Abstract
Background
Increases in low-density lipoprotein cholesterol (LDL-C) can occur on carbohydrate restricted ketogenic diets. Lean metabolically healthy individuals with a low triglyceride-to-high-density lipoprotein cholesterol ratio appear particularly susceptible, giving rise to the novel “lean mass hyper-responder” (LMHR) phenotype.
Objectives
The purpose of the study was to assess coronary plaque burden in LMHR and near-LMHR individuals with LDL-C ≥190 mg/dL (ketogenic diet [KETO]) compared to matched controls with lower LDL-C from the Miami Heart (MiHeart) cohort.
Methods
There were 80 KETO individuals with carbohydrate restriction-induced LDL-C ≥190 mg/dL, high-density lipoprotein cholesterol ≥60 mg/dL, and triglyceride levels ≤80 mg/dL, without familial hypercholesterolemia, matched 1:1 with MiHeart subjects for age, gender, race, hyperlipidemia, hypertension, and smoking status. Coronary artery calcium and coronary computed tomography angiography (CCTA) were used to compare coronary plaque between groups and correlate LDL-C to plaque levels.
Results
The matched mean age was 55.5 years, with a mean LDL-C of 272 (maximum LDL-C of 591) mg/dl and a mean 4.7-year duration on a KETO. There was no significant difference in coronary plaque burden in the KETO group as compared to MiHeart controls (mean LDL 123 mg/dL): coronary artery calcium score (median 0 [IQR: 0-56]) vs (1 [IQR: 0-49]) (P = 0.520) CCTA total plaque score (0 [IQR: 0-2] vs [IQR: 0-4]) (P = 0.357). There was also no correlation between LDL-C level and CCTA coronary plaque.
Conclusions
Coronary plaque in metabolically healthy individuals with carbohydrate restriction-induced LDL-C ≥190 mg/dL on KETO for a mean of 4.7 years is not greater than a matched cohort with 149 mg/dL lower average LDL-C. There is no association between LDL-C and plaque burden in either cohort. (Diet-induced Elevations in LDL-C and Progression of Atherosclerosis [Keto-CTA]; NCT057333255)
Key words: atherosclerosis, coronary CT angiography, ketogenic diet, LDL cholesterol, lean mass hyper-responder, plaque
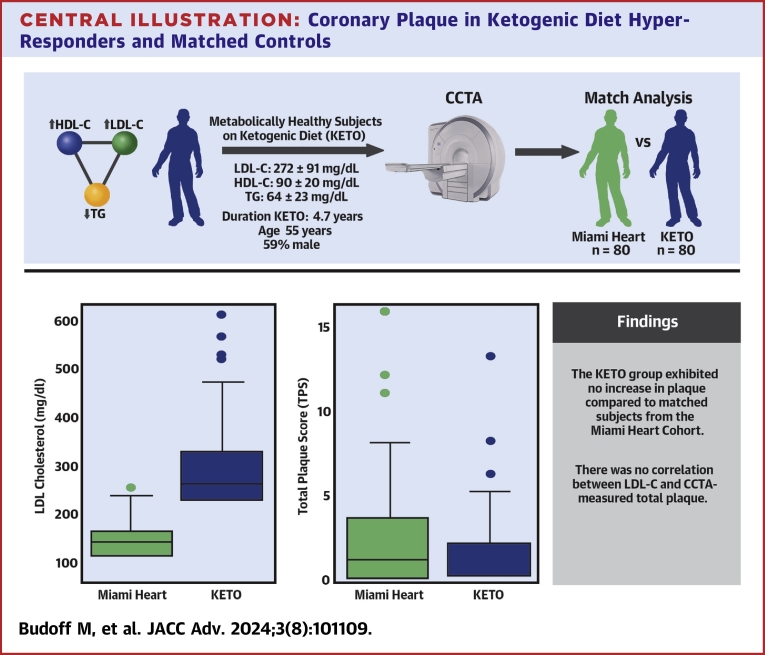
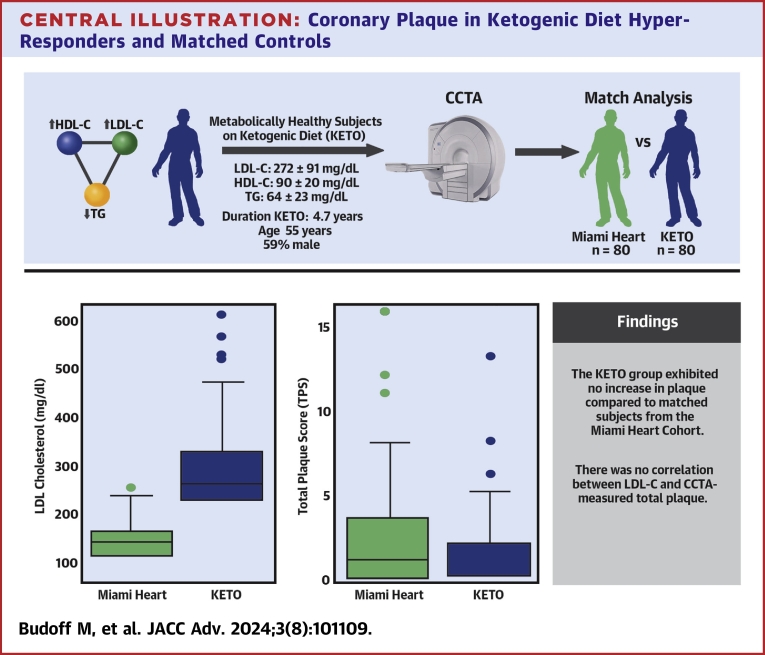
Central Illustration
Despite medical innovations, atherosclerotic cardiovascular disease (ASCVD) remains the leading cause of mortality in the United States and the developed world.1 Standard of care seeks to reduce low-density lipoprotein cholesterol (LDL-C) and its major carrier protein, ApoB,2 well-known risk factor for ASCVD. Lipid-lowering medications, including statins, ezetimibe, and PCSK9 inhibitors, primarily target LDL-C and have shown efficacy in high-risk populations for cardiovascular event reduction.3 The persistent burden of ASCVD may be due, in large part, to other risk factors that are generally less amenable to pharmacotherapy, including insulin resistance, and atherogenic dyslipidemia, among others.1,4
The majority of the clinical trials involving lipid-lowering therapy have a high preponderance of patients considered “metabolically unhealthy,” as determined by the presence of criteria for metabolic syndrome.
