Abstract
Objectives:
Falls in hospitals pose a significant safety risk, leading to injuries, prolonged hospitalization, and lasting complications. This study explores the potential of augmented reality (AR) technology in healthcare facility design to mitigate fall risk.
Background:
Few studies have investigated the impact of hospital room layouts on falls due to the high cost of building physical prototypes. This study introduces an innovative approach using AR technology to advance methods for healthcare facility design efficiently.
Methods:
Ten healthy participants enrolled in this study to examine different hospital room designs in AR. Factors of interest included room configuration, door type, exit side of the bed, toilet placement, and the presence of IV equipment. AR trackers captured trajectories of the body as participants navigated through these AR hospital layouts, providing insights into user behavior and preferences.
Results:
Door type influenced the degree of backward and sideways movement, with the presence of an IV pole intensifying the interaction between door and room type, leading to increased sideways and backward motion. Participants displayed varying patterns of backward and sideways travel depending on the specific room configurations they encountered.
Conclusions:
AR can be an efficient and cost-effective method to modify room configurations to identify important design factors before conducting physical testing. The results of this study provide valuable insights into the effect of environmental factors on movement patterns in simulated hospital rooms. These results highlight the importance of considering environmental factors, such as the type of door and bathroom location, when designing healthcare facilities.
Keywords: fall prevention, evidence-based design, patient room, risk, augmented reality, built environment
Introduction
Falls pose a significant and preventable problem in healthcare settings (Callis, 2016; Hartholt et al., 2011). According to the Agency for Healthcare Research and Quality, an estimated 700,000 to 1 million falls occur annually in U.S. hospitals, with nearly one third experiencing minor injuries and a smaller proportion suffering from serious injuries like soft tissue wounds, fractures, or head trauma (Callis, 2016; Cameron et al., 2010; Chaeibakhsh et al., 2021; Hughes, 2008; Lusardi et al., 2017; Pati, Valipoor, Cloutier, et al., 2021; Phelan et al., 2015; Piatkowski et al., 2021; Spoelstra et al., 2012; Toye et al., 2019). The consequences of falls extend beyond immediate physical harm, leading to prolonged and costly hospital stays, increased healthcare expenses, and a decline in patients’ quality of life (Callis, 2016; Chaeibakhsh et al., 2021; Hartholt et al., 2011; Lusardi et al., 2017; Novin et al., 2021; Pati, Valipoor, Cloutier, et al., 2021; Pati, Valipoor, Lorusso, et al., 2021; Phelan et al., 2015; Selçuk, 2022; Toye et al., 2019; Zhao et al., 2019). Furthermore, falls can result in long-term disability that impairs patients’ independence often necessitating extensive rehabilitation (Pati, Valipoor, Lorusso, et al., 2021; Spoelstra et al., 2012). Given the far-reaching impact of falls, implementing effective strategies to minimize the occurrence of falls and enhance patient safety is a critical focus area in healthcare (Lusardi et al., 2017).
Several variables contribute to a patient’s fall risk, with the likelihood of falling being directly proportional to the number of risk factors present during an incident (Callis, 2016; Phelan et al., 2015; Zhao et al., 2019). These risk factors can be categorized as either intrinsic or extrinsic (Callis, 2016; Novin et al., 2021; Piatkowski et al., 2021). Intrinsic factors pertain to the patient’s characteristics (e.g., age, comorbidities, previous falls, gait, sensory impairments, musculoskeletal deficits, cognitive impairment; Callis, 2016; Lusardi et al., 2017; Novin et al., 2021; Pati, Valipoor, Cloutier, et al., 2021; Phelan et al., 2015; Spoelstra et al., 2012; Zhao et al., 2019). Extrinsic factors are associated with the hospital’s physical environment, medications, bathroom equipment, lighting, flooring, and footwear (Callis, 2016; Chaeibakhsh et al., 2021; Novin et al., 2021; Pati et al., 2009; Phelan et al., 2015; Selçuk, 2022; Spoelstra et al., 2012; Valipoor et al., 2020). While many fall-prevention strategies focus on patient factors, another strategy is to consider environmental factors that affect the risk of falling (Novin et al., 2021; Pati, Valipoor, Cloutier, et al., 2021; Pati, Valipoor, Lorusso, et al., 2021; Phelan et al., 2015; Selçuk, 2022; Valipoor et al., 2020). Environmental factors within hospital settings, including the layout and placement of objects, slip risk, and the force required for opening doors, significantly influence human motion and consequently impact fall risk (Callis, 2016; Chaeibakhsh et al., 2021; Novin et al., 2021; Pati, Valipoor, Cloutier, et al., 2021; Pati, Valipoor, Lorusso, et al., 2021; Selçuk, 2022). Cluttered spaces, inadequate lighting, and uneven flooring surfaces can impede proper navigation and increase the risk of trips and slips (Novin et al., 2021; Pati, Valipoor, Cloutier, et al., 2021; Pati, Valipoor, Lorusso, et al., 2021; Valipoor et al., 2020; Zhao et al., 2019). Therefore, designing hospital rooms and environments to minimize the risk of falling represents a key strategy for reducing fall risk (Novin et al., 2021; Selçuk, 2022).
Hospital settings present a distinct landscape for falls, particularly during patient transfers, walking from the bed to the restroom and within the restroom itself (Hitcho et al., 2004). Confined spaces, the presence of medical equipment and the active involvement of healthcare professionals are driving factors in these settings (Hitcho et al., 2004). While existing literature predominantly highlights forward falls, the dynamic environment of community living introduces the possibility of backward and sideways falls, influenced by distinct layouts and diverse activities (Crenshaw et al., 2017). Forward falls in hospitals are often associated with patients walking too fast or rushing toward a destination (Robinovitch et al., 2013). However, a backward loss of balance may be more problematic than a forward loss of balance; balance recovery during backward descent is more likely to result in a full fall to the ground (Hsiao & Robinovitch, 1997; Robinovitch et al., 2013). Additionally, sideways falls, especially from standing height, pose a substantial risk of hip fracture in the controlled environment of hospitals (Robinovitch et al., 2022; Robinovitch et al., 2013). Therefore, environmental factors may influence both the overall risk of falling and the risk of direction-specific falls.
Recognizing the significant impact of environmental factors on patient safety, healthcare organizations have increasingly focused on incorporating design elements that promote fall prevention (Chaeibakhsh et al., 2021; Novin et al., 2021). This approach involves a comprehensive evaluation of room layout, furniture arrangement, flooring surfaces, lighting conditions, and accessibility features (Chaeibakhsh et al., 2021; Novin et al., 2021). For example, strategically positioning furniture and equipment to facilitate unobstructed pathways can enhance patient mobility and reduce the potential for accidental tripping or collisions (Chaeibakhsh et al., 2021; Pati, Valipoor, Cloutier, et al., 2021; Pati, Valipoor, Lorusso, et al., 2021). Other design features, such as slip-resistant flooring materials, appropriate lighting levels throughout the facility, and handrails and grab bars in critical areas, further contribute to a safer environment (Chaeibakhsh et al., 2021; Novin et al., 2021; Pati, Valipoor, Cloutier, et al., 2021; Pati, Valipoor, Lorusso, et al., 2021; Selçuk, 2022; Valipoor et al., 2020).
Despite the existence of design guidelines addressing various environmental features within hospital rooms, such as object layout and placement, there remains a significant gap in empirical evidence to guide a safer arrangement of these elements (Novin et al., 2021; Pati, Valipoor, Lorusso, et al., 2021; Selçuk, 2022). The gap in empirical evidence can be attributed to several factors. First, conducting studies involving physical alterations to real-world hospital rooms is expensive, time-consuming, and often impractical. Further, constructing multiple, exploratory room layouts to alleviate these concerns requires substantial financial resources and presents logistical challenges, such as where the prototype rooms would be built and how to accommodate diverse patient populations. To date, these constraints have hindered the acquisition of comprehensive empirical evidence regarding the optimal layout of hospital rooms to minimize fall risk.
