Abstract
Objective:
This study aimed to evaluate the effectiveness and feasibility of the posterior-only approach for debridement, interbody fusion, and internal fixation in treating upper thoracic tuberculosis.
Methods:
This study retrospectively analysed the clinical and radiographic data of 8 patients diagnosed with upper thoracic tuberculosis. All patients underwent posterior approach debridement, interbody fusion, and internal fixation. We conducted pre- and postoperative assessments of the visual analog scale (VAS), Oswestry disability index (ODI) scores, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), ASIA score, and kyphotic Cobb angle.
Results:
Back pain and lower limb weakness were the most common presenting symptoms. The mean duration of surgery, amount of blood loss, and volume of postoperative drainage were 262.5 ± 43.3 min, 625.0 ± 333.8 mL, and 285.0 ± 118.1 mL, respectively. Patients were followed up for 36 to 48 months. Three months after surgery, there was a significant improvement in VAS and ODI scores, which further improved until the final follow-up. A statistically significant difference was observed between the preoperative and postoperative periods (P < .05). At the final follow-up, lower extremity function had fully returned to normal in all 5 paralyzed patients. The ESR and CRP returned to normal, 18.1 ± 7.3 mm/h and 9.95 ± 5.41 mg/L, respectively, within 3 months postoperatively. There were statistical differences between the preoperative and postoperative periods (P < .05). The average kyphotic correction rate was (71.5 ± 7.3)%, and the average loss of correction angle was (3.5 ± 1.4)°. Intervertebral bone fusion was achieved by all patients within 15 months (mean 8.3 ± 3.2 months) postoperatively.
Conclusion:
The posterior-only approach seems an effective, safe, and reliable treatment method for upper thoracic tuberculosis, with favourable clinical and radiological outcomes.
Level of Evidence:
Level IV, Therapeutic study.
Keywords: Upper thoracic tuberculosis, Spinal tuberculosis, Posterior only approach, Posterior debridement
Highlights
Upper thoracic tuberculosis is a rare disease under-reported in the literature.
The posterior approach is an effective method for completely decompressing the spinal cord, correcting kyphosis, and facilitating the recovery of spinal cord function.
The posterior-only approach is a straightforward, safe, reliable, and efficient treatment option for upper thoracic tuberculosis.
Introduction
Spinal tuberculosis accounts for 50% of all cases of osteoarticular tuberculosis.1 The thoracic spine is the most common site of spinal tuberculosis, making it more vulnerable to severe physical damage, including vertebral collapse, kyphosis, and paralysis.2-4 Nonetheless, despite the severity of upper thoracic tuberculosis (T1-T4), responsible for only 5.9% of all spinal tuberculosis cases,2 there are limited reports detailing its diagnosis and treatment.
Surgical intervention during concomitant pharmaceutical treatment for spinal tuberculosis is necessary when there are pronounced neurological deficits, marked deformities (kyphosis), and significant instability.5,6 The surgical approach for spinal tuberculosis is a long-standing issue of controversy.7-9 Since spinal tuberculosis primarily affects the anterior column of the vertebra, the anterior surgical approach offers a direct path to the diseased vertebral body lesions, allowing for a more extensive surgical field and providing convenience in debridement and reconstructing anterior column defects.10,11 Anterior approach debridement is a preferred technique among some scholars for treating upper thoracic tuberculosis because of its numerous advantages.11-13
The anterior approach to the upper thoracic spine is particularly challenging due to the sternum, clavicle, ribs, and mediastinal organs. Accessing the upper thoracic tuberculous area through the anterior approach poses an additional challenge as thoracotomy to reach the upper thoracic vertebrae is complicated by the complex anatomy that hinders the approach.14 Additionally, reconstruction of the surgical area and deformity correction through the anterior approach is challenging, especially when dealing with moderate or severe kyphosis.15 The posterior approach has a better corrective effect on kyphotic deformity than the anterior approach.8 Furthermore, according to some scholars, anterior debridement may be unnecessary in treating tuberculous spondylitis.16 Therefore, we prefer the posterior approach for upper thoracic tuberculosis, and we performed debridement, bone grafting, and internal fixation in 1 stage. This study summarizes our experience managing and following up on 8 patients with upper thoracic tuberculosis. It discusses the feasibility and effectiveness of posterior-only approach debridement, intervertebral fusion, and internal fixation for treating upper thoracic tuberculosis.
