Abstract
Background
Māori are over-represented in Aotearoa New Zealand morbidity and mortality statistics. Other populations with high health needs include Pacific peoples and those living with material deprivation. General practice has evolved into seven models of primary care: Traditional, Corporate, Health Care Home, Māori, Pacific, Trusts / Non-governmental organisations (Trust/NGOs) and District Health Board / Primary Care Organisations (DHB/PHO). We describe nurse work in relation to these models of care, populations with high health need and patient health outcomes.
Methods
We conducted a cross-sectional study (at 30 September 2018) of data from national datasets and practices at patient level. Six primary outcome measures were selected because they could be improved by primary care: polypharmacy (≥ 65 years), glucose control testing in adults with diabetes, immunisations (at 6 months), ambulatory sensitive hospitalisations (0–14, 45–64 years) and emergency department attendances. Analysis adjusted for patient and practice characteristics.
Results
Nurse clinical time, and combined nurse, nurse practitioner and general practitioner clinical time, were substantially higher in Trust/NGO, Māori, and Pacific practices than in other models. Increased patient clinical complexity was associated with more clinical input and higher scores on all outcome measures. The highest rates of preventative care by nurses (cervical screening, cardiovascular risk assessment, depression screening, glucose control testing) were in Māori, Trust/NGO and Pacific practices. There was an eightfold difference, across models of care, in percentage of depression screening undertaken by nurses and a fivefold difference in cervical screening and glucose control testing. The highest rates of nurse consultations afterhours and with unenrolled patients, improving access, were in PHO/DHB, Pacific, Trust/NGO and Māori practices. Work not attributed to nurses in the practice records meant nurse work was underestimated to an unknown degree.
Conclusions
Transferring work to nurses in Traditional, Health Care Home, and Corporate practices, would release general practitioner clinical time for other work. Worse patient health outcomes were associated with higher patient need and higher clinical input. It is plausible that there is insufficient clinical input to meet the degree of patient need. More practitioner clinical time is required, especially in practices with high volumes of complex patients.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12939-024-02288-z.
Keywords: Nursing, Models of care, Primary care, Māori, Pacific, Deprivation, Patient health outcomes, Immunisations, Ambulatory sensitive hospitalisations, Emergency department attendance
Background
Historical context
In 1901 Aotearoa New Zealand became the first country in the world to register nurses. Ten years later, nurses were sent to remote locations to care for indigenous Māori communities overwhelmed by introduced infectious diseases, under the Native Health Nursing Scheme. Today, Māori remain over-represented in morbidity and mortality statistics [1]; postcolonial power relations continue to marginalise Māori as Other in their own country [2–4]. Cultural safety is defined by those who receive health services, and nurses are required to provide culturally safe care that defines therapeutic partnerships as respectful and empowering [3]. To improve patient health outcomes nurses, and other health workers, must be “pro-equity, culturally safe, Tiriti compliant and anti-racist” [1].
Before 1938 patients paid the full cost of primary care. The Social Security Act of 1938 introduced subsidies for primary care by general medical practitioners (GPs) who retained the right to set patient co-payments. GPs typically owned the practice in which they worked. Most practices were small – many with only one GP. Few registered nurses (RNs) worked in these practices until the government introduced a subsidy for nurse salaries in 1970 [5], which saw RN numbers rapidly increase. By 1999, 94% of practices included one or more RNs [6]; today there are few practices without RNs. Initially employed as a doctor’s assistant, the RN role has progressively extended and become more autonomous [7]. In many countries RNs work in primary care, although employment titles may differ, such as practice nurse (NZ, Australia, UK) or office nurse (US). In Aotearoa New Zealand, the 2001 Primary Health Care Strategy signalled the need for more primary health care nurses with “generalist knowledge and skills as well as developing advanced skills in particular areas of professional practice” [8].
The first Nurse Practitioner (NP) in Aotearoa New Zealand was registered under a legislated scope of practice in 2001. A NP can provide the same range of services as a GP as a lead provider of care with prescriber status, refer to secondary care, and issue standing orders and death certificates. NPs can access general medical, aged residential care, and Accident Compensation Corporation subsidies [9]. There were 604 practicing NPs on the Nursing Council of New Zealand (NCNZ) -Te Kaunihera Tapuhi o Aotearoa register on 23 April 2022; 23 NPs were Māori, 9 were Pacific, and about half were working in primary health care (K Hoare, personal communication, 2022).
Registered Nurses in primary care and community care settings
The NCNZ reported 56,951 practising RNs (excluding NPs and enrolled nurses) as of 31 March 2020 [10]. In community settings, the areas of practice with the largest numbers were: primary health care 4,428 (8.6%); practice nursing 2927 (5.7%), with fewer than 220 Māori RNs [11, 12]; mental health community 2,424 (4.7%) including 15% Māori RNs; and district nursing 1,493 (2.8%) [12]. RNs can qualify to prescribe in primary health and specialty teams, or in community health [13].
Practice nursing is a distinct area of practice, working in general practice / primary care. Work includes childhood immunisations—identifying enrolled infants and children, administering immunisations, and managing the cold chain process. PNs undertake systematic screening, such as cardio-vascular risk assessment, and often lead the care for patients with long term conditions. RNs who work to standing orders from GPs or NPs can provide medications to patients in settings such as nurse-led sexual health clinics and provide antibiotics for a sore throat to prevent rheumatic fever or deliver intravenous antibiotics for cellulitis. RN work includes health education, wound care, recalls and screening, outreach, and home visiting.
This study
Multiple models of primary care have arisen over the last 20–30 years. Further description is provided in an overview paper from this study [14]. Briefly, these can be seen as responses to a series of overlapping and often-incompatible stressors, opportunities and societal trends: a new and international focus on primary health care; shifting funding away from fee-for-services to capitation; advancing scopes of nursing practice, to include Nurse Practitioner; introduction of non-regulated workforce into primary care to improve access for groups underserved by traditional general practice; development of District Health Boards and Primary Health Organisations; trends in business management including a focus on private investment opportunities; a drive to address health inequities, especially for Māori; assertion of Māori sovereignty over their health care; and concerns that primary health care continues to fail Pacific peoples. Government has been willing to invest in primary care but it has been unclear which, if any, models of care lead to improved patient health outcomes. The New Zealand Ministry of Health sought research to guide investment in general practice models of care that deliver best patient health outcomes. The models they identified were Traditional, Corporate and Health Care Home. In consultation with the Ministry of Health and the Health Research Council, we extended the classification to also recognise: Māori practices, Pacific practices, practices owned by Trusts or Non-governmental Organisations, and practices owned by District Health Boards or Primary Health Organisations.
This paper describes nurse work within primary care / general practice in Aotearoa New Zealand. Other findings from this study are reported elsewhere in this Journal [14]. The enquiry was at the level of practice rather than individual patient or nurse. Our priority was to consider the care of those less well-served by the current health system; this is disproportionately people who are Māori, Pacific, or living with deprivation.
We hypothesised that: nurse workload and type of services provided would vary between models of primary care; that nurse workload would be greater for patients with higher need as a natural response to need and an explicit aim to address health equity; that nurse consultations would be longer than doctors due to attending to social as well as medical needs; that nurse prescribing, diagnosis and treatment would be more prevalent in practice models with higher patient need; and that greater nurse workload would be associated with better patient health outcomes.
