Abstract
Background
A robotic arm-assisted and a computed tomography (CT)- based navigation system have been reported to improve the accuracy of component positioning in total hip arthroplasty (THA). However, no study has compared robotic arm-assisted THA (rTHA) to CT-based navigated THA (nTHA) concerning accuracy of cup placement and acetabular fractures using the direct anterior approach (DAA). This study aimed to compare the accuracy of cup placement and the presence of intraoperative acetabular fractures between rTHA and nTHA using DAA in the supine position.
Methods
We retrospectively investigated 209 hips of 188 patients who underwent rTHA or nTHA using DAA (rTHA using the Mako system: 85 hips of 79 patients; nTHA: 124 hips of 109 patients). After propensity score matching for age and sex, each group consisted of 73 hips. We evaluated clinical and radiographic outcomes, comparing postoperative cup orientation and position, measured using a three-dimensional templating software, to preoperative CT planning. Additionally, we investigated the prevalence of occult acetabular fracture.
Results
Clinical outcomes were not significantly different between the groups at 1 year postoperatively. The mean absolute error of cup orientation was significantly smaller in the rTHA group than in nTHA (inclination: 1.4° ± 1.2° vs. 2.7° ± 2.2°, respectively; p = 0.0001, anteversion: 1.5° ± 1.3° vs. 2.2° ± 1.7°, respectively; p = 0.007). The cases within an absolute error of 5 degrees in both RI and RA were significantly higher in the rTHA (97.3%) than in nTHA group (82.2%) (p = 0.003). The absolute error of the cup position was not significantly different between the two groups. The prevalence of occult acetabular fracture did not differ significantly between the two groups (rTHA: n = 0 [0%] vs. nTHA: n = 1 [1.4%]).
Conclusion
Cup placement using DAA in the supine position in rTHA was more accurate with fewer outliers compared to nTHA. Therefore, rTHA performed via DAA in a supine position would be useful for accurate cup placement.
Keywords: Total hip arthroplasty; Direct anterior approach; Robotic surgical procedures, Surgical navigation systems, computer-assisted surgery
Introduction
Primary total hip arthroplasty (THA) is a useful surgery with long term results for reducing pain and improving hip function [1]. However, complications such as dislocation, implant impingement, periprosthetic fracture, and infection, can occur [2, 3]. In particular, dislocation is one of the main reasons for revision THA [2]. Mispositioning of the acetabular cup is one risk factor for dislocation [4, 5]; therefore, optimal and accurate cup placement is essential for preventing implant impingement during THA.
Technologies such as robotic-assisted surgery, computed tomography (CT)-based navigation, imageless navigation, and accelerometer navigation have been reported to increase the accuracy and precision of acetabular cup placement [6–10]. In particular, robotic arm-assisted THA with the Mako system (Mako; Stryker, Kalamazoo, MI, USA) and CT-based navigation systems are capable of creating patient-specific models from preoperative CT images and can adjust the cup orientation and position during surgery [11]. Thus, both technologies enable the reproduction of preoperative plans for cup orientation and positioning [6, 12–14]. The Mako system is comprised of a CT-based navigation system and a robotic arm with haptic control of the instruments. Previous reports have shown that robotic arm-assisted THA achieved more accurate cup placement than THA using manual guidance and fluoroscopy [13–16]. However, only a few reports have compared robotic arm-assisted surgery with CT-based navigated THA in terms of cup placement [6, 17, 18]. According to clinical outcomes, previous reports have compared robotic arm-assisted surgery with manual or portable navigation; however, to the best of our knowledge, no studies have compared it with CT-based navigated THA [19, 20]. Moreover, in previous studies, differences in the surgical approach affected cup orientation with and without the Mako systems [21, 22]. To our knowledge, no reports have compared robotic arm-assisted THA (rTHA) to CT-based navigated THA (nTHA) using the direct anterior approach (DAA) in the supine position.
Recently, the press-fit technique for cementless cups has become a popular fixation technique [23]. Hasegawa et al. showed the prevalence rate of periprosthetic occult fractures of the acetabulum, which were not found on routine postoperative radiographs, to be 8.4% [24]. Intraoperative acetabular fractures most frequently occur during insertion of the acetabular component [25, 26]. In the rTHA, the surgeon can confirm the cup’s center of rotation (COR) on display during cup insertion. In contrast, in the nTHA, the surgeon can confirm the cup position with respect to final reamer position during cup insertion. Because the surgeon can confirm whether the component reaches the target position, the surgeon might avoid further cup impaction after full cup seating. It may lead to reduce fracture risk. To our knowledge, no reports compared the prevalence rates of occult fractures between rTHA and nTHA using DAA.
We hypothesized that rTHA would offer better cup placement accuracy than nTHA and have similar short-term clinical outcomes. This study aimed to clarify the accuracy of cup orientation and positioning and to compare the prevalence rates of occult acetabular fractures between the rTHA and nTHA groups with matched patient background analysis.
Methods
Patients
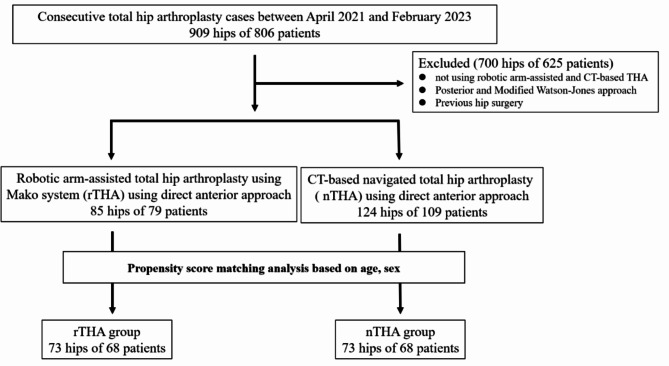
Between April 2021 and February 2023, we examined 909 hips of 806 consecutive THA patients. Inclusion criteria were: (1) males and females, (2) age 18–90 years, (3) undergoing elective primary hip arthroplasty using rTHA or nTHA. Exclusion criteria were: (1) not using robotic arm-assisted and CT-based navigation, (2) posterior and modified Watson-Jones approach, (3) previous hip surgery. Based on these criteria, we assessed 85 hips of 79 patients who underwent rTHA using the Mako system (Stryker Kalamazoo, MI, USA) and 124 hips of 109 patients who underwent nTHA using a CT-based navigation system (Stryker CT-Hip system Ver1.3; Stryker Kalamazoo, MI, USA). This study was approved by our institutional review board (H2020-068). All patients provided informed consent. Propensity score matching was used to match the patients’ backgrounds for sex and age between the two groups using the JMP® program (version 16.0; SAS Institute Inc., Cary, NC, USA). Finally, 73 hips from each group were included in this study (Fig. 1). One facility performed rTHA and the other nTHA. The surgeons overlapped in both groups. Regarding patient demographics, no significant differences were found between the two groups (Table 1).
Fig. 1.
Patient demographic flow chart
Table 1.
