Abstract
Background
Respiratory Syncytial Virus (RSV) is an important pathogen causing acute respiratory illnesses in adults. RSV infection can lead to severe outcomes, including hospitalizations and even death. Despite the increased recognition of the burden in older adults, immediate post-discharge care needs among adults hospitalized with RSV are not well characterized and have not been compared to other serious medical conditions (such as influenza, acute myocardial infarction (MI), and stroke) for which there have been long-standing disease prevention efforts.
Objectives
This study aims to describe the immediate post-discharge care needs among adults hospitalized with RSV in the United States and descriptively compare it to those hospitalized with influenza, acute MI, or stroke.
Design
Retrospective observational cohort study.
Patients
Adults aged ≥ 18 years, hospitalized with a primary diagnosis of RSV, influenza, acute MI, or stroke from January 01, 2016, to December 31, 2019, were identified from the Premier Healthcare Database using the International Classification of Diseases (ICD-10) codes.
Main measures
Immediate post-discharge care was categorized into three different levels of care based on the discharge dispositions. Descriptive analyses were performed.
Key results
In total, 3,629 RSV, 303,577 influenza, 388,682 acute MI, and 416,750 stroke hospitalizations were identified, the majority occurred among patients aged ≥ 65 years. Professional home care needs were the highest for RSV hospitalizations (19.1%), followed by influenza (17.7%), stroke (15.4%), and acute MI (9.8%). Additionally, institutional care needs immediately following discharge were similar for RSV, influenza, and acute MI hospitalizations (14.2%, 15.8%, and 14.1%, respectively).
Conclusions
Immediate post-discharge care needs among adults hospitalized with RSV, especially in older adults, can be considerable and comparable to influenza and acute MI discharges. With recently approved RSV vaccines, efforts to increase vaccination in older adults are needed to prevent RSV and associated healthcare consequences.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12890-024-03251-y.
Keywords: Respiratory Syncytial Virus, Respiratory infections, Adults, Hospitalization, Post-discharge care
Introduction
Respiratory Syncytial Virus (RSV) is a common cause of acute respiratory illnesses in adults and usually causes mild, cold-like symptoms; however, RSV is increasingly recognized as a cause of serious illness among older adults, immunocompromised adults, and those with underlying medical conditions such as chronic heart and lung conditions [1–3]. Each year in the United States (US), RSV infection results in an estimated 60,000-160,000 hospitalizations, 119,000 emergency department admissions, 1.4 million outpatient visits, and 6,000–10,000 deaths among adults aged 65 years and older [4, 5]. RSV also imposes a substantial economic burden, with annual hospitalization costs in adults exceeding $1 billion in the US [6].
The burden of RSV in adults has remained largely underrecognized from the healthcare system, provider, and patient perspectives [4, 5, 7]. The limited awareness is due to multiple factors, including infrequent RSV testing, [8] lack of RSV-specific anti-viral treatments, [9] low sensitivity of standard-of-care clinical testing approaches, [10, 11] and no effective targeted prevention until the recent regulatory approval of RSV vaccines for older adults [12]. Attempts to raise awareness have been made by comparing the clinical, economic, and humanistic burden of RSV to a well-recognized viral illness, influenza, that causes a significant public health burden [13–18]. Previous studies have reported substantial care needs among adults hospitalized with influenza following discharge [13, 17]. Additionally, few studies reported similar or worse clinical outcomes in adults hospitalized with RSV than influenza [13, 14, 17, 19]. These studies indicated that follow-up care after RSV-associated hospitalization is common and extends well beyond the acute phase of the illness. However, these studies were limited by sample size and geography, which made it difficult to discern whether the post-discharge care was attributable to the RSV infection or other underlying conditions.
The clinical outcomes and the intensity of healthcare resource use associated with RSV hospitalization and post-discharge care have not been considered in the context of other common causes of hospitalization, such as acute myocardial infarction (MI) and stroke. These conditions are often targets for prevention by healthcare providers and healthcare systems due to their prevalence, high costs, availability of lifestyle and medication strategies for prevention and risk reduction, and the potential for additional care needs after hospitalization [20–24]. In this new era of RSV vaccine availability for older adults, [12] mobilization of primary prevention efforts should prioritize costly diseases that lead to hospitalization and higher-level care following discharge. We aim to further understand the medical care needs immediately after discharge from RSV hospitalizations and descriptively compare that to the care needs of other common acute medical events such as influenza, acute MI, or stroke hospitalizations.
Methods
Data source
This retrospective cohort study utilized data from the Premier Healthcare Database (PHD), which contains all-payer hospital administrative and billing data from a nationwide network of US hospitals captured across a geographically diverse area. Inpatient admissions include over 160 million visits, with more than 9 million per year since 2012, representing approximately 25% of annual US inpatient admissions [25]. This dataset includes information on demographics and disease states, admission and discharge diagnoses, data on billed services, patient dispositions, and discharge health status, with less than 0.01% missing data [25]. All data in PHD were structured, de-identified, and fully compliant with the Health Insurance Portability and Accountability Act of 1996 (HIPAA); [26, 27] The study did not require informed consent or institutional review board approval.
Study population
The study population consisted of adults aged ≥ 18 years, hospitalized with a primary diagnosis of RSV, influenza, acute MI, or stroke between January 1, 2016, to December 31, 2019, defined as the assessment period. Data beyond 2019 were not included to limit the impact of the COVID-19 pandemic on changes in patient preferences for receiving medical services as well as changes in hospital discharge considerations [28, 29]. The four conditions were identified using the International Classification of Diseases, 10th revision, Clinical Modification (ICD-10-CM) codes (Table S1 in Supplemental Material 1). Hospitalizations were classified into four different cohorts (RSV, influenza, acute MI, and stroke). Because a patient could have multiple hospitalizations due to the four conditions of interest during the assessment period, we allowed patients to contribute to more than one disease cohort or the same disease cohort more than once if the additional hospitalization met the inclusion/exclusion criteria described below.
