Abstract
Background
Over the years, with the improvement of diagnostic and therapeutic capabilities for hip joint diseases and the advancements in surgical technology, hip arthroscopy has been extensively used. At present, there is ongoing controversy among scholars about whether it is necessary to close the joint capsule after hip arthroscopy. In addition, the clinical effect of repairing the hip joint capsule after hip arthroscopy remains uncertain.
Purpose
To evaluate the effect of our modified shoelace suture technique on postoperative hip function and to investigate whether complete closure of the hip capsule is reliable and safe.
Study Design
Retrospective study; Levels of evidence: III.
Methods
A retrospective review was conducted on patients undergoing hip arthroscopy by a solitary high-volume hip arthroscopic surgeon. The patients were categorized into two groups. The first group consisted of patients who underwent the modified shoelace continuous capsular closure technique. The other group consisted of those who did not receive capsular closure after hip arthroscopy. Patient-reported outcomes including modified Harris Hip Score (mHHS), Hip Outcome Score of Activities of Daily Living (HOS-ADL), Hip Outcome Score Sport-Specific Subscale (HOS-SSS), and visual analogue scale (VAS) were obtained at a minimum of 12 months. Any complications during follow-up were identified and recorded.
Results
A total of 100 patients were followed up for 12–15 months, with an average of (12.3 ± 5.3) months in the study. There were 50 patients in the shoelace capsular closure group (CC group) and 50 patients in the non-capsular closure group (NC group). The surgical time in the suture group was significantly longer than that in the non-suture group. However, there was no statistically significant disparity in the length of hospital stay between the two groups. The mHHS, HOS-SSS, HOS-ADL, and VAS of the CC and NC group were significantly improved compared to preoperative scores at 6 and 12 postoperative months (P < 0.001). Compared with the NC group, the CC group showed a significant improvement in the mHHS, HOS-SSS, HOS-ADL, and VAS at 6 postoperative months (t = 4.885, P<0.001; t = 5.984, P<0.001; t = 4.279, P<0.001; t = 3.875, P<0.001). The mHHS, HOS-SSS, HOS-ADL, and VAS at 12 postoperative months were significantly better in the CC group than in the NC group (t = 5.165, P<0.001; t = 3.697, P<0.001; t = 4.840, P<0.001; t = 3.579, P = 0.001). There were no serious complications during the perioperative period.
Conclusion
The modified shoelace continuous capsular closure technique is a reliable and secure method that can be used as an alternative to the conventional capsular closure. It is recommended to perform routine intraoperative repair of the articular capsule at the end of hip arthroscopy, as this has a positive influences on the functional results at short-term follow-up.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12891-024-07894-0.
Keywords: Hip arthroscopy, Capsular closure, Capsulotomy, Femoroacetabular impingement
Introduction
With the improvement of diagnostic and therapeutic capabilities for hip diseases and the progress of surgical technology, hip arthroscopic surgery has experienced rapid development and is now extensively utilized for treating hip internal lesions and peripheral hip diseases [1]. However, hip arthroscopy usually requires an incision of the hip capsule to achieve adequate surgical view and workspace. Most surgeons who perform hip arthroscopic surgery opt to perform an interportal capsulotomy [2], which involves making a horizontal cut in the anterior part of the hip joint capsule. A systematic evaluation found that the interportal capsulotomy was used in 60% of cases, the T-capsulotomy was employed in 16% of cases, and usage of a capsulotomy was not reported in 23%. In addition to this, performing capsular closure is a crucial technical strategy to reduce the rate of prosthetic replacement compared to unrepaired capsulotomy [3]. Surgeons may use a “T” incision to improve joint exposure [4], but this technique can harm the iliofemoral ligament and the articular capsule, potentially affecting the hip joint. However, there remains a great deal of controversy among scholars regarding the necessity to incise the capsule during arthroscopy and whether the capsule should be repaired at the end of the procedure.
More surgeons now consider hip capsule closure to be vital and that the chances of routinely performing a complete hip capsule closure are higher. This approach has become common practice among an increasing number of hip surgeons [5].A multicenter analysis with a 10-year follow-up showed factors associated with conversion to total hip replacement after undergoing hip arthroscopy included older age, higher grading and capsular nonrepair [6]. Complete capsular repair is a crucial component of hip arthroscopy and can return the hip to a purely functional state. There is an increasing amount of research demonstrating the functional and clinical advantages of performing complete capsular closure during hip arthroscopy [7–9]. A study comparing four different suture methods concluded that shoelaces, double shoelaces [10, 11], and Quebec City Slider (QCS) [12]were better sutures [13].
Thus, our research team has modified a continuous stitching technique based on Soshi Uchida [10], whose suture method involves using a suture pass and the suture lasso to perform separate fine suture operations with one thread in the joint cavity. Nevertheless, arthroscopic thread grasping and removal prolongs the operative time. Therefore, the suture method in this study performs two passes of a single thread ex vivo through two preplaced cannulas [14]. This not only more closely resembles the X-stitch effect of a shoelace, but also generally results in a shorter suture time, with closure of the joint capsule through the completion of 2–3 X-stitches. It is unnecessary to separate and expose the upper surface of the joint capsule. A 90°suture hook can be used to continuously suture the substantial part of the joint capsule. We carried out a retrospective cohort study to ascertain the effect of the modified shoelace stitching technique on the functional outcome. The hypothesis is that the dual cannula combined with the modified shoelace continuous capsular closure technique improves the functional outcome and is a reliable and safe strategy for completely closing the hip joint capsule.
