Abstract
Chronic hypobaric hypoxia at high altitudes can impair cognitive functions, especially causing deficits in learning and memory, which require therapeutic intervention. Here, we showed that mice subjected to hypobaric hypoxia (simulating an altitude of 5000 m) for one month experienced significant cognitive impairment, accompanied by increased biomarker levels of oxidative stress in the brain and blood. Oral administration of a novel formulation of edaravone, a free radical scavenger approved for the treatment of ischaemic stroke and amyotrophic lateral sclerosis, significantly alleviated oxidative stress and cognitive impairments caused by chronic hypobaric hypoxia. Furthermore, oral edaravone treatment also mitigated neuroinflammation and restored hippocampal neural stem cell exhaustion. Additionally, periostin (Postn) is vital in the cognitive deficits caused by chronic hypobaric hypoxia and may be a molecular target of edaravone. In conclusion, our results suggest that oxidative stress plays a crucial role in the cognitive deficits caused by chronic hypobaric hypoxia and that oral edaravone is a potential medicine for protecting against cognitive deficits caused by chronic hypobaric hypoxia in high-altitude areas.
Subject terms: Learning and memory, Psychiatric disorders
Introduction
Hypobaric hypoxia in high-altitude areas is characterized by a decrease in the partial pressure of oxygen due to low barometric pressure, which poses a major challenge to the health of more than 400 million people worldwide [1]. The brain, an organ with high metabolic and oxygen consumption rates, is particularly susceptible to hypoxia. Chronic hypobaric hypoxia significantly impairs cognitive functions, especially learning and memory abilities [2]. The prevalence of cognitive impairment among elderly individuals living in high-altitude areas is nearly twice as high as that in other regions of the world [3]. Furthermore, the cognitive deficits caused by hypobaric hypoxia in high-altitude areas can persist even after returning to lower altitudes [4]. However, there is currently a substantial lack of effective therapeutic approaches to cognitive impairments due to hypobaric hypoxia.
The balance between oxidation and antioxidant systems is disturbed in response to hypobaric hypoxia and subsequently induces oxidative stress [5]. The degree of cognitive impairment caused by hypobaric hypoxia was found to be associated with the level of oxidative stress [6]. These findings suggest that oxidative stress is a potential therapeutic target for cognitive impairment due to hypobaric hypoxia. Edaravone is a free radical scavenger with antioxidant and neuroprotective effects and is approved to treat ischaemic stroke and amyotrophic lateral sclerosis [7]. As edaravone is available in an injection formula, which is less suitable for chronic oxidative stress conditions, we developed a novel edaravone solid dispersion formula with 50% oral bioavailability [8]. In the present study, we investigated the effects of orally administered edaravone on oxidative stress and cognitive deficits in mice exposed to chronic hypobaric hypoxia and its underlying mechanisms, with the aim of identifying a potential therapeutic approach for preventing and treating cognitive impairments induced by chronic hypobaric hypoxia in high-altitude areas.
Materials and methods
Ethics and animals
All procedures were conducted according to the guidelines of the Institutional Animal Care Committee of Army Medical University. Male adult C57BL/6 mice (aged 8-9 weeks) were housed in a specific pathogen-free facility under a 12-hour light-dark cycle and had free access to standard chow and water.
Study design
This study used an oral edaravone formulation with a bioavailability of approximately 50% in rats [8] and 60% in humans (data not shown). The formulation is a self-nanomicellizing solid dispersion combined with the vehicle Soluplus, which can be dissolved in water. We chose a 24 mg/kg dose in this study because our previous study has shown that this dose is the pharmacologically maximal effective dose for inhibiting cognitive decline in aged APP/PS1 mice [9].
Mice were randomly divided into the following four groups to test the effectiveness of edaravone in preventing or treating hypobaric hypoxia (Fig. 1A): plain+vehicle, high-altitude (HA)+vehicle, HA+treatment and HA+prevention. In the plain+vehicle group, mice were housed at an altitude of 300 m (Chongqing, China) and received the vehicle (Soluplus) from Days 0 to 45. The remaining mice were housed in a hypobaric chamber simulating an altitude of 5000 m. In the HA+vehicle group, mice housed in a hypobaric chamber received Soluplus from Days 0 to 45. In the HA+treatment group, mice housed in a hypobaric chamber were given Soluplus from Days 0 to 28, followed by the edaravone solid dispersion formula from Days 29 to 45. In the HA+prevention group, mice housed in a hypobaric chamber were given the edaravone solid dispersion formula from Days 0 to 45. Both edaravone and Soluplus formulations were dissolved in drinking water to generate a final concentration of 24 mg/kg (Auzone Biotech, Suzhou, China).
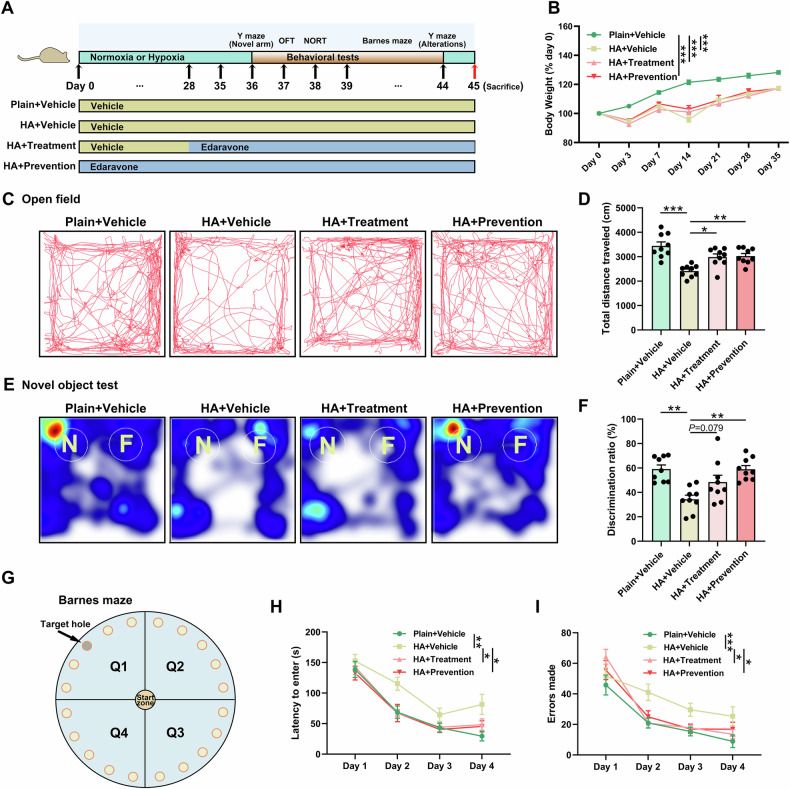
Fig. 1. Edaravone alleviated locomotor and cognitive impairments caused by chronic hypobaric hypoxia.
A Study design: Eight- to nine-week-old C57BL/6 male mice were randomly allocated to the following groups: plain+vehicle, HA+vehicle, HA+treatment and HA+prevention. All mice underwent a battery of behavioural tests from Days 36–44 and were sacrificed on Day 45. B Changes in body weight from Day 0 to Day 35 in the plain+vehicle, HA+vehicle, HA+treatment and HA+prevention groups. C, D Representative trajectory diagrams (C) and total distance travelled (D) of mice in the open field test. E, F Representative heatmaps (E) and discrimination ratios (F) of mice in the plain+vehicle, HA+vehicle, HA+treatment and HA+prevention groups in the novel object recognition test. “N” and “F” represent “novel object” and “familiar object”, respectively. G–I Diagram of the Barnes maze (G) and latency to enter the target hole (H) and errors made (I) during the learning acquisition period. Data are presented as mean ± SEM. Statistical comparisons were performed by two-way (B, H, I) and one-way (D, F) ANOVA with Tukey’s post hoc test. N = 9/group. *P < 0.05, **P < 0.01, ***P < 0.001. HA, high altitude; NORT, novel object recognition test; OFT, open field test.