Material and Methods
General materials
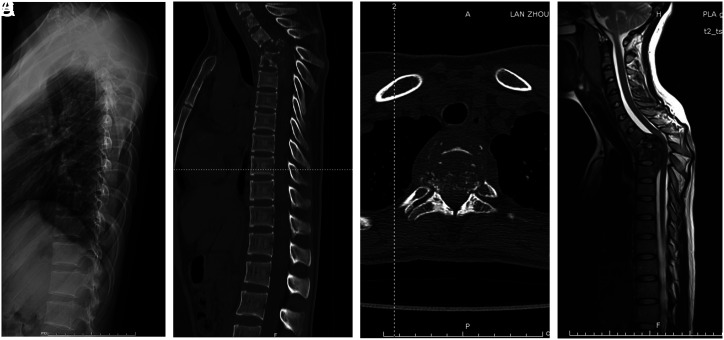
A retrospective analysis was conducted on the clinical and imaging data of 13 consecutive patients with upper thoracic tuberculosis admitted between January 2013 and November 2019. However, only 8 patients were followed up for over 2 years and had complete medical records. Approval for this study was granted by the The 940th Hospital of Joint Logistics Support Force of Chinese PLA of the authors’ affiliated institutions (approval number: 2020KYLL002). Informed consent was obtained from the patients who agreed to take part in the study. All patients underwent serological tests, which included erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and T-SPOT, as well as imaging examinations, such as plain radiographs, computed tomography (CT), and magnetic resonance imaging (MRI) after admission. These tests are shown in Figure 1. The clinical diagnosis of upper thoracic tuberculosis was based on the clinical-radiographic-hematologic correlation commonly used for diagnosing tuberculosis, and the postoperative pathological examination confirmed the diagnosis.
Figure 1.
(A) Preoperative lateral X-ray showed no obvious abnormality. (B) In preoperative CT, destructive segments are located at T2-5. The local kyphotic Cobb angle was 47°. (C) Axial CT showed that the vertebra was full of star-like bone destruction with lesions protruding into the spinal canal. (D) Preoperative MRI, the spinal cord was severely compressed by the abscess and sequestrum.
Preoperative management
Among the 8 patients, 6 were administered a course of anti-tuberculous drugs (including isoniazid at 300 mg/day, rifampicin at 450 mg/day, pyrazinamide at 750 mg/day, and ethambutol at 750 mg/day) for 3 to 4 weeks before surgery. Two patients underwent emergency spinal cord decompression due to neurological damage and did not receive anti-tuberculosis drug treatment before the operation. ESR and CRP levels were monitored to evaluate the effectiveness of the anti-tuberculosis treatment. Additionally, preoperative nutritional support was provided to address any anemia or hypoproteinemia present.
Surgical procedure
After administering general anesthesia, the patient was positioned prone, and a posterior approach was used to access the upper thoracic vertebra. A midline incision was made, and posterior elements, including lamina, facet joints, and transverse processes, were exposed. Under C-arm fluoroscopic guidance, the damaged vertebra was identified, and pedicle screws were inserted. Generally, we preferred longer segmental fixation, at least 2 levels superior and inferior to the level of decompression. Partial removal of the ribs and costotransverse articulations was included for lateral exposure. Costotransversectomy at the severe lesion segment was performed to drain the prevertebral abscess and expose diseased vertebral bodies. The intercostal nerve on the focal side was sacrificed if necessary. Various spatulas removed the lesions, including sequestrum, abscess, caseous material, and necrotic disc tissue, until the normal bleeding bone was exposed. In general, a partial resection of the damaged is performed. If there was any space-occupying lesion in the spinal canal, adequate decompression of the spinal canal was performed. The abscess was drained, and necrotic tissue was curetted as thoroughly as possible. The surgical field was washed with a large volume of normal saline until the rinsing fluid was clear. The kyphosis was corrected by installing permanent rods and exerting decompression at the middle anchoring point. The interbody defect was measured, and a suitable length of autologous iliac bone graft and rib bone graft or titanium mesh cages with autogenous bone grafts were taken to repair the interbody defect. The bone graft was immobilized with appropriate compression. After complete hemostasis, 500 mg of isoniazid and 1000 mg of streptomycin were injected into the operative area, and a drainage tube was inserted before suturing the incision. The material debrided was sent for histopathologic examination. A single surgeon performed the surgical procedure.
