Abstract
Background
Abnormal posture is known to affect the efficacy of exercise therapy for musculoskeletal diseases. However, no studies to date have examined the effect of exercise programs should take into account the posture of the upper body in patients with rotator cuff disease. This study aimed to assess how rotator cuff and corrective exercises impact shoulder function and muscle strength post-arthroscopic rotator cuff repair surgery, providing tailored rehabilitation programs for patients with forward posture.
Methods
Ninety male patients who underwent arthroscopic rotator cuff repair participated in this study. The patients were randomly divided into three groups corrective exercise group (CEG, n = 29), rotator cuff exercise group (REG, n = 27), and control group (CG, n = 28). Each group was instructed to apply different exercise programs to correct posture and enhance rotator cuff strength. All patients were checked by the American Shoulder and Elbow Surgeons (ASES) score, Constant score and muscle strength, and range of motion preoperatively and postoperatively at 6 months and 1 year.
Results
ASES shoulder function scores showed significant difference between the three groups (p = 0.002, F = 7.03), indicating that the corrective exercise program was more beneficial than rotator cuff exercises (p = 0.009, F = 3.78). A significant intergroup difference in mean Constant score was also noted (p = 0.025, F = 3.86), while a statistically significant interaction between time and group was observed (p = 0.032, F = 2.96).
Conclusions
These results suggested that a corrective exercise program can improve shoulder muscle strength and function after rotator cuff repair in male patients with a forward shoulder posture.
Keywords: Rotator cuff, Rehabilitation, Forward shoulder posture, Corrective exercise, Rotator cuff exercise
Background
Shoulder pain resulting from musculoskeletal disorders is a common issue, affecting up to 70% of individuals [1]. About 50% of patients with shoulder pain may continue to experience discomfort for up to 12 months after their initial diagnosis and treatment [2]. Treatment for shoulder pain can include various interventions, such as education, exercise, manual therapy, electrical therapy, injections, medications, and surgery. However, up to 25% of individuals who receive these treatments may still experience recurrent pain, which can hinder the recovery process [3].
After arthroscopic rotator cuff repair, patients typically experience shoulder pain for about three months. If the pain persists, it can reduce the range of motion in the shoulder joint, leading to postoperative joint contraction [4]. Persistent shoulder pain at 1 week postoperative is reportedly associated with surgical duration and cuff tear size. Shoulder joint motion is often limited by pain that appears within 2 months of surgery [5]. Shoulder pain after surgery is associated to longer recovery time, postoperative complications, delayed return to preoperative lifestyle, and sutured tendons [6].
Previous research has examined the effects of exercise therapy on pain reduction and the return to daily activities following rotator cuff repair [7]. Recently, there has been growing interest in the potential for early return to sports as a means of reducing post-surgery pain in athletes [8]. The rehabilitation process typically includes strengthening exercises for the rotator cuff muscles, such as the supraspinatus, infraspinatus, and subscapularis, which aim to improve muscle strength [9]. Additionally, exercises that focus on strengthening the shoulder joint may also aid in patient recovery [10, 11].
The current modern lifestyle often involves reduced physical activity at work, increased use of smartphones, and prolonged periods of sedentary. These factors increase the risk of misalignment of the shoulder joint. A forward shoulder posture is common in individuals who spend extended periods in sedentary positions and is a risk factor for musculoskeletal problems. In addition to traditional risk factors such as sex, age, and physical fitness, upper-body posture can also affect the recovery of patients with rotator cuff injuries [12].
Many exercise programs do not take into account individual posture and lifestyle patterns. Poor postures such as forward neck and shoulder postures can result in additional stress on the upper body, particularly the shoulder joint. For this reason, exercise programs should take into account the posture of the upper body, especially after shoulder surgery [13].
Patients who have undergone arthroscopic rotator cuff repair surgery often exhibit a forward shoulder posture, which is also commonly seen in the general population. This abnormal posture can negatively impact the effectiveness of exercise, especially during postoperative rehabilitation. As a result, the design of rotator cuff and corrective exercises should take into account the specific indications and the individual’s upper-body posture characteristics.
The hypothesis of this study is that in patients with forward shoulder posture undergoing rotator cuff repair, corrective exercises will have a more positive impact on postoperative recovery of shoulder range of motion, shoulder function, and muscle strength compared to rotator cuff exercises.
Methods
Study design
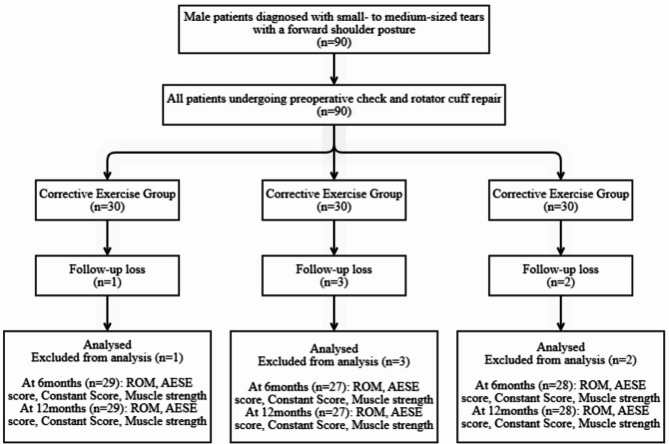
The sample size calculated using G*Power 3.1.9.7 (Universität Düsseldorf, Germany). A study that had achieved a power of 0.95 with a 0.3 effect size and an α of (p) 0.05 was taken as a reference. We estimated a follow-up loss rate of 20%, and ultimately, 30 patients per group participated in the study. Ninety male patients diagnosed with small- to medium-sized tears with a forward shoulder posture at the Samsung Medical Center Orthopedic Surgery Department participated in this study. All patients received arthroscopic rotator cuff repair, which a single orthopedic surgeon performed. The patients were randomly divided into a corrective exercise group (CEG, n = 30), rotator cuff exercise group (REG, n = 30), or control group (CG, n = 30). The exclusion criteria were patients with cuff tears caused by traumatic injury, large or massive cuff tears, and a history of shoulder surgery. Patients in each group received either corrective exercise or rotator cuff exercise education between 10 and 12 weeks after surgery. They were also encouraged to continue the instructed exercises at home. To improve patient compliance, videos were provided, and exercise participation was encouraged through telephone. Range of motion, ASES score, Constant score, and strength tests were conducted at 6 and 12 months post-surgery. During the follow-up for shoulder surgery, six participants were excluded. Two were excluded due to personal problems, while four refused to take the post-operative test. Ultimately, corrective exercise group (CEG, n = 29), rotator cuff exercise group (REG, n = 27), or control group (CG, n = 28) total 84 male patients enrolled in this study (Fig. 1). Table 1 shows the characteristics of participants. This study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the Institutional Review Board of Sungkyunkwan University College of Medicine, Samsung Medical Center (no. SMC 2020-07-057). Table 1 shows the characteristics of participants.