Method
Ethics statement
Approved by the Ethics Committee (NO: ZF2021-030-01), this retrospective cohort study was conducted in the center of the present authors from January 2021. The informed consent was obtained from all patients before initiation of the study.
Patients
The present study was a retrospective cohort study including patients who were diagnosed with femoral acetabular impingement and acetabular labral injury. The patients underwent hip arthroscopy surgery between January 2019 and January 2022 at the institution of the present authors. Inclusion criteria: (1) a confirmed diagnosis of FAI [15] with glenoid labral injury and hip arthroscopy; (2) the presence of hip osteoarthritis (Tonnis stage 0 or 1); (3) undergoing intraoperative acetabular glenoid labral repair; (4) demonstrating satisfactory compliance with the study and the ability to cooperate in completing follow-up. Exclusion criteria: (1) a history of previous ipsilateral hip surgery; (2) a history of acetabular fracture, avascular necrosis, Legg-Calve-Perthes disease, bone tumoror and lumbar radiculopathy; (3) lateral center-edge angle (CE) < 25°and medullary dysplasia; (4) poor compliance and inability to cooperate with the study; (5) osteoarthritis of the hip (Tonnis grade > 1).
All patients underwent hip arthroscopy under general anesthesia for glenoid labral repair and femoral osteoplasty. They were then divided into shoelace capsular closure group (CC group) and non-capsular closure group (NC group) according to whether the capsule was sutured. All patients were examined preoperatively using X-ray, 3D CT, and MRI to clarify their conditions.
Surgery procedures
All surgeries were performed according to a previous study [5] by the senior author at a single institution. All patients were operated in the supine position on a traction bed, and 2 or 3 portals (The anterolateral portal (ALP), the mid-anterior portal (MAP) and the proximal mid-anterior portal (PMAP)) were made by standard procedure. In all hips the capsulotomy was done by an interportal cut. We didn’t perform any T-shaped capsulotomies meaning that the zona orbicularis is preserved in all patients.
Each patient began with diagnostic arthroscopy, including assessment of the glenoid labral tear and the extent and degree of the tear. Arthroscopic management, which involved decompression of the anterior inferior iliac spine, trimming of the rim, and refixation of the labrum, was performed based on preoperative imaging, a thorough physical examination, and the arthroscopic situation. After arthroscopic diagnosis and treatment, the control group did not suture the joint capsule. In contrast, the experimental group sutured the joint capsule according to a modified shoelace with continuous capsular closure. The details are shown in Figs. 1 and 2. Specific operations are shown in Supplementary Attachment 1.
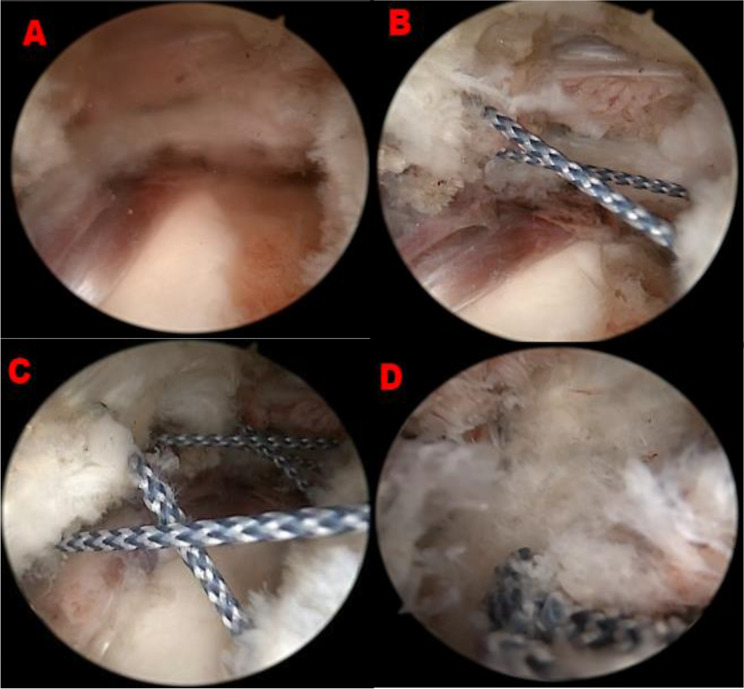
Fig. 1.
