Abstract
Background:
Vertebral artery (VA) stump syndrome (VASS) is an embolic source for cerebral infarction (CI) in the posterior circulation after VA occlusion.
Case Description:
A 63-year-old patient with a history of hypertension presented to our emergent department with dizziness, vomiting, and gait disturbance. Head magnetic resonance imaging (MRI) showed acute CIs in the bilateral cerebellar hemispheres and the vermis. Magnetic resonance angiography revealed patency of the VA and basilar artery. Left subclavian artery digital subtraction angiography (DSA) revealed severe left VA orifice stenosis and collateral flow from the deep cervical artery into the left V2 segment. Right VA angiography showed retrograde flow to the left V4 segment, branching bihemispheric posterior inferior cerebellar artery (PICA), and to-and-flow appearance in the proximal PICA segment and VA. VASS was diagnosed, and conservative treatment with aspirin was administered. Worsened nausea and gait disturbance had developed during hospitalization. MRI revealed an enlarged posterior circulation CI. Follow-up DSA revealed proximal to-and-flow appearance translocation to the proximal V4 segment and poor PICA flow. We performed proximal V4 segment parent artery occlusion (PAO) by endovascular therapy. No recurrence of symptoms or CI was observed. The patient was discharged on day 32 of hospitalization with 1 on the modified Rankin scale.
Conclusion:
We reported a rare case of VASS involving bihemispheric PICA. No CI recurrence was observed after performing PAO of the proximal V4 segment. When treating acute cases of bilateral cerebellar CI due to VASS, the contribution of PICA variations should be considered.
Keywords: Bihemispheric posterior inferior cerebellar artery, Parent artery occlusion, Vertebral stump syndrome
INTRODUCTION
The carotid artery stump has been well-reported as an embolic source for ischemic strokes.[1] The rare vertebral artery (VA) stump syndrome (VASS) could cause an embolic stroke in the posterior circulation and is associated with a high risk of recurrence.[4,6] We report the first case of VASS involving a bihemispheric posterior inferior cerebellar artery (PICA), a rare PICA variant, and the successful endovascular treatment performed.
CASE REPORT
A 63-year-old male with a history of hypertension presented to our hospital’s Emergency Department with dizziness, vomiting, and gait disturbance. Head magnetic resonance (MR) imaging (MRI) revealed acute cerebral infarctions (CIs) in the vermis and bilateral cerebellar hemispheres [Figure 1a]. MR angiography detected a poorly visualized left V4 segment [Figure 1b]. A conservative treatment with aspirin was administered on admission. Left subclavian artery digital subtraction angiography (DSA) revealed severe stenosis in the VA origin, with a delayed anterograde flow in the VA and collateral flow from the deep cervical artery to the V2 segment [Figures 2a and b]. The anterograde flow was diminished in the V3 segment. Right VA angiography showed retrograde flow from the right to the left V4 segment through the union, with a to-and-flow lesion in the proximal portion of the V4 segment [Figure 2c]. Three-dimensional rotational angiography revealed a bihemispheric PICA variant [Figure 2d]. VASS associated with bihemispheric PICA was diagnosed. The medication treatment was maintained. On hospitalization day 14, the dizziness and gait disturbance symptoms worsened. MRI revealed an enlarged CI [Figure 2e]. MR angiography showed a shortening of the left V4 segment [Figure 2f]. Repeated late-phase VA angiography detected poor left PICA condition and extension of the to-and-flow lesion from the V3 segment of the VA to the PICA orifice [Figure 2g]. We concluded that the discrepancy in the VA showed by MR angiography and the late phase of the VA angiography indicated a stagnated flow that could lead to new thrombi formation. We performed parent artery occlusion (PAO) to prevent recurrent stroke and repeated embolism.
Figure 1:
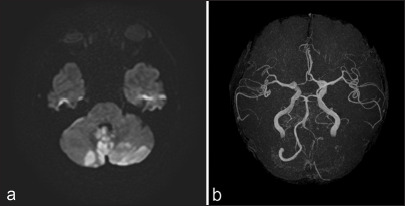
(a) Initial head magnetic resonance (MR) imaging reveals bilateral cerebellar infarctions. , (b) The MR angiography does not depict the left V4 segment of the vertebral artery (VA).