Postoperative management
The drainage tube remained in place for 48-96 hours and was removed when drainage volume decreased to <50 mL over 24 hours. Nutritional support was enhanced during the perioperative period, and physical therapy and rehabilitation training were implemented to prevent deep venous thrombosis and facilitate early recovery of nerve function. Postoperatively, conventional quadruple anti-tuberculosis therapy (isoniazid at 300 mg/day, rifampicin at 450 mg/day, pyrazinamide at 750 mg/day, and ethambutol at 750 mg/day) was continued for 3 months, followed by the continuation of triple anti-tuberculosis therapy (isoniazid 300 mg/day, rifampicin 450 mg/day, ethambutol 750 mg/day). The decision to discontinue pharmacotherapy was made according to the patient’s progress assessed in the follow-up. However, the treatment cycle with the use of anti-tuberculous drugs was at least 12 months.
Follow-up assessment
After being discharged, patients underwent monthly assessments to monitor their clinical response and neurological function, which included visual analog scale (VAS), Oswestry disability index (ODI) scores, ESR, CRP, and ASIA classification, as well as the early detection of complications such as drug-related side effects and disease reactivation. X-rays and CT scans were performed every 3-6 months to evaluate kyphosis correction and bony fusion. The kyphotic angle is formed by the upper and lower endplate lines of the upper and lower vertebrae with a maximum inclination of the kyphosis.17 The determination of bone graft fusion was based on the presence of continuous bony trabeculae formed between the graft and host bone. The criteria for spinal tuberculosis cure required:18,19 1) disappearance of all clinical symptoms and normal ESR levels following repeat laboratory testing, 2) CT evidence of bone graft fusion at the lesion site without paravertebral inflammation, and 3) no symptom recurrence for over 6 months after discontinuation of anti-tuberculosis drugs.
Statistical analysis
We conducted a paired-sample t-test to evaluate the differences in ESR, CRP, VAS, ODI scores, and Cobb’s angle between preoperative and 3-month postoperative, and 3-month postoperative and final follow-up values. Statistical significance was considered when P < .05. All statistical calculations were performed using SPSS version 20 (IBM SPSS Corp.; Armonk, NY, USA) for Windows.
Results
The study involved 8 patients, 5 of whom were female and 3 were male, with a mean age of 56.9 ± 12.7 years (range: 32-71 years) at presentation. All were monitored for an average of 42.3 ± 4.3 months (range: 36-48 months). The most frequent presenting symptom was pain, comprising thoracodorsal pain and intercostal neuralgia, while other common symptoms included lower limb weakness and fever. Clinical findings revealed that spinal tenderness and paralysis were most notable. Table 1 provides a detailed record of clinical presentation, physical examination, and neurological assessment. No patients exhibited pulmonary tuberculosis on chest radiographs, and histological examinations of sputum for acid-fast bacilli yielded negative results in all cases. Single-segment lesions were present in only 2 cases, whereas the remaining 6 had multi-vertebral lesions (Table 2).
Table 1.
Clinical presentation of the patients in our series
| Clinical symptoms and signs | No. of patients |
|---|---|
| Symptoms | |
| Thoracodorsal pain Intercostal neuralgia Subjective weakness of lower limbs Subjective loss of sensations Low-grade fever Other constitutional symptoms (night sweats, weight loss, and malaise) |
6 2 5 3 5 3 |
| Clinical signs | |
| Spinal tenderness Paralysis of lower limbs Pyramidal-tract involvement Discharging sinus Spinal deformity or gibbus |
6 5 2 0 3 |
Table 2.
Clinical data, perioperative outcomes, and complications
| Case no. | Age (y)/ gender | Segments | Operation time (minutes) | Blood loss (ml) | Postoperative drainage volume (ml) | Hospitalization (days) | Duration of follow-up (months) | Fusion time (months) | Complications | Relapse |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 66/F | T3-T4 | 240 | 500 | 300 | 27 | 40 | 6 | No | No |
| 2 | 32/F | T2-T5 | 330 | 1300 | 450 | 42 | 48 | 15 | Reoperation, Sinus | No |
| 3 | 53/M | T3-T5 | 290 | 600 | 400 | 14 | 47 | 6 | No | No |
| 4 | 68/M | T2-T3 | 250 | 350 | 150 | 24 | 42 | 6 | No | No |
| 5 | 48/F | T3 | 220 | 400 | 200 | 12 | 36 | 6 | No | No |
| 6 | 60/M | T2-T4 | 300 | 900 | 400 | 15 | 46 | 9 | Sinus | No |
| 7 | 57/M | T3-T4 | 270 | 650 | 200 | 15 | 40 | 8 | No | No |
| 8 | 71/M | T4 | 200 | 300 | 180 | 20 | 39 | 10 | No | No |
| Mean ± SD | 56.9 ± 12.7 | _ | 262.5 ± 43.3 | 625.0 ± 333.8 | 285.0 ± 118.1 | 21.1 ± 9.9 | 42.3 ± 4.3 | 8.3 ± 3.2 | _ | _ |
F, female; M, male.