A battery of behavioural tests was conducted on Days 36 to 44, including the Y maze, open field test, novel object recognition test, and Barnes maze. To ensure the safety of the researchers, behavioural tests and sacrifice were conducted at a simulated altitude of 3000 m for the mice exposed to hypobaric hypoxia.
To assess cell proliferation in the dentate gyrus (DG), mice were treated with 5 intraperitoneal injections of bromodeoxyuridine (BrdU, Sigma‒Aldrich) dissolved in sterile saline at a dose of 100 mg/kg, with a 12-hour interval between injections from Day 43 to Day 45.
Behavioural assays
Mice were acclimated to the test room overnight on Day 35. A battery of behavioural tests was scheduled to prevent carry-over influences from previous testing experiences following previous protocols [10]. An overhead camera with a tracking system and Noldus Observer software (Ethovision 11.0) were used to record and analyse the tracks.
Open field test
The open field test was performed to assess general locomotor function. The apparatus was made of white Plexiglas (40 cm × 40 cm × 40 cm). The mouse was placed in the centre zone and then allowed free access to the entire arena. The total distance travelled during the 10-minute period was recorded and analysed.
Novel object recognition
Novel object recognition is a valid test to evaluate episodic-like declarative memory, which was performed in the open field apparatus. Twenty-four hours after habituation (open field test), the mouse was allowed to explore two identical objects for 10 min in the open field arena during the acquisition phase. Two hours later, a 5-minute retrieval phase was performed with one novel object and one familiar object in the arena. The time spent exploring the familiar and novel objects was recorded. The discrimination ratio was calculated as follows: 100% × novel object time/(novel object time + familiar object time).
Y maze
The Y maze was used to assess spatial recognition memory. In the novel arm exploration test, the mouse was initially placed in the start arm and allowed to explore this maze for 5 min with the novel arm closed. Thirty minutes later, the mouse was allowed free access to all arms for 5 min. Entries and time spent in the novel arm were recorded and analysed. For the spontaneous alteration test, the mouse was placed in one arm and allowed free access to all arms for 8 min, and entries in each arm were recorded. The percentage of spontaneous alteration was calculated as follows: 100% × number of triads containing entries into all 3 arms/maximum possible alternations (the total number of arms entered - 2).
Barnes maze
The Barnes maze was used to assess learning and memory functions. The apparatus was made of a white circular platform (91 cm diameter) with 20 holes 5 cm in diameter and a black escape box placed under the target hole. Spatial cues around the maze and white noise (80 dB) were applied to facilitate and motivate the mouse to find the target hole. During each test, the mouse was initially placed in a nontransparent cylinder in the start zone for 10 s. Then, the cylinder was lifted, and the white noise was turned on. When the mouse was in the target hole, the buzzer was turned off. In the adaptation phase (Day 0), the mouse was allowed to explore the maze for 180 s and 120 s to be in the box. During the learning acquisition phase (Days 1–4), the mouse was trained to find and enter the target hole within 180 s. Once the target hole was found, all mice were allowed to stay in the box for 60 s. If the target hole was not found within 180 s, the mice were guided to the target hole and allowed to stay in the hole for an additional 60 s. Three trials per day with a 15-minute interval were conducted for four consecutive days. In the probe phase (Day 5), the mouse was allowed to explore the maze in a 90-second period. The latency to enter the target hole and errors made during each trial were recorded and analysed.
Proteomic analysis
The plasma samples were first depleted of the abundant proteins by CaptureSelect Proteomics Depletion Products (Life Technologies). Next, the proteins in the plasma samples were extracted, and the protein concentration was determined by the bicinchoninic acid method. The proteins were then digested and labelled with a tandem mass tag reagent. The labelled peptides were analysed by nanoflow liquid chromatography-tandem mass spectrometry using an Easy-nLC system (Thermo) connected to a Q_Exactive HF-X (Thermo). Mass spectra were analysed using Proteome Discoverer (Thermo, V.2.4) against the UniProt database. A fold change > 1.2 or < 0.83 and a P value < 0.05 were used to identify differentially expressed proteins. Gene Ontology (GO) enrichment analysis of annotated differentially expressed proteins was performed.
Biochemical assays
As previously described [11], the levels of malondialdehyde (MDA), superoxide dismutase (SOD) and glutathione peroxidase (GSH-Px) and the ratio of glutathione (GSH)/glutathione disulfide (GSSG) were assessed using the MDA detection kit, total SOD assay kit with WST-8, total GSH-Px assay kit, and GSH and GSSG assay kit (Beyotime), respectively.
Immunofluorescence staining and cell counting
After being anaesthetized with phenobarbital, the mice were transcardially perfused with 0.01 M phosphate-buffered saline (PBS). Then, the brains were dissected and sampled as previously described [12]. Coronal brain sections (30 μm in thickness) were washed in 0.01 M PBS and then incubated in 0.3% Triton X-100 for 1 h at room temperature. For BrdU staining, the sections were incubated in 2 N HCl for 30 min at 37 °C to denature DNA before being treated with the primary antibody. Next, the sections were incubated with primary antibodies, including rabbit anti-ionized calcium-binding adapter molecule-1 (Iba1) (1:1000, 019-19741, Wako), mouse anti-glial fibrillary acidic protein (GFAP) (1:1000, MAB360, Millipore), rabbit anti-sex determining region Y-Box 2 (Sox2) (1:1000, AB5603, Millipore), rabbit anti-doublecortin (DCX) (1:1000, 4604S, Cell Signaling Technology), mouse anti-BrdU (1:500, MAB3424, Millipore) and rabbit anti-Prox1 (1:500, 925202, Biolegend), at 4 °C overnight. After being washed in 0.01 M PBS, the sections were incubated with fluorescence-tagged secondary antibodies, including Cy3 (1:500, donkey anti-rabbit, Jackson ImmunoResearch), Alexa 488 (1:500, donkey anti-mouse, Jackson ImmunoResearch), and Alexa 488 (1:500, donkey anti-goat, Jackson ImmunoResearch), for 2 h at 37 °C. Finally, 4’,6-diamidino-2-phenylindole (DAPI, Sigma‒Aldrich) was used to stain the nuclei. The staining was photographed using a Zeiss microscope.
According to previous methods [13], radial glial cells were marked by Sox2 immunoreactivity colabelled with GFAP, which extended an apical process traversing the granule cell layer. Five matched sections spanning the rostrocaudal extent of the DG were counted to assess the number of Iba1+, Sox2+/GFAP+, DCX+ and BrdU+ cells in the DG, as well as the area fraction of Prox1+, under the same conditions in a blinded manner.
RNA sequencing
Total RNA from the hippocampus was extracted using TRIzol (Invitrogen) following the manufacturer’s instructions. The quality and quantity of RNA were confirmed by a NanoDrop and Agilent 2100 bioanalyzer (Thermo). cDNA was generated, amplified, and purified to obtain sequencing libraries, which were subsequently sequenced on the BGIseq500 platform. Raw reads were filtered with SOAPnuke (v1.5.2), and the clean reads were aligned to the mouse reference genome (GRCm38.p6) using HISAT2 (v. 2.0.4). The gene expression level was analysed using RSEM (v1.2.12), and differentially expressed transcripts and genes were analysed by DESeq2 (v1.4.5) with a P value < 0.05. GO enrichment analysis of annotated differentially expressed genes (DEGs) was performed by Phyper.
