Abstract
Background
Several preliminary studies have been conducted in the field of the prevalence of depression, anxiety, and stress in the elderly population. These studies have examined the prevalence in limited geographic areas with small sample sizes. Also, there are many limitations in the meta-analysis studies. The objective of the present study was to synthesize the global prevalence statistics of depression, anxiety, and stress in the elderly population through a systematic review and meta-analysis.
Methods
The present systematic review included retrieval of primary studies from the oldest relevant study up to 2023. To find the relevant studies, international databases such as Scopus, Embase, PubMed, and Web of Science (WoS) were systematically searched. Also, a manual search was performed through the Google Scholar search engine and a review of the sources of related articles. The qualitative assessment of the studies was conducted using the Joanna Briggs Institute (JBI) checklist. Due to a high heterogeneity among the study results, a Random Effects model was chosen.
Results
A total of 42 articles on depression, 47 articles on anxiety and 13 articles on stress were included in the meta-analysis. The overall estimates for prevalence based on a random-effects model were as follows: depression, 19.2% (95% CI: 13.0 − 27.5%); anxiety, 16.5% (95% CI: 11.1 − 22.8%); and stress, 13.9% (95% CI: 5.5 − 30.9%). The highest prevalence of depression and anxiety was recorded in Africa. The prevalence of depression was higher in nursing homes, and stress was more prevalent in individuals with COVID-19 compared to other populations.
Conclusion
The findings revealed a high prevalence of depression, anxiety, and stress in the elderly population. Therefore, it is recommended that healthcare professionals and policymakers pay more attention to the prevention and management of these disorders in the elderly population.
Keywords: Prevalence, Depression, Anxiety, Elderly population, Systematic review, Meta‑analysis
Introduction
Old age is a sensitive phase in human life, and addressing the issues, needs, and diseases associated with this stage of life is a social imperative [1]. The World Health Organization (WHO) defines individuals aged 65 and above as elderly, and a large portion of the elderly population live in developing countries [2]. Today, advancements in technology, increased life expectancy, and declining fertility rates have led to a global rise in the elderly population, making aging a paramount public health challenge [3, 4]. According to United Nations reports, the global elderly population is projected to double by 2050, reaching one billion individuals compared to 524 million in 2010. Thus, older adults will comprise a substantial proportion of the world’s total population in the near future [5, 6].
The process of aging features diverse physiological changes in various bodily systems [7]. According to the WHO, aging is a relative, intrinsic, psychological, and social phenomenon [8]. With aging, chronic diseases such as cardiovascular diseases, cancer, respiratory diseases, and diabetes can threaten the health of the elderl [9, 10]. Furthermore, the onset of old age significantly influences individuals’ psychological capacity, and may lead elderly individuals to experience various psychological challenges [11], including depression, anxiety, and stress [12]. Depression in the elderly is a serious mental health concern that can contribute to physical illnesses, reduce post-treatment recovery, and even lead to suicide attempt [13]. Anxiety, another significant psychological issue in the elderly (an unpleasant and vague feeling associated with a sense of uncertainty about an unknown factor) [14–18], can impair functional capabilities and overall quality of life when its intensity increases [19]. Another prominent psychological issue is stress, which affects 5–50% of elderly individuals [20] and has a potentially profound impact on their mental and physical health. The prevalence of stress among the elderly has been gradually increasing and is predicted to double over the next decade [21].
The meta-analysis study by Zenebe et al. found the prevalence of depression in the elderly to be 31.74% [22], Sarokhani et al. prevalence of depression and meta-analysis in Iranian elderly is 43% [23], Abdoli et al. prevalence of major depression (MDD) among the elderly was 13.3% [24], and Yan et al. reported the prevalence of depression and anxiety in Chinese elderly during the Covid-19 era as 26% and 23%, respectively [25].
Several preliminary studies have been conducted in recent years in the field of the prevalence of depression, anxiety, and stress in the elderly population in different regions of the world [26–29]. However, these studies have examined the prevalence in limited geographic areas with small sample sizes. Furthermore, none of the reviewed studies have investigated potential factors such as the study year, sample size, and average age of the elderly subjects. Additionally, given the changing population demographics in different parts of the world, the prevalence rates have not been reported separately for different continents. Also, there are many limitations in the meta-analysis studies. Therefore, it appears necessary to conduct a systematic review and meta-analysis to consolidate, summarize, and resolve discrepancies in the results of previous studies, investigate potential factors, and provide an overall estimate of the prevalence of depression, anxiety, and stress in the elderly population. To our knowledge, such a study has not been conducted thus far. Therefore, the present study aims to determine the global prevalence of depression, anxiety, and stress in the elderly through a systematic review and meta-analysis.
Method
A systematic review and meta-analysis was conducted following the PRISMA 2020 guidelines, comprising Identification, Screening, Eligibility, and Inclusion [30]. To reduce publication bias and errors, all stages of the search, assessment, article selection, and data extraction were independently carried out by two researchers (M.K and Z.K) and, in case of disagreements, consensus was initially reached through discussion and ultimately by consulting a third party (A.J).
Finding studies
To find articles relevant to the research question (“What is the global prevalence of depression, anxiety, and stress in the elderly?“), international databases, including Scopus, Embase, PubMed, and Web of Science (WoS), were examined. Search strategies in the databases were formulated by utilizing relevant and validated keywords, including MeSH terms, and combining them using OR and AND operators. For instance, the search strategy in PubMed was structured as follows:
(((Prevalence[MeSH Terms]) OR (Prevalence[Title/Abstract])) AND (((((((((Depressive Disorder[MeSH Terms]) OR (Depression[MeSH Terms])) OR (Depression*[Title])) OR (Depressiv*[Title])) OR (Anxiety*[Title])) OR (Anxieties[Title])) OR (Anxiety[MeSH Terms])) OR (Stress*[Title])) OR (Stress Disorders, Traumatic, Acute[MeSH Terms]))) AND ((((((Elderly[Title/Abstract]) OR (Old*[Title/Abstract])) OR (Geriat*[Title/Abstract])) OR (Elderlys[Title/Abstract])) OR (Elderlies[Title/Abstract])) OR (Aged[Title/Abstract])). No time restrictions were imposed in the search for studies to retrieve all potentially relevant articles up to July 2023. Ultimately, to maximize the comprehensiveness of the search, the Google Scholar search engine and manual examination of all articles related to the study’s objectives were conducted.
Inclusion criteria
Observational studies.
Availability of the full-text article.
Reporting the prevalence rates of depression, anxiety, and stress in the elderly.
Specified sample size.
Exclusion criteria
Interventional studies, case series, case reports, letters to the editor, conference papers, theses, qualitative studies, animal studies, systematic reviews, and meta-analyses.
Studies indexed in more than one database.
Selection process of studies
All studies obtained from the databases were imported into the EndNote X8. Initially, studies that were duplicated across different databases were excluded. Subsequently, the titles and abstracts of studies were reviewed using inclusion and exclusion criteria, and studies unrelated to the topic were excluded. In the eligibility stage, a thorough examination of the full text of the studies was conducted, and studies not aligned with the research objectives were excluded. Finally, articles meeting all inclusion criteria underwent a qualitative assessment. The searchers conducting the article extraction were blind to the authors, institutions, and journals being examined.
Qualitative evaluation
The qualitative assessment of the studies was conducted using the Joanna Briggs Institute (JBI) checklist, a standard and widely recognized tool for evaluating the quality of prevalence studies [31]. This checklist comprises nine distinct questions covering sample frame, participants, sample size, participants, study subjects and the setting described in detail, data analysis, valid methods for identifying conditions, measuring the situation, statistical analysis, and adequate response rate. Each item was assessed as “Yes” if indicated, “No” if not indicated, or “NA” if not reported. Scores ranged from a minimum of 0 to a maximum of 9 based on the number of “Yes” responses.
Data extraction
To extract data, a pre-prepared electronic form based on the checklist was utilized. The items included in this checklist were the first author, publication year, country and continent, mean age, sample size, diagnostic tool, prevalence percentage, study population, and the qualitative assessment score.
Statistical analysis
The index examined in this study was the prevalence percentage of depression, anxiety, and stress in the elderly. To combine the results from different studies, the prevalence rates reported in each study were employed. Heterogeneity among the studies was assessed using the I2 statistic, and due to a high heterogeneity (I2 > 75%) among the study results, a Random Effects model was chosen. In this model, parameter variations among studies are also calculated, so that the results of the model have a higher generalizability in heterogeneity conditions than the Fixed Effects model. Funnel plot and Begg and Mazumdar rank correlation were used to check publication bias. Additionally, for assessing the relationship between the global prevalence percentages of depression, anxiety, and stress in the elderly and the publication year, mean age, and sample size, Meta-Regression was employed. Subgroup analyses were performed based on different continents. Data were analyzed using Comprehensive Meta-Analysis (Version 2) software, and a P-value of less than 0.05 was considered statistically significant.