Carbohydrate-restricted diets (CRDs) including ketogenic diets (KETO) that typically include <25 g/d carbohydrate to induce the metabolic state of nutritional ketosis—have gained popularity among the public for weight loss, diabetes management, as well as for non-obesity-related conditions such as treatment of epilepsy,5 neurodegenerative diseases and mental health diseases,6, 7, 8 polycystic kidney disease,9 and other chronic conditions. Change in LDL-C among studies on KETO vary widely, ranging from decreases in LDL-C10,11 to moderate or large increases in LDL-C.12,13
While heterogeneity in LDL-C response to CRD is multifactorial (including contribution from permissive genetics, saturated fat, and fiber intake), studies including subjects with normal body mass index (BMI) (<25 kg/m2; cited above12,13) appear more likely to exhibit increases in LDL-C with carbohydrate restriction, with evidence for an inverse association between BMI and LDL-C change with carbohydrate restriction.13
In fact, a set of recent meta-analyses of 41 randomized controlled human trials including <130 g/d carbohydrates found that LDL-C increased only in trials including subjects with “normal” (lean) BMI <25 kg/m2, whereas LDL-C did not change in studies of subjects with overweight or class I obesity and decreased in subjects with class II obesity.14
Lean mass hyper-responders (LMHRs) are individuals who, upon adopting a CRD, exhibit striking increases in LDL-C to ≥200 mg/dL, in conjunction with elevated high-density lipoprotein cholesterol (HDL-C) ≥80 mg/dL and triglycerides ≤70 mg/dL.13,15 Of note, the phenotype is defined only by this triad of lipid markers and not definitionally by any marker of “leanness,” although LMHR is typified by also being of low-normal BMI.
Recent advances and increased utilization of clinical imaging techniques such as coronary artery calcium (CAC) scans and coronary computed tomography angiography (CCTA) allow us to interrogate coronaries and the presence and burden of atherosclerotic plaque. Multiple studies have previously used CCTA and plaque quantification for the evaluation of progression or regression of ASCVD. Gathering prospective CCTA data on LMHRs will provide novel data, given that their high LDL-C/ApoB exists largely in the absence of other traditional ASCVD risk factors or genetic lipid dysregulation.
Thus, to provide first evidence on relative coronary plaque burden in LMHR and near-LMHR individuals, we sought to test whether individuals with this phenotype and LDL-C ≥190 mg/dL (mean 272 mg/dL), for a mean of 4.7 years and drawn from the parent prospective KETO-CCTA study, exhibited different coronary plaque burden compared to individuals matched 1:1 from the population-based MiHeart (Miami Heart) cohort. These data, combined with those that will be produced by the parent prospective study, will provide preliminary evidence, laying the groundwork for future investigation of risk associated with elevated LDL-C in metabolically healthy persons with CRD.