Figure 2:
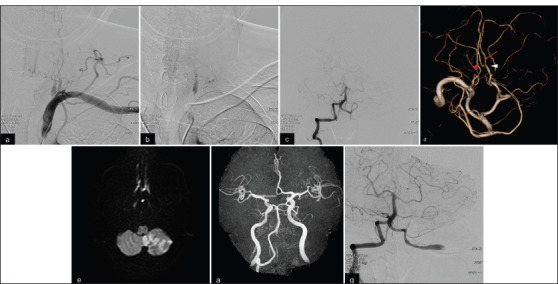
(a, b) Left subclavian artery angiography shows severe stenosis of the left VA with stagnated distal blood flow and collateral flow from the deep cervical artery to the V2 segment. (c) Right VA angiography reveals retrograde flow to the left V4 segment, which extended to the left posterior inferior cerebellar artery (PICA), and a to-and-flow appearance in the intracranial VA. (d) Three-dimensional rotation angiography reveals a bihemispheric PICA. White arrowhead, the supratonsillar segment of the left PICA; red arrow, the left hemispheric branch; red arrowhead, the right hemispheric branch. (e,f) Follow-up magnetic resonance (MR) imaging reveals enlarged cerebellar infarction, and MR angiography shows poorly visualized left VA. (g) Repeated DSA shows poor filling of the left PICA and proximal translocation of the to-and-flow appearance.
With the patient under general anesthesia, a 6 Fr sheath introducer was inserted through the right femoral artery. A 6 Fr ENVOY catheter (Cerenovus, Fremont, CA, USA) was navigated to the right VA. An intermediate catheter (Guidepost; Tokai Medical Products, Aichi, Japan) was then advanced to the VA near the union. A microcatheter (Headway Duo, Terumo, Tokyo, Japan) was guided to the V3 segment of the left VA using a microwire (SynchroSELECT soft; Stryker, Freemont, CA, USA; Figure 3a). PAO, performed with coils, occluded the V3 segment [Figure 3b]. Post-treatment DSA revealed retrograde flow from the right VA to the left V4 segment, with good filling of the PICA.
Figure 3:

(a) An intermediate catheter (arrowhead) and microcatheter (arrow) were introduced into the right V4 and left V3 segments, respectively. (b) Parent artery occlusion with coils was performed in the left extracranial vertebral artery. (c) Postoperative magnetic resonance imaging reveals no new ischemic infarctions.
Head MRI on the following day showed no new acute CIs [Figure 3c], and symptoms did not worsen after the treatment. Rehabilitation was performed, and the patient was discharged home on day 32 of hospitalization with a score of 1 on the modified Rankin scale.
DISCUSSION
VASS was first reported by Nguyen et al.[6] as a recurrent posterior circulation stroke due to VA origin occlusion. To the best of our knowledge, this is the first case of VASS associated bihemispheric PICA, which perfuses bilateral cerebellum. Kawano et al.[4] proposed the following definitive diagnostic criteria for VASS: (1) acute ischemic stroke in the posterior circulation; (2) VA origin occlusion detected on MR angiography, duplex ultrasonography, three-dimensional computed tomography angiography, and/or DSA; (3) distal anterograde flow in the ipsilateral VA; and (4) absence of other ischemic stroke causes. Our patient experienced an acute cerebellar stroke due to severe stenosis in the left VA origin. The anterograde flow in the left VA was preserved, assisted by collateral flow from the deep cervical artery, and a to-and-flow appearance was observed in the ipsilateral distal V3 segment. Based on these findings, we judged that the left VA origin was nearly occluded. The to-and-flow appearance site in the ipsilateral VA changed with every DSA. When the acute CI increased, the responsible PICA was found to be in a poor condition. These findings confirmed the diagnosis of VASS. Furthermore, we detected angiographical changes at the flow stagnation site; these changes could lead to thrombosis.[4]
In this case, the bilateral VASS and PICA lesions resulted in bilateral CIs. The patient had a bihemispheric PICA because the left PICA exhibited a rare variation. PICA variations, like anterior inferior cerebellar artery-PICA complex or hypoplasia, were reported, but bihemispheric PICA is rare.[2] To the best of our knowledge, we reported the first case of VASS associated with a bihemispheric PICA. The PICA and VASS variants should be considered when treating patients with bilateral CIs dominated by bilateral PICA and VA origin occlusion.
No standard treatment for VASS has been established. Kawano et al.[4] demonstrated that the recurrence rate in the non-medication group was higher than in the anticoagulation therapy group. Therefore, they recommended anticoagulation therapy to prevent recurrent stroke. Conversely, Suzuki et al.[8] reported a patient with VASS treated with antiplatelet therapy. Like them, we considered that the disease pathogenesis was artery-to-artery embolism due to atherosclerotic changes, prescribing initially conservative treatment with aspirin. Medical treatment should be considered on a case-by-case basis.