Methods
A cross sectional, observational study was conducted of all Aotearoa New Zealand general practices and enrolled patients as of 30 September 2018. The date was chosen because funding changes in December 2018 were likely to confound data interpretation. Further detail on methods can be found in Supplementary file 1 of the primary outcomes paper for this study. Numbers of practices and patients contributing data varies between analyses so is specified in each section of results and in Table captions.
Data sources
Data came from national datasets, held by the Ministry of Health, and from practice information held by Primary Health Organisations (PHOs). All general practices belong to a PHO, which contracts to a District Health Board (DHB) to provide primary care services. DHBs were responsible for publicly funded regional health services; they ceased to exist as independent entities from 1 July 2022. National datasets included PHO registers, inpatient, outpatient, laboratories, pharmaceutical dispensing, immunisations, the Virtual Diabetes Register, the Index of Multiple Deprivation (IMD) and the Measuring Multimorbidity Index (M3) at patient level.
The Virtual Diabetes Register lists all individuals considered to have diabetes based on administrative data [15]. The IMD assigns a deprivation score to individuals based on the geographic zone of their residential address. The index is constructed from seven domains, which can be used independently: employment, income, crime, housing, education, health, and access. We used all domains except health [16]. The M3 index is a score assigned to each person based on number and type of conditions they have, derived from hospital discharge coding [17].
Data from these sources are available for all practices. The workforce numbers and Full Time Equivalents come from a practice survey sent to practices by all participating PHOs, so are self-declared rather than calculated from the PHO/practice data extracts.
The national PHO register lists patients enrolled in each practice. Included is the patient unique identifier, their National Health Index (NHI), used throughout the health system. Processes linking patient-level data using an encrypted NHI are well-established. At the time of this study PHO registers were constructed quarterly.
Every practice in Aotearoa New Zealand uses an electronic medical record. All PHOs extract data from practices, although details vary between PHOs. We requested data on number and length of consultations and the profession of the clinician seen.
Identifying RN, NP, GP work
Across most practices, nurse activity was much harder to identify and analyse than GP activity. GPs tended to use only one named-provider template to record their time, which had exploitable characteristics that aided classification. For example, GP templates would consistently be coded with the GP’s Medical Council number and names nearly always began with “Dr”. Nurses, on the other hand, used both generic and named-provider templates. When named-provider templates were used by nurses, the practitioner profession was often not specified, making it more difficult to identify nurse activities. Generic templates were inconsistently named across practices, such as, for example: “nurse”, “nurs”, “nur”, “N1”, and “IUCD nurse”. Many practices used a wide range of generic templates for different services, such as, “diabetes clinic”.
Unclassified names on templates were cross-checked with the register of practicing nurses held by the Nursing Council of New Zealand—Te Kaunihera Tapuhi o Aotearoa. Together with manual classification of inconsistent template names, “hidden” nurse templates were identified, which accounted for a significant portion of nurse work in the appointment data.
Defining practice models
In addition to the models identified by the granting bodies – Traditional, Corporate and Health Care Home – the research team recognised that there were additional, distinct, models of care. Working with the funders, we defined seven models as follows.
Traditional practice
Typically centred upon the general practitioner, with mainly nursing support, operating as a small business, and owned by one or more doctors. These ranged from small to large organisations and served both high need and lower need populations. This is the longest-standing model and constitutes the majority of practices. Individual practices have a high degree of autonomy over service delivery.
Corporate practice
A group of practices owned and run as a for-profit business entity. Some delivered high volumes of care, with low costs for patients and often without the need for an appointment. Corporate practices had a relatively high degree of standardisation in business and clinical processes and information technology across different sites. Most corporate practices were Traditional practices before being bought by a corporate entity.
Health Care Home (HCH)
An adaptation of the Patient Centred Medical Home; the New Zealand HCH Collaborative maturity matrix focuses on business efficiency and sustainability [18]. It is a relatively new concept in Aotearoa New Zealand, with the first practice formally enrolling in the programme in 2011. Only 14 had been fully certificated as mature HCHs by 30 September 2018 (A Maxwell, personal communication 2018). At the time of this study those not certificated were at different stages of meeting the maturity matrix criteria. Most had been Traditional practices prior to embarking on the HCH programme.
PHO/DHB practices
Practices owned by a PHO or a District Health Board (DHB). This was a small group that had mostly been taken over by a PHO or DHB to continue to provide primary care services in a specific location, often an underserved and/or rural area.
Trust/NGO practices
One or more practices owned by an entity that was a not-for-profit trust or non-governmental organisation. They had a stated purpose, identifying a health or social goal. Many were in small communities or served populations with high need. They provided, for example, salary and premises to attract and retain staff.
Māori practices
Practices owned and governed by Māori organisations, serving mostly Māori and some non-Māori patients. They were identified through lists from the Ministry of Health and DHBs together with web searches, direct contact with practices or were known to investigators. There may be a small number of practices we did not identify as Māori practices.
Pacific practices
Practices owned and governed by Pacific organisations, serving mostly Pacific and some non-Pacific patients. They were identified through lists from the Ministry of Health and DHBs together with web searches, direct contact with practices or were known to investigators. There may be a small number of practices we did not identify as Pacific practices.
Traditional, Corporate, PHO/DHB or Trust/NGO were re-considered as ownership types. We assigned every practice to one of these ownership types although some practices were difficult to categorise. HCH, Māori and Pacific practices could overlap with each other and with the ownership types.
On 30 September 2018, the NZ population was about 4,921,300 of whom 4,561,097 (92.7%) were enrolled in one of 988 general practices, leaving 360,203 people (7.3%) not enrolled [19]. This latter group is largely outside our data collection. Overall, non-enrolled people are less likely to have acute secondary care interactions than enrolled. The main exception is 1–4 year olds, and to a lesser extent 5–9 year olds, who seek secondary care more often than enrolled patients, more for Māori and Pacific children, and those in more deprived districts (G Jackson, personal communication, 2022). The unenrolled population may also include people at high need who seek and receive few services.
Primary health outcomes
The period of analysis was the year 1 October 2017 to 30 September 2018. The six study outcomes were as follows.
Polypharmacy
Patients over 64 years old taking 5 or more long term medications over two consecutive quarters, using methods specified by the Health Safety and Quality Commission [20].
Glucose control in diabetes
Patients on the national Virtual Diabetes Register with one or more glycated haemoglobin (HbA1c) tests in the previous year.
6 Month immunisation
Children who had received all the scheduled immunisations by age 6 months; includes only children who were 6 months old at some point during the period of analysis.
Child ASH Admissions
The number of ambulatory sensitive hospital admissions for children who were under 15 years of age at the end of the analysis period.
Adult ASH Admissions
The number of ambulatory sensitive hospital admissions for adults who were between 45 and 64 years of age at the end of the analysis period.
ED attendances
The number of attendances at an Emergency Department for each patient over the period of analysis.
Explanatory variables
The explanatory variables for outcomes analysed were patient factors, practice factors and measures of primary care clinical input.
Patient characteristics
Age, gender, Māori or Pacific ethnicity, deprivation quintile score 5 (most deprived area, Q5) of the area the patient lives in, Index of Multiple Deprivation (IMD) score of the area the patient lives in distance to the nearest ED, being on the Virtual Diabetes Register and a multimorbidity score (M3); in the previous year having gout, being dispensed a selective serotonin reuptake inhibitor (SSRI, usually for depression), dispensed tramadol (for moderate to severe pain) or dispensed an antibiotic; during the previous year, whether patient changed their enrolled practice (a measure of practice continuity), and had a first medical specialist assessment (FSA) in secondary care, or did not attend a FSA.