Western blot analysis
The brain samples were homogenized in radioimmunoprecipitation assay lysis buffer mixed with protease and phosphatase inhibitors (Beyotime), and western blot analysis was performed as previously described [14]. Blots were treated with primary antibodies, including anti-lysyl oxidase-like 1 (LOXL1) (1:1000, ab313585, Abcam), anti-periostin (Postn) (1:500, sc-398631, Santa-Cruz), anti-interferon stimulated gene 15 (ISG15) (1:1000, 2743, Cell Signaling Technology), anti-superoxide dismutase-3 (Sod3) (1:1000, ab80946, Abcam), anti-peroxiredoxin (Prdx) 4 (1:1000, ab184167, Abcam), anti-aldehyde dehydrogenase 1a1 (ALDH1a1) (1:1000, ab52492, Abcam), anti-Prdx6 (1:1000, ab133348, Abcam), anti-glutathione S-transferase M1 (GSTM1) (1:1000, PA5-79337, Invitrogen), and anti-β-actin (1:1000, 4970, Cell Signaling Technology), at 4 °C overnight, and IRDye 800 CW-conjugated secondary antibodies for 2 h at room temperature, subsequently. The blots were scanned using an Odyssey fluorescent scanner. The relative band intensities were normalized to the loading control (β-actin).
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (version 25.0 for Windows, IBM Corp.). Data with a normal distribution are presented as mean ± SEM. One-way ANOVA with Tukey’s post hoc test was conducted for multiple comparisons. Data collected at repeated time points were analysed by two-way ANOVA with Tukey’s post hoc test. For all statistical comparisons, *P < 0.05, **P < 0.01, and ***P < 0.001.
Results
Edaravone alleviated hypobaric hypoxia-induced cognitive impairments
The body weight was significantly reduced in mice exposed to hypobaric hypoxia compared to mice housed in plain area from Day 0 to Day 35 (P < 0.001) (Fig. 1B). However, edaravone administration did not restore this body weight loss in either the treatment or prevention group (Fig. 1B). Chronic hypobaric hypoxia significantly impaired spontaneous locomotor functions in HA+vehicle mice, as evidenced by the decreased total distance travelled in the open field test (P < 0.001) (Fig. 1C, D). In comparison with the HA+vehicle group, edaravone administration significantly increased the total distance travelled in mice in both the HA+treatment (P < 0.05) and HA+prevention (P < 0.01) groups (Fig. 1C, D).
In the novel object recognition test, HA+vehicle mice showed a lower discrimination ratio than plain+vehicle mice (P < 0.01), and the memory deficits were significantly reversed in the HA+prevention group (P < 0.01) (Fig. 1E, F). In addition, the HA+treatment group also showed a tendency towards a higher discrimination ratio than the HA+vehicle group (P = 0.079) (Fig. 1E, F).
For the novel arm exploration test in the Y maze, mice in the HA+vehicle group showed fewer novel arm entries than those in the plain+vehicle group (P < 0.05) (Fig. S1A). However, there was no significant effect of edaravone on novel arm entries in mice exposed to chronic hypobaric hypoxia (Fig. S1A). In addition, mice from the four groups showed an indistinguishable percentage of time spent in the novel arm (Fig. S1A) and spontaneous alterations (Fig. S1B).
During the learning acquisition period of the Barnes maze, the latency to enter the target hole (P < 0.01) and the number of errors made (P < 0.001) in the HA+vehicle group were significantly increased over time compared to those in the plain+vehicle group (Fig. 1G-I). Mice in the HA+treatment or HA+prevention group performed much better in the latency and errors made over time in the acquisition period than those in the HA+vehicle group (P < 0.05 for all comparisons) (Fig. 1G-I). In the probe trial, there was no significant difference among the four groups in latency to enter the target hole or errors made (Fig. S1C).
Edaravone restored alterations in the plasma protein expression profile induced by hypobaric hypoxia
A total of 1053 proteins were detected in the plasma of mice in control conditions and those exposed to chronic hypobaric hypoxia. The hierarchical clustering heatmap presents the protein expression profile in the plasma of plain+vehicle and HA+vehicle mice (Fig. 2A). There were 239 upregulated proteins and 14 downregulated proteins in the HA+vehicle group compared to the plain+vehicle group (Fig. 2B). Based on these differentially expressed proteins, the top 15 GO enrichments included 4 pathways related to oxidative stress, such as hydrogen peroxide catabolic process, cellular detoxification, reactive oxygen species metabolic process, hydrogen peroxide metabolic process, and cellular oxidant detoxification (Fig. 2C).
Fig. 2. Edaravone abrogated alterations in the plasma protein expression profile caused by hypobaric hypoxia.
A Hierarchical clustering heatmap of differentially expressed proteins in plasma between the plain+vehicle and HA+vehicle mice. B, C Volcano plot (B) and significantly enriched biological processes (C) of differentially expressed proteins between the HA+vehicle and plain+vehicle groups. D, E Volcano plot (D) and significantly enriched biological processes (E) of differentially expressed proteins between the HA+treatment and HA+vehicle groups. HA, high altitude. N = 3/group.
There were 51 proteins that were upregulated and 91 proteins that were downregulated in the HA+treatment group compared to the HA+vehicle group (Fig. 2D), and these differentially expressed proteins were mainly involved in oxidative stress, such as the hydrogen peroxide catabolic process, hydrogen peroxide metabolic process, cell redox homeostasis, reactive oxygen species metabolic process, and response to oxidative stress, indicating that edaravone can effectively balance the oxidation‒reduction system under chronic hypobaric hypoxia (Fig. 2E).
Thirty proteins were upregulated and 21 proteins were downregulated in the HA+prevention group compared to the HA+vehicle group (Fig. S2A). The differentially expressed proteins between the two groups were mainly involved in immune responses, such as the T cell receptor signalling pathway, antigen processing and presentation of peptide antigen, antigen processing and presentation of exogenous peptide antigen, endocytosis, antigen processing and presentation of exogenous antigen, receptor-mediated endocytosis, antigen processing and presentation of peptide antigen via MHC class I, antigen processing and presentation, and positive regulation of interleukin-8 production (Fig.e S2B).