Patients’ demographics
| rTHA (n = 73 hips) | nTHA (n = 73 hips) | p-value | |
|---|---|---|---|
| Number of patients | 68 | 68 | |
| Sex (patient) | 0.48 | ||
| male | 10 | 9 | |
| female | 58 | 59 | |
| Age (years) | 69.3 ± 8.8 | 69.2 ± 8.6 | 0.98 |
| BMI (kg/m2) | 24.2 ± 4.4 | 25.4 ± 4.7 | 0.094 |
| Diagnosis (hip) | 0.25 | ||
| DDH | 39 | 32 | |
| OA | 24 | 27 | |
| ONFH | 6 | 7 | |
| RDC | 4 | 2 | |
| SIF | 0 | 4 | |
| RA | 0 | 1 | |
| Cup size (hip) (mm) | 0.17 | ||
| 44 mm | 0 | 2 | |
| 46 mm | 6 | 6 | |
| 48 mm | 21 | 36 | |
| 50 mm | 24 | 13 | |
| 52 mm | 10 | 6 | |
| 54 mm | 7 | 6 | |
| 56 mm | 4 | 3 | |
| 58 mm | 1 | 1 |
Values are expressed as means ± standard deviation or as numbers (n). p-values in bold indicate statistical significance (p < 0.05)
rTHA Robotic arm-assisted total hip arthroplasty, nTHA Navigated total hip arthroplasty using computed tomography-based navigation system, BMI Body mass index, DDH Developmental dysplasia of the hip, OA Osteoarthritis; ONFH Osteonecrosis of the femoral head, RDC Rapidly destructive coxarthropathy, SIF, Subchondral insufficient fracture of the femoral head, RA Rheumatoid arthritis
Preoperative planning
All preoperative plans were made using CT-based simulation software ZedHip (LEXI, Tokyo, Japan) based on preoperative CT images obtained with a helical CT scanner (Aquilion Precision System, Toshiba Medical System, Tokyo, Japan) (SOMATOM go, Siemens Healthcare, Erlangen, Germany). The slice thickness and pitch were 1 mm in both groups. The functional pelvic plane (FPP) was used to plan the cup orientation. The target cup orientation basically aimed for a radiographic inclination (RI) of 40° and radiographic anteversion (RA) of 15°. The RA target was set in consideration of the risk of iliopsoas impingement caused by anterior cup edge overhang. Subsequently, the preoperative plans made by ZedHip were traced to each software in either the Mako system or CT-based navigation system.
Surgical technique
All surgeries were performed using DAA in the supine position on a normal operating table under general anesthesia. The skin incision was made 1 cm distal and lateral to the anterior superior iliac spine, parallel to the tensor fasciae latae. Dissection through the interval between tensor fasciae latae and sartorius muscles was performed. We incised the anterior capsule as a triangular flap, based on the femoral attachment, along the side of the vertical band of the iliofemoral ligament [27]. After anterior capsulotomy, femoral neck osteotomy was performed following preoperative planning. After implantation, the capsule was repaired. One team performed all surgeries under the supervision of two senior hip arthroplasty surgeons with > 20 years of experience (I.T. and T.H.). All hips were implanted with cementless hemispherical cups. The acetabular component was placed using press-fit fixation. Screw fixation for cup implantation was performed when the surgeon deemed it necessary.
rTHA
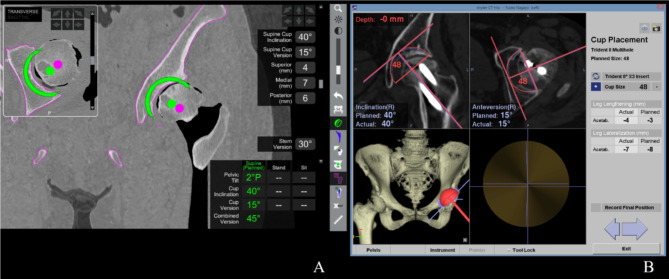
In the rTHA group, three pins (4-mm diameter) were inserted at the contralateral side of the iliac crest to attach to the pelvic array. The surface registration area were the external iliac plate, anterior periarticular area within 5 cm of the acetabular rim, and intra-acetabular region. After pelvic registration, the acetabulum was prepared with a planned reamer using a robotic arm. Acetabular cup implantation was based on the orientation and positioning indicated by the software, which was displayed as the real-time error of inclination, anteversion, and COR (Fig. 2A). All acetabular cups were Trident HA hemispherical cup (Stryker, Kalamazoo, MI, USA).
Fig. 2.
Acetabular component orientation and positioning (A) Robotic arm-assisted system and (B) CT-based navigation system
nTHA
In the nTHA group, two pins (5-mm diameter) were inserted at the contralateral side of the iliac crest to attach to the pelvic array. The surface registration area was an external iliac plate and anterior periarticular area within 5 cm of the acetabular rim. An acceptable range for the surface match registration accuracy was 1 mm. The acetabulum was reamed using real-time errors of inclination and anteversion. Finally, the cup was implanted in accordance with inclination, anteversion, and COR (Fig. 2B). The acetabular components were PINNACLE (DePuy Synthes, Warsaw, IN, USA) in 38 hips, Trident II Tritanium (Stryker) in 26 hips, Trident HA hemispherical (Stryker) in 5 hips, and Anasta cup (Teijin Nakashima Medical, Okayama, Japan) in 4 hips.
Evaluations
Clinical outcomes were assessed using the following measures: pre- and postoperative Japanese Orthopedic Association (JOA) scores as physician-reported outcomes, the Japanese Orthopedic Association Hip Disease Evaluation Questionnaire (JHEQ) score, and the postoperative Forgotten Joint Score-12 (FJS-12) as a patient-reported outcome (PROMs) [28–30]. JOA scores ranged from 0 (worst) to 100 (best) and JHEQ scores ranged from 0 (worst) to 84 (best). Additionally, we examined the operative time, intraoperative blood loss, perioperative complications, and complications up to 1 year postoperatively.
Radiographic outcomes were assessed cup orientation and positioning. We routinely obtained CT images at two weeks postoperatively to assess for complications such as occult fractures. The data were uploaded to the three-dimensional templating software, ZedHip. The ZedHip automatically matched the preoperative and postoperative FPP and differences between the pre-and postoperative orientation and cup center position were measured.
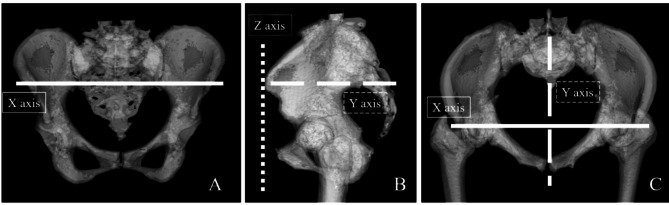
The absolute error of the cup orientation (RI and RA) between preoperative planning and postoperative CT measurements were investigated. Each value was compared between the two groups. We assessed outliers of RI and RA that were > 5 degrees. Additionally, cup orientation with and without screws in rTHA and nTHA were assessed. The absolute error of the COR between the preoperative planning and postoperative CT measurements were also investigated. The COR was defined by the coordinates on the x-, y-, and z-axes using ZedHip. The x-axis (horizontal axis) is the line connecting the bilateral anterior superior iliac spines. The z-axis (vertical axis) was vertical to the x-axis, parallel to the FPP, and through the pubic tubercle. The y-axis (sagittal axis) was perpendicular to the x- and z-axes (Fig. 3). Each value was compared between the two groups. Additionally, we examined the cup orientation and positioning based on BMI categories (below 25, 25 to 30, and above 30), Kellgren-Lawrence grade (KL grade) of osteoarthritis, and the presence or absence of screw insertion within each group. The prevalence rates of acetabulum occult fracture using postoperative CT images were compared between the two groups.
Fig. 3.