Results
Study characteristics
Summary of the study selection process
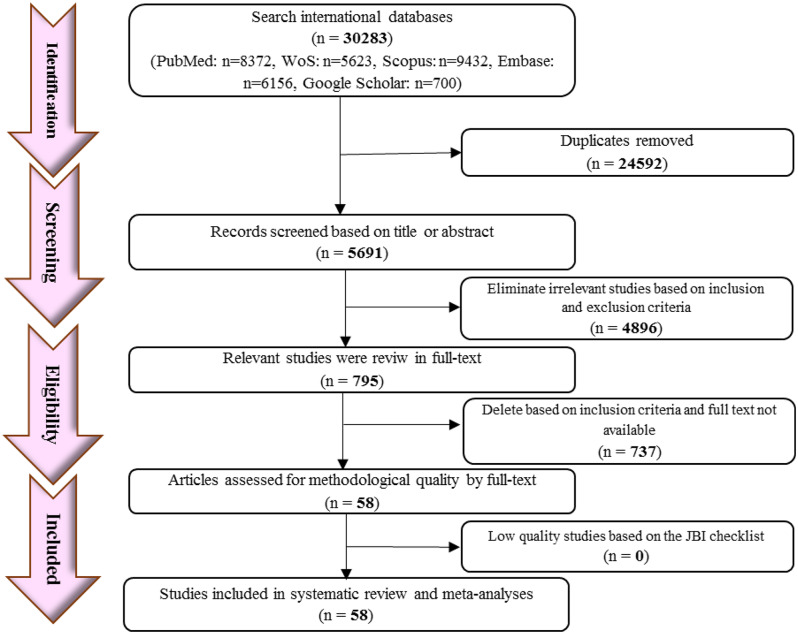
The initial search using predefined search strategies across various databases, a total of 30,283 studies were retrieved, of which 24,592 duplicate and overlapping studies across different databases were excluded. Following the evaluation of titles and abstracts, 5,691 studies were retained, while 4,896 studies were subsequently excluded for being irrelevant to the topic. Consequently, 795 remaining studies underwent a full-text review, with 737 studies excluded for failing to meet inclusion criteria. Ultimately, 58 articles meeting the entry criteria were included in the meta-analysis. The flowchart of the PRISMA 2020 process is depicted in Fig. 1.
Fig. 1.
PRISMA 2020 flow diagram for article selection
General specifications of the studies
The oldest study included in this analysis dated back to 1987, while the most recent study was published in 2023. The majority of studies (14 studies) were related to the United States. The study with the largest and smallest sample sizes belonged to Maercker et al. with 65,512 participants [32], and Kvaal et al. with 40 participants [33] respectively. The details of the studies that met the inclusion criteria for the systematic review and meta-analysis are summarized in Table 1.
Table 1.
Summary of studies included in the systematic review and meta-analysis
| First author, Year, Reference | Age (years) | Country/ Continent | Sample size (n) | Prevalence (%) | Diagnostic tool | Population | Quality Score | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Depression | Anxiety | Stress | |||||||||||
| Babazadeh, 2015 [34] | 68.2±6.8 | Iran / Asia | 383 | 1.3 | 3.1 | 1.3 | DASS- 21 | General Population | 7 | ||||
| Thapa, 2020 [35] | 71.1±8.2 | Nepal / Asia | 794 | 15.4 | 18.1 | 12.1 | DASS- 21 | General Population | 7 | ||||
| Blazer, 1987 [29] | ˃ 60 | USA / America | 3000 | 2.1 | - | - | DSM-III | General Population | 5 | ||||
| Kirmizioglu, 2009 [36] | ˃ 65 | Turkey / Europe | 462 | - | 17.1 | - | DSM-IV | General Population | 6 | ||||
| Wongpakaran, 2019 [37] | 69.24±6.8 | Thailand/Asia | 803 | 23.7 | 6.4 | - | DSM-IV | General Population | 6 | ||||
| Raeisvandi, 2023 [38] | 69.86±7.2 | Iran/ Asia | 301 | 45.5 | 35.5 | 40.2 | DASS- 21 | General Population | 9 | ||||
| Jayakody, 2018 [39] | 64.44±10.77 | Australia / Australia | 151 | 27.51 | 5.89 | 5.64 | DASS- 21 | General Population | 7 | ||||
| Chen, 2022 [40] | 70.2±7.1 | China/ Asia | 966 | 7.8 | 6.3 | - | DASS- 21 | Hospitalization | 8 | ||||
| Milani and Lavie, 1998 [41] | 71±4 | USA / America | 268 | 18 | - | - | SF-36 | Coronary Heart Disease | 6 | ||||
| Malhotra, 2023 [42] | 67.4±6.5 | India / Asia | 690 | 7.83 | 12.02 | 5.2 | DASS- 21 | COVID-19 | 6 | ||||
| Maercker, 2008 [32] | 75.2±7.5 | Switzerland / Europe | 65,512 | 2.3 | 4.2 | - | DSM-IV | General Population | 5 | ||||
| Molyneux, 2008 [43] | 79.2 | Ireland / Europe | 100 | 21 | - | - | GDS-15 | Hospitalization | 6 | ||||
| Lindesay, 1989 [44] | ˃ 65 | England / Europe | 890 | 13.5 | 3.7 | - | DSM-III | General Population | 5 | ||||
| Pasha, 2023 [45] | 71.4 | Iran / Asia | 140 | 62.9 | 97.1 | 58.6 | DASS- 21 | COVID-19 | 8 | ||||
| Marsa, 2020 [46] | 72.1 | Iran / Asia | 436 | 60.3 | 51.7 | 24.6 | DASS- 21 | General Population | 7 | ||||
| Barakat, 2019 [28] | 66.2±7.73 | Egypt / Africa | 756 | 60 | 38 | - | Beck’s | General Population | 6 | ||||
| Lu, 2023 [47] | 72.74±6.5 | China / Asia | 1173 | 37.34 | 32.74 | - | DASS- 21 | General Population | 8 | ||||
| Canuto, 2018 [48] | 65-84 | Germany, Italy, England, Spain, Switzerland, and Israel / Europe | 3142 | - | 17.2 | - | CIDI65+ | General Population | 7 | ||||
| Zhang, 2015 [49] | 72.8±5.3 | France/Europe | 1974 | - | 11 | - | DSM-IV | General Population | 6 | ||||
