, Eli Lilly, Takeda, Kyowa Kirin, MSD, Eisai, Novartis, Ono, Sumitomo, Chugai, Meiji Seika, Mundi pharma, GSK, BMS, and Nippon Shinyaku. Other authors do not have a conflict of interest. Shinsuke Iida is an editorial board member for Cancer Science.
ETHICS STATEMENTS
Approval of the research protocol by an Institutional Reviewer Board: The study protocol was approved by the Protocol Review Committee of Japan Clinical Oncology Group (JCOG) and the institutional review board of each participating center.
Informed Consent: Written informed consent was obtained from all patients before enrollment.
Registry and the Registration No. of the study/trial: jRCTs031180218.
Animal Studies: N/A.
Supporting information
Appendix S1.
ACKNOWLEDGMENTS
We would like to thank the patients who participated in this study and their families as well as the clinical research coordinators and operations staff at the participating sites. We also thank the staff as follows: the members of the JCOG Data Center and JCOG Operations Office for their support in this study; Dr. Keiichi Ishihara (Nippon Medical School), Dr. Mitsuaki Tatsumi (Osaka University Hospital), Dr. Hidetaka Sato (Japanese Red Cross Medical Center), and Dr. Tomohiro Kaneta (Tohoku University) for their central review for interim PET imaging; Dr. Jun‐Ichi Tamaru (Saitama Medical University) and Dr. Naoko Asano (Nagano Prefectural Shinshu Medical Center) for their central review for histopathology specimens; Dr. Satoshi Ishikura (Radiation Therapy Support Center) for his QA/QC for ISRT; Dr. Tatsuya Suzuki (National Cancer Center Hospital), Dr. Michinori Ogura (Japanese Red Cross Aichi Medical Center Nagoya Daini Hospital), Dr. Kensei Tobinai (National Cancer Center), and Dr. Tomomitsu Hotta (National Cancer Center) for their enlightening advice on this study.
Kusumoto S, Munakata W, Machida R, et al. Interim PET‐guided ABVD or ABVD/escalated BEACOPP for newly diagnosed advanced‐stage classic Hodgkin lymphoma (JCOG1305). Cancer Sci. 2024;115:3384‐3393. doi: 10.1111/cas.16281
Statement of prior presentation: This study was presented at the 64th American Society of Hematology Annual Meeting and Exposition, New Orleans, USA, December 10–13, 2022 (poster presentation abstract #1614).
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request. After deidentification, individual participant data that underlie the results reported in this article, will be shared if researchers, whose proposed use of the data has been approved by the investigators from the Japan Clinical Oncology Group‐Lymphoma Study Group (JCOG‐LSG), identified this purpose. Proposals for access should be sent to the corresponding author.
REFERENCES
- 1. Bonadonna G, Zucali R, Monfardini S, De Lena M, Uslenghi C. Combination chemotherapy of Hodgkin's disease with adriamycin, bleomycin, vinblastine, and imidazole carboxamide versus MOPP. Cancer. 1975;36:252‐259. [DOI] [PubMed] [Google Scholar]
- 2. Canellos GP, Anderson JR, Propert KJ, et al. Chemotherapy of advanced Hodgkin's disease with MOPP, ABVD, or MOPP alternating with ABVD. N Engl J Med. 1992;327:1478‐1484. [DOI] [PubMed] [Google Scholar]
- 3. Diehl V, Franklin J, Pfreundschuh M, et al. Standard and increased‐dose BEACOPP chemotherapy compared with COPP‐ABVD for advanced Hodgkin's disease. N Engl J Med. 2003;348:2386‐2395. [DOI] [PubMed] [Google Scholar]
- 4. Sieber M, Bredenfeld H, Josting A, et al. 14‐day variant of the bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone regimen in advanced‐stage Hodgkin's lymphoma: results of a pilot study of the German Hodgkin's lymphoma study group. J Clin Oncol. 2003;21:1734‐1739. [DOI] [PubMed] [Google Scholar]
- 5. Viviani S, Zinzani PL, Rambaldi A, et al. ABVD versus BEACOPP for Hodgkin's lymphoma when high‐dose salvage is planned. N Engl J Med. 2011;365:203‐212. [DOI] [PubMed] [Google Scholar]