Edaravone ameliorated hypobaric hypoxia-induced oxidative stress and neuroinflammation in the brain
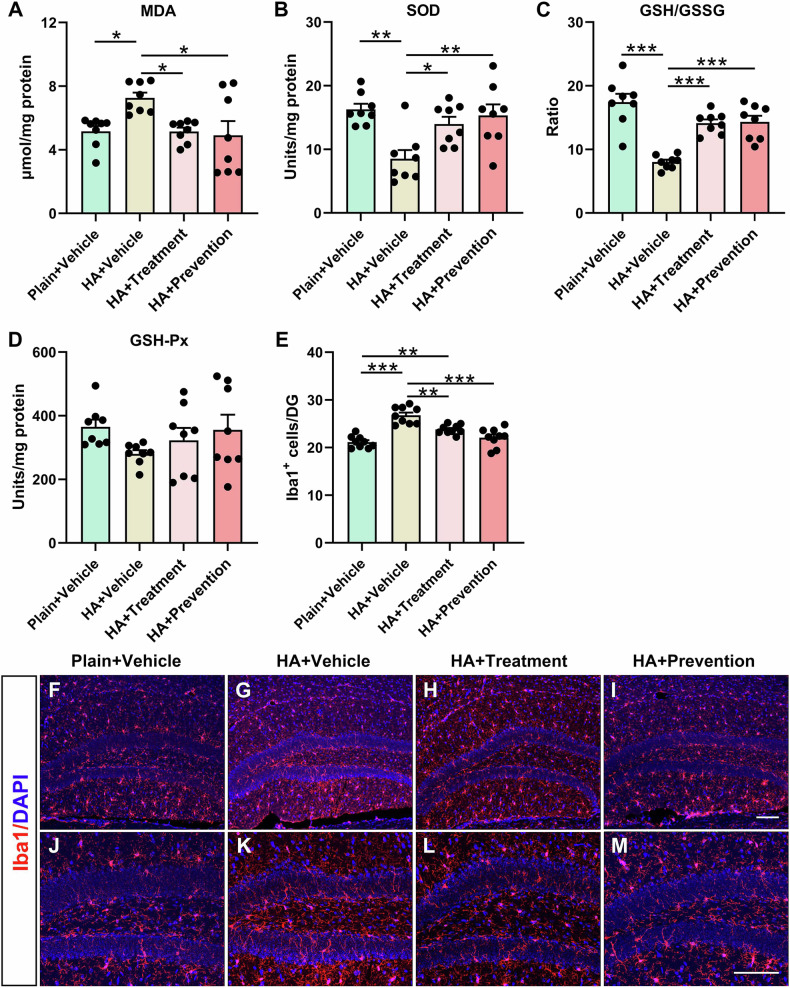
The levels of MDA (P < 0.05) were significantly increased, while the levels of SOD (P < 0.01) and GSH/GSSG (P < 0.001) were markedly decreased in the brains of HA+vehicle mice compared to plain+vehicle mice (Fig. 3A-C). HA+treatment and HA+prevention partially reversed these changes in MDA (P < 0.05 for both comparisons), SOD (P < 0.05 for HA+treatment; P < 0.01 for HA+prevention), and GSH/GSSG (P < 0.001 for both comparisons) (Fig. 3A-C). The levels of GSH-Px were comparable among the four groups (Fig. 3D).
Fig. 3. Edaravone reduced oxidative stress and inflammation in the brain caused by chronic hypobaric hypoxia.
A–D Levels of MDA (A), SOD (B), GSH/GSSG ratio (C), and GSH-Px (D) in the brain tissues of plain+vehicle, HA+vehicle, HA+treatment and HA+prevention mice. Data are presented as mean ± SEM. N = 8/group. E Quantitative analysis of Iba1+ immunofluorescence staining within the dentate gyrus of plain+vehicle, HA+vehicle, HA+treatment and HA+prevention mice. N = 9/group. F–M Representative images of Iba1+ cells in the dentate gyrus region. Scale bar = 100 µm. Data are presented as mean ± SEM. Statistical comparisons were performed by one-way ANOVA with Tukey’s post hoc test. *P < 0.05, **P < 0.01, ***P < 0.001. GSH/GSSG, reduced glutathione/oxidized glutathione disulfide; GSH-Px, glutathione peroxidase; HA, high altitude; Iba1, ionized calcium-binding adapter molecule-1; MDA, malondialdehyde; SOD, superoxide dismutase.
The immunofluorescence staining results showed that the number of microglia (Iba1+) in the DG was significantly increased in HA+vehicle mice (P < 0.001) compared to plain+vehicle mice (Fig. 3E-M), suggesting that hypobaric hypoxia increased the inflammation levels in the hippocampus of mice. Furthermore, mice in the HA+treatment (P < 0.01) and HA+prevention (P < 0.001) groups had fewer Iba1+ cells in the DG than those in the HA+vehicle group (Fig. 3E-M).
Edaravone enhanced hippocampal neurogenesis impaired by hypobaric hypoxia
Neurogenesis was disturbed by chronic hypobaric hypoxia, as evidenced by the reduced number of neural progenitor cells (NPCs) (Sox2+/GFAP+) in the DG of mice in the HA+vehicle group compared with that of mice in the plain+vehicle group (P < 0.001) (Fig. 4A-H, Q). Administration of edaravone significantly increased the number of Sox2+/GFAP+ cells in the DG in the HA+treatment (P < 0.01) and HA+prevention (P < 0.01) groups compared to the HA+vehicle group (Fig. 4A-H, Q). The number of Sox2+ cells in the DG of HA+vehicle mice was also less than that in the plain+vehicle group (P < 0.01), while edaravone treatment and prevention did not significantly influence the number of Sox2+ cells in the DG (Fig. 4A-H, R).
Fig. 4. Edaravone restored hippocampal neural stem cell exhaustion caused by chronic hypobaric hypoxia.
A–H Representative images of Sox2+/GFAP+ colabelled radial glia-like neural progenitor cells in the dentate gyrus region. The arrows indicate Sox2+/GFAP+ colabelled cells. Scale bar = 100 µm. Q, R Quantitative analysis of Sox2+/GFAP+ (Q) and Sox2+ (R) immunofluorescence staining within the dentate gyrus of plain+vehicle, HA+vehicle, HA+treatment and HA+prevention mice. I–P Representative images of DCX+ cells in the dentate gyrus region. Scale bar = 100 µm. S Quantitative analysis of DCX+ immunofluorescence staining within the dentate gyrus of plain+vehicle, HA+vehicle, HA+treatment and HA+prevention mice. Data are presented as mean ± SEM. Statistical comparisons were performed by one-way ANOVA with Tukey’s post hoc test. N = 9/group. *P < 0.05, **P < 0.01, ***P < 0.001. DCX, doublecortin; GFAP, glial fibrillary acidic protein; HA, high altitude; Sox2, sex determining region Y-Box 2.
Mice in the HA+vehicle (P < 0.001), HA+treatment (P < 0.05) or HA+prevention (P < 0.05) groups showed significantly higher numbers of DCX+ cells in the DG than the plain+vehicle group, indicating that chronic hypobaric hypoxia exacerbated NPC differentiation in the hippocampus (Fig. 4I-P, S). In addition, the numbers of DCX+ cells in the HA+treatment (P < 0.05) and HA+prevention (P < 0.05) groups were significantly lower than those in HA+vehicle mice (Fig. 4I-P, S). Furthermore, the numbers of BrdU+ cells in the DG were comparable among the four groups (Fig. S3A-D, I). The area fraction of Prox1+ cells in the HA+vehicle group was slightly decreased compared to that in the plain+vehicle group (P = 0.062), while there was no significant difference between the HA+treatment or HA+prevention group and the HA+vehicle group (Fig. S3E-H, J).
Edaravone restored alterations in brain gene expression induced by hypobaric hypoxia
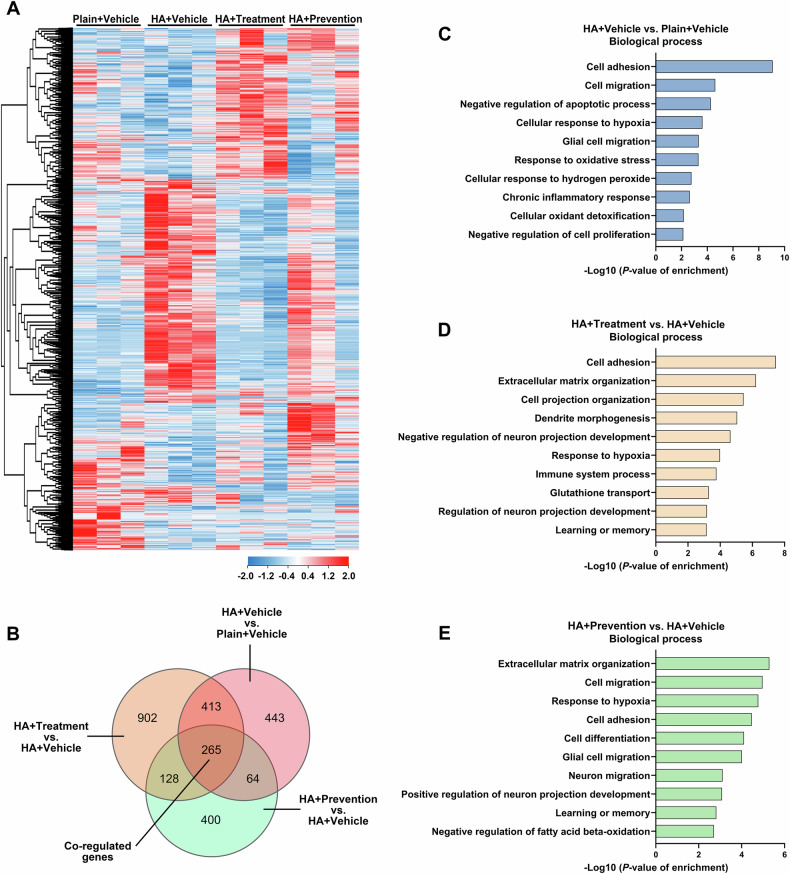
The hierarchical clustering heatmap showed the gene expression profile in the hippocampus of plain+vehicle, HA+vehicle, HA+treatment and HA+prevention mice (Fig. 5A). There were 1185 DEGs between the HA+vehicle and plain+vehicle groups, 1708 DEGs between the HA+treatment and HA+vehicle groups, and 857 DEGs between the HA+prevention and HA+vehicle groups (Fig. 5B); 265 DEGs were coregulated by hypobaric hypoxia and edaravone treatment and prevention (Fig. 5B).