| Curran, 2020 [50] | ˃ 60 | England / Europe | 1863 | 8 | 2.6 | - | DASS- 21 | General Population | 5 | ||||
| Richardson, 2012 [51] | 76.5±9.2 | USA / America | 378 | 31 | - | - | DSM-IV-TR | General Population | 6 | ||||
| Zhang, 2012 [52] | 68.96±7.1 | China / Asia | 284 | 35.2 | 42.9 | - | DSM-IV-TR | General Population | 5 | ||||
| Kang, 2016 [53] | 72.2±5.9 | South korea / Asia | 1204 | - | 38.1 | - | GMS-B3 | General Population | 6 | ||||
| Sari and Manungkalit, 2019 [54] | 75-90 | Indonesia / Asia | 145 | 65.5 | 15.2 | 0.7 | HARS, SPST-20, GDS | General Population | 6 | ||||
| Malhotra, 2023 [42] | 67.45 ± 6.5 | India / Asia | 690 | 7.83 | 12.02 | 5.2 | DASS-21 | COVID-19 | 7 | ||||
| Dura, 1990 [55] | 68.1±8.3 | USA / America | 756 | 30 | - | - | DSM-III | General Population | 5 | ||||
| Nayak, 2019 [56] | 66.5 | India / Asia | 244 | 46.7 | 57.3 | - | GDS-15 | General Population | 7 | ||||
| Prina, 2011 [57] | ˃ 65 | China and India/Asia | 15,021 | - | 2.9 | - | GMS | General Population | 6 | ||||
| Yang, 2021 [58] | ˃ 65 | China/Asia | 953 | 19.4 | 44 | - | SDS and SAS | General Population | 7 | ||||
| Gum, 2009 [59] | ˃ 65 | USA / America | 1461 | - | 7 | - | DSM-III | General Population | 5 | ||||
| Raeisvandi, 2022 [60] | 69.86 | Iran / Asia | 301 | 45.5 | 35.5 | 40.2 | DASS-21 | General Population | 8 | ||||
| Ganatra, 2008 [61] | ˃ 65 | Pakistan /Asia | 402 | 22.9 | - | - | DSM-III | General Population | 6 | ||||
| Mehta, 2003 [62] | 74±3 | USA / America | 3075 | - | 20 | - | DSM-III | General Population | 5 | ||||
| Choulagai, 2013 [63] | 78 | Nepal / Asia | 78 | 66.7 | - | - | GDS-15 | Geriatric Homes | 7 | ||||
| Murrell, 1983 [64] | ˃ 60 | USA / America | 2517 | 13.7 | - | - | CES-D | General Population | 5 | ||||
| Sjoberg, 2017 [65] | ˃ 60 | Sweden / Europe | 3353 | 21 | - | - | DSM-IVTR/DSM-5 | General Population | 7 | ||||
| Assil and Zeidan, 2013 [27] | ˃ 60 | Sudanese / Africa | 300 | 47.5 | - | - | GDS | General Population | 5 | ||||
| El-Gabalawy, 2011 [66] | 67.1±0.1 | Canada / America | 12,792 | 7.7 | 4.9 | - | CIDI | General Population | 6 | ||||
| Anwar, 2023 [26] | ˃ 60 | Myanmar/Asia | 864 | - | 68 | 93 | CAS | COVID-19 | 7 | ||||
| de Oliveira Andrade, 2022 [67] | ˃ 65 | Brazil / America | 380 | 28.7 | 26.1 | - | GDS and GAD | COVID-19 | 7 | ||||
| Neville and Teri, 2011 [68] | 86.2 | USA / America | 148 | - | 11 | - | CAS | General Population | 5 | ||||
| Suri, 2018 [69] | ˃ 65 | India / Asia | 697 | 23 | 38 | - | HAM-D and HAM-A | General Population | 7 | ||||
| Mackenzie, 2011 [70] | ˃ 65 | USA / America | 12,312 | - | 2.80 | - | GAD | General Population | 7 | ||||
| Cohen, 2006 [71] | 70.3±2.5 | USA / America | 1074 | - | 15.6 | - | DSM-III | General Population | 5 | ||||
| Maung, 2022 [72] | ˃ 65 | Malaysia / Asia | 178 | 23.6 | 18.5 | 7.9 | DASS-21 | General Population | 8 | ||||
| Suradom, 2019 [73] | 68.39±6.74 | Thailand / Asia | 803 | 23.66 | 16.84 | - | HAMD-7 | General Population | 8 | ||||
| Yao, 2021 [74] | ˃ 65 | China / Asia | 206 | - | 30.1 | - | HAMA | Diabetes and hypertension | 7 | ||||
| Mutepfa, 2021 [75] | 71.8±9.1 | Botswana / Africa | 378 | - | 18.6 | - | GAD-7 | General Population | 5 | ||||
| Zhang and Cooper, 2010 [76] | ˃ 65 | USA / America | 56,182 | 0.8 | 1.2 | - | ICD-9 | Colorectal Cancer | 5 | ||||
| Choi and McDougall-1, 2007 [77] | 76.2 | USA / America | 81 | 4.6 | - | - | GDS | Hospitalization | 6 | ||||
| Choi and McDougall-2, 2007 [77] | 76.2 | USA / America | 130 | 1.96 | - | - | GDS | General Population | 6 | ||||
| Bloch, 2014 [78] | ˃ 75 | France/Europe | 52 | - | 30.5 | - | GAD | After the fall | 7 | ||||
| Gonçalves, 2011 [79] | 68±8 | Australia / Australia | 3035 | - | 2.76 | - | GAD | General Population | 5 | ||||
| Forlani, 2014 [80] | 83.7±6.2 | Italy / Europe | 366 | 25.2 | 21.04 | - | CAMDEXR | General Population | 7 | ||||
| Taha and Rahman, 2006 [81] | 65.0±4.5 | Egypt / Africa | 332 | 57.1 | 34.1 | - | HAMA | Geriatric Homes | 6 | ||||