Practice characteristics
Very Low Cost Access (VLCA) practices agree to receive increased capitation funding while limiting their fees to patients. Practice uptake of this contract is voluntary subject to having an enrolled population of ≥ 50% Māori, Pacific or people living in Quintile 5 areas. Practices were designated as either urban or rural based on the rural status of a majority of their enrolled patients. The percentage of patient consultations, in the previous year, with the same GP was used as a measure of personal continuity.
Primary care clinical input
Activities recorded in the Practice Management System were attributed to a Nurse, NP, Doctor or Other. Other included health care assistants, dieticians, physiotherapists, Quit smoking providers and unidentified persons. Total Consultations refers to the number of face-to-face consultations with a GP or NP in the previous year. Time spent with each patient, according to the practice appointment book, considered to be clinical time, were cumulated to a proportion of Full Time Equivalent (FTE) per 1000 enrolled patient, separately for GP, NP and nurse.
Uncertainty in classifications
Some factors may represent both patient characteristics and clinician input; for example, attending a VLCA practice might be patient choice, but a practice might opt into a VCLA contract in response to local patient poverty. Having a FSA reflects patient need and a referral from primary care in response to that need; Did Not Attend a FSA might indicate a patient barrier to access. Total Consultations, GP and Nurse clinical time can also be seen as markers of both patient need and system response.
Regression analyses
Multilevel mixed effects regression analyses used patient-level data adjusted for clustering at practice level. All analyses were conducted in R statistical software [21, 22]. Statistical significance is cited at p ≤ 0.05. Variables that do not appear in the final regressions were not statistically significant. The comparators used in the regressions vary between practice models. Ownership categories Corporate, PHO/DHB and Trust/NGO were compared to Traditional. HCH, Māori practices and Pacific practices were compared with not-HCH, not-Māori practices and not-Pacific practices, respectively.
Results
Practice models
The study included 924 practices with 4,491,964 enrolled patients. Each practice was classified to one ownership category from Traditional, Corporate, PHO/DHB or Trust/NGO. Where relevant, we also classified practices as Māori or Pacific practices or Health Care Homes, which overlapped with the ownership categories as shown in Table 1. Most Māori and Pacific practices were owned by a Trust or NGO. Ten practices were HCH, Māori and Trust/NGO; one was HCH, Māori and Corporate; and one was HCH, Pacific and Trust/NGO.
Table 1.
Practice models showing overlapping categories across 924 practices
|
Traditional (n = 695) |
Corporate (n = 103) |
PHO/DHB (n = 27) |
Trust/NGO (n = 99) |
|
|---|---|---|---|---|
| Māori practice (n = 65) | 3 | 3 | 0 | 59 |
| Pacific practice (n = 15) | 4 | 0 | 0 | 11 |
| Health Care Home (n = 127) | 90 | 14 | 7 | 16 |
PHOs and practices contributing data
Data on activities, consultations and clinical time, measured as FTE, came from practice data provided by PHOs. At the time of the study there were 35 PHOs in Aotearoa New Zealand, of which 13 provided at least some data. Overall, enrolled patient population demographics covered by these PHOs was considered representative of the country. Full data were not available from every practice in every PHO. Data were missing for the following reasons: data were not recorded at practice level, not collected from practices by the PHO, or was not in a form that could not validly be compared across practices. The variance in available data reflected the widely varying data management capabilities of PHOs, and also the widely varying data sharing arrangements between PHOs and practices. The number of practices contributing data to each analysis is reported. Analyses that combine data from different practice numbers should be seen as indicative only, as not all practices contributed full data to each calculation.
Full or partial data were contributed by 415 (60%) of 695 Traditional practices, 66 (64%) of 103 Corporate practices, 18 (67%) of 27 PHO/DHB practices, 43 (43%) of 99 Trust/NGO practices, 25 (38%) of 65 Māori practices, 12 (80%) of 15 Pacific practices, and 94 (74%) of 127 HCH practices.
Practitioner consultations, defining GPs
Data in Table 2 came from 292 practices in 10 PHOs over a three-year period. These data on consultations were taken from the appointment book and represent face to face consultations, but not telephone, email or other contacts. Of consultations with a doctor, 82% were vocationally registered in general practice, 17% had no vocational registration (primarily doctors in a postgraduate training pathway) and 1% with other specialist vocational registration. For this study, all doctors are referred to as GPs. Compared with GP consultations, RN consultations were shorter by 14% and NP consultations were longer by 16%.
Table 2.
Face-to-face consultation number and length, by practitioner; data from 292 practices in 10 Primary Health Organisations
| Number consultations | Full Time Equivalent consultations | Full Time Equivalent per 10,000 consultations | Minutes per consultation, average | |
|---|---|---|---|---|
| General Practitioners | 4,218,012 (63.1%) | 417.1 (66.1%) | 0.99 | 11.4 |
| Nurse Practitioners | 38,113 (0.6%) | 4.4 (0.7%) | 1.15 | 13.2 |
| Registered Nurses | 1,551,883 (23.2%) | 132.4 (21%) | 0.85 | 9.9 |
| Other | 873,014 (13.1%) | 77.4 (12.3%) | 0.89 | 10.3 |
Note: Other includes health care assistants, dieticians, physiotherapists, Quit smoking providers and unidentified persons
Registered Nurse and Nurse Practitioner activities
Data in Table 3 came from 212 to 364 practices and show the proportions of activities undertaken by RN and NP combined, or by GP.
Table 3.
Percentage of activities by RN and NP, or GP, by practice model, rural or urban; number of practices contributing to each calculation is shown in the first row of data
| Cervical screening | Cardiovascular risk assessment | Depression screening with PHQ9 | Glucose control testing | Consultations after hours | Consultations unenrolled patients | Dispensed medicines | |
|---|---|---|---|---|---|---|---|
| Practice N | 276 | 220 | 212 | 384 | 275 | 277 | 291 |
| Traditional | 39 (57) | 52 (45) | 7 (91) | 9 (89) | 19 (72) | 23 (66) | < 1.2 (99) |
| Corporate | 58 (31) | 61 (26) | 19 (76) | 11 (82) | 21 (67) | 23 (64) | < 1.2 (99) |
| PHO/DHB | 17 (81) | 43 (58) | 1 (99) | 27 (72) | 45 (40) | 41 (50) | < 1.2 (100) |
| Trust/NGO | 71 (23) | 68 (26) | 21 (75) | 11 (81) | 27 (46) | 37 (55) | 5 (95) |
| HCH | 42 (49) | 47 (40) | 4 (88) | 8 (89) | 17 (61) | 18 (55) | < 1.2 (99) |
| Māori | 61 (32) | 70 (14) | 33 (66) | 11 (87) | 26 (57) | 36 (58) | 3 (97) |
| Pacific | 78 (21) | 73 (20) | 5 (95) | 5 (93) | 41 (46) | 40 (59) | < 1.2 (100) |
| Rural | 59 (36) | 62 (37) | 24 (76) | 20 (75) | 26 (71) | 35 (60) | 4 (96) |
| Urban | 41 (54) | 52 (42) | 7 (90) | 8 (89) | 20 (70) | 24 (65) | < 1.2 (99) |
Note 1 Results are percentage by RN and NP (%GP)
Note 2 Percentages by RN, NPs and GPs may not sum to 100 due to work by Others
Summing RN and NP contributions across preventative care (cervical screening, cardiovascular risk assessment, depression screening and glucose control testing) showed the strongest RN and NP contribution was in Māori, Trust/NGO, Pacific and Corporate practices. The percentage of RNs and NPs undertaking each activity varied dramatically between models of care. There was an eightfold difference in percentage of depression screening undertaken by RNs and NPs, a fivefold difference in cervical screening and glucose control testing and a twofold difference in cardiovascular risk assessment.