Perioperative outcomes
On average, the operation time, blood loss, and postoperative drainage volume were 262.5±43.3 minutes (range: 200-330 minutes), 625.0 ± 333.8 mL (range: 300-1300 mL), and 285.0 ± 118.1 mL (range: 150-450 mL), respectively. A detailed summary of the patients’ perioperative outcomes is provided in Table 2.
Pain and functional recovery
All cases experienced a significant reduction in preoperative VAS and ODI scores at 3 months post operation, and further improvement was observed up until the final follow-up period, with a significant difference noted between preoperative and 3-month postoperative, and 3-month postoperative and final follow-up values (P < .05) (Table 3). Out of 8 cases, 5 patients (5/8) showed remarkable neurological recovery as indicated by their postoperative ASIA classification score despite having had lower limb paralysis before surgery. At the final follow-up, symptoms of tuberculosis were fully resolved.
Table 3.
VAS, ODI, ESR, CRP, and ASIA classification score
| Case no. | VAS | ODI | ESR (mm/h) | CRP (mg/L) | ASIA | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-op | 3 m post-op | Final follow-up | Pre-op | 3 m post-op | Final follow-up | Pre-op | 3 m post-op | Final follow-up | Pre-op | 3 m postop | Final follow-up | Pre-op | 3 m post-op | Final follow-up | |
| 1 | 4 | 2 | 0 | 46.7% | 11.1% | 4.4% | 66 | 12 | 15 | 25.3 | 4.95 | 2.38 | D | E | E |
| 2 | 5 | 2 | 1 | 66% | 28% | 12% | 37 | 18 | 3 | 18.9 | 4.48 | 1.87 | C | E | E |
| 3 | 4 | 1 | 0 | 40% | 10% | 4% | 41 | 14 | 11 | 58.2 | 10.3 | 6.8 | E | E | E |
| 4 | 4 | 1 | 1 | 35.6% | 11.1% | 4.4% | 38 | 29 | 10 | 20.8 | 17.1 | 5.9 | D | E | E |
| 5 | 5 | 1 | 0 | 28% | 8% | 4% | 26 | 10 | 4 | 13.2 | 5.9 | 2.6 | E | E | E |
| 6 | 6 | 2 | 2 | 55.6% | 31.1% | 17.8% | 45 | 28 | 19 | 29.1 | 18.5 | 9.2 | C | D | E |
| 7 | 6 | 2 | 1 | 52% | 24% | 12% | 39 | 21 | 7 | 19.1 | 11.2 | 5.5 | D | E | E |
| 8 | 4 | 0 | 0 | 22.2% | 8.9% | 2.2% | 21 | 13 | 9 | 15.4 | 7.2 | 3.5 | E | E | E |
| Mean ± SD | 4.8 ± 0.9 | 1.4 ± 0.7 | 0.6 ± 0.7 | (43.3 ± 14.7)% | (16.5 ± 9.5)% | (7.6 ± 5.6)% | 39.1 ± 13.5 | 18.1 ± 7.3 | 9.8 ± 5.4 | 25.00 ± 14.34 | 9.95 ± 5.41 | 4.72 ± 2.56 | _ | _ | _ |
| P | 0.000* | 0.02** | 0.000* | 0.001** | 0.005* | 0.014** | 0.02* | 0.003** | |||||||
ASIA: American Spinal Injury Association; CRP: C-reactive protein; ESR: erythrocyte sedimentation rate; ODI, Oswestry disability index; VAS, visual analog scale.
*Compared with preoperative.
**Compared with 3 months postoperative.
Laboratory outcomes
Preoperatively, the average ESR and CRP levels were 39.1 ± 13.5 mm/h (range: 21-66 mm/h) and 25.00 ± 14.34 mg/L (range: 13.2-58.2 mg/L), respectively, but both returned to normal within 3 months following the operation. Statistical significance was observed between preoperative, 3-month postoperative, and final follow-up values (P < .05) (Table 3).