Methods
Prospective parent (KETO) study
The original KETO study is designed to measure the progression of subclinical coronary atherosclerosis in participants exhibiting the LMHR or near-LMHR phenotypes, with LDL-C ≥190 mg/dL, HDL-C ≥60 mg/dL, and triglycerides ≤80 mg/dL, prospectively over a 1-year period by cardiac CCTA. Loser lipid criteria than previously cited LMHR criteria were used to increase study generalizability and increase the chances that recruitment goals were met in line with additional recruitment criteria, including but not limited to.
-
•
LDL-C ≥190 mg/dL for ≥24 months prior to enrollment, on a CRD
-
•
HDL-C ≥60 mg/dL and triglycerides ≤80 mg/dL
-
•
Negative for genetic familial hypercholesterolemia
-
•
Normal blood pressure
-
•
No use of medications that would alter lipid levels
CCTA and CAC imaging
CCTA images were used to evaluate each segment based on the amount of plaque and severity of stenosis according to the methods previously published.16 In each coronary artery segment, coronary atherosclerosis was defined as tissue structure >1 mm2 that existed within the coronary lumen that could be differentiated from surrounding epicardial fat, pericardial tissue, and vessel lumen itself. A total plaque score (TPS) was developed to semiquantitate the plaque in each participant with the use of the 15-segment American Heart Association model of the coronary arteries. Each plaque was assigned a score of 1 when plaque volume was small, 2 for medium plaque volume, and 3 for large plaque volume. TPS per person was determined by summing the number of interpretable coronary segments (maximum of 15 segments) with individual plaque scores (range 1-3). Segment involvement score (SIS) was graded as normal (no stenosis), stenosis 1% to 29%, 30% to 49%, 50% to 69%, >70% by visual semiquantification method, with assignment of scores of 0, 1, 2, 3, or 4, respectively. Stenosis was not measured when the vessel diameter was <2 mm. Total stenosis score (TSS) per person was calculated by summing all the 15 individual segment stenosis score with a possible score ranging from 0 to 60. The Lundquist Institute CCTA core lab made all measures using level 3 expert readers. The lab’s performance on measures of interobserver variations of plaque severity score and segment stenosis score have been previously reported.16
Participants underwent electrocardiogram-gated CAC assessment on multidetector computed tomography (Revolution 256, General Electric Healthcare Technologies). Each scan extended from 1 cm below the carina to the bottom of the heart for a complete acquisition. Scan parameters included prospective electrocardiogram-triggering, field of view was fixed at 25 cm, 512 × 512 matrix size, and a peak tube voltage of 120 kV. CAC was quantified using the validated Agatston score method 21. CAC measurements were performed on dedicated workstations using AW VolumeShare TM (GE Medical Systems).
Statistical methods
All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc). There were 80 subjects from the prospective parent KETO study matched, 1:1, with subjects from the population-based MiHeart cohort study for age, gender, race, diabetes mellitus, hypertension, hyperlipidemia, and past smoking status. There were 20 subjects from the prospective KETO study not matched because they fell outside the age range (40-65) for the MiHeart cohort. A subgroup analysis of 35 individuals meeting full LMHR criteria of LDL-C ≥200 mg/dL, HDL-C ≥80 mg/dL, and triglycerides ≤70 mg/dL was also included. Continuous variables are presented as mean ± SD unless otherwise noted for nonparametric variables. Categorical variables are reported as frequencies with percentages. The Wilcoxon rank-sum test evaluated CAC and CCTA outcomes between groups. A supplemental multivariable linear regression was performed, with CCTA and CAC as outcome variables and cohort, age, and BMI serving as covariates. This analysis aimed to address the lower BMI among individuals in the KETO cohort. The Spearman correlation assessed the potential relationship between LDL-C and TPS specifically. All tests were 2-tailed, and statistical significance was defined as a P value <0.05. The study was approved by the institutional review board at The Lundquist Institute.