As an alternative to building physical iterations of every room layout, virtual reality (VR) technology using head-mounted displays (HMDs) offers a practical and efficient means to assess the impact of a variety of design factors on user behavior without the need for extensive physical alterations (Atwal et al., 2014; Pucher et al., 2014). Integrating core physical features such as beds, chairs, and equipment into a virtual environment through augmented reality (AR) may allow for investigations about how different room configurations influence user behaviors more effectively than VR alone. An augmented virtual environment creates a single configurable testing space with reduced cost compared to constructing multiple full-scale physical rooms. Further, the VR technology records positional data through the HMD and other body trackers, which may be useful in quantifying how design features influence patient movement and subsequent fall risk. While VR is increasingly applied in various healthcare settings, such as surgery training, it has also demonstrated remarkable utility in other medical applications as well. For instance, VR-based simulations have been widely employed for medical education and training, allowing medical professionals to practice surgical procedures in a risk-free virtual environment (Al-Hiyari & Jusoh, 2020; Jamal et al., 2023; Mao et al., 2021; Pulijala et al., 2018; Rogers et al., 2021; Suh et al., 2023). More recently, VR has been incorporated into the design process, sometimes as a result of restrictions resulting from COVID-19 (Jafarifiroozabadi et al., 2022; Jawed et al., 2021; Neo et al., 2021; Qi et al., 2022; Shultz & Jha, 2021; Wingler et al., 2020). Additionally, AR has emerged as a valuable tool in healthcare research, providing a bridge between virtual simulations and real-world environments (Piatkowski et al., 2021). AR systems merge elements of the physical and virtual environment, whereas VR systems immerse participants entirely in a virtual realm (Bin et al., 2020). An example of intermixed AR is in the surgical field, where AR can be used to provide supplementary data to the surgeon, such as segmented anatomy, with the data being augmented directly on the patient while the surgery is performed (Bin et al., 2020). In neuroscience, AR is leveraged to capture brain signals and understand the effects of conditions like brain loss or Alzheimer’s disease (Bin et al., 2020). Notably, AR innovations include a “neurogoggle” integrating video games and brain imaging for rehabilitating conditions like Parkinson’s disease and strokes (Cardin et al., 2016). Additionally, 360-degree cameras, serving as a form of “virtual contact,” are placed in diverse settings like schools, homes, and recreational areas, alleviating mental strain for children in hospitals and allowing them to stay connected with loved ones (Bin et al., 2020). In patient room design, AR technology offers an immersive exploration of environmental factors, enhancing efficiency in assessing interventions and addressing limitations associated with relying solely on VR technology (Piatkowski et al., 2021).
The goal of this study was to determine the feasibility of using AR within an iterative design process to examine the influence of certain environmental features and room layouts on patient behavior. Specifically, we created eight different room layouts by varying the location of the bathroom, the location of the toilet within the bathroom, and the type of door (sliding vs. swinging door) to examine how these critical design features influence locomotor behaviors associated with higher rates of falling, defined here as the distance traveled in forward, backward, and sideways directions. As a pilot study, a secondary goal of this research was to provide preliminary guidance on design features for future investigations within frail elderly populations.
Method
Subjects
Ten healthy participants (five males and five females) participated in this study approved by the University of Utah Institutional Review Board. Mean age, weight, and height of subjects were 26.2 ± 3.5 years, 160 ± 22.5 lbs (72.6 ± 10.2 kg), and 66.54 ± 4.13 inches (169 ± 10.5 cm), respectively. Participants were excluded if had a history of brain injuries, abnormal walking patterns, susceptibility to motion sickness, visual impairments, significant visual acuity deficits, known neurological or musculoskeletal disorders that interfered with mobility, or any self-reported medical conditions that could potentially interfere with their performance in the AR environment.
Data Collection and Analysis
In our study, we utilized six sources of tracking data to comprehensively analyze participants’ movements within the virtual environment and to capture both positional and rotational data. All data were recorded at 2 Hz due to software limitations. These sources included the headset, two hand controllers, a tracker positioned on the lumbar spine, and two trackers attached to the feet. It is worth noting that the presence of the VR hand controller did not interfere with the participants’ ability to grip the IV pole.
VIVE trackers were placed on the lumbar spine and dorsum of both feet. Each VIVE tracker had a battery life of approximately 3 hr and was recharged between sessions to ensure uninterrupted data collection. The back tracker (lumbar spine) was fastened using an adjustable belt, while strong adhesive tape was used to firmly secure the foot trackers (dorsum) to the participants’ shoes. Finally, we activated the trackers to synchronize seamlessly with the UNITY system, facilitating the process of data collection and subsequent analysis.
Room Design
Differentiation of physical and virtual environments.
In this section, we provide a detailed description of the physical objects introduced into the AR scenarios and clarify which elements were part of the physical environment and which were incorporated virtually.
Physical environment.
The experimental sessions were conducted in a room measuring 21′ × 28′ = 588 square feet with a desk area that is approximately 2.5′ × 6′ = 15 square feet for a total of 602 square feet. The AR computer system is positioned on a dedicated desk. A researcher, responsible for data monitoring and participant safety, was stationed at this desk throughout the sessions. The physical room, mirroring the virtual environment, comprised the bed, toilet/grab bar, and IV pole. These elements were present in the room where the study was conducted and served as tangible components for participants to interact with during the virtual experience.
Virtual environment.
The VR environment was developed using Unity 3D software (Unity.2019.4.31f1) and was experienced through an HTC Valve Index headset, which allowed participants to move around and interact with objects in the virtual space (Vatsa et al., 2021). Our VR environment consisted of eight hospital room variations, each with a distinct layout determined by the positioning of various objects, including a bed, chair, family sofa, toilet with grab bars, and sink. These rooms served as the backdrop for our study. We examined the significance of distinct headwall and footwall configurations (defined below), toilet location, and sliding and swinging doors. We also considered how patient egress from the sides of the bed affected movement through the space. The use of an IV pole was also integrated into the performance scenarios.
Patient Room Layouts
While there were many other configurations that could be tested, for study feasibility, the final choices were resolved through extensive discussion among the research team and feedback from the project’s advisory committee (AC) of leading healthcare architects. In a prior phase of AR testing, multiple room configurations were modeled, and the bathroom location on the footwall was preferred by the AC (Piatkowski et al., 2021). As a result, the footwall configuration was adapted to create a headwall layout (with the same bathroom). The team felt documenting any biomechanical changes associated with a head-wall and footwall configuration would be fundamental to address a gap in the literature to empirically establish the relationship between the bathroom-to-bed location and safety (e.g., stability, the risk of falls). The swing door and sliding door configuration were included due to the increasing trend for sliding doors for patient toilet rooms. The team felt there would be a significant contribution to the body of knowledge for patient room design with empirical evidence evaluating two predominant door types and measures of biomechanical stability to further inform decision-making beyond door cost and square footage. The toilet location in each layout was mirrored to evaluate whether a specific condition of movement performed by the AC would be replicated in the pilot study with naive subjects, as well as to evaluate whether the mirrored locations would result in turning differences that have been indicated in the literature as a risk for falls (Pati, Valipoor, Lorusso, et al., 2021).
Differentiated Visualization
Figures 1–4 illustrate immersive VR screenshots and spatial arrangements of different headwall and footwall configurations, inside and outside wall toilets, sliding and swinging doors, and close and far bed exit positions. Yellow highlights and arrows are incorporated to visually distinguish between the two, facilitating a clearer understanding of the distinct configurations.
Figure 1.

Immersive virtual reality screenshots of a footwall room configuration (left) and headwall room configuration (right). used in this study. The headwall room configuration features the bathroom positioned at the head (top) end of the bed, while the footwall room configuration (left) places the bathroom at the foot (bottom) end of the bed. The yellow rectangles serve to highlight and emphasize the notable differences between these rooms, allowing for a clearer visual understanding of the distinct Immersive virtual reality screenshots of a footwall room configuration (left) and headwall room configuration (right). used in this study. The headwall room configuration features the bathroom positioned at the head (top) end of the bed, while the footwall room configuration (left) places the bathroom at the foot (bottom) end of the bed. The yellow rectangles serve to highlight and emphasize the notable differences between these rooms, allowing for a clearer visual understanding of the distinct configurations.
Figure 4.