Fig. 1.
Study flow chart
Table 1.
Participants’ characteristics
| Corrective exercise group (n = 29) | Rotator cuff exercise group (n = 27) | Control group (n = 28) |
p value | |
|---|---|---|---|---|
| Age, years | 58.21 ± 6.55 | 58.95 ± 9.05 | 59.96 ± 7.74 | 0.698 |
| Height, cm | 168.67 ± 9.05 | 169.83 ± 5.78 | 168.77 ± 6.27 | 0.719 |
| Weight, kg | 70.40 ± 8.54 | 70.17 ± 10.96 | 71.63 ± 12.21 | 0.860 |
| Body mass index, kg/m2 | 24.68 ± 2.16 | 24.31 ± 3.44 | 25.07 ± 3.46 | 0.656 |
| Dominant arm, right/left | 28/1 | 27/0 | 26/2 | |
| Involved side, right/left | 22/7 | 20/7 | 17/11 | |
| Tear size, small/medium | 8/21 | 10/17 | 8/20 | |
| Forward shoulder angle, ° | 33.72 ± 6.36 | 31.52 ± 5.27 | 31.00 ± 6.35 | 0.508 |
Values are presented as mean ± standard deviation or n, as appropriate
Forward shoulder posture measurement
All patients underwent an assessment of their forward shoulder posture before surgery, and the examination method was as follows. Each participant was evaluated three times for forward shoulder posture while standing upright and looking straight ahead. Prior to the measurement, the participants were instructed to move their shoulders forward while keeping their bodies relaxed. Markers were placed on the acromion and spinous process of the seventh cervical vertebra (C7) to evaluate the forward shoulder angle and upper-body posture.
The patients were captured on camera using a smartphone in the sagittal plane with two markers. The angle of the forward shoulder was calculated by measuring the distance from a vertical extension running from the posterior to a line that connects the C7 and acromial markers (Fig. 2). An angle exceeding or equal to 22 degrees was classified as an abnormal forward shoulder angle [14].
Fig. 2.
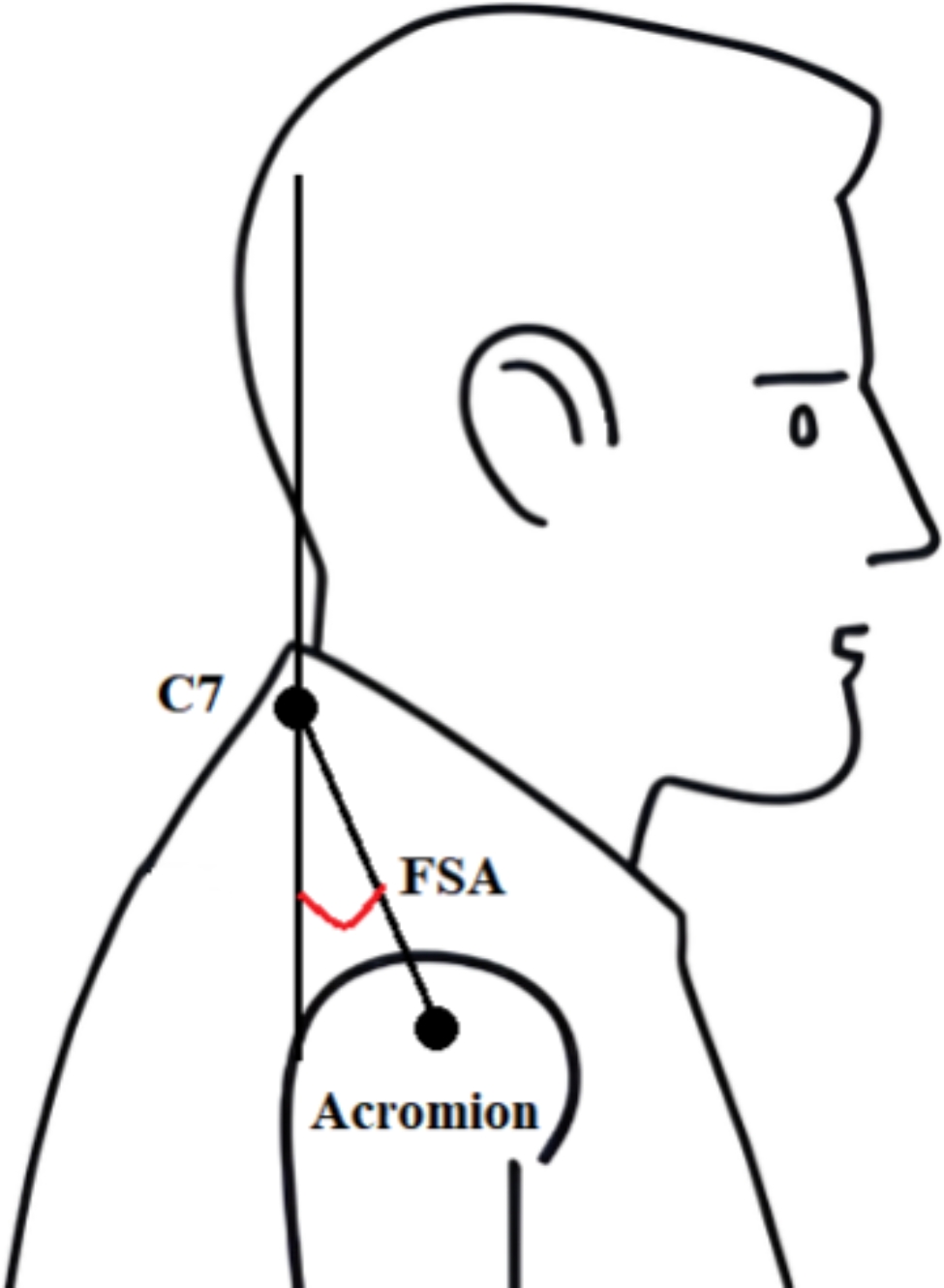
Forward shoulder angle assessment performed in the sagittal plane
Range of motion(ROM) measurement
The ROM of the shoulder was evaluated before the surgery and at 6 months and 1 year after the surgery. To measure the shoulder joint ROM, the participant was seated and the ROM of forward flexion, abduction, and external rotation was measured in degrees using a goniometer. Moreover, the ROM of internal rotation was assessed using the back-scratch method at the spinal level. This test was repeated twice and the average value was analyzed [15].
