Abstract
Teaching medical rounds in intensive care units (ICUs) are essential for resident education. However, the ICU’s high workload can hinder these rounds. We propose a new approach that is based on the constructivist theory of learning communities. This approach emphasizes active, collaborative learning through interaction. In the ICU, it encourages active learning, peer interaction, and shared responsibility among residents. Our model involves structured teaching rounds that promote active learning, collaboration, and reflection, all integrated into the ICU workflow. This new approach aims to enhance the learning experience; improve teaching round effectiveness; and, ultimately, contribute to better patient care.
Keywords: teaching rounds, intensive care, collaborative learning
In the early 20th century, William Osler advocated for an interaction model between senior doctors, apprentices, and patients, similar to today’s medical rounds. This historical model involved conducting rounds at the patient’s bedside. The lead doctor would listen as apprentices presented the patient’s history and relevant data, demonstrate further elements of the history or physical examination skills, model effective patient communication, and discuss the theory behind the disease and treatment (1). Today, medical rounds play a crucial role in teaching hospitals, serving dual purposes in patient care and medical education. They facilitate discussions and planning for patient care among doctors and students. Additionally, they present a unique opportunity for students to engage in patient care and educational activities, particularly as time for these activities diminishes. This underscores the significance of medical rounds in both immediate patient health management and the continuous training of future medical professionals (2). Rounds have evolved because of changes in medical education, technology, and labor policies. They are now more focused on shared decision-making, involving patients and their families in medical care (3). Restrictions on working hours and time pressures have promoted a standardized approach in preparing for rounds, reducing the time dedicated to education. The adoption of models such as family-centered rounds (4, 5) and competency-based education have changed the perceptions of rounds (6), more closely linking clinical and educational activities. However, these have also created tensions because of the divergent needs of participants. In addition, the use of technology has altered the dynamics of rounds, potentially affecting bedside teaching and the implementation of clinical education.
Medical rounds, an essential aspect of bedside teaching, have declined because of factors such as rising patient numbers, time limitations, and the heavy workload in hospitals (7). Despite its long-standing tradition in medicine, it is estimated that only between 8 and 17% of medical training uses this method today (8). It is interesting that the intensive care unit (ICU) presents a unique context in which case-based bedside learning, complemented by didactic lectures, is the main educational method in nearly 91% of instances (9). Bedside learning cultivates a setting that encourages the engagement of all team members—residents, interns, nurses, and therapists. This is achieved through strategies that promote group interaction, introduce team members, stimulate learners with thought-provoking questions, and teach at different levels of understanding.
Although it is acknowledged that medical rounds play a crucial role in medical education, there is considerable diversity in their practice. A survey from Latin America highlighted significant differences in the duration and nature of clinical rounds among various countries. This contrast was particularly pronounced when comparing academic and nonacademic ICUs. In academic environments, brief, nonmultidisciplinary morning rounds were more common, underlining the challenges due to time and resource constraints that academic intensivists face in delivering high-quality clinical care (10).
These strategies involve all healthcare personnel in patient care, fostering a valuable interprofessional environment. This highlights the significance of practice communities in medical education (11, 12). Such communities are essential for intensivist training, incorporating the entire multidisciplinary team in medical rounds and most ICU activities (13). Therefore, these settings allow intensivists to refine teamwork abilities, communication skills, and intensive care knowledge.
On the basis of the theory of learning communities, we have developed a model for medical rounds that enables meaningful learning without disrupting the ICU workflow.
Theory
Social constructivism is a learning theory that posits that individuals construct knowledge through interaction with others and the surrounding world. This theory underscores the notion that learning is a social process and that knowledge is constructed rather than transmitted. According to this theory, language is a tool used by individuals to construct knowledge, whereas culture provides the context for this learning. Here, students are not merely passive recipients of information but actively participate in the knowledge-construction process.
Learning communities are a pedagogical strategy based on the premise that learning is a social and collaborative process. In a learning community, students collaborate to construct knowledge, often through discourse and collaboration. This approach aligns with the social constructivism theory, which suggests that knowledge is constructed through interaction with others and the environment. Learning communities can take various forms, ranging from informal study groups to professional communities of practice. However, all learning communities prioritize collaboration, interaction, and the collective construction of knowledge. According to Wenger, these communities have three main components (11).