Inclusion and exclusion criteria
The study included hospitalizations for one of the four conditions of interest (RSV, influenza, acute MI, or stroke), and primary diagnosis was used to determine the reason for hospitalization. Patients were admitted from a non-healthcare facility point of origin (i.e., community-dwelling individuals) and subsequently discharged or transferred to either home or self-care, home health organization, hospice-home, hospice-medical facility, another rehab facility, skilled nursing facility (SNF), intermediate care facility (ICF), long-term care (LTC) hospital, or other facilities, or those who died during their hospital stay. These discharge dispositions were the 10 most common and accounted for approximately 98% of discharge records. Hospitalizations in which patients were admitted from clinics or transferred from inpatient facilities, LTC facilities, or home health aides were excluded. Hospitalizations were also excluded if the patient had more than one diagnosis of conditions of interest (RSV, influenza, acute MI, or stroke) in the primary and secondary diagnosis positions during the same hospitalization. Lastly, readmissions due to the primary diagnosis of one of the four conditions within 90 days of any prior hospitalization related to those conditions were excluded. The included hospitalizations, referred to as qualifying hospitalizations, were analyzed separately for each of the four conditions of interest (Algorithm S1 and Figure S1 in Supplemental Material 1).
Socio-demographic, clinical characteristics, and healthcare resource utilization
Demographics (age, sex, race), hospital geographic region, and payer type were captured. Risk conditions assessed included cardiopulmonary, cardiovascular, hematological, hepatic, metabolic, neurologic, pulmonary, and renal conditions, as well as immunocompromising and obesity-related comorbidities. These conditions were defined based on RSV and influenza risk factors outlined by the US Advisory Committee of Immunization Practices (ACIP) [30, 31] and were further identified using ICD-9-CM and ICD-10-CM codes (Supplemental Material 2). All comorbidities were assessed during each qualifying hospitalization as well as during a period of up to 12 months prior to the qualifying hospitalization at the same hospital facility. The qualifying hospitalizations were classified as high-risk if at least one primary or secondary diagnosis of the mentioned comorbidities was present. Charlson comorbidity index (CCI) was calculated to summarize morbidity. Assessment of healthcare resource utilization included intensive care unit (ICU) admission, mechanical ventilator use, inpatient length of stay (LOS), and length of ICU stay.
Measured outcomes
The primary study outcome was immediate post-discharge care categorized into three levels as outlined in Table 1: elevated, moderate, and same or lower level of care. In-hospital death was also captured.
Table 1.
Levels of immediate post-discharge care
| Admitting source* | Discharge disposition category | Discharge disposition description† | Levels of care |
|---|---|---|---|
| Non-Healthcare Facility Point of Origin | Death | Expired | In-hospital death |
| Rehabilitation Facility |
Discharged/transferred to another rehab facility |
Elevated care | |
| LTC Facility | Discharged/transferred to SNF | Elevated care | |
| Discharged/transferred to ICF | |||
| Discharged to hospice-medical facility | |||
| Discharged/transferred to a LTC hospital | |||
| Hospital or Inpatient Facility | Discharged/ transferred to other facility | Elevated care | |
| Home Health | Discharged to home health organization | Moderate care | |
| Discharged to hospice-home | |||
| Home or Self-Care | Discharged to home or self-care | Same or lower care |
List of Abbreviations: ICF: Intermediate Care Facility; LTC: Long-term Care; SNF: Skilled Nursing Facility
Notes:
*Only “Non-Healthcare Facility Point of Origin” as admitting source was utilized
†Feasibility assessments were conducted. Top 10 discharge disposition codes were used for the analysis
Statistical analysis
All analyses were conducted at the hospitalization level. Descriptive statistics were used to summarize socio-demographic, hospital and clinical characteristics, and healthcare resource utilization. Categorical variables were described using frequencies and percentages, while for continuous variables, mean and standard deviation were reported. To describe the immediate post-discharge care, frequencies, and percentages of discharge disposition categories, along with the defined levels of care (as outlined in Table 1) were reported. A Sankey diagram was employed to visually represent the transition in care. The results were separately summarized for each of the four cohorts. Analyses were also stratified by age (18–64 [younger adults] vs. ≥65 [older adults] years). Data management and analysis were conducted using SAS version 9.4 (SAS Institute, Cary, NC).