Cup position is defined in three-dimensional space with the X-axis, Y-axis, and Z- axis. The straight line indicates the X-axis (A). The X-axis (horizontal axis) is the line connecting the bilateral anterior superior iliac spines. A straight line with short dots represents the Z-axis (B). The Z-axis (vertical axis) was vertical to the X-axis. A straight line with long dots represents the Y-axis (B, C). The Y-axis (sagittal axis) was perpendicular to the X- and Z-axis
Statistical analysis
Continuous variable data are presented as the mean ± standard deviation. We used non-parametric tests because the distributions of the preoperative JOA and JHEQ score significantly deviated from normality. Continuous and categorized data were analyzed using the Mann–Whitney U and chi-squared tests, respectively. All statistical analyses were performed using JMP version 16. Differences were considered statistically significant at a p-value of 0.05. A power analysis using G*power (3.1; Düsseldorf, Germany) indicated that the sample size of this study (effect size f, 0.50; alpha error probability, 0.05; power, 0.90) was 70 hips. Thus, 73 hips in each group would be sufficient to detect statistically significant differences.
Results
Clinical outcomes
There were no significant differences in the pre- and postoperative JOA scores, JHEQ scores, and FJS-12 between the two groups (Table 2). Surgical time and blood loss were not significantly different between the two groups (surgical time: rTHA 107.7 ± 25.4 min, nTHA 110.6 ± 24.7 min, p = 0.34; blood loss: rTHA 281.6 ± 182.3 ml, nTHA 326.6 ± 2 10.1 ml, p = 0.12). No cup-related complications occurred in either group. Perioperatively, one case of periprosthetic fracture around the femoral stem was observed in the rTHA group, and two cases of superficial infection were observed in the nTHA group. No complications were observed in either group for up to 1 year postoperatively.
Table 2.
Comparison of clinical outcomes between the two groups
| Clinical outcomes | rTHA | nTHA | p-value |
|---|---|---|---|
| Preoperative | |||
| JOA score | 46.8 ± 12.4 | 48.6 ± 11.6 | 0.12 |
| JHEQ score | 22.2 ± 11.8 | 18.1 ± 13.1 | 0.064 |
| Postoperative | |||
| JOA score | 87.9 ± 8.9 | 90.8 ± 9.4 | 0.089 |
| JHEQ score | 59.4 ± 14.2 | 61.9 ± 16.5 | 0.26 |
| FJS-12 | 71.5 ± 20.9 | 68.7 ± 23.2 | 0.70 |
Values are expressed as mean ± standard deviation. P-values in bold indicate statistical significance (p < 0.05)
rTHA Robotic arm-assisted total hip arthroplasty, nTHA Navigated total hip arthroplasty using CT-based navigation system, JOA score Japanese Orthopaedic Association score, JHEQ Japanese Orthopaedic Association Hip-Disease Evaluation Questionnaire, FJS-12 Forgotten joint score-12
Radiographic outcomes
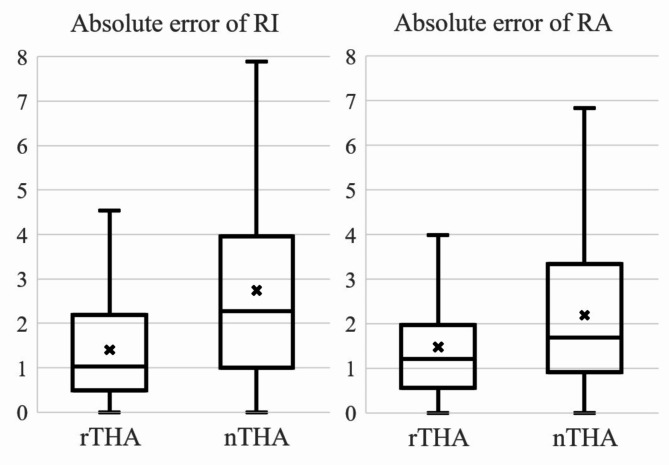
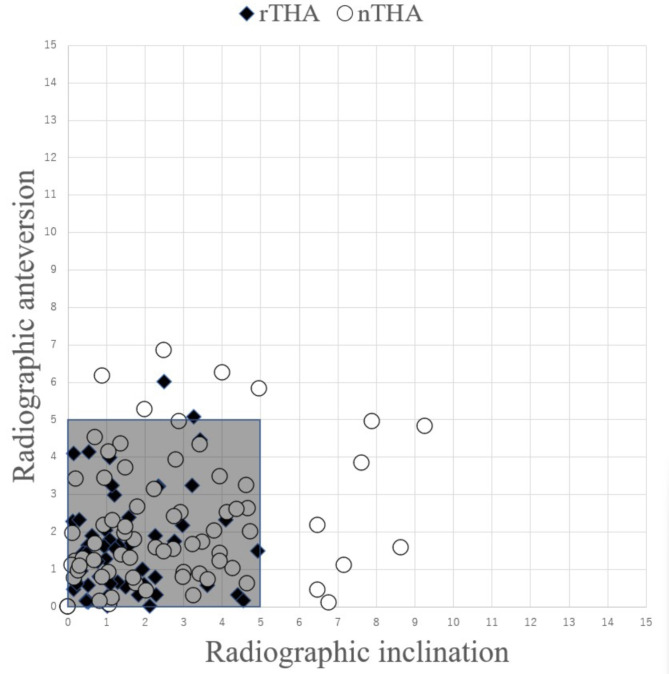
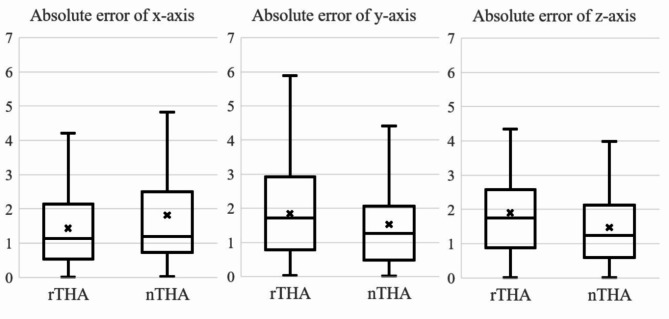
The absolute error of RI in the rTHA group was significantly smaller than that in the nTHA groups (1.4° ± 1.2°, 2.7° ± 2.2°, respectively) (p = 0.0001). Similarly, the absolute error of RA in the rTHA group was smaller than that in the nTHA group (1.5 °± 1.3°, 2.2° ± 1.7°, respectively) (p = 0.007) (Fig. 4). Scatter plot of the absolute error of RI and RA are shown in Fig. 5. The rates of placement within 5 degrees were 97.3% (71 hips) in the rTHA group and 82.2% (60 hips) in nTHA; there was significant difference between the two groups (p = 0.002). In the rTHA group, the absolute errors of RI were 1.4° ± 0.6° with screw (n = 4) and 1.4° ± 1.2° without screw (n = 69) and 1.0° ± 1.5° with screw and 1.5° ± 1.3° without screw in the absolute errors of RA. In the nTHA group, the absolute errors of RI were 2.2° ± 2.0° with screw (n = 22) and 2.9° ± 2.3° without screw (n = 51) and 1.8° ± 1.6° with screw and 2.3° ± 1.7° without screw in the absolute errors of RA. Statistical analysis was not performed due to the small number of cases, but results were similar in both groups for the presence or absence of screws. The mean absolute errors of the x-, y-, and z-axes were 1.4 ± 1.2 mm, 1.8 ± 1.3 mm, and 1.8 ± 1.2 mm in the rTHA group, respectively, and 1.8 ± 1.6 mm, 1.5 ± 1.3 mm, and 1.5 ± 1.2 mm in the nTHA group, respectively. There was no significant difference between two groups (Fig. 6).