Modified Shoelace Continuous Capsular Closure Technique. (A) Arthroscopic images of right hip. The scope is inserted into ALP and is situated the outside of capsule, revealing the edge of the hip capsule. The femoral neck can be seen at the bottom of the image. (ALP, anterolateral portal). (B) Using A suture catcher and A suture shuttle with wire loop, the suture was shuttled back and forth in the double channel (C) The suture is repeated back and forth over the line, typically two-three times, with a distance of 6–7 mm between each stitch, and eventually forming shoelace suture.(D) The ends of the high-strength sutures are gradually stretched tightly in the cannula
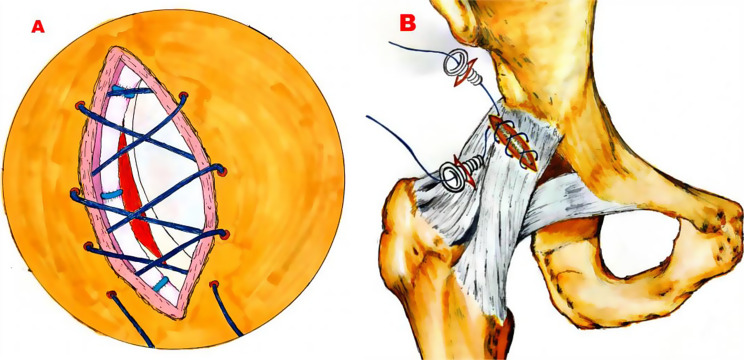
Fig. 2.
Artistic rendering of arthroscopic and surgical images of the right hip. (A) Arthroscopic and surgical views of right hip capsular suture management. The suture strand utilized for capsular repair is colored dark for easy identification. Before being tightened, the stitch shuttle moves back and forth in a manner like tightening shoelaces. (B) Anterior view of a right hip after modified shoelace continuous capsular closure in 2 cannula portals
Postoperative rehabilitation
After the surgery, the patient was administered anti-inflammatory and analgesic medications as a part of routine postoperative care. On the day of surgery, patients were able to commence hip flexion and extension exercises while utilizing double crutches for ground ambulation. Within six months of the treatment, two follow-up visits were conducted, during which an MRI scan of the hip joint was performed to assess the recovery of the joint capsule.
Methods of assessment
Preoperative patient-reported outcomes (PROs) and PROs at final follow-up were obtained, including Visual Analog Scale (VAS) for pain and modified Harris Hip Score (mHHS) [16], Hip Outcome Score-Activities of Daily Living (HOS-ADL) and Hip Outcome Score Sport-Specific Subscale (HOS-SS) [17].
Statistical analysis
The data obtained were statistically analyzed using SPSS 25.0 statistical software to compare the demographics and surgical conditions between the two types of surgery studied (shoelace closure and without closure) and to analyze the differences in functional outcome scores between preoperative and follow-up. Continuous variableswere described using mean ± standard deviation. Paired sample t-test was used within groups, while two sample t-test was employed between groups for metric data that conform to normal distribution and homogeneity of variance. In cases where metric data did not conform to a normal distribution, the odd sum test was used. Chi square test was used for counting data, while repeated measures analysis of variance and multivariate comparison of variance were used for inter-group comparison. 95% confidence intervals were included for all continuous variables, and P < 0.05 was set as the threshold for statistical significance.
Results
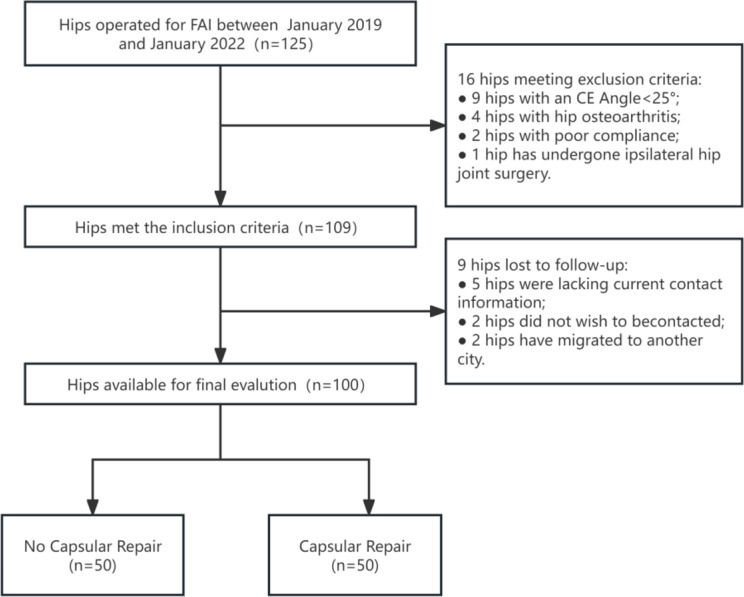
Consecutive series of 125 hip surgeries performed using the same method were eligible for evaluation (Fig. 3). 16 hips (9 hips with an CE Angle < 25°,4 hips with hip osteoarthritis, 2 hips with poor compliance, 1 hip has undergone ipsilateral hip joint surgery) were excluded based on the eligibility criteria. Additionally, 9 hips (5 hips lacking current contact information, 2 hips not wishing to be contacted, 2 hips having migrated to another city) were lost to follow-up (after a minimal one year of follow-up without complication). As shown in Table 1, a total of 100 patients meeting the study criteria were identified: 50 patients in CC group and 50 patients in NC group. The age of all patients at the time of surgery was 40.94 ± 11.80 years, (range 13–74 years). The patient demographics are shown in Table 1. There were 64 females and 34 males among them. 63 cam-type, 3 clamp-type, and 34 mixed-type FAI types were found. The situation during surgery: The surgical procedure was slightly greater in the CC group (109.88 ± 5.31 min) compared to the NC group (105.96 ± 3.08 min). The difference was statistically significant (P<0.05). There was no statistically significant difference in the number of labral repairs, femoral osteoplasty, aetabular osteoplasty, the mean anchors per patient, and the length of hospital stay between the two groups (P > 0.05). (Table 2)
Fig. 3.