Shoulder function assessment
The function of the shoulder was evaluated before the surgery and 6 months and 1 year after the surgery. The assessments were done using two questionnaires: the American Shoulder and Elbow Surgeons (ASES) questionnaire and the Constant score. The ASES was created by the American Shoulder and Elbow Surgeons. The ASES score consists of two subscores: activity of daily living (ADL) and a pain visual analog scale (VAS), but it is reported as a single overall score. It is a patient-reported score with subscales for pain and function, ranging from 0 (worst pain and functional loss) to 50 (no pain and excellent function). The two subscores are summed for a maximum total score of 100, as previously described [16].
The Constant score, which was introduced by Constant and Murley, is another commonly used questionnaire. The Constant score is comprised of four subscales: pain (up to 15 points), ADL (up to 20 points), ROM (up to 40 points), and strength (up to 25 points). The total score ranges from 0 to 100, with higher scores indicating better shoulder function [17].
Muscle strength
Muscle strength was measured using a handheld dynamometer to measure the isometric strength of the shoulder’s scaption, external and internal rotation. The muscle contraction was isometric, and the final value was recorded as the average of two measurements [18].
The measurement of scaption strength is performed by flexing the shoulder 90 degrees forward flexion and abducting the arm 30–40 degrees to match the scapular plane position of the scapula. The examiner places the handheld dynamometer on the patient’s forearm and measures the patient’s strength. To measure internal and external rotation strength, the patient maintains a position with the elbow flexed at 90 degrees and abducted at 0 degrees. The examiner places the handheld dynamometer on the inner side of the forearm to measure internal rotation strength, and on the outer side of the forearm to measure external rotation strength. The results were recorded in pounds (lb). This study calculated the percentage deviation (%) between the injured and non-injured sides as affected side/non-affected side × 100 and analyzed the absolute values of these deviations. The muscle strength of the shoulder was evaluated before the surgery and 6 months and 1 year after the surgery.
Exercise program
All exercise programs were instructed by a clinical exercise specialist with over 10 years of clinical experience.
ROM exercises
All the participants underwent ROM exercises after surgery. Additionally, they used a continuous passive motion machine for 30 min after the surgery to improve their ROM for 2–4 weeks.
At 6 weeks postoperatively, the participants performed passive shoulder flexion exercises on a table by sliding their arms forward and backward. Gradually, they performed passive external rotation exercises using a medical stick for 10 weeks postoperatively without experiencing any pain [19].
Corrective exercise program
All patients were educated on the following exercise program and began exercising between 10 and 12 weeks postoperatively. The program aimed to strengthen the weakened lower trapezius, serratus anterior, and infraspinatus muscles by carrying out strengthening exercises. Meanwhile, the tight muscles, such as the upper trapezius and pectoral muscles, were subjected to stretching exercises. The exercise intensity was set at a moderate level, with a rating of perceived exertion (RPE) of 13. The corrective exercise program lasted for 50 min, consisting of a 15 min warm-up and stretching period, 30 min of strength exercises, and a 5 min cool-down. The patients were instructed to perform the exercise program at home three times a week, including three sets of 15 repetitions for each exercise (Table 2).
Table 2.
Exercise program
| Corrective exercise program | Rotator cuff exercise program | Intensity | |
|---|---|---|---|
|
Warm up (15 min) |
Upper body ergometer Pectoralis stretching Latissimus dorsi stretching |
Upper body ergometer Shoulder flexion stretching Shoulder rotation stretching |
RPE 11 |
|
Main exercise (30 min) |
Shoulder shrug Scapular re-protraction Punch exercise Prone shoulder abduction |
Scaption Band Internal rotation Band external rotation Band extension |
RPE 13 |
|
Cool down (5 min) |
Pectoralis stretching Latissimus dorsi stretching |
Shoulder flexion stretching Shoulder rotation stretching |
RPE 11 |
RPE: Rating of perceived exertion
After the initial exercise education, we provided an at-home video exercise program to enhance exercise compliance. We also held telephone-based educational sessions to encourage at-home exercising and provided feedback on the exercise program to increase adherence rates.
Rotator cuff exercise program
All patients were educated on the following exercise program and began exercising between 10 and 12 weeks postoperatively. The rotator cuff exercise program aimed to strengthen the supraspinatus, infraspinatus, and teres minor muscles. The stretching exercises were designed to aid in the recovery of limited ROM after surgery. A TheraBand was used for the rotator cuff exercises, and participants were instructed to avoid using compensatory mechanisms during the exercise.
The exercise intensity was determined using the RPE and maintained at a level perceived by the participants as RPE 13. This was achieved by adjusting the band resistance. The exercise program consisted of a 15 min warm-up and stretching period, followed by a 30 min strength exercise, and 5 min cool-down. Patients were instructed to conduct the exercise program at home three times a week with three sets of 15 repetitions each (Table 2).