Work to support access was measured by summing RN and NP contributions to consultations after hours and consultations with unenrolled patients. The strongest nurse contribution was in PHO/DHB, Pacific, Trust/NGO and Māori practices.
Compared with urban practices, NPs and RNs in rural practices were more likely to undertake cardiovascular risk assessment, depression screening and testing glucose control. A low percentage of dispensed medicines was attributed to RNs and NPs, across all practice models, at the time of this study.
RN, NP, and Health Care Assistant (HCA) clinical time associations with patient need for health services
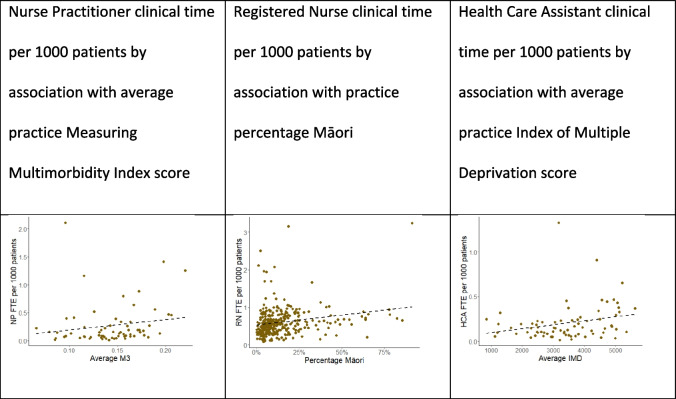
Data in the scatterplots came from 373 practices for RN Full Time Equivalent (FTE), 224 practices for NP FTE, and 201 practices for HCA FTE. Scatterplots suggest an increase in NP, RN, and HCA FTE, respectively, with an increasing: average practice M3 score, practice percentage Māori and average practice IMD (Fig. 1). Practices with no RN, NP or HCA were not included in these plots.
Fig. 1.
Scatter plots: NP, RN, and HCA clinical time (Full Time Equivalent) per 1000 patients by average practice Measuring Multimorbidity Index score, percentage Māori, average practice Index of Multiple Deprivation score.Note. Each dot represents a practice, and the dashed line is a univariate regression
RN, NP and GP FTE associations between practice models and characteristics
Data in Table 4 come from 67 practices for NP data, 364 for RN data and 375 for GP data Calculation of RN numbers per 1000 patients include only those practices where there is a RN present, and similarly a NP or GP. Incomplete data means that calculations do not necessarily provide direct comparisons across the same practices, so that results are indicative only.
Table 4.
RN, NP, GP FTE per 1000 patients by practice model or characteristic; (numbers in brackets are number of practices contributing data to each analysis)
| Registered Nurses | Nurse Practitioners | General Practitioners | Registered Nurses + Nurse Practitioners | Registered Nurses + Nurse Practitioners + General Practitioners | Registered Nurses + Nurse Practitioners: General Practitioners | |
|---|---|---|---|---|---|---|
| Overall | 0.55 (364) | 0.14 (67) | 0.63 (375) | 0.69 | 1.32 | 1.10 |
| Practice model | ||||||
| Traditional | 0.52 (270) | 0.14 (29) | 0.63 (273) | 0.66 | 1.29 | 1.05 |
| Corporate | 0.58 (61) | 0.08 (20) | 0.60 (63) | 0.66 | 1.26 | 1.10 |
| Primary Health Organisation / District Health Board | 0.64 (7) | 0.19 (3) | 0.63 (9) | 0.83 | 1.46 | 1.32 |
| Trust / Non-governmental Organisation | 0.90 (26) | 0.19 (15) | 0.69 (30) | 1.09 | 1.78 | 1.58 |
| Māori provider | 0.79 (16) | 0.19 (11) | 0.68 (19) | 0.98 | 1.66 | 1.44 |
| Pacific provider | 0.87 (7) | 0 (0) | 0.67 (8) | 0.87 | 1.54 | 1.30 |
| Health Care Home | 0.59 (33) | 0.08 (15) | 0.60 (37) | 0.67 | 1.27 | 1.12 |
| Practice characteristic | ||||||
| Rural | 0.65 (28) | 0.20 (8) | 0.71 (28) | 0.85 | 1.56 | 1.20 |
| Urban | 0.54 (336) | 0.13 (347) | 0.63 (59) | 0.67 | 1.3 | 1.06 |
| Very Low Cost Access | 0.58 (130) | 0.18 (27) | 0.59 (347) | 0.76 | 1.35 | 1.29 |
| Not Very Low Cost Access | 0.54 (234) | 0.12 (40) | 0.64 (237) | 0.66 | 1.3 | 1.03 |
| Patients enrolled | ||||||
| > 20,000 (N = 8) | 0.53 (5) | 0.04 (3) | 0.60 (5) | 0.57 | 1.17 | 0.95 |
| > 10,000–20,000 (N = 86) | 0.55 (41) | 0.07 (15) | 0.57 (42) | 0.62 | 1.19 | 1.09 |
| > 2,000–10,000 (N = 615) | 0.53 (247) | 0.17 (42) | 0.62 (249) | 0.70 | 1.32 | 1.13 |
| < 2,000 (N = 215) | 0.65 (71) | 0.85 (7) | 0.77 (79) | 1.50 | 2.27 | 1.95 |
| Patient characteristics | ||||||
| Māori > 30% | 0.67 (37) | 0.19 (20) | 0.68 (44) | 0.86 | 1.54 | 1.26 |
| Pacific > 30% | 0.51 (40) | 0.19 (3) | 0.55 (43) | 0.70 | 1.25 | 1.27 |
| Deprivation quintile 5 > 30% | 0.65 (94) | 0.19 (27) | 0.65 (105) | 0.84 | 1.49 | 1.29 |
| Index of Multiple Deprivation > median | 0.57 (273) | 0.13 (53) | 0.63 (295) | 0.70 | 1.33 | 1.11 |
| Measuring Multimorbidity Index > median | 0.68 (28) | 0.47 (11) | 0.75 (32) | 1.15 | 1.9 | 1.53 |
Results are median FTE per 1000 enrolled patients (number of practices contributing data)
Traditional, Corporate and HCH have the lowest FTE for nursing workforce (RN + NP) and total workforce (RN + NP + GP) and the lowest ratio of nursing to general practitioner workforce (RN + NP:GP). Trust/NGO, Māori, Pacific and PHO/DHB practices have the highest nursing workforce, total workforce, and ratio.
NP numbers per 1000 patients were higher in Trust/NGO, Māori and PHO/DHB practices, small practices, rural practices, VLCA practices, and practices with more multimorbidity. There were no NPs in Pacific practices.
Nursing workforce and total workforce was higher in small practices, rural practices, practices with more multimorbidity, more Māori patients and more patients living in deprivation.