Diagram showing the inclusion criteria and the exclusion criteria applied to the data
Table 1.
Baseline characteristics of participants
| Characteristics | Total | CC group(n = 50) | NC group(n = 50) | P-value | Χ2 value / t value |
|---|---|---|---|---|---|
| Age (years) | 40.94 ± 11.80 | 40.74 ± 1.84 | 44.6 ± 2.12 | 0.279 | -1.217 |
| Female (%) | 63(63) | 31(62) | 32(64) | 0.836 | 0.043 |
| Male (%) | 37(37) | 19(38) | 18(36) | ||
| BMI (kg/m2) | 22.85 ± 4.47 | 23.10 ± 4.16 | 22.60 ± 4.75 | 0.559 | 0.577 |
| FAI type: | |||||
| Cam type | 63(63) | 30(60) | 33(66) | 0.743 | 0.594 |
| Pincer type | 3(3) | 2(4) | 1(2) | ||
| Mixed type | 34(34) | 18(36) | 16(32) | ||
| Alpha Angle, deg | 57.80 ± 5,23 | 58.58 ± 5.12 | 57.02 ± 5.21 | 1.510 | 0.134 |
| LCEA, deg | 31.31 ± 3.74 | 30.76 ± 3.71 | 31.86 ± 3.68 | 1.488 | 0.140 |
Note Data are presented as number (percentage) or mean ± SD standard deviation. CC group: shoelace capsular closure group; NC group: non-capsular closure group
Table 2.
Comparison of surgical data and inpatient days between two groups
| CC group | NC group | P-value | Χ2 value / t-value |
|
|---|---|---|---|---|
| Labral repair (n) | 47 | 48 | 0.646 | 0.211 |
| Femoral osteoplasty (n) | 41 | 39 | 0.617 | 0.250 |
| Acetabular osteoplasty (n) | 39 | 35 | 0.832 | 0.362 |
| Mean anchors per patient (n) | 2.22 ± 0.97 | 2.18 ± 1.09 | 0.846 | 0.194 |
| Suture time of joint capsule (minutes) | 8.72 ± 3.56 | 0 | < 0.001 | 17.320 |
| Traction time (minutes) | 69.83 ± 11.64 | 72.65 ± 10.26 | 0.202 | -1.285 |
| Operation time (minutes) | 109.88 ± 5.31 | 105.96 ± 3.08 | < 0.001 | 4.516 |
| Inpatient days (days) | 4.88 ± 0.21 | 5.12 ± 0.20 | 0.388 | -0.823 |
Note Data are presented as  standard deviation
standard deviation
All patients completed a 12-month follow-up, and a comparison of preoperative HOS-ADL scores, mHHS scores, and HOS-SSS scores between the two groups showed no statistically significant differences in scores between the two groups (P > 0.05). Among them, the HOS-ADL score, mHHS score, and HOS-SSS score were notably higher than those before surgery at the third and sixth month of follow-up (P < 0.001). (Table 3)
Table 3.
Patient-reported outcomes in patients
| CC group | NC group | P-value | t-value | |
|---|---|---|---|---|
| mHHS | ||||
| Preoperative | 57.88 ± 6.82 | 58.36 ± 7.72 | 0.742 | -0.330 |
| 6th month of follow-up | 76.76 ± 3.82 | 71.86 ± 5.98 | < 0.001 | 4.885 |
| 12th month of follow-up | 86.08 ± 2.75 | 82.48 ± 4.09 | < 0.001 | 5.165 |
| HOS-SSS | ||||
| Preoperative | 40.94 ± 5.79 | 42.11 ± 6.36 | 0.340 | 0.958 |
| 6th month of follow-up | 74.38 ± 5.06 | 68.61 ± 8.84 | < 0.001 | 5.984 |
| 12th month of follow-up | 86.16 ± 4.39 | 82.72 ± 4.90 | < 0.001 | 3.697 |
| HOS-ADL | ||||
| Preoperative | 51.14 ± 5.48 | 51.57 ± 4.88 | 0.679 | 0.415 |
| 6th month of follow-up | 76.82 ± 3.94 | 72.28 ± 6.37 | < 0.001 | 4.279 |
| 12th month of follow-up | 88.82 ± 2.66 | 84.85 ± 5.16 | < 0.001 | 4.840 |
| VAS | ||||
| Preoperative | 5.56 ± 0.76 | 5.48 ± 0.84 | 0.618 | 0.500 |
| 6th month of follow-up | 2.22 ± 0.65 | 2.78 ± 0.79 | < 0.001 | 3.875 |
| 12th month of follow-up | 0.86 ± 0.70 | 1.44 ± 0.91 | < 0.001 | 3.579 |
Note Data are presented as  S standard deviation. mHHS, modified Harris Hip Score; HOS-SSS, Hip Outcome Score Sport-Specific Subscale; HOS-ADL, the hip function score for daily activities; VAS, visual analog scale. Statistically significant (P < 0.05). CC group: shoelace capsular closure group; NC group: non-capsular closure group.
S standard deviation. mHHS, modified Harris Hip Score; HOS-SSS, Hip Outcome Score Sport-Specific Subscale; HOS-ADL, the hip function score for daily activities; VAS, visual analog scale. Statistically significant (P < 0.05). CC group: shoelace capsular closure group; NC group: non-capsular closure group.