-
•
The domain, which refers to the area of shared interest or knowledge that unites the members of the community. This common domain provides a sense of identity and shared purpose to the members of the community.
-
•
The community, which refers to the relationships and interaction among community members. In a learning community, members engage in joint activities, help each other, and share information and resources.
-
•
The practice, which refers to the knowledge, skills, tools, concepts, language, and methods that community members develop as they interact and learn together. This shared practice is what enables community members to address the problems and challenges of their domain.
Teaching Rounds
Medical rounds are a teaching method used in clinical settings where educators simultaneously care for patients and instruct trainees. Given the time constraints, efficient strategies are needed to assess trainee knowledge and skills, teach swiftly, and provide feedback. The quality of supervision during these rounds significantly impacts clinical competence and knowledge. However, in our ICU, we identified several weaknesses associated with medical rounds:
-
1.
Absence of interprofessionalism: Other professional groups may not participate because of high care loads. Spending about 2 hours on academic medical rounds can detract from their daily care tasks. This lack of interprofessionalism shrinks learning communities in the ICU and hinders the development of communication and leadership skills in intensivist training.
-
2.
Preparation: Many educators do not prepare in advance for the medical round. Preparation should include recognizing participating patients and defining objectives within the learning community.
-
3.
Teacher training: Many professionals lack medical teaching training, which could limit their use of diverse didactic tools and strategies that promote meaningful learning.
-
4.
Level of difficulty: Asking highly difficult questions without considering the experience level of the community members may discourage participation, particularly from peripheral participants.
-
5.
Reflection: Despite providing feedback, there is no built-in time for reflection at the end of the medical round.
Considering these issues from the perspective of practice communities, and on the basis of suggestions by Ramani (14), Chan and colleagues (15), and Carlos and colleagues (3), we propose a new structure for medical rounds Figure 1:
Figure 1.
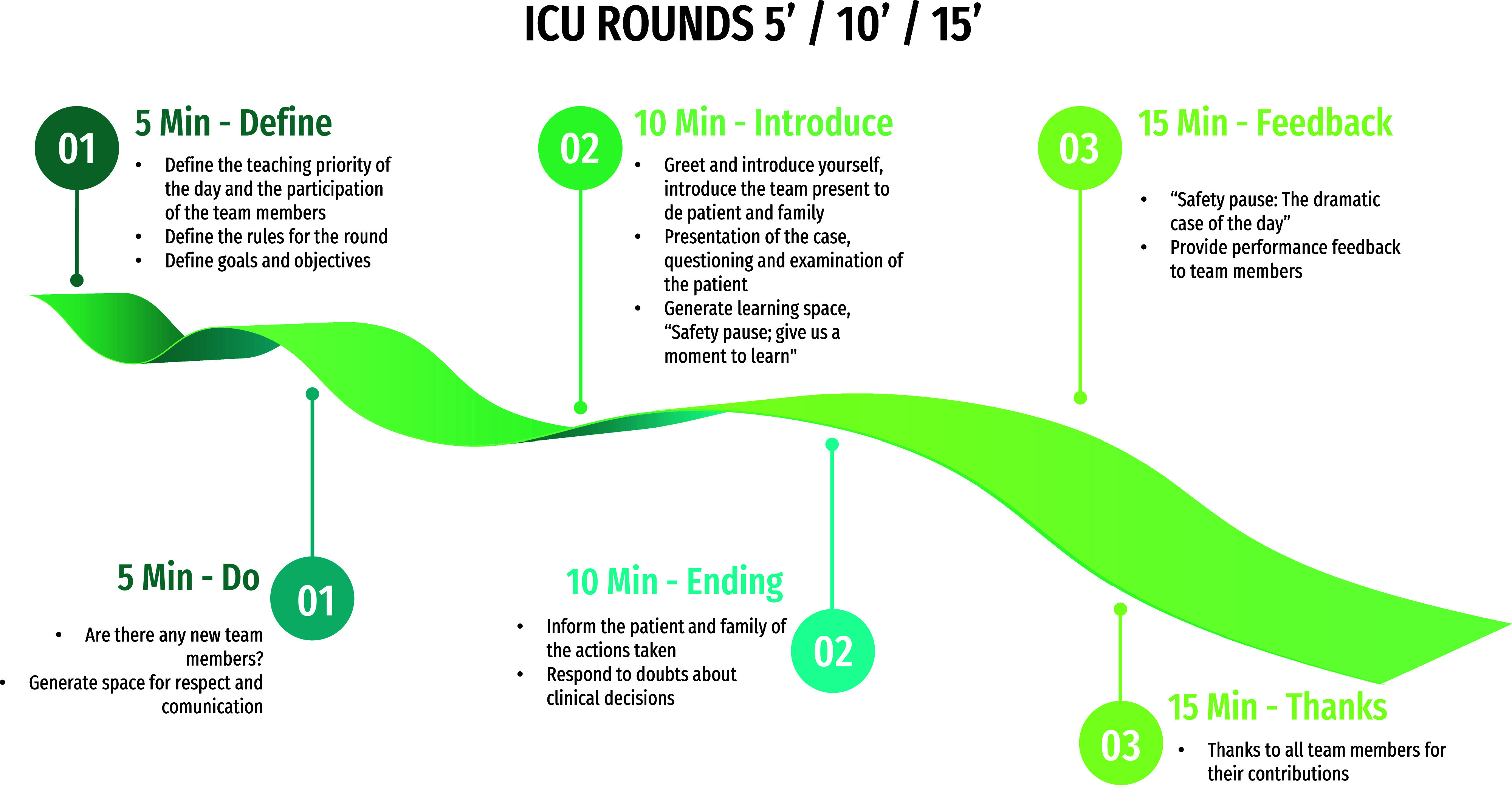
Intensive care unit rounds at 5, 10, and 15 minutes.
Checklist for medical rounds (5 min before round start)
-
•
Meet new team members: If any, learn their profession and training level. Briefly introduce them to the group and discuss their round expectations.
-
•
Establish round guidelines: duration, start time, and sequence (e.g., the most critically ill patient goes first).
-
•
Identify goals and expected outcomes based on team members’ professions and duties, particularly for students. Everyone should be clear on their tasks, so confirm this with a quick question round.