Primary care clinical input
Table 5 presents selected outputs from six regressions that show associations of primary care clinical input for each primary outcome along with other explanatory variables including models of care. Direct effects were estimated for a total count of consultations with a NP or GP, and as RN and GP clinical time (as full time equivalent). Interactions were estimated if the direct effect was statistically significant, and test for different effects between the exclusive models of care – Corporate, PHO/DHB and Trust/NGO, with Traditional as a reference category. For full regression outputs , see the full report on the primary outcomes from this study in the Journal [14]; here we report the associations with nurse work and primary study outcomes.
Table 5.
Selected output from final models for patient health outcomes across 924 practices. Age and some other patient characteristics omitted – full regression outputs in primary outcomes paper, Supplementary file 2
|
Variable (Reference values) |
Polypharmacy Age 65 + N = 399,227 R2 = 0.364 |
Glucose control testing in diabetes N = 133,985 R2 = 0.1366 |
6 month immunisations N = 26,859 R2 = 0.0795 |
Child ASH admissions N = 511,845 R2 not applicable |
Adult ASH admissions N = 655,088 R2 not applicable |
ED attendances N = 2,500,000 R2 not applicable |
|---|---|---|---|---|---|---|
| Overall average | 38.2% | 86.9% | 75.6% | 31 per 1000 children |
38 per 1000 adults |
254 per 1000 patients |
| Practice models | ||||||
| Corporate (Traditional) | 37.5% (38.3%) | 86.3% (87.0%) | 74.3% (75.7%) | -9.3% | 20.9% *** | 1.4% |
| PHO/DHB (Traditional) | 35.5% (38.3%) | 86.5% (86.9%) | 74.9% (75.6%) | -14.5% | 10.0% | 10.3% |
| Trust/NGO (Traditional) | 38.1% (38.2%) | 88.4% (86.7%) | 79.3% (75.2%) | 38.3% ** | 31.5% *** | 15.4% ** |
| HCH Practice (All others) | 38.7% (38.1%) | 86.2% (87.1%) | 78.5% (74.8%) *** | 5.6% | -5.4% | -11.2% *** |
| Māori Practice (All others) | 34.7% (38.0%) * | 82.9% (87.0%) ** | 61.8% (76.4%) *** | -0.4% | 5.9% | 9.6% |
| Pacific Practice (All others) | 36.9% (38.2%) | 83.6% (87.0%) | 66.5% (75.7%) * | -8.5% | -12.1% | -15.1% * |
| Patient characteristics | ||||||
| Māori (Not Māori) | 37.8% (38.2%) | 85.5% (87.1%) *** | 68.4% (77.0%) *** | 28.1% *** | 27.4% *** | 20.8% *** |
| Pacific (Not Pacific) | 34.2% (38.3%) *** | 85.5% (87.1%) *** | 76.1% (75.6) * | 40.2% *** | 28.0% *** | 19.5% *** |
| Quintile 5 (Not Q5) | 86.3% (87.1%) *** | |||||
|
IMD (25th, 50th, 75th centiles) (ASH&ED ref: average IMD) |
36.0% *** 38.5% 41.0% |
78.1% *** 76.1% 73.9% |
-11.2% *** 0.5% 13.1% |
-10.5% *** 0.5% 11.4% |
-8.2% *** 0.0% 8.9% |
|
|
M3 (25th, 50th, 75th centiles) (ASH&ED ref: M3 = 0) |
34.9% *** 38.0% 44.1% |
88.3% *** 87.6% 86.3% |
19.3% *** 64.8% 256.6% |
20.4% *** 49.2% 118.6% |
13.8% *** 32.8% 77.5% |
|
| Continuity of practice (No continuity) | -24.3% *** | -18.9% *** | -20.2% *** | |||
|
Distance to Nearest ED (1, 20, 100 km) (ASH&ED ref: average distance) |
76.8% *** 74.9% 66.0% |
3.2% -1.3% -18.1% |
6.1% *** -3.0% -33.4% |
|||
|
First Specialist Assessment (FSA 1, 2, 3) (ASH&ED ref: FSA = 0) |
39.8% *** 42.1% 44.3% |
87.8% *** 88.9% 90.0% |
45.9% *** 112.9% 210.7% |
45.1% *** 110.5% 205.5% |
46.1% *** 113.6% 212.2% |
|
|
First Specialist Assessment Did Not Attend (FSA DNA 1, 2, 3) (ASH&ED ref: FSA DNA = 0) |
67.9% *** 58.9% 49.2% |
15.5% ** 33.4% 54.2% |
50.9% *** 127.6% 243.3% |
50.7% *** 127.2% 242.5% |
||
| Practice characteristics | ||||||
| VLCA (not VLCA) | 86.2% (87.3%) * | 74.1% (76.3%) * | ||||
| Urban (Rural) | 38.1% (38.9%) | 86.7% (87.8%) * | 75.9% (73.6%) | -3.4% | -0.3% | |
|
Continuity of GP (25th, 50th, 75th centiles) (ASH&ED ref: Continuity = 0) |
-6.6% *** -8.6% -12.7% |
|||||
| Primary care clinician input | ||||||
|
GP + NP consultations (Consultations 1, 2, 3) (ASH&ED ref: Consultations = 0) |
25.4% *** 28.3% 34.6% |
81.8% *** 83.1% 85.3% |
73.8% *** 74.3% 75.2% |
8.7% *** 18.2% 39.8% |
8.1% *** 16.9% 36.7% |
7.5% *** 15.5% 33.3% |
|
RN hours (Hours 1, 2, 4) (ASH&ED ref: average hours) |
86.0% *** 86.2% 86.6% |
74.1% *** 74.3% 75.1% |
||||
|
GP hours (Hours 1, 2, 4) (ASH&ED ref: average hours) |
74.8% *** 75.3% 75.4% |
0.4% 0.0% 0.0% |
||||
| Interactions | ||||||
| GP + NP Consultations X Corporate |
4.1% *** (3.5%) |
1.0% (1.0%) |
0.2% (0.5%) |
10.8% ** (8.7%) |
6.2% *** (8.1%) |
7.6% (7.5%) |
| GP + NP Consultations X PHO/DHB |
4.7% *** (3.5%) |
1.1% (1.0%) |
0.4% (0.5%) |
8.7% (8.7%) |
11.0% * (8.1%) |
8.5% * (7.5%) |
| GP + NP Consultations X Trust/NGO |
4.1% *** (3.5%) |
0.9% (1.0%) |
0.1% (0.5%) |
9.5% (8.7%) |
6.5% ** (8.1%) |
7.3% (7.5%) |
| RN hours X Corporate |
0.3% * (1.1%) |
0.2% (1.9%) |
||||
| RN hours X PHO/DHB |
1.1% (1.1%) |
0.7% (1.9%) |
||||
| RN hours X Trust/NGO |
1.1% (1.1%) |
- 0.5% * (1.9%) |
||||
| GP hours X Corporate |
0.1% (0.8%) |
5.5% * (0.6%) |
||||
| GP hours X PHO/DHB |
0.3% (0.8%) |
4.2% (0.6%) |
||||
| GP hours X Trust/NGO |
0.8% (0.8%) |
4.4% (0.6%) |
||||
Polypharmacy, glucose control testing and immunisation results are logistic regressions
For binary variables, results are % of patients with that outcome, i.e. if variable = 1 (the result if variable = 0 is given in brackets)
For continuous variables, results are % of patients with that outcome, at specified value of variable, e.g. 25th, 50th, 75th centile, or 1, 2, 4 h
ASH and ED results are negative binomial regressions
For binary variables, results are % change from the reference value i.e. result if variable = 1 compared to value if variable = 0
For continuous variables, results are % change, at stated values, relative to the stated reference value; e.g. at GP hours 1, 2 or 4 compared to average hours)
Traditional practice is used as a reference for Corporate, PHO/Trust and Trust/NGO practice models including in Interactions
The value for Traditional practice is given in brackets. This value can vary slightly as the R margin command does not implement MEM (Marginal Effect at the Mean). We coded our own version of MEM but it is an approximation and there is some variability
*p < 0.05
**p < 0.01
***p < 0.001
There was a positive association between NP or GP number of consultations and each of the six patient outcomes; and a positive association between RN clinical time and glucose control testing and immunisation rates. Interactions suggest small differences between models of care in the relationship between clinical inputs and patient outcomes. For immunisations, in a Traditional practice, an additional hour of RN time was associated with a small increase in immunisation rates, and a with a small decrease in a Trust/NGO practice. In a Traditional practice, an additional contact with a NP or GP was associated with an increase of 8.7% in ASH admissions, with a higher increase in a Corporate practice.
