Abstract
Background
Antenatal attachment is a fundamental concept relative to human transition to parenthood and may be influenced by several factors. The aim of this study is to find the best model to explain maternal antenatal attachment based on the interaction among sociodemographic, clinical, and psychological variables.
Methods
Pregnant women (N = 407) were interviewed during the second trimester of pregnancy while waiting for medical consultations. A sociodemographic, obstetric, and psychometric protocol was used. Statistical analyses: path analysis. Independent variables: psychopathological symptomatology, depression, anxiety, stress, occupational stress, attitudes about pregnancy and motherhood, coping styles, marital satisfaction, sociodemographic, and clinical variables. Dependent variables: maternal antenatal attachment in its several dimensions; quality of attachment (QA), intensity of preoccupation (IP), and global attachment (GA).
Results
Depression, anxiety, attitudes, and marital satisfaction explained 37% of maternal antenatal QA. Age, depression, anxiety, attitudes, and marital satisfaction explained 26% of maternal antenatal IP. Age, depression, anxiety, attitudes, and marital satisfaction explained 34% of the statistical variance of maternal antenatal GA.
Conclusions
Factors like emotional states (depression and anxiety), attitudes towards pregnancy and motherhood, marital satisfaction, and a sociodemographic variable (age) contribute significantly for the explanation of maternal antenatal attachment.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12884-024-06836-x.
Keywords: Antenatal attachment, Pregnancy, Mother, Path analysis, Structural equation modelling
Background
Among the consequences of Bowlby´s attachment theory [1], the concept of maternal antenatal attachment (MAA) emerged as the emotional bond established between the mother and her infant before birth [2–4]. Instruments developed by several authors [2–4] to assess MAA supported this concept. The importance of MAA is the impact that it has on child’s health and, also on child’s and mother’s psychological development during pre and postnatal life [5–7]. Some studies highlighted the predictive role of prenatal attachment on child’s socioemotional, behavioural, and cognitive development in early childhood, and on parents’ mental health during the perinatal period [5, 8, 9]. Namely, it was found that secure pregnant women when compared with insecure ones presented higher rates of global and quality of prenatal maternal attachment [10].
A systematic review performed by Trombetta et al. (2021) [11] showed that higher levels of prenatal attachment are associated with better parent-to-infant attachment during post-partum. Also, other studies in this review suggest that the relationship between antenatal attachment and parent-to-infant attachment is mediated by childbirth experiences (i.e., caesarean delivery, traumatic childbirth experiences), as well as by the need for neonatal intensive care and psychological symptoms (i.e., postpartum depression). Also, it was observed that women expressing fear of birth and experiencing depressive symptoms in pregnancy and as well as after delivery are at a very high risk relative to impaired bonding after birth [12].
The development of maternal antenatal attachment (MAA) involves sociodemographic, obstetric and psychological aspects. High MAA is present in women that are: younger [13], Caucasian, Asian or Hispanic vs. Afro-American [7], more educated [14, 15], stably employed [16], and primigravid [14, 15]. Some studies concluded that higher levels of MAA are associated with low educational levels [13], and with low levels of women’s socioeconomic status [4]. Also, couples living out-of-wedlock present higher antenatal attachment levels than married couples [17]. Both anxious and avoidant romantic styles of adult attachment were significantly associated with low levels of maternal prenatal attachment [18], and specifically with low levels of quality of attachment [10].
Other studies found no significant relationships between MAA and sociodemographic variables [6, 19, 20].
Obstetric variables are also relevant for MAA. Planned pregnancy [21], probably due to motivational aspects, is one of those variables. Gestational age which associates with a positive perception of foetal movements [15], is another one.
However, some studies failed to observe significant associations between, one side, MAA, and on other side, pregnancy planning [22], gestational time or parity [20].
Relative to psychological variables, higher levels of MAA are associated with a positive perception of social support [13], positive and favourable attitudes towards pregnancy [23], higher marital satisfaction [15, 24, 25], a shorter time of marital relationship [6, 24], and marital partner agreement relative to pregnancy [26]. Also, coping style is a favourable predictor of MAA [27].
Decreases in MAA happen in women with high levels of marital control [19], favourable perception of their body image particularly at the third trimester [28], or with negative feelings towards the forthcoming birth [13]. It seems that feelings of marital control, positive body image (third trimester) or a negative perception about the future infant relate to a psychological experience where the pregnant woman takes the benefits of the situation to the detriment of the unborn infant.
Psychopathology also relates to MAA. Maternal depression associates with low MAA [9, 10, 12, 13, 19]. In depressive conditions, foetal closeness may be felt as a source of anger, guilt or as something invasive [19], impacting negatively on the pregnant woman [29] or contributing for low maternal responsivity towards the new-born infant [30].
Some studies suggest that anxiety decreases maternal antenatal quality of attachment [21], and the same happens with high levels of stress which seem to decrease prenatal attachment levels [31]. Other studies consider that anxiety activates negative emotions but seems to have no negative effects upon attachment even when associated with negative emotions towards to the foetus [32].
Psychopathological symptoms experienced by pregnant women and its relationship with MAA were investigated less frequently. Negative emotional states, thinking focused on external conditions, difficulties about the description of emotional experiences, aspects connected to maternal imagination, and emotional investment towards the foetus relate negatively with MAA [6]. In the domain of psychosomatics, cardiac symptoms are more salient when the affection towards the foetus is lower, while gastric symptoms relate positively with the progress of maternal representation of the foetus as a separate person [23].
Not all studies confirm the significant associations between MAA and psychological variables [33] or psychopathological variables, namely prenatal depression [15, 34].
However, some authors consider that the promotion of antenatal affection can be beneficial for the infant´s development. For example, Cildir et al. (2020) [8] showed that the antenatal emotional bond is a good predictor of development in childhood being even stronger than severe maternal depression.