-
•
Encourage a respectful and communicative setting: For instance, implement a “Safety Pause” for mobile device usage rules.
-
•
Decide on the day’s learning focus and how team members will participate in it (answer any related queries).
This initial stage helps allocate roles and define boundaries for the activity. It ensures everyone’s involvement, including those at the edges, by recognizing their role in the group. It also reduces the time pressure often experienced by professionals with the highest care burden (16).
Checklist for medical rounds (10 min per visit*)
-
•
Greet the patient and their family and introduce the team (clinic teacher).
-
•
Discuss the case, engage in dialogue, and check in with the patient and family (clinic teacher and team, students included).
-
•Incorporate a learning moment: “Safety Pause: Learning Time,” facilitated by the clinic teacher.
-
◦Discuss the case as a team (address unresolved issues and tasks, invite input from team members, and problem-solve collectively).
-
◦Confirm the medical plan with guidance from the medical teacher (if there is uncertainty, carve out time for questions and answers).
-
◦
-
•
Inform the patient and their family about the actions taken (clinic teacher or designated individual).
-
•
Address any inquiries about the medical decisions (group participation is encouraged).
The latter part of this process ensures inclusivity, promotes collaboration, and encourages interaction based on everyone’s role.
Checklist for medical rounds (15 min, postround)
-
•
Initiate a “Safety Pause: The Dramatic Case of the Day.” Discuss the expectations, emotions, and new insights involved, along with possible areas for improvement. Reflect on a complex or challenging case, chosen either by the clinical teacher or by the team members.
-
•
Acknowledge and thank all team members for their contributions.
-
•
Feedback is generally given in a private room, focusing on observable behavior and its improvement and avoiding judgments about the individual’s personality. It should be specific, providing both concrete examples of what was done well and areas for improvement, thus facilitating its understanding and applicability. In addition, it should be descriptive, using words to clarify the observed behaviors and their impact on learning or work. Finally, the feedback should directly address the observed attitudes, behaviors, and knowledge, allowing the receiver to understand and act on it (17).
The usual duration of the full round is between 120 and 150 minutes.
Discussion
Teams in the ICU often consist of intensivists, clinical pharmacists, respiratory therapists, dietitians, nurses, clinical psychologists, and physicians in training (18). Multiple factors shape the effectiveness of these teams, clear communication, trust in each other’s skills, knowledge about team members, and leadership that combines authority with cooperation.
