Abstract
Neuronal voltage-gated calcium channels play a pivotal role in the conversion of electrical signals into calcium entry into nerve endings that is required for the release of neurotransmitters. They are under the control of a number of cellular signaling pathways that serve to fine tune synaptic activities, including G-protein coupled receptors (GPCRs) and the opioid system. Besides modulating channel activity via activation of second messengers, GPCRs also physically associate with calcium channels to regulate their function and expression at the plasma membrane. In this mini review, we discuss the mechanisms by which calcium channels are regulated by classical opioid and nociceptin receptors. We highlight the importance of this regulation in the control of neuronal functions and their implication in the development of disease conditions. Finally, we present recent literature concerning the use of novel μ-opioid receptor/nociceptin receptor modulators and discuss their use as potential drug candidates for the treatment of pain.
Keywords: G-protein coupled receptors, Voltage-gated calcium channels, Mu opioid receptor, Nociception opioid receptor
Introduction
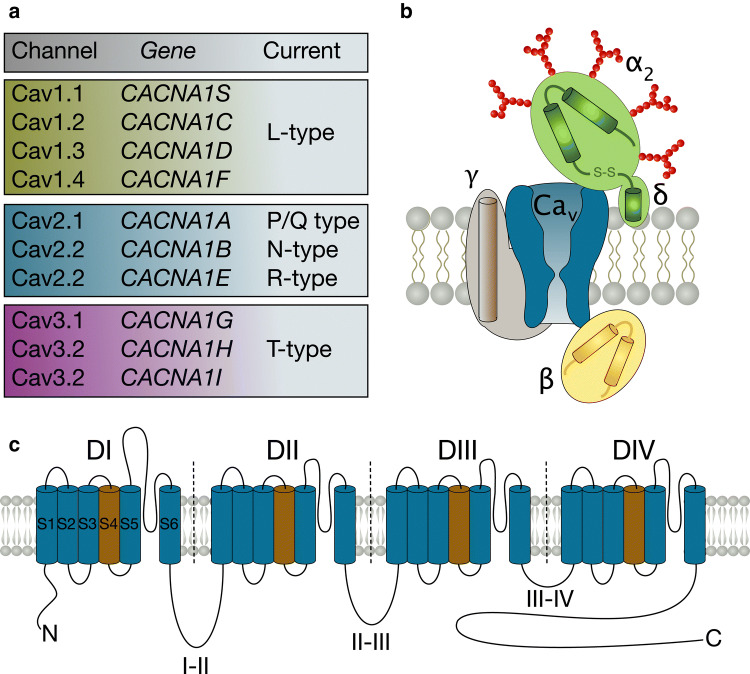
Calcium (Ca2+) is a highly versatile signaling molecule that operates over a wide spatiotemporal range to regulate a plethora of cellular processes (Berridge et al. 2003). Among the various ion channels and receptors that allow the flux of Ca2+ across cellular membranes, voltage-gated Ca2+ channels (VGCCs) represent one of the most important players by converting electrical signals into intracellular Ca2+ elevations (Catterall 2011). VGCCs are pore-forming multisubunit complexes and are activated in response to electrical depolarizations of the plasma membrane to allow the entry of Ca2+ along its electrochemical gradient. Among the ten genes that encode the pore-forming subunits of mammalian VGCCs, seven genes encode the high-voltage-activated channel subfamily that comprise L-type (Cav1.1 to Cav1.4), P/Q-type (Cav2.1), N-type (Cav2.2), and R-type (Cav2.3) channels. In addition, three genes encode the low-voltage-activated subfamily, the so-called T-type channels (Cav3.1 to Cav3.3) (for reviews see (Catterall 2011; Zamponi et al. 2015; Dolphin 2018b). At the structural level, the Cav pore-forming subunits of VGCCs share a similar membrane topology of four homologous domains, each made of six transmembrane helices (S1 to S6), and a re-entrant loop (P-loop) that comprises the pore of the channel and contains elements responsible for Ca2+ selectivity (Wu et al. 2015, 2016; Zhao et al. 2019) (Fig. 1). These four transmembrane domains are connected via intracellular linkers (loops I–II, II–II, and III–IV) and are flanked by cytoplasmic amino- and carboxy-terminal regions that serve as hubs for various regulatory pathways. In addition to the Cav pore-forming subunit, high-voltage-activated channels associate with ancillary subunits (Fig. 1) including the cytoplasmic β-subunit (β1 to β4) that belongs to the membrane-associated guanylate kinase family (Buraei and Yang 2010), the α2δ-subunit (α2δ1 to α2δ4), a highly glycosylated extracellular protein that remains bound to the plasma membrane (Dolphin 2018a), and in some circumstances the transmembrane γ-subunit (γ1 to γ1) (Black 2003; Kang and Campbell 2003). These ancillary subunits serve important functions ranging from channel trafficking, subcellular membrane localization, and gating of the channel (Simms and Zamponi 2014; Campiglio and Flucher 2015).
Fig. 1.
Diversity, composition and structure of voltage-gated calcium channels. a Diversity of voltage-gated calcium channels. The high-voltage activated subfamily comprises Cav1.x (L-type channels) and Cav2.x (P/Q-, N- and R-types channels), while Cav3.x (T-type channels) form the low-voltage-activated subfamily. b Schematic representation of the calcium channel complex consisting of the Cav pore-forming subunit and β, α2δ and γ ancillary subunits. c Membrane topology of the Cav subunit. Transmembrane segments depicted in brown constitute the voltage-sensor of the channel, whereas the extracellular/re-entrant loops connecting segments S5 and S6 hold elements of the selectivity filter and pore permeation
Given the crucial importance of calcium ions, it is not surprising that VGCCs are under the control by several regulatory pathways that allow for the spatiotemporal regulation of the calcium signal. One of the most important regulatory mechanisms relies on heterotrimeric G-protein coupled receptors (GPCRs). In this mini review, we focus on the molecular mechanisms by which opioid receptors (OR) and nociceptin receptors (NOP) regulate VGCCs. We highlight the physiological importance of these regulations and their roles as therapeutic targets.