An additional contact with a NP or GP was associated with an absolute increase in adult ASH, by varying amounts, in Traditional, Corporate, PHO/DHB and in a Trust/NGO practice.
Discussion
Four key findings arise from this study. First, we found that populations with more health need had more primary care clinical input, but potentially not enough to address those needs: we discuss opportunities for greater nurse input. Second, wide variation in specific clinical activities carried out also indicates the potential for increased nurse involvement especially in preventative activities. Third, increased primary care clinical input overall was associated with better and worse patient health outcomes – we discuss potential causal mechanisms. Fourth, nurse work was under-recorded in clinical records, with implications for improving data quality and analysis.
Nurse input in relation to patient health outcomes
The regression interactions between primary care clinical input and models of care suggest small but real differences between models in terms of how work is prioritised, organised, and supported. The differences are likely to be principally in the way nurse work is organised. While some findings are small in absolute terms, it should be noted that they are cumulative over time and over the six outcomes measured. Furthermore, there are likely to be similar, small but cumulative differences accruing across the multiple health outcomes we did not measure.
The association between primary care clinical input and variation in ASH and ED attendances, in particular, are of a magnitude that, if causation were properly understood, would justify interventions to reduce hospital workload.
More clinician FTE and consultations were associated with increased glucose control testing and higher immunisation rates at age 6 months. Both are considered direct measures of quality of care, and both have been national health targets with associated resourcing and active support from PHOs. Health Care Homes and Traditional practices had high rates of glucose control testing and immunisation rates at age 6 months and lower ratios of RN and NPs to GPs than Māori and Pacific practices; they also had practices with small numbers of enrolled Māori and Pacific patients.
Increasing primary care clinical input was also associated with worse predicted outcomes for polypharmacy, ASH rates and ED attendances. The most plausible explanation is that, for glucose control testing and immunisations, the increase in clinical input was sufficient to meet patient need, but for the remaining outcomes additional input was not sufficient to fully mitigate worse patient health outcomes. This suggests a need for more workforce, and that further research into clinical input by nurses and other practitioners could support targeting FTE to gain additional benefit to patients.
The overall average immunisation rate (Table 5) was 75.6% with the highest percentage undertaken by Health Care Home practices (78%). Māori practices (61.8%) and Pacific practices (66.5%) had immunisation rates below the overall average. Living in a Quintile 5 deprivation area has been associated with a delay in child immunisation (18). Independently, rates were lower for Māori patients, Pacific patients, attending a VLCA practice, higher deprivation and greater distance to ED. The effect of ethnicity remained after adjustment for deprivation and vice-versa. Strategies to improve access for these populations should include nurse and community health worker outreach, which has been effective for specific populations, but has never been resourced to support mainstream adoption [23].
The literature supports a positive association between nurse work and a wider range of patient health outcomes than were measured in the current study. A recent systematic review identified 23 studies reporting quantitative outcomes from nurse-led interventions in primary care. Improvements were reported for weight loss, pelvic floor muscle strength and endurance, blood pressure and glycaemic control, exercise self-efficacy, social activity, improved diet and physical activity levels, and reduced tobacco use [24]. An earlier Cochrane systematic review of 18 randomised trials of primary health care services found that care delivered by nurses, compared to doctors, could generate better outcomes for a broad range of patient conditions. There was strong evidence that number of return visits was higher for nurses. Blood pressure outcomes were slightly improved in nurse-led care, and other clinical outcomes were similar[25].
Nurse input increased as patient need increased
Across multiple measures we see increasing RN and NP activities and time associated with increasing patient need. This is evident in the scatterplots, measures of preventative care, work to support access, association with models of care where there is most need, and in the regressions.
RNs and NPs supported access to care (consultations after hours, consultations with unenrolled patients) in all practice models with highest levels in Māori, Pacific and Trust/NGO practices.
Trust/NGO, Māori, and Pacific practices had substantially higher FTE for nursing workforce, a relatively small increase in GP FTE, and a higher ratio of nursing to medicine compared to Traditional, Corporate and HCH practices.
Nursing workforce, and combined nursing and medical workforce, was higher in small practices, rural practices, practices with more multimorbidity, more Māori patients and more patients living in deprivation. NPs had a larger presence in small practices, rural practices, VLCA practices, and practices with more multimorbidity.
As assessed from the appointment book, RNs contributed 23.2% of all face-to-face consultations and NP contributed 0.6%. Consultations with RNs, not attributed to them in the appointment book can include, for example, patients seen for screening or triage ahead of a GP consultation and patients presenting without an appointment.
Compared with GP consultations, NP consultations were longer by about 16% and RN consultations were shorter by about 14%. NP consultations often include a comprehensive clinical and social assessment. Many of the activities undertaken by RNs can lower the average length of consultation, such as checking a wound, giving an immunisation, measuring blood pressure, testing blood glucose, or assaying proteinuria. Length of consultation has been found to be slightly longer in nurse-led primary care, compared to doctor-led care [25]. In the current study RN consultations were shorter than GP consultations, probably reflecting a predominance of short tasks worked around doctors’ appointments.
Potential to increase nurse work
Preventative care (cervical screening, cardiovascular risk assessment, depression screening, glucose control testing) varied dramatically between models of care in terms of the percentage undertaken by RNs and NPs. There was an eightfold difference in percentage of depression screening undertaken by RNs and NPs, a fivefold difference in cervical screening and HbA1c testing and a twofold difference in cardiovascular risk assessment. In Māori, Trust/NGO and Pacific practices, RNs and NPs, compared to GPs, had a higher overall rate of preventative care.
In rural practices, compared with urban practices, NPs undertook six times as many depression screens, and RNs undertook twice as many. Similar results were noted for glucose control tests on people with diabetes and cardiovascular risk assessments.
Together, this variation in the activities undertaken by nurses suggests there is an opportunity to markedly increase nursing input in preventative care, especially in Traditional, Health Care Home and urban practices, releasing GP FTE for other work.
Invisible nurse work
Work not attributed to RNs in the practice records meant nurse work was underestimated to an unknown degree (see Data Sources). Even tasks such as immunisations, which were nearly always undertaken by nurses, were not necessarily attributed to them. This may be driven by an ability to claim a higher fee-for-service when that service is undertaken by a GP, rather than a RN or NP. For example, ACC (previously the Accident Compensation Corporation) pays a lesser rate to NPs providing the same service as a GP [26], which may result in GPs claiming for NP work to maximise practice income. All consultations and FTE were calculated from face-to-face consultations. In addition to such consultations, RNs undertook multiple other activities. High volumes of work, more likely done by a RN than a GP, include telephone enquiries to assess clinical need, relay results, and coordinate care. Proper measurement of nurse input needs aligning data collection with a national data standard that requires identification of practitioners.