To improve adherence to the at-home program, a video program was distributed. Telerehabilitation sessions were conducted, and feedback on the exercise program was provided to improve participant compliance.
Statistical analysis
The data analysis was performed using Windows SPSS/PC ver. 21 (IBM Corp., Armonk, NY, USA). All variables were analyzed using descriptive statistics. Data are presented as mean (M) and standard deviation (SD).
The Kolmogorov-Smirnov test was performed to confirm data normality. To assess the intergroup differences in shoulder function and strength, repeated-measures ANOVA analysis of variance was conducted. For post-hoc test, one-way ANOVA analysis was conducted to confirm the differences between groups. A significance level of α = 0.05 was used for all statistical analyses.
Results
Shoulder ROM
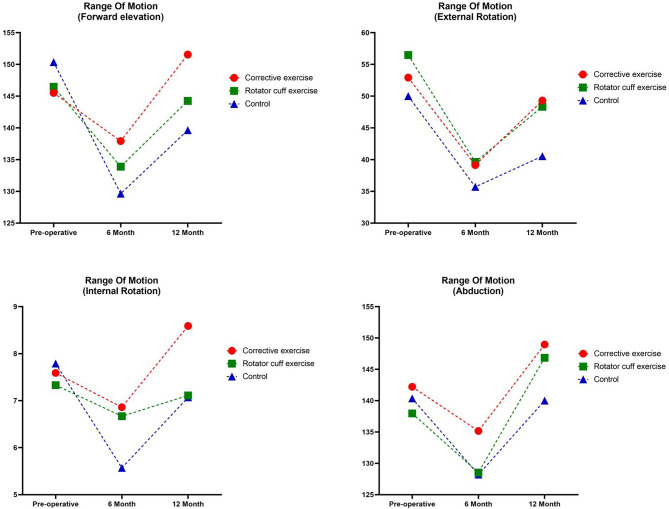
ROM significantly increased after the 6 and 12 months of exercise in all groups but not a significant the intergroup difference, the interaction between time and group (Table 3; Fig. 3).
Table 3.
Postoperative shoulder range of motion
| Variable | Group | Preoperative | 6 months postoperative | 12 months postoperative | Effect | F | p value | partial η2 |
|---|---|---|---|---|---|---|---|---|
| Forward elevation | CE | 145.52 ± 27.59 | 137.93 ± 16.56 | 151.55 ± 12.76 | G | 0.95 | 0.392 | 0.023 |
| RE | 146.48 ± 23.85 | 133.89 ± 20.21 | 144.26 ± 10.63 | T | 15.31 | 0.000*** | 0.159 | |
| C | 150.36 ± 19.90 | 129.64 ± 21.69 | 139.64 ± 20.99 | G×T | 1.92 | 0.124 | 0.045 | |
| External rotation | CE | 52.93 ± 16.18 | 39.14 ± 15.53 | 49.31 ± 15.10 | G | 1.86 | 0.162 | 0.283 |
| RE | 56.48 ± 17.42 | 39.63 ± 15.50 | 48.33 ± 13.45 | T | 28.97 | 0.000*** | 0.263 | |
| C | 50.00 ± 19.27 | 35.71 ± 17.68 | 40.54 ± 15.53 | G×T | 0.573 | 0.669 | 0.014 | |
| Internal rotation | CE | 7.59 ± 4.18 | 6.86 ± 2.99 | 8.59 ± 2.73 | G | 0.902 | 0.410 | 0.022 |
| RE | 7.33 ± 3.60 | 6.67 ± 2.76 | 7.11 ± 2.90 | T | 6.53 | 0.002** | 0.075 | |
| C | 7.79 ± 3.20 | 5.57 ± 3.49 | 7.07 ± 3.20 | G×T | 1.50 | 0.205 | 0.036 | |
| Abduction | CE | 142.21 ± 30.96 | 135.17 ± 21.48 | 148.97 ± 13.45 | G | 0.977 | 0.381 | 0.024 |
| RE | 137.96 ± 30.20 | 128.52 ± 22.31 | 146.85 ± 11.19 | T | 12.43 | 0.000*** | 0.133 | |
| C | 140.36 ± 23.96 | 128.21 ± 24.35 | 140.00 ± 20.18 | G×T | 0.51 | 0.704 | 0.012 |
Values are presented as mean ± standard deviation
CE: corrective exercise; RE: rotator cuff exercise; C: Control; G: group; T: time
*p < 0.05, **p < 0.01, ***p < 0.001
Fig. 3.
Changes in shoulder range of motion
Shoulder function
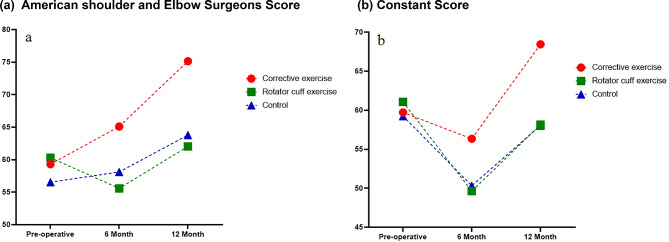
Changes in mean ASES score
ASES score significantly increased after the 6 and 12 weeks of exercise in all groups (p = 0.000, F = 16.74), and there was also a significant intergroup difference (p = 0.002, F = 7.03) and a significant interaction between time and group (p = 0.009, F = 3.78). Post hoc analysis revealed that the corrective exercise group had significantly higher ASES scores than the rotator cuff and control groups at 6 and 12 months after surgery (p < 0.001) (Table 4; Fig. 4a).
Table 4.