In these teams, each member brings unique expertise and skills. The team’s success hinges on the ability of members to collaborate, leveraging their individual knowledge to reach a common goal. Transactive memory systems are mechanisms that groups and organizations use to organize and share specialized knowledge (19). These systems evolve through shared experiences within the group, meaning that they are shaped and fine-tuned as members work together on specific tasks and learn about each other’s strengths and areas of knowledge.
These systems are idiosyncratic; that is, they are specific and unique to each group or organization. This idiosyncratic nature is because transactive memory systems are based on the specific interactions and experiences of the group members. This makes them especially difficult to imitate by other groups or competitors, as an external group cannot simply observe and replicate the transactive memory system of a successful group without having the same experiences and internal dynamics.
In terms of competitive advantage, transactive memory systems can be a valuable source for organizations. By facilitating the transfer and efficient use of specialized knowledge within the group, these systems can enhance creativity, efficiency, and responsiveness to environmental changes.
Some evidence suggests that ICU teams can develop transactive memory systems that align with patient care needs and priorities, enhancing performance in these critical settings (20). Clear communication is vital, as it allows for the exchange of information, ideas, and viewpoints among team members with diverse backgrounds, experiences, and skills. Trust is key for teams to work effectively in high-stress situations, even without a shared past. Leadership should maintain a balance between authority and collaboration to encourage a team-oriented environment.
Working together across different professions, or interprofessionalism, is essential to patient care (21). One study, which used surveys that were specifically designed for each professional group in the ICU, highlights the importance of interprofessional teaching in the ICU. Although all providers participate in rounds, teaching is infrequent. It is suggested that there are opportunities to improve interprofessional education and collaboration in the ICU (22). Some evidence suggests better patient outcomes when care is given by an interprofessional team. An analysis of historical data involving over 100,000 patients showed lower mortality rates when multidisciplinary rounding teams were used, compared with when nonmultidisciplinary teams were used for rounds (23). A systematic review of 43 studies aimed to pinpoint the most effective methods for conducting rounds. It emphasized that multidisciplinary rounding teams, well-defined roles during rounds, and a structured approach focused on specific objectives are crucial for enhancing ICU rounds (24).
Each member of the ICU team—critical care nurses, advanced practice providers, pharmacists, respiratory care professionals, rehabilitation specialists, dietitians, social workers, case managers, intensivists, and nonintensivist physicians—brings unique expertise and viewpoints to patient care. They are essential in a team that must cater to the diverse needs of patients and families in the ICU. The ICU environment distinctly differs from the rest of the hospital in terms of workload, emotional strain, patient complexity, and interdisciplinarity, making teaching in the ICU uniquely challenging (25, 26).
Nurses’ roles in rounds involve active participation in patient care review and planning, contributing a critical perspective on daily care, treatment responses, and specific patient needs. As patient advocates, nurses facilitate communication between the patient and the medical team, ensuring that the patient’s perspectives and preferences are central to the care plan. Leveraging their clinical knowledge and experience, nurses support decision-making and care planning, which is essential for safe, timely, and effective patient care progression. The active involvement of nurses in rounds is associated with high-quality patient care, emphasizing the significance of their inclusion and effective participation in this process (27).
Some evidence shows that when nursing staff and intensivists work together and use a round tool, it improves the daily review of patient metrics in the ICU. This includes conducting awakening and spontaneous breathing tests, which notably shorten the length of ICU stays and the need for mechanical ventilation (28). Enhanced education and experience in the nursing field have been associated with reduced mortality rates in ICU patients (29).
Gonzalo and colleagues (30), in their interviews with internal medicine faculty about medical rounds, identified strategies such as preparation and role assignment that could potentially apply to the ICU. However, it is worth noting that ICU teams may include a wider range of healthcare professionals, including intensivists, nurses, pharmacists, respiratory therapists, and other specialists. Given the severity of patients’ conditions and the need for ongoing monitoring, ICU rounds may be more frequent and longer. Teaching in the ICU might require a more focused approach to critical care skills and procedures, which could affect the selection of teaching topics during rounds.
