Dear Editor,
We read with great interest the recent article by Tobing et al.7) concerning a surgical technique in which the temporal muscle is unseparated from the dura mater to avoid muscle damage and chewing impairment after cranioplasty. The authors describe their experience in twenty-three patients submitted to decompressive craniectomy for severe head injury, malignant ischemia, or hemorrhagic stroke. The well-known difficulty in dissecting the temporal muscle from the dura mater in the cranioplasty procedure supports the author’s proposed reconstructive technique, in which the autologous bone flap, titanium mesh, or bone cement are placed above the temporal muscle, still attached to the dura mater. In our previous paper on preservation of the temporal muscle in decompressive craniectomy to avoid adherence of the temporal muscle to the dura mater, we suggested placing a polyethylene sheet under the temporal muscle and skin flap.4) A polyethylene sheet has been previously applied in neurosurgery following craniectomy for craniosynostosis, in which a polyethylene film to retard the regrowth of bone was sewn in place with silk sutures.2) Polyethylene is a common polymer material that exhibits minimal foreign body reaction and is mostly used for packaging. As an implant in humans, it has been proven to be stable for many years.1,3,5,6,8) Our very long experience in the use of a temporary implant in the extradural compartment after decompressive craniectomy corroborates its use, given the lack of surgical complications and indisputable benefits in the cranioplastic reconstruction due to absence of adherence with the surrounding tissues. Once the polyethylene sheet has been placed in the decompressive craniectomy, in the cranioplasty procedure the skin flap and the temporal muscle are found already detached from the dura mater (FIGURE 1). If the polyethylene sheet has been placed only under the temporal muscle, the external surface of the temporal muscle which adheres to the subcutaneous tissue, may be left untouched. The plastic sheet never adheres to the tissues, whereas the temporal muscle, covered by a thin layer of connective tissue, shows a variable degree of retraction of the edges. In our patients, no infections occurred, and epidural hematoma, which is a known complication after decompressive craniectomy, is prevented through a large surgical drain placed partly epidural and partly subcutaneous through a small slot in the polyethylene sheet. Today, we can confirm the effectiveness and benefits of this inexpensive device, which can serve as the sterilized envelope of a surgical drainage bag.
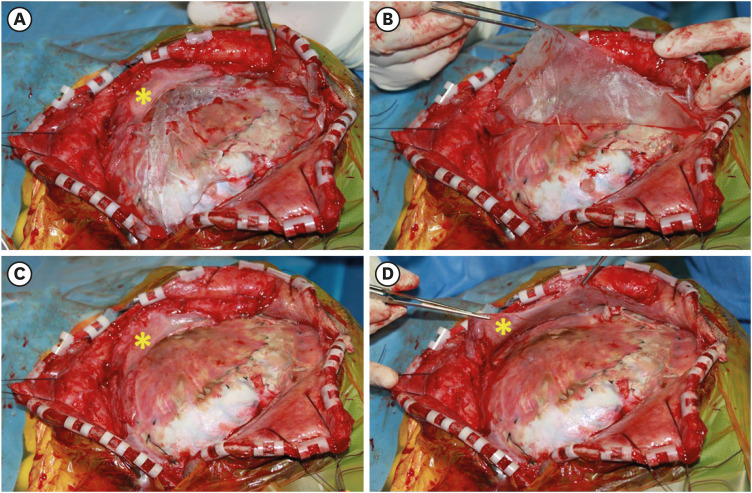
FIGURE 1. Intraoperative findings in the reconstructive procedure after decompressive craniectomy. (A) After opening of the cutaneous and subcutaneous tissue without any adherence, the polyethylene sheet previously placed in the decompressive craniectomy under the temporal muscle and subcutaneous tissue, lie on the dura mater and an added strip of dural patch. The external surface of the temporal muscle (yellow asterisk) is covered by a thin layer of connective tissue, unlike the dural patch which does not have any overlying connective tissue. (B) The polyethylene sheet can be lift and removed without any adherence. (C) Note the connective tissue covering the dura mater. (D) The partially retracted temporal muscle is raised to show the internal surface and the absence of any adherence. After scraping of the bone edges, the autologous bone flap can be placed and fixed with titanium microplates.