Results
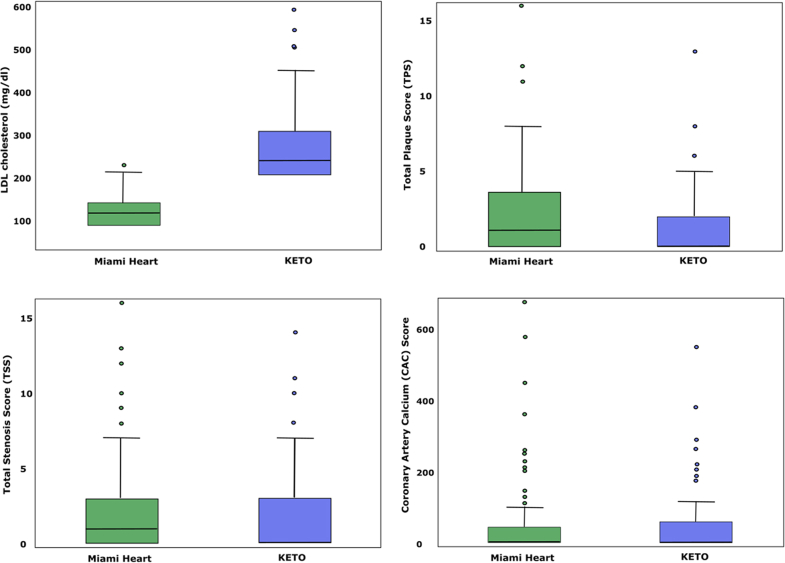
Subjects from both the KETO study and matched MiHeart cohort had a mean age of 55.5 years, and were 59% male, and primarily identified as White (90%). Systolic blood pressure measurements and HbA1c levels were similar between groups. KETO subjects had been on KETO for 4.7 ± 2.8 years and exhibited total cholesterol of 369 ± 95 mg/dL and LDL-C of 272 ± 91 mg/dL, as compared to 205 ± 40 mg/dL and 123 ± 38 mg/dL for MiHeart subjects (Figure 1). As LMHR subjects as a population are, typically, quite lean compared to the general population, perfect matching on BMI was not possible: mean BMI for the KETO group was 22.5 ± 2.7 kg/m2 as compared to 25.8 ± 3.6 kg/m2 for the MiHeart group. Corresponding HDL-C and triglycerides for the 2 cohorts were 90 ± 20 mg/dL and 64 ± 23 mg/dL, versus 63 ± 19 mg/dL and 96 ± 45 mg/dL, respectively (Table 1), again necessarily differing between groups because of the unique characteristics of the LMHR profile. Per protocol, KETO subjects had exhibited normal LDL-C levels (122 ± 36 mg/dL) prior to adoption of KETO and tested negative for genetic familial hypercholesterolemia. There were 44 (55%) of KETO subjects who presented with zero CAC and 38 (48%) of MiHeart subjects with CAC 0 (P = 0.423).
Figure 1.
Plaque Scores and LDL-C Level
Total plaque score (TPS) (green bars) and LDL-C (blue line) between n = 80 KETO subjects (left) matched 1:1 to 80 Miami Heart (MiHeart) subjects (right). Group TPS median, IQR, and mean LDL-C ± SD are provided in inset. KETO = ketogenic diet; LDL-C = low-density lipoprotein cholesterol.
Table 1.
Characteristics of 160 Total Subjects, 80 KETO Subjects Matched 1:1 to 80 MiHeart Subjects for Age, Gender, Race, Diabetes Mellitus, Hypertension, and Past Smoking Status
| KETO (n = 80) | MiHeart (n = 80) | P Value | |
|---|---|---|---|
| Age (y) | 55.5 ± 7.9 | 55.5 ± 7.4 | 0.951a |
| Duration on ketogenic diet (y) | 4.7 ± 2.8 | -- | |
| Body mass index (kg/m2) | 22.5 ± 2.7 | 25.8 ± 3.6 | <0.001a |
| Male (%) | 47 (59) | 47 (59) | - |
| Race | - | ||
| White, non-Hispanic | 72 (90) | 72 (90) | |
| Asian/Asian-Indian | 2 (3) | 2 (3) | |
| Hispanic | 6 (8) | 6 (8) | |
| Lipid markers | |||
| Total cholesterol, mg/dL | 369 ± 95 | 205 ± 40 | <0.001a |
| LDL-C, mg/dL | 272 ± 91 | 123 ± 38 | <0.001a |
| Non-HDL-C, mg/dL | 279 ± 90 | 142 ± 40 | <0.001a |
| HDL-C, mg/dL | 90 ± 20 | 63 ± 19 | <0.001a |
| Triglycerides, mg/dL | 64 ± 23 | 96 ± 45 | <0.001a |
| Other risk factors or medications | |||
| Systolic BP, mm Hg | 117 ± 12 | 116 ± 10 | 0.488a |
| Diastolic BP, mm Hg | 76 ± 8 | 73 ± 6 | 0.012a |
| hsCRP (mg/L) | 0.5 (0.3-0.9) | 0.7 (0.4-1.5) | 0.007b |
| Hemoglobin A1C (%) | 5.4 ± 0.3 | 5.5 ± 0.2 | 0.075a |
| Hyperlipidemia medication | 0 (0) | 26 (33) | - |
| Hypertension medication | 1 (1) | 0 (0) | - |
| Past smoker | 2 | 2 | - |
Values are Mean ± SD, n (%), or median (IQR).