Results
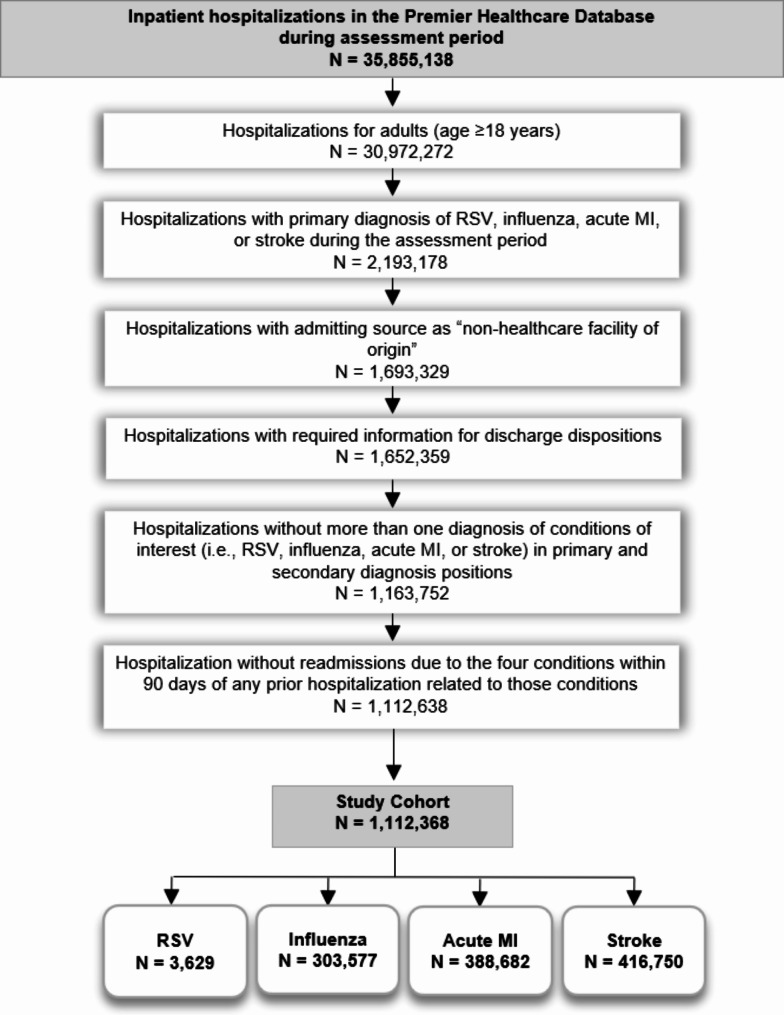
Among 1,112,638 qualifying hospitalizations identified from the PHD during the assessment period (Fig. 1), there were 3,629 RSV, 303,577 influenza, 388,682 acute MI, and 416,750 stroke hospitalizations, with mean ages of 71.4, 65.5, 65.9, and 69.8 years, respectively (Table 2). A high proportion of hospitalizations were observed among older adults (≥ 65 years), ranging from 70.5% in RSV cohort to 53.6% in acute MI cohort. There were more females in RSV and influenza cohorts, more males in the acute MI cohort, and similar gender distribution in the stroke cohort (Table 2). Approximately half of the hospitalizations in RSV, influenza, and stroke cohorts had a cardiovascular comorbidity. In the acute MI cohort, all hospitalizations with acute MI at presentation were counted towards the pre-existing cardiovascular comorbid condition frequencies (Table 3). Pulmonary comorbidities were common in RSV (43.8%) and influenza (71.2%) cohorts. Most qualifying hospitalizations (> 90%) included a diagnosis of a high-risk condition.
Fig. 1.
Flow diagram of study cohort
List of Abbreviations: ICD: International Classification of Diseases; MI: Myocardial Infarction; N: Number of unique hospitalizations; RSV: Respiratory Syncytial Virus
Table 2.
Socio-demographic characteristics for adults hospitalized with RSV, influenza, acute MI, or stroke
| Characteristics | RSV [N = 3,629] |
Influenza [N = 303,577] |
Acute MI [N = 388,682] |
Stroke [N = 416,750] |
|---|---|---|---|---|
| Age (in years) [Mean (SD)] | 71.4 (15.7) | 65.5 (16.4) | 65.9 (13.6) | 69.8 (13.9) |
| Age group (in years) [N (%)] | ||||
| 18–64 | 1,070 (29.5) | 128,751 (42.4) | 180,234 (46.4) | 142,648 (34.2) |
| ≥ 65 | 2,559 (70.5) | 174,826 (57.6) | 208,448 (53.6) | 274,102 (65.8) |
| Sex [N (%)] | ||||
| Male | 1,312 (36.2) | 135,696 (44.7) | 244,451 (62.9) | 207,683 (49.8) |
| Female | 2,317 (63.8) | 167,838 (55.3) | 144,162 (37.1) | 208,981 (50.1) |
| Unknown | - | 43 (0.0) | 69 (0.0) | 86 (0.0) |
| Race [N (%)] | ||||
| White | 2,707 (74.6) | 229,437(75.6) | 299,314 (77.0) | 297,034 (71.3) |
| Black | 433 (11.9) | 45,023 (14.8) | 44,563 (11.5) | 72,715 (17.4) |
| Asian | 97 (2.7) | 5,339 (1.8) | 9,076 (2.3) | 11,191 (2.7) |
| Other | 305 (8.4) | 19,300 (6.4) | 28,447 (7.3) | 28,235 (6.8) |
| Unable to determine | 87 (2.4) | 4,478 (1.5) | 7,282 (1.9) | 7,575 (1.8) |
| Hospital Geographic Region [N (%)] | ||||
| Midwest | 684 (18.8) | 67,826 (22.3) | 78,769 (20.3) | 79,628 (19.1) |
| Northeast | 1,204 (33.2) | 45,770 (15.1) | 59,551 (15.3) | 63,341 (15.2) |
| South | 1,420 (39.1) | 137,955 (45.4) | 185,620 (47.8) | 207,639 (49.8) |
| West | 321 (8.8) | 52,026 (17.1) | 64,742 (16.7) | 66,142 (15.9) |
| Payer Type [N (%)] | ||||
| Medicare | 2,690 (74.1) | 198,275 (65.3) | 215,123 (55.3) | 276,971 (66.5) |
| Medicaid | 321 (8.8) | 37,994 (12.5) | 34,987 (9.0) | 36,018 (8.6) |
| Commercial | 505 (13.9) | 47,385 (15.6) | 104,018 (26.8) | 74,375 (17.8) |
| Uninsured | 61 (1.7) | 11,924 (3.9) | 22,340 (5.7) | 19,266 (4.6) |
| Others | 52 (1.4) | 7,999 (2.6) | 12,214 (3.1) | 10,120 (2.4) |
List of Abbreviations: MI: Myocardial Infarction; N: Number of unique hospitalizations; RSV: Respiratory Syncytial Virus
Table 3.