A study on interprofessional work in ICUs identifies various forms of interaction, including collaboration, coordination, and networking (31). These interactions are crucial for patient care, but they significantly differ from the idealized concept of a team functioning as a single entity. Collaboration involves communication between professionals about specific problems. Coordination entails working concurrently on shared tasks and convening to review and discuss the work. Networking occurs through meetings (virtual or in person), as required on the basis of specific skills or knowledge. The study also emphasizes hierarchical structures and the dominance of medicine in ICUs, which influence interprofessional interactions. Doctors often make the primary decisions, whereas other health professionals frequently serve as information collectors during rounds.
This dynamic indicates a need for more formalized structures for communication and collaboration among health professionals to overcome the barriers created by hierarchy and medical dominance. Our proposed round structure could surmount these challenges by establishing nonhierarchical roles and efficient communication during the ICU workflow.
Interprofessional education offers several crucial advantages. First, it underscores the need to develop a deeper understanding of other team members’ viewpoints and to agree on shared models for implementing specific practices. This is seen as beneficial in promoting understanding and collaboration among various healthcare professionals. A further advantage is the ability to coordinate a wide range of expertise in quality improvement projects, where diverse professionals collaborate to address issues. This demonstrates how interprofessional education can act as a driving force for enhancing the use of evidence in health care (32). During the pandemic, the ICUs were characterized by a great appreciation for the commitment, cooperation, and willingness of everyone involved in the work of the coronavirus disease (COVID-19) ICUs. A climate of trust, camaraderie, and solidarity was observed, with a focus on mutual support and receptive learning on the job. This collaborative atmosphere was crucial in compensating for other shortcomings and was considered essential for maintaining the quality of patient care through interprofessional collaboration (33).
In learning communities, the theory recognizes students as individuals who transition from legitimate peripheral participation to full group membership (11). In the context of the medical round, students become active participants within the “community” after mastering the topics discussed (34). This structured approach helps us overcome previously identified limitations and meet training objectives for professionals, allowing them to actively participate in a significant number of activities. This provides access to enriching experiences that strengthen their knowledge and skills in a supervised environment.
From our perspective, this approach promotes interdisciplinarity by bringing together professionals and students from various medical fields. It offers a practical solution for teaching medical rounds and provides tools for untrained educators, making their practice easier and balancing role and task assignments.
This method creates opportunities for guided reflection and enhances the clinical teacher’s ability to identify participant expectations and the required knowledge levels. It promotes inclusivity and legitimizes participation in medical rounds, ensuring that the questions asked align with the participants’ training level. Additionally, it encourages students to explore their clinical reasoning processes in a safe environment (35), fostering the constructive feedback that is crucial for developing critical thinking skills.
We firmly believe in the need to reinforce learning communities within ICUs through strategies that deliver effective and relevant learning across all professional levels.
Footnotes
Author disclosures are available with the text of this article at www.atsjournals.org.
The most critical and complex patients could take more time: Approaches beyond 10 minutes are allowed, as long as the instructor believes that the discussion will deepen aspects that stimulate knowledge by adding 5 minutes. Complex patients do not necessarily have to be the sickest patients. They can also include those for whom the clinical decisions present a challenge to the objectives of the day, such as important bioethical decisions or patients with uncertain diagnoses. Cases that definitely require a more extensive and time-consuming discussion may be chosen for intensive care department morbidity and mortality academic meetings.