Functional outcomes after surgery as evaluated by the ASES, constant score
| Variable | Group | Preoperative | 6 months postoperative | 12 months postoperative | Effect | F | p value | partial η2 |
|---|---|---|---|---|---|---|---|---|
| ASES | CE | 59.31 ± 16.31 | 65.10 ± 9.12 | 75.14 ± 9.73 | G | 7.03 | 0.002** | 0.148 |
| RE | 60.30 ± 10.37 | 55.59 ± 7.34 | 62.04 ± 11.12 | T | 16.74 | 0.000*** | 0.171 | |
| C | 56.54 ± 13.22 | 58.11 ± 9.96 | 63.73 ± 15.12 | G×T | 3.78 | 0.009** | 0.085 | |
| Post-hoc | CE > RE, C### | CE > RE, C### | ||||||
| Constant | CE | 59.72 ± 16.20 | 56.34 ± 10.25 | 68.45 ± 10.89 | G | 3.86 | 0.025* | 0.087 |
| RE | 61.07 ± 11.50 | 49.63 ± 8.21 | 58.15 ± 8.94 | T | 21.76 | 0.000*** | 0.212 | |
| C | 59.25 ± 14.13 | 50.32 ± 9.47 | 58.04 ± 13.73 | G×T | 2.96 | 0.032* | 0.068 | |
| Post-hoc | CE > RE# | CE > RE, C## |
Values are presented as mean ± standard deviation
CE: corrective exercise; RE: rotator cuff exercise; C: Control; G: group; T: time
The result of RM ANOVA was described: *p < 0.05, **p < 0.01, ***p < 0.001
The result of One-way ANOVA for post-hoc was described: #p < 0.05, ##p < 0.01, ###p < 0.001
Fig. 4.
Changes in shoulder functional score
Changes in mean constant score
The constant score significantly increased after the 6 and 12 weeks of exercise in all groups (p = 0.000, F = 21.76), and there was also a significant intergroup difference (p = 0.025, F = 3.86) and a significant interaction between time and group (p = 0.032, F = 2.96). Post hoc analysis revealed that the corrective exercise group had significantly higher constant scores than the rotator cuff and control groups at 12 months after surgery (Table 4; Fig. 4b).
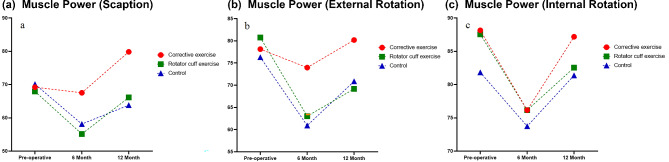
Changes in muscle strength
Changes in the scaption muscle strength ratio
The scaption muscle strength ratio significantly increased after the 6 and 12 months of exercise in all groups (p = 0.002, F = 7.81). There was a significant group (p = 0.025, F = 3.88) but not a significant interaction between the groups (p = 0.124, F = 1.97). Post hoc analysis revealed that the corrective exercise group had a higher scaption muscle strength ratio than the rotator cuff exercise 6 months after the surgery (p < 0.05). Moreover, after 12 months, the corrective exercise group showed a higher scaption muscle strength ratio than the rotator cuff and control groups (Table 5; Fig. 5a).
Table 5.
Changes in shoulder muscle strength ratio during follow-up
| Variable | Group | Preoperative | 6 months postoperative | 12 months postoperative | Effect | F | p value | partial η2 |
|---|---|---|---|---|---|---|---|---|
| Scaption | CE | 69.22 ± 24.27 | 67.53 ± 22.29 | 79.84 ± 18.74 | G | 3.88 | 0.025* | 0.087 |
| RE | 67.94 ± 25.66 | 55.16 ± 18.15 | 66.13 ± 14.06 | T | 7.81 | 0.002** | 0.088 | |
| C | 70.12 ± 22.64 | 58.14 ± 13.74 | 63.81 ± 13.02 | G×T | 1.97 | 0.124 | 0.046 | |
| Post-hoc | CE > RE# | CE > RE, C### | ||||||
| External Rotation | CE | 78.14 ± 19.04 | 73.98 ± 23.74 | 80.20 ± 13.61 | G | 4.15 | 0.019* | 0.093 |
| RE | 80.76 ± 16.11 | 63.03 ± 14.82 | 69.18 ± 14.45 | T | 13.48 | 0.000*** | 0.143 | |
| C | 76.31 ± 18.13 | 60.92 ± 16.42 | 70.90 ± 13.20 | G×T | 2.01 | 0.103 | 0.047 | |
| Post-hoc | CE > RE# | CE > RE, C## | ||||||
| Internal Rotation | CE | 88.15 ± 16.01 | 83.95 ± 19.10 | 87.19 ± 10.13 | G | 5.41 | 0.006* | 0.118 |
| RE | 87.56 ± 8.59 | 76.16 ± 9.80 | 82.54 ± 9.57 | T | 11.94 | 0.000*** | 0.128 | |
| C | 81.84 ± 15.12 | 73.74 ± 8.94 | 81.37 ± 7.51 | G×T | 0.97 | 0.427 | 0.023 | |
| Post-hoc | CE > RE# |
Values are presented as mean ± standard deviation
CE: corrective exercise; RE: rotator cuff exercise; C: Control; G: group; T: time
The result of RM ANOVA was described: *p < 0.05, **p < 0.01, ***p < 0.001
The result of One-way ANOVA for post-hoc was described: #p < 0.05, ##p < 0.01, ###p < 0.001
Fig. 5.
Changes in shoulder muscle strength
Changes in external rotation muscle strength ratio
The external rotation muscle strength significantly increased after 6 and 12 months of exercise in all groups (p = 0.000, F = 13.48). There was a significant group (p = 0.019, F = 4.15) but not a significant interaction between the groups (p = 0.103, F = 2.01). Post hoc analysis revealed that the corrective exercise group had a higher external rotation muscle strength than the rotator cuff exercise 6 months after the surgery (p < 0.05). Moreover, after 12 months, the corrective exercise group showed a higher external rotation muscle strength than the rotator cuff and control groups (Table 5; Fig. 5b).
Changes in internal rotation muscle strength ratio
The internal rotation muscle strength significantly increased after 6 and 12 months of exercise in all groups (p = 0.000, F = 11.94). There was a significant group (p = 0.006, F = 5.41) but not a significant interaction between the groups (p = 0.427, F = 0.97). Post hoc analysis revealed that the corrective exercise group had a higher internal rotation muscle strength than the rotator cuff exercise 6 months after the surgery (p < 0.05). However, there was no significant difference between the groups after 12 weeks (Table 5; Fig. 5c).