BP = blood pressure; HDL-C = high-density lipoprotein cholesterol; hsCRP = high-sensitivity C-reactive protein; KETO = ketogenic diet; LDL-C = low-density lipoprotein cholesterol; MiHeart = Miami Heart.
Independent t-test.
Wilcoxon rank-sum test.
Median CAC score was 0 for KETO subjects (IQR: 0-56), and 1 for MiHeart subjects 0 (IQR: 0-49) (P = 0.520). Median CCTA TSS, TPS, and SIS, were all 0 for KETO subjects and 1 for MiHeart subjects, with no differences between groups (all P > 0.20) (Table 2). In multivariable regression analysis, there was no difference in CAC and CCTA outcomes with adjustment for BMI (and age) between KETO and MiHeart subjects (Supplemental Table 1). In the subset of KETO subjects meeting all 3 stricter LMHR criteria (35/80), median CAC score was 0 for KETO subjects (IQR: 0-47), and 0 for matched MiHeart subjects 0 (IQR: 0-23), P = 0.849. Median TSS, TPS, and SIS were all 0 for KETO subjects and 0 for matched MiHeart subjects, with no differences between groups (all P > 0.20), (Supplemental Table 2). There was no significant correlation between plaque burden, as measured by TPS, and LDL-C level in the fully matched group (r = 0.12, P = 0.29) (Figure 2) or subgroup (r = 0.05, P = 0.662).
Table 2.
CCTA Semiquantitative Measures Compared Between 80 KETO Subjects Matched 1:1 to 80 MiHeart Subjects
| KETO (n = 80) | MiHeart (n = 80) | P Value | |
|---|---|---|---|
| CAC score | 0 (0-56) | 1 (0-49) | 0.520 |
| CCTA scores | |||
| Total stenosis score | 0 (0-3) | 1 (0-3) | 0.357 |
| Total plaque score | 0 (0-2) | 1 (0-4) | 0.245 |
| Segment involvement score | 0 (0-2) | 1 (0-3) | 0.336 |
Values are median (IQR). Group comparisons performed by the Wilcoxon rank-sum test.
CAC = coronary artery calcium; CCTA = coronary computed tomography angiography; KETO = ketogenic diet; MiHeart = Miami Heart.
Figure 2.
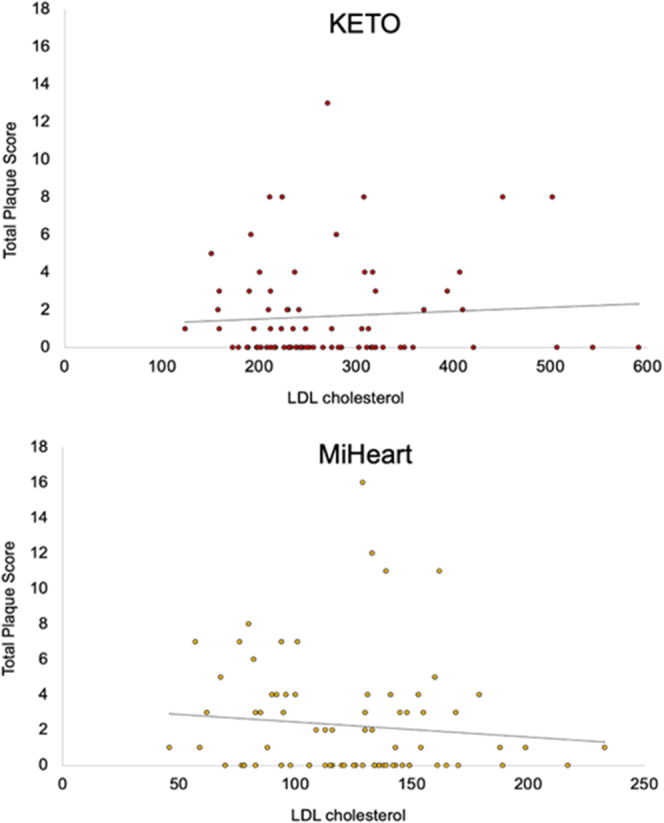
LDL-C Does Not Correlate With Total Plaque Score
Total plaque score (TPS) plotted against LDL-C (mg/dL), including between KETO subjects (top) matched 1:1 to 80 Miami Heart (MiHeart) subjects (bottom). X-axes are adjusted for group LDL-C range. Abbreviations as in Figure 1.