The Opioid Receptor Family
The existence of receptors for opiates was first proposed in 1954 based on structure–activity relationship studies of a series of synthetic opiates for antinociceptive activity (Beckett and Casy 1954). Additional structure–activity relationship analysis led to the notion that more than one OR type may exist in the mammalian nervous system (Portoghese 1965) and the existence of three ORs named after the prototypic drugs used was proposed: the μ receptor (mu for morphine, MOR), the κ receptor (kappa for ketocyclazocine, KOR), and the δ receptor (delta for deferens, DOR) (Lord et al. 1977). The three ORs were later cloned and in vitro studies have confirmed that recombinant receptors have pharmacological profiles and functional characteristics consistent with their endogenous counterparts (Evans et al. 1992; Kieffer 1995; Kieffer et al. 1992). Subsequently, a search for related receptors by homology cloning led to the identification of the nociceptin receptor (NOP), initially called ORL1 (Mollereau et al. 1994) or LC132 (Bunzow et al. 1994), and named after its endogenous ligand nociceptin (Meunier et al. 1995).
In terms of their neuronal distribution, MOR is present throughout the nervous system where the highest density is found in the thalamus, the caudate putamen, the neocortex, the nucleus accumbens, the amygdala, the interpeduncular complex, the inferior and superior colliculi (Mansour et al. 1987), and to a comparatively moderate extent in the periaqueductal gray and raphe nuclei (Hawkins et al. 1988). MOR is also highly expressed in the dorsal horn of the spinal cord (Besse et al. 1990) where it mediates parts of the analgesic effects of MOR agonists. In contrast, DOR is discretely distributed in the central nervous system with a gradient ranging from high expression levels in forebrain structures to relatively low levels in hindbrain regions (Mansour et al. 1987; Kitchen et al. 1997). In the spinal cord, DOR is present in the dorsal horn (Besse et al. 1990) (although in different neuronal subsets than MOR) where it also plays a role in mediating the analgesic effects of DOR agonists. KOR is located predominantly in the cerebral cortex, nucleus accumbens, claustrum and hypothalamus (Kitchen et al. 1997; Mansour et al. 1987) and has been implicated in several physiological functions including the central regulation of nociception. Finally, the NOP receptor is observed at relatively high densities in the cortex, the anterior olfactory nucleus, the lateral septum, the ventral forebrain, the hippocampus, the amygdala, the substantia nigra, the ventral tegmental area, the locus coeruleus, the brain stem nuclei, and also in the dorsal horn of the spinal cord (Neal Jr et al. 1999). This diffuse distribution in the central nervous system suggests a role for NOP receptors in several physiological functions including motor and aggressive behaviors, reinforcement and reward, as well as nociception.
An important feature in the functioning of ORs is their ability to form heterodimers. For instance, several OR interacting complexes composed of MOR-DOR, MOR-KOR, and DOR-KOR have been described (Fujita et al. 2014). This association provides another layer of functional regulation, best documented for MOR-DOR heterodimers where binding of DOR antagonists enhance the binding affinity for MOR agonists via an allosteric modulation, therefore enhancing morphine-induced analgesia (Fujita et al. 2014). The situation is however divergent for MOR-NOP heterodimers where binding of NOP ligands rather reduces MOR signaling despite an increased MOR agonist affinity for the protomer (Pan et al. 2002). This aspect could potentially be exploited therapeutically and the agonist 3-iodobenzoyl naltrexamine (IBNtx-A) that is thought to act on MOR-NOP heterodimers has shown potent analgesic effects without the occurrence of usual side effects associated with classical MOR agonists (Majumdar et al. 2011). Another example are bivalent ligands that provide a bridge between two receptors and prevent their internalization. Such ligand composed of a MOR agonist (oxymorphone) and DOR antagonist (naltrindole) has shown analgesic activity with comparatively decreased development of tolerance and dependence (Daniels et al. 2005; Lenard et al. 2007).
OR/NOP-Dependent Regulation of Voltage-Gated Calcium Channels
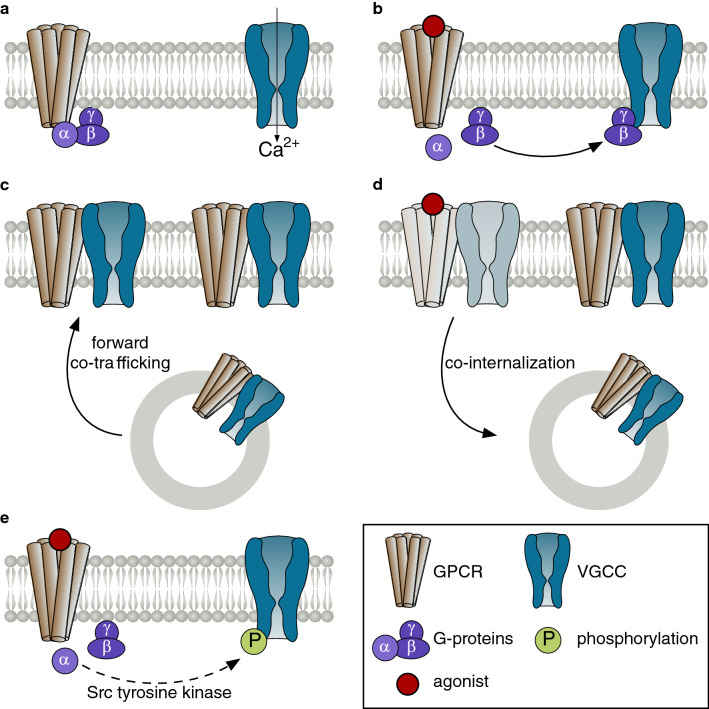
It is well established that VGCCs are potently regulated by a wide range of GPCRs including all OR and NOP receptors. For instance, MOR, DOR, KOR, and NOP agonists all inhibit VGCCs. This regulation essentially affects the Cav2 subfamily (Cav2.1, Cav2.2, and to some extent Cav2.3) and has been documented both on native and recombinant channels (Tsunoo et al. 1986; Morikawa et al. 1999; Carabelli et al. 1998; Toth et al. 1996; Bourinet et al. 1996; Schroeder et al. 1991; Berecki et al. 2016). Mechanistically, this inhibition occurs via activation of heterotrimeric G-proteins upon agonist binding, triggering the exchange of GDP from GTP from the Gα-subunit and the concomitant release of the Gβγ-dimer (Wettschureck and Offermanns 2005) (Fig. 2a, b). While the Gβγ-dimer can modulate several signaling pathways, it also interacts directly with the calcium channel (Fig. 2b) within a Gβγ-binding pocket formed by several channel molecular determinants (essentially the I-II loop and the amino terminal region (Herlitze et al. 1996, 1997; Zamponi et al. 1997; De Waard et al. 1997; Agler et al. 2005)), producing a gating switch from a “willing” to reluctant” state manifested by a hyperpolarized shift of the voltage-dependence of activation of the channel and a potent inhibition of the calcium current (Bean 1989). This is thought to occur predominantly through stabilization of the closed conformation of the channel (Patil et al. 1996; Jones et al. 1997). Additional alterations of the channel ion permeability may also partially contribute to the inhibitory effect of Gβγ (Kuo and Bean 1993). Furthermore, based on the observation that Cavβ and Gβγ share similar channel binding determinants, it was proposed that dissociation of Cavβ upon binding of Gβγ to the channel may contribute to induce the reluctant state of the channel (Sandoz et al. 2004) although this notion has been challenged (Hümmer et al. 2003). Regardless of the exact molecular mechanisms underlying Gβγ-dependent inhibition of Cav2 channels, an important feature is the observation that this inhibition can be overcome experimentally by strong membrane depolarizations which are believed to trigger the transient dissociation of the Gβγ moiety from the channel, which led to the concept of voltage-dependent inhibition (Ikeda 1991). Of physiological importance is the observation that significant recovery from Gβγ inhibition can also occur in response to bursts of action potential waveforms and may constitute a form of short-term synaptic plasticity sensitive to action potential timing and duration (Brody et al. 1997).