Differentiating far (left panel) and close (right panel) sides. By incorporating the yellow arrows, we effectively draw attention to the starting point of participants.
Figure 5 serves the same purpose as in Figures 1–4, effectively drawing attention to key features and distinguishing between physical and virtual components. This consistent visual differentiation enhances the overall clarity and aids in comprehending the distinctions between the real and virtual aspects of the room configurations, contributing to a more comprehensive understanding of the study setup.
Figure 5.
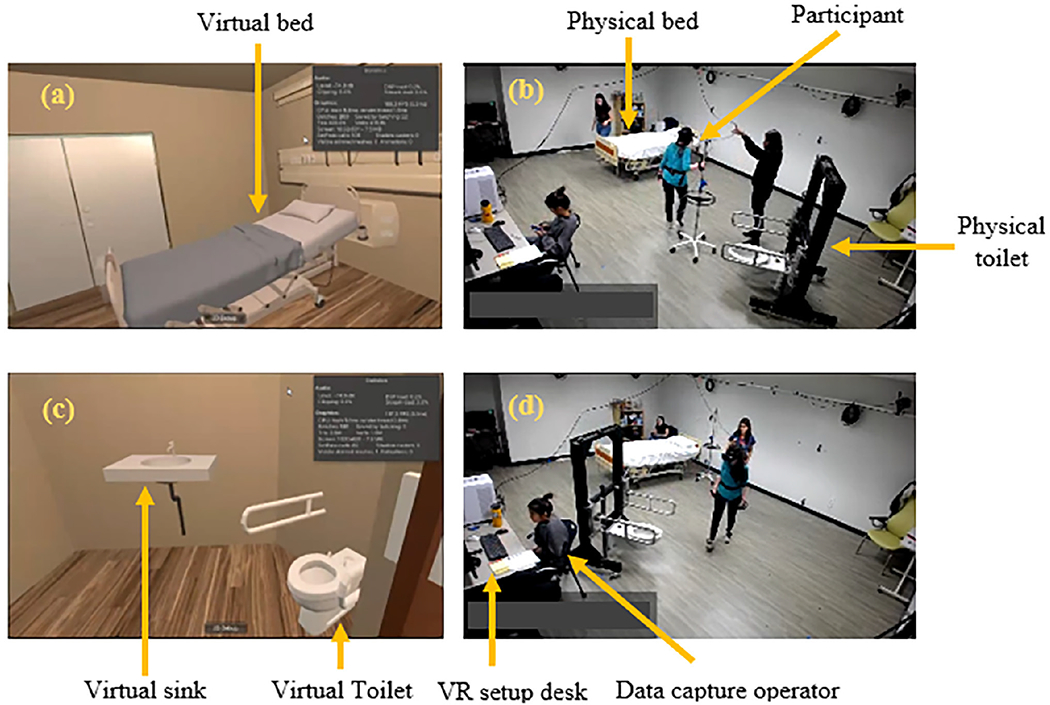
Visual representation of participant perspectives in physical and virtual environments. (a) Depicts the participant’s view in the virtual room, featuring a clear shot of the bed and the participant walking toward it. (b) Represents the participant’s presence in the physical room, highlighting the physical bed and toilet. (c) Illustrates the participant’s perspective of the virtual bathroom. (d) Displays the participant’s movement toward the physical bathroom in the physical room. Panels (a) and (c) showcase views corresponding to panels (b) and (d), respectively.
Headwall and footwall configurations: We studied two distinct room types in our study, headwall and footwall configurations (Figure 1), determined by the positioning of the bathroom relative to the bed. In the headwall configuration, the bathroom is located at the head (top) end of the bed, while in the footwall configuration, the bathroom is positioned at the foot (bottom) end of the bed.
Inside and outside wall toilets: We incorporated two distinct toilet placements within the bathroom space—on the inside and outside (exterior) walls of the bathroom (Figure 2). In the headwall condition, the inside wall toilet was positioned closer to the bed, within the bathroom space itself. The locations were investigated to validate the results of a prior study investigating architects’ perceptions of the designs (Piatkowski et al., 2021).
Sliding and swinging door: We incorporated two different types of doors for the bathroom. a sliding door and a swinging door (Figure 3). These objects were implemented in the AR environment. To interact with these virtual doors, a hand-held controller was used. Participants could use the controller to simulate actions like pushing or pulling the doors, depending on the type of door. This approach allowed us to assess how participants’ interactions with the doors influenced their navigation and experience within the AR environment, but did not mimic the force requirements of moving a physical object with inertia. The sliding door allowed for lateral opening and closing of the bathroom entrance; the swinging door featured an outward opening, swinging away from the bathroom space. These variations in door types provided participants with different experiences when interacting with the bathroom entrance, simulating realistic scenarios commonly encountered in healthcare settings.
Close and far bed exit positions: In our study, the exit location from the bed within the AR environment was based on whether the IV was placed in the participant’s right or left arm. To establish a clear distinction, we designated the side of the bed that is closer to the bathroom as the close side, and the side that is farther away as the far side (Figure 4). This designation allowed for consistent referencing and accurate analysis of participant movements and interactions in relation to the bed and the bathroom within the virtual environment. By differentiating between the close and far sides of the bed, we were able to assess specific behaviors and spatial relationships that may have an impact on participant performance and navigation during the simulated tasks.
Figure 2.

Spatial arrangement of inside (left) and outside (right) toilets. The inside toilet is positioned closer to the bed within the bathroom space, while the outside toilet is further away from the bed. The yellow circles specify the locations of the toilets, highlighting their positions in relation to the surrounding elements. Additionally, the inside and outside walls of the bathroom are tagged.
Figure 3.

Bathroom Door Types. The figure showcases the two different door types implemented for the bathroom within the headwall and footwall room configurations. The sliding door smoothly glides along a track, allowing lateral opening and closing of the bathroom entrance. In contrast, the swinging door features an outward opening mechanism, swinging away from the bathroom space. The yellow arrows help to visually distinguish between the two door types.
To enhance the realism of the VR experience, the room in which the study was conducted contained physical objects including the bed, toilet, toilet grab bars, and IV pole (Figure 5).
Trials
During the study, each participant completed 64 trials that were randomized based on several factors: room configuration (four configurations: headwall bathroom vs. footwall bathroom and inside wall toilet vs. outside wall toilet), door type (swing or sliding), starting side of the bed (close or far), and presence of an IV pole (IV or no IV). The 64 trials were divided into two sets (32 in each set) with one trial of each condition per set presented in a randomized order.
Before commencing the trials, participants were given the opportunity to explore a randomly assigned room within the VR environment. This acclimation period allowed the participants to familiarize themselves with the virtual space and gain an understanding of the room’s layout and features. Additionally, to minimize any potential challenges or confusion related to interacting with different door types, subjects were given sufficient time to become familiar with how to use the hand-held controller to operate the sliding and swinging doors before starting the trials. This preliminary familiarization aimed to promote a smoother and more seamless experience during the actual trial sessions.
At the beginning of each trial, participants were instructed to sit on the bed and stand up, assuming a T-pose position where their arms were extended horizontally to the sides and their legs were straightened, resembling the shape of the letter T. This T-pose position served as a reference point for data calibration and ensured consistent starting positions across trials. After holding the T-pose for a brief moment, participants then sat back on the bed and commenced the trial by standing up and following the instructions to walk toward the bathroom, sit on the toilet, simulate hand washing at a lavatory, and walk back to the bed. It is important to note that participants were explicitly instructed not to close the bathroom door when returning to the bed, allowing for an unrestricted flow of movement during the trial. Additionally, participants were informed that they were not required to return to the same side of the bed they started from, providing flexibility in their movements within the virtual environment.
Throughout the study, participants were instructed to hold the IV pole, which featured a center-mounted tracker enabling real-time tracking of its position and movements within the virtual environment. To enhance the realism of the IV pole interaction, a tube was securely attached to participants’ arm using a wristband. This tube served as a physical representation of the limitations imposed by an actual IV pole in the real world, simulating the associated physical interaction and constraints within the AR environment. The wristband ensured a stable and comfortable attachment of the tube throughout the study session, allowing participants to experience a more authentic IV pole manipulation experience. Furthermore, to align with the specific trial conditions, the attachment of the IV pole varied based on the side of the bed. In trials starting from the far side of the bed, the IV tube was attached to the participant’s right arm. Conversely, in trials starting from the close side of the bed, the IV tube was attached to the participant’s left arm.