At the 12th month of follow-up, VAS ratings in both groups considerably improved compared to preoperative scores. In comparison to the preoperative score, the CC group showed a more pronounced improvement in HOS-ADL, mHHS, and HOS-SSS scores at the 6-month and 12-month postoperative follow-ups. (Table 4, P < 0.001) No major complications (dislocations, compartment syndrome due to fluid extravasation, or neurovascular injuries) were reported.
Table 4.
Comparison of preoperative and postoperative outcomes between two groups
| Preoperative | 6th month of follow-up | 12th month of follow-up |
p-value from the 6th month |
p-value from the 12th month |
|
|---|---|---|---|---|---|
| mHHS | |||||
| CC group | 57.88 ± 6.82 | 76.76 ± 3.82 | 86.08 ± 2.75 | < 0.001 | < 0.001 |
| NC group | 58.36 ± 7.72 | 71.86 ± 5.98 | 82.48 ± 4.09 | < 0.001 | < 0.001 |
| HOS-SSS | |||||
| CC group | 40.94 ± 5.79 | 74.38 ± 5.06 | 86.16 ± 4.39 | < 0.001 | < 0.001 |
| NC group | 42.11 ± 6.36 | 68.61 ± 8.84 | 82.72 ± 4.90 | < 0.001 | < 0.001 |
| HOS-ADL | |||||
| CC group | 51.14 ± 5.48 | 76.82 ± 3.94 | 88.82 ± 2.66 | < 0.001 | < 0.001 |
| NC group | 51.57 ± 4.88 | 72.28 ± 6.37 | 84.85 ± 5.16 | < 0.001 | < 0.001 |
| VAS | |||||
| CC group | 5.56 ± 0.76 | 2.22 ± 0.65 | 0.86 ± 0.70 | < 0.001 | < 0.001 |
| NC group | 5.48 ± 0.84 | 2.78 ± 0.79 | 1.44 ± 0.91 | < 0.001 | < 0.001 |
Note Statistically significant (P < 0.001). CC group: shoelace capsular closure group; NC group: non-capsular closure group
No major complications (vascular injury, infection, fracture, lower limb phlebitis or deep vein thrombosis, and other serious complications) occurred. Postoperative perineal numbness affected 6 patients in the CC group and 4 patients in the NC group. All 10 patients’ numbness gradually subsided two weeks following surgery. No patients underwent hip arthroplasty after conversion. There were no iatrogenic chondral or labral damage.
Discussion
The most important finding of this study is that the modified shoelace continuous capsular closure group significantly improves the mHHS, HOS-SSS, HOS-ADL, and VAS at 6 postoperative months compared to the non-capsular closure group, without significantly increasing inpatient days or complications. There is currently some evidence indicating that the modified shoelace stitching technique is a safe and dependable technique, which appears to be an alternative to the conventional capsular closure. Also, it is recommended to routinely repair the articular capsule at the end of the hip arthroscopy, as it positively influences the functional results at short-term follow-up.
This study demonstrated that hip arthroscopic surgery for FAI with acetabular labrum injury was clinically effective as the HOS-ADL score, HOS-SSS score, and mHHS score were considerably improved in both groups of patients at a 12-month follow-up after hip arthroscopic surgery. Besides, at the follow-up 12 months after the operation, the HOS-ADL score, HOS-SSS score, and mHHS score in the CC group were higher than those in the NC group, suggesting that the articular capsule suture during hip arthroscopy would achieve superior clinical efficacy. This study held similarities to other ones. With 32 patients in each group and an average follow-up of 2.5 years, Frank et al. [18] compared the clinical outcomes of capsular closure versus non-capsular closure including both types of closure. At the last follow-up, the capsular closure group’s motor performance and patient satisfaction levels were higher than those of the non-capsular closure group. The study conducted by Domb et al. [19] investigated the impact of articular capsule sutures on mid-term outcomes following hip arthroscopy. The results indicated that the non-suture group had lower satisfaction and mHHS ratings. Furthermore, a higher percentage of patients in the non-suture group (18.5%) required joint replacement surgery than in the suture group (10.5%) following a 5-year follow-up. Despite the fact that the suture of the articular capsule did not affect the results of the short-term follow-up when compared to the non-suture group, the study also suggested that the suture group’s clinical performance was significantly better than the non-suture group’s during the mid-term follow-up.
The stability system of the hip joint consists of a dynamic stability system and a static stability system, which is made up of the glenoid labrum, articular capsule, and osseous acetabulum. Important ligaments around the hip articular capsule include the iliofemoral ligament (ILF), pubofemoral ligament(PFL), eischiofemoral ligament(ISFL), zona orbicularis (ZO) [20]. The most robust and thickest ligament is the ILF, which is shaped like an inverted “Y” and is situated in front of the hip articular capsule. It contributes to restricting external rotation, femoral head forward displacement, and hip joint overextension [21]. The femoral head will move excessively inside the acetabulum when the ILF is torn or relaxed, leading to joint instability and clinical symptoms. The instability of the hip joint will therefore unavoidably be affected by any partial damage to the hip articular capsule, particularly when the capsule is moderately loosened when flexing forward [22]. During hip arthroscopic surgery, the articular capsule is typically transversely sliced between 12 o’clock and 3 o’clock positions in the anterior aspect of the hip joint, where the iliofemoral ligament runs. Consequently, certain scholars have postulated that the standard hip arthroscopy approach could potentially disrupt the micro-stability of the hip joint.