Fig. 4.
The absolute error of radiographic inclination and anteversion between two groups
Fig. 5.
Scattergram of postoperative cup orientation plots with the absolute error of inclination and anteversion in the rTHA and nTHA groups
Fig. 6.
The absolute error of cup center position (x-, y-, and z-axes) in the rTHA and the nTHA groups
There was no statistically significant difference in cup orientation or position between groups based on KL grade and the presence/absence of screw insertion (Tables 3 and 4). Regarding BMI, there was no significant difference in cup orientation. Additionally, higher BMI was not associated with greater deviation in cup placement (Table 5).
Table 3.
Comparison of cup orientation and position according to KL grade variations between the two groups
| rTHA | nTHA | |||||
|---|---|---|---|---|---|---|
| KL grade 3 (n = 9) |
KL grade 4 (n = 53) |
p-value | KL grade 3 (n = 8) | KL grade 4 (n = 52) |
p-value | |
| RI (°) | 0.9° ± 0.9° | 1.6° ± 1.3° | 0.22 | 2.9° ± 1.8° | 2.7° ± 2.0° | 0.95 |
| RA (°) | 1.8° ± 2.0° | 1.5° ± 1.2° | 0.94 | 2.7° ± 1.5° | 2.1° ± 1.7° | 0.12 |
| X axis (horizontal) (mm) | 1.1 ± 1.3 | 1.5 ± 1.2 | 0.47 | 1.5 ± 1.2 | 1.8 ± 1.7 | 0.97 |
| Y axis (sagittal) (mm) | 2.0 ± 1.6 | 1.8 ± 1.2 | 0.99 | 1.2 ± 1.1 | 1.7 ± 1.3 | 0.71 |
| Z axis (vertical) (mm) | 1.4 ± 1.2 | 2.0 ± 1.3 | 0.25 | 1.5 ± 0.9 | 1.5 ± 1.1 | 0.82 |
rTHA Robotic arm-assisted total hip arthroplasty, nTHA Navigated total hip arthroplasty using CT-based navigation system, KL Kellgren-Lawrence classification, RI Radiographic inclination, RA Radiographic anteversion
Table 4.
Comparison of the cup orientation and position with and without screws between the two groups
| rTHA | nTHA | |||||
|---|---|---|---|---|---|---|
| with screw (n = 4) |
without screw (n = 69) |
p-value | with screw (n = 22) |
without screw (n = 51) |
p-value | |
| RI (°) | 1.4° ± 0.6° | 1.4° ± 1.2° | 0.91 | 2.2° ± 2.0° | 2.9° ± 2.3° | 0.49 |
| RA (°) | 1.0° ± 1.5° | 1.5° ± 1.3° | 0.67 | 1.8° ± 1.6° | 2.3° ± 1.7° | 0.54 |
| X axis (horizontal) (mm) | 2.5 ± 1.9 | 1.4 ± 1.1 | 0.56 | 2.2 ± 2.1 | 1.5 ± 1.3 | 0.69 |
| Y axis (sagittal) (mm) | 1.4 ± 1.4 | 1.9 ± 1.3 | 0.95 | 1.3 ± 1.2 | 1.6 ± 1.3 | 0.62 |
| Z axis (vertical) (mm) | 1.5 ± 1.3 | 1.9 ± 1.3 | 0.52 | 1.2 ± 1.1 | 1.6 ± 1.2 | 0.20 |
rTHA Robotic arm-assisted total hip arthroplasty, nTHA Navigated total hip arthroplasty using CT-based navigation system, RI Radiographic inclination, RA Radiographic anteversion
Table 5.
Comparison of cup orientation and position according to BMI in each group
| BMI | rTHA | nTHA | ||||||
|---|---|---|---|---|---|---|---|---|
| BMI < 25 (n = 49) |
25 ≤ BMI ≤ 30 (n = 18) |
30 < BMI (n = 6) |
p-value | BMI < 25 (n = 39) |
25 ≤ BMI ≤ 30 (n = 22) |
30 < BMI (n = 12) |
p-value | |
| RI (°) | 1.4° ± 1.2° | 1.7° ± 1.4° | 0.7° ± 0.7° | 0.14 | 2.7° ± 2.1° | 2.8° ± 2.4° | 2.8° ± 2.6° | 0.99 |
| RA (°) | 1.6° ± 1.4° | 1.5° ± 1.1° | 1.0° ± 0.6° | 0.81 | 2.3° ± 1.9° | 1.7° ± 1.1° | 2.7° ± 1.7° | 0.30 |
| X axis (horizontal) (mm) | 1.1 ± 0.9 | 2.3 ± 1.4 | 1.6 ± 1.6 | 0.020 | 1.7 ± 1.8 | 2.0 ± 1.5 | 1.9 ± 1.3 | 0.46 |
| Y axis (sagittal) (mm) | 1.9 ± 1.4 | 1.7 ± 1.1 | 1.8 ± 1.4 | 0.86 | 1.3 ± 1.2 | 1.8 ± 1.4 | 1.9 ± 1.3 | 0.13 |
| Z axis (vertical) (mm) | 1.9 ± 1.2 | 2.1 ± 1.7 | 1.4 ± 1.1 | 0.49 | 1.3 ± 1.1 | 1.7 ± 1.2 | 1.5 ± 1.3 | 0.28 |
Values are expressed as mean ± standard deviation. P-values in bold indicate statistical significance (p < 0.05)
BMI Body mass index, THA Total hip arthroplasty, CT Computed tomography, RI Radiographic inclination, RA Radiographic anteversion, rTHA Robotic arm-assisted total hip arthroplasty, nTHA Navigated total hip arthroplasty using CT-based navigation system,
There were no acetabular fractures intraoperatively in either group. No cases of occult fracture of the acetabulum occurred in the rTHA group and one case of occult fracture was found in the nTHA group. There was no significant difference between the two groups. In case of occult fracture, additional treatment and limited weight-bearing were unnecessary.