Facing controversies relative to the association between MAA and the already mentioned variables, this study aims to determine, in the fields of sociodemographic, clinical, and psychological variables, which is the best model for the explanation of maternal antenatal attachment. This can be innovative once that studies about MAA are scarce, especially when variables as psychopathological symptoms, attitudes, emotional states (depression, anxiety, and stress), coping, marital satisfaction and occupational stress are observed while interacting with sociodemographic and clinical factors using path analyses modelling.
Methods
As a part of a broader investigation, a cross-sectional study was performed with 407 women, at a single interview during the second trimester of pregnancy (for statistical description of the sample, see Camarneiro, 2011 [35]). Recruitment was performed in health centres at the centre of Portugal, and it lasted for eighteen months.
Inclusion/exclusion criteria
In order to get a sample with characteristics of homogeneity relative to health and family status, inclusion and exclusion criteria were defined as follows. Inclusion: pregnant women out of obstetrical risk, with a stable marital relationship, being at the second trimester of pregnancy, and willingness to participate in the study. Exclusion: pregnant women without marital partner, and non-biological fathers.
Participants
Because 44 of the participants were unemployed at the moment, they could not answer about occupational stress and so they were not included in this study. Also, due to missing data about marital partners, the socioeconomic status of 6 participants could not be assessed. This way the present study was performed with only 357 women. According to current trends, participants were: young (years old, M = 29.70, SD = 4.52), well educated (years of educational success: M = 12.55, SD = 3.46), living mostly between the highest and the average socioeconomic status (Graffar’s, I – 10.1%, II – 69.5%, III – 20.2%), not smoking (95.5%), not drinking (93.6%), mainly experiencing a planned pregnancy (77.9%), being at the second trimester of pregnancy (gestational weeks: M = 21.20, SD = 2.34), and presenting a good weight gain (kilograms, M = 5.16, SD = 2.43).
Instruments
The protocol included several instruments. A Sociodemographic and Clinical Questionnaire (original Portuguese version [35], pp. 555–556) was created for the broader investigation which includes sociodemographic information (age, education, socioeconomic status, occupational status, marital status, household) and clinical information (pregnancy planning, gestational age, expected delivery date, expected hospital for delivery, difficulties trying to get pregnant, obstetric history, gynaecological history).
For psychological variables, the following instruments were selected.
Maternal antenatal attachment - Maternal Antenatal Attachment Scale (MAAS) [2], a self-report scale with 19 items; Portuguese version [36], includes two sub-scales, Quality of Attachment (QA; mother’s thoughts and feelings relative to the infant) and Intensity of Preoccupation (IP; mother’s worries relative to the infant), and a Global Attachment (GA; an appreciation of maternal attachment including both aspects of QA and of IP) scale.
Emotional states - Depression, Anxiety and Stress Scales (DASS-42), a self-report questionnaire with 42 items and including subscales Depression (D), Anxiety (A) and Stress (S) [37]; Portuguese version [38].
Occupational stress - Perceived Stress Scale, an adaptation for the professional context (PSS-14) [26], a self-report instrument that includes 14 items; Portuguese version [39].
Psychopathological symptomatology - Brief Symptom Inventory (BSI) [40]; Portuguese version [41], a self-report questionnaire with 53 items. Only the three indexes were used (Global Severity Index, GSI; Positive Symptom Total, PST; Positive Symptom Distress Index, PSDI).
Attitudes towards pregnancy and motherhood - Attitudinal Scale about Pregnancy and Motherhood (ASPM) [42], a self-report instrument having 42 items related with subscales: Imagined Son (IS), Good Mother (GM), Pregnancy as a Factor for Change and Personal Growth (PFCPG), Difficult Aspects of Pregnancy and Motherhood (DAPM), Relationship with Own Mother (ROM), Husband/Partner Support (HPS), Body Image and Need for Dependence (BIND). According to scoring instructions, negative results in ASPM subscales should be regarded as positive from a psychological point of view.
Satisfaction with marital life - taking into account only the Total Score (TS) of the Scale about Satisfaction with Marital Life (SSML) [43], a self-report instrument using 44 items.
Coping styles - Inventory of Problems Resolution (IPR) [44], using only the Total Score (IPR-TS).
Cronbach’s alphas were determined for all scales, and for their dimensions in the sample under study (Table 1). Because the BSI variables are indexes there are no Chronbach’s alphas to report.
Table 1.
Internal consistency for all scales and scales’ dimensions used in this study
| Scales | Dimensions | Cronbach’s alpha |
|---|---|---|
| MAAS | GA - Global Attachment | 0.75 |
| QA - Quality of Attachment | 0.71 | |
| IP - Intensity of Attachment | 0.62 | |
| DASS-42 | D - Depression | 0.91 |
| A - Anxiety | 0.81 | |
| S - Stress | 0.92 | |
| PSS-14 | PSS - Occupational Stress | 0.77 |
| BSI | GSI - Global Severity Index | n.a. |
| PST - Positive Symptoms Total | n.a. | |
| PSDI - Positive Symptoms Distress Index | n.a. | |
| ASPM | IS - Imagined Son | 0.80 |
| GM - Good Mother | 0.68 | |
| PFCPG - Pregnancy as a Factor of Change & Personal Growth | 0.77 | |
| DAPM - Difficult Aspects of Pregnancy & Motherhood | 0.66 | |
| ROM - Relationship with Own Mother | 0.81 | |
| HPS - Husband/Partner Support | 0.75 | |
| BIND - Body Image and Need for Dependence | 0.63 | |
| SSML | SSML-TS - Scale about Satisfaction with Marital Life - Total Score | 0.98 |
| IPR | IPR-TS - Inventory of Problems Resolution - Total Score | 0.78 |
n.a. - not applicable, because GSI, PST and PSDI are indexes and so Chronbach’s alphas cannot be calculated
Procedure
While waiting for medical consultations related to their pregnancies, women were interviewed by the first author in a private room, during 20 to 25 min. As participants were waiting for their consultations there were no pressures of any kind. During the interviews, the social ambience was always kind and there seemed to be no difficulties. Ethical recommendations of the Helsinki declaration were respected and signed informed consent was obtained. Ethical committee decision, CE 02/08 of Maternidade Bissaya Barreto (Portugal).