After analyzing a case report of severe hip joint instability following hip arthroscopy, Yeung [23] concluded that factors including articular capsule incision without suture and iliopsoas muscle amputation were high-risk factors for hip instability post-hip arthroscopy. The relative contributions of the acetabular labium and ILF to the stability of the hip joint were investigated directly by Myers et al. [24] Based on the study, it was shown that cutting both the labium and ILF simultaneously resulted in a greater increase in lateral rotation and anterior flexion movement compared to cutting only the ILF. A pelvic labrum repair alone did not normalize lateral rotation or anterior flexion movement. However, combining pelvic labrum repair with ILF repair can completely return these parameters to their original, undamaged state. Consequently, the biomechanics and anatomy currently available indicate that the articular capsule, particularly the ILF, is essential for the micro stability of the hip joint.
Therefore, an increasing number of scholars recommend routine suturing of the joint capsule in hip arthroscopy. The main suturing methods for the joint capsule include single-edge suturing, multiple intermittent suturing, continuous suturing, and special suturing methods. Benedetto’s research team [25] reported their suturing method, in which the length of the incision between the hip joint capsule channels was only 2 cm. Therefore, they opted for high-strength sutures to directly perform single-pair suturing on both sides. Currently, however, most scholars still choose the multiple intermittent suture method. This procedure entails intermittently suturing 2–4 stitches on both sides of the joint capsule incision to close the joint capsule [26–28]. Ajay’s study [29] described in detail the method of intermittent suturing in the article. The study sutured a total of 4 stitches and divided the 4 groups of sutures into 2 groups. Besides, the article also pointed out that the risk of multiple intermittent sutures is: (1) There was a risk of entanglement, incomplete knotting, leakage, or even breakage of the sutures. (2) It was easy for the needle spacing to be too wide to completely close the joint capsule; (3) If the distance from the incision edge was too close, it was easy to tear off and cause suture failure. In order to achieve complete closure of the joint capsule, Uchida [10] proposed using a strong suture to continuously sew the joint capsule back and forth through the “shoelace” method within the channel, which could more fully close the joint capsule and even achieve the effect of pulling and tightening the joint capsule. William [30] proposed a special suturing method. For patients with T-shaped incisions, the longitudinal joint capsule was usually sutured intermittently along the edges. However, in cases of transverse incisions paralleled to the labrum, this study employed double-line anchors on the labrum to suture the labrum and joint capsule together. This suturing technique offered the benefit of correctly fixing the joint capsule on the hip joint, hence enhancing surgical efficiency, as opposed to traditional pure soft tissue suturing repair. However, a potential drawback of this approach was that if the anchor was loose, both labrum repair and joint capsule repair would be affected. It was crucial to clinically evaluate whether the micro-movement of the joint capsule would also affect labrum healing. Mei Dan [31] reported a self-made suture gun tool similar to shoulder arthroscopy. The tool enabled rapid suturing of the hip joint capsule, thereby maintaining the anatomical structure and integrity of the iliofemoral ligament. As a result, it reduced the incidence of postoperative instability and pain.
This study showed that employing modified shoelace continuous capsular closure would increase the extended operation time by approximately 8.7 min, but the extended time was not clinically impactful. This was because this suture method eliminated the need to separate and expose the upper surface of the hip capsule. Instead, it involved using a 90° suture hook to continuously suture the substantial part of the joint capsule. The use of dual-channel wiring technology greatly mitigated the difficulty of intraoperative operations. Furthermore, this study additionally showed that there were no statistically significant variations between the two groups in terms of the hospital stay or any serious postoperative consequences. Due to the author’s employment of the continuous shoelace approach to suture the articular capsule throughout the trial, the transitory numbness in the lower limbs also vanished two weeks following the procedure. The reason was that final joint capsule suturing was after addressing arthroscopic examination and management of the affected hip. The traction bed was then loosened (There was no significant difference in traction time between the two groups). The peripheral interval was evaluated, and the cam-shaped deformity at the femoral neck junction was decompressed and shaped. The suture operation time would neitehr prolong the intraoperative traction time, nor would it lead to an escalation in complications due to excessive traction.
This study has an assortment of significant limitations. There was a large risk of selection bias in the original group allocations in addition to the retrospective character of the study, which restricted the ability to control confounding factors. Initially, no patient received capsular closure. Nevertheless, the senior surgeon altered his method and started consistently closing all capsules. Both groups underwent procedures that were successfully performed well outside of the hip arthroscopy learning curve thresholds previously identified, despite the two groups’ different temporal relationships. Furthermore, even though theoretically capsular closure might have an impact on the postoperative range of motion, we didn’t track or report it for this population. Randomizing closure versus non-closure in these athletes should be considered in future investigations. All patients in our series were operated on by the senior author, a single surgeon. This restricts the generalizability of our findings even while it aids in reducing potential confounders including operating technique, posture, and rehabilitation. Last but not least, the size of each cohort in the series as a whole limits our analysis. Despite this, we believe the study to be worthwhile due to the presence of notable disparities among the groups.