Clinical characteristics and healthcare resource utilization for adults hospitalized with RSV, influenza, acute MI, or stroke
| Characteristics | RSV [N = 3,629] |
Influenza [N = 303,577] |
Acute MI [N = 388,682] |
Stroke [N = 416,750] |
|---|---|---|---|---|
| CCI [Mean (SD)] | 2.9 (2.4) | 3.0 (2.5) | 3.1 (2.2) | 3.8 (2.3) |
| Risk conditions [N (%)] | ||||
| Cardiopulmonary | 198 (5.5) | 21,279 (7.0) | 11,574 (3.0) | 8,492 (2.0) |
| Cardiovascular | 2,030 (55.9) | 166,549 (54.9) | 388,682 (100.0) | 203,549 (48.8) |
| Hematological | 638 (17.6) | 41,996 (13.8) | 30,756 (7.9) | 27,249 (6.5) |
| Hepatic | 104 (2.9) | 12,946 (4.3) | 6,169 (1.6) | 6,909 (1.7) |
| Metabolic | 1,349 (37.2) | 108,623 (35.8) | 157,666 (40.6) | 167,403 (40.2) |
| Neurologic | 897 (24.7) | 67,252 (22.2) | 103,024 (26.5) | 377,531 (90.6) |
| Pulmonary | 1,591 (43.8) | 216,071 (71.2) | 82,984 (21.4) | 79,340 (19.0) |
| Renal | 1,067 (29.4) | 74,321 (24.5) | 87,775 (22.6) | 81,971 (19.7) |
| Immunocompromising | 621 (17.1) | 45,778 (15.1) | 22,807 (5.9) | 30,531 (7.3) |
| Obesity-related | 424 (11.7) | 45,680 (15.0) | 34,589 (8.9) | 28,501 (6.8) |
| Risk Group [N (%)] | ||||
| High-risk | 3,311 (91.2) | 282,039 (92.9) | 388,682 (100.0) | 402,259 (96.5) |
| Healthcare Resource Utilization | ||||
| ICU admission [N (%)] | 111 (3.1) | 58,402 (19.2) | 106,291 (27.3) | 93,638 (22.5) |
| MV Use [N (%)] | 19 (0.5) | 48,098 (15.8) | 23,112 (5.9) | 6,527 (1.6) |
| Length of inpatient stay [Mean (SD)] | 4.0 (2.8) | 4.3 (4.4) | 3.3 (3.1) | 4.2 (4.8) |
| Length of ICU stay [Mean (SD)] | 2.3 (2.3) | 2.8 (3.8) | 1.5 (1.6) | 1.9 (2.4) |
List of Abbreviations: CCI: Charlson Comorbidity Index; ICU: Intensive Care Unit; MI: Myocardial Infarction; MV: Mechanical Ventilator; N: Number of unique hospitalizations; RSV: Respiratory Syncytial Virus
The proportion of ICU admissions was highest in the acute MI cohort (27.3%) and lowest in the RSV cohort (3.1%). The highest proportion of mechanical ventilator use was reported for influenza hospitalizations (15.8%), followed by acute MI (5.9%), stroke (1.6%), and RSV (0.5%) hospitalizations. The mean inpatient LOS was similar for RSV, influenza, acute MI, and stroke cohorts, ranging from 3.3 to 4.3 days. The mean ICU LOS ranged from 1.5 to 2.8 days.
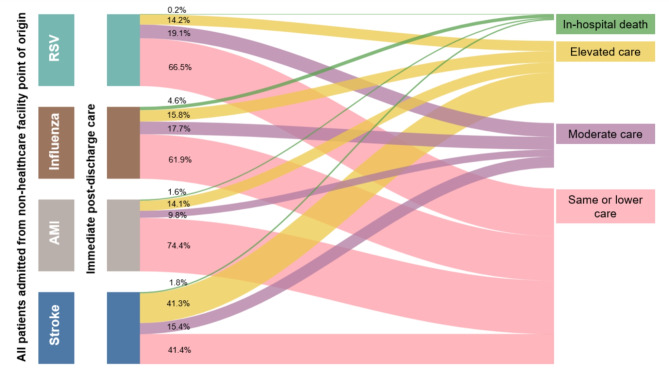
Most hospitalizations for RSV, influenza, or acute MI were associated with patients being discharged to home or self-care (61.9–74.4%), with the exception of the stroke cohort (41.4%) (Fig. 2 and Table S2 in Supplemental Material 1). Moderate care needs were 19.1% in the RSV cohort, similar to influenza (17.7%) and the stroke cohort (15.4%). Acute MI cohort had the lowest (9.8%) moderate care needs. Elevated care immediately after hospital discharge was 14.2% for RSV, similar to influenza (15.8%) and acute MI (14.1%). A notable proportion of the stroke cohort needed elevated care (41.3%).
Fig. 2.
Immediate post-discharge care or in-hospital death among adults hospitalized with RSV, influenza, acute MI, or stroke
List of Abbreviations: MI: Myocardial Infarction; RSV: Respiratory Syncytial Virus
In age-stratified analysis, the mean ages ranged from 50.2 to 54.1 years for younger adults and 76.3 to 79.8 years for older adults (Table S3 in Supplemental Material 1). The hospital LOS between younger and older adults was similar across the four cohorts. Most younger adults also had high-risk conditions similar to the older adults across the four cohorts. Interestingly, ICU admissions were similar or slightly higher in the younger than older cohorts across all four conditions (Table S4 in Supplemental Material 1). In general, older adults needed greater levels of both elevated and moderate care as compared to younger adults across all four cohorts (Table 4). Among older adults, the percentage with elevated level of care needs was similar for RSV (18.8%), influenza (21.4%), and acute MI (19.3%), but not stroke (48.1%). A need for a moderate level of post-hospitalization care was also prevalent among older adults, ranging from 14.1% in the acute MI cohort to 23.9% in the RSV cohort. A noteworthy proportion of younger adults also needed either elevated or moderate care immediately after discharge: 11.0%, 18.9%, 13.0%, and 39.7% of RSV, influenza, acute MI, and stroke hospitalizations, respectively.