Discussion
This study aimed to assess and compare the effects of corrective and rotator cuff exercises on the ROM, strength, and function of the shoulder joint in patients with a forward shoulder posture after undergoing arthroscopic rotator cuff repair surgery.
The shoulder joint has the widest range of motion and can move in more directions than any other joint. Its unique characteristics are essential for proper shoulder function [20].
The importance of shoulder joint instability and ROM cannot be overstated. An increased ROM in the shoulder joint can lead to instability, while improved stability can limit ROM. Therefore, normal ROM and shoulder joint stability are two important factors in shoulder function [21].
After undergoing rotator cuff repair surgery, all patients must wear an abduction brace for 4–6 weeks to maintain the repaired rotator cuff’s stability. However, during this period, overactive shoulder motion is restricted, resulting in a limited shoulder range of motion. After the brace is removed, shoulder movements may continue to be restricted [22].
In this study, the ROM of the shoulder joint increased postoperatively in all three groups, but no significant differences were observed between the groups. These results suggest that ROM in the shoulder joint is influenced more by the anatomical integrity of the rotator cuff than by differences in the strength or muscle activation of the rotator cuff muscles [23]. Previous studies have shown that a forward shoulder and head posture reduced the forward flexion range of up to 15° and the flexion velocity by 8% [24, 25] contributing to an imbalance in the upper trapezius, lower trapezius, and serratus anterior muscles, leading to altered shoulder movements. Baskurt et al. [26] demonstrated that corrective exercises could help to improve ROM in forward flexion, external rotation, internal rotation, and abduction of the shoulder joint in patients with subacromial impingement syndrome or frozen shoulder conditions. In our study, ROM did not show significant differences between groups compared to previous studies. However, the greatest improvement in ROM was revealed with CEG.
In the present study, we used various measurement methods and questionnaires to evaluate shoulder joint function to confirm changes between the groups after corrective exercises [27, 28]. The results of this study showed that at 6 and 12 months after surgery, the CEG group had the highest shoulder joint function scores. These results are thought to be due to the fact that a corrective exercise program effectively improves the position and orientation of the scapula and muscle imbalance, leading to better shoulder function.
Patients with a forward shoulder posture result in changes in their biomechanics and muscle activation patterns in the shoulder joints. As a result, the serratus anterior muscle weakens, leading to shoulder joint instability and decreased shoulder function [29]. The optimal scapular position and coordinated muscle activation of the surrounding muscles require functional shoulder joint stability. The sequence of muscle activation and engagement is crucial in the generation of shoulder joint movements when moving the arm [30]. The pectoral muscles are the most important muscles related to forward shoulder posture. Shortening the major and minor pectoralis muscles pulls the scapula into the rib cage, resulting in scapular mispositioning. In contrast, the weakening of muscles such as the serratus anterior, rhomboid, middle, and lower trapezius is characteristic of altered scapular positioning. These muscular imbalances play a fundamental role in creating a forward shoulder posture [13].
Considering these aspects, the exercise program consisted of stretching exercises for the shortened pectoralis muscles and a strength training program for lengthening the serratus anterior, rhomboid, middle, and lower trapezius muscles [25]. A corrective exercise program can strengthen the muscles around the weakened shoulder joint and correct muscle activation imbalances. Compared to previous studies, this exercise program used in this study improved the shoulder joint stability, and shoulder function through improved the forward shoulder posture [31].
Patients with a forward shoulder posture who undergo rotator cuff repair surgery often experience acute pain and inflammatory reactions during the postoperative phase. These factors can exacerbate muscle imbalances and lead to repetitive patterns of impaired movement [32]. Therefore early exercise intervention is crucial for improving muscle imbalance and increasing joint function postoperatively [33].
The results of this study showed that scaption strength and external rotation strength in the corrective exercise group were better than those in the rotator cuff exercise group at 6 months after surgery, and scaption strength in the corrective exercise group was better than that in the other two groups at 12 months after surgery. The results of this study showed that scaption strength, internal rotation, and external rotation strength in the corrective exercise group were better than those in the rotator cuff exercise group at 6 months after surgery, and scaption strength in the corrective exercise group was better than that in the other two groups at 12 months after surgery. The results from this study were similar to previous studies, which have shown that corrective exercise programs increase upper-body muscle strength in middle-aged women who experience shoulder pain [34, 35].
Corrective exercises for postural correction alter the scapular position to an anatomically normal position and inhibit excessive activity of the upper trapezius while activating the middle trapezius, lower trapezius, serratus anterior, and rhomboid muscles. These changes can reduce the load on the shoulder joint, allowing more efficient shoulder joint movements [36]. These changes increase shoulder joint stability and promote mechanoreceptors, which positively affect muscle strength, resulting in significant differences in muscle strength between groups [37]. For this reason, it is believed that this study also showed a significant difference in strength improvement in the group that performed the corrective exercise program compared to the rotator cuff strength exercise group.
The optimal position of the scapula is parallel to the spine and is positioned approximately 3 inches from the midline of the thorax. The scapula is located between the second and seventh thoracic vertebrae, parallel to the ribs, and tilted about 30° from the frontal plane [38]. However, forward shoulder posture experience altered scapular position and movement could affect the coupling force of the scapular muscles between the trapezius and serratus anterior muscles, which are crucial for scapular movement and lead to the breakdown of movement patterns. Overall, muscle imbalance around the shoulder joint can increase stress on the shoulder joint [39, 40].
Kibler et al. [41] reported that it is important to first stabilize the proximal musculature before initiating movement of the distal musculature to enhance overall body movements. In order to achieve anatomical stability by balancing the muscular forces around the scapula, corrective exercises should focus on the proximal musculature of the shoulder joint. These exercises also help in dynamic stabilization of the scapula by engaging the surrounding muscles during active arm movements [42].