Participants were instructed to walk at their own pace and were not required to finish the trials within a limited time. They were encouraged to mention any discomfort or need for a break during the study. By incorporating these instructions and adaptations, we aimed to create a realistic and participant-centered environment for the study of IV pole handling within the VR setting.
Data Processing Component
Kinematic data from the lumbar-mounted body tracker was used to quantify the influence of the different design variables on movement and behaviors associated with falls or exposure to falls: total time (exposure to falls), time in bathroom (exposure to high-fall risk area), distance traveled in backward direction (high fall-risk behavior), and distance traveled in the sideways direction (high fall-risk behavior). The total trial time was defined as the duration from the start of the trial (standing from the bed after the T-pose) to the end of the trial (sitting back on the bed). The total time spent in the bathroom was defined as the duration starting from the time the subject touched the door handle to open the door and entered the bathroom, and ending when they touched the door handle from inside the bathroom.
Variables were selected based on their significance to exposure and subsequent risk of fall-related injury. Total time, path length, and time in bathroom were chosen as variables associated with exposure to falling—larger values indicate patients would be standing and moving for longer/farther, which would increase the exposure to the risk of falling. Distance backward and sideways were chosen as direction-specific exposure measures related to fall-related injury (e.g., hip fracture) and failed balance recover (backward falls). Total trial time and total path length represent the overall duration and distance of participants’ activities and may indicate prolonged exposure to potential fall hazards. Time in the bathroom was selected based on the significance of specific areas like bathrooms in contributing to fall incidents (Abreu et al., 2012; Pati et al., 2021; Vaccari et al., 2014). The selection of distance backward and distance sideways was based on evidence that specific directional movements contribute to risk for falls and subsequent injuries (Yang et al., 2020). Specifically, distance backward was motivated because losses of balance in the backward direction are more difficult to recover from to prevent a fall (Hsiao & Robinovitch, 1997). Distance sideways was motivated because falls initially directed sideways from standing height pose a substantial risk of hip fracture (Yang et al., 2020). To yield continuous positional data from 2 Hz data, positional data were resampled to 10 Hz and subsequently low-pass filtered using a fourth order, 1 Hz Butterworth filter. Then, we calculated the instantaneous velocity vector v from the filtered positional data using the central difference method, and calculated the angle θ between the instantaneous orientation and instantaneous velocity, v. Forward, sideways, and backward motion was categorized using this angle θ (forward: ; sideways: ; and backward: ; see Figure 6).
Figure 6.
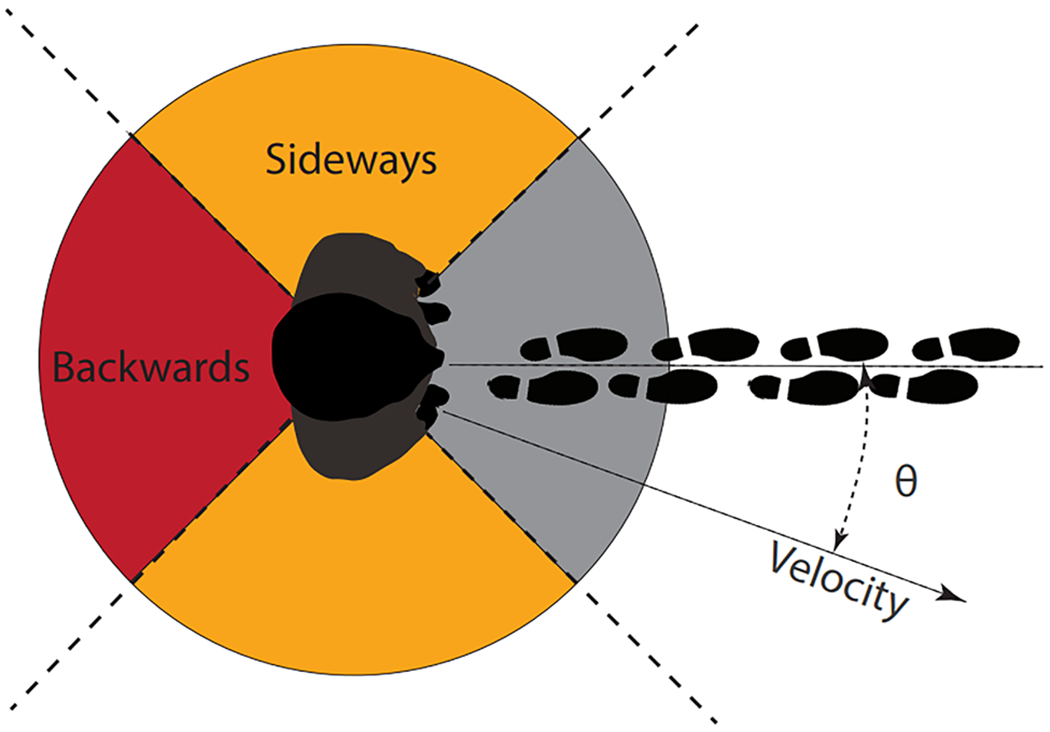
Visualization of Angles θ and Motion Areas. The plot depicts the angles θ between the instantaneous orientation and velocity of the lumbar tracker, showcasing the forward (− π/4 < θ < π/4), sideways (π/4 < |θ| < 3 π/4), and backward (3 π/4 < |θ| < π) motion areas. This graphical representation offers insights into participants’ movement patterns within the virtual environment.
Statistical Analysis Component
In our study, we utilized General Linear Mixed-Effect Regression Models to analyze each outcome. General Linear Mixed-Effect Regression Models, often referred to as Mixed Models, are a statistical method suitable for analyzing nested and multiple measured data (Jiang & Nguyen, 2007). In this context, the term “mixed” indicates the incorporation of both fixed effects (factors with specific levels we are studying) and random effects (variability that is not of primary interest but needs to be accounted for; Jiang & Nguyen, 2007). Our model incorporated fixed effects, including room configuration (head-wall vs. footwall), toilet location (inside vs. outside wall), door type (slide vs. swing), exit side of the bed (far vs. close), presence of an IV pole (yes vs. no), and set number (first vs. second). Two-way interactions (Room × Door, Room × IV Pole, and Door × IV Pole) were introduced to the model to capture potential combined effects. The statistical significance of these interactions was assessed against an α level set to .05, and nonsignificant interaction terms were excluded from the final model before presenting the results. Restricted maximum likelihood (REML) was employed for estimation within these models. REML is a robust method that provides unbiased estimates of variance components, a crucial aspect in understanding the variability within our data (Jiang & Nguyen, 2007). Participants were treated as random effects using random intercepts, acknowledging and accounting for individual differences that may impact the observed outcomes. This approach enhances the validity of our statistical analysis and ensures a more accurate representation of the relationships between the studied factors and outcomes.
Results
Total Trial Time
Overall, the mixed-effects model analysis revealed significant associations between several fixed effects and the total trial time, our primary dependent variable. Longer trial durations were observed in swing door configurations compared to slide door configurations (p = .019), in trials with an IV pole compared to without an IV pole (p < .001; Figure 7). The side of the bed from which the trial originated significantly influenced trial times (p < .001). Trials starting from the far side of the bed took more time to be completed compared to those that started from the close side of the bed. Also, participants took longer to complete the first set of trials, and as they progressed to subsequent sets, the trial times decreased, indicating a learning effect (p < .001).
Figure 7.