The second remark concerns the placement of the bone flap over the temporal muscle, unseparated from the dura mater. This surgical choice may be very effective in some patients who would benefit from a variable indirect revascularization process—i.e., encephalo-myo-synangiosis— from the temporal muscle to the dura mater, subdural area, or brain surface. Obviously, if the neurosurgeon wishes to try this option, the dura mater must have some openings created during decompressive craniectomy to facilitate synangiosis, which provides new blood flow to the ischemic brain tissue. There are no clinical studies on this matter; however, the growth of new capillaries and arteries in the brain—as in some patients with Moyamoya disease—cannot be excluded. However, the esthetic result of the proposed technique may be undesirable, given that a lump may result in the skin immediately above the zygomatic arch due to the lower portion of the bone flap being pushed by the underlying retracted temporal muscle. The final issue is the fusion of the bone flap if the autologous bone is reimplanted. The inferior bone edges of the craniectomy are covered by the temporal muscle, which can partly prevent the fusion of the bone flap and increase its resorption risk.
In conclusion, we greatly appreciate the findings of Tobing et al.,7) as they enhance our awareness of the risks of damaging the temporal muscle, its functional anatomy, and the esthetic issues that can result in this surgical procedure.
Footnotes
Funding: No funding was obtained for this study.
Conflict of Interest: The authors have no financial conflicts of interest.
References
- 1.Couldwell WT, Chen TC, Weiss MH, Fukushima T, Dougherty W. Cranioplasty with the Medpor porous polyethylene flexblock implant. Technical note. J Neurosurg. 1994;81:483–486. doi: 10.3171/jns.1994.81.3.0483. [DOI] [PubMed] [Google Scholar]
- 2.Fowler FD, Ingraham FD. A new method for applying polyethylene film to the skull in the treatment of craniosynostosis. J Neurosurg. 1957;14:584–586. doi: 10.3171/jns.1957.14.5.0584. [DOI] [PubMed] [Google Scholar]
- 3.Liu JK, Gottfried ON, Cole CD, Dougherty WR, Couldwell WT. Porous polyethylene implant for cranioplasty and skull base reconstruction. Neurosurg Focus. 2004;16:ECP1. doi: 10.3171/foc.2004.16.3.14. [DOI] [PubMed] [Google Scholar]
- 4.Missori P, Paolini S, Ciappetta P, Seferi A, Domenicucci M. Preservation of the temporal muscle during the frontotemporoparietal approach for decompressive craniectomy: technical note. Acta Neurochir (Wien) 2013;155:1335–1339. doi: 10.1007/s00701-013-1695-z. [DOI] [PubMed] [Google Scholar]
- 5.Perozzo FA, Ku YC, Kshettry VR, Sikder P, Papay FA, Rampazzo A, et al. High-density porous polyethylene implant cranioplasty: a systematic review of outcomes. J Craniofac Surg. 2024;35:1074–1079. doi: 10.1097/SCS.0000000000010135. [DOI] [PubMed] [Google Scholar]
- 6.Rubin JP, Yaremchuk MJ. Complications and toxicities of implantable biomaterials used in facial reconstructive and aesthetic surgery: a comprehensive review of the literature. Plast Reconstr Surg. 1997;100:1336–1353. doi: 10.1097/00006534-199710000-00043. [DOI] [PubMed] [Google Scholar]
- 7.Tobing HG, Santoso F, Satriawan RR, Nafisah ZF, Paat BE, Wayne TM. Unseparated temporal muscle and duramater cranioplasty methods following decompressive craniectomy: technical note. Korean J Neurotrauma. 2024;20:101–107. doi: 10.13004/kjnt.2024.20.e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wellisz T, Dougherty W, Gross J. Craniofacial applications for the Medpor porous polyethylene flexblock implant. J Craniofac Surg. 1992;3:101–107. doi: 10.1097/00001665-199209000-00009. [DOI] [PubMed] [Google Scholar]