Fig. 2.
Model for opioid receptor-dependent regulation of calcium channels. a Schematic representation of the opioid receptor, heterotrimeric G-proteins, and calcium channel in the absence of opioid agonist. b Activation of the receptor upon binding of an opioid agonist triggers the release of G-proteins where binding of the Gβγ dimer directly onto the channel inhibits calcium influx (voltage-dependent inhibition). c Direct interaction of the receptor and the channel allows for a co-trafficking to the plasma membrane and provides another layer of control over the expression of the channel. d Consequently, receptor/channel interaction promotes agonist-dependent co-internalization of the protein complex. e Activation of Gα initiates a cascade of downstream signaling events eventually leading to the phosphorylation of the channel by a Src tyrosine kinase and producing a voltage-independent inhibition of the calcium current
Although G-proteins represent one of the primary mediators for OR/NOP receptor-dependent modulation of Cav2 channels, several studies have documented the physical association of Cav2.2 channels with NOP receptors in DRG neurons (Beedle et al. 2004), as well as with MOR and DOR expressed with recombinant Cav2.2 channels in tsA-201 cells (Evans et al. 2010; Chee et al. 2008) (Fig. 2c, d). At least in the case of NOP receptors, this interaction is direct and occurs through the binding of the receptor with the carboxy-terminal region of the channel. The formation of GPCR-channel signaling complexes appears to serve several functions. First, it allows for a better functional coupling of the channel with the receptor (Bünemann et al. 2003). Indeed, Gβγ-dependent inhibition of the channel does not require a diffusible second messenger therefore indicating that the channel should be in close proximity with the receptor in order for the regulation to occur. Second, the GPCR-channel interaction serves as a means of control of the channel density in the plasma membrane (Fig. 2c, d). This aspect has been demonstrated for Cav2.2-NOP complexes where activation of the receptor produces an agonist-dependent internalization of the protein complex, providing an additional level of control over the Ca2+ influx (Altier et al. 2006; Evans et al. 2010). Because this type of regulation involves the removal of channels from the plasma membrane it cannot be overcome by membrane depolarizations. However, despite the notion that Cav2.2 channels interact with MOR, they are not co-internalized in response to receptor agonist unless NOP receptors are also present, suggesting that biochemical coupling of the channel with the receptor may not be sufficient to mediate agonist-dependent internalization of the channel (Evans et al. 2010). In addition to Gβγ-induced modulation, an additional Gα-mediated inhibition that relies on pp60c-src tyrosine kinase (Fig. 2e) has also been described (Raingo et al. 2007). This inhibition is insensitive to membrane depolarizations and is thus considered voltage-independent. Ergo, Cav2.2 channels undergo direct opioid receptor family-mediated voltage-dependent modulation by Gβγ, as well as multiple forms of voltage-independent regulation by these receptors.
Role of Alternative Splicing in OR-Dependent Regulation of Cav2 Channels
There are important differences in the ability of Cav2 channel variants to respond to G-protein regulation. For instance, alternative splicing of exon 37 of Cav2.2 channels produces two channel variants (exon 37a and exon 37b) that differ in their C-terminal region. Expression of exon 37a-containing channels is restricted to the dorsal root ganglia, preferentially in nociceptive neurons, while expression of exon 37b-containing channels is widely found throughout the nervous system (Bell et al. 2004). Although Gβγ-induced voltage-dependent inhibition is virtually identical for both channel variants, activation of tyrosine kinase inhibits channels containing exon 37a but not exon 37b (Raingo et al. 2007) (Fig. 2e), and this has been shown to enhance morphine-induced analgesia in rodents (Andrade et al. 2010). Cav2.1 channel variants may also differ in their responsiveness to G-protein regulation. For instance, a mutation (R192Q) in Cav2.1 associated with type-1 familial hemiplegic migraine (FHM-1) has been shown to hinder MOR agonist-induced voltage-dependent inhibition of the channel (Weiss et al. 2008; Melliti et al. 2003). Although the underlying mechanism by which this mutation alters G-protein regulation is not fully established, it was proposed that it may rely on its effect on the gating properties of the channel, especially on its voltage-dependent inactivation that appears to play an important role in the inhibition mediated by Gβγ (Weiss et al. 2007). In addition to splicing of the channel, a recent study reported that alternative splicing of the C-terminal region of MORs alters their ability to modulate Cav2.2 channels (Gandini et al. 2019). Notably, coexpression of MOR1 and MOR1C variants, with exon 37a-containing Cav2.2 channels produced a potent agonist-independent inhibition of the calcium current, a regulation that required Src tyrosine kinase. In contrast, this regulation was not observed when the channel was coexpressed with MOR1O, a short MOR C-terminal splice variant. Furthermore, none of the MOR variants were able to produce agonist-independent inhibition of exon 37b-containing Cav2.2 channels. This highlights the notion that not only splicing of Cav2.2 modulates the ability of the channel to undergo G-protein regulation, but also splicing of the receptor dictates the multiple facets of this regulation.