Conclusions
Functional outcome ratings are comparable with those of the other techniques, but capsular closure appears to produce better clinical results. This method, in our perspective, is easily comprehensible and marks an indisputable advancement in our field. Longer-term studies will be necessary to evaluate the outside-in technique’s effectiveness in managing FAI in comparison to other hip arthroscopy procedures. To clarify the benefits of shoelace sutures, it is necessary to conduct a randomized controlled trial involving groups using traditional intermittent sutures and shoelace sutures.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Abbreviations
- mHHS
modified Harris Hip Score
- HOS-ADL
Hip Outcome Score of Activities of Daily Living
- HOS-SSS
Hip Outcome Score Sport-Specific Subscale
- VAS
Visual Analogue Scale
- CC group
Shoelace Capsular Closure Group
- NC group
Non-Capsular Closure Group
Author contributions
Weiming Yang and Yang Lv contributed to all aspects of the manuscript.Da Guo, Dingkun Lin were involved in revising the article critically for important intellectual content. Patient recruitment: Da Guo, Weiming Yang. Data collection and curation: Peng Yang, Yang LV.Data acquisition and statistical analysis:Xiaolong Zeng, Meiping Yang.Writing-review and editing: Ningjing Zeng.All authors read and approved the final manuscript.
Funding
This study was supported by the Project of Guangzhou Basic and Applied Basic Research Foundation (No. 2023A03J0749).
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
We confirm that all experiments were performed in accordance with the Declaration of Helsinki. The study was approved by the Ethical Committee of The Second Affiliated Hospital of Guangzhou University of Chinese Medicine, NO. ZE2023-104-01. Each patient provided written informed consent before participating in the study.
Consent for publication
Consent was obtained.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yang Lv and Ningjing Zeng contributed equally to this work and should be regarded as co-first authors.
References
- 1.Lee MS, Fong S, Owens JS, Mahatme RJ, Kim DN, Gillinov SM, et al. Outcomes after concomitant hip arthroscopy and Periacetabular Osteotomy: a systematic review. Orthop J Sports Med. 2023;11:23259671231160559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hartwell MJ, Moulton SG, Zhang AL. Capsular management during hip arthroscopy. Curr Rev Musculoskelet Med. 2023;16:607–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Riff AJ, Kunze KN, Movassaghi K, Hijji F, Beck EC, Harris JD, et al. Systematic review of Hip Arthroscopy for Femoroacetabular Impingement: the importance of Labral Repair and Capsular Closure. Arthroscopy. 2019;35:646–e6563. [DOI] [PubMed] [Google Scholar]
- 4.Özbek EA, Miller L, James M, Mauro CS. Hip Capsular Closure in Distraction: a technique to allow Easier Closure of T and Interportal Capsulotomies. Arthrosc Tech. 2023;12:e1305–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Capsular Management at the Time of Hip Arthroscopy for Femoroacetabular Impingement Syndrome Varies With Geography and Surgeon Subspecialty Training. A Cross-Sectional, Multinational Surgeon Survey - PubMed. https://pubmed.ncbi.nlm.nih.gov/38401665/. Accessed 14 Jul 2024. [DOI] [PubMed]
- 6.Boos AM, Wang AS, Lamba A, Okoroha KR, Ortiguera CJ, Levy BA, et al. Long-term outcomes of primary hip arthroscopy: Multicenter Analysis at Minimum 10-Year follow-up with attention to Labral and Capsular Management. Am J Sports Med. 2024;52:1144–52. [DOI] [PubMed] [Google Scholar]
- 7.Nho SJ, Beck EC, Kunze KN, Okoroha K, Suppauksorn S. Contemporary Management of the hip Capsule during arthroscopic hip preservation surgery. Curr Rev Musculoskelet Med. 2019;12:260–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dasari SP, Kasson LB, Condon JJ, Mameri ES, Kerzner B, Khan ZA, et al. Systematic review and Meta-analysis of studies comparing complete Capsular Closure against Unrepaired Hip Capsules during Hip Arthroscopy. Orthop J Sports Med. 2023;11:23259671231197435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lv Y, Yang M, Hu C, Guo D, Zhao C, Wei L, et al. Capsule closure has better hip function than non-closure in hip arthroscopy for femoracetabular impingement: a systematic review and meta-analysis. Heliyon. 2024;10:e31088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Uchida S, Pascual-Garrido C, Ohnishi Y, Utsunomiya H, Yukizawa Y, Chahla J, et al. Arthroscopic shoelace Capsular Closure technique in the hip using Ultratape. Arthrosc Tech. 2017;6:e157–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arthroscopic Double Shoelace Capsular Plication Technique for the Treatment of Borderline Hip Dysplasia Associated With. Capsular Laxity - PubMed. https://pubmed.ncbi.nlm.nih.gov/31700788/. Accessed 14 Jul 2024. [DOI] [PMC free article] [PubMed]