Radiological outcomes
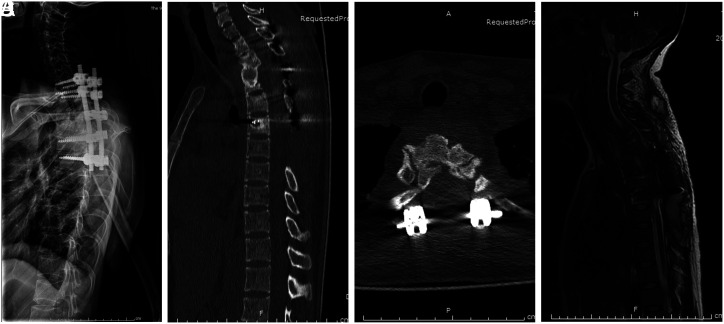
At 3 months post operation, the mean kyphotic Cobb angle was significantly reduced to (6.3 ± 3.2)° (range: 3°–12°) and was (9.8 ± 3.9)° (range: 5°–16°) at the final follow-up. Statistical significance was noted between the preoperative and 3-month postoperative measurements (P < .05). The kyphotic correction rate reached (71.5 ± 7.3)%, but there was a loss of correction angle at the final follow-up, measured at (3.5 ± 1.4)° with a loss rate of correction at (25.1 ± 10.7)% (Table 4). CT scans were conducted as part of a routine examination to assess bone fusion, achieved in all patients, on average, within 15 months (8.3 ± 3.2 months) (Figure 2).
Table 4.
Kyphotic angle correction
| Case no. | Kyphotic Cobb angle | |||||
|---|---|---|---|---|---|---|
| Pre-op | 3 m post-op | Correction rate (%) | Final follow-up | Angle lost | Lost rate (%) | |
| 1 | 15° | 3° | 80% | 8° | 5° | 41.7% |
| 2 | 47° | 12° | 74.5% | 16° | 4° | 11.4% |
| 3 | 36° | 9° | 75% | 12° | 3° | 11.1% |
| 4 | 14° | 4° | 71.4% | 7° | 3° | 30% |
| 5 | 9° | 3° | 66.7% | 5° | 2° | 33.3% |
| 6 | 39° | 8° | 79.5% | 14° | 6° | 19.4% |
| 7 | 18° | 6° | 66.7% | 9° | 3° | 25% |
| 8 | 12° | 5° | 58.3% | 7° | 2° | 28.6% |
| Mean ± SD | 23.8 ± 14.6 | 6.3 ± 3.2 | (71.5 ± 7.3)% | 9.8 ± 3.9 | 3.5 ± 1.4 | (25.1 ± 10.7)% |
| P | 0.004* | 0.000** | ||||
*Compared with preoperative.
**Compared with 3 months postoperative.
Figure 2.
(A) Postoperative lateral X-ray film, local kyphosis had improved significantly. (B) Postoperative CT, solid bone fusion in diseased segments. The local kyphotic Cobb angle was 16°. (C) Axial CT showed that the intervertebral bone graft had achieved bone fusion. (D) Postoperative MRI, spinal cord compression wholly relieved.
Complications
No perioperative complications were associated with decompression; however, 1 patient experienced a loosening of the instrumentation due to unresolved spinal tuberculosis and required reoperation. No instances of wound infection, infectious meningitis, or tuberculosis recurrence occurred. Two patients experienced sinus tract formation, which healed following bone fusion. None of the patients experienced side effects related to anti-tuberculous drugs during follow-up.
Discussion
Spinal tuberculosis in the upper thoracic region is rare,3 and there is limited literature on its treatment.20,21 Early diagnosis of upper thoracic tuberculosis can be challenging due to the lack of obvious systemic and local symptoms and barriers presented by various tissues and organs, which can make it difficult to detect abnormalities with X-rays in the early stages of the disease. As the disease progresses, infection-related loss or collapse of the anterior column support in the upper thoracic region can cause further deformity, instability, and even spinal cord injury, leading to progressive kyphosis as the mobile cervical column topples over the fixed thoracic spine. Thus, early diagnosis and treatment of upper thoracic tuberculosis pose a significant challenge.
In spinal tuberculosis, mycobacteria are transported via end arterioles and deposited near the vertebral endplate’s anterior aspect, with the vertebral body’s anterior portion being most commonly affected.5 Consequently, many scholars view anterior radical debridement as the gold standard for the surgical treatment of spinal tuberculosis.22 Similarly, anterior approach debridement has been utilized by many scholars in the effective treatment of upper thoracic tuberculosis.13,23 However, performing anterior approach thoracic spine surgery can be challenging, particularly in the upper thoracic region, requiring significant experience and expertise and may not be feasible in general practice.