Protocol
The protocol followed this sequence: invitation to the participants and Informed Consent; Sociodemographic and Clinical Questionnaire; Maternal Antenatal Attachment Scale; Depression, Anxiety and Stress Scales; Perceived Stress Scale; Brief Symptom Inventory; Attitudinal Scale about Pregnancy and Motherhood; Scale of Satisfaction with Marital Life; and Inventory of Problems Resolution. While the Sociodemographic and Clinical Questionnaire was verbally answered by participants and their answers were recorded by the first author, all the other questionnaires were filled by participants themselves.
Data Analysis
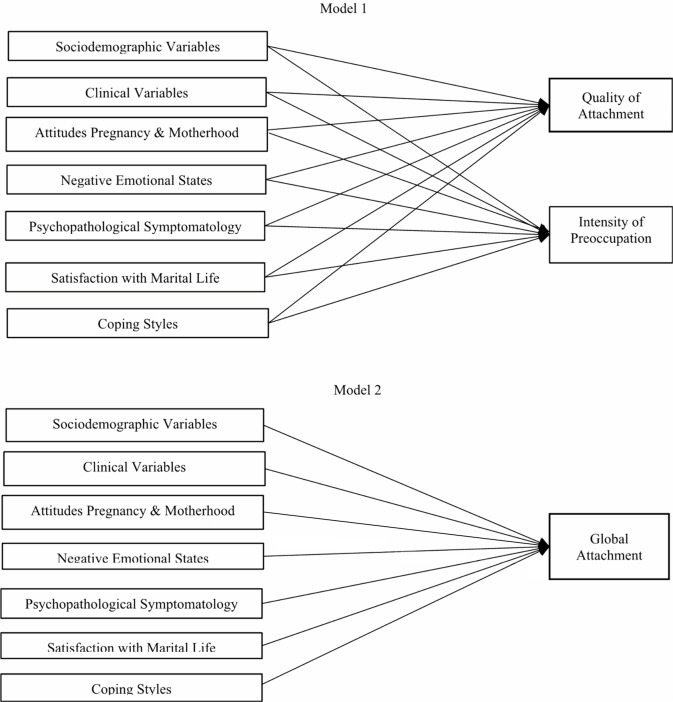
The estimated path analysis modelled the data of the current study at the individual level of analysis, addressing the ratings from females with two being estimated: Model 1 depicting the explanatory variables (sociodemographic and clinical variables, attitudes about pregnancy and motherhood, negative emotional states, occupational stress, psychopathological symptomatology, satisfaction with marital life and coping styles) of maternal antenatal attachment (in two dimensions: quality of attachment and intensity of preoccupation), and Model 2 illustrating those explanatory variables able to explain global maternal antenatal attachment. Explanatory variables were selected according to the general knowledge about prenatal maternal attachment, namely: (a) sociodemographic variables, age [13], education [14, 15], socioeconomic status [4]; (b) clinical variables, gestational age [15], planned pregnancy [21], number of previous pregnancies [15], parity [23]; (c) negative emotional states, depression [9], stress [31], anxiety [21]; (d) psychopathological symptomatology [9, 10, 12, 13, 19], satisfaction with marital life [15, 24, 25], and coping [27].
The maximum likelihood estimation was applied with model adjustment indices not being able to be produced because the models were just identified, meaning the number of free parameters of the current models was equal to the known observed values, generating solutions with zero degrees of freedom [45].
Figure 1 provides summarized visual information on the factorial rationale applied to the tested models. Data analyses were performed using lavaan [46] for the R environment [47].
Fig. 1.
Visual depiction of the Path Analyses Models (Model 1 and Model 2) Summarizing the Relationships between the Study Variables. Note: Each explanatory variable is represented generically in the visual representation to facilitate comprehensiveness. The analyses were performed with the manifest subscales included in each dimension. Models were tested separately
Results
Quality of attachment (QA) was explained by attitudes about pregnancy and motherhood (ASPM). Having in mind that negative scores of ASPM are positive from a psychological point of view, results must be read this way. Mainly a negative association was found for the mothers’ imagined son (meaning a favourable attitude) and a positive association for challenging aspects related to pregnancy and maternity (meaning a non-favourable attitude). Also, maternal depression presents a negative association with the outcome (QA) while anxiety presents a positive association. Mothers’ marital satisfaction reveal a positive association with QA.
Intensity of preoccupation (IP), in terms of sociodemographic variables, is only negatively associated with age. Relative to attitudes about pregnancy and motherhood, the imagined child contributes with a negative association to explain this outcome (IP), meaning a favourable attitude, as well as mothers’ body image and need for dependence, also meaning a favourable attitude. Regarding negative emotional states, a similar pattern was revealed with depression and anxiety contributing to explain mothers’ IP, the former with a negative association and the latter with a positive one. About mothers’ marital satisfaction, it was positively associated with the outcome (IP).
The current model explained 37% of the variance of QA and 26% of the variance of IP. The standardized residual covariance between variables was 0.44 (p < .001). Table 2 presents the detailed coefficient results for Model 1.
Table 2.