Discussion
The rTHA group was more accurate for cup orientation in both RI and RA than the nTHA group using DAA in the supine position. The number of cases within 5 degrees of the absolute error for both RI and RA were significantly greater in the rTHA group than nTHA. There were no significant differences in the clinical outcomes, cup position, and the prevalence rate of occult fracture between the two groups. This study is the first report to show the differences in cup placement between rTHA and nTHA using DAA in the supine position. In this study, the absolute errors of RI and RA were significantly smaller in the rTHA group than in the nTHA group. Additionally, the rates of outlier cup placement were significantly smaller in the rTHA group than in nTHA.Although some reports assessed cup orientation using robotic arm-assisted THA, there have been no reports accurately evaluating the use of CT after rTHA through DAA in the supine position (Table 6) [6, 12–14, 16–18, 31–33]. Moreover, no reports have compared rTHA to nTHA using DAA cup orientation (Table 7) [6, 17, 18]. We consider the reasons for this difference between the two groups, such as the number of pins for connecting the tracker to pelvis, surface registration area, and use of a hand-held or robotic arm. First, tracker stability can affect surgical accuracy. In the external fixation of the pelvis for pelvic fracture, the number and diameter of pins have been reported to affect frame rigidity [34]. Thus, the tracker stability was also considered to depend on the number and diameter of pins. The rTHA group had three pins (4-mm diameter) compared to two pins (5-mm diameter) in the nTHA group. The rTHA group had more pin insertions, however, they were of a smaller diameter than those used in the nTHA group. Direct comparison between the two groups is difficult because the number of pins and diameters are different in the two groups, however, there were no cases of obvious intraoperative pin loosening in both groups. Second, the surface registration areas for rTHA and nTHA were different in this study. In the rTHA group, the registration areas were the external iliac plate and anterior periarticular area within 5 cm of the acetabular rim, and the intra-acetabular region following the instruction of the Mako system. In contrast, only the external iliac plate and anterior periarticular area within 5 cm of the acetabular rim were used as the registration areas in the nTHA group, according to a previous report [35]. Docquier et al. showed that a larger sampling area increased registration accuracy [36]. Thus, registration area differences may affect registration accuracy, which may affect cup orientation. Third, In the nTHA group, the surgeon determined the reaming direction using a handheld reamer [6]. In contrast, in the rTHA group, the haptic arm placed the reamer within 15° of the cup placement target from center. Previous reports have shown that RI decreases while RA increases in the nTHA group preoperative plan because of the difference in interface stress between the craniomedial and inferior portion in the acetabulum [37, 38]. In the rTHA, the robot haptic arm guides the cup holder to the target cup orientation; however, in the nTHA group, cup placement is performed handheld. Therefore, in nTHA, surgeons need to control the cup orientation by the surgeon himself. In rTHA, the surgeon does not need to control the cup orientation. The use of haptic arm is an advantage of rTHA in preventing cup malalignment.
Table 6.
The accuracy of robotic arm-assisted THA in various surgical approaches
| Author | Approach | Number of hips | Assessment modality | RI | RA | Target angle | |
|---|---|---|---|---|---|---|---|
| RI | RA | ||||||
| Shaw et al. [12] | PL | 141 | radiograph | 42.5 ± 5.3 | 25.6 ± 5.4 | NA | 22–25 |
| Guo et al. [14] | PL | 45 | CT | 41.5 ± 4.2 | 21.1 ± 5.7 | 40 | 20 |
| Kamara et al. [16] | PL | 98 | radiograph | 40.5 ± 3.7 | 19.4 ± 4.4 | 40 | 20 |
| Shibanuma et al. [17] | PL | 30 | radiograph | 42.2 ± 2.2 | 20.3 ± 1.6 | 40 | 20 |
| Redmond et al. [31] | PL | 35 | radiograph | 39.9 ± 2.5 | 17.4 ± 3.4 | 40 | 20 |
| Kanawade et al. [32] | PL | 43 | CT | 39.1 ± 3.8 | 18.9 ± 4.1 | 40 | 20 |
| Ando et al. [6] | PL/mWJ | 27/2 | CT | 2.0 ± 1.4* | 1.9 ± 1.4* | 40 | 15 |
| Sato et al. [33] | mWJ | 84 | CT | 1.1 ± 1.0* | 1.2 ± 1.1* | 40 | -† |
| Tamaki et al. [18] | ALS | 52 | CT | 1.1 ± 0.9* | 1.3 ± 1.0* | 38.8 ± 1.5 | 15.8 ± 1.7 |
| Domb et al. [13] | PL/DAA | 52/14 | radiograph | 40.9 ± 3.2 | 18.4 ± 3.7 | 40 | 20 |
| Our study | DAA | 73 | CT | 1.4 ± 1.2* | 1.5 ± 1.3* | 40 | 15 or 20 |
Values are expressed as mean ± standard deviation
* Absolute error of the cup angle between the preoperative and postoperative measurement
† The cup anteversion angle was fine-tuned for each patient
Abbreviations: RI, Radiographic inclination; RA, Radiographic anteversion; PL, Posterolateral approach; NA, Not available; CT, Computed tomography; mWJ, Modified Watson-Jones approach; ALS, Anterolateral approach in the supine position; DAA, Direct anterior approach
Table 7.
Direct comparison of radiographic inclination and anteversion between robotic arm-assisted THA and CT navigated THA
| Author | Approach | Each number of hips | Assessment modality | RI | RA | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| rTHA | nTHA | Target angle (rTHA/nTHA) |
p-value | rTHA | nTHA | Target angle (rTHA/nTHA) |
p-value | ||||
| Ando et al. [6] | PL/mWJ | 27/2 | CT | 2.0 ± 1.4* | 3.5 ± 2.4* | 40/40 | 0.007 | 1.9 ± 1.4* | 2.8 ± 2.3* | 15/15 | 0.108 |
| Shibanuma et al. [17] | PL | 30 | radiograph | 42.2 ± 2.2 | 40.5 ± 4.5 | 40/40 | 0.07 | 20.3 ± 1.6 | 19.9 ± 3.6 | 20/20 | 0.11 |
| Tamaki et al. [18] | ALS | 52 | CT | 1.1 ± 0.9* | 2.2 ± 1.5* | 38.8/38.4 | < 0.01 | 1.3 ± 1.0* | 3.3 ± 2.5* | 15.8/12.0 | < 0.01 |
| Our study | DAA | 73 | CT | 1.4 ± 1.2* | 2.7 ± 2.2* | 40/40 | 0.0001 | 1.5 ± 1.3* | 2.2 ± 1.7* | 15 or 20/15 or 20 | 0.007 |
Values are expressed as mean ± standard deviation. P-values in bold indicate statistical significance (p < 0.05)
*Absolute error of the cup angle between the preoperative and postoperative measurement is indicated
THA Total hip arthroplasty, CT Computed tomography, RI Radiographic inclination, RA Radiographic anteversion, rTHA Robotic arm-assisted total hip arthroplasty, nTHA Navigated total hip arthroplasty using CT-based navigation system, PL Posterolateral approach, mWJ Modified Watson-Jones approach, ALS Anterolateral approach in the supine position, DAA Direct anterior approach
In our study, cup orientation regardless of the presence or absence of screws did not differ significantly between the two groups. Fujishiro et al. showed that the cup orientation could undergo changes during screw fixation [39]. Garcia reported the cases of either the lateralized cup position tended to use the screws [23]. If cup installation could not be done as planned, we considered that surgeons were more likely to perform screw insertion to improve stability. Tabata et al. reported that intraoperative primary cup stability was influenced by the exactness of the reaming procedure and accurate cup insertion [40]. We believe that there was no significant difference in the presence or absence of screws because rTHA and nTHA allows for accurate cup orientation and placement. It should be noted that the number of screw insertion cases in this study was small. A large-scale study will be necessary in the future.
In this study, COR levels were not significantly different between the two groups. No reports have compared the COR of rTHA to nTHA using DAA (Table 8) [6, 8, 18, 33, 41]. Compared to imageless navigation, rTHA and nTHA are both capable of creating a patient-specific model generated from preoperative imaging and intraoperative registration [11]. We considered that both technologies would be useful for the accuracy of cup COR.
Table 8.