Scapular malalignment due to muscle imbalance causes an imbalance between muscle length and strength. Muscle imbalance in the shoulder joint ultimately influences its functional movement [14]. The corrective exercise program implemented in this study addresses muscle imbalances caused by postural asymmetry and positively influences muscle activation, leading to improved outcomes compared with other programs.
The strength of this study lies in its focus on patients who underwent rotator cuff repair and have a forward shoulder posture. While many researchers have examined the effects of exercise following rotator cuff repair, studies specifically targeting patients with certain postures, as in this research, are rare. Additionally, this study distinguished itself by separating participants into groups to clearly assess the effects of rotator cuff exercises and corrective exercises. It is already somewhat established in the literature that combining rotator cuff exercises and corrective exercises can yield positive results. However, there are very few studies that have evaluated these two types of exercises independently. Therefore, the greatest strength of this study is its verification of the effects of corrective exercises in patients with forward shoulder posture who have undergone rotator cuff repair.
This study has several limitations. First, variations in the daily activity levels of participants could not be controlled. The extent to which the exercise program was performed may vary depending on each patient’s activity level or regular exercise habits, but this was beyond our control. Second, we could not standardize the participants’ understanding of each exercise program. Although we used consistent language and expressions during exercise education to convey the same information, individual comprehension could not be controlled. Lastly, while the exercise program was encouraged via phone calls following a single education session, there was no separate process in place to verify whether the exercises were actually performed.
Conclusion
Our study found that a corrective exercise program can enhance the strength and function of shoulder muscles in male patients with a forward shoulder posture undergoing rotator cuff repair surgery. For these patients, corrective exercises can be beneficial in improving both shoulder function and muscle strength.
Abbreviations
- ADL
Activity of daily living
- ASES
American Shoulder and Elbow Surgeons
- CEG
Corrective exercise group
- CG
Control group
- REG
Rotator cuff exercise group
- ROM
Range of motion
- RPE
Rating of perceived exertion
- VAS
Visual analog scale
Author contributions
Conceptualization, S.M.L. and M.S.C.; methodology, M.K.K.; formal analysis, Y.J.P.; investigation, Y.G.S. and K.B.M.; resources, S.M.L. and Y.G.S.; data curation, H.H.M. and J.M.P; original draft preparation, M.S.C.; and review and editing, S.M.L. and M.S.S. All authors have read and agreed to the published version of the manuscript.
Funding
This study received no external funding.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
This study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the Institutional Review Board of Sungkyunkwan University College of Medicine, Samsung Medical Center (no. SMC 2020-07-057). Informed consent was obtained from all participants and/or their legal guardians prior to their involvement in the study. Identifying details of the participants have been omitted to protect their privacy.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sergienko S, Kalichman L. Myofascial origin of shoulder pain: a literature review. J Bodyw Mov Ther. 2015;19(1):91–101. [DOI] [PubMed] [Google Scholar]
- 2.Dube MO, Desmeules F, Lewis J, Roy JS. Rotator cuff-related shoulder pain: does the type of exercise influence the outcomes? Protocol of a randomised controlled trial. BMJ Open. 2020;10(11):e039976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Conti M, Garofalo R, Delle Rose G, Massazza G, Vinci E, Randelli M, et al. Post-operative rehabilitation after surgical repair of the rotator cuff. Chir Organi Mov. 2009;93(Suppl 1):S55–63. [DOI] [PubMed] [Google Scholar]
- 4.Keener JD. Revision rotator cuff repair. Clin Sports Med. 2012;31(4):713–25. [DOI] [PubMed] [Google Scholar]
- 5.Mazuquin BF, Wright AC, Russell S, Monga P, Selfe J, Richards J. Effectiveness of early compared with conservative rehabilitation for patients having rotator cuff repair surgery: an overview of systematic reviews. Br J Sports Med. 2018;52(2):111–21. [DOI] [PubMed] [Google Scholar]
- 6.Kim YS, Chung SW, Kim JY, Ok JH, Park I, Oh JH. Is early passive motion exercise necessary after arthroscopic rotator cuff repair? Am J Sports Med. 2012;40(4):815–21. [DOI] [PubMed] [Google Scholar]
- 7.Nikolaidou O, Migkou S, Karampalis C. Rehabilitation after rotator cuff repair. Open Orthop J. 2017;11:154–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Altintas B, Anderson N, Dornan GJ, Boykin RE, Logan C, Millett PJ. Return to sport after arthroscopic rotator cuff repair: is there a difference between the recreational and the competitive athlete? Am J Sports Med. 2020;48(1):252–61. [DOI] [PubMed] [Google Scholar]
- 9.Mollison S, Shin JJ, Glogau A, Beavis RC. Postoperative rehabilitation after rotator cuff repair: a web-based survey of AANA and AOSSM members. Orthop J Sports Med. 2017;5(1):2325967116684775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Turgut E, Duzgun I, Baltaci G. Effects of scapular stabilization exercise training on scapular kinematics, disability, and pain in subacromial impingement: a randomized controlled trial. Arch Phys Med Rehabil. 2017;98(10):1915–23. e3. [DOI] [PubMed] [Google Scholar]
- 11.Page MJ, Green S, McBain B, Surace SJ, Deitch J, Lyttle N, et al. Manual therapy and exercise for rotator cuff disease. Cochrane Database Syst Rev. 2016;2016(6):CD012224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bodin J, Ha C, Chastang JF, Descatha A, Leclerc A, Goldberg M, et al. Comparison of risk factors for shoulder pain and rotator cuff syndrome in the working population. Am J Ind Med. 2012;55(7):605–15. [DOI] [PubMed] [Google Scholar]