- 12.The Quebec City Slider. A Technique for Capsular Closure and Plication in Hip Arthroscopy - PubMed. https://pubmed.ncbi.nlm.nih.gov/27909663/. Accessed 14 Jul 2024. [DOI] [PMC free article] [PubMed]
- 13.Murata Y, Fukase N, Brady AW, Douglass BW, Bryniarski AR, Dornan GJ, et al. Biomechanical evaluation of 4 suture techniques for hip Capsular Closure. Orthop J Sports Med. 2022;10:23259671221089946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang W, Zeng N, Gao S, Zhao C, Xie H, Lin D, et al. Dual Cannula Combined with modified Shoelace continuous Capsular Closure technique in hip arthroscopic surgery. Arthrosc Tech. 2024;13:102833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.The Warwick Agreement on. femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement - PubMed. https://pubmed.ncbi.nlm.nih.gov/27629403/. Accessed 14 Jul 2024. [DOI] [PubMed]
- 16.Gao G, Liu R, Dong H, Ao Y, Wang J, Xu Y. High prevalence of acetabular rim osteophytes after hip arthroscopy for treatment of FAI. BMC Musculoskelet Disord. 2022;23(1):71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lau BC, Scribani M, Lassiter T, et al. Correlation of Single Assessment Numerical Evaluation Score for Sport and Activities of Daily Living to Modified Harris Hip Score and hip outcome score in patients undergoing arthroscopic hip surgery:[J].The American. J Sports Med. 2019;47(11):2646–50. 10.1177/03635465198634111. [DOI] [PubMed] [Google Scholar]
- 18.Frank RM, Lee S, Bush-Joseph CA, Kelly BT, Salata MJ, Nho SJ. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: a comparative matched-pair analysis. Am J Sports Med. 2014;42:2634–42. [DOI] [PubMed] [Google Scholar]
- 19.Patient-Reported Outcomes of Capsular Repair Versus Capsulotomy in Patients Undergoing Hip Arthroscopy. Minimum 5-Year Follow-up-A Matched Comparison Study - PubMed. https://pubmed.ncbi.nlm.nih.gov/29373289/. Accessed 14 Jul 2024. [DOI] [PubMed]
- 20.New insight into the iliofemoral ligament based on the anatomical study of the hip joint capsule - PubMed. https://pubmed.ncbi.nlm.nih.gov/31867743/. Accessed 14 Jul 2024. [DOI] [PMC free article] [PubMed]
- 21.The role of the iliofemoral ligament as a stabilizer of the hip joint - PubMed. https://pubmed.ncbi.nlm.nih.gov/34377546/. Accessed 14 Jul 2024.
- 22.Estébanez-de-Miguel E, González-Rueda V, Bueno-Gracia E, Pérez-Bellmunt A, López-de-Celis C, Caudevilla-Polo S. The immediate effects of 5-minute high-force long axis distraction mobilization on the strain on the inferior ilio-femoral ligament and hip range of motion: a cadaveric study. Musculoskelet Sci Pract. 2020;50:102262. [DOI] [PubMed] [Google Scholar]
- 23.Yeung M, Khan M, Williams D, Ayeni OR. Anterior hip capsuloligamentous reconstruction with Achilles allograft following gross hip instability post-arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2017;25:3–8. [DOI] [PubMed] [Google Scholar]
- 24.Myers CA, Register BC, Lertwanich P, Ejnisman L, Pennington WW, Giphart JE, et al. Role of the acetabular labrum and the iliofemoral ligament in hip stability: an in vitro biplane fluoroscopy study. Am J Sports Med. 2011;39(Suppl):S85–91. [DOI] [PubMed] [Google Scholar]
- 25.Di Benedetto P, Zangari A, Giardini P, Mancuso F, Castriotta L, Causero A. Capsular closure after hip arthroscopy: our experience. Acta Biomed. 2020;91:92–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harris JD. Capsular Management in Hip Arthroscopy. Clin Sports Med. 2016;35:373–89. [DOI] [PubMed] [Google Scholar]
- 27.Atzmon R, Sharfman ZT, Haviv B, Frankl M, Rotem G, Amar E, et al. Does capsular closure influence patient-reported outcomes in hip arthroscopy for femoroacetabular impingement and labral tear? J Hip Preserv Surg. 2019;6:199–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ortiz-Declet V, Mu B, Chen AW, Litrenta J, Perets I, Yuen LC, et al. Should the Capsule be repaired or plicated after hip arthroscopy for Labral tears Associated with Femoroacetabular Impingement or Instability? A systematic review. Arthroscopy. 2018;34:303–18. [DOI] [PubMed] [Google Scholar]
- 29.Lall AC, Ankem HK, Diulus SC et al. Capsular Management of the Hip During Arthroscopic Acetabular Chondral Resurfacing: Pearls, Pitfalls, and Optimal Surgical Technique. Arthrosc Tech. 2021;10(2):e587-e597. Published 2021 Jan 18. 10.1016/j.eats.2020.10.045. https://pubmed.ncbi.nlm.nih.gov/33680797/. Accessed 14 Jul 2024. [DOI] [PMC free article] [PubMed]
- 30.Slikker W, Van Thiel GS, Chahal J, Nho SJ. The use of double-loaded suture anchors for labral repair and capsular repair during hip arthroscopy. Arthrosc Tech. 2012;1:e213–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mei-Dan O, Young DA. A novel technique for Capsular Repair and Labrum Refixation in Hip Arthroscopy using the SpeedStitch. Arthrosc Tech. 2012;1:e107–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.