Table 4.
Immediate post-discharge care stratified by age group (in years) among adults hospitalized with RSV, influenza, acute MI, or stroke
| Cohorts | RSV | Influenza | Acute MI | Stroke | |||||
|---|---|---|---|---|---|---|---|---|---|
| Levels of care* [N (%)] |
Discharge dispositions [N (%)] |
18–64 [N = 1,070] |
≥ 65 [N = 2,559] |
18–64 [N = 128,751] |
≥ 65 [N = 174,826] |
18–64 [N = 180,234] |
≥ 65 [N = 208,448] |
18–64 [N = 142,648] |
≥ 65 [N = 274,102] |
| In-hospital death | Death |
1 (0.1) |
8 (0.3) |
4,275 (3.3) |
9,590 (5.5) |
1,154 (0.6) |
5,233 (2.5) | 1,165 (0.8) |
6,426 (2.3) |
| Elevated care | Rehabilitation Facility |
3 (0.3) |
36 (1.4) |
936 (0.7) |
2,655 (1.5) |
578 (0.3) |
2,714 (1.3) | 24,570 (17.2) | 53,732 (19.6) |
| LTC Facility |
26 (2.4) |
437 (17.1) |
7,054 (5.5) |
32,378 (18.5) |
2,198 (1.2) |
21,387 (10.3) | 11,757 (8.2) | 73,011 (26.6) | |
| Hospital or Inpatient Facility |
6 (0.6) |
7 (0.3) |
2,645 (2.1) |
2,392 (1.4) |
11,795 (6.5) |
16,117 (7.7) | 4,041 (2.8) |
5,020 (1.8) |
|
| Total |
35 (3.3) |
480 (18.8) |
10,635 (8.3) | 37,425 (21.4) |
14,571 (8.1) |
40,218 (19.3) | 40,368 (28.3) | 131,763 (48.1) | |
| Moderate care | Home Health |
82 (7.7) |
611 (23.9) |
13,599 (10.6) | 40,095 (22.9) |
8,812 (4.9) |
29,408 (14.1) | 16,269 (11.4) | 48,056 (17.5) |
| Same or lower care | Home or Self-Care |
952 (89.0) |
1,460 (57.1) | 100,242 (77.9) | 87,716 (50.2) | 155,697 (86.4) | 133,589 (64.1) | 84,846 (59.5) | 87,857 (32.1) |
List of Abbreviations: LTC: Long-term Care; MI: Myocardial Infarction; N: Number of unique hospitalizations; RSV: Respiratory Syncytial Virus
*Only “Non-Healthcare Facility Point of Origin” as admitting source was considered
Discussion
Our study found that approximately one-third of RSV hospitalizations resulted in institutional and professional home care needs immediately following discharge and were comparable to care needs of adults hospitalized with influenza or acute MI. RSV hospitalizations had similar durations of inpatient and ICU stays when compared with influenza, acute MI, and stroke hospitalizations. Consistent with the age-related trends for RSV-associated hospitalizations in the US [32] and other prior studies, [1, 4, 17, 19, 33] the present study found that a high percentage of RSV hospitalizations were among older adults (> 70%) and adults with high-risk conditions (> 90%). Further, our study found that a notable proportion (11%) of younger adults with RSV also required a higher level of care post-discharge than prior to admission. Among these younger adults, about 90% had at least one of the underlying risk conditions, demonstrating that even younger adults with underlying risk conditions required additional healthcare resources after RSV hospitalization discharge.
Few studies have documented the post-discharge care needs for adults hospitalized with RSV. A chart-review study [34] reported that 76% of older adults and 73% of other adults without chronic lung disease hospitalized with RSV required follow-up care after discharge, indicating a substantial post-discharge burden is present across different age groups. In a prospective global study that included adults ≥ 18 years who were hospitalized with RSV, 24.5% required professional home care, and 11.6% required institutional care after discharge [13]. In a retrospective study of US adults hospitalized with RSV, 10–16% required skilled nursing either at home or at a nursing facility post-discharge compared with 6.7% before the RSV admissions [34]. Among the subgroups examined, older adults and immunocompromised adults most frequently required skilled nursing [34]. This is consistent with our study, where older adults discharged from RSV hospitalization entered institutional care and home health programs at a much higher proportion than younger adults. However, in contrast to our study, many of these previous studies had limited sample sizes, and some did not indicate whether the higher-level care needs were immediately following discharge or within a defined period post-discharge.
The higher-level care needs after RSV hospitalization may partially be explained by the acute functional decline associated with RSV hospitalization in older adults [35]. In a longitudinal US study, older adults who were living in a community with assistance prior to admission had a significant decline in instrumental activities of daily living at 6 months after RSV hospitalization, while there were no significant changes in older adults living independently in the community [35]. This highlights that even among community-dwelling individuals, certain subgroups are at higher risk for functional decline from RSV hospitalization and the ensuing loss of independence that contributes to the need for elevated care after discharge.