- 6. Skoetz N, Trelle S, Rancea M, et al. Effect of initial treatment strategy on survival of patients with advanced‐stage Hodgkin's lymphoma: a systematic review and network meta‐analysis. Lancet Oncol. 2013;14:943‐952. [DOI] [PubMed] [Google Scholar]
- 7. Wongso D, Fuchs M, Plutschow A, et al. Treatment‐related mortality in patients with advanced‐stage hodgkin lymphoma: an analysis of the german hodgkin study group. J Clin Oncol. 2013;31:2819‐2824. [DOI] [PubMed] [Google Scholar]
- 8. Gallamini A, Hutchings M, Rigacci L, et al. Early interim 2‐[18F]fluoro‐2‐deoxy‐D‐glucose positron emission tomography is prognostically superior to international prognostic score in advanced‐stage Hodgkin's lymphoma: a report from a joint Italian‐Danish study. J Clin Oncol. 2007;25:3746‐3752. [DOI] [PubMed] [Google Scholar]
- 9. Press OW, Li H, Schoder H, et al. US intergroup trial of response‐adapted therapy for stage III to IV Hodgkin lymphoma using early interim fluorodeoxyglucose‐positron emission tomography imaging: southwest oncology group S0816. J Clin Oncol. 2016;34:2020‐2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Johnson P, Federico M, Kirkwood A, et al. Adapted treatment guided by interim PET‐CT scan in advanced Hodgkin's lymphoma. N Engl J Med. 2016;374:2419‐2429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gallamini A, Tarella C, Viviani S, et al. Early chemotherapy intensification with escalated BEACOPP in patients with advanced‐stage Hodgkin lymphoma with a positive interim positron emission tomography/computed tomography scan after two ABVD cycles: long‐term results of the GITIL/FIL HD 0607 trial. J Clin Oncol. 2018;36:454‐462. [DOI] [PubMed] [Google Scholar]
- 12. Barrington SF, Qian W, Somer EJ, et al. Concordance between four European centres of PET reporting criteria designed for use in multicentre trials in Hodgkin lymphoma. Eur J Nucl Med Mol Imaging. 2010;37:1824‐1833. [DOI] [PubMed] [Google Scholar]
- 13. Cheson BD, Pfistner B, Juweid ME, et al. Revised response criteria for malignant lymphoma. J Clin Oncol. 2007;25:579‐586. [DOI] [PubMed] [Google Scholar]
- 14. Ogura M, Itoh K, Kinoshita T, et al. Phase II study of ABVd therapy for newly diagnosed clinical stage II‐IV Hodgkin lymphoma: Japan clinical oncology group study (JCOG 9305). Int J Hematol. 2010;92:713‐724. [DOI] [PubMed] [Google Scholar]
- 15. Biggi A, Gallamini A, Chauvie S, et al. International validation study for interim PET in ABVD‐treated, advanced‐stage hodgkin lymphoma: interpretation criteria and concordance rate among reviewers. J Nucl Med. 2013;54:683‐690. [DOI] [PubMed] [Google Scholar]
- 16. Stephens DM, Li H, Schoder H, et al. Five‐year follow‐up of SWOG S0816: limitations and values of a PET‐adapted approach with stage III/IV Hodgkin lymphoma. Blood. 2019;134:1238‐1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Evens AM, Cilley J, Ortiz T, et al. G‐CSF is not necessary to maintain over 99% dose‐intensity with ABVD in the treatment of Hodgkin lymphoma: low toxicity and excellent outcomes in a 10‐year analysis. Br J Haematol. 2007;137:545‐552. [DOI] [PubMed] [Google Scholar]
- 18. Luminari S, Fossa A, Trotman J, et al. Long‐term follow‐up of the response‐adjusted therapy for advanced Hodgkin lymphoma trial. J Clin Oncol. 2023;42:JCO2301177. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request. After deidentification, individual participant data that underlie the results reported in this article, will be shared if researchers, whose proposed use of the data has been approved by the investigators from the Japan Clinical Oncology Group‐Lymphoma Study Group (JCOG‐LSG), identified this purpose. Proposals for access should be sent to the corresponding author.