Coefficients, standard errors and P-values for the path analysis model explaining quality of attachment and intensity of preoccupation (n = 357)
| Quality of Attachment | Intensity of Preoccupation | |||||||
|---|---|---|---|---|---|---|---|---|
| B | SE | p | b | B | SE | p | β | |
| Sociodemographic Variables | ||||||||
| Age | -0.08 | 0.10 | 0.438 | -0.04 | -0.43 | 0.17 | 0.011 | -0.14 |
| Education | -0.04 | 0.15 | 0.783 | -0.02 | -0.31 | 0.26 | 0.241 | -0.08 |
| Socioeconomic Status | 1.38 | 1.09 | 0.204 | 0.06 | 0.29 | 1.91 | 0.879 | 0.01 |
| Clinical Variables | ||||||||
| Gestational Age | 0.30 | 0.16 | 0.066 | 0.08 | 0.32 | 0.29 | 0.271 | 0.05 |
| Planned Pregnancy | 1.76 | 1.00 | 0.078 | 0.08 | 2.45 | 1.75 | 0.162 | 0.07 |
| Number of Previous Pregnancies | -0.55 | 0.57 | 0.337 | -0.06 | -0.25 | 1.01 | 0.801 | -0.02 |
| Parity | 1.01 | 1.10 | 0.356 | 0.06 | 0.25 | 1.92 | 0.897 | 0.01 |
| Attitudes about Pregnancy & Motherhood | ||||||||
| Imagined Son | -0.85 | 0.17 | < 0.001 | -0.28 | -0.94 | 0.30 | 0.002 | -0.20 |
| Good Mother | -0.06 | 0.15 | 0.709 | -0.02 | -0.13 | 0.26 | 0.632 | -0.03 |
| Pregnancy Factor of Change & Personal Growth | -0.19 | 0.14 | 0.177 | -0.07 | -0.46 | 0.25 | 0.059 | -0.10 |
| Difficult Aspects of Pregnancy & Motherhood | 0.27 | 0.13 | 0.043 | 0.11 | -0.15 | 0.24 | 0.514 | -0.04 |
| Relationship with Own Mother | 0.07 | 0.18 | 0.717 | 0.02 | -0.38 | 0.32 | 0.230 | -0.06 |
| Husband/Partner Support | 0.41 | 0.31 | 0.190 | 0.08 | 0.50 | 0.55 | 0.362 | 0.06 |
| Body Image and Need for Dependence | -0.24 | 0.21 | 0.256 | -0.06 | -0.78 | 0.36 | 0.032 | -0.12 |
| Negative Emotional States | ||||||||
| Occupational Stress | 0.04 | 0.07 | 0.571 | 0.03 | 0.01 | 0.11 | 0.911 | 0.01 |
| Depression | -0.51 | 0.12 | < 0.001 | -0.32 | -0.46 | 0.20 | 0.024 | -0.18 |
| Stress | -0.05 | 0.09 | 0.570 | -0.04 | 0.02 | 0.16 | 0.886 | 0.01 |
| Anxiety | 0.33 | 0.15 | 0.030 | 0.14 | 0.64 | 0.27 | 0.018 | 0.17 |
| Psychopathological Symptomatology | ||||||||
| Global Severity Index | 0.55 | 3.64 | 0.879 | 0.03 | -7.05 | 6.38 | 0.270 | -0.23 |
| Positive Symptoms Total | -0.02 | 0.10 | 0.851 | -0.03 | 0.24 | 0.18 | 0.170 | 0.23 |
| Positive Symptoms Distress Index | -0.45 | 1.52 | 0.767 | -0.02 | 0.47 | 2.67 | 0.859 | 0.01 |
| Satisfaction with Marital Life | ||||||||
| SSML-TS - Total Scale | 0.05 | 0.02 | 0.003 | 0.17 | 0.08 | 0.03 | 0.005 | 0.18 |
| Coping Styles | ||||||||
| IPR-TS - Total Scale | 0.05 | 0.04 | 0.244 | 0.06 | 0.03 | 0.07 | 0.718 | 0.02 |
Global attachment (GA) is related with the previously mentioned patterns. According to path analysis, those patterns explained around 34% of GA variance. Table 3 illustrates the coefficients. GA was explained by age (negative association), imagined son, body image and need for dependence (negative associations meaning a favourable attitude), depression (negative association), anxiety (positive association) and marital satisfaction (positive association).
Table 3.