Discussion
Current ASCVD prevention guidelines recommend pharmacotherapy for LDL-C ≥190 mg/dL, irrespective of 10-year ASCVD risk score; however, there are limited data on ASCVD progression in individuals with elevated LDL-C in the absence of metabolic disease and/or familial hypercholesterolemia. This has raised questions as to whether the preponderance of existing data applies to those with the LMHR or near-LMHR phenotype on CRD or whether this phenotype might be an underappreciated physiological response with a possibly unique risk profile (Central Illustration).17
Central Illustration.
Coronary Plaque in Ketogenic Diet Hyper-Responders and Matched Controls
Coronary plaque was assessed by coronary CT angiography in cholesterol hyper-responders to a ketogenic diet (KETO) and a matched cohort (Miami Heart) (n = 80 each). There was no difference in plaque score between groups, and there was no correlation between LDL-C level and plaque burden. CCTA = coronary computed tomography angiography; CT = computed tomography; LDL-C = low-density lipoprotein cholesterol.
The parent (KETO) study is an observational prospective study designed to determine the effects of diet-induced hypercholesterolemia on atherosclerosis observed in persons at otherwise low risk of ASCVD. CCTA has been established as an exceptional quantitative technique to evaluate plaque burden, stenosis severity, and ASCVD risk. Similar plaque burden compared to matched controls from a population-based study (MiHeart) is inconsistent with the expectation that almost 5 years exposure to very high LDL-C in LMHR patients increases atherosclerosis. The prospective study will evaluate quantitative plaque changes over 1 year of exposure to very high LDL-C invoked by KETO, with an average LDL of 272 mg/dL.
Although clinical caution should be exercised,15 while complete data on this unique phenotype are outstanding, the questions are scientifically legitimate: what is the absolute level of risk associated with elevated LDL-C in otherwise metabolically healthy persons on CRD, and why does this response occur?
One hypothesis to explain the emergence of LMHR-spectrum phenotype in CRD is the lipid energy model, which posits that the lipid triad of high LDL-C, high HDL-C, and low triglycerides arises in the context of relatively lean people adopting carbohydrate restriction to meet systemic energy needs. Typically, when a relatively lean, metabolically healthy person assumes carbohydrate restriction sufficient to deplete hepatic glycogen stores, increased free fatty acids released by adipocytes are taken up by hepatocytes and resynthesized into very low-density lipoproteins (VLDL). Increased VLDL export from the liver, in combination with increased VLDL turnover mediated by lipoprotein lipase in peripheral tissues (adipocytes and myocytes), generates increased LDL as part of the ApoB lineage. Lipoprotein lipase activity similarly reduces triglycerides content in these lipoproteins and increases the transfer of surface membrane components to ApoA particles, increasing HDL-C; this can explain the triad of high LDL-C, high HDL-C, and low triglycerides that defines LMHR.17
The current prospective KETO study will rigorously test whether carbohydrate restriction-induced LDL-C elevations are atherosclerotic and lead to plaque progression. Future studies will be needed to replicate the findings of this study and should be conducted in parallel with mechanistic investigations to further understand the phenomenon and therapeutic trials to assess the relative efficacy of different treatments for LDL-C lowering in this group of patients.18,19 The data presented in this manuscript provide first insight into risk and, interestingly, show no group differences between coronary plaque from individuals in the KETO study versus matched subjects from the population-based MiHeart cohort.
Study limitations
Limitations of this study include the relatively low sample size (n = 80 per group) and discrepancies present between groups, including slightly lower BMI in the KETO versus MiHeart group (22.5 vs 25.8 kg/m2) as well as higher HDL-C and lower triglycerides. This was a necessary limitation of the study, given the exceptional lipid triad (high LDL-C and HDL-C and low triglycerides) defining LMHR and near-LMHR subjects, ie, it was not possible to match KETO subjects to MiHeart subjects on these parameters because the LMHR population is so phenotypically unique. However, given that MiHeart subjects were non-obese and exhibited generally considered healthy levels of HDL-C (63 mg/dL) and triglycerides (96 mg/dL), this should not bias the results.