Fig. 5. Edaravone abrogated alterations in brain gene expression induced by hypobaric hypoxia.
A Hierarchical clustering heatmap of differentially expressed genes in the hippocampus of plain+vehicle, HA+vehicle, HA+treatment and HA+prevention mice. B Venn diagram of differentially expressed genes regulated by chronic hypobaric hypoxia and edaravone treatment and prevention. C–E Significantly enriched biological processes of the differentially expressed genes between the plain+vehicle and HA+vehicle groups (C), between the HA+treatment and HA+vehicle groups (D), and between the HA+prevention and HA+vehicle groups (E) analysed by Gene Ontology analysis. N = 3/group. HA, high altitude.
Based on the DEGs between the HA+vehicle and plain+vehicle groups, GO analysis showed significant enrichment of biological processes involved in oxidative stress and hypoxia (cellular response to hypoxia, response to oxidative stress, cellular response to hydrogen peroxide, cellular oxidant detoxification), neurogenesis (glial cell migration, negative regulation of cell proliferation), and inflammation (chronic inflammatory response) (Fig. 5C). The DEGs between the HA+treatment or HA+prevention and HA+vehicle groups were also mainly involved in oxidative stress, neurogenesis and inflammation (Fig. 5D, E).
Edaravone regulated Postn in the attenuation of detrimental effects induced by hypobaric hypoxia
There are 265 coregulated DEGs by hypobaric hypoxia and edaravone treatment or prevention in hippocampus, the GO analysis showed significant enrichment of biological processes included oxidative stress (response to oxygen-containing compound, response to superoxide, response to oxygen radical, and cellular oxidant detoxification), neurogenesis (cell differentiation, neurogenesis, neuron differentiation, and negative regulation of neural precursor cell proliferation), inflammation (phagocytosis) and cell adhesion (Figure S4A). Cluster analysis of biological processes identified that Postn, Vcam1, Sfrp1 and Bmp6 as the hub genes, linking neurogenesis-related genes, cell adhesion-related genes and response to oxygen-containing compound-related genes (Figure S4B).
Furthermore, we found that there were 16 molecules that were altered in both the brain (DEGs in hippocampus) and blood (differentially expressed proteins in plasma) under chronic hypobaric hypoxia (Fig. 6A, B). Among the 16 molecules, 8 of them are involved in modulating oxidative stress, including Loxl1, Postn, Isg15, Sod3, Prdx4, Aldh1a1, Prdx6, and Gstm1, indicating that oxidative stress is a critical mechanism involved in the effects of chronic hypobaric hypoxia on brain. The protein expressions of these 8 molecules in brain among groups were validated (Fig. 6C-K). Specifically, the protein expression of Postn was decreased in the brain of both HA+treatment (P < 0.05) and HA+prevention (P < 0.05) mice compared to HA+vehicle mice (Fig. 6C, E).
Fig. 6. Postn was detrimental for mice in chronic hypobaric hypoxia, and edaravone can regulate its expression.
A Venn diagram of the 16 differentially expressed molecules altered in both the hippocampus and plasma regulated by chronic hypobaric hypoxia. N = 3/group. B Hierarchical clustering heatmap of the 16 differentially expressed genes in the hippocampus among plain+vehicle, HA+vehicle, HA+treatment and HA+prevention groups. N = 3/group. C–K Representative western blots (C) and quantitative analysis (D–K) for the protein expressions of LOXL1, Postn, ISG15, Sod3, Prdx4, ALDH1a1, Prdx6, and GSTM1 in plain+vehicle, HA+vehicle, HA+treatment and HA+prevention mice. Data are presented as mean ± SEM. Statistical comparisons were performed by one-way ANOVA with Turkey post hoc test. N = 8/group. *P < 0.05, **P < 0.01, ***P < 0.001. ALDH1a1, aldehyde dehydrogenase 1a1; GSTM1, glutathione S-transferase M1; HA, high altitude; ISG15, interferon stimulated gene 15; LOXL1, lysyl oxidase like; Postn, periostin; Prdx, peroxiredoxin; Sod3, superoxide dismutase-3.
The above data suggested that Postn is a critical gene regulating the brain damage caused by hypobaric hypoxia and edaravone treatment or prevention, and it has the potential to be a biomarker for the severity of brain damage and predict cognitive deficits in individuals exposed to hypobaric hypoxia.
Discussion
In this study, we provided evidence that chronic hypobaric hypoxia results in cognitive impairments partially by inducing an increased oxidative stress response, neuroinflammation and neural stem cell exhaustion. Oral administration of edaravone, a free radical scavenger, can effectively abrogate these alterations in mice as a treatment and prevention modality. Furthermore, Postn, an extracellular matrix (ECM) protein, plays a critical role in the cognitive deficits caused by chronic hypobaric hypoxia and may be a molecular target of edaravone.
There is an increasing number of people, approximately 40 million or more, travelling to or visiting high-altitude areas each year [15]. However, exposure to hypobaric hypoxia in high-altitude environments is detrimental to human health, especially for those that live in low-altitude areas. The body systemically responds to hypobaric hypoxia, and the effects of hypobaric hypoxia on the nervous, respiratory, circulatory, digestive, and metabolic systems are time- and altitude-dependent [16]. Several studies have revealed that acute hypobaric hypoxia exposure alters the expression of immune-related genes and oxidative stress markers in blood [16], which may be the cause of acute responses induced by hypobaric hypoxia, such as acute mountain sickness. In our study, we housed mice at a simulated altitude of 5000 m for one month and found that chronic hypobaric hypoxia stress caused alterations in protein expression related to oxidative stress in the blood. This evidence indicates that the oxidative stress response is one of the main stress responses caused by chronic hypobaric hypoxia.