Posterior extensive circumferential decompressive reconstructive techniques are often used in treating upper thoracic spine disease, and posterior-only approaches can achieve subtotal vertebrectomy.24 This approach provides adequate operating space by removing the facet joint, diapophysis, and even thoracic nerve roots, resulting in direct visualization of the surfaces of the vertebral body and the outside of the dura mater,25 which facilitates thorough removal of focal tuberculosis and complete spinal decompression without damaging the spinal cord. In our clinical study, the operation time, blood loss, and postoperative drainage volume were 262.5 ± 43.3 minutes, 625.0 ± 333.8 mL, and 285.0 ± 118.1 mL, respectively, which were more significant than the anterior approach or posterior approach reported in the literature,23,26 which may be related to the operative technique of the surgeon. All patients significantly relieved postoperative symptoms, with a marked reduction in VAS and ODI scores. During the follow-up period, ESR and CRP levels significantly decreased and returned to normal within 3 months postoperatively. No cases of spinal cord injury occurred during the operation, and patients with paralysis symptoms experienced the return of neurological function to normal following the operation. Therefore, satisfactory clinical results were achieved through posterior approach surgery.
Regarding complications and bone graft fusion, only 1 patient experienced complications related to instrumentation and required reoperation due to unresolved spinal tuberculosis. In contrast, all others achieved excellent bone fusion during follow-up without relapse. Our clinical study’s average bone graft fusion time was 8 months, consistent with the literature reports.27,28 A single posterior incision was used for posterior fixation, lesion removal, spinal cord decompression, and bone graft fusion, resulting in a clinical cure.
A posterior approach with pedicle screw fixation is known to have a better effect on kyphotic correction.9 In our study, the average postoperative kyphotic Cobb angle was 6.3° ± 3.2°, statistically and significantly better than before the operation and superior to the results reported in the literature for the anterior approach technique.20,27 Our kyphotic correction rate was similar to that of a previous study,9 and posterior approach long-segment pedicle screw fixation was particularly beneficial for correcting kyphosis. However, the loss of correction angle and rate were notably higher than those reported in the literature,9 possibly due to the older age of our patients and the presence of osteoporosis impacting the maintenance of the kyphotic correction rate. Additionally, some patients received an iliac bone block for anterior column bone grafting, which made them prone to kyphotic correction loss following the operation. This is consistent with literature reports that autogenous iliac bone graft is less effective than titanium mesh cages in maintaining kyphotic correction.25 Moreover, although postoperative residual kyphosis was low in our study, the slight loss of correction angle at the final follow-up also contributed significantly to the loss rate of correction.
Surgical intervention accompanied by anti-tuberculosis treatment is indicated in patients with spinal tuberculosis who present with significant deformity and instability, neurological deficits, and spinal cord or neural root compression.5 Posterior approach surgery is minimally invasive, safe, reliable, and effective for treating upper thoracic tuberculosis, with favorable clinical and radiological outcomes.
Limitations
This is a retrospective study. The sample size is too small, the follow-up time is not long enough, and more indicators are needed to assess the effectiveness of the surgery, which may affect the credibility of this study. Further studies involving more extensive patient series, extended follow-up periods, and case-control comparisons are necessary to achieve a consensus on this issue.
Conclusion
The posterior-only approach is an effective, safe, and reliable treatment method for upper thoracic tuberculosis, with favorable clinical and radiological outcomes.
Data Availability Statement:
The data that support the findings of this study are available on request from the corresponding author.
Funding Statement
This study was supported by Chinese People’s Liberation Army Medical Technology Youth Training Program (No. 20QNPY071) and the Natural Science Foundation of Gansu Province (No. 21YF1FA179, No. GSWSKY2020-05 and No. 2021yxky008).
Footnotes
Ethics Committee Approval: This study was approved by the Ethics Committee of The 940th Hospital of Joint Logistics Support Force of Chinese PLA (approval number: 2020KYLL002; date: 2020.04).
Informed Consent: Informed consent was obtained from the patients who agreed to take part in the study.
Peer-review: Externally peer reviewed.
Author Contributions: Concept – T.Z., S.L.; Design – T.Z., S.L.; Supervision – S.L.; Resources – T.Z., L.M.; Materials – H.L.; Data Collection and/or Processing – T.Z., L.M.; Analysis and/or Interpretation – L.Z.; Literature Search – C.Y.; Writing – T.Z., L.M.; Critical Review – S.L.