Limitations of the study
Despite collecting the largest data set on primary care in Aotearoa New Zealand, there remain large gaps in the available data, including, for example, on primary mental health. Analyses drew on data from different numbers of practices, largely due to differences in the data PHOs routinely extracted from practices. There was no reason to think that relevant data were systematically missing. Nevertheless, analyses that combined data from different numbers of practices, such as FTE calculations, should be taken as indicative only. Practice numbers contributing to each analysis are reported.
Study investigators and data managers all agreed that nurse and NP activities were widely under-recorded in the Practice Management System (PMS). Despite extensive efforts to identify and correct omissions, we acknowledge an unknown residual level of under-reporting. Systematic errors were identified where recording was tied to claiming payment for fee-for-service activities directly linked to practices invoicing systems. This meant that some activities could be invoiced only in the name of a doctor regardless of whether the work was undertaken in full, or in part, by a nurse or NP. The activities most likely to be affected include: glucose control testing, depression screening, and cardiovascular risk assessment.
There is no universally agreed list of conditions that constitute ambulatory sensitive hospitalisations. Any list includes conditions that are only partially preventable by access to effective primary care [19], such as respiratory illnesses like pre-school asthma that contribute to child ASH. Many unwell children or adults need to go to hospital, and many unwell persons go directly to hospital, bypassing acute primary care. It is well recognised that many factors outside of primary care influence the need for hospitalisation. Nevertheless, at practice level, ASH admissions are widely seen to be a measure that reflects on quality of primary care. Furthermore, in our study we measure variance between practices after statistical adjustments have been made for a wide range of patient and other factors.
We note that the date of the cross-sectional analysis was 2018. The date was chosen because we anticipated that funding changes in 2018/2019 would confound the analyses that looked back 1 or 3 years. While primary care delivery changed during the COVID 19 pandemic, many facets have returned to pre-pandemic models of care. The data from this study provides a basis to evaluate any subsequent changes particularly with respect to patient outcomes.
In the regressions, interactions hint at differences between models of care with respect to the relationship nurse clinical input and outcomes between models of care. Variations between practice models can also be seen in the screening and preventive activities undertaken by nurses. It would require further research to explore reasons for such differences.
Conclusions
Differences between models of care were apparent in the specific activities undertaken by nurses. In Māori, Pacific and Trust/NGO practices, RNs and NPs compared to GPs, contributed a higher rate of preventative care. The wide variation in the percentage of specific activities undertaken by nurses identifies an opportunity to markedly increase nursing input in preventative care, especially in Traditional, Health Care Home and urban practices, releasing GP FTE for other work.
Increasing RN, NP and GP activities and time were consistently associated with increasing patient need across multiple measures. Increasing primary care clinical input was associated with both better and worse patient health outcomes. The most plausible explanation is that additional clinical input was not sufficient to fully mitigate worse patient health outcomes. This suggests a need for more clinical workforce, and that further research into work undertaken by nurses and other practitioners could support targeting FTE to gain additional benefit to patients.
Nurse work is systematically under-recorded within the practice computer record. Measurement of nurse work needs to align data collection with a national data standard that mandates identification of practitioners. This is a minimum first step to planning nurse workforce to meet patient need and equitable patient health outcomes.
Supplementary Information
Acknowledgements
The authors acknowledge Erin Meads for advice on primary care data collection; CEOs and data managers for access to PHO and practice data; and the Steering Committee appointed by the funders, for facilitating access to national data.
The following people meet authorship criteria for the Journal and PubMed citation.
Primary Care Models Research Group Co-investigators
University of Auckland, Aotearoa New Zealand, highreliabilityconsulting@gmail.com
University of Auckland, Aotearoa New Zealand, bruce.arroll@auckland.ac.nz
WellSouth Primary Care Network, Aotearoa New Zealand, carol.atmore@wellsouth.org.nz
University of Otago, Aotearoa New Zealand, peter.crampton@otago.ac.nz
University of Otago, Aotearoa New Zealand, tony.dowell@otago.ac.nz
Independent Researcher, Aotearoa New Zealand, tana.fishman@gmail.com
University of Otago, Aotearoa New Zealand, robin.gauld@otago.ac.nz
University of Auckland, Aotearoa New Zealand, m.harwood@auckland.ac.nz
Te Whatu Ora-Health New Zealand Counties Manukau, Aotearoa New Zealand, Gary.Jackson@middlemore.co.nz
Te Whatu Ora-Health New Zealand, Aotearoa New Zealand, Rawiri.McKreeJansen@health.govt.nz
University of Auckland, Aotearoa New Zealand, n.kerse@auckland.ac.nz
University of Auckland, Aotearoa New Zealand, d.lampshire@auckland.ac.nz
University of Otago, Aotearoa New Zealand, lynn.mcbain@otago.ac.nz
Datacraft Analytics, Aotearoa New Zealand, jayden@datacraft.nz
Karolinska Institutet, Sweden, jovretbis@aol.com
Te Whatu Ora-Health New Zealand Counties Manukau, Aotearoa New Zealand, t.percival@auckland.ac.nz
Health Hawkes Bay—Te Oranga o Te Matau-a-Māui, Aotearoa New Zealand, roshan.perera@healthhb.co.nz
University of Cambridge, United Kingdom, mr108@cam.ac.uk
Pacific Perspectives, Aotearoa New Zealand, debbie@pacificperspectives.co.nz
Comprehensive Care PHO, Aotearoa New Zealand, jacqueline@comprehensivecare.co.nz
University of Otago, Aotearoa New Zealand, tim.stokes@otago.ac.nz
University of Otago, Aotearoa New Zealand, maria.stubbe@otago.ac.nz
Others
Sapere Research Group, Aotearoa New Zealand, dwatt@thinksapere.com
Sapere Research Group, Aotearoa New Zealand, Chris.peck@health.govt.nz
Abbreviations
- DHB
District Health Board; responsible for publicly funded health services in a geographical area; ceased to exist as independent entities from 1 July 2022
- ED
Emergency department
- FSA
First specialist assessment
- FSA DNA
Did not attend first specialist assessment
- FTE
Full time equivalent; refers to hours of work
- GP
General practitioner; family physician
- HCH
Health care home
- IMD
Index of Multiple Deprivation
- M3
Measuring Multimorbidity Index
- NGO
Non-governmental organisation
- NP
Nurse Practitioner
- PHO
Primary Health Organisation; all general practices belong to a PHO, which contracts to a DHB to provide primary care services
- Q5
Quintile 5 (most deprived) on NZ Deprivation Index
- RN
Registered nurse
- SSRI
Selective serotonin re-uptake inhibitor; a widely used category of antidepressant
- VLCA
Very low cost access; practice with higher subsidies and lower fees
Authors’ contributions
NS, TK, TL jointly designed the study, led analysis and interpretation, and wrote the final manuscript. KH, JC, JM, SH and co-investigators, and others, listed below contributed to study design and methods; data collection, analysis and interpretation; and review of the manuscript.