The present study found that the needs for professional home health or institutional care immediately after discharge were comparable between the RSV and influenza cohorts. Additionally, hospitalizations with RSV exhibited a similar mean length of hospital and ICU stay as hospitalizations with influenza. This corroborates findings from prior studies which reported that the morbidity, mortality, and medical resource utilization of RSV hospitalizations were of similar magnitude as influenza hospitalizations [13, 14]. A previous study by Pastula et al. 2017, also reported a higher mean LOS (6 days) for RSV hospitalizations as compared to influenza hospitalizations (3.6 days) [15]. Similar trends were also seen in other countries [17, 18]. Unlike a few other published studies, [13, 14, 17, 36] our study found lower ICU admissions and mechanical ventilator use in patients hospitalized with RSV as compared to those with influenza. This is likely due to the higher proportion of underlying pulmonary conditions in the influenza cohort (71.2%) than in the RSV cohort (43.8%). Furthermore, lower utilization of high-intensity care (such as ICU admission and mechanical ventilator use) despite similar lengths of hospital and ICU stays in the RSV cohort as compared to the influenza cohort suggests that there may be differences in the type of resources used in the hospital across the two cohorts depending on underlying risk conditions. Given how infrequent RSV testing is in the US, this finding may not be representative of all patients with RSV infection [8].
Our study is unique in that we descriptively compared healthcare utilization and post-discharge care of RSV to completely different but important medical events of acute MI and stroke. Healthcare providers and payer organizations have focused on these common but serious medical conditions because effective preventive interventions are available. There have been substantial investments and awareness towards disease prevention efforts for influenza, acute MI, and stroke [20, 37]. By documenting that healthcare resource utilization and overall immediate post-discharge care needs for adults hospitalized with RSV are similar to needs of adults hospitalized with influenza, acute MI, or stroke, this study underscores the need for prioritizing RSV prevention efforts among older adults similar to influenza, acute MI, and stroke. With the recent regulatory approvals and US Advisory Committee on Immunization Practices (ACIP) recommendations of RSV vaccines for adults aged ≥ 75 years and those 60 to 74 years with risk conditions, [12, 38, 39] efficient implementation and high uptake among older adults will be important for RSV prevention [31].
Several limitations of this study should be noted. The PHD is an administrative and billing data set, not collected for research purposes; therefore, there may be reporting errors and omissions, thereby leading to potential misclassification. Although the admitting source was limited to a non-healthcare facility point of origin, mostly involving community-dwelling individuals, the extent of patients’ specific health and functional assistance needs in that setting prior to the hospitalization is unknown. Despite data contribution from over 1,190 hospitals across the US, [25] the patients hospitalized with RSV, influenza, acute MI, or stroke in the current study may not be representative of all US adults. In particular, RSV testing is not generally routinely conducted in adults presenting to the hospital with acute respiratory symptoms [8]. Therefore, the RSV cohort is an undercount of RSV-associated hospitalizations and may not be representative of the full clinical spectrum of adults hospitalized with RSV. This study only considered primary hospital diagnosis for identification of hospitalizations associated with conditions of interest. In the case of RSV, it is possible that hospitals use a different code as the primary diagnosis if an underlying condition is exacerbated that requires serious management, further undercounting patients with RSV and potentially impacting the representativeness of this cohort.
This study required a 90-day clean post-discharge period (i.e., no subsequent hospitalization associated with either of the four conditions of interest within 90 days of their previous hospitalizations associated with any of the four conditions of interest) to identify qualifying hospitalizations for inclusion. Readmissions within a short window due to the four conditions were not included and it is likely that there is additional higher-level care after discharge from the readmission that is not captured in the current study. Furthermore, since this study descriptively summarized outcomes associated with RSV hospitalizations to influenza, acute MI, and stroke hospitalizations using summary measures, no statistical inference testing was done across the four cohorts or in a pairwise fashion. When characterizing cardiovascular comorbidities, all acute MI hospitalizations were identified as having these and given that acute MI can occasionally result from non-cardiovascular factors, [40] it is possible that not all patients hospitalized with acute MI had cardiovascular comorbidities. This potential misclassification is not likely to impact the results presented in this study. Despite these limitations, the study includes information on a large number of patients across demographic profiles, payers, and diverse US geographic regions that improved prior study limitations on care immediately after discharge.
In conclusion, this study documents that immediate post-discharge care needs among adults hospitalized with RSV infection are considerable, especially among older adults. Adults discharged from RSV hospitalization had similar or higher use of professional home care as compared to adults discharged from influenza, acute MI, or stroke hospitalization. Elevated care involving institutional care immediately after discharge from RSV hospitalization was common with similar frequency as discharge from influenza or acute MI hospitalization. Given the substantial care needs following RSV hospitalizations, efforts to implement preventive strategies, including RSV vaccination in older adults, are needed to reduce the continued healthcare burden after RSV hospitalization.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable.
Author contributions
RS, JJ, KY, EB, PS, NA, AG, and MS participated in conceptualizing and designing the study, as well as interpreting the results. JJ contributed to the data analysis for this manuscript. PS, NA, and RS drafted the manuscript. RS, JJ, KY, EB, PS, NA, AG, and MS critically reviewed and approved the final version to be published and agreed to be accountable for all aspects of this work.
Funding
The study was sponsored by Pfizer Inc., Collegeville, PA, USA.
Data availability
The proprietary data supporting the results of this study is owned by PINC AI™ Applied Sciences but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Interested researchers may contact solutioncenter@premierinc.com for data access requests.
Declarations
Ethics approval and consent to participate
Premier Healthcare database was accessed through a commercial data licensing agreement where data used for the study was already de-identified prior to its release to study investigators, as set forth in the Data Use Agreement. Since patients cannot be contacted directly, obtaining informed consent was not applicable. The study database on health services research was fully compliant with the Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule and federal guidance on Public Welfare and the Protection of Human Subjects (45 CFR 46 § 46.101). Institutional Review Board (IRB) approval was not required.