- 13.Kibler WB, Sciascia A, Wilkes T. Scapular dyskinesis and its relation to shoulder injury. J Am Acad Orthop Surg. 2012;20(6):364–72. [DOI] [PubMed] [Google Scholar]
- 14.Thigpen CA, Padua DA, Michener LA, Guskiewicz K, Giuliani C, Keener JD, et al. Head and shoulder posture affect scapular mechanics and muscle activity in overhead tasks. J Electromyogr Kinesiol. 2010;20(4):701–9. [DOI] [PubMed] [Google Scholar]
- 15.Hanney WJ, Kolber MJ, Marshall JS. The reliability of clinical measurements designed to quantify shoulder mobility. Phys Ther Rev. 2011;16(6):413–22. [Google Scholar]
- 16.Richards RR, An KN, Bigliani LU, Friedman RJ, Gartsman GM, Gristina AG, et al. A standardized method for the assessment of shoulder function. J Shoulder Elb Surg. 1994;3(6):347–52. [DOI] [PubMed] [Google Scholar]
- 17.Placzek JD, Lukens SC, Badalanmenti S, Roubal PJ, Freeman DC, Walleman KM, et al. Shoulder outcome measures: a comparison of 6 functional tests. Am J Sports Med. 2004;32(5):1270–7. [DOI] [PubMed] [Google Scholar]
- 18.Kolber MJ, Beekhuizen K, Cheng MS, Fiebert IM. The reliability of hand-held dynamometry in measuring isometric strength of the shoulder internal and external rotator musculature using a stabilization device. Physiother Theory Pract. 2007;23(2):119–24. [DOI] [PubMed] [Google Scholar]
- 19.Jeong JY, Shim SB, Hong JH, Im W, Lee SM, Yoo JC. Effect of preoperative frozen shoulder on clinical outcomes after arthroscopic rotator cuff repair. Orthop J Sports Med. 2020;8(7):2325967120934449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Halder AM, Itoi E, An KN. Anatomy and biomechanics of the shoulder. Orthop Clin North Am. 2000;31(2):159–76. [DOI] [PubMed] [Google Scholar]
- 21.Veeger HE, van der Helm FC. Shoulder function: the perfect compromise between mobility and stability. J Biomech. 2007;40(10):2119–29. [DOI] [PubMed] [Google Scholar]
- 22.Ross D, Maerz T, Lynch J, Norris S, Baker K, Anderson K. Rehabilitation following arthroscopic rotator cuff repair: a review of current literature. J Am Acad Orthop Surg. 2014;22(1):1–9. [DOI] [PubMed] [Google Scholar]
- 23.Gazielly DF, Gleyze P, Montagnon C. Functional and anatomical results after rotator cuff repair. Clin Orthop Relat Res. 1994(304):43–53. [PubMed]
- 24.Malmstrom EM, Olsson J, Baldetorp J, Fransson PA. A slouched body posture decreases arm mobility and changes muscle recruitment in the neck and shoulder region. Eur J Appl Physiol. 2015;115(12):2491–503. [DOI] [PubMed] [Google Scholar]
- 25.Kibler WB, Sciascia A. Evaluation and management of scapular dyskinesis in overhead athletes. Curr Rev Musculoskelet Med. 2019;12(4):515–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baskurt Z, Baskurt F, Gelecek N, Ozkan MH. The effectiveness of scapular stabilization exercise in the patients with subacromial impingement syndrome. J Back Musculoskelet Rehabil. 2011;24(3):173–9. [DOI] [PubMed] [Google Scholar]
- 27.Kirkley A, Griffin S, Dainty K. Scoring systems for the functional assessment of the shoulder. Arthroscopy. 2003;19(10):1109–20. [DOI] [PubMed] [Google Scholar]
- 28.Longo UG, Vasta S, Maffulli N, Denaro V. Scoring systems for the functional assessment of patients with rotator cuff pathology. Sports Med Arthrosc Rev. 2011;19(3):310–20. [DOI] [PubMed] [Google Scholar]
- 29.Quek J, Pua YH, Clark RA, Bryant AL. Effects of thoracic kyphosis and forward head posture on cervical range of motion in older adults. Man Ther. 2013;18(1):65–71. [DOI] [PubMed] [Google Scholar]
- 30.Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26(2):325–37. [DOI] [PubMed] [Google Scholar]
- 31.Comel JC, Nery RM, Garcia EL, da Silva Bueno C, de Oliveira Silveira E, Zarantonello MM, et al. A comparative study on the recruitment of shoulder stabilizing muscles and types of exercises. J Exerc Rehabil. 2018;14(2):219–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sahrmann S. Diagnosis and treatment of movement impairment syndromes. St. Louis: Mosby; 2002. [Google Scholar]
- 33.Sepehri S, Sheikhhoseini R, Piri H, Sayyadi P. The effect of various therapeutic exercises on forward head posture, rounded shoulder, and hyperkyphosis among people with upper crossed syndrome: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2024;25(1):105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Choi SH, Lee BH, Chung EJ. The effects of stability exercises on shoulder pain and function of middle-aged women. J Phys Ther Sci. 2013;25(2):155–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ludewig PM, Reynolds JF. The association of scapular kinematics and glenohumeral joint pathologies. J Orthop Sports Phys Ther. 2009;39(2):90–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wegner S, Jull G, O’Leary S, Johnston V. The effect of a scapular postural correction strategy on trapezius activity in patients with neck pain. Man Ther. 2010;15(6):562–6. [DOI] [PubMed] [Google Scholar]
- 37.Lephart SM, Fu FH. Proprioception and neuromuscular control in joint stability. Champaign, IL: Human Kinetics; 2000. [Google Scholar]
- 38.Sahrmann S, Azevedo DC, Dillen LV. Diagnosis and treatment of movement system impairment syndromes. Braz J Phys Ther. 2017;21(6):391–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stackhouse SK, Stapleton MR, Wagner DA, McClure PW. Voluntary activation of the infraspinatus muscle in nonfatigued and fatigued states. J Shoulder Elb Surg. 2010;19(2):224–9. [DOI] [PubMed] [Google Scholar]
- 40.Kendall FP, McCreary EK, Provance PG, Rodgers MM, Romani WA, Muscles: testing and function with posture and pain. 5th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 41.Kibler WB, Press J, Sciascia A. The role of core stability in athletic function. Sports Med. 2006;36(3):189–98. [DOI] [PubMed] [Google Scholar]
- 42.Mottram SL. Dynamic stability of the scapula. Man Ther. 1997;2(3):123–31. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.