Additionally, the lipid energy model to explain the LMHR phenotype highlights the dynamic nature of lipids in LMHR subjects. As LDL-C levels can vary over the course of weeks and even days, single measurements may be conceived of as snapshots and imperfect reflections of average levels or area under the curve for LDL-C exposure. That said, the KETO group subjects maintained their diets throughout the study period, making it unlikely that many exhibited large fluctuations in LDL-C levels; thus, the group average of 272 mg/dL is likely a reliable measure of group average LDL-C.
Finally, we do not, in this preliminary analysis, report on the LDL particle profiles of the KETO/LMHR subjects as compared to the MiHeart cohort. It is plausible, if not likely, that LMHR-type subjects exhibit high LDL-C primarily from large buoyant LDL rather than small, dense LDL, which is more atherogenic. Nevertheless, exceptionally high LDL-C, as seen in LMHR, is necessarily coincident with an overall high LDL-P and ApoB level, and LDL particle profiles in the final published analysis from the prospective study.
Conclusions
After a mean duration of 4.7 years of carbohydrate restriction-induced elevations in LDL-cholesterol (mean 272 mg/dL), a metabolically healthy cohort of subjects with CRD did not have a greater atherosclerotic plaque burden than participants from a population-based cohort with markedly lower LDL-C. Given the preponderance of prior evidence on LDL-C as a risk factor for atherosclerotic disease, the increasing prevalence of LMHR and near-LMHR phenotypes with the rise in popularity of CRD, and the general lack of evidence on this phenotype, the study of LMHR and near-LMHR should be a research priority.
Perspectives.
COMPETENCY IN MEDICAL KNOWLEDGE AND COMMUNICATION SKILLS: LMHR is an emerging phenotype of growing research interest, with little known with respect to mechanism and risk. Physicians’ awareness of unique aspects of the phenotype, such as the inverse association between BMI and LDL-C change and the LDL-C suppression response to carbohydrate reintroduction, may facilitate individualized patient management. Furthermore, patients presenting with the LMHR or near LMHR phenotype often identify with the phenotype, as a community has arisen on social media focusing on LMHR and may be more receptive to clinical advice from physicians who acknowledge the unique aspects of their profile, are aware of ongoing research in this area, and engage in open discussion of the knowns and unknowns with these patients.
TRANSLATIONAL OUTLOOK: Understanding the mechanisms underlying the highly heterogenous LDL-C response to carbohydrate restriction, as well as the risk associated with high LDL-C on CRDs, and finally, treatment options, will take a multidisciplinary approach and may draw from many levels of research ranging from in vitro basic science studies to meta-analyses of existing clinical trials. In the opinion of this research team, research priorities should include dissecting the driving mechanism behind the LMHR phenotype by testing elements of the lipid energy model, along with comparing lifestyle (carbohydrate introduction, saturated fat reduction, increasing fiber) and pharmacological treatment (statin, ezetimibe, PCSK9i) options in LMHR in randomized controlled trials. Longer-term follow-up (eg,2-, 5-year CCTA measurements) of this and similar cohorts will also be essential to properly evaluate the risk associated with the phenotype.
Funding support and author disclosures
This study was funded by the Citizen Science Foundation, 7320 S Rainbow Blvd, #102-182, Las Vegas, NV, United States. The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental tables, please see the online version of this paper.