Coefficients, standard errors, and P-Values for the path analysis model explaining global attachment (n = 357)
| Global Attachment | ||||
|---|---|---|---|---|
| B | SE | p | β | |
| Sociodemographic Variables | ||||
| Age | -0.24 | 0.11 | 0.032 | -0.11 |
| Education | -0.17 | 0.17 | 0.339 | -0.06 |
| Socioeconomic Status | 0.87 | 1.26 | 0.488 | 0.04 |
| Clinical Variables | ||||
| Gestational Age | 0.31 | 0.19 | 0.104 | 0.07 |
| Planned Pregnancy | 2.08 | 1.15 | 0.072 | 0.09 |
| Number of Previous Pregnancies | -0.41 | 0.66 | 0.534 | -0.04 |
| Parity | 0.66 | 1.27 | 0.605 | 0.03 |
| Attitudes about Pregnancy & Motherhood | ||||
| Imagined Son | -0.89 | 0.20 | < 0.001 | -0.26 |
| Good Mother | -0.09 | 0.17 | 0.610 | -0.03 |
| Pregnancy Factor of Change & Personal Growth | -0.32 | 0.16 | 0.050 | -0.10 |
| Difficult Aspects of Pregnancy & Motherhood | 0.07 | 0.16 | 0.636 | 0.03 |
| Relationship with Own Mother | -0.14 | 0.21 | 0.496 | -0.03 |
| Husband/Partner Support | 0.45 | 0.36 | 0.212 | 0.08 |
| Body Image and Need for Dependence | -0.49 | 0.24 | 0.041 | -0.11 |
| Negative Emotional States | ||||
| Occupational Stress | 0.03 | 0.08 | 0.734 | 0.02 |
| Depression | -0.48 | 0.13 | < 0.001 | -0.27 |
| Stress | -0.02 | 0.10 | 0.872 | -0.01 |
| Anxiety | 0.47 | 0.18 | 0.007 | 0.18 |
| Psychopathological Symptomatology | ||||
| Global Severity Index | -2.99 | 4.21 | 0.477 | -0.14 |
| Positive Symptoms Total | 0.10 | 0.12 | 0.377 | 0.14 |
| Positive Symptoms Distress Index | -0.02 | 1.76 | 0.991 | 0.00 |
| Satisfaction with Marital Life | ||||
| SSML-TS - Total Scale | 0.06 | 0.02 | 0.001 | 0.20 |
| Coping Styles | ||||
| IPR-TS - Total Scale | 0.04 | 0.05 | 0.428 | 0.04 |
Discussion
After path analysis, we can have a clearer picture of the interaction among the most important variables (sociodemographic, clinical, and psychological) for the understanding of maternal antenatal attachment (MAA). These interactions may be approached by some models that are able to statistically explain MAA and its dimensions. Pregnant women presenting higher levels of antenatal global attachment (GA) are younger, have better mental representations about their infants (imagined son), easily accept their body image and need for dependence, present better satisfaction with marital life, higher levels of anxiety and lower levels of depression. These variables explain 34% of the variance of GA.
The highest values of quality of attachment (QA) are displayed by women with positive (from a psychological point of view) attitudes towards the imagined infant, higher (also from a psychological point of view) difficulties about pregnancy and motherhood, higher Satisfaction with Marital Life, less depression, and higher anxiety. These independent variables explain 37% of the variance of QA. The highest values of maternal intensity of preoccupation (IP) are characteristic of women that: are younger, have more positive attitudes relatively to the imagined child, and a better acceptance of body image and need for dependence, less depression and more anxiety, and higher marital life satisfaction. Independent variables are able to explain 26% of maternal IP. Variables explaining GA also explain IP and QA, except age as it does not contribute to explain QA.
Maternal age is the most relevant of all sociodemographic variables because its relationship with MAA is very consistent in several studies. In our study, the contribution of a lower maternal age for a highest GA and IP is similar to other authors’ observations [13]. However, age does not predict QA. Possibly this reflects the idealization of the future infant that goes with the assessment of QA and that probably is invulnerable to the psychological processes that usually go along maturation induced by the increase of age.
Maternal attitudes in the domain of the imagined child can explain GA, QA and IP. According with Raphael-Leff (1995, 2009) [48, 49], the relationship between mother and infant in uterus is modelled by the mother’s imaginary life, both conscious and phantasmatic. In their systematic review, Trombetta et al. [11] support the hypothesis that attachment begins to develop during pregnancy based at the development of affects, fantasies and mental representations about the unborn child influencing the relationship with the real infant after birth.
In this study, attitudes relative to difficult aspects of pregnancy and motherhood help to increase QA. It is our opinion that the assessment of attitudes on difficult aspects of pregnancy and motherhood is related to maternal concern about conditions for foetal, infant, and maternal development. So, higher results about this variable should be read as a signal of a favourable attitude. In effect, prenatal attachment impacts parents’ affects and cognitions as well as their interactions with the infant during the early post-partum period, enhancing the establishment of early, secure, and healthy relationships usually associated with more positive outcomes in infants’ development and post-natal infant-to-parent attachment [50–52]. Relative to body image and need for dependence a higher IP is expected. So, women presenting a favourable attitude about their relationship with their bodies seem to be experiencing the IP in a positive way. In fact, during the second trimester, concerns increase about body changes possibly because these changes are not easy to control. It should not be forgotten that the fear for the irreversibility of events underwent by the body has a deep symbolic meaning [53].
High depression levels have a negative impact upon both maternal QA, IP and GA, which is compatible with other authors’ findings [13, 54]. Anxiety contributes to the explanation of GA as also to maternal QA and to maternal IP. When anxiety increases, so increase maternal GA, QA, and maternal IP; however, most of the studies in this area suggest that women with high levels of anxiety and depression are characterized by low attachment [19]. It is possible that the increase of anxiety in gestation is a consequence of a maturational growth process experienced by the pregnant woman as a moment of self-transformation and higher susceptibility to anxiety evoking situations [53]. We also suppose that this unexpected result of our study is a consequence of specific cultural factors. As a matter of fact, in the Portuguese language the word “anxiety” often means positive and intense expectation.
Maternal QA, IP and GA is also explained by the increase observed in results of marital satisfaction. Ponti et al. (2021) [18] show that anxious romantic attachments are strictly linked to lower levels of prenatal attachment. Fiskin (2023) [25] states that couples’ dyadic adjustment increases prenatal attachment among pregnant women. Obviously, the questions of social support are very important for the assessment of marital satisfaction and for that reason it is expectable that positive aspects of support provided in couples’ communication help to raise prenatal maternal attachment.
Finally, looking back to previous scientific literature, we can see how important it is to look at MAA from the several facets that constitute it. First of all, QA and IP are explained by different models; age and body image and need for dependence only contribute to IP, while difficult aspects of pregnancy and motherhood only contribute to QA. At a second place, GA is explained by the same variables that explain QA and IP, except by difficult aspects of pregnancy and motherhood. This means that, as a marker of psychological health during gestation, MAA must be considered as related with various information.
The need to put together the several variables of Models 1 and 2 can also be related to the clinical work in the field of obstetrical high-risk. In this domain, pregnant women should be assessed about MAA and, according to results these explanatory variables should be carefully addressed.