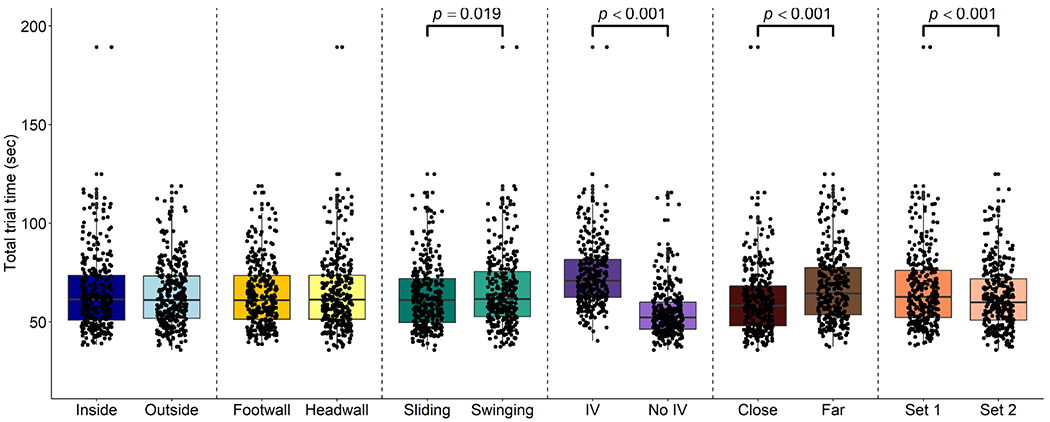
Box and jitter plots for total trial time for each set of factors. Different factors (e.g., door type) are illustrated in different colors, with shading indicating different levels within a factor (e.g., sliding verses swinging door). Total trial time was influenced by Door type, IV pole presence, bed side, and set number, which exerted significant influence on the results, as indicated by the p-values and brackets. Each dot on the box plots represents one trial.
Total Path Length
The fixed effects modeling revealed significant effects on the dependent variable, total path length, for various factors (Figure 8). Notably, the inside/outside wall orientation of the toilet influenced the total path length, with participants showing longer path lengths for bathrooms with an inside wall configuration compared to an outside wall configuration (p < .001). Comparing the door configurations, participants took longer to traverse the bathroom with a swing door compared to a sliding door (p < .001). The presence of an IV pole also had a substantial impact on the total path length, with participants taking longer paths when an IV pole was present compared to visits without an IV pole (p < .001). Furthermore, the side of the bed from which participants started their trial affected the total path length, with participants taking longer path lengths when starting from the far side compared to the close side of the bed (p < .001). Additionally, the set number had a notable effect on the total path length, indicating a learning effect as participants exhibited different path lengths across different sets of visits (p = .03).
Figure 8.
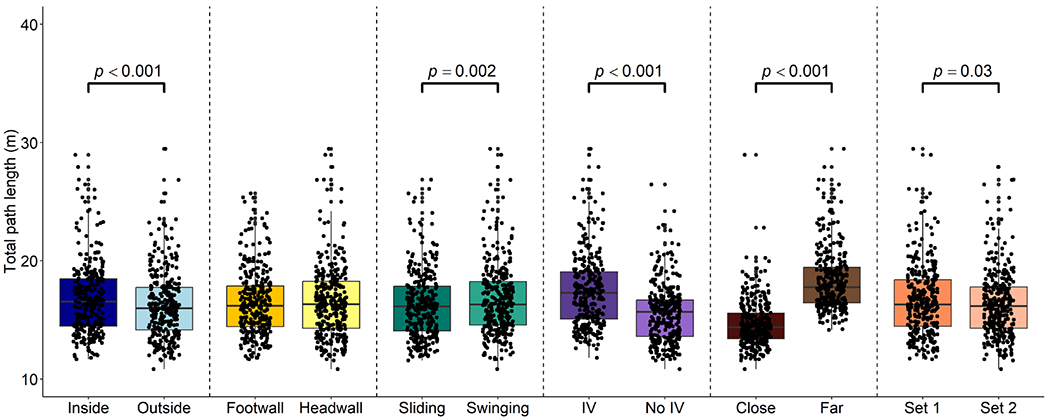
Box and jitter plots depict total path length across various sets of factors. Distinct factors, such as door type, are visually distinguished by unique colors, while different shading patterns within a factor group, like sliding versus swinging doors, indicate various levels. The factors including toilet position, door type, IV pole presence, side of the bed, and set number were all associated with increased total path length. Significant factors are indicated with p-values and brackets. Each dot represents a single trial.
Time in Bathroom
The analysis using a mixed-effects model revealed significant associations between several fixed effects and the duration of time spent in the bathroom, our primary dependent variable (Figure 9). There was a significant difference in the time spent in the bathroom based on the door configuration (p = .005). Specifically, participants took longer to use the bathroom when it had a swing door compared to a sliding door. Participants spent more time in the bathroom when an IV pole was present compared to visits without an IV pole (p < .001). Additionally, participants tended to spend different amounts of time in the bathroom as they progressed through subsequent sets, suggesting a learning effect (p < .001).
Figure 9.
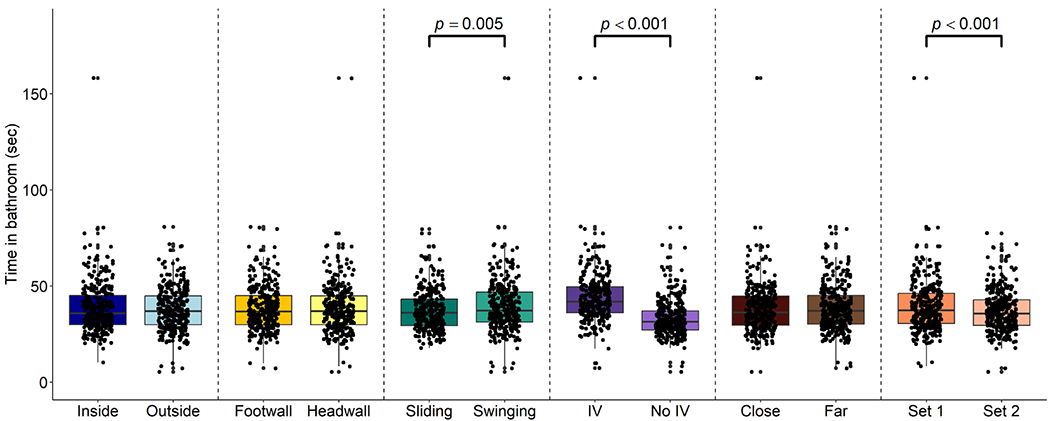
Total time in the bathroom for each combination of factors are presented in box and jitter plots. Each factor, like door type, is represented by a different color, while within-factor variations, such as sliding and swinging door options, are highlighted with varying shading. The door type, IV pole presence, and set number all had a significant impact on the time spent in the bathroom, as indicated by the p-values and brackets. Each dot represents a single trial.
Forward and Backward Motion
Total distance backward.
The fixed effects analysis tests revealed significant effects on the dependent variable, total distance backward, for several factors (Figure 10). Among them, the footwall/head-wall configuration showed a significant impact, with participants exhibiting more backward movement distances (p = .003). Specifically, participants displayed increased backward movement when in the footwall configuration. Additionally, the type of door (p < .001) and the presence of an IV pole (p < .001) also had highly significant effects, indicating their significant influence on participants’ total distance backward. Specifically, participants displayed more backward movement when using a swing door compared to a sliding door (p <.001). The interaction between door type and the presence of an IV pole was also highly significant (p < .001), suggesting their combined impact on participants’ backward movement behavior.
Figure 10.
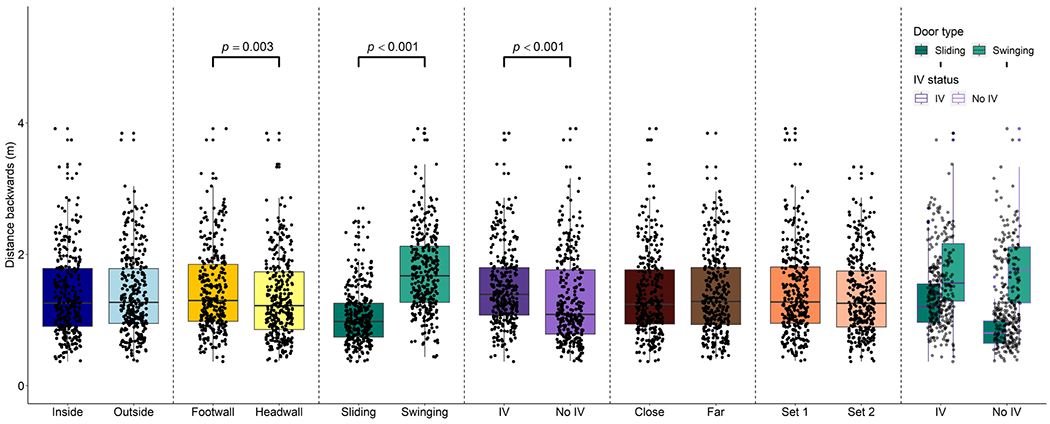
Box and jitter plots were generated to illustrate the distribution of distance backwards across distinct sets of factors. Each factor, such as door type, is assigned a unique color for visual differentiation, and shading is utilized to indicate specific factor levels, such as sliding and swinging doors. The room configuration, door type, IV pole presence increase the distance traveling backwards, as indicated by the p-values and brackets. Also, the interaction between IV pole and door type can push participants to move more backwards, with each dot representing an individual trial.