Harnessing OR Modulation of N-Type Calcium Channels as Pain Therapeutics
Opioid receptors can be targeted in a range of neurological conditions such as depression and anxiety (Crowley et al. 2016; Peciña et al. 2019) and this may involve modulation of a range of molecular targets in the CNS. On the other hand, a clear link has been established between opioid receptor agonists and actions on Cav2.2 channels in the context of pain relief. Cav2.2 calcium channels are prominently expressed in afferent sensory fiber nerve terminals in the spinal cord, where they control the release of neurotransmitters such as substance P and glutamate (for review see (Bourinet et al. 2014)). As discussed above, OR activation inhibits Cav2.2 channel activity, thus reducing the transmission of afferent pain signals (Heinke et al. 2011; Kondo et al. 2005; Beaudry et al. 2011). Opioids also contribute to analgesia at the level of higher brain centers (Diaz et al. 1995; Goodchild et al. 2004), where a functional link to Cav2.2 channels has, however, not been clearly established. Although agonists of all types of OR have been shown to produce analgesia in preclinical models (King et al. 1997; Darland et al. 1998; Field et al. 1999; Courteix et al. 2004; Nozaki et al. 2012; Beck and Dix 2019; Conibear et al. 2020), clinically used opioid analgesics have so far predominantly been targeted towards the MOR subtype. While effective analgesics, MOR agonists such as morphine suffer from adverse effects, such as addiction, the development of tolerance, constipation, itch and respiratory depression. Novel compounds such as oliceridine/TRV130 are biased MOR ligands that prevent arrestin recruitment to the receptor, and show an improved therapeutic window compared to morphine and efficacy in conditions of moderate to severe pain (Schmid et al. 2017). There are no clinically approved DOR agonists for the treatment of pain, and to our knowledge only one clinically used analgesic that targets KOR (i.e., pentazocine, (Gear et al. 1996)). This is mostly due to CNS side effects such as sedation, dysphoria, and motor problems. However, bivalent agonists that use a linker molecule to combine oxymorphone (a MOR agonist) and naltrindole (a DOR antagonist) have been developed, and have been shown to result in reduced development of tolerance and reduced reward seeking in preclinical models of pain (Daniels et al. 2005; Lenard et al. 2007). In addition, efforts have been made to selectively target peripheral KOR (Beck and Dix 2019). One such compound (JT09) is highly efficacious as an analgesic without the development of CNS effects.
So far, there are also no clinically approved analgesics that target the NOP receptor. In rodents, supraspinal effects of nociceptin have been reported to be hypernociceptive, whereas they produce analgesia at the spinal level. In contrast, a number of NOP receptor agonists have been shown to have analgesic effects in non-human primates even when delivered systemically [for review see (Lin and Ko 2013)]. Compared with opioids, these agonists do not appear to suffer from the development of itch, sedation, dependence or constipation. The dual targeted MOR/NOP agonist Cebranopadol (Linz et al. 2014) has successfully completed phase II clinical trials for chronic low back pain [oral delivery; (Christoph et al. 2017)]. This compound has also shown efficacy in a phase II trial against cancer pain (Koch et al. 2019). AT121 is also a MOR/NOP dual ligand that has been shown to mediate analgesia in non-human primates (Ding et al. 2018). Although the in vivo pharmacological activity of these various OR targeting compounds would fit with an inhibitory action on Cav2.2 channels expressed in the afferent pain pathway, there is to date no unequivocal evidence that these channels are the most critical downstream effector of OR family agonists. While alternative splicing of Cav2.2 modulates the analgesic effects of morphine in rodents (Jiang et al. 2013; Andrade et al. 2010), we are not aware of studies that have examined the effect of opioid agonists such as morphine in Cav2.2 null mice. Instead, it is important to note that ORs act on other molecular targets that are expressed in the afferent pain pathway, such as G-protein coupled inwardly rectifying potassium (GIRK) channels (Ikeda et al. 2002; Marker et al. 2004, 2005) and TREK 1 channels (Devilliers et al. 2013). That said, a contribution of Cav2.2 inhibition to the analgesic effects of clinically used and preclinically developed OR agonists is consistent with the notion that direct inhibition of these channel by selective peptide-based blockers mediates pain relief in both animals and humans [see (Zamponi et al. 2015)].
Concluding Remarks
Since the pioneering work by Dunlap and Fischbach in the late 1970s reporting the first evidence that voltage-gated calcium channels are regulated by G-protein coupled receptors (Dunlap and Fischbach 1978, 1981), tremendous progress in the understanding of basic processes and molecular interactions that govern the regulation have been made. This has led not only to a greater understanding of their mechanisms of action and physiological importance, but also to the development of novel pharmacopeia. Much work remains to be done to further clarify the role of OR heterodimerization, their trafficking to and from the plasma membrane with regard to the calcium channels, and to explore the extent and diversity of channel and receptor splice variants and their respective functional relationship. Nonetheless, all these aspects offer a tremendous opportunity for selective pharmacological manipulation with the potential to provide new generations therapeutics devoid of the usual side effects associated with classical opioid agonists.