Limitations
A limitation in this study is the absence of adult attachment among predictor variables. It also would be important to consider the assessment of maternal perception about self-efficacy for the maternal role.
Finally, because the current models were just identified no testable implications can be refuted due to model complexity with perfect fit occurring [45]. Thus, results should be interpreted cautiously and future studies using structural equation modelling should intend to model overidentified models.
Conclusion
This study contributes to the understanding of the process related with the creation of the psychological attachment between mother and infant since its’ prenatal underpinning.
In summary, there are several variables playing a crucial part of female antenatal attachment: emotional states (depression and anxiety), attitudes relative to gestational and maternal process, maternal age, and marital satisfaction. Taking these observations together one can assume two conclusions: during gestation, women are sensitive to information (internal, marital, and external) relative to their condition as well as motivated to respond expressing emotions (anxiety and depression) while adapting their attitudes towards the reproductive process that is going on.
The implications of these results are twofold. At first, interventions with pregnant women should give special attention to the development of maternal antenatal attachment. For that, specific support addressed to emotional signs as also to attitudes, marital communication and maturation variables as age should always be at the front line of intervention programs. The working through of these aspects should help pregnant women who need to change positively their attitudes relative to gestation and motherhood.
We hope that these conclusions will help psychologists to provide interventions organized on an empirical basis.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The section “Acknowledgments” is not applicable to this study.
Abbreviations
- MAA
Maternal antenatal attachment
- MAAS
Maternal antenatal attachment scale
- QA
Quality of attachment
- IP
Intensity of Preoccupation
- GA
Global Attachment
- DASS-42
Depression, Anxiety and stress scales
- D
Depression
- A
Anxiety
- S
Stress
- PSS-14
Perceived stress scale
- BSI
Brief symptom inventory
- GSI
Global severity index
- PST
Positive symptom total
- PSDI
Positive symptom distress index
- ASPM
Attitudinal scale about pregnancy and motherhood
- IS
Imagined son
- GM
Good mother
- PFCPG
Pregnancy as a factor for change and personal growth
- DAPM
Difficult aspects of pregnancy and motherhood
- ROM
Relationship with own mother
- HPS
Husband/Partner support
- BIND
Body image and need for dependence
- SSML
Scale about satisfaction with marital life
- TS
Total score
- IPR
Inventory of problems resolution
Author contributions
APFC, first author, was responsible for the investigation, performed the data collection, and also wrote the main manuscript text and produced Table 1; MSR, second author, was responsible for the statistical analysis as well as for writing the procedure and interpretation of path analysis, and also produced Tables 2 and 3 as also Figure 1; JMRMJ, third author, accompanied and supervised the investigation, participated in the writing of the main manuscript text and also in its review.
Funding
This study was not funded by any institutions; the study results exclusively from the authors work.
Data availability
Availability of data and materials: The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Ethical Committee of Maternidade Bissaya Barreto, Coimbra, Portugal (decision, CE 02/08). All participants signed Informed Consent forms at the moment of recruitment.
Consent for publication
The section “Consent for publication” is not applicable for this study.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bowlby J. The nature of the child’s tie to his mother. Int J Psychoanal. 1958;39:350–73. http://www.psychology.sunysb.edu/attachment/online/nature%20of%20the%20childs%20tie%20bowlby.pdf. [PubMed] [Google Scholar]
- 2.Condon JT. The assessment of antenatal emotional attachment: development of a questionnaire instrument. Brit J Med Psychol. 1993;66:167–83. 10.1111/j.2044-8341.1993.tb01739.x. Doi.org/. [DOI] [PubMed] [Google Scholar]
- 3.Cranley MS. Development of a tool for the measurement of maternal attachment during pregnancy. Nurs Res. 1981;30(5):281–84. https://www.ncbi.nlm.nih.gov/pubmed/6912989. [PubMed] [Google Scholar]
- 4.Muller ME. Development of the antenatal attachment inventory. West J Nurs Res. 1993;15(2):199–215. 10.1177/019394599301500205. [DOI] [PubMed] [Google Scholar]
- 5.Branjerdporn G, Meredith P, Strong J, Garcia J. Associations between maternal-foetal attachment and infant developmental outcomes: a systematic review. Matern Child Health J. 2017;21(3):540–53. 10.1007/s10995-016-2138-2. [DOI] [PubMed]
- 6.Vedova AMD, Dabrassi F, Imbasciati A. Assessing antenatal attachment in a sample of Italian women. J Reprod Infant Psychol. 2008;26(2):86–98. 10.1080/02646830701805349. [Google Scholar]
- 7.Wilson ME, White MA, Cobb B, Curry R, Greene D, Popovich D. Family dynamics, parental-fetal attachment and infant temperament. J Adv Nurs. 2000;31(1):204–10. 10.1046/j.1365-2648.2000.01245.x. [DOI] [PubMed] [Google Scholar]
- 8.Cildir AD, Ozbek A, Topuzoglu A, Orcin E, Janbakhishov CE. Association of prenatal attachment and early childhood emotional, behavioral, and developmental characteristics: a longitudinal study. Infant Ment Health J. 2020;41(4):517–29. 10.1002/imhj.21822. [DOI] [PubMed] [Google Scholar]