Consent for publication
Not applicable.
Competing interests
RS, JJ, EB are employees of Pfizer Inc. and hold Pfizer stock. KY was an employee of Pfizer Inc. at the time this study was conducted. PS, NA, AG, and MS are employees of Complete HEOR Solutions (CHEORS) which received financial compensation from Pfizer Inc. for this study, including manuscript preparation. The authors have no other relevant financial relationships to disclose.
Clinical trial number
Clinical trial number is not applicable as this study was a retrospective observational study.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Falsey AR, Hennessey PA, Formica MA, Cox C, Walsh EE. Respiratory syncytial virus infection in Elderly and high-risk adults. N Engl J Med. 2005;352(17):1749–59. 10.1056/NEJMoa043951. [DOI] [PubMed] [Google Scholar]
- 2.Mesa-Frias M, Rossi C, Emond B, et al. Incidence and economic burden of respiratory syncytial virus among adults in the United States: a retrospective analysis using 2 insurance claims databases. J Manag Care Spec Pharm Published Online May. 2022;3:1–13. 10.18553/jmcp.2022.21459. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. RSV in Older Adults and Adults with Chronic Medical Conditions. Published July 14, 2023. Accessed August 22. 2023. https://www.cdc.gov/rsv/high-risk/older-adults.html
- 4.Mclaughlin JM, Khan F, Begier E, Swerdlow DL, Jodar L, Falsey AR. Rates of medically attended RSV among US adults: a systematic review and Meta-analysis. Open Forum Infect Dis. 2022;9(7). 10.1093/OFID/OFAC300. [DOI] [PMC free article] [PubMed]
- 5.Centers for Disease Control and Prevention. RSV Surveillance and Research | CDC. https://www.cdc.gov/rsv/research/index.html
- 6.Choi Y, Hill-Ricciuti A, Branche AR, et al. Cost determinants among adults hospitalized with respiratory syncytial virus in the United States, 2017–2019. Influenza Other Respir Viruses. 2022;16(1):151–8. 10.1111/irv.12912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amand C, Tong S, Kieffer A, Kyaw MH. Healthcare resource use and economic burden attributable to respiratory syncytial virus in the United States: a claims database analysis. BMC Health Serv Res. 2018;18(1):294. 10.1186/s12913-018-3066-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rozenbaum MH, Judy J, Tran D, Yacisin K, Kurosky SK, Begier E. Low levels of RSV testing among adults hospitalized for lower respiratory tract infection in the United States. Infect Dis Ther. 2023;12(2):677–85. 10.1007/s40121-023-00758-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Talbot HK, Belongia EA, Walsh EE, Schaffner W. Respiratory Syncytial Virus in older adults a Hidden Annual Epidemic. Infect Dis Clin Pract. 2016;24(6):295–302. 10.1097/IPC.0000000000000455. [Google Scholar]
- 10.Onwuchekwa C, Moreo LM, Menon S, et al. Underascertainment of respiratory syncytial virus infection in adults due to Diagnostic Testing limitations: a systematic literature review and Meta-analysis. J Infect Dis. 2023;228(2):173–84. 10.1093/infdis/jiad012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ramirez J, Carrico R, Wilde A, et al. Diagnosis of respiratory syncytial virus in adults substantially increases when adding Sputum, Saliva, and Serology Testing to nasopharyngeal Swab RT–PCR. Infect Dis Ther. 2023;12(6):1593–603. 10.1007/s40121-023-00805-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kingwell K. RSV vaccines score landmark FDA approvals. Nat Rev Drug Discov. 2023;22(7):523–5. 10.1038/d41573-023-00085-x. [DOI] [PubMed] [Google Scholar]
- 13.Falsey AR, Walsh EE, House S, et al. Risk factors and medical resource utilization of respiratory Syncytial Virus, Human Metapneumovirus, and influenza-related hospitalizations in Adults—A Global Study during the 2017–2019 Epidemic Seasons (hospitalized Acute Respiratory Tract infection [HARTI] Study). Open Forum Infect Dis. 2021;8(11). 10.1093/OFID/OFAB491. [DOI] [PMC free article] [PubMed]
- 14.Ackerson B, Tseng HF, Sy LS, et al. Severe morbidity and mortality Associated with respiratory Syncytial Virus Versus Influenza infection in hospitalized older adults. Clin Infect Dis. 2019;69(2):197–203. 10.1093/CID/CIY991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pastula ST, Hackett J, Coalson J, et al. Hospitalizations for respiratory syncytial virus among adults in the United States, 1997–2012. Open Forum Infect Dis. 2017;4(1). 10.1093/ofid/ofw270. [DOI] [PMC free article] [PubMed]
- 16.Falsey AR, Walsh EE, Osborne RH, et al. Comparative assessment of reported symptoms of influenza, respiratory syncytial virus, and human metapneumovirus infection during hospitalization and post-discharge assessed by respiratory intensity and impact questionnaire. Influenza Other Respir Viruses. 2022;16(1):79–89. 10.1111/irv.12903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Atamna A, Babich T, Froimovici D, et al. Morbidity and mortality of respiratory syncytial virus infection in hospitalized adults: comparison with seasonal influenza. Int J Infect Dis. 2021;103:489–93. 10.1016/J.IJID.2020.11.185. [DOI] [PubMed] [Google Scholar]
- 18.Lee N, Lui GCY, Wong KT, et al. High morbidity and mortality in adults hospitalized for respiratory Syncytial Virus infections. Clin Infect Dis. 2013;57(8):1069–77. 10.1093/cid/cit471. [DOI] [PubMed] [Google Scholar]
- 19.Hartnett J, Donga P, Ispas G, et al. Risk factors and medical resource utilization in US adults hospitalized with influenza or respiratory syncytial virus in the hospitalized Acute respiratory tract infection study. Influenza Other Respir Viruses. 2022;16(5):906–15. 10.1111/irv.12994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. Prevention Works: CDC Strategies for a Heart-Healthy and Stroke-Free America. https://www.cdc.gov/dhdsp/docs/Prevention_works.pdf
- 21.Centers for Disease Control and Prevention. Heart Disease and Stroke. Published July 8. 2022. Accessed August 22, 2023. https://www.cdc.gov/chronicdisease/resources/publications/factsheets/heart-disease-stroke.htm#:~:text=Leading%20risk%20factors%20for%20heart,unhealthy%20diet%2C%20and%20physical%20inactivity
- 22.McCarthy CP, Murphy S, Rehman S, et al. Home-time after discharge among patients with type 2 myocardial infarction. J Am Heart Assoc. 2020;9(10). 10.1161/JAHA.119.015978. [DOI] [PMC free article] [PubMed]
- 23.Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-Day readmissions after hospitalization for heart failure, Acute Myocardial Infarction, or Pneumonia. JAMA. 2013;309(4):355. 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Olson-Mack L, Rockwell JM, Lugo S, Brandstein K, Calara R. Abstract TP28: Stroke Care doesn’t end at Hospital Discharge: what patients need after Hospital Discharge May not always be obvious. Stroke. 2022;53(Suppl1). 10.1161/str.53.suppl_1.TP28.