Chronic hypobaric hypoxia induces impairments in the nervous system, and one of the most common manifestations is cognitive deficits [17, 18]. Our data revealed that episodic-like declarative memory, spatial recognition memory, and learning and memory functions (especially during training period) were impaired in mice exposed to chronic hypobaric hypoxia. Moreover, the levels of oxidative stress and inflammation were elevated in the brains of mice exposed to chronic hypobaric hypoxia. These results are consistent with previous studies in which oxidative stress and inflammation may contribute to the cognitive impairments caused by hypobaric hypoxia [15, 19, 20]. In addition, hippocampal neurogenesis deficits are strongly proposed to contribute to cognitive impairments [21]. Neural stem cells differentiate into neurons and glial cells from the subgranular zone of the DG in the hippocampus [22], and an imbalance of self-renewal and differentiation of neuronal stem cells causes deficits in learning and working memory [23]. Our study showed that the NPC pool is reduced in mice exposed to chronic hypobaric hypoxia, as evidenced by a decreased number of neural stem cells (radial glia-like NPCs) in the DG subregion of the hippocampus. The number of neuroblasts and immature neurons (DCX+) was significantly increased, while the granule cells (Prox1+) were slightly reduced in mice exposed to chronic hypobaric hypoxia. As a critical intrinsic regulator of neurogenesis in the adult DG of the hippocampus, Prox1 is required for maintenance of intermediate progenitors, maturation of granule neurons in DG, differentiation and maturation of glutamatergic interneurons, as well as specification of DG cell identity over CA3 pyramidal fate [24]. Thus, even if the neural progenitor cell differentiation is exacerbated by chronic hypobaric hypoxia, the area fraction of Prox1+ in DG was not significantly changed and even with a decreased tendency, suggesting that the maturation of granule neurons in DG is impaired. These data indicate that NPC differentiation is exacerbated under chronic hypobaric hypoxia exposure, and some cells cannot differentiate into mature neurons, which may be a reason for exhaustion of the hippocampal NPC pool. Considering that genetic and environmental factors that disrupt the balance between NPC self-renewal and differentiation can cause cognitive deficits [25, 26], it is speculated that hippocampal NPC pool exhaustion may contribute to cognitive impairments under chronic hypobaric hypoxia. Moreover, since oxidative stress and neuroinflammation play crucial roles in regulating hippocampal neurogenesis [27], it is plausible that cognitive function impairment in chronic hypobaric hypoxia could stem from their disruption of hippocampal neurogenesis.
Productivity and quality of life are impaired due to the cognitive dysfunctions induced by hypobaric hypoxia. Moreover, no effective drug is available for the treatment or prevention of cognitive deficits caused by hypobaric hypoxia in high-altitude areas, especially for long-term stays. Oxygen therapy is an effective treatment, but it is not available for most people. Many drugs, such as the corticosterone synthesis inhibitor metyrapone and isradipine, are not suitable for long-term use due to potential side effects [28]. Thus, it is necessary to investigate safer and more effective treatments for chronic hypobaric hypoxia. Our results indicate that oxidative stress occurs in the central nervous system as a response to chronic hypobaric hypoxia. According to previous studies, edaravone has the potential to alleviate cognitive impairments induced by traumatic brain injury, ischaemic stroke and dementia [7, 29, 30]. Furthermore, our previous study found that edaravone can alleviate microgliosis and cognitive deficits in an Alzheimer’s disease mouse model [30]. Edaravone could also increase endogenous neurogenesis and improve motor functions in ischaemic rats [31]. However, whether edaravone has protective effects against cognitive impairments induced by chronic hypobaric hypoxia remains unclear. The present study showed that application of oral edaravone can significantly alleviate oxidative stress, as well as the neuroinflammation and hippocampal neurogenesis deficits. This evidence suggests that edaravone is an effective therapeutic for the treatment and prevention of cognitive impairments and related pathological changes caused by chronic hypobaric hypoxia in the absence of oxygen supply. It further confirms that oxidative stress is a cause of inflammation and neurogenesis impairment in this condition and a crucial therapeutic target for cognitive impairments induced by chronic hypobaric hypoxia. Moreover, the oral formulation of edaravone used in the study has a comparable pharmacokinetic profile with the intravenous formulation, which has been identified in our Phase I clinical trial. This oral formulation is characterized by its rapid absorption, achieving peak blood concentrations within one hour following oral administration. The convenience of carrying and consuming the oral formulation significantly enhance its practicality in the application in high-altitude areas to prevent and treat chronic diseases associated with high altitudes.
Skeletal muscle protein loss, low appetite and central fatigue lead to a decline in motor function in exposure to hypobaric hypoxia [32, 33]. Our results found that administration of edaravone significantly increased general exploratory behaviours in mice exposed to chronic hypobaric hypoxia, while body weight loss was not reversed by edaravone treatment or prevention. It is speculated that the improved motor function is more likely to be due to decreased central fatigue, other than less skeletal muscle protein loss and appetite loss. Besides, the body weight loss may not be effectively restored solely through antioxidant intervention without getting rid of the hypobaric hypoxia condition. Overall, the above data indicate that edaravone may be an effective treatment and prevention for cognitive impairments and motor function decline caused by chronic hypobaric hypoxia.
Our study found that the oxidation and antioxidant systems are disturbed in both plasma and brain, and can be modulated by the oral formulation edaravone. Specifically, the expression of Postn is upregulated in both the brain and plasma of mice exposed to chronic hypobaric hypoxia, which was reduced by orally administered edaravone in brain. Postn, an ECM protein, is normally expressed at low levels in adult tissues [34, 35], and this 90-kDa protein may easily pass blood-brain barrier and can move or be secreted into various body fluids, such as blood [36]. There are several studies suggesting that plasma Postn might be a potential biomarker for brain disorders. Recently, an observational prospective study has suggested that the plasma level of Postn was associated with decline of cognitive capacities in older adults during a 4-year follow-up, and may serve as a predictive biomarker for cognitive decline among older adults [37]. Serum Postn concentrations can also predict the clinical prognosis among patients with traumatic brain injury and subarachnoid hemorrhage [36, 38]. Based on our data, we proposed that Postn may also have the potential to be a biomarker for the severity of brain damage and predict cognitive deficits in long-term residents at high-altitude areas.
Previous studies have shown that Postn is involved in regulating oxidative stress response, cell stemness and differentiation, and inflammation in several types of cells [34, 39, 40]. For example, upregulation of Postn has been found to exacerbate intracellular reactive oxygen species (ROS)-dependent vascular smooth muscle cell calcification in rats [39]. Postn also regulates the stemness or differentiation of bone, mesenchymal, and hematopoietic stem cells in a cell-specific manner [34, 40]. Additionally, Postn mediates glioma-associated macrophage infiltration and M2 polarization induced by hypoxia [41]. According to these pieces of evidence, it is speculated that edaravone alleviates oxidative stress, hippocampal neurogenesis deficits and neuroinflammation by regulating Postn, subsequently enhancing cognitive functions in mice exposed to chronic hypobaric hypoxia.
Furthermore, the present study revealed that the effects of oral edaravone treatment and prevention are comparable in ameliorating cognitive dysfunction, oxidative stress, neuroinflammation and neurogenesis deficits. Thus, edaravone is an effective therapeutic for the treatment and prevention of chronic hypobaric hypoxia. However, the pharmacological effects may be different between short- and long-term application of oral edaravone in individuals with chronic hypobaric hypoxia. The protein expression profile in the plasma revealed that edaravone treatment mainly reversed the expression of proteins related to oxidative stress, while edaravone prevention was more likely to modulate proteins related to immune responses. In the edaravone treatment group, after exposure to the hypobaric hypoxic environment for one month, the oxidant and antioxidant balance was disturbed, and the level of oxidative stress was significantly elevated. As expected, the most obvious effect of edaravone treatment was reducing the level of oxidative stress. Apart from oxidative stress, hypobaric hypoxia exposure also induces impairments in immune function [42]. Reduced numbers of lymphocytes and T cells and increased levels of inflammatory cytokines are the most notable alterations in the immune system induced by hypobaric hypoxia at high altitudes [42–44]. In the edaravone prevention group, the oxidative stress response was inhibited by edaravone, and the immune response was the principle first pathological response in this condition. Thus, we observed that edaravone prevention mainly regulated proteins related to innate and adaptive immune responses. It seems the antioxidant effect of edaravone on plasma is stronger in treatment group than in prevention group, which might due to the sudden increase in the antioxidant defense mechanisms overcoming a prolonged inhibitory oxidative effect in the short-term application of edaravone [45]. While our study has demonstrated the efficacy of both preventive and therapeutic measures, we assert that the significance of prevention surpasses that of treatment. We advocate for the preemptive aversion of neurological damage and cognitive decline through proactive strategies, as this is deemed more desirable than the subsequent remediation of such damage post-occurrence. It would be necessary to perform clinical trials to test its efficacy and optimal treatment regime in humans who are exposed to chronic hypobaric hypoxia, and to further investigate the varied pharmacological effects between treatment and prevention application of oral edaravone.