Total distance sideways.
The fixed effects analysis revealed significant effects on the dependent variable, total distance sideways (Figure 11). The arrangement of the foot-wall/head-wall room demonstrated a significant effect (p < 0.001), indicating that the footwall configuration caused increased sideways motion in participants during the trial. The door configuration significantly influenced the dependent variable. Specifically, the use of a swing door caused more sideways motion compared to a sliding door (p < .001). Additionally, the presence of an IV pole resulted in increased sideways motion (p < .001). Participants exhibited increased sideways motion during Set 1 (p = .006). The interaction between the foot-wall/head-wall room and door type was also significant (p < .001), indicating that the combined effect of these factors significantly impacted participants’ sideways movement behavior. Specifically, participants exhibited increased sideways motion when encountering the swing door in the footwall configuration, compared to other combinations of door types and room orientations.
Figure 11.
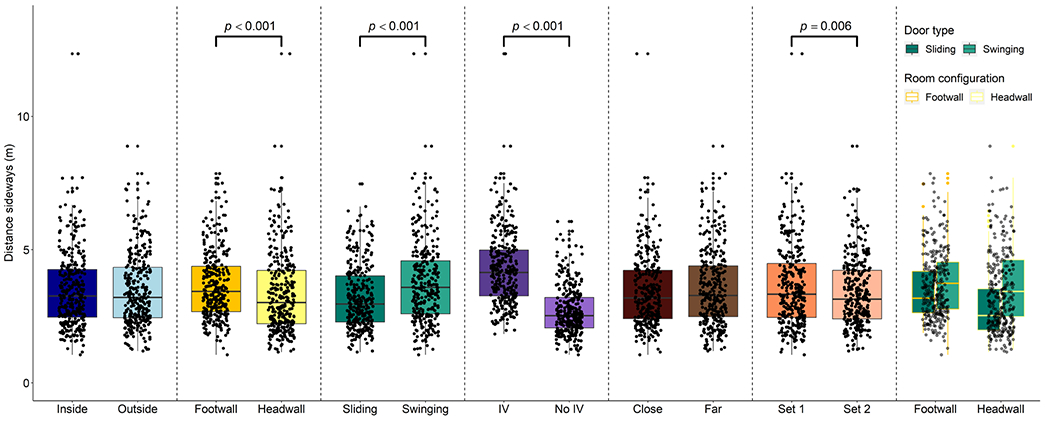
These box and jitter plots serve as visual representations of distance sideways distributions across multiple factor combinations. Each factor, such as door type, is allocated a unique color for clear differentiation, with shading employed to denote specific factor levels, such as sliding and swinging doors. The room configuration, door type, IV pole presence and set number exhibited increased sideways motions, as highlighted by the p-values and brackets. The interaction between room configuration and door type affected sideways traveling, with each dot representing an individual trial.
We have summarized all the pertinent results in Table 1, offering a clear overview of significant factors influencing trial time, path length, time in the bathroom, distance backward, and distance sideways. The table provides a concise representation, complementing the detailed insights conveyed by the figures.
Table 1.
The Table Provides a Detailed Summary of Significant Findings Related to Trial Time, Path Length, Time in the Bathroom, Distance Backward, and Distance Sideways Based on Various Influencing Factors. a
| Trial Time |
Path Length |
Time in Bathroom |
Distance Backward |
Distance Sideways |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Factors | β | SE | p | β | SE | p | β | SE | p | β | SE | p | β | SE | p |
| Toilet location | 0.645 | .791 | .415 | 0.515 | .124 | <.001 | 0.550 | .619 | .375 | −.010 | .037 | .778 | −0.013 | .071 | .853 |
| Room configuration | −0.742 | .791 | .348 | −0.058 | .124 | .639 | 0.295 | .619 | .633 | .111 | .037 | .003 | 0.096 | .100 | <.001 |
| Door type | −1.858 | .791 | .019 | −0.377 | .124 | .002 | −1.746 | .619 | .005 | −.929 | .052 | <.001 | −0.777 | .100 | <.001 |
| IV status | 18.711 | .791 | <.001 | 1.920 | .124 | <.001 | 10.393 | .619 | <.001 | −.062 | .052 | <.001 | 1.543 | .071 | <0.001 |
| Exit side of the bed | −7.306 | .791 | <.001 | −3.720 | .124 | <.001 | −0.440 | .619 | .478 | −.028 | .037 | 0.443 | −0.137 | .071 | .052 |
| Set number | 3.081 | .791 | <.001 | 0.269 | .124 | .030 | 2.052 | .619 | <.001 | .044 | .037 | 0.240 | 0.194 | .071 | .006 |
| Door Type × IV Pole | .520 | .074 | <0.001 | ||||||||||||
| Room Configuration× Door Type | 0.480 | .141 | <.001 | ||||||||||||
The beta coefficients (β), standard errors (SE), and p values are reported for each comparison. Reference levels for each variable were established as follows: outboard for toilet location, headwall for room configuration, swinging door for doortype, no IV for IV pole, right side of the bed for exit side of the bed position, and Set 2 for set number. Noteworthy interactions between door type and IV pole, as well as room configuration and door type, are also presented, contributing to a thorough understanding of the observed dynamics.
Discussion
We utilized AR technology to assess how specific environmental design elements might affect patient behavior and fall risk. This innovative approach offers insights into fall risk without the need for extensive physical room alterations, providing a promising step toward enhancing patient safety in healthcare environments. In addition to investigating the impact of various design factors on user behavior within an AR hospital room, another goal of this study is to provide recommendations for the design of physical rooms to test frail elderly subjects. While conclusions about specific effects should be made cautiously, several effects warrant discussion and further investigation as they may have clinical relevance.
The most dominant factor in our models for every outcome was the presence of an IV pole. An IV pole likely served as a constant, moving obstacle that, because of its nature, participants needed to continuously navigate around, and move with them (Pati, Valipoor, Cloutier, et al., 2021). Our results showing that the presence of an IV pole led to increased backward and sideways movement suggests IV poles likely increase fall risk in these directions (Novin et al., 2021). This finding underscores the need for healthcare organizations to prioritize a stable IV pole selection, acknowledging their ecological relevance in hospital settings. While these results suggest that IV poles elicit differences in patient movement (Pati, Valipoor, Cloutier, et al., 2021), these results have more impact when considering future studies; it is more crucial to ensure that future investigations of patient behaviors and mobility in hospital settings include an IV pole when relevant. This approach aligns with the ecological context of hospital settings, where IV poles are ubiquitous and often integral to patient care.
A second factor that warrants further investigation is the door type (Novin et al., 2021; Pati, Valipoor, Lorusso, et al., 2021). We observed that participants exhibited different movement patterns depending on whether the room had a swinging door or a sliding door. Our results suggest that sliding doors may alter movements in a beneficial way (e.g., minimizing sideways and backward motion). However, definitive conclusions about the impact of door type require further research using physical doors and real patient populations, especially those of older age that may be at a higher risk of falls.