Comparison of cup COR between robotic arm-assisted THA and navigated THA using CT-based navigation system
| Author | Approach | Each number of hips | Assessment modality | rTHA | nTHA | ||||
|---|---|---|---|---|---|---|---|---|---|
| X axis (horizontal) (mm) |
Y axis (sagittal) (mm) |
Z axis (vertical) (mm) |
X axis (horizontal) (mm) |
Y axis (sagittal) (mm) |
Z axis (vertical) (mm) |
||||
| Ando et al. [6] | PL/mWJ | 27/2 | CT | 1.6 ± 1.6 | 1.8 ± 1.7* | 2.2 ± 1.4† | 1.9 ± 1.6 | 3.1 ± 2.5* | 3.7 ± 2.5† |
| Tamaki et al. [18] | ALS | 52 | CT | 1.3 ± 1.3 | 1.7 ± 1.5 | 2.0 ± 2.0 | 1.6 ± 1.4 | 1.8 ± 1.3 | 2.6 ± 2.3 |
| Sato et al. [33] | mWJ | 84 | CT | 1.2 ± 0.9 | 1.1 ± 0.9 | 2.0 ± 1.3 | - | - | - |
| Matsuki et al. [8] | DAA | 50 | CT | - | - | - | 2.1 ± 1.7 | 1.7 ± 1.4 | 1.8 ± 1.4 |
| Iwana et al. [41] | PL | 117 | CT | - | - | - | 1.9 ± 1.5 | 1.4 ± 1.2 | 1.9 ± 1.3 |
| Our study | DAA | 73 | CT | 1.4 ± 1.2 | 1.8 ± 1.3 | 1.8 ± 1.2 | 1.8 ± 1.6 | 1.5 ± 1.3 | 1.5 ± 1.2 |
Values are expressed as mean ± standard deviation. Absolute error of the cup center of rotation between the preoperative and postoperative measurement are indicated
Abbreviation: COR, Center of rotation; THA, Total hip arthroplasty; CT, Computed tomography; rTHA, Robotic arm-assisted total hip arthroplasty; nTHA, Navigated total hip arthroplasty using CT-based navigation system; PL, Posterolateral approach; mWJ, Modified Watson-Jones approach; ALS, Anterolateral approach in the supine position; DAA, Direct anterior approach
*Significant difference between the two groups
†Significant difference between the two groups
In the present study, accurate placement of the cup in the supine position was enabled in the rTHA group using DAA. In DAA, previous reports used robotic arm-assisted surgery, navigation systems, and fluoroscopy (Table 9) [7–10, 42–45]. Use of a mechanical alignment guide and fluoroscopy tended to cause large absolute errors in the RA compared to nTHA using DAA [8, 45]. Compared to rTHA and nTHA, imageless navigation requires less equipment, spares exposing the patient to radiation, and removes the expense of preoperative imaging [11]. However, portable navigation cannot assess the cup position during surgery and create patient-specific models; there is also a risk of inaccuracies, such as pelvic deformity.
Table 9.
The accuracy of radiographic inclination and anteversion using DAA
| Author | Approach | Number of hips | Device | Assessment modality | RI | RA | Target angle | |
|---|---|---|---|---|---|---|---|---|
| RI | RA | |||||||
| Kamath et al. [7] | DAA | 33 | CT free robotic assisted (ROSA) | radiograph | 1.8 ± 1.3* | 2.6 ± 2.3* | 40 | 15 |
| Matsuki et al. [8] | DAA | 50 | CT-based navigation (Stryker) | CT | 2.8 ± 2.5* | 2.8 ± 1.9* | 40 | 15 |
| Nogler et al. [42] | DAA | 22 | CT-based navigation (Stryker) | CT | 1.3 (0.6–2.2) * | 2.4 (1.0-3.2) * | 45 | 20 |
| Tsukada et al. [9] | DAA | 69 | Imageless-navigation (OrthoPilot) | CT | 2.8 ± 2.5* | 4.2 ± 3.0* | 45 | 15 |
| Lass et al. [43] | DAA | 65 | Imageless-navigation (Navitrack) | CT | 3.0 ± 2.5* | 5.5 ± 3.6* | 40 | 15 |
| Hasegawa et al. [10] | DAA | 55 | Accelerometer-based navigation (Naviswiss) | CT | 4.1 ± 3.2* | 4.3 ± 3.2* | 40 | 15 |
| Okamoto et al. [44] | DAA | 115 | Accelerometer-based navigation (Hip-align) | CT | 3.1 ± 2.2* | 2.8 ± 2.3* | 40 | 15 or 20 |
| Kolodychuk et al. [45] | DAA | 99 | Accelerometer-based navigation (Hip-align) | radiograph | 1.8 ± 1.6* | 3.2 ± 3.1* | 40 | 15 |
| Our study | DAA | 73 | Robotic arm-assisted (Mako) | CT | 1.4 ± 1.2* | 1.5 ± 1.3* | 40 | 15 or 20 |
Values are expressed as mean ± standard deviation and parentheses indicted interquartile range
* Absolute error of the cup angle between the preoperative and postoperative measurement
DAA Direct anterior approach, RI Radiographic inclination, RA Radiographic anteversion, CT Computed tomography
In this study, we compared rTHA with nTHA, and found no differences in physician- and patient-reported outcomes in the short term. A previous study reported that postoperative FJS score tended to be higher in the rTHA group compared to the manual THA group, while no significant differences were found in other PROMs between the two groups [21]. Zahaf reported that semi-elliptical cracks tend to concentrate stress, which could lead to implant loosening [46]; however, robotic haptic arm by enabling more precise reaming, may reduce this risk and positively impact long-term outcomes. Although there was no significant difference in short-term PROMs, further research on long-term outcomes is necessary.
Our study showed that robotic surgery enabled more accurate cup placement than nTHA. However, not all hospitals can afford robotic systems owing to their high cost. Some studies suggest rTHA is cost-effective, citing reduced use of rehabilitation services [47] and a lower dislocation rate than manual THA [48]. Additionally, previous reports indicate that the COVID-19 pandemic limited surgical experience for orthopedic residents [49], and robotic systems could enhance training by offering more precise surgeries, further highlighting the potential cost-effectiveness of rTHA.
In the present study, occult fractures were detected in one hip in the nTHA group and no hips in the rTHA group. Hasegawa et al. showed that the prevalence rate of occult fractures of the acetabulum was 8.4%, and peripheral self-locking cups may increase this risk [25]. In this study, because only hemispherical cups were used, the acetabular cup design may not have affected these differences. The incidence of occult fracture was no significant difference in the two groups.
This study had limitations. First, the sample size is relatively small; however, it is reasonable to perform statistical analyses because the power analysis determined the sample size to be sufficient. In addition, the patient characteristics were matched using propensity score matching. Second, we did not investigate the clinical outcomes; we compared just acetabular cup orientation and position. Although these differences are statistically significant, it is unclear if there is a clinical difference. However, there is a significant difference in the outliers between the two groups. These differences may affect clinical outcomes. In the future, long-term follow-ups and clinical outcome evaluations will be necessary.
Conclusions
The rTHA group exhibited a greater accuracy in cup orientation and fewer outliers than the nTHA group; however, the COR levels and prevalence of occult fractures were not significantly different between the two groups. The application of DAA rTHA could be useful for achieving more accurate cup placements with fewer outliers.
Acknowledgements
This work was supported by JSPS KAKENHI [Grant Number JP23K10426].