Endovascular therapy is an additional treatment to prevent recurrence, especially when the medical treatment has failed. Several studies reported using coil embolization of the proximal portion of the ipsilateral VA.[3,5,6] Endovascular revascularization using percutaneous transluminal angioplasty or stent is an alternative strategy following mechanical thrombectomy for basilar or posterior cerebral artery occlusion.[7,9] This strategy is useful for acute stroke with major trunk occlusion in these arteries. In this case, we performed PAO through the contralateral VA and occluded the distal site where the thrombus was estimated to form due to the stagnated blood flow. This method is most suitable for preventing new embolization. It is also considered safe due to the access root, as the device avoids the dangerous zone involving the thrombus.
Our patient presented bilateral CIs due to VASS, which was associated with a rare PICA variant, a bihemispheric PICA. Despite the antiplatelet therapy, the stagnated blood flow at the intracranial VA continued to produce new thrombi. We performed endovascular PAO in the extracranial VA through the contralateral VA, assuming embolism could not occur given the VA occlusion by coils distal to the lesion, where thrombi might form. We should consider the possibility of VASS with a PICA variant as the cause of stroke when treating patients with bilateral CIs and occlusion in the VA origin.
CONCLUSION
We believe that we reported the first case of a patient with VASS associated with a bihemispheric PICA. No recurrent CI was observed after performing endovascular PAO in the extracranial VA. When treating patients with acute bilateral CIs due to VASS, we should consider the possible contribution of PICA variations.
Footnotes
How to cite this article: Morimoto T, Fujimoto K, Ko S, Nishioka T, Tokunaga H. Vertebral artery stump syndrome associated with a bihemispheric posterior inferior cerebellar artery. Surg Neurol Int. 2024;15:350. doi: 10.25259/SNI_488_2024
Contributor Information
Takayuki Morimoto, Email: t.morimoto@naramed-u.ac.jp.
Kenta Fujimoto, Email: kentaf@nara-hp.jp.
Sung-Chul Ko, Email: chocchenchocho@gmail.com.
Toshikazu Nishioka, Email: t-nishioka@nara-jadecom.jp.
Hidemori Tokunaga, Email: h-tokunaga@nara-jadecom.jp.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Barnett HJ, Peerless SJ, Kaufmann JC. “Stump” on internal carotid artery--a source for further cerebral embolic ischemia. Stroke. 1978;9:448–56. doi: 10.1161/01.str.9.5.448. [DOI] [PubMed] [Google Scholar]
- 2.Carlson AP, Alaraj A, Dashti R, Aletich VA. The bihemispheric posterior interior cerebellar artery: Anatomic variations and clinical relevance in 11 cases. J Neurointerv Surg. 2013;5:601–4. doi: 10.1136/neurintsurg-2012-010527. [DOI] [PubMed] [Google Scholar]
- 3.Ji R, Li B, Xu Z. Retrograde recanalisation for vertebral artery stump syndrome: A case report. Stroke Vasc Neurol. 2022;7:462–4. doi: 10.1136/svn-2021-001407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kawano H, Inatomi Y, Hirano T, Yonehara T. Vertebral artery stump syndrome in acute ischemic stroke. J Neurol Sci. 2013;324:74–9. doi: 10.1016/j.jns.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 5.Maeoka R, Nakagawa I, Ohnishi H, Kuga Y, Nakase H, Ohnishi H. A thread of hope for successful revascularization for acute embolic basilar artery occlusion due to miserable vertebral artery stump syndrome. A technical report. J Clin Neurosci. 2020;73:299–303. doi: 10.1016/j.jocn.2020.01.073. [DOI] [PubMed] [Google Scholar]
- 6.Nguyen TN, Raymond J, Mahmoud M, Weill A, Roy D, Guilbert F. Vertebral artery stump syndrome. J Neurol Neurosurg Psychiatry. 2008;79:91–2. doi: 10.1136/jnnp.2007.124826. [DOI] [PubMed] [Google Scholar]
- 7.Okamoto A, Nakagawa I, Kotsugi M, Yokoyama S, Yamada S, Park YS, et al. Endovascular vertebral artery orifice angioplasty for the prevention of acute ischemic stroke following vertebral artery stump syndrome. Surg Neurol Int. 2022;13:382. doi: 10.25259/SNI_515_2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Suzuki M, Dembo T, Hara W, Tajima T, Yamashita M, Oji S, et al. Vertebral artery stump syndrome. Intern Med. 2018;57:733–6. doi: 10.2169/internalmedicine.9317-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yamano A, Nakai Y, Akutagawa K, Igarashi H, Tsukada K, Terakado T, et al. Fatal recurrent ischemic stroke caused by vertebral artery stump syndrome. Surg Neurol Int. 2021;12:445. doi: 10.25259/SNI_384_2021. [DOI] [PMC free article] [PubMed] [Google Scholar]