References
- 1. Linfors EW, Neelon FA. Sounding boards. The case of bedside rounds. N Engl J Med . 1980;303:1230–1233. doi: 10.1056/NEJM198011203032110. [DOI] [PubMed] [Google Scholar]
- 2. Stickrath C, Noble M, Prochazka A, Anderson M, Griffiths M, Manheim J, et al. Attending rounds in the current era: what is and is not happening. JAMA Intern Med . 2013;173:1084–1089. doi: 10.1001/jamainternmed.2013.6041. [DOI] [PubMed] [Google Scholar]
- 3. Carlos WG, Kritek PA, Clay AS, Luks AM, Thomson CC. Teaching at the bedside. Maximal impact in minimal time. Ann Am Thorac Soc . 2016;13:545–548. doi: 10.1513/AnnalsATS.201601-018AS. [DOI] [PubMed] [Google Scholar]
- 4. COMMITTEE ON HOSPITAL CARE and INSTITUTE FOR PATIENT- AND FAMILY-CENTERED CARE. Patient- and family-centered care and the pediatrician’s role. Pediatrics . 2012;129:394–404. doi: 10.1542/peds.2011-3084. [DOI] [PubMed] [Google Scholar]
- 5. Schneider D, Rosa RG, Santos RDRMD, Fogazzi DV, Rech GS, Silva DBD, et al. Effects of participation in interdisciplinary rounds in the intensive care unit on family satisfaction: a cross-sectional study. Crit Care Sci . 2023;35:203–208. doi: 10.5935/2965-2774.20230274-en. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rabinowitz R, Farnan J, Hulland O, Kearns L, Long M, Monash B, et al. Rounds today: a qualitative study of internal medicine and pediatrics resident perceptions. J Grad Med Educ . 2016;8:523–531. doi: 10.4300/JGME-D-15-00106.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Peters M, Ten Cate O. Bedside teaching in medical education: a literature review. Perspect Med Educ . 2014;3:76–88. doi: 10.1007/s40037-013-0083-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Crumlish CM, Yialamas MA, McMahon GT. Quantification of bedside teaching by an academic hospitalist group. J Hosp Med . 2009;4:304–307. doi: 10.1002/jhm.540. [DOI] [PubMed] [Google Scholar]
- 9. Chudgar SM, Cox CE, Que LG, Andolsek K, Knudsen NW, Clay AS. Current teaching and evaluation methods in critical care medicine: has the Accreditation Council for Graduate Medical Education affected how we practice and teach in the intensive care unit? Crit Care Med . 2009;37:49–60. doi: 10.1097/CCM.0b013e31819265c8. [DOI] [PubMed] [Google Scholar]
- 10. Castro R, Nin N, Ríos F, Alegría L, Estenssoro E, Murias G, et al. Latin-American Intensive Care Network - LIVEN ( www.redliven.org) The practice of intensive care in Latin America: a survey of academic intensivists. Crit Care . 2018;22:39. doi: 10.1186/s13054-018-1956-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hodson N. Landscapes of practice in medical education. Med Educ . 2020;54:504–509. doi: 10.1111/medu.14061. [DOI] [PubMed] [Google Scholar]
- 12. Egan T, Jaye C. Communities of clinical practice: the social organization of clinical learning. Health (London) . 2009;13:107–125. doi: 10.1177/1363459308097363. [DOI] [PubMed] [Google Scholar]
- 13. Dorman T, Angood PB, Angus DC, Clemmer TP, Cohen NH, Durbin CG, Jr, et al. American College of Critical Care Medicine Guidelines for critical care medicine training and continuing medical education. Crit Care Med . 2004;32:263–272. doi: 10.1097/01.CCM.0000104916.33769.9A. [DOI] [PubMed] [Google Scholar]
- 14. Ramani S. Twelve tips to improve bedside teaching. Med Teach . 2003;25:112–115. doi: 10.1080/0142159031000092463. [DOI] [PubMed] [Google Scholar]
- 15. Chan SJ, Archibald HL, Conner SM. NET Rounding: a novel approach to efficient and effective rounds for the modern clinical learning environment. BMC Med Educ . 2022;22:600. doi: 10.1186/s12909-022-03599-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pratt D, Magill MK. Educational contracts: a basis for effective clinical teaching. J Med Educ . 1983;58:462–467. [PubMed] [Google Scholar]
- 17. Burgess A, van Diggele C, Roberts C, Mellis C. Feedback in the clinical setting. BMC Med Educ . 2020;20(Suppl. 2):460. doi: 10.1186/s12909-020-02280-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Donovan AL, Aldrich JM, Gross AK, Barchas DM, Thornton KC, Schell-Chaple HM, et al. University of California, San Francisco Critical Care Innovations Group Interprofessional care and teamwork in the ICU. Crit Care Med . 2018;46:980–990. doi: 10.1097/CCM.0000000000003067. [DOI] [PubMed] [Google Scholar]
- 19. Argote L, Fahrenkopf E. Knowledge transfer in organizations: the roles of members, tasks, tools, and networks. Organ Behav Hum Decis Process . 2016;136:146–159. [Google Scholar]