Abbreviations
- VGCC
Voltage-gated calcium channel
- OR
Opioid receptor
- MOR
Mu opioid receptor
- DOR
Delta opioid receptor
- KOR
Kappa opioid receptor
- NOP
Nociceptin receptor
Author Contributions
NW and GWZ reviewed the literature and wrote the manuscript.
Funding
NW is supported by the Institute of Organic Chemistry and Biochemistry. GWZ is supported by a grant from the Canadian Institutes for Health Research and holds a Canada Research Chair.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Agler HL, Evans J, Tay LH, Anderson MJ, Colecraft HM, Yue DT (2005) G protein-gated inhibitory module of N-type (ca(v)2.2) ca2+ channels. Neuron 46:891–904 [DOI] [PubMed] [Google Scholar]
- Altier C, Khosravani H, Evans RM, Hameed S, Peloquin JB, Vartian BA, Chen L, Beedle AM, Ferguson SS, Mezghrani A, Dubel SJ, Bourinet E, McRory JE, Zamponi GW (2006) ORL1 receptor-mediated internalization of N-type calcium channels. Nat Neurosci 9:31–40 [DOI] [PubMed] [Google Scholar]
- Andrade A, Denome S, Jiang YQ, Marangoudakis S, Lipscombe D (2010) Opioid inhibition of N-type Ca2+ channels and spinal analgesia couple to alternative splicing. Nat Neurosci 13:1249–1256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bean BP (1989) Neurotransmitter inhibition of neuronal calcium currents by changes in channel voltage dependence. Nature 340:153–156 [DOI] [PubMed] [Google Scholar]
- Beaudry H, Dubois D, Gendron L (2011) Activation of spinal mu- and delta-opioid receptors potently inhibits substance P release induced by peripheral noxious stimuli. J Neurosci 31:13068–13077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck TC, Dix TA (2019) Targeting peripheral ϰ-opioid receptors for the non-addictive treatment of pain. Future Drug Discov 1:FDD17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckett A-H, Casy AF (1954) Synthetic analgesics: stereochemical considerations. J Pharm Pharmacol 6:986–1001 [DOI] [PubMed] [Google Scholar]
- Beedle AM, McRory JE, Poirot O, Doering CJ, Altier C, Barrere C, Hamid J, Nargeot J, Bourinet E, Zamponi GW (2004) Agonist-independent modulation of N-type calcium channels by ORL1 receptors. Nat Neurosci 7:118–125 [DOI] [PubMed] [Google Scholar]
- Bell TJ, Thaler C, Castiglioni AJ, Helton TD, Lipscombe D (2004) Cell-specific alternative splicing increases calcium channel current density in the pain pathway. Neuron 41:127–138 [DOI] [PubMed] [Google Scholar]
- Berecki G, Motin L, Adams DJ (2016) Voltage-gated R-type calcium channel inhibition via human μ-, δ-, and κ-opioid receptors is voltage-independently mediated by Gβγ protein subunits. Mol Pharmacol 89:187–196 [DOI] [PubMed] [Google Scholar]
- Berridge MJ, Bootman MD, Roderick HL (2003) Calcium signalling: dynamics, homeostasis and remodelling. Nat Rev Mol Cell Biol 4:517–529 [DOI] [PubMed] [Google Scholar]
- Besse D, Lombard MC, Zajac JM, Roques BP, Besson JM (1990) Pre-and postsynaptic distribution of μ, δ and κ opioid receptors in the superficial layers of the cervical dorsal horn of the rat spinal cord. Brain Res 521:15–22 [DOI] [PubMed] [Google Scholar]
- Black JL (2003) The voltage-gated calcium channel gamma subunits: a review of the literature. J Bioenerg Biomembr 35:649–660 [DOI] [PubMed] [Google Scholar]
- Bourinet E, Altier C, Hildebrand ME, Trang T, Salter MW, Zamponi GW (2014) Calcium-permeable ion channels in pain signaling. Physiol Rev 94:81–140 [DOI] [PubMed] [Google Scholar]
- Bourinet E, Soong TW, Stea A, Snutch TP (1996) Determinants of the G protein-dependent opioid modulation of neuronal calcium channels. Proc Natl Acad Sci USA 93:1486–1491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody DL, Patil PG, Mulle JG, Snutch TP, Yue DT (1997) Bursts of action potential waveforms relieve G-protein inhibition of recombinant P/Q-type Ca2+ channels in HEK 293 cells. J Physiol 499:637–644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bünemann M, Frank M, Lohse MJ (2003) Gi protein activation in intact cells involves subunit rearrangement rather than dissociation. Proc Natl Acad Sci USA 100:16077–16082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunzow JR, Saez C, Mortrud M, Bouvier C, Williams JT, Low M, Grandy DK (1994) Molecular cloning and tissue distribution of a putative member of the rat opioid receptor gene family that is not a μ, δ or κ opioid receptor type. FEBS Lett 347:284–288 [DOI] [PubMed] [Google Scholar]
- Buraei Z, Yang J (2010) The ß subunit of voltage-gated Ca2+ channels. Physiol Rev 90:1461–1506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campiglio M, Flucher BE (2015) The role of auxiliary subunits for the functional diversity of voltage-gated calcium channels. J Cell Physiol 230:2019–2031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carabelli V, Carra I, Carbone E (1998) Localized secretion of ATP and opioids revealed through single Ca2+ channel modulation in bovine chromaffin cells. Neuron 20:1255–1268 [DOI] [PubMed] [Google Scholar]