Supplemental Tables
References
- 1.Libby P. The changing landscape of atherosclerosis. Nature. 2021;592(7855):524–533. doi: 10.1038/s41586-021-03392-8. [DOI] [PubMed] [Google Scholar]
- 2.Kohli-Lynch C.N., Thanassoulis G., Moran A.E., Sniderman A.D. The clinical utility of apoB versus LDL-C/non-HDL-C. Clin Chim Acta. 2020;508:103–108. doi: 10.1016/j.cca.2020.05.001. [DOI] [PubMed] [Google Scholar]
- 3.Wang N., Woodward M., Huffman M.D., Rodgers A. Compounding Benefits of cholesterol-lowering therapy for the reduction of major cardiovascular events: Systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2022;15(6) doi: 10.1161/CIRCOUTCOMES.121.008552. [DOI] [PubMed] [Google Scholar]
- 4.Dugani S.B., Moorthy M.V., Li C., et al. Association of lipid, Inflammatory, and metabolic Biomarkers with age at Onset for Incident coronary heart disease in Women. JAMA Cardiol. 2021;6(4):437–447. doi: 10.1001/jamacardio.2020.7073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martin-McGill K.J., Bresnahan R., Levy R.G., Cooper P.N. Ketogenic diets for drug-resistant epilepsy. Cochrane Database Syst Rev. 2020;6 doi: 10.1002/14651858.CD001903.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Phillips M., Deprez L., Mortimer G., et al. Randomized crossover trial of a modified ketogenic diet in Alzheimer’s disease. Alzheimer's Res Ther. 2021;13:51. doi: 10.1186/s13195-021-00783-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Danan A., Westman E.C., Saslow L.R., Ede G. The ketogenic diet for Refractory mental illness: a Retrospective analysis of 31 inpatients. Front Psychiatry. 2022;13 doi: 10.3389/fpsyt.2022.951376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Norwitz N.G., Sethi S., Palmer C.M. Ketogenic diet as a metabolic treatment for mental illness. Curr Opin Endocrinol Diabetes Obes. 2020;27(5):269–274. doi: 10.1097/MED.0000000000000564. [DOI] [PubMed] [Google Scholar]
- 9.Cukoski S., Lindemann C.H., Arjune S., et al. Feasibility and impact of ketogenic dietary interventions in polycystic kidney disease: KETO-ADPKD-a randomized controlled trial. Cell Rep Med. 2023;4 doi: 10.1016/j.xcrm.2023.101283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wood R.J., Fernandez M.L., Sharman M.J., et al. Effects of a carbohydrate-restricted diet with and without supplemental soluble fiber on plasma low-density lipoprotein cholesterol and other clinical markers of cardiovascular risk. Metabolism. 2007;56(1):58–67. doi: 10.1016/j.metabol.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 11.Lim S.S., Noakes M., Keogh J.B., Clifton P.M. Long-term effects of a low carbohydrate, low fat or high unsaturated fat diet compared to a no-intervention control. Nutr Metab Cardiovasc Dis. 2010;20(8):599–607. doi: 10.1016/j.numecd.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 12.Buren J., Ericsson M., Damasceno N.R.T., Sjodin A. A ketogenic low-carbohydrate high-fat diet increases LDL cholesterol in healthy, Young, normal-weight Women: a randomized controlled Feeding trial. Nutrients. 2021;13(3):814. doi: 10.3390/nu13030814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Norwitz N.G., Feldman D., Soto-Mota A., Kalayjian T., DS L. Elevated LDL-cholesterol with a carbohydrate-restricted diet: evidence for a ‘lean mass hyper-responder’ phenotype. Curr Dev Nutr. 2021;6:1–10. doi: 10.1093/cdn/nzab144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Soto-Mota A., Flores-Huardo Y., Norwitz N.G., et al. Increased LDL cholesterol in adults with normal but not high body weight: a meta-analysis. Am J Clin Nutr. 2024;119(3):740–747. doi: 10.1016/j.ajcnut.2024.01.009. [DOI] [PubMed] [Google Scholar]
- 15.Norwitz N.G., Mindrum M.R., Giral P., et al. Elevated LDL-cholesterol levels among lean mass hyper-responders on low-carbohydrate ketogenic diets deserve urgent clinical attention and further research. J Clin Lipidol. 2022;16(6):765–768. doi: 10.1016/j.jacl.2022.10.010. [DOI] [PubMed] [Google Scholar]
- 16.Pagali S.R., Madaj P., Gupta M., et al. Interobserver variations of plaque severity score and segment stenosis score in coronary arteries using 64 slice multidetector computed tomography: a substudy of the ACCURACY trial. J Cardiovasc Comput Tomogr. 2010;4(5):312–318. doi: 10.1016/j.jcct.2010.05.018. [DOI] [PubMed] [Google Scholar]
- 17.Norwitz N.G., Soto-Mota A., Kaplan B., et al. The lipid energy model: reimagining lipoprotein Function in the context of carbohydrate-restricted diets. Metabolites. 2022;12(5):460. doi: 10.3390/metabo12050460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rasouli L., Budoff M.J., Park R., Aziz D.C. Plasma Homocysteine Predicts progression of atherosclerosis. Atherosclerosis. 2005;181(1):159–165. doi: 10.1016/j.atherosclerosis.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 19.Gupta A., Lau E., Varshney R., et al. The Identification of Calcified coronary plaque is associated with Initiation and Continuation of pharmacological and lifestyle preventive Therapies: a Systematic review and meta-analysis. JACC Cardiovasc Imaging. 2017;10(8):833–842. doi: 10.1016/j.jcmg.2017.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.