Another finding of this study was that the bathroom orientation affects participant behaviors that may relate to falling (Novin et al., 2021; Pati, Valipoor, Lorusso, et al., 2021). Specifically, the footwall configuration led to increased sideways motion during the trials compared to the headwall orientation. This finding contradicted our expectations that participants would travel more safely in rooms where they had a clear line-of-sight from the bed to the bathroom (i.e., the footwall configuration). While the increased sideways and backward motion in the Footwall condition contradicts this expectation, the cause remains unclear. Speculatively, increased sideways and backward motion in the Footwall configuration may be due to the participants’ path toward the bathroom relative to the motion of the door. In the footwall configuration, the motion of the door—both swinging and sliding—occurs toward the back-right oblique plane (~120°) of the participants’ straight-line path from the bed to the bathroom. In the headwall configuration, the motion of the door occurs in the front-right oblique plane (~30°). This difference in the articulation plane of the door may have caused more backward and sideways steps to open the door. However, further research should explore this finding using physical doors and more in-depth biomechanical analyses.
In our study, the inside wall toilet configuration was associated with longer path lengths traveled by patients. However, it’s essential to note that this longer path length did not significantly affect other measured factors, such as total trial time, time spent in the bathroom, or total distances traveled backward or sideways that may be more associated with the risk of falls. Thus, in this study, the location of the bathroom appears to be more significant than the location of the toilet within the bathroom to patient behaviors and possible fall risk.
Patients required more time to complete trials when initiating from the side of the bed, which was situated farther from the bathroom in contrast to the close side. Furthermore, commencing trials from the far side of the bed resulted in patients covering greater total distances in forward, backward, and sideways movements. Intuitively, patients who exit the bed on the side opposite of the bathroom can be expected to travel longer distances, navigate more obstacles, and potentially experience increased risks for falls. Participants also demonstrated varying movement patterns across different sets of trials, indicating a learning effect (Cuttler et al., 2017; Morris & O’Riordan, 2017). Similar to supporting literature that identifies unfamiliar environments as a risk, our results suggest that patients may also acclimate to their environment and may adopt behaviors that reduce fall risk with increasing familiarity. However, it is unclear whether similar adaptation, or the rate of adaptation, is a function of the AR environment.
Additional limitations of this study include data collection a rate of 2 Hz, which was used in an earlier testing phase of the project and was due to processing capabilities associated with processor shortages during COVID-19. The capture rate did not allow for the detailed analysis of individual steps. However, it allowed for a feasible approach for data analysis of directional motion (e.g., forward, backward, and sideways motion presented here). Further, as indicated, the results establish recommendations for the study of frail elderly subjects, rather than guiding specific decisions about room design for an aging population in acute care environments. Another limitation of this study was the focus on factors that are above the floor surface. These factors (e.g., interactions with the door) are mostly likely to alter one’s likelihood of falling due to weight shifting (Robinovitch et al., 2013). However, surface-related factors, like the coefficient of friction of the floor, potential for tripping hazards, and the interface between shoes, socks, or barefoot walking and the floor may influence the risk of falls, particularly trips and slips, in hospital rooms. Since this study was focused on design factors related to the room configuration, we are unable to make conclusions about these potential fall hazards.
Conclusion
Overall, our innovative approach presents an efficient and cost-effective method for gaining critical insights into fall risk within healthcare environments. AR technology can effectively reduce part of the burden from resource-intensive physical room alterations, saving time and financial resources. Notably, AR may not be able to completely eliminate the need for physical iterations of design due to inherent limitations of the interactions with objects. For example, physical aspects like door operation, patient populations that may not tolerate AR, biomechanical measures, and interactions with walls and other environments that may not be physically represented are factors that may still require physical assessment. Additionally, acclimation to the virtual environment may not fully replicate real-world experiences. Despite these limitations, AR offers valuable tool for initial testing and exploration in the field of healthcare room design, paving the way for more targeted and cost-effective physical alterations and improvements.
By bridging the gap between AR simulations and real-world environments, these results provide evidence for healthcare professionals, architects, and designers that AR-based strategies can be implemented to study the interactions between patients and their environment, including behaviors that may lead to falls. Ultimately, knowledge gained from the AR simulations may generate preliminary, actionable recommendations that may have a positive impact on patient outcomes and contribute to the overall improvement of healthcare facilities. The findings of this pilot study will also be used to inform decisions for a physical mockup that will be used to evaluate features as used by frail elderly participants.
Implications for Practice.
AR technology can effectively reduce part of the burden from resource-intensive physical room alterations, saving time and financial resources.
Integrating core physical features into a virtual environment through (AR) may allow for investigations about how different room configurations influence user behaviors more effectively than VR alone.
Preliminary testing suggests that sliding doors may alter movements in a beneficial way (e.g., minimizing sideways and backward motion) as compared to swinging doors.
Differences between a headwall and footwall bathroom location remain inconclusive based on the results of this pilot study.
Results suggesting IV poles likely increase fall-risk underscore the need for healthcare organizations to prioritize a stable IV pole selection.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was funded under grant number 1R18HS025606 from the Agency for Healthcare Research and Quality (AHRQ), U.S. Department of Health and Human Services (HHS).
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Abreu C, Mendes A, Monteiro J, & Santos FR (2012). Falls in hospital settings: a longitudinal study. Revista latino-americana de enfermagem, 20, 597–603. [DOI] [PubMed] [Google Scholar]
- Al-Hiyari N, & Jusoh S. (2020). The current trends of virtual reality applications in medical education [Conference session]. 2020 12th International Conference on Electronics, Computers and Artificial Intelligence (ECAI), IEEE, Bucharest, Romania, June 25–27, 2020. 10.1109/ECAI50035.2020.9223158 [DOI] [Google Scholar]
- Atwal A, Money A, & Harvey M (2014). Occupational therapists’ views on using a virtual reality interior design application within the pre-discharge home visit process. Journal of Medical Internet Research, 16(12), e283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bin S, Masood S, & Jung Y (2020). Virtual and augmented reality in medicine. In Biomedical information technology (pp. 673–686). Elsevier. [Google Scholar]
- Callis N (2016). Falls prevention: Identification of predictive fall risk factors. Applied Nursing Research, 29, 53–58. [DOI] [PubMed] [Google Scholar]
- Cameron ID, Murray GR, Gillespie LD, Robertson MC, Hill KD, Cumming RG, & Kerse N (2010). Interventions for preventing falls in older people in nursing care facilities and hospitals. Cochrane Database of Systematic Reviews, 9(9), CD005465. [DOI] [PubMed] [Google Scholar]
- Cardin S, Ogden H, Perez-Marcos D, Williams J, Ohno T, & Tadi T (2016). Neurogoggles for multimodal augmented reality. Proceedings of the 7th Augmented Human International Conference 2016, Geneva, Switzerland, February 25–27, 2016. [Google Scholar]
- Chaeibakhsh S, Novin RS, Hermans T, Merryweather A, & Kuntz A (2021). Optimizing hospital room layout to reduce the risk of patient falls. arXiv preprint arXiv:2101.03210. 10.48550/arXiv.2101.03210 [DOI] [Google Scholar]