- Catterall WA (2011) Voltage-gated calcium channels. Cold Spring Harb Perspect Biol 3:a003947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chee MJ, Mörl K, Lindner D, Merten N, Zamponi GW, Light PE, Beck-Sickinger AG, Colmers WF (2008) The third intracellular loop stabilizes the inactive state of the neuropeptide Y1 receptor. J Biol Chem 283:33337–33346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christoph A, Eerdekens MH, Kok M, Volkers G, Freynhagen R (2017) Cebranopadol, a novel first-in-class analgesic drug candidate: first experience in patients with chronic low back pain in a randomized clinical trial. Pain 158:1813–1824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conibear AE, Asghar J, Hill R, Henderson G, Borbely E, Tekus V, Helyes Z, Palandri J, Bailey C, Starke I, von Mentzer B, Kendall D, Kelly E (2020) A novel G protein-biased agonist at the δ opioid receptor with analgesic efficacy in models of chronic pain. J Pharmacol Exp Ther 372:224–236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courteix C, Coudoré-Civiale MA, Privat AM, Pélissier T, Eschalier A, Fialip J (2004) Evidence for an exclusive antinociceptive effect of nociceptin/orphanin FQ, an endogenous ligand for the ORL1 receptor, in two animal models of neuropathic pain. Pain 110:236–245 [DOI] [PubMed] [Google Scholar]
- Crowley NA, Bloodgood DW, Hardaway JA, Kendra AM, McCall JG, Al-Hasani R, McCall NM, Yu W, Schools ZL, Krashes MJ, Lowell BB, Whistler JL, Bruchas MR, Kash TL (2016) Dynorphin controls the gain of an amygdalar anxiety circuit. Cell Rep 14:2774–2783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniels DJ, Lenard NR, Etienne CL, Law PY, Roerig SC, Portoghese PS (2005) Opioid-induced tolerance and dependence in mice is modulated by the distance between pharmacophores in a bivalent ligand series. Proc Natl Acad Sci USA 102:19208–19213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darland T, Heinricher MM, Grandy DK (1998) Orphanin FQ/nociceptin: a role in pain and analgesia, but so much more. Trends Neurosci 21:215–221 [DOI] [PubMed] [Google Scholar]
- De Waard M, Liu H, Walker D, Scott VE, Gurnett CA, Campbell KP (1997) Direct binding of G-protein betagamma complex to voltage-dependent calcium channels. Nature 385:446–450 [DOI] [PubMed] [Google Scholar]
- Devilliers M, Busserolles J, Lolignier S, Deval E, Pereira V, Alloui A, Christin M, Mazet B, Delmas P, Noel J, Lazdunski M, Eschalier A (2013) Activation of TREK-1 by morphine results in analgesia without adverse side effects. Nat Commun 4:2941 [DOI] [PubMed] [Google Scholar]
- Diaz A, Ruiz F, Florez J, Hurle MA, Pazos A (1995) Mu-opioidreceptor regulation during opioid tolerance and supersensitivity inrat central nervous system. J Pharmacol Exp Ther 274:1545–1551 [PubMed] [Google Scholar]
- Ding H, Kiguchi N, Yasuda D, Daga PR, Polgar WE, Lu JJ, Czoty PW, Kishioka S, Zaveri NT, Ko MC (2018) A bifunctional nociceptin and mu opioid receptor agonist is analgesic without opioid side effects in nonhuman primates. Sci Transl Med 10:eaar3483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolphin AC (2018a) Voltage-gated calcium channel α 2δ subunits: an assessment of proposed novel roles. F1000 Res 7:1830. 10.12688/f1000research.16104.1 [DOI] [PMC free article] [PubMed]
- Dolphin AC (2018b) Voltage-gated calcium channels: their discovery, function and importance as drug targets. Brain Neurosci Adv 2:1–8. 10.1177/2398212818794805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlap K, Fischbach GD (1978) Neurotransmitters decrease the calcium ocmponent of sensory neurone action potentials. Nature 276:837–839 [DOI] [PubMed] [Google Scholar]
- Dunlap K, Fischbach GD (1981) Neurotransmitters decrease the calcium conductance activated by depolarization of embryonic chick sensory neurones. J Physiol 317:519–535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans CJ, Keith DE, Morrison H, Magendzo K, Edwards RH (1992) Cloning of a delta opioid receptor by functional expression. Science 258:1952–1955 [DOI] [PubMed] [Google Scholar]
- Evans RM, You H, Hameed S, Altier C, Mezghrani A, Bourinet E, Zamponi GW (2010) Heterodimerization of ORL1 and opioid receptors and its consequences for N-type calcium channel regulation. J Biol Chem 285:1032–1040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field MJ, Carnell AJ, Gonzalez MI, McCleary S, Oles RJ, Smith R, Hughes J, Singh L (1999) Enadoline, a selective kappa-opioid receptor agonist shows potent antihyperalgesic and antiallodynic actions in a rat model of surgical pain. Pain 80:383–389 [DOI] [PubMed] [Google Scholar]
- Fujita W, Gomes I, Devi LA (2014) Revolution in GPCR signalling: opioid receptor heteromers as novel therapeutic targets: IUPHAR review 10. Br J Pharmacol 171:4155–4176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandini MA, Souza IA, Raval D, Xu J, Pan YX, Zamponi GW (2019) Differential regulation of Cav2.2 channel exon 37 variants by alternatively spliced μ-opioid receptors. Mol Brain 12:98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gear RW, Gordon NC, Heller PH, Paul S, Miaskowski C, Levine JD (1996) Gender difference in analgesic response to the kappa-opioid pentazocine. Neurosci Lett 205:207–209 [DOI] [PubMed] [Google Scholar]
- Goodchild CS, Nadeson R, Cohen, E (2004) Supraspinal and spinal cord opioid receptors are responsible for antinociception following intrathecal morphine injections. Eur J Anaesthesiol 21(3):179–185 [DOI] [PubMed] [Google Scholar]
- Hawkins KN, Knapp RJ, Gehlert DR, Lui GK, Yamamura MS, Roeske LC, Hruby VJ, Yamamura HI (1988) Quantitative autoradiography of [3H] CTOP binding to mu opioid receptors in rat brain. Life Sci 42:2541–2551 [DOI] [PubMed] [Google Scholar]
- Heinke B, Gingl E, Sandkühler J (2011) Multiple targets of μ-opioid receptor-mediated presynaptic inhibition at primary afferent Aδ- and C-fibers. J Neurosci 31:1313–1322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herlitze S, Garcia DE, Mackie K, Hille B, Scheuer T, Catterall WA (1996) Modulation of Ca2+ channels by G-protein beta gamma subunits. Nature 380:258–262 [DOI] [PubMed] [Google Scholar]