| Kvaal, 2001 [33] | ˃ 70 | Norway / Europe | 40 | - | 41 | - | STAI | Hospitalization | 5 | ||||
| Arbus, 2014 [82] | 73.8±8.5 | France / Europe | 3651 | - | - | 3.7 | DSM-IV | General Population | 6 | ||||
| Bunce, 2012 [83] | 66.61±5.638 | Brazil / America | 120 | 15.38 | 8.33 | - | GDS | General Population | 7 | ||||
| Silveira and Portuguez, 2017 [84] | ˃ 60 | USA / America | 397 | 16.6 | 4.5 | - | GAD- 7 | General Population | 7 | ||||
DASS- 21: Depression, Anxiety, Stress Scale 21
GDS-15: Geriatric Depression Scale-15
GMS-B3: Geriatric Mental State Schedule
HARS: Hamilton Anxiety Rating Scale
SPST-20: Suan Prung Stress Test 20
GDS: Geriatric Depression Scale
GAD: Geriatric Anxiety Scale
GMS: Geriatric Mental State
SDS: self-rating depression scale
CAS: Coronavirus Anxiety Scale
SAS: self-rating anxiety scale
CIDI: Composite International Diagnostic Interview
HAM-D: Hamilton depression rating
HAM-A: Hamilton anxiety rating scale
CAMDEXR: Cambridge Mental Disorders of the Elderly Examination-Revised
Meta-analysis of global prevalence of depression, anxiety, and stress in the elderly
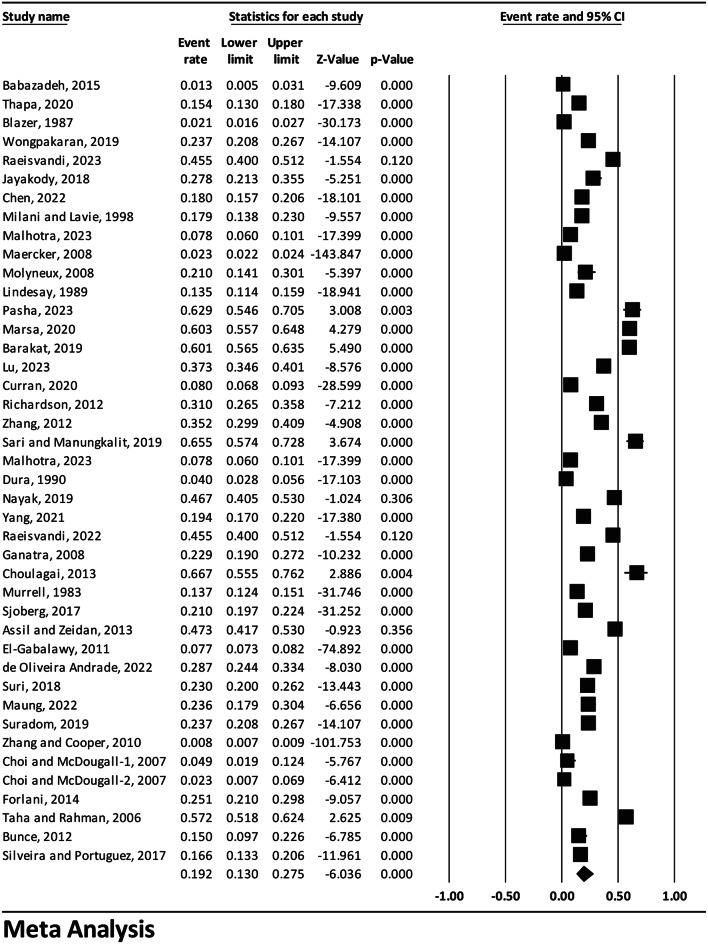
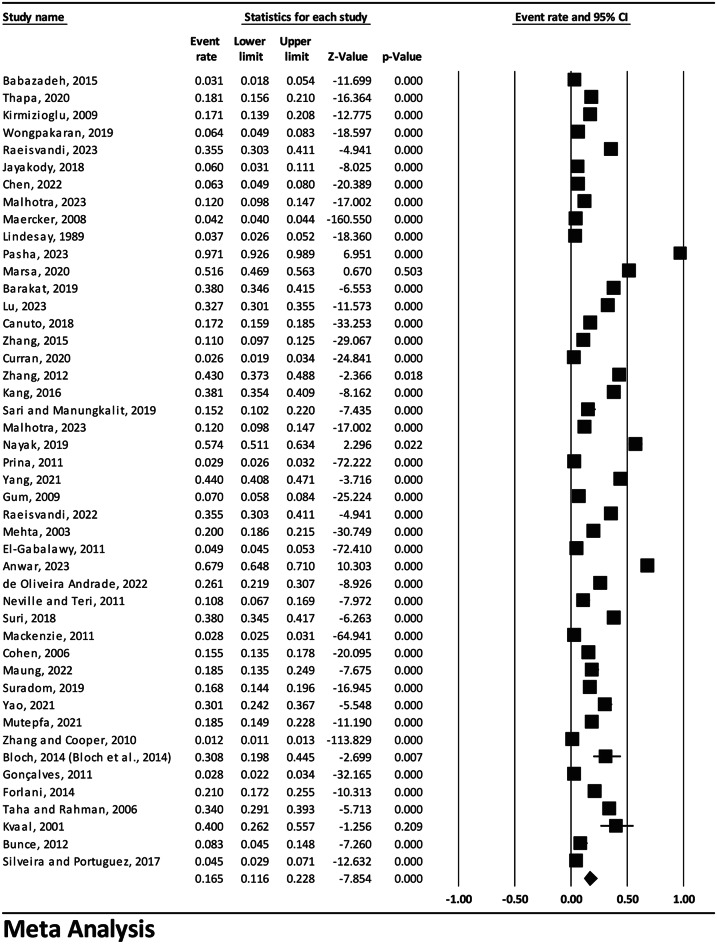
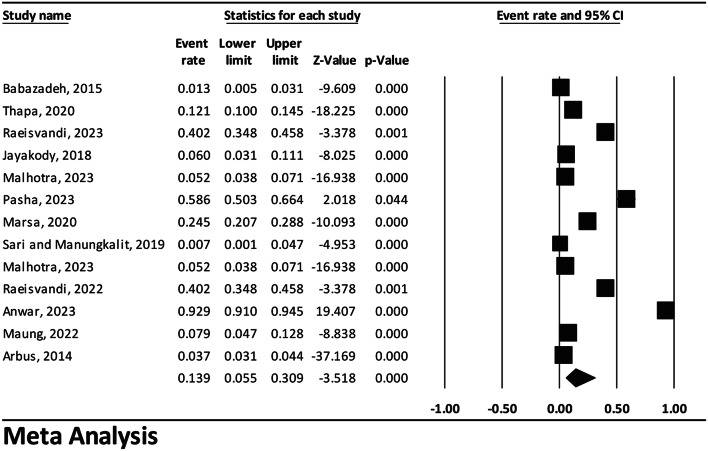
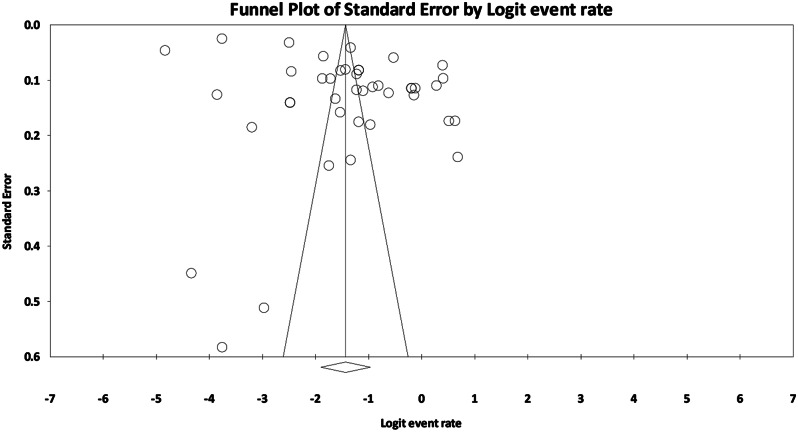
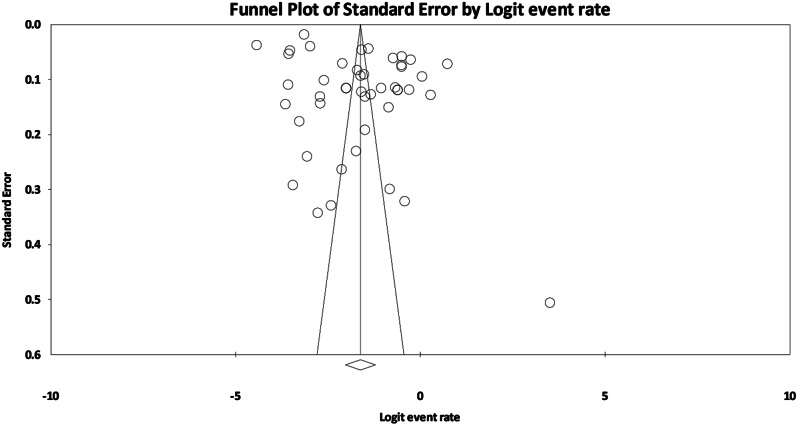
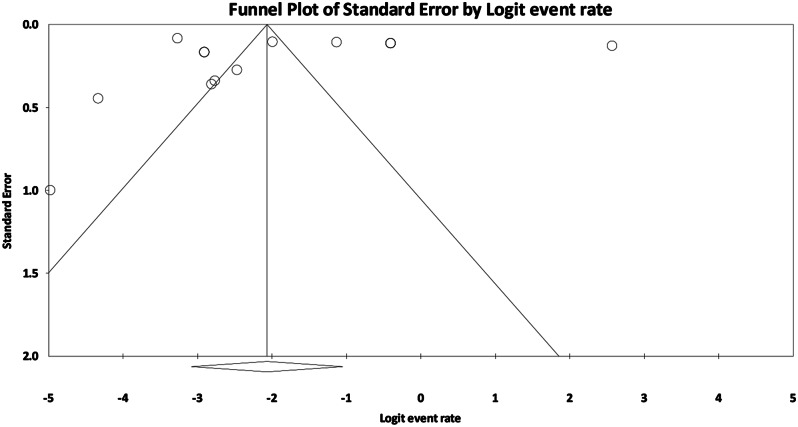
In total, there were 42 studies reporting the prevalence of depression with a sample size of 161,085 individuals, 46 studies reporting the prevalence of anxiety with a sample size of 194,170 individuals, and 13 studies reporting the prevalence of stress with a sample size of 2,306 individuals. The I2 test results indicated a notable heterogeneity among the studies for global prevalence rates of depression, anxiety, and stress in the elderly (I2 Depression = 99.70, I2 Anxiety = 99.70, and I2 Stress = 99.32). Therefore, a random-effects model was applied to analyze the data. As a result, the combined estimates of the prevalence rates for depression was equal to 19.2% (95% CI: 13.0-27.5), 16.5% (95% CI: 11.1–22.8) for anxiety, and 13.9% (95% CI: 5.5–30.9) for stress. Based on the random-effects model, in Figs. 2, 3 and 4 the black square represents the percentage; the horizontal line represents the 95% confidence interval for each study; and the diamond sign represents the overall prevalence percentage for all studies. Based on the results of Begg and Mazumdar rank correlation, there was no publication bias in the studies at the level of 0.1 (P-value (Depression) = 0.121, P-value (Anxiety) = 0.172 and P-value (Stress) = 0.854) (Figs. 5, 6 and 7).
Fig. 2.
Forest plot of the overall estimate of the global prevalence of depression in the elderly based on the random effects model
Fig. 3.
Forest plot of the overall estimate of the global prevalence of anxiety in the elderly based on the random effects model
Fig. 4.
Forest plot of the overall estimate of the global prevalence of stress in the elderly based on the random effects model
Fig. 5.
Funnel plot of the results related to the overall estimate of the global prevalence of depression in the elderly
Fig. 6.
Funnel plot of the results related to the overall estimate of the global prevalence of anxiety in the elderly
Fig. 7.
Funnel plot of the results related to the overall estimate of the global prevalence of stress in the elderly
Meta-regression analysis
Using meta-regression analysis, the relationship between the year of the study, sample size, mean age, and JBI score with the overall prevalence of depression, anxiety, and stress worldwide was examined. The results indicated that with an increase in the year, age, and JBI score, the prevalence of depression, anxiety, and stress exhibits an upward trend, while an increase in the sample size was associated with a downward trend (P < 0.001) (Table 2).
Table 2.