- 9.Rollè L, Giordano M, Santoniccolo F, Trombetta T. Prenatal attachment and perinatal depression: a systematic review. IJERPH. 2020;17(8):2644. 10.3390/ijerph17082644. [DOI] [PMC free article] [PubMed]
- 10.Zhang L, Wang L, Yuan Q, Huang C, Cui S, Zhang K, Zhou X. The mediating role of prenatal depression in adult attachment and maternal-fetal attachment in primigravida in the third trimester. BMC Pregnancy Childbirth. 2021;21:307. 10.1186/s12884-021-03779-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trombetta T, Giordano M, Santoniccolo F, Vismara L, Vedova AMD, Rollè L. Pre-natal attachment and parent-to-infant attachment: a systematic review. Front Psychol. 2021;12:620942. 10.3389/fpsyg.2021.620942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hildingsson I, Rubertsson C. Postpartum bonding and association with depressive symptoms and prenatal attachment in women with fear of birth. BMC Pregnancy Childbirth. 2022;22:66. 10.1186/s12884-021-04367-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rubertsson C, Pallant JF, Sydsjö G, Haines HM, Hildingsson I. Maternal depressive symptoms have a negative impact on antenatal attachment – findings from a Swedish community sample. J Reprod Infant Psychol. 2015;33(2):153–64. 10.1080/02646838.2014.992009. [Google Scholar]
- 14.Caglayan ISC, Cicek AU, Yilmaz Y, Sahin AE. Prenatal attachment and childhood trauma. J Nerv Ment Dis. 2023;211(4):281–88. 10.1097/NMD.0000000000001610. [DOI] [PubMed]
- 15.Ulu PG, Bayraktar S. Investigation of variables related to antenatal bonding levels in pregnant women. Neuropsychiatr Invest. 2018;56(2):1–8. 10.5455/NYS.20180629015333. [Google Scholar]
- 16.Honjo S, Arai S, Kaneko H, Ujiie T, Murase S, Sechiyama H, et al. Antenatal depression and maternal-fetal attachment. Psychopathology. 2003;36(6):304–11. 10.1159/000075189. [DOI] [PubMed] [Google Scholar]
- 17.Lorensen M, Wilson ME, White MA. Norwegian families: transition to parenthood. Health Care Women Int. 2004;25:334–48. 10.1080/07399330490278394. [DOI] [PubMed] [Google Scholar]
- 18.Ponti L, Smorti M, Ghinassi S, Tani F. The relationship between romantic and prenatal maternal attachment: the moderating role of social support. Int J Psychol. 2021;56(1):143–50. 10.1002/ijop.12676. [DOI] [PubMed] [Google Scholar]
- 19.Condon JT, Corkindale C. The correlates of antenatal attachment in pregnant women. Brit J Med Psychol. 1997;70:359–72. 10.1111/j.2044-8341.1997.tb01912.x. [DOI] [PubMed]
- 20.Righetti PL, Dell´Avanzo M, Grigio M, Nicolini U. Maternal/paternal antenatal attachment and fourth-dimensional ultrasound technique: a preliminary report. Br J Psychol. 2005;96(Pt1):129–37. 10.1348/000712604X15518. [DOI] [PubMed] [Google Scholar]
- 21.White O, McCorry NK, Scott-Heyes G, Dempster M, Manderson J. Maternal appraisals of risk, coping and antenatal attachment among women hospitalised with pregnancy complications. J Reprod Infant Psychol. 2008;26(2):74–85. 10.1080/02646830801918455. [Google Scholar]
- 22.Bielawska-Batorowicz E, Siddiqui A. A study of antenatal attachment with Swedish and Polish expectant mothers. J Reprod Infant Psychol. 2008;36(4):373–84. 10.1080/02646830802426144. [Google Scholar]
- 23.Siddiqui A, Hagglof B, Eisemann M. An exploration of antenatal attachment in Swedish expectant mothers. J Reprod Infant Psychol. 1999;17(4):369–80. 10.1080/02646839908404602. [Google Scholar]
- 24.Čėsnaitė G, Domža G, Ramašauskaitė D, Volochovič J, Bužinskienė D. Factors affecting the maternal-foetal relationship. Acta Med Litu. 2019;26(2):118–24. 10.6001/actamedica.v26i2.4032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fiskin G. Dyadic Adjustment and prenatal attachment in couples during pregnancy. Am J Fam Ther. 2023;51(4):408–20. 10.1080/01926187.2021.1981174. [Google Scholar]
- 26.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385 – 96. https://pdfs.semanticscholar.org/bed9/2e978f5bca851a79b16d8499b8ca21eeb3d6.pdf [PubMed]
- 27.Mikulincer M, Florian V. Maternal-fetal bonding, coping strategies and mental health during pregnancy – the contribution of attachment style. J Soc Clin Psychol. 1999;18:255–76. 10.1521/jscp.1999.18.3.255. [Google Scholar]
- 28.Huang H-C, Wang S-Y, Chen C-H. Body image, maternal-fetal attachment, and choice of infant feeding method: a study in Taiwan. Birth. 2004;31(3):183–88. 10.1111/j.0730-7659.2004.00303.x. [DOI] [PubMed] [Google Scholar]
- 29.Kunkel GF, Doan HMK. Fetal attachment and depression: measurement matters. J Prenat Perinat Psychol Health. 2003;18(2):149–66. https://www.proquest.com/docview/198724664. [Google Scholar]
- 30.Flykt M, Kanninen K, Sinkkonen J, Punamäki R-L. Maternal depression and dyadic interaction: the role of maternal attachment style. Infant Child Dev. 2010;19:530–50. 10.1002/icd.679. [Google Scholar]
- 31.Şanh Y, Akbağ NNA. Effects of stress in pregnancy on prenatal attachment, and contributing factors. Psychiatr Danub. 2022;34(1):25–33. 10.24869/psyd.2022.25. [DOI] [PubMed] [Google Scholar]
- 32.Figueiredo B, Pacheco A, Costa R. Depression during pregnancy and postpartum period in adolescent and adult Portuguese mothers. Arch Womens Ment Health. 2007;10:103-09. https://link.springer.com/article/10.1007/s00737-007-0178-8 [DOI] [PubMed]
- 33.Lindgren K. Relationships among maternal-fetal attachment, antenatal depression, and health practices in pregnancy. Res Nurs Health. 2001;24:203–17. 10.1002/nur.1023. [DOI] [PubMed] [Google Scholar]
- 34.Vedova AMD, Cristini C, Bizzi F. Prenatal attachment, distress symptoms and psychosocial variables in a sample of Italian first-time parents. Life Span Disab. 2019;22:255–85. http://www.lifespanjournal.it/client/abstract/ENG349_5.%20Della%20Vedova.pdf.