Funding
The project was funded by the New Zealand Ministry of Health via a competitive Request for Proposal managed by the Health Research Council of New Zealand. Grant reference HRC 18/788. The funders provided a Steering Committee to guide us in terms of what were the most policy-relevant issues to pursue, and to facilitate access to people and data. They had no role in collection, analysis or interpretation of data, nor in any decision about publication.
Availability of data and materials
Data for this project were collected on condition of anonymity of patients, practices and PHOs, with an agreement to delete data once the purpose of the project was met. Data collected from practices and PHOs are not available. Data collated from national data sets is available in summary form on request to author TK (t.kenealy@auckland.ac.nz).
Declarations
Ethics approval and consent to participate
Ethics approval was granted by the Massey University Human Ethics Committee: Human Ethics Southern A Committee, reference SOA 18/58. The research was conducted in accordance with New Zealand National Ethical Standards, which are based on two sets of principles: Te Ara Tika principles and bioethics principles. Te Ara Tika is a set of Māori ethical principles that draws on a foundation of tikanga (Māori protocols and practices). The quantitative data were all collected anonymously so that no individual consent was required.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nicolette Sheridan, Email: n.sheridan@massey.ac.nz.
The Primary Care Models Study Group:
Tim Stokes, Nelson Aguirre-Duarte, Bruce Arroll, Carol Atmore, Peter Crampton, Anthony Dowell, Tana Fishman, Robin Gauld, Matire Harwood, Gary Jackson, Rawiri Jansen, Ngaire Kerse, Debra Lampshire, Jayden MacRae, John Øvretveit, Teuila Percival, Roshan Perera, Martin Roland, Debbie Ryan, Jacqueline Schmidt-Busby, and Maria Stubbe
References
- 1.Reid P. Structural reform or a cultural reform? Moving the health and disability sector to be pro-equity, culturally safe, Tiriti compliant and anti-racist. N Z Med J. 2021;134:7–10. [PubMed] [Google Scholar]
- 2.Smith LT. Decolonizing Methodologies. Research and Indigenous Peoples 2nd ed. London: Zed Books; 2012.
- 3.Ramsden IM. Cultural Safety and Nursing Education in Aotearoa and Te Waipounamu. Unpublished doctoral thesis. Wellington: Victoria University of Wellington; 2002.
- 4.Durie M. Whaiora. Māori health and development. 2nd ed. Auckland: Oxford University Press; 2007.
- 5.Docherty B, Sheridan N, Kenealy T. Painting a new picture for practice nurses in a capitated environment: who holds the brush? N Z Med J. 2008;121:11–4. [PubMed] [Google Scholar]
- 6.Kenealy T, Kenealy H, Arroll B, Scott D, Scragg R, Simmons D. Diabetes care by General Practitioners in South Auckland: changes from 1990 to 1999. NeN Z Med J. 2002;115:U219–225. [PubMed] [Google Scholar]
- 7.Walker L, Clendon J, Nelson K. Nursing roles and responsibilities in general practice: three case studies. J Prim Health Care. 2015;7:236–43. [PubMed] [Google Scholar]
- 8.King A: The Primary Health Care Strategy. Wellington: Ministry of Health; 2001.
- 9.Nurse Practitioners in New Zealand [https://www.health.govt.nz/system/files/documents/pages/nurse-practitioners-in-new-zealand.pdf] Accessed on 10 Sep 2022
- 10.Nursing Council of New Zealand: Pūrongo ā-Tau 2020 mō te tau ka mutu i te 31 Poutūterangi. 2020 Annual Report for the year ended 31 March. Wellington: Nursing Council of New Zealand; 2020.
- 11.Hewitt SL, Sheridan NF, Hoare K, Mills JE. Understanding the general practice nursing workforce in New Zealand: an overview of characteristics 2015–19. Aust J Prim Health. 2021;27:22–9. [DOI] [PubMed] [Google Scholar]
- 12.Nursing Council of New Zealand: The New Zealand Nursing Workforce: A profile of Nurse Practitioners, Registered Nurses and Enrolled Nurses 2018–2019. Wellington: Te Kaunihera Tapuhi o Aotearoa / Nursing Council of New Zealand; 2019.
- 13.Medicines (Designated Prescriber – Registered Nurses) Notice 2022 [https://gazette.govt.nz/notice/id/2022-gs1892] Accessed on 28 Aug 2022
- 14.Sheridan N, Love T, Kenealy T. Primary Care Models Study Group: Is there equity of patient health outcomes across models of general practice in Aotearoa New Zealand? A national cross-sectional study. Int J Equity Health. 2023;22:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chan WC, Papaconstantinou D, Lee M, Telfer K, Jo E, Drury PL, Tobias M. Can administrative health utilisation data provide an accurate diabetes prevalence estimate for a geographical region? Diabetes Res Clin Pract. 2018;139:59–71. [DOI] [PubMed] [Google Scholar]
- 16.Exeter DJ, Zhao J, Crengle S, Lee A, Browne M. The New Zealand Indices of Multiple Deprivation (IMD): A new suite of indicators for social and health research in Aotearoa. New Zealand PLoS One. 2017;12:e0181260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stanley J, Sarfati D. The new measuring multimorbidity index predicted mortality better than Charlson and Elixhauser indices among the general population. J Clin Epidemiol. 2017;92:99–110. [DOI] [PubMed] [Google Scholar]
- 18.Health Care Home Collaborative: Health Care Home Model of Care Requirements. Wellington: Health Care Home Collaborative; 2017.
- 19.Estimated population of NZ [https://www.stats.govt.nz/indicators/population-of-nz] Accessed on 22 Feb 2023
- 20.People aged 65 years and over dispensed five or more unique long term medications [https://nsfl.health.govt.nz/system/files/documents/pages/slm_ahbd_polypharmacy_people_aged_65_years_and_over_dispensed_five_or_more_unique_long_term_medications.pdf] Accessed on 26 Sep 2022
- 21.RStudio Team. RStudio: Integrated Development for R. Boston: RStudio Inc; 2019.
- 22.R Core Team. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2020.
- 23.Sheridan NF, Kenealy TW, Connolly MJ, Mahony F, Barber PA, Boyd MA, Carswell P, Clinton J, Devlin G, Doughty R, Dyall L, Kerse N, Kolbe J, Lawrenson R, Moffitt A. Health equity in the New Zealand health care system: a national survey. Int J Equity Health. 2011;10:45. [DOI] [PMC free article] [PubMed]
- 24.Lukewich J, Asghari S, Marshall EG, Mathews M, Swab M, Tranmer J, Bryant-Lukosius D, Martin-Misener R, Norful AA, Ryan D, Poitras ME. Effectiveness of registered nurses on system outcomes in primary care: a systematic review. BMC Health Serv Res. 2022;22:440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Laurant M, van der Biezen M, Wijers N, Watananirun K, Kontopantelis E, van Vught AJ: Nurses as substitutes for doctors in primary care. Cochrane Database Syst Rev 2018, 7:CD001271. [DOI] [PMC free article] [PubMed]
- 26.ACC1520 – March 2021 Medical practitioners’, nurses’ and nurse practitioners’ costs [https://www.acc.co.nz/assets/provider/med-nurses-pracs-costs-may2021-acc1520.pdf ] Accessed on 2 Oct 2022
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data for this project were collected on condition of anonymity of patients, practices and PHOs, with an agreement to delete data once the purpose of the project was met. Data collected from practices and PHOs are not available. Data collated from national data sets is available in summary form on request to author TK (t.kenealy@auckland.ac.nz).