- 25.PINC AI™ Applied Sciences PInc. PINC AITM Healthcare Database: Data That Informs and Performs (White Paper). 2023. https://offers.pinc-ai.com/PINC-AI-Healthcare-Database-White-Paper-LP.html
- 26.Rosenthal N, Cao Z, Gundrum J, Sianis J, Safo S. Risk factors Associated with In-Hospital mortality in a US National Sample of patients with COVID-19. JAMA Netw Open. 2020;3(12):e2029058. 10.1001/jamanetworkopen.2020.29058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fusco M, Di, Shea KM, Lin J, et al. Health outcomes and economic burden of hospitalized COVID-19 patients in the United States. J Med Econ. 2021;24(1):308–17. 10.1080/13696998.2021.1886109. [DOI] [PubMed] [Google Scholar]
- 28.Jones CD, Bowles KH. Emerging Challenges and Opportunities for Home Health Care in the time of COVID-19. J Am Med Dir Assoc. 2020;21(11):1517–8. 10.1016/j.jamda.2020.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shang J, Chastain AM, Perera UGE, et al. COVID-19 preparedness in US Home Health Care Agencies. J Am Med Dir Assoc. 2020;21(7):924–7. 10.1016/j.jamda.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grohskopf LA, Alyanak E, Broder KR, Walter EB, Fry AM, Jernigan DB. Prevention and Control of Seasonal Influenza with vaccines: recommendations of the Advisory Committee on Immunization practices — United States, 2019–20 influenza season. MMWR Recommendations Rep. 2019;68(3):1–21. 10.15585/mmwr.rr6803a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Melgar M, Britton A, Roper LE, et al. Use of Respiratory Syncytial Virus vaccines in older adults: recommendations of the Advisory Committee on Immunization practices — United States, 2023. MMWR Morb Mortal Wkly Rep. 2023;72(29):793–801. 10.15585/mmwr.mm7229a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.RSV Res & National Center for Immunization & Respiratory Diseases, Surveillance. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2022-10-19-20/04-RSV-Adults-Melgar-508.pdf
- 33.Branche AR, Falsey AR. Respiratory syncytial virus infection in older adults: an under-recognized Problem. Drugs Aging. 2015;32(4):261–9. 10.1007/s40266-015-0258-9. [DOI] [PubMed] [Google Scholar]
- 34.Walsh E, Lee N, Sander I, et al. RSV-associated hospitalization in adults in the USA: a retrospective chart review investigating burden, management strategies, and outcomes. Health Sci Rep. 2022;5(3). 10.1002/hsr2.556. [DOI] [PMC free article] [PubMed]
- 35.Branche AR, Saiman L, Walsh EE, et al. Change in functional status associated with respiratory syncytial virus infection in hospitalized older adults. Influenza Other Respir Viruses. 2022;16(6):1151–60. 10.1111/irv.13043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Begley KM, Monto AS, Lamerato LE et al. Comparisons of Respiratory Syncytial Virus (RSV) and Influenza: Population Characteristics and Clinical Outcomes in Hospitalized Adults. medRXiv. Published online 2022:2011–2022.
- 37.Centers for Disease Control and Prevention. Historical Reference of Seasonal Influenza Vaccine Doses Distributed. Accessed July 23. 2023. https://www.cdc.gov/flu/prevent/vaccine-supply-historical.htm
- 38.Centers for Disease Control and Prevention. Advisory Committee on Immunization Practices (ACIP). Published June 28, 2024. https://www.cdc.gov/vaccines/acip/recommendations.html
- 39.Centers for Disease Control and Prevention. Healthcare Providers: RSV Vaccination for Adults 60 Years of Age and Over. Published July 2024. Accessed July 19. 2024. https://www.cdc.gov/vaccines/vpd/rsv/hcp/older-adults.html
- 40.Mechanic OJ, Gavin M, Grossman SA. Acute Myocardial Infarction.; 2023. Accessed September 27, 2023. https://www.ncbi.nlm.nih.gov/books/NBK459269/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The proprietary data supporting the results of this study is owned by PINC AI™ Applied Sciences but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Interested researchers may contact solutioncenter@premierinc.com for data access requests.