- 35.Camarneiro AP. Vinculação pré-natal e organização psicológica do homem e da mulher durante a gravidez: Relação com o tipo de parto e com a patologia obstétrica dos II e III trimestres de gestação. Prenatal attachment and psychological organization of both men and women during pregnancy: relationship with type of delivery and with obstetrical pathology at the II and at the III gestational trimesters. Doctoral Thesis in Clinical Psychology, Lisbon University; 2011. https://repositorio.ul.pt/bitstream/10451/6526/6/ulsd062931_td_tese.pdf.
- 36.Camarneiro AP, Justo J. Padrões De vinculação pré-natal. Contributos para a adaptação da maternal and paternal Antenatal attachment scale em casais durante o segundo trimestre de gestação na região Centro De Portugal. Rev Port Pedopsiquiatr. 2010;28:7–22. https://www.academia.edu/26028077/Padr%C3%B5es_de_Vincula%C3%A7%C3%A3o_Pr%C3%A9_Natal_Contributos_para_a_adapta%C3%A7%C3%A3o_da_Maternal_and_Paternal_Antenatal_Attachment_Scale_em_casais_durante_o_2o_trimestre_de_gravidez_na_regi%C3%A3o_centro_de_Portugal. [Google Scholar]
- 37.Lovibond SH, Lovibond PF. Manual for the depression anxiety stress scales, 2nd ed. Sydney: Psychological Foundation Monograph (original, 1995); 2004.
- 38.Pais-Ribeiro JL, Honrado A, Leal I. Contribuição para o estudo da adaptação portuguesa das escadas de Depressão Ansiedade Stress de Lovibond e Lovibond. Psychologica. 2004;36:235–46. https://www.redalyc.org/pdf/362/36250207.pdf.
- 39.Peixoto FA. Tabagismo e Stress: estudo sobre professoras portuguesas. Dissertação de Mestrado (Master Thesis). Faculty of Psychology and Educational Sciencies, Lisbon University; 2005.
- 40.Derogatis L. BSI: brief symptom inventory. National Computer Systems Minneapolis; 1982. https://psycnet.apa.org/record/2004-14941-001
- 41.Canavarro MC. Inventário De Sintomas Psicopatológicos: BSI. In: Simões MR, Gonçalves M, Almeida LS, editors. Testes e Provas Psicológicas em Portugal. Volume II. APPORT, Braga; 1999:95–109.
- 42.Xavier MR, Paul MC. Construção e validação de uma escala de atitudes sobre a gravidez e a maternidade. In: Almeida LS, Machado C, Simões MR, editors. IV Conferência Internacional Avaliação Psicológica: Formas e Contextos. APPORT, Braga; 1996:419–24.
- 43.Narciso I, Costa ME. Amores satisfeitos mas não perfeitos. Cadernos de Consulta Psicológica. 1996;12:115–30. 10.1590/S1516-44462010000300018.
- 44.Vaz-Serra A. Um estudo sobre coping: o inventário de resolução de problemas. Rev Psiquiatr Clin. 1998;9(4):301–16. http://rihuc.huc.min-saude.pt/handle/10400.4/1004. [Google Scholar]
- 45.Goodboy AK, Kline RB. Statistical and practical concerns with published communication research featuring structural equation modeling. Commun Res Rep. 2017;34(1):68–77. 10.1080/08824096.2016.1214121. [Google Scholar]
- 46.Rosseel Y, lavaan. An R package for structural equation modeling. J Stat Softw. 2012;48:1–36. 10.18637/jss.v048.i02. [Google Scholar]
- 47.R Core Team. R: a language and environment for statistical computing [Computer software]; 2023. http://www.R-project.org/.
- 48.Raphael-Leff J. Pregnancy. The inside story. 1st ed. Lanham (Maryland): Jason Aronson Inc. Publishers; 1995.
- 49.Raphael-Leff J. Psychological processes of childbearing. 4ªed. London: The Anna Freud Centre; 2009.
- 50.Murphy TP, Laible DJ. The influence of attachment security on preschool children’s empathic concern. Int J Behav Dev. 2013;37(5):436–40. 10.1177/0165025413487502. [Google Scholar]
- 51.Zimmer-Gembeck MJ, Webb HJ, Pepping CA, Swan K, Merlo O, Skinner EA, Avdagic E, Dunbar M. Review: is parent–child attachment a correlate of children’s emotion regulation and coping? Int J Behav Dev. 2017;41(1):74–93. 10.1177/0165025415618276.
- 52.Matthies LM, Müller M, Doster A, Sohn C, Wallwiener M, Reck C, Wallwiener S. Maternal-fetal attachment protects against postpartum anxiety: the mediating role of postpartum bonding and partnership satisfaction. Arch Gynecol Obstet. 2020;301(1):107–17. 10.1007/s00404-019-05402-7. [DOI] [PubMed] [Google Scholar]
- 53.Colman L, Colman A. Gravidez: a Experiência Psicológica. Lisboa: Colibri; 1991.
- 54.Medina NY, Edwards RC, Zhang Y, Hans SL. A longitudinal investigation of young mothers’ prenatal attachment, depressive symptoms, and early parenting behavior. J Reprod Infant Psychol. 2022;40(2):196–211. 10.1080/02646838.2021.1886257. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Availability of data and materials: The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.