In summary, this preclinical study deepens the understanding of the effects of chronic hypobaric hypoxia on the brain and highlights the effectiveness of edaravone as a therapeutic treatment for cognitive impairments induced by chronic hypobaric hypoxia in high-altitude areas. And, Postn is critical in the cognitive deficits caused by chronic hypobaric hypoxia and may be a molecular target of edaravone. Furthermore, the optimal therapeutic regime of oral edaravone for chronic hypobaric hypoxia exposure needs to be further explored and validated in clinical trials.
Supplementary information
Acknowledgements
Suzhou Auzone Biotech supported the cost of animal, reagents and measurements of this study.
Author contributions
Yan-Jiang Wang: Conceptualization; Resources; Supervision; Writing - review & editing. Juan Liu: Conceptualization; Supervision; Writing - review & editing. Yuan-Yuan Ma: Data curation; Investigation; Project administration; Validation; Visualization; writing - original draft. Xin Li: Data curation; Visualization; Methodology; Writing - original draft. Zhong-Yuan Yu: Formal analysis; Project administration; Validation. Tong Luo: Project administration; Methodology. Cheng-Rong Tan: Data curation; Formal analysis; Project administration. Yu-Di Bai: Investigation; Project administration. Gang Xu: Investigation; Resources; Supervision. Bin-Da Sun: Resources; Validation. Xian-Le Bu: Methodology; Validation; Writing - review & editing. Yu-Hui Liu: Methodology; Writing - review & editing. Wang-Sheng Jin: Methodology; Writing - review & editing. Yu-Qi Gao: Conceptualization; Resources; Supervision; Writing - review & editing. Xin-Fu Zhou: Conceptualization; Resources; Supervision; Writing - review & editing.
Funding
This work was supported by the National Natural Science Foundation of China (92249305), High-Level Talents Innovation Project of PLA- Youth Talents of Science and Technology, the Special Funding for Chongqing Postdoctoral Research Project, and the Natural Science Foundation of Shigatse, China.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
Competing interests
The patent application for edaravone in the prevention and treatment of cognitive impairment induced by chronic hypobaric hypoxia is currently being prepared, Daping Hospital and Suzhou Auzone Biotech are the patent owners, and Yan-Jiang Wang, Yuan-Yuan Ma and Xin-Fu Zhou are the patent inventors. Xin-Fu Zhou is an employee of Suzhou Auzone Biotech. Other authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Yuan-Yuan Ma, Xin Li.
Contributor Information
Juan Liu, Email: liujuan961@163.com.
Yan-Jiang Wang, Email: yanjiang_wang@tmmu.edu.cn.
Supplementary information
The online version contains supplementary material available at 10.1038/s41398-024-03133-1.
References
- 1.Chen X, Zhang J, Lin Y, Li Y, Wang H, Wang Z, et al. Mechanism, prevention and treatment of cognitive impairment caused by high altitude exposure. Front Physiol. 2023;14:1191058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang G, Zhou S-M, Yuan C, Tian H-J, Li P, Gao Y-Q. The effects of short-term and long-term exposure to a high altitude hypoxic environment on neurobehavioral function. High Alt Med Biol. 2013;14:338–41. [DOI] [PubMed] [Google Scholar]
- 3.Urrunaga-Pastor D, Chambergo-Michilot D, Runzer-Colmenares FM, Pacheco-Mendoza J, Benites-Zapata VA. Prevalence of cognitive impairment and dementia in older adults living at high altitude: a systematic review and meta-analysis. Dement Geriatr Cogn Disord. 2021;50:124–34. [DOI] [PubMed] [Google Scholar]
- 4.Yu L, Chen Y, Wang W, Xiao Z, Hong Y. Multi-vitamin B supplementation reverses hypoxia-induced Tau hyperphosphorylation and improves memory function in adult mice. J Alzheimers Dis. 2016;54:297–306. [DOI] [PubMed] [Google Scholar]
- 5.Pena E, El Alam S, Siques P, Brito J. Oxidative stress and diseases associated with high-altitude exposure. Antioxidants. 2022;11:267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bailey DM, Brugniaux JV, Filipponi T, Marley CJ, Stacey B, Soria R, et al. Exaggerated systemic oxidative‐inflammatory‐nitrosative stress in chronic mountain sickness is associated with cognitive decline and depression. J Physiol. 2018;597:611–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cui XP, Ye JX, Lin H, Zhou H, Ye S, Mu JS. Effects of edaravone combined with Oxiracetam on neuronal apoptosis in rats with cerebral infarction through targeting SIRT1/NF-κB inflammatory pathway. Eur Rev Med Pharmacol Sci. 2022;26:218–24. [DOI] [PubMed] [Google Scholar]
- 8.Parikh A, Kathawala K, Tan CC, Garg S, Zhou X-F. Self-nanomicellizing solid dispersion of edaravone: part I: oral bioavailability improvement. Drug Des Devel Ther. 2018;12:2051–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parikh A, Kathawala K, Li J, Chen C, Shan Z, Cao X, et al. Self-nanomicellizing solid dispersion of edaravone: part II: in vivo assessment of efficacy against behavior deficits and safety in Alzheimer’s disease model. Drug Des Devel Ther. 2018;12:2111–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ma Y, Liu T, Li X, Kong A, Xiao R, Xie R, et al. Estrogen receptor β deficiency impairs gut microbiota: a possible mech anism of IBD-induced anxiety-like behavior. Microbiome. 2022;10:160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lu MC, Zhao J, Liu YT, Liu T, Tao MM, You QD, et al. CPUY192018, a potent inhibitor of the Keap1-Nrf2 protein-protein interaction, alleviates renal inflammation in mice by restricting oxidative stress and NF-kappaB activation. Redox Biol. 2019;26:101266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang J, Sun BL, Xiang Y, Tian DY, Zhu C, Li WW, et al. Capsaicin consumption reduces brain amyloid-beta generation and attenuates Alzheimer’s disease-type pathology and cognitive deficits in APP/PS1 mice. Transl Psychiatry. 2020;10:230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang R, Cai Y, Xiao R, Zhong H, Li X, Guo L, et al. Human amniotic epithelial cell transplantation promotes neurogenesis and ameliorates social deficits in BTBR mice. Stem Cell Res Ther. 2019;10:153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yu ZY, Chen DW, Tan CR, Zeng GH, He CY, Wang J, et al. Physiological clearance of Abeta by spleen and splenectomy aggravates Alzheimer-type pathogenesis. Aging Cell. 2022;21:e13533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang H, Zhang X, Liu Z, Mei Y, Liu Y, Wei X, et al. Time-course effects and mechanisms of hypobaric hypoxia on nervous system in mice. Neurosci Lett. 2023;801:137163. [DOI] [PubMed] [Google Scholar]
- 16.Manella G, Ezagouri S, Champigneulle B, Gaucher J, Mendelson M, Lemarie E, et al. The human blood transcriptome exhibits time-of-day-dependent response to hypoxia: Lessons from the highest city in the world. Cell Rep. 2022;40:111213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dalong G, Yufei Q, Lei Y, Pengfei L, Anqi Y, Zichuan G, et al. Modulation of thalamic network connectivity using transcranial direct current stimulation based on resting-state functional magnetic resonance imaging to improve hypoxia-induced cognitive impairments. Front Neurosci. 2022;16:955096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yan X. Cognitive impairments at high altitudes and adaptation. High Alt Med Biol. 2014;15:141–5. [DOI] [PubMed] [Google Scholar]