Abbreviations
- THA
Total hip arthroplasty
- rTHA
Robotic arm-assisted total hip arthroplasty
- nTHA
Navigated total hip arthroplasty using computed tomography-based navigation system
- DAA
Direct anterior approach
- PL
Posterolateral
- COR
Center of rotation
- FPP
Functional pelvic plane
- RI
Radiographic inclination
- RA
Radiographic anteversion
Author contributions
All authors have read and approved the manuscript. TO: Conception and design; drafting of the article. TI: Drafting of the article, acquisition and analysis of the data. HT: acquisition and analysis of the data. YM: acquisition of the data. TK: acquisition of the data. TK: acquisition of the data. TK; acquisition of the data. KY; acquisition of the data. TS: conception and design, final approval of the article.
Funding
We received no specific funding from any funding body to conduct this study.
Data availability
Data associated with this study is retained at the Department of Orthopedic surgery, Yamaguchi university graduate school of medicine and Yamaguchi prefectural grand medical center. The datasets generated and/or analyzed in this study are available from the corresponding author on reasonable request. If there are any questions, please contact the corresponding author.
Declarations
Ethics approval and consent to participate
This retrospective, case-control study was approved by the Institutional Review Board of Yamaguchi University Graduate School of Medicine (the ethics committee of Yamaguchi University Graduate School of Medicine, reference number: H2020-068) and all patients provided informed consent. The ethical standards from the 1964 Helsinki declaration and its later amendments were upheld.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.McLaughlin JR, Lee KR. Total hip arthroplasty with an uncemented tapered femoral component. J Bone Joint Surg Am. 2008;90:1290–6. [DOI] [PubMed] [Google Scholar]
- 2.Phillips CB, Barrett JA, Losina E, Mahomed NN, Lingard EA, Guadagnoli E, et al. Incidence rates of dislocation, pulmonary embolism, and deep infection during the first six months after elective total hip replacement. J Bone Joint Surg Am. 2003;85:20–6. [DOI] [PubMed] [Google Scholar]
- 3.Lindahl H, Malchau H, Herberts P, Garellick G. Periprosthetic femoral fractures: classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthroplasty. 2005;20:857–65. [DOI] [PubMed] [Google Scholar]
- 4.Nishii T, Sugano N, Miki H, Koyama T, Takao M, Yoshikawa H. Influence of component positions on dislocation: computed tomographic evaluations in a consecutive series of total hip arthroplasty. J Arthroplasty. 2004;19:162–6. [DOI] [PubMed] [Google Scholar]
- 5.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–20. [PubMed] [Google Scholar]
- 6.Ando W, Takao M, Hamada H, Uemura K, Sugano N. Comparison of the accuracy of the cup position and orientation in total hip arthroplasty for osteoarthritis secondary to developmental dysplasia of the hip between the Mako robotic arm-assisted system and computed tomography-based navigation. Int Orthop. 2021;45:1719–25. [DOI] [PubMed] [Google Scholar]
- 7.Kamath AF, Durbhakula SM, Pickering T, Cafferky NL, Murray TG, Wind MA, et al. Improved accuracy and fewer outliers with a novel CT-free robotic THA system in matched-pair analysis with manual THA. J Robot Surg. 2022;16:905–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Matsuki Y, Imagama T, Tokushige A, Yamazaki K, Sakai T. Accuracy of cup placement using computed tomography-based navigation system in total hip arthroplasty through the direct anterior approach. J Orthop Sci. 2023;28:370–5. [DOI] [PubMed] [Google Scholar]
- 9.Tsukada S, Wakui M. Decreased accuracy of acetabular cup placement for imageless navigation in obese patients. J Orthop Sci. 2010;15:758–63. [DOI] [PubMed] [Google Scholar]
- 10.Hasegawa M, Naito Y, Tone S, Sudo A. Accuracy of a novel accelerometer-based navigation (Naviswiss) for total hip arthroplasty in the supine position. BMC Musculoskelet Disord. 2022;23:537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wasterlain AS, Buza JA, Thakkar SC, Schwarzkopf R, Vigdorchik J. Navigation and robotics in total hip arthroplasty. JBJS Rev. 2017;5:e2. [DOI] [PubMed] [Google Scholar]
- 12.Shaw JH, Rahman TM, Wesemann LD, Jiang ZC, Lindsay-Rivera G, Davis K. Comparison of postoperative instability and Acetabular Cup Positioning in robotic-assisted Versus Traditional Total Hip Arthroplasty. J Arthroplasty. 2022;37:S881–9. [DOI] [PubMed] [Google Scholar]
- 13.Domb BG, Chen JW, Lall AC, Perets I, Maldonado DR. Minimum 5-year outcomes of robotic-assisted primary total hip arthroplasty with a nested comparison against manual primary total hip arthroplasty: a propensity score-matched study. J Am Acad Orthop Surg. 2020;28:847–56. [DOI] [PubMed] [Google Scholar]
- 14.Guo DH, Li XM, Ma SQ, Zhao YC, Qi C, Xue Y. Total hip arthroplasty with robotic arm assistance for Precise Cup positioning: a case-control study. Orthop Surg. 2022;14:1498–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sicat CS, Buchalter DB, Luthringer TA, Schwarzkopf R, Vigdorchik JM. Intraoperative technology use improves accuracy of functional safe zone targeting in total hip arthroplasty. J Arthroplasty. 2022;37:S540–5. [DOI] [PubMed] [Google Scholar]
- 16.Kamara E, Robinson J, Bas MA, Rodriguez JA, Hepinstall MS. Adoption of robotic vs fluoroscopic guidance in total hip arthroplasty: is acetabular positioning improved in the learning curve? J Arthroplasty. 2017;32:125–30. [DOI] [PubMed] [Google Scholar]
- 17.Shibanuma N, Ishida K, Matsumoto T, Takayama K, Sanada Y, Kurosaka M, et al. Early postoperative clinical recovery of robotic arm-assisted vs. image-based navigated total hip arthroplasty. BMC Musculoskelet Disord. 2021;22:314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tamaki Y, Goto T, Wada K, Omichi Y, Hamada D, Sairyo K. Robotic arm-assisted total hip arthroplasty via a minimally invasive anterolateral approach in the supine position improves the precision of cup placement in patients with developmental dysplasia of the hip. J Orthop Sci. 2023. 10.1016/j.jos.2023.01.012. [DOI] [PubMed]
- 19.Fontalis A, Kayani B, Haddad IC, Donovan C, Tahmassebi J, Haddad FS. Patient-reported outcome measures in conventional total hip arthroplasty versus robotic-arm assisted arthroplasty: a prospective cohort study with minimum 3 years’ follow-up. J Arthroplasty. 2023;38:S324–9. [DOI] [PubMed] [Google Scholar]
- 20.Singh V, Realyvasquez J, Simcox T, Rozell JC, Schwarzkopf R, Davidovitch RI. Robotics versus navigation versus conventional total hip arthroplasty: does the use of technology yield superior outcomes? J Arthroplasty. 2021;36:2801–7. [DOI] [PubMed] [Google Scholar]
- 21.Nakata K, Nishikawa M, Yamamoto K, Hirota S, Yoshikawa H. A clinical comparative study of the direct anterior with mini-posterior approach: two consecutive series. Two Consecutive Ser J Arthroplasty. 2009;24:698–704. [DOI] [PubMed] [Google Scholar]