Meta-regression of the relationship between year, sample size, average age and JBI score
| Disorder | Variable | Relationship | Tau- squared | Model Q | P-value |
|---|---|---|---|---|---|
| Depression | Year | Straight | 2.07 | 5.77 | 0.000 |
| Sample size | Inverse | 0.81 | 23.22 | 0.000 | |
| Age | Straight | 1.23 | 8.23 | 0.000 | |
| JBI scor | Straight | 1.32 | 9.97 | 0.000 | |
| Anxiety | Year | Straight | 1.36 | 8.28 | 0.000 |
| Sample size | Inverse | 1.28 | 11.62 | 0.000 | |
| Age | Straight | 1.56 | 8.37 | 0.000 | |
| JBI scor | Straight | 1.44 | 9.10 | 0.000 | |
| Stress | Year | Straight | 2.33 | 6.97 | 0.000 |
| Sample size | Inverse | 2.98 | 0.32 | 0.000 | |
| Age | Straight | 2.65 | 3.26 | 0.000 | |
| JBI scor | Straight | 2.79 | 4.30 | 0.000 |
Subgroup analysis
Considering the high heterogeneity among studies regarding the prevalence of depression, anxiety, and stress in the elderly (I2 > 99%), subgroup analysis was conducted based on the continent and the study population (Table 3). The highest prevalence of depression and anxiety was recorded in Africa, with estimates of 55.1% (95% CI: 47.7–62.3) and 29.5% (95% CI: 19.4–42.1) respectively. Additionally, the prevalence of depression was higher in nursing homes (60.7%), and stress was more prevalent in individuals with COVID-19 (18.2%) compared to other populations (Table 3).
Table 3.
Subgroup analysis to estimate the prevalence of depression, anxiety and stress by continent and study population
| Type of disorder | Subgroups | Number Studies | Prevalence % | P-value | P-value between | I2 | Tau | |
|---|---|---|---|---|---|---|---|---|
| Depression | Continent | Africa | 3 | 55.1 (95% CI: 47.7–62.3) | 0.176 | 0.000 | 85.80 | 0.244 |
| America | 12 | 0.08 (95% CI: 3.7–16.6) | 0.000 | 99.63 | 1.438 | |||
| Asia | 20 | 28.3 (95% CI: 21.7–36.0) | 0.000 | 98.16 | 0.792 | |||
| Australia | 1 | 27.8 (95% CI: 21.3–35.5) | 0.000 | 0.000 | 0.000 | |||
| Europe | 6 | 12.3 (95% CI: 4.1–31.5) | 0.001 | 99.82 | 1.485 | |||
| Population | COVID-19 | 4 | 20.9 (95% CI: 7.0–48.3) | 0.039 | 0.000 | 98.81 | 1.280 | |
| General Population | 31 | 19.6 (95% CI: 13.0–28.6) | 0.000 | 99.68 | 1.394 | |||
| Geriatric Homes | 2 | 60.7 (95% CI: 51.4–69.3) | 0.024 | 56.67 | 0.214 | |||
| Hospitalization | 3 | 15.1 (95% CI: 9.2–24.0) | 0.000 | 76.40 | 0.421 | |||
| Anxiety | Continent | Africa | 3 | 29.5 (95% CI: 19.4–42.1) | 0.002 | 0.000 | 95.31 | 0.477 |
| America | 10 | 7.4 (95% CI: 3.5–15.3) | 0.000 | 99.72 | 1.290 | |||
| Asia | 22 | 26.3 (95% CI: 16.7–39.0) | 0.001 | 99.52 | 1.378 | |||
| Australia | 2 | 3.8 (95% CI: 1.8–7.9) | 0.000 | 79.65 | 0.505 | |||
| Europe | 9 | 11.9 (95% CI: 6.6–20.7) | 0.000 | 99.44 | 0.989 | |||
| Population | COVID-19 | 5 | 30.8 (95% CI: 19.8–44.5) | 0.760 | 0.000 | 99.43 | 1.563 | |
| General Population | 35 | 44.6 (95% CI: 16.8–76.3) | 0.000 | 99.65 | 1.233 | |||
| Hospitalization | 2 | 17.2 (95% CI: 2.2–66.3) | 0.171 | 97.68 | 1.602 | |||
| Stress | Population | COVID-19 | 4 | 18.2 (95% CI: 9.0–84.7) | 0.360 | 0.651 | 99.69 | 3.273 |
| General Population | 9 | 9.3 (95% CI: 4.1–20.0) | 0.000 | 98.78 | 1.308 | |||
Discussion
The global prevalence statistics of depression, anxiety, and stress in the elderly was standardized using a systematic review and meta-analysis approach. After reviewing studies retrieved from various databases, a total of 43 studies on the prevalence of depression with a sample size of 161,085 individuals, 47 studies on the prevalence of anxiety with a sample size of 194,170 individuals, and 13 studies on the prevalence of stress with a sample size of 2,306 individuals were included in the meta-analysis. The overall estimated prevalence rates were 19.2% for depression, 16.5% for anxiety, and 11.2% for stress based on the random-effects model.
The highest qualitative assessment score, based on the JBI checklist, was obtained by Raeisvandi et al. with a score of 9, reporting depression, anxiety, and stress prevalence rates of 45.5%, 35.5%, and 40.2%, respectively [38]. Villagrasa et al. reported a prevalence of anxiety in Spanish elderly individuals as 11% [25]. Sarokhani et al. reported the prevalence of depression in Iranian elderly individuals as 43% [23]. Abdoli et al. estimated the prevalence of major depressive disorder (MDD) in the elderly as 13.3% [24]. The statistical differences reported in the present study compared to other studies may be attributed to variations in study methodology, data collection tools, the number of articles included in the study, as well as geographical and population differences.
The meta-regression analysis indicated an increasing trend in the global prevalence of depression, anxiety, and stress with age among the elderly. Reasons for this trend may include excessive weight gain [85], tobacco consumption [86, 87], excessive consumption of alcoholic beverages and coffee [86], inadequate and irregular sleep patterns [88], diseases such as Alzheimer’s and dementia [89], loneliness [90], fear of falling from bed [91], and various physical illnesses such as stroke [92] and heart diseases [93]. Therefore, health authorities and policymakers need to take action to address and prevent cognitive, physical, and mental health issues in the elderly.
Given the changing demographics, cultures, races, genetics, treatment types, socio-economic statuses, stress factors, diagnostic tools, and more across different countries and regions, we decided to conduct subgroup analysis. The highest prevalence rates of depression and anxiety were reported among elderly individuals in Africa. Limited access to mental health outgoing services, lack of trust in medical services, stigma, and social barriers, along with concerns about antidepressant and anti-anxiety medications, may contribute to the increased risk of depression and anxiety in the African population [94, 95].
The results demonstrated that the prevalence of depression in elderly residents of nursing homes was higher than in other elderly populations. This finding suggests a correlation between the elderly’s place of residence and their levels of anxiety, stress, and depression. These findings are consistent with the study by Vigod et al., which indicated that the living environment of the elderly was an important and influential factor in their mental health and psychiatric conditions [96]. It is plausible that psychosocial variables present in the living environment, such as a sense of belonging and acceptance, feeling valued and effective, warmer social interactions, and greater daily life responsibilities, along with the sense of being supported and having positive and meaningful social roles in relationships with spouses, children, sons-in-law, daughters-in-law, and grandchildren residing in the same household, contribute significantly to the observed differences [46].
Furthermore, this study revealed that the prevalence of stress during the COVID-19 pandemic was higher, consistent with Salari et al. [97], Al Maqbali et al. [98], and Zhang et al. [99]. The COVID-19 virus, originating from China, not only presents physical health challenges but also causes fatigue, stress, and anxiety [100]. Fears of death, illness, the spread of false news and rumors, and reduced social interactions were among the factors that heightened stress due to the coronavirus.
The high prevalence of depression, anxiety, and stress found in the present systematic review and meta-analysis underscores the need for further investigation and follow-up for these conditions. Depression, anxiety, and stress are considered among the most significant health challenges facing the elderly, with far-reaching health and economic consequences, including an increased risk of suicide. The implementation of policies and strategies to reduce and control risk factors can mitigate the long-term burden of these disorders on society. Identifying populations at higher risk and providing effective and regular quality medical care can slow down the disease progression and reduce its adverse effects.
One of the limitations of this study was the limited number of studies conducted on the prevalence of stress in cardiac patients. It is recommended to conduct more studies with larger sample sizes in different countries to better understand the prevalence of stress in the elderly. Other limitations of the current research were not accessing all articles and unpublished reports, different reporting methods, non-random selection of some samples, methodological heterogeneity, and inadequate and low-quality reporting in some studies. Furthermore, the high heterogeneity in studies (over 99%) led us to perform subgroup analysis, which reduced the level of heterogeneity; however, heterogeneity was still high in the sugroups, possibly due to differences in sample size, demographic characteristics, and study methodology. Further systematic reviews and meta-analyses are recommended in the field of the prevalence of other mental disorders in the elderly and also the prevalence of depression, anxiety, and stress in other populations such as diabetic patients, hemodialysis patients, cancer patients, etc., while addressing the limitations mentioned in the current study.