- 19.Xu G, Shi Y-K, Sun B-D, Liu L, E G-J, He S, et al. DL-3-n-butylphthalide improved physical and learning and memory performance of rodents exposed to acute and chronic hypobaric hypoxia. Mil Med Res. 2021;8:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ji W, Zhang Y, Luo J, Wan Y, Liu J, Ge R-L. Memantine ameliorates cognitive impairment induced by exposure to chronic hypoxia environment at high altitude by inhibiting excitotoxicity. Life Sci. 2021;270:119012. [DOI] [PubMed] [Google Scholar]
- 21.Chauhan G, Kumar G, Roy K, Kumari P, Thondala B, Kishore K, et al. Hypobaric hypoxia induces deficits in adult neurogenesis and social interaction via cyclooxygenase-1/ EP1 receptor pathway activating NLRP3 inflammasome. Mol Neurobiol. 2022;59:2497–519. [DOI] [PubMed] [Google Scholar]
- 22.Yin B-K, Lázaro D, Wang Z-Q. TRRAP-mediated acetylation on Sp1 regulates adult neurogenesis. Comput Struct Biotechnol J. 2023;21:472–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gradari S, Herrera A, Tezanos P, Fontán-Lozano Á, Pons S, Trejo JL. The role of Smad2 in adult neuroplasticity as seen through hippocampal-dependent spatial learning/memory and neurogenesis. J Neurosci. 2021;41:6836–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stergiopoulos A, Elkouris M, Politis PK. Prospero-related homeobox 1 (Prox1) at the crossroads of diverse pathways during adult neural fate specification. Front Cell Neurosci. 2015;8:454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fu C-H, Iascone DM, Petrof I, Hazra A, Zhang X, Pyfer MS, et al. Early seizure activity accelerates depletion of hippocampal neural stem cells and impairs spatial discrimination in an Alzheimer’s disease model. Cell Rep. 2019;27:3741–51.e3744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hu X, An J, Ge Q, Sun M, Zhang Z, Cai Z, et al. Maternal high-fat diet reduces type-2 neural stem cells and promotes premature neuronal differentiation during early postnatal development. Nutrients. 2022;14:2813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mishra V, Shuai B, Kodali M, Shetty GA, Hattiangady B, Rao X, et al. Resveratrol treatment after status epilepticus restrains neurodegeneration and abnormal neurogenesis with suppression of oxidative stress and inflammation. Sci Rep. 2015;5:17807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Muthuraju S, Pati S. Effect of hypobaric hypoxia on cognitive functions and potential therapeutic agents. Malays J Med Sci. 2014;21:41–5. [PMC free article] [PubMed] [Google Scholar]
- 29.Ling J, Yu Q, Li Y, Yuan X, Wang X, Liu W, et al. Edaravone improves intermittent hypoxia-induced cognitive impairment and hippocampal damage in rats. Biol Pharm Bull. 2020;43:1196–201. [DOI] [PubMed] [Google Scholar]
- 30.Jiao S-S, Yao X-Q, Liu Y-H, Wang Q-H, Zeng F, Lu J-J, et al. Edaravone alleviates Alzheimer’s disease-type pathologies and cognitive deficits. Proc Natl Acad Sci USA. 2015;112:5225–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang S, Kong D-W, Ma G-D, Liu C-D, Yang Y-J, Liu S, et al. Long-term administration of salvianolic acid A promotes endogenous neurogenesis in ischemic stroke rats through activating Wnt3a/GSK3β/β-catenin signaling pathway. Acta Pharmacol Sin. 2022;43:2212–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yang F, Zhou L, Song J, WangJinMei A, Yang Y, Tang Z-W, et al. Liver CEBPβ modulates the kynurenine metabolism and mediates the motility for hypoxia-induced central fatigue in mice. Front Physiol. 2019;10:243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kushwaha AD, Varshney R, Saraswat D. Effect of hypobaric hypoxia on the fiber type transition of skeletal muscle: a synergistic therapy of exercise preconditioning with a nanocurcumin formulation. J Physiol Biochem. 2023;79:635–52. [DOI] [PubMed] [Google Scholar]
- 34.Suresh A, Biswas A, Perumal S, Khurana S. Periostin and integrin signaling in stem cell regulation. Adv Exp Med Biol. 2019;1132:163–76. [DOI] [PubMed] [Google Scholar]
- 35.Dorafshan S, Razmi M, Safaei S, Gentilin E, Madjd Z, Ghods R. Periostin: biology and function in cancer. Cancer Cell Int. 2022;22:315. [DOI] [PMC free article] [PubMed]
- 36.Kanamaru H, Kawakita F, Nakano F, Miura Y, Shiba M, Yasuda R, et al. Plasma periostin and delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Neurotherapeutics. 2019;16:480–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sánchez-Sánchez JL, Ader I, Jeanson Y, Planat-Benard V, Vellas B, Casteilla L, et al. Periostin plasma levels and changes on physical and cognitive capacities in community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2023;78:424–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dong X-Q, Yu W-H, Du Q, Wang H, Zhu Q, Yang D-B, et al. Serum periostin concentrations and outcomes after severe traumatic brain injury. Clin Chim Acta. 2017;471:298–303. [DOI] [PubMed] [Google Scholar]
- 39.Sun X-J, Ma W-Q, Zhu Y, Liu N-F. POSTN promotes diabetic vascular calcification by interfering with autophagic flux. Cell Signal. 2021;83:109983. [DOI] [PubMed] [Google Scholar]
- 40.Wang Q-N, Yan Y-Z, Zhang X-Z, Lv J-X, Nie H-P, Wu J, et al. Rescuing effects of periostin in advanced glycation end-products (AGEs) caused osteogenic and oxidative damage through AGE receptor mediation and DNA methylation of the CALCA promoter. Chem Biol Interact. 2022;354:109835. [DOI] [PubMed] [Google Scholar]
- 41.Guo X, Xue H, Shao Q, Wang J, Guo X, Chen X, et al. Hypoxia promotes glioma-associated macrophage infiltration via periostin and subsequent M2 polarization by upregulating TGF-beta and M-CSFR. Oncotarget. 2016;7:80521–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li Q, Xu Z, Fang F, Shen Y, Lei H, Shen X. Identification of key pathways, genes and immune cell infiltration in hypoxia of high-altitude acclimatization via meta-analysis and integrated bioinformatics analysis. Front Genet. 2023;14:1055372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Park H-Y, Jung W-S, Kim S-W, Kim J, Lim K. Effects of interval training under hypoxia on hematological parameters, hemodynamic function, and endurance exercise performance in amateur female runners in Korea. Front Physiol. 2022;13:919008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rohm I, Aderhold N, Ratka J, Goebel B, Franz M, Pistulli R, et al. Hypobaric hypoxia in 3000 m altitude leads to a significant decrease in circulating plasmacytoid dendritic cells in humans. Clin Hemorheol Microcirc. 2016;63:257–65. [DOI] [PubMed] [Google Scholar]
- 45.Khodr B, Howard J, Watson K, Khalil Z. Effect of short-term and long-term antioxidant therapy on primary and secondary ageing neurovascular processes. J Gerontol A Biol Sci Med Sci. 2003;58:B698–B708. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.