- Crenshaw JR, Bernhardt KA, Achenbach SJ, Atkinson EJ, Khosla S, Kaufman KR, & Amin S (2017). The circumstances, orientations, and impact locations of falls in community-dwelling older women. Archives of Gerontology and Geriatrics, 73, 240–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuttler SJ, Barr-Walker J, & Cuttler L (2017). Reducing medical-surgical inpatient falls and injuries with videos, icons and alarms. BMJ Open Quality, 6(2), e000119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartholt KA, van Beeck EF, Polinder S, van der Velde N, van Lieshout EM, Panneman MJ, van der Cammen TJ, & Patka P (2011). Societal consequences of falls in the older population: Injuries, healthcare costs, and long-term reduced quality of life. Journal of Trauma and Acute Care Surgery, 71(3), 748–753. [DOI] [PubMed] [Google Scholar]
- Hitcho EB, Krauss MJ, Birge S, Claiborne Dunagan W, Fischer I, Johnson S, Nast PA, Costantinou E, & Fraser VJ (2004). Characteristics and circumstances of falls in a hospital setting: A prospective analysis. Journal of General Internal Medicine, 19(7), 732–739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsiao ET, & Robinovitch SN (1997). Common protective movements govern unexpected falls from standing height. Journal of Biomechanics, 31(1), 1–9. [DOI] [PubMed] [Google Scholar]
- Hughes R (2008). Patient safety and quality: An evidence-based handbook for nurses. AHRQ. [PubMed] [Google Scholar]
- Jafarifiroozabadi R, Joshi R, Joseph A, & Wingler D (2022). Perceived usability of seating in an outpatient waiting area: A combined approach utilizing virtual reality and actual seating prototypes. Health Environments Research & Design Journal, 15(2), 248–261. [DOI] [PubMed] [Google Scholar]
- Jamal SA, Khan A, Shah S, Siddiqui SW, & Khan S (2023). Smart learning: An interactive dissection simulator for medical students through virtual reality. Research Square. 10.21203/rs.3.rs-3152538/v1 [DOI] [Google Scholar]
- Jawed YT, Golovyan D, Lopez D, Khan SH, Wang S, Freund C, Imran S, Hameed UB, Smith JP, & Kok L (2021). Feasibility of a virtual reality intervention in the intensive care unit. Heart & Lung, 50(6), 748–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang J, & Nguyen T (2007). Linear and generalized linear mixed models and their applications (Vol. 1). Springer. [Google Scholar]
- Lusardi MM, Fritz S, Middleton A, Allison L, Wingood M, Phillips E, Criss M, Verma S, Osborne J, & Chui KK (2017). Determining risk of falls in community dwelling older adults: A systematic review and meta-analysis using posttest probability. Journal of Geriatric Physical Therapy, 40(1), 1–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao RQ, Lan L, Kay J, Lohre R, Ayeni OR, & Goel DP (2021). Immersive virtual reality for surgical training: A systematic review. Journal of Surgical Research, 268, 40–58. [DOI] [PubMed] [Google Scholar]
- Morris R, & O’Riordan S (2017). Prevention of falls in hospital. Clinical Medicine, 17(4), 360–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neo JRJ, Won AS, & Shepley MM (2021). Designing immersive virtual environments for human behavior research. Frontiers in Virtual Reality, 2, 603750. [Google Scholar]
- Novin RS, Taylor E, Hermans T, & Merryweather A (2021). Development of a novel computational model for evaluating fall risk in patient room design. Health Environments Research & Design Journal, 14(2), 350–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pati D, Harvey TE Jr, Reyers E, Evans J, Waggener L, Serrano M, Saucier R, & Nagle T (2009). A multidimensional framework for assessing patient room configurations. Health Environments Research & Design Journal, 2(2), 88–111. [DOI] [PubMed] [Google Scholar]
- Pati D, Valipoor S, Cloutier A, Yang J, Freier P, Harvey TE, & Lee J (2021). Physical design factors contributing to patient falls. Journal of Patient Safety, 17(3), e135–e142. [DOI] [PubMed] [Google Scholar]
- Pati D, Valipoor S, Lorusso L, Mihandoust S, Jamshidi S, Rane A, & Kazem-Zadeh M (2021). The impact of the built environment on patient falls in hospital rooms: An integrative review. Journal of Patient Safety, 17(4), 273–281. [DOI] [PubMed] [Google Scholar]
- Phelan EA, Mahoney JE, Voit JC, & Stevens JA (2015). Assessment and management of fall risk in primary care settings. Medical Clinics, 99(2), 281–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piatkowski M, Taylor E, Wong B, Taylor D, Foreman KB, & Merryweather A (2021). Designing a patient room as a fall protection strategy: The perspectives of healthcare design experts. International Journal of Environmental Research and Public Health, 18(16), 8769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pucher PH, Batrick N, Taylor D, Chaudery M, Cohen D, & Darzi A (2014). Virtual-world hospital simulation for real-world disaster response: Design and validation of a virtual reality simulator for mass casualty incident management. Journal of Trauma and Acute Care Surgery, 77(2), 315–321. [DOI] [PubMed] [Google Scholar]
- Pulijala Y, Ma M, Pears M, Peebles D, & Ayoub A (2018). Effectiveness of immersive virtual reality in surgical training—A randomized control trial. Journal ofOral and Maxillofacial Surgery, 76(5), 1065–1072. [DOI] [PubMed] [Google Scholar]
- Qi F, Lu Z, & Chen Y (2022). Investigating the influences of healthcare facility features on way-finding performance and associated stress using virtual reality. Health Environments Research & Design Journal, 15(4), 131–151. [DOI] [PubMed] [Google Scholar]
- Robinovitch SN, Dojnov A, Komisar V, Yang Y, Shishov N, Yu Y, Bercovitz I, Cusimano MD, Becker C, & Mackey DC (2022). Protective responses of older adults for avoiding injury during falls: Evidence from video capture of real-life falls in long-term care. Age and Ageing, 51(12), afac273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinovitch SN, Feldman F, Yang Y, Schonnop R, Leung PM, Sarraf T, Sims-Gould J, & Loughin M (2013). Video capture of the circumstances of falls in elderly people residing in longterm care: An observational study. The Lancet, 381(9860), 47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers MP, DeSantis AJ, Janjua H, Barry TM, & Kuo PC (2021). The future surgical training paradigm: Virtual reality and machine learning in surgical education. Surgery, 169(5), 1250–1252. [DOI] [PubMed] [Google Scholar]
- Selçuk E (2022). Evidence based design in healthcare facilities. Bilecik Şeyh Edebali Üniversitesi Fen Bilimleri Dergisi, 9(2), 1056–1076. [Google Scholar]
- Shultz J, & Jha R (2021). Using Virtual Reality (VR) mock-ups for evidence-based healthcare facility design decisions. International Journal of Environmental Research and Public Health, 18(21), 11250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoelstra SL, Given BA, & Given CW (2012). Fall prevention in hospitals: An integrative review. Clinical Nursing Research, 21(1), 92–112. [DOI] [PubMed] [Google Scholar]
- Suh I, McKinney T, & Siu K-C (2023). Current perspective of metaverse application in medical education, research and patient care. Virtual Worlds, 2(2), 115–128. [Google Scholar]
- Toye C, Slatyer S, Kitchen S, Ingram K, Bronson M, Edwards D, Van Schalkwyk W, Pienaar C, Wharton P, & Bharat C (2019). Bed moves, ward environment, staff perspectives and falls for older people with high falls risk in an acute hospital: A mixed methods study. Clinical Interventions in Aging, 14, 2223–2237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaccari É, Lenardt MH, Willi MH, Betiolli SE, & de Oliveira ES (2014). Safety of the hospital environment in terms of preventing falls on the part of the elderly: a descriptive study. Online Brazilian Journal of Nursing, 13(3), 271–281. [Google Scholar]
- Valipoor S, Pati D, Kazem-Zadeh M, Mihandoust S, & Mohammadigorji S (2020). Falls in older adults: A systematic review of literature on interior-scale elements of the built environment. Journal of Aging and Environment, 34(4), 351–374. [Google Scholar]
- Vatsa S, Taylor D, Chaeibakhsh S, Butter D, Novin RS, Taylor E, Foreman B, Wong B, & Merryweather A (2021). Using virtual reality to inform fall risk prevention in patient rooms [Conference session]. The 33rd Annual International Occupational Ergonomics and Safety Conference, September 16–17, 2021, pp. 1–6. https://web.archive.org/web/20230605133247/http://https://www.isoes.info/conferences/2021/Papers/isoes.2021_098.pdf [Google Scholar]
- Wingler D, Joseph A, Bayramzadeh S, & Robb A (2020). Using virtual reality to compare design alternatives using subjective and objective evaluation methods. Health Environments Research & Design Journal, 13(1), 129–144. [DOI] [PubMed] [Google Scholar]
- Yang Y, Komisar V, Shishov N, Lo B, Korall AM, Feldman F, & Robinovitch SN (2020). The effect of fall biomechanics on risk for hip fracture in older adults: a cohort study of video-captured falls in longterm care. Journal of bone and mineral research, 35(10), 1914–1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao YL, Bott M, He J, Kim H, Park SH, & Dunton N (2019). Evidence on fall and injurious fall prevention interventions in acute care hospitals. The Journal of Nursing Administration, 49(2), 86–92. [DOI] [PubMed] [Google Scholar]