- Herlitze S, Hockerman GH, Scheuer T, Catterall WA (1997) Molecular determinants of inactivation and G protein modulation in the intracellular loop connecting domains I and II of the calcium channel alpha1A subunit. Proc Natl Acad Sci USA 94:1512–1516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hümmer A, Delzeith O, Gomez SR, Moreno RL, Mark MD, Herlitze S (2003) Competitive and synergistic interactions of G protein beta(2) and Ca(2+) channel beta(1b) subunits with Ca(v)2.1 channels, revealed by mammalian two-hybrid and fluorescence resonance energy transfer measurements. J Biol Chem 278:49386–49400 [DOI] [PubMed] [Google Scholar]
- Ikeda K, Kobayashi T, Kumanishi T, Yano R, Sora I, Niki H (2002) Molecular mechanisms of analgesia induced by opioids and ethanol: is the GIRK channel one of the keys. Neurosci Res 44:121–131 [DOI] [PubMed] [Google Scholar]
- Ikeda SR (1991) Double-pulse calcium channel current facilitation in adult rat sympathetic neurones. J Physiol 439:181–214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang YQ, Andrade A, Lipscombe D (2013) Spinal morphine but not ziconotide or gabapentin analgesia is affected by alternative splicing of voltage-gated calcium channel CaV2.2 pre-mRNA. Mol Pain 9:67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones LP, Patil PG, Snutch TP, Yue DT (1997) G-protein modulation of N-type calcium channel gating current in human embryonic kidney cells (HEK 293). J Physiol 498:601–610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang MG, Campbell KP (2003) Gamma subunit of voltage-activated calcium channels. J Biol Chem 278:21315–21318 [DOI] [PubMed] [Google Scholar]
- Kieffer BL (1995) Recent advances in molecular recognition and signal transduction of active peptides: receptors for opioid peptides. Cell Mol Neurobiol 15:615–635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kieffer BL, Befort K, Gaveriaux-Ruff C, HiRTH CHRISTIANG (1992) The delta-opioid receptor: isolation of a cDNA by expression cloning and pharmacological characterization. Proc Natl Acad Sci 89:12048–12052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King MA, Rossi GC, Chang AH, Williams L, Pasternak GW (1997) Spinal analgesic activity of orphanin FQ/nociceptin and its fragments. Neurosci Lett 223:113–116 [DOI] [PubMed] [Google Scholar]
- Kitchen I, Slowe SJ, Matthes HWD, Kieffer B (1997) Quantitative autoradiographic mapping of μ-, δ-and κ-opioid receptors in knockout mice lacking the μ-opioid receptor gene. Brain Res 778:73–88 [DOI] [PubMed] [Google Scholar]
- Koch ED, Kapanadze S, Eerdekens MH, Kralidis G, Létal J, Sabatschus I, Ahmedzai SH (2019) Cebranopadol, a novel first-in-class analgesic drug candidate: first experience with cancer-related pain for up to 26 weeks. J Pain Symptom Manage 58:390–399 [DOI] [PubMed] [Google Scholar]
- Kondo I, Marvizon JC, Song B, Salgado F, Codeluppi S, Hua XY, Yaksh TL (2005) Inhibition by spinal mu- and delta-opioid agonists of afferent-evoked substance P release. J Neurosci 25:3651–3660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo CC, Bean BP (1993) G-protein modulation of ion permeation through N-type calcium channels. Nature 365:258–262 [DOI] [PubMed] [Google Scholar]
- Lenard NR, Daniels DJ, Portoghese PS, Roerig SC (2007) Absence of conditioned place preference or reinstatement with bivalent ligands containing mu-opioid receptor agonist and delta-opioid receptor antagonist pharmacophores. Eur J Pharmacol 566:75–82 [DOI] [PubMed] [Google Scholar]
- Lin AP, Ko MC (2013) The therapeutic potential of nociceptin/orphanin FQ receptor agonists as analgesics without abuse liability. ACS Chem Neurosci 4:214–224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linz K, Christoph T, Tzschentke TM, Koch T, Schiene K, Gautrois M, Schröder W, Kögel BY, Beier H, Englberger W, Schunk S, De Vry J, Jahnel U, Frosch S (2014) Cebranopadol: a novel potent analgesic nociceptin/orphanin FQ peptide and opioid receptor agonist. J Pharmacol Exp Ther 349:535–548 [DOI] [PubMed] [Google Scholar]
- Lord JAH, Waterfield AA, Hughes J, Kosterlitz HW (1977) Endogenous opioid peptides: multiple agonists and receptors. Nature 267:495–499 [DOI] [PubMed] [Google Scholar]
- Majumdar S, Grinnell S, Le Rouzic V, Burgman M, Polikar L, Ansonoff M, Pintar J, Pan YX, Pasternak GW (2011) Truncated G protein-coupled mu opioid receptor MOR-1 splice variants are targets for highly potent opioid analgesics lacking side effects. Proc Natl Acad Sci USA 108:19778–19783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansour A, Khachaturian H, Lewis ME, Akil HUDA, Watson SJ (1987) Autoradiographic differentiation of mu, delta, and kappa opioid receptors in the rat forebrain and midbrain. J Neurosci 7:2445–2464 [PMC free article] [PubMed] [Google Scholar]
- Marker CL, Luján R, Loh HH, Wickman K (2005) Spinal G-protein-gated potassium channels contribute in a dose-dependent manner to the analgesic effect of mu- and delta- but not kappa-opioids. J Neurosci 25:3551–3559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marker CL, Stoffel M, Wickman K (2004) Spinal G-protein-gated K+ channels formed by GIRK1 and GIRK2 subunits modulate thermal nociception and contribute to morphine analgesia. J Neurosci 24:2806–2812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melliti K, Grabner M, Seabrook GR (2003) The familial hemiplegic migraine mutation R192Q reduces G-protein-mediated inhibition of P/Q-type (Ca(V)2.1) calcium channels expressed in human embryonic kidney cells. J Physiol 546:337–347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meunier J-C, Mollereau C, Toll L, Suaudeau C, Moisand C, Alvinerie P, Butour J-L, Guillemot J-C, Ferrara P, Monsarrat B (1995) Isolation and structure of the endogenous agonist of opioid receptor-like ORL 1 receptor. Nature 377:532–535 [DOI] [PubMed] [Google Scholar]