Declaration of Interests: The authors have no conflicts of interest to declare.
References
- 1. Jain AK, Rajasekaran S, Jaggi KR, Myneedu VP. Tuberculosis of the spine. J Bone Joint Surg Am. 2020;102(7):617 628. ( 10.2106/JBJS.19.00001) [DOI] [PubMed] [Google Scholar]
- 2. Shi T, Zhang Z, Dai F, et al. Retrospective study of 967 patients with spinal tuberculosis. Orthopedics. 2016;39(5):e838 e843. ( 10.3928/01477447-20160509-03) [DOI] [PubMed] [Google Scholar]
- 3. Yao Y, Song W, Wang K, et al. Features of 921 patients with spinal tuberculosis: A 16-year investigation of a general hospital in southwest china. Orthopedics. 2017;40(6):e1017 e1023. ( 10.3928/01477447-20171012-03) [DOI] [PubMed] [Google Scholar]
- 4. Sharma A, Chhabra HS, Chabra T, Mahajan R, Batra S, Sangondimath G. Demographics of tuberculosis of spine and factors affecting neurological improvement in patients suffering from tuberculosis of spine: A retrospective analysis of 312 cases. Spinal Cord. 2017;55(1):59 63. ( 10.1038/sc.2016.85) [DOI] [PubMed] [Google Scholar]
- 5. Heyde CE, Lübbert C, Wendt S, Rodloff A, Völker A, von der Höh NH. Spinal tuberculosis. Z Orthop Unfall. 2022;160(1):74 83. ( 10.1055/a-1285-4994) [DOI] [PubMed] [Google Scholar]
- 6. Mak KC, Cheung KM. Surgical treatment of acute tb spondylitis: indications and outcomes. Eur Spine J. 2013;22(suppl 4):603 611. ( 10.1007/s00586-012-2455-0) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Muheremu A, Niu X, Wu Z, Tian W. Study on anterior and posterior approaches for spinal tuberculosis: A meta-analysis. Eur J Orthop Surg Traumatol. 2015;25(suppl 1):S69 S76. ( 10.1007/s00590-014-1508-y) [DOI] [PubMed] [Google Scholar]
- 8. Yang P, Zang Q, Kang J, Li H, He X. Comparison of clinical efficacy and safety among three surgical approaches for the treatment of spinal tuberculosis: A meta-analysis. Eur Spine J. 2016;25(12):3862 3874. ( 10.1007/s00586-016-4546-9) [DOI] [PubMed] [Google Scholar]
- 9. Liu H, Luo J, Wang X, Dong X, Hao D. Efficacy of surgery via the single anterior and single posterior approaches for treatment of thoracic spinal tuberculosis. J Int Med Res. 2020;48(1):300060519896743. ( 10.1177/0300060519896743) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yaldz C, Özdemir N, Yaman O, Feran HG, Tansug T, Minoglu M. A retrospective study of 39 patients treated with anterior approach of thoracic and lumbar spondylodiscitis: clinical manifestations, anterior surgical treatment, and outcome. Med (Baltim). 2015;94(47):e2110. ( 10.1097/MD.0000000000002110) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Srivastava SK, Marathe NA, Bhosale SK, et al. Outcome analysis of anterior reconstruction with rib grafts in tuberculosis of the thoracic spine. Asian J Neurosurg. 2020;15(3):648 652. ( 10.4103/ajns.AJNS_52_20) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mihir B, Vinod L, Umesh M, Chaudhary K. Anterior instrumentation of the cervicothoracic vertebrae: approach based on clinical and radiologic criteria. Spine. 2006;31(9):E244 E249. ( 10.1097/01.brs.0000214883.11874.80) [DOI] [PubMed] [Google Scholar]
- 13. Okyere I, Lamina A, Owusu B. Full median sternotomy approach for treatment of upper thoracic vertebral tuberculosis in a developing country: case report and short literature review. Pan Afr Med J. 2017;28:112. ( 10.11604/pamj.2017.28.112.12948) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hu H, Winters HAH, Paul RMA, Wuisman PIJM. Internal thoracic vessels used as pedicle graft for anastomosis with vascularized bone graft to reconstruct c7-t3 spinal defects: A new technique. Spine. 2007;32(5):601 605. 10.1097/01.brs.0000256383.29014.42 [DOI] [PubMed] [Google Scholar]
- 15. Chen Y, Lü G, Wang B, Li L, Kuang L. Posterior vertebral column resection with intraoperative manual retraction for the treatment of posttubercular kyphosis in upper thoracic spine or cervicothoracic junction. Clin Spine Surg. 2017;30(8):E1055 E1061. ( 10.1097/BSD.0000000000000479) [DOI] [PubMed] [Google Scholar]