Conclusion
The results of this study indicated a high prevalence of depression, anxiety, and stress in the elderly. Therefore, healthcare professionals and policymakers need to pay more attention to prevention and control of these disorders.
Acknowledgements
We would like to thank the esteemed officials of that center for accepting the financial expenses of this study. This study is the result of research project No. 50003251 approved by the Student Research Committee of Kermanshah University of Medical Sciences.
Author contributions
M.K, A.Z and A.J contributed to the design, Z.K, R. P. K, A.J and M. K participated in most of the study steps. M.K, B.E, M.R and A.Z prepared the manuscript. M.K, J. S.M, A.Z and A.J assisted in designing the study, and helped in the, interpretation of the study. All authors have read and approved the content of the manuscript.
Funding
None.
Data availability
Datasets are available through the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Conflict of interest
There is no confict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kalstad AA, Myhre PL, Laake K, Tveit SH, Schmidt EB, Smith P, et al. Effects of n-3 fatty acid supplements in elderly patients after myocardial infarction: a randomized, controlled trial. Circulation. 2021;143(6):528–39. [DOI] [PubMed] [Google Scholar]
- 2.Whittington FJ, Kunkel SR, de Medeiros K. Global aging–comparative perspectives on aging and the life course. Culture. 2019;3:4. [Google Scholar]
- 3.Hurjui I, Hurjui CM. Population aging and the influence on healthcare spending. ROMANIAN J Legal Med. 2018;26(4):453–6. [Google Scholar]
- 4.McMaughan DJ, Oloruntoba O, Smith ML. Socioeconomic status and access to healthcare: interrelated drivers for healthy aging. Front Public Health. 2020;8:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mar L. Population Aging in Canada: examining the caregiving needs of the elderly. Sociol Imagination: Undergrad J. 2020;6(1):67–78. [Google Scholar]
- 6.Mealy A, Sorensen J. Effects of an aging population on hospital costs related to elective hip replacements. Public Health. 2020;180:10–6. [DOI] [PubMed] [Google Scholar]
- 7.Wang J, Maxwell CA, Yu F. Biological processes and biomarkers related to frailty in older adults: a state-of-the-science literature review. Bio Res Nurs. 2019;21(1):80–106. [DOI] [PubMed] [Google Scholar]
- 8.Phillips DR, Gyasi RM. Global aging in a comparative context. Oxford University Press US; 2021.
- 9.Larsen PD. Geroscience: the intersection of basic aging biology, chronic disease, and health. LWW; 2019. pp. 187–8. [DOI] [PubMed]
- 10.Valieiny N, Poorcheraghi H, Pashaeypoor S. Nursing interventions in prevention of fall in older adults; an Integrated review study. J Gerontol. 2022;6(4):14–27. [Google Scholar]
- 11.Lee K, Jeong G-C, Yim J. Consideration of the psychological and mental health of the elderly during COVID-19: a theoretical review. Int J Environ Res Public Health. 2020;17(21):8098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hosseini FS, Sharifi N, Jamali S. Correlation anxiety, stress, and depression with perceived social support among the elderly: a cross-sectional study in Iran. Agein Int. 2021;46:108–14. [Google Scholar]
- 13.Mawar S, Koul P, Das S, Gupta S. Association of physical problems and depression with elder abuse in an urban community of North India. Indian j Community med. 2018;43(3):165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yu J, Rawtaer I, Fam J, Jiang MJ, Feng L, Kua EH, et al. Sleep correlates of depression and anxiety in an elderly A sian population. Psychogeriatrics. 2016;16(3):191–5. [DOI] [PubMed] [Google Scholar]
- 15.Nazari B, Bakhshi S, Kaboudi M, Dehghan F, Ziapour A, Montazeri N. A comparison of quality of life, anxiety and depression in children with cancer and healthy children, Kermanshah-Iran. Int J Pediatr. 2017;5(7):5305–14. [Google Scholar]
- 16.Karami N, Kazeminia M, Karami A, Salimi Y, Ziapour A, Janjani P. Global prevalence of depression, anxiety, and stress in cardiac patients: a systematic review and meta-analysis. J Affect Disord. 2023;324:175–89. [DOI] [PubMed] [Google Scholar]
- 17.Momeni K, Salimi Y, Majzoobi MR, Ziapour A, Janjani P. Anxiety, coping style and hopelessness during COVID-19 pandemic: an Iranian population-based study. Health Sci Rep. 2023;6(5):e1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salehi N, Afrashteh MY, Majzoobi MR, Ziapour A, Janjani P, Karami S. Does coping with pain help the elderly with cardiovascular disease? The association of sense of coherence, spiritual well-being and self-compassion with quality of life through the mediating role of pain self-efficacy. BMC Geriatr. 2023;23(1):393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sinoff G. Thanatophobia (death anxiety) in the elderly: the problem of the child’s inability to assess their own parent’s death anxiety state. Front Med. 2017:11. [DOI] [PMC free article] [PubMed]
- 20.Issalillah F, Aisyah N. The Elderly and the determinants of stress. J Soc Sci Stud. 2022;2(1):9–12. [Google Scholar]
- 21.Ansari S, Kang TK. Stress of aged elderly: a review. Indian J Health Wellbe. 2019;10(4–6):162–5. [Google Scholar]
- 22.Zenebe Y, Akele B, W/Selassie M, Necho M. Prevalence and determinants of depression among old age: a systematic review and meta-analysis. Ann Gen Psychiatry. 2021;20(1):55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sarokhani D, Parvareh M, Dehkordi AH, Sayehmiri K, Moghimbeigi A. Prevalence of depression among Iranian elderly: systematic review and meta-analysis. Iran J Psychiatry. 2018;13(1):55. [PMC free article] [PubMed] [Google Scholar]
- 24.Abdoli N, Salari N, Darvishi N, Jafarpour S, Solaymani M, Mohammadi M, et al. The global prevalence of major depressive disorder (MDD) among the elderly: a systematic review and meta-analysis. Neurosci BiobehavRev. 2022;132:1067–73. [DOI] [PubMed] [Google Scholar]
- 25.Yan Y, Du X, Lai L, Ren Z, Li H. Prevalence of depressive and anxiety symptoms among Chinese older adults during the COVID-19 pandemic: a systematic review and meta-analysis. J Geriatric Psychiatry Neurol. 2022;35(2):182–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Anwar A, Yadav UN, Huda MN, Das S, Rosenbaum S, Ali AM et al. Anxiety and stress related to COVID-19 among the community dwelling older adults residing in the largest refugee camp of the world. Community Mental Health J. 2023:1–12. [DOI] [PMC free article] [PubMed]
- 27.Assil S, Zeidan Z. Prevalence of depression and associated factors among elderly Sudanese: a household survey in Khartoum State. EMHJ-Eastern Mediterranean Health J. 19 (5), 435–440, 2013. 2013. [PubMed]
- 28.Barakat MM, Elattar NF, Zaki HN. Depression, anxiety and loneliness among elderly living in geriatric homes. Am J Nurs Res. 2019;7(4):400–11. [Google Scholar]
- 29.Blazer D, Hughes DC, George LK. The epidemiology of depression in an elderly community population. Gerontol. 1987;27(3):281–7. [DOI] [PubMed] [Google Scholar]
- 30.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372. [DOI] [PMC free article] [PubMed]
- 31.Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evidence-Based Healthc. 2015;13(3):147–53. [DOI] [PubMed] [Google Scholar]
- 32.Maercker A, Forstmeier S, Enzler A, Krüsi G, Hörler E, Maier C, et al. Adjustment disorders, posttraumatic stress disorder, and depressive disorders in old age: findings from a community survey. Comprehens Psychiatry. 2008;49(2):113–20. [DOI] [PubMed] [Google Scholar]
- 33.Kvaal K, Macijauskiene J, Engedal K, Laake K. High prevalence of anxiety symptoms in hospitalized geriatric patients. Int J Geriatric Psychiatry. 2001;16(7):690–3. [DOI] [PubMed] [Google Scholar]
- 34.Babazadeh T, Sarkhoshi R, Bahadori F, Moradi F, Shariat F. Prevalence of depression, anxiety and stress disorders in elderly people residing in Khoy, Iran (2014–2015). J Anal Res Clin Med. 2016;4(2):122–8. [Google Scholar]
- 35.Thapa DK, Visentin DC, Kornhaber R, Cleary M. Prevalence and factors associated with depression, anxiety, and stress symptoms among older adults: a cross-sectional population‐based study. Nurs Health Sci. 2020;22(4):1139–52. [DOI] [PubMed] [Google Scholar]
- 36.Kirmizioglu Y, Doğan O, Kuğu N, Akyüz G. Prevalence of anxiety disorders among elderly people. Int J Geriatric Psychiatry: J Psychiatry Late Life Allied Sci. 2009;24(9):1026–33. [DOI] [PubMed] [Google Scholar]