- Mollereau C, Parmentier M, Mailleux P, Butour J-L, Moisand C, Chalon P, Caput D, Vassart G, Meunier J-C (1994) ORL1, a novel member of the opioid receptor family: cloning, functional expression and localization. FEBS Lett 341:33–38 [DOI] [PubMed] [Google Scholar]
- Morikawa H, Mima H, Uga H, Shoda T, Fukuda K (1999) Opioid potentiation of N-type Ca2+ channel currents via pertussis-toxin-sensitive G proteins in NG108-15 cells. Pflugers Arch 438:423–426 [DOI] [PubMed] [Google Scholar]
- Neal CR Jr, Mansour A, Reinscheid R, Nothacker H, Civelli O, Akil H, Watson SJ Jr (1999) Opioid receptor-like (ORL1) receptor distribution in the rat central nervous system: comparison of ORL1 receptor mRNA expression with 125I-[14Tyr]-orphanin FQ binding. J Comp Neurol 412:563–605 [PubMed] [Google Scholar]
- Nozaki C, Le Bourdonnec B, Reiss D, Windh RT, Little PJ, Dolle RE, Kieffer BL, Gavériaux-Ruff C (2012) δ-Opioid mechanisms for ADL5747 and ADL5859 effects in mice: analgesia, locomotion, and receptor internalization. J Pharmacol Exp Ther 342:799–807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan YX, Bolan E, Pasternak GW (2002) Dimerization of morphine and orphanin FQ/nociceptin receptors: generation of a novel opioid receptor subtype. Biochem Biophys Res Commun 297:659–663 [DOI] [PubMed] [Google Scholar]
- Patil PG, de Leon M, Reed RR, Dubel S, Snutch TP, Yue DT (1996) Elementary events underlying voltage-dependent G-protein inhibition of N-type calcium channels. Biophys J 71:2509–2521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peciña M, Karp JF, Mathew S, Todtenkopf MS, Ehrich EW, Zubieta JK (2019) Endogenous opioid system dysregulation in depression: implications for new therapeutic approaches. Mol Psychiatry 24:576–587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Portoghese PS (1965) A new concept on the mode of interaction of narcotic analgesics with receptors. J Med Chem 8:609–616 [DOI] [PubMed] [Google Scholar]
- Raingo J, Castiglioni AJ, Lipscombe D (2007) Alternative splicing controls G protein-dependent inhibition of N-type calcium channels in nociceptors. Nat Neurosci 10:285–292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandoz G, Lopez-Gonzalez I, Grunwald D, Bichet D, Altafaj X, Weiss N, Ronjat M, Dupuis A, De Waard M (2004) Cavbeta-subunit displacement is a key step to induce the reluctant state of P/Q calcium channels by direct G protein regulation. Proc Natl Acad Sci USA 101:6267–6272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmid CL, Kennedy NM, Ross NC, Lovell KM, Yue Z, Morgenweck J, Cameron MD, Bannister TD, Bohn LM (2017) Bias factor and therapeutic window correlate to predict safer opioid analgesics. Cell 171:1165–1175.e13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroeder JE, Fischbach PS, Zheng D, McCleskey EW (1991) Activation of mu opioid receptors inhibits transient high- and low-threshold Ca2+ currents, but spares a sustained current. Neuron 6:13–20 [DOI] [PubMed] [Google Scholar]
- Simms BA, Zamponi GW (2014) Neuronal voltage-gated calcium channels: structure, function, and dysfunction. Neuron 82:24–45 [DOI] [PubMed] [Google Scholar]
- Toth PT, Shekter LR, Ma GH, Philipson LH, Miller RJ (1996) Selective G-protein regulation of neuronal calcium channels. J Neurosci 16:4617–4624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsunoo A, Yoshii M, Narahashi T (1986) Block of calcium channels by enkephalin and somatostatin in neuroblastoma-glioma hybrid NG108-15 cells. Proc Natl Acad Sci USA 83:9832–9836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss N, Sandoval A, Felix R, Van den Maagdenberg A, De Waard M (2008) The S218L familial hemiplegic migraine mutation promotes deinhibition of Ca(v)2.1 calcium channels during direct G-protein regulation. Pflugers Arch 457:315–326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss N, Tadmouri A, Mikati M, Ronjat M, De Waard M (2007) Importance of voltage-dependent inactivation in N-type calcium channel regulation by G-proteins. Pflugers Arch 454:115–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wettschureck N, Offermanns S (2005) Mammalian G proteins and their cell type specific functions. Physiol Rev 85:1159–1204 [DOI] [PubMed] [Google Scholar]
- Wu J, Yan Z, Li Z, Qian X, Lu S, Dong M, Zhou Q, Yan N (2016) Structure of the voltage-gated calcium channel Ca(v)1.1 at 3.6 Å resolution. Nature 537:191–196 [DOI] [PubMed] [Google Scholar]
- Wu J, Yan Z, Li Z, Yan C, Lu S, Dong M, Yan N (2015) Structure of the voltage-gated calcium channel Cav11 complex. Science 350:aad2395 [DOI] [PubMed] [Google Scholar]
- Zamponi GW, Bourinet E, Nelson D, Nargeot J, Snutch TP (1997) Crosstalk between G proteins and protein kinase C mediated by the calcium channel alpha1 subunit. Nature 385:442–446 [DOI] [PubMed] [Google Scholar]
- Zamponi GW, Striessnig J, Koschak A, Dolphin AC (2015) The physiology, pathology, and pharmacology of voltage-gated calcium channels and their future therapeutic potential. Pharmacol Rev 67:821–870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y, Huang G, Wu Q, Wu K, Li R, Lei J, Pan X, Yan N (2019) Cryo-EM structures of apo and antagonist-bound human Cav3.1. Nature 576:492–497 [DOI] [PubMed] [Google Scholar]