- 16. Wang ST, Ma HL, Lin CP, et al. Anterior debridement may not be necessary in the treatment of tuberculous spondylitis of the thoracic and lumbar spine in adults a retrospective study. Bone Joint J. 2016;98 -B(6):834 839. ( 10.1302/0301-620X.98B6.36472) [DOI] [PubMed] [Google Scholar]
- 17. Ye S, Sun J, Jing J. Isolated posterior instrumentation for selected cases of thoracic and lumbar spinal tuberculosis without radical debridement. Z Orthop Unfall. 2022;160(6):679 685. ( 10.1055/a-1851-5509) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nene AM, Patil S, Kathare AP, Nagad P, Nene A, Kapadia F. Six versus 12 months of anti tubercular therapy in patients with biopsy proven spinal tuberculosis: A single center, open labeled, prospective randomized clinical trial-a pilot study. Spine. 2019;44(1):E1 E6. ( 10.1097/BRS.0000000000002811) [DOI] [PubMed] [Google Scholar]
- 19. Guo Y, Xu M, Li L, Gu B, Zhang Z, Diao W. Comparative efficacy of traditional conservative treatment and ct-guided local chemotherapy for mild spinal tuberculosis. BMC Musculoskelet Disord. 2022;23(1):589. ( 10.1186/s12891-022-05545-w) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jiang H, Xiao ZM, Zhan XL, He ML. Anterior transsternal approach for treatment of upper thoracic vertebral tuberculosis. Orthop Surg. 2010;2(4):305 309. ( 10.1111/j.1757-7861.2010.00104.x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zhang H, Sheng B, Tang M, et al. One-stage surgical treatment for upper thoracic spinal tuberculosis by internal fixation, debridement, and combined interbody and posterior fusion via posterior-only approach. Eur Spine J. 2013;22(3):616 623. ( 10.1007/s00586-012-2470-1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Talu U, Gogus A, Ozturk C, Hamzaoglu A, Domanic U. The role of posterior instrumentation and fusion after anterior radical debridement and fusion in the surgical treatment of spinal tuberculosis: experience of 127 cases. J Spinal Disord Tech. 2006;19(8):554 559. ( 10.1097/01.bsd.0000211202.93125.c7) [DOI] [PubMed] [Google Scholar]
- 23. Li Z, Li K, Tang B, et al. Analysis of the curative effect of the anterior approach to the lower cervical spine for cervicothoracic spinal tuberculosis. J Craniofac Surg. 2020;31(2):480 483. ( 10.1097/SCS.0000000000006097) [DOI] [PubMed] [Google Scholar]
- 24. Omran K, Abdel-Fattah AS. Posterior extensive circumferential decompressive reconstructive technique in surgical treatment of upper thoracic spine compressive lesions. World Neurosurg. 2019;123:e501 e508. ( 10.1016/j.wneu.2018.11.194) [DOI] [PubMed] [Google Scholar]
- 25. Wu W, Wang S, Li Z, Lin R, Lin J. Posterior-only approach with titanium mesh cages versus autogenous iliac bone graft for thoracic and lumbar spinal tuberculosis. J Spinal Cord Med. 2021;44(4):598 605. ( 10.1080/10790268.2019.1675953) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zeng H, Shen X, Luo C, et al. Comparison of three surgical approaches for cervicothoracic spinal tuberculosis: A retrospective case-control study. J Orthop Surg Res. 2015;10:100. ( 10.1186/s13018-015-0238-0) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lin B, Shi J-S, Zhang H-S, Xue C, Zhang B, Guo Z-M. Subscapularis transthoracic versus posterolateral approaches in the surgical management of upper thoracic tuberculosis: A Prospective, Randomized Controlled Study. Medicine. 2015;94(47):e1900. ( 10.1097/MD.0000000000001900) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Liu Z, Wang X, Xu Z, et al. Two approaches for treating upper thoracic spinal tuberculosis with neurological deficits in the elderly: A retrospective case-control study. Clin Neurol Neurosurg. 2016;141:111 116. ( 10.1016/j.clineuro.2016.01.002) [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.



 Content of this journal is licensed under a
Content of this journal is licensed under a