- 37.Wongpakaran N, Wongpakaran T, Lerttrakarnnon P, Jiraniramai S, Sirirak T, Assanangkornchai S, et al. Prevalence, clinical and psychosocial variables of depression, anxiety and suicidality in geriatric tertiary care settings. Asian J Psychiatry. 2019;41:38–44. [DOI] [PubMed] [Google Scholar]
- 38.Raeisvandi A, Amerzadeh M, Hajiabadi F, Hosseinkhani Z. Prevalence and the affecting factors on depression, anxiety and stress (DASS) among elders in Qazvin City, in the Northwest of Iran. BMC Geriatr. 2023;23(1):202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jayakody DM, Almeida OP, Speelman CP, Bennett RJ, Moyle TC, Yiannos JM, et al. Association between speech and high-frequency hearing loss and depression, anxiety and stress in older adults. Maturitas. 2018;110:86–91. [DOI] [PubMed] [Google Scholar]
- 40.Chen J-L, Luo R, Liu M. Prevalence of depression and anxiety and associated factors among geriatric orthopedic trauma inpatients: a cross-sectional study. World J Clin Cases. 2022;10(3):919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Milani RV, Lavie CJ. Prevalence and effects of cardiac rehabilitation on depression in the elderly with coronary heart disease. Am J Cardiol. 1998;81(10):1233–6. [DOI] [PubMed] [Google Scholar]
- 42.Malhotra V, Javed D, Bharshankar R, Singh V, Gautam N, Mishra S, et al. Prevalence and predictors of Depression, anxiety and stress among Elderly during COVID-19: a cross-sectional study from Central India. Mymensingh Med J. 2023;32(2):556–66. [PubMed] [Google Scholar]
- 43.Molyneux G, McCarthy G, McEniff S, Cryan M, Conroy R. Prevalence and predictors of carer burden and depression in carers of patients referred to an old age psychiatric service. Int Psychogeriatr. 2008;20(6):1193–202. [DOI] [PubMed] [Google Scholar]
- 44.Lindesay J, Briggs K, Murphy E. The Guy’s/Age concern survey: prevalence rates of cognitive impairment, depression and anxiety in an urban elderly community. Br J Psychiatry. 1989;155(3):317–29. [PubMed] [Google Scholar]
- 45.Pasha H, Omidvar S, Faramarzi M, Bakhtiari A. Depression, anxiety, stress, and PTSD symptoms during the first and second COVID-19 waves: a comparison of elderly, middle-aged, and young people in Iran. BMC Psychiatry. 2023;23(1):190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Marsa R, Younesi SJ, Barekati S, Ramshini M, Ghyasi H. A comparative study on stress, anxiety and depression between nursing-home elderly residents and home-dwelling elderly people. Iran J Agein. 2020;15(2):176–87. [Google Scholar]
- 47.Lu L, Shen H, Tan L, Huang Q, Chen Q, Liang M, et al. Prevalence and factors associated with anxiety and depression among community-dwelling older adults in Hunan, China: a cross-sectional study. BMC Psychiatry. 2023;23(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Canuto A, Weber K, Baertschi M, Andreas S, Volkert J, Dehoust MC, et al. Anxiety disorders in old age: psychiatric comorbidities, quality of life, and prevalence according to age, gender, and country. Am J Geriatric Psychiatry. 2018;26(2):174–85. [DOI] [PubMed] [Google Scholar]
- 49.Zhang X, Norton J, Carrière I, Ritchie K, Chaudieu I, Ancelin M-L. Generalized anxiety in community-dwelling elderly: prevalence and clinical characteristics. J Affect Disord. 2015;172:24–9. [DOI] [PubMed] [Google Scholar]
- 50.Curran E, Rosato M, Ferry F, Leavey G. Prevalence and factors associated with anxiety and depression in older adults: gender differences in psychosocial indicators. J Affect Disord. 2020;267:114–22. [DOI] [PubMed] [Google Scholar]
- 51.Richardson TM, Friedman B, Podgorski C, Knox K, Fisher S, He H, et al. Depression and its correlates among older adults accessing aging services. Am J Geriatric Psychiatry. 2012;20(4):346–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang Z, Shi Z, Wang L, Liu M. Post-traumatic stress disorder, anxiety and depression among the elderly: a survey of the hard‐hit areas a year after the Wenchuan earthquake. Stress Health. 2012;28(1):61–8. [DOI] [PubMed] [Google Scholar]
- 53.Kang H-J, Bae K-Y, Kim S-W, Shin I-S, Yoon J-S, Kim J-M. Anxiety symptoms in Korean elderly individuals: a two-year longitudinal community study. Int Psychogeriatr. 2016;28(3):423–33. [DOI] [PubMed] [Google Scholar]
- 54.Sari N, Manungkalit M. The best predictor of anxiety, stress, and depression among institutionalized elderly. Int J Public Health Sci. 2019;8(4):419–26. [Google Scholar]
- 55.Dura JR, Stukenberg KW, Kiecolt-Glaser JK. Chronic stress and depressive disorders in older adults. J Abnorm Psychol. 1990;99(3):284. [DOI] [PubMed] [Google Scholar]
- 56.Nayak S, Mohapatra MK, Panda B. Prevalence of and factors contributing to anxiety, depression and cognitive disorders among urban elderly in Odisha–A study through the health systems’ Lens. Arch Gerontol Geriatr. 2019;80:38–45. [DOI] [PubMed] [Google Scholar]
- 57.Prina AM, Ferri CP, Guerra M, Brayne C, Prince M. Prevalence of anxiety and its correlates among older adults in Latin America, India and China: cross-cultural study. Br J Psychiatry. 2011;199(6):485–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yang Z, Jia H, Lu Y, Liu S, Dai M, Zhang H. Prevalence and related factors of depression and anxiety in a cohort of Chinese elderly caregivers in the nursing home. J Affect Disord. 2021;295:1456–61. [DOI] [PubMed] [Google Scholar]
- 59.Gum AM, King-Kallimanis B, Kohn R. Prevalence of mood, anxiety, and substance-abuse disorders for older americans in the national comorbidity survey-replication. Am J Geriatric Psychiatry. 2009;17(9):769–81. [DOI] [PubMed] [Google Scholar]
- 60.Raeisvandi A, Amerzadeh M, Hajiabadi F, Hosseinkhani Z. Prevalence, modifiable and risk factors of depression, anxiety and stress (DASS) among elders in the northwest of Iran; 2022. [DOI] [PMC free article] [PubMed]
- 61.Ganatra HA, Zafar SN, Qidwai W, Rozi S. Prevalence and predictors of depression among an elderly population of Pakistan. Agin Mental Health. 2008;12(3):349–56. [DOI] [PubMed] [Google Scholar]
- 62.Mehta KM, Simonsick EM, Penninx BW, Schulz R, Rubin SM, Satterfield S, et al. Prevalence and correlates of anxiety symptoms in well-functioning older adults: findings from the health aging and body composition study. J Am Geriatr Soc. 2003;51(4):499–504. [DOI] [PubMed] [Google Scholar]
- 63.Choulagai P, Sharma C, Choulagai B. Prevalence and associated factors of depression among elderly population living in geriatric homes in Kathmandu Valley. J Inst Med Nepal. 2013;35(1):39–44. [Google Scholar]
- 64.Murrell SA, Himmelfarb S, Wright K. Prevalence of depression and its correlates in older adults. Am J Epidemiol. 1983;117(2):173–85. [DOI] [PubMed] [Google Scholar]
- 65.Sjöberg L, Karlsson B, Atti A-R, Skoog I, Fratiglioni L, Wang H-X. Prevalence of depression: comparisons of different depression definitions in population-based samples of older adults. J Affect Disord. 2017;221:123–31. [DOI] [PubMed] [Google Scholar]
- 66.El-Gabalawy R, Mackenzie CS, Shooshtari S, Sareen J. Comorbid physical health conditions and anxiety disorders: a population-based exploration of prevalence and health outcomes among older adults. Gen Hosp Psychiatry. 2011;33(6):556–64. [DOI] [PubMed] [Google Scholar]
- 67.De Oliveira Andrade N, Correia Silva Azambuja H, Carvalho Reis Martins T, Manoel Seixas RA, Moretti Luchesi B. Factors associated with depressive and anxiety symptoms in older adults during the COVID-19 pandemic: a Brazilian study. Agin Mental Health. 2022;26(8):1564–71. [DOI] [PubMed] [Google Scholar]
- 68.Neville C, Teri L. Anxiety, anxiety symptoms, and associations among older people with dementia in assisted-living facilities. Int J Mental Health Nurs. 2011;20(3):195–201. [DOI] [PubMed] [Google Scholar]
- 69.Suri M. A pilot study on prevalence of malnutrition, pain, depression and anxiety in elderly population in Delhi. J Clin Gerontol Geriatr. 2018;9(3):91–8. [Google Scholar]
- 70.Mackenzie CS, Reynolds K, Chou K-L, Pagura J, Sareen J. Prevalence and correlates of generalized anxiety disorder in a national sample of older adults. Am J Geriatric Psychiatry. 2011;19(4):305–15. [DOI] [PubMed] [Google Scholar]
- 71.Cohen CI, Magai C, Yaffee R, Walcott-Brown L. The prevalence of anxiety and associated factors in a multiracial sample of older adults. Psychiatric Serv. 2006;57(12):1719–25. [DOI] [PubMed] [Google Scholar]
- 72.Maung TM, Jain T, Jagannathan M, Noordin NB, Zhen VCY, Oo WM et al. Prevalence of depression, stress and anxiety and impact of exercise on mental health and physical performance among institutionalised older adults of Northern Malaysia. J Posit School Psychol. 2022:6681–91.