- 20. Kruser JM, Solomon D, Moy JX, Holl JL, Viglianti EM, Detsky ME, et al. Impact of interprofessional teamwork on aligning intensive care unit care with patient goals: a qualitative study of transactive memory systems. Ann Am Thorac Soc . 2023;20:548–555. doi: 10.1513/AnnalsATS.202209-820OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Artis KA, Dyer E, Mohan V, Gold JA. Accuracy of laboratory data communication on ICU daily rounds using an electronic health record. Crit Care Med . 2017;45:179–186. doi: 10.1097/CCM.0000000000002060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Petri CR, Beltran CP, Sullivan AM, Anandaiah A. Who is teaching residents in the intensive care unit? Perceptions of interprofessional teaching at an academic medical center. ATS Scholar . 2023;4:320–331. doi: 10.34197/ats-scholar.2023-0008OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kim MM, Barnato AE, Angus DC, Fleisher LA, Kahn JM. The effect of multidisciplinary care teams on intensive care unit mortality. Arch Intern Med . 2010;170:369–376. doi: 10.1001/archinternmed.2009.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lane D, Ferri M, Lemaire J, McLaughlin K, Stelfox HT. A systematic review of evidence-informed practices for patient care rounds in the ICU*. Crit Care Med . 2013;41:2015–2029. doi: 10.1097/CCM.0b013e31828a435f. [DOI] [PubMed] [Google Scholar]
- 25. Doyle S, Sharp M, Winter G, Khan MMKS, Holden R, Djondo D, et al. Twelve tips for teaching in the ICU. Med Teach . 2021;43:1005–1009. doi: 10.1080/0142159X.2020.1859097. [DOI] [PubMed] [Google Scholar]
- 26. Papazian L, Hraiech S, Loundou A, Herridge MS, Boyer L. High-level burnout in physicians and nurses working in adult ICUs: a systematic review and meta-analysis. Intensive Care Med . 2023;49:387–400. doi: 10.1007/s00134-023-07025-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Merriman C, Freeth D. Interprofessional ward rounds in an adult intensive care unit: an appreciative inquiry into the central collaboration between the consultant and the bedside nurse. J Interprof Care . 2024;38:435–443. doi: 10.1080/13561820.2021.1985441. [DOI] [PubMed] [Google Scholar]
- 28. Lancaster B, Shifrin MM, Gast S. Using a standardized rounding tool to improve the incidence of spontaneous awakening and breathing trials. Crit Care Nurse . 2022;42:e1–e8. doi: 10.4037/ccn2022854. [DOI] [PubMed] [Google Scholar]
- 29. Kelly DM, Kutney-Lee A, McHugh MD, Sloane DM, Aiken LH. Impact of critical care nursing on 30-day mortality of mechanically ventilated older adults. Crit Care Med . 2014;42:1089–1095. doi: 10.1097/CCM.0000000000000127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gonzalo JD, Heist BS, Duffy BL, Dyrbye L, Fagan MJ, Ferenchick G, et al. The art of bedside rounds: a multi-center qualitative study of strategies used by experienced bedside teachers. J Gen Intern Med . 2013;28:412–420. doi: 10.1007/s11606-012-2259-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Alexanian JA, Kitto S, Rak KJ, Reeves S. Beyond the team: understanding interprofessional work in two North American ICUs. Crit Care Med . 2015;43:1880–1886. doi: 10.1097/CCM.0000000000001136. [DOI] [PubMed] [Google Scholar]
- 32. Rak KJ, Kahn JM, Linstrum K, Caplan EA, Argote L, Barnes B, et al. Enhancing implementation of complex critical care interventions through interprofessional education. ATS Scholar . 2021;2:370–385. doi: 10.34197/ats-scholar.2020-0169OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hennus MP, Young JQ, Hennessy M, Friedman KA, de Vries B, Hoff RG, et al. Supervision, interprofessional collaboration, and patient safety in intensive care units during the COVID-19 pandemic. ATS Scholar . 2021;2:397–414. doi: 10.34197/ats-scholar.2020-0165OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Cruess RL, Cruess SR, Steinert Y. Medicine as a community of practice: implications for medical education. Acad Med . 2018;93:185–191. doi: 10.1097/ACM.0000000000001826. [DOI] [PubMed] [Google Scholar]
- 35. Remtulla R, Hagana A, Houbby N, Ruparell K, Aojula N, Menon A, et al. Exploring the barriers and facilitators of psychological safety in primary care teams: a qualitative study. BMC Health Serv Res . 2021;21:269. doi: 10.1186/s12913-021-06232-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