- 22.Kunze KN, Huddleston HP, Romero J, Chiu YF, Jerabek SA, McLawhorn AS. Accuracy and precision of acetabular component position does not differ between the anterior and posterior approaches to total hip arthroplasty with robotic assistance: a matched-pair analysis. Arthroplast Today. 2022;18:68–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.García-Rey E, García-Cimbrelo E, Cruz-Pardos A. Cup press fit in uncemented THA depends on sex, acetabular shape, and surgical technique. Clin Orthop Relat Res. 2012;470:3014–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hasegawa K, Kabata T, Kajino Y, Inoue D, Tsuchiya H. Periprosthetic occult fractures of the acetabulum occur frequently during primary THA. Clin Orthop Relat Res. 2017;475:484–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sharkey PF, Hozack WJ, Callaghan JJ, Kim YS, Berry DJ, Hanssen AD, et al. Acetabular fracture associated with cementless acetabular component insertion a report of 13 cases. J Arthroplasty. 1999;14:426–31. [DOI] [PubMed] [Google Scholar]
- 26.Davidson D, Pike J, Garbuz D, Duncan CP, Masri BA. Intraoperative periprosthetic fractures during total hip arthroplasty: evaluation and management. J Bone Joint Surg. 2008;90:2000–12. [DOI] [PubMed] [Google Scholar]
- 27.Imagama T, Matsuki Y, Okazaki T, Kaneoka T, Kawakami T, Yamazaki K, Sakai T. Change in hip laxity after anterior capsular suture in total hip arthroplasty using direct anterior approach. Sci Rep. 2024;27:14:2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Imura S. The Japanese Orthopaedic Association: evaluation chart of hip joint functions. J Jpn Orthop Assoc. 1995;69:864–7. [Google Scholar]
- 29.Matsumoto T, Kaneuji A, Hiejima Y, Sugiyama H, Akiyama H, Atsumi T, et al. Japanese Orthopaedic Association hip disease evaluation questionnaire (JHEQ): a patient-based evaluation tool for hip-joint disease. The Subcommittee on Hip Disease evaluation of the Clinical Outcome Committee of the Japanese Orthopaedic Association. J Orthop Sci. 2012;17(1):25–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Behrend H, Giesinger K, Giesinger JM, Kuster MS. The forgotten joint as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty. 2012;27(3):430–6. [DOI] [PubMed] [Google Scholar]
- 31.Redmond JM, Gupta A, Hammarstedt JE, Petrakos AE, Finch NA, Domb BG. The learning curve associated with robotic-assisted total hip arthroplasty. J Arthroplasty. 2015;30:50–4. [DOI] [PubMed] [Google Scholar]
- 32.Kanawade V, Dorr LD, Banks SA, Zhang Z, Wan Z. Precision of robotic guided instrumentation for acetabular component positioning. J Arthroplasty. 2015;30:392–7. [DOI] [PubMed] [Google Scholar]
- 33.Sato K, Sato A, Okuda N, Masaaki M, Koga H. A propensity score-matched comparison between Mako robotic arm-assisted system and conventional technique in total hip arthroplasty for patients with osteoarthritis secondary to developmental dysplasia of the hip. Arch Orthop Trauma Surg. 2023;143:2755–61. [DOI] [PubMed] [Google Scholar]
- 34.Encinas-Ullán CA, Martínez-Diez JM, Rodríguez-Merchán EC. The use of external fixation in the emergency department: applications, common errors, complications and their treatment. EFORT Open Rev. 2020;5:204–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hananouchi T, Takao M, Nishii T, Miki H, Iwana D, Yoshikawa H, et al. Comparison of navigation accuracy in THA between the mini-anterior and posterior approaches. Int J Med Rob Comput Assist Surg. 2009;5:20–5. [DOI] [PubMed] [Google Scholar]
- 36.Docquier PL, Paul L, Cartiaux O, Banse X. Registration accuracy in computer-assisted pelvic surgery. Comput Aided Surg. 2009;14:37–44. [DOI] [PubMed] [Google Scholar]
- 37.Kitada M, Nakamura N, Iwana D, Kakimoto A, Nishii T, Sugano N. Evaluation of the accuracy of computed tomography-based navigation for femoral stem orientation and leg length discrepancy. J Arthroplasty. 2011;26:674–9. [DOI] [PubMed] [Google Scholar]
- 38.Nishii T, Sakai T, Takao M, Sugano N. Fluctuation of cup orientation during press-fit insertion: a possible cause of malpositioning. J Arthroplasty. 2015;30:1847–51. [DOI] [PubMed] [Google Scholar]
- 39.Fujishiro T, Hayashi S, Kanzaki N, Hashimoto S, Shibanuma N, Kurosaka M. Effect of screw fixation on acetabular component alignment change in total hip arthroplasty. Int Orthop. 2014;38:1155–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tabata T, Kaku N, Hara K, Tsumura H. Initial stability of cementless acetabular cups: press-fit and screw fixation interaction—An in vitro biomechanical study. Eur J Orthop Surg Traumatol. 2015;25:497–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Iwana D, Nakamura N, Miki H, Kitada M, Hananouchi T, Sugano N. Accuracy of angle and position of the cup using computed tomography-based navigation systems in total hip arthroplasty. Comput Aided Surg. 2013;18:187–94. [DOI] [PubMed] [Google Scholar]
- 42.Nogler M, Mayr E, Krismer M, Thaler M. Reduced variability in cup positioning: the direct anterior surgical approach using navigation. Acta Orthop. 2008;79:789–93. [DOI] [PubMed] [Google Scholar]
- 43.Lass R, Kubista B, Olischar B, Frantal S, Windhager R, Giurea A. Total hip arthroplasty using imageless computer-assisted hip navigation: a prospective randomized study. J Arthroplasty. 2014;29:786–91. [DOI] [PubMed] [Google Scholar]
- 44.Okamoto M, Kawasaki M, Okura T, Ochiai S, Yokoi H. Comparison of accuracy of cup position using portable navigation versus alignment guide in total hip arthroplasty in supine position. Hip Int. 2021;31:492–9. [DOI] [PubMed] [Google Scholar]
- 45.Kolodychuk NL, Raszewski JA, Gladnick BP, Kitziger KJ, Peters PC, Waddell BS. Handheld navigation improves accuracy in direct anterior total hip replacement. Arthroplast Today. 2022;17:58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zahaf S, Dahmane M, Belaziz A, Bouri I. Failure analysis of semi-elliptical crack behavior in the cement mantle of a total hip prosthesis. Mater Phys Mech. 2022;48(2):242–71. [Google Scholar]
- 47.Pierce J, Needham K, Adams C, Coppolecchia A, Lavernia C. Robotic-assisted total hip arthroplasty: an economic analysis. J Comp Eff Res. 2021;10(16):1225–34. [DOI] [PubMed] [Google Scholar]
- 48.Emara AK, Zhou G, Klika AK, Koroukian SM, Schiltz NK, Higuera-Rueda CA, et al. Is there increased value in robotic arm-assisted total hip arthroplasty? Bone Joint J. 2021;103–B(9):1488–96. [DOI] [PubMed] [Google Scholar]
- 49.Moldovan F, Gligor A, Moldovan L, Bataga T. The impact of the COVID-19 pandemic on the orthopedic residents: a pan-romanian survey. Int J Environ Res Public Health. 2022;19(15):9176. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data associated with this study is retained at the Department of Orthopedic surgery, Yamaguchi university graduate school of medicine and Yamaguchi prefectural grand medical center. The datasets generated and/or analyzed in this study are available from the corresponding author on reasonable request. If there are any questions, please contact the corresponding author.