- 73.Suradom C, Wongpakaran N, Wongpakaran T, Lerttrakarnnon P, Jiraniramai S, Taemeeyapradit U et al. Prevalence and associated factors of comorbid anxiety disorders in late-life depression: findings from geriatric tertiary outpatient settings. Neuropsychiatric Disease Treat. 2019:199–204. [DOI] [PMC free article] [PubMed]
- 74.Yao M, Li H, Luo Y, Li L, Yu J. High prevalence of post-stroke anxiety in elderly patients following COVID-19 outbreak. Front Psychiatry. 2021;12:699869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mutepfa MM, Motsamai TB, Wright TC, Tapera R, Kenosi LI. Anxiety and somatization: prevalence and correlates of mental health in older people (60 + years) in Botswana. Agin Mental Health. 2021;25(12):2320–9. [DOI] [PubMed] [Google Scholar]
- 76.Zhang AY, Cooper GS. Recognition of depression and anxiety among elderly colorectal cancer patients. Nurs Res Practice. 2010;2010. [DOI] [PMC free article] [PubMed]
- 77.Choi NG, McDougall GJ. Comparison of depressive symptoms between homebound older adults and ambulatory older adults. Agin Mental Health. 2007;11(3):310–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bloch F, Blandin M, Ranerison R, Claessens Y, Rigaud A, Kemoun G. Anxiety after a fall in elderly subjects and subsequent risk of developing post traumatic stress disorder at two months. A pilot study. J Nutr Health Agin. 2014;18:303–6. [DOI] [PubMed] [Google Scholar]
- 79.Gonçalves DC, Pachana NA, Byrne GJ. Prevalence and correlates of generalized anxiety disorder among older adults in the Australian national survey of mental health and well-being. J Affect Disord. 2011;132(1–2):223–30. [DOI] [PubMed] [Google Scholar]
- 80.Forlani M, Morri M, Belvederi Murri M, Bernabei V, Moretti F, Attili T, et al. Anxiety symptoms in 74 + community-dwelling elderly: associations with physical morbidity, depression and alcohol consumption. PLoS ONE. 2014;9(2):e89859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Taha T, Rahman A. Anxiety and depression in lone elderly living in their own homes and going to geriatric clubs versus those living in geriatric homes. 2006.
- 82.Arbus C, Hergueta T, Duburcq A, Saleh A, Le Guern M-E, Robert P, et al. Adjustment disorder with anxiety in old age: comparing prevalence and clinical management in primary care and mental health care. Eur Psychiatry. 2014;29(4):233–8. [DOI] [PubMed] [Google Scholar]
- 83.Bunce D, Batterham PJ, Mackinnon AJ, Christensen H. Depression, anxiety and cognition in community-dwelling adults aged 70 years and over. J Psychiatric Res. 2012;46(12):1662–6. [DOI] [PubMed] [Google Scholar]
- 84.Silveira MMd, Portuguez MW. Analysis of life quality and prevalence of cognitive impairment, anxiety, and depressive symptoms in older adults. Estudos De Psicol (Campinas). 2017;34:261–8. [Google Scholar]
- 85.Do Cetin DC, Nasr G. Obesity in the elderly: more complicated than you think. Clevel Clin J Med. 2014;81(1):51. [DOI] [PubMed] [Google Scholar]
- 86.Barbosa MB, Pereira CV, Cruz DTd, Leite ICG. Prevalence and factors associated with alcohol and tobacco use among non-institutionalized elderly persons. Revista Brasileira De Geriatria E Gerontol. 2018;21:123–33. [Google Scholar]
- 87.Pang S, Subramaniam M, Abdin E, Lee SP, Chua BY, Shafie SB, et al. Prevalence and predictors of tobacco use in the elderly. Int J Geriatric Psychiatry. 2016;31(7):716–22. [DOI] [PubMed] [Google Scholar]
- 88.Rodriguez JC, Dzierzewski JM, Alessi CA. Sleep problems in the elderly. Med Clin. 2015;99(2):431–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Niu H, Álvarez-Álvarez I, Guillén-Grima F, Aguinaga-Ontoso I. Prevalence and incidence of Alzheimer’s disease in Europe: a meta-analysis. Neurología (English Edition). 2017;32(8):523–32. [DOI] [PubMed] [Google Scholar]
- 90.Chawla K, Kunonga TP, Stow D, Barker R, Craig D, Hanratty B. Prevalence of loneliness amongst older people in high-income countries: a systematic review and meta-analysis. PLoS ONE. 2021;16(7):E0255088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Salari N, Darvishi N, Ahmadipanah M, Shohaimi S, Mohammadi M. Global prevalence of falls in the older adults: a comprehensive systematic review and meta-analysis. J Orthop Surg Res. 2022;17(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Rajati F, Rajati M, Rasulehvandi R, Kazeminia M. Prevalence of stroke in the elderly: a systematic review and meta-analysis. Interdisciplinary Neurosurg. 2023:101746.
- 93.Colpani V, Baena CP, Jaspers L, Van Dijk GM, Farajzadegan Z, Dhana K, et al. Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: a systematic review and meta-analysis. Eur J Epidemiol. 2018;33:831–45. [DOI] [PubMed] [Google Scholar]
- 94.Gottlieb SS, Khatta M, Friedmann E, Einbinder L, Katzen S, Baker B, et al. The influence of age, gender, and race on the prevalence of depression in heart failure patients. J Am Coll Cardiol. 2004;43(9):1542–9. [DOI] [PubMed] [Google Scholar]
- 95.Kaboudi M, Dehghan F, Ziapour A. The effect of acceptance and commitment therapy on the mental health of women patients with type II diabetes. Ann Trop Med Public Health. 2017;10(6):1709–13. [Google Scholar]
- 96.Vigod SN, Tarasoff LA, Bryja B, Dennis C-L, Yudin MH, Ross LE. Relation between place of residence and postpartum depression. CMAJ. 2013;185(13):1129–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob Health. 2020;16(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Al Maqbali M, Al Sinani M, Al-Lenjawi B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: a systematic review and meta-analysis. J Psychosom Res. 2021;141:110343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zhang L, Pan R, Cai Y, Pan J. The prevalence of post-traumatic stress disorder in the general population during the COVID-19 pandemic: a systematic review and single-arm meta-analysis. Psychiatry Investigat. 2021;18(5):426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Shanbehzadeh S, Tavahomi M, Zanjari N, Ebrahimi-Takamjani I, Amiri-Arimi S. Physical and mental health complications post-COVID-19: scoping review. J Psychosom Res. 2021;147:110525. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Datasets are available through the corresponding author upon reasonable request.