Abstract
Background
Dysphagia, a common complication of acute stroke, is associated with increased mortality and morbidity. Acupuncture, a widely used swallowing therapy in China, has been suggested as an effective therapy for treating Post-Stroke Dysphagia (PSD) by recent meta-analyses and guidelines. The use of resting-state functional Magnetic Resonance Imaging (rs-fMRI) and Diffusion Tensor Imaging (DTI) could explore the change of regional spontaneous neural activity, functional relationships between brain regions, and white matter connectivity patterns after acupuncture intervention for PSD. This trial aims to evaluate the efficacy of acupuncture treatment for PSD and explore its central mechanism by neuroimaging.
Methods/design
This randomized controlled trial will recruit 40 PSD patients. All patients will be randomized to either the Real Acupuncture (RA) or Sham Acupuncture (SA) group by a ratio of 1:1. All patients will receive immediate acupuncture treatment in the MRI scanning room, followed by four weeks of long-term acupuncture treatment. The primary outcomes are the rs-fMRI and DTI indicators, which will be evaluated after the immediate and long-term acupuncture treatment. The secondary outcomes are the scales that assess the efficacy, including the Functional Oral Intake Scale (FOIS), Water Swallowing Test (WST), Swallowing Quality Of Life Questionnaire (SWAL-QOL), and National Institute of Health Stroke Scale (NIHSS). The modified version of the Massachusetts General Hospital Acupuncture Sensation Scale (M-MASS) and fMRI sensation record table will also be evaluated.
Discussion
This protocol presents the design of a randomized, single-blind trial that will evaluate the efficacy and explore the neural plasticity of acupuncture treatment for PSD. This trial will deepen our insight into the clinical value of acupuncture for PSD and initially probe into the time-dosage-effect mechanism of acupuncture.
Trial registration numbers
Chinese Clinical Trial Registry (www.chictr.org.cn) ChiCTR2300067480. This study was registered on 9th January 2023.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12906-024-04657-1.
Keywords: Acupuncture, Dysphagia, Resting-state functional magnetic resonance imaging, Diffusion tensor imaging
Background
Dysphagia, a common complication of acute stroke, occurs in 37–78% of stroke patients [1]. Post-stroke dysphagia (PSD) is associated with poor outcomes, including increased mortality and morbidity due in part to aspiration, pneumonia, and malnutrition [2–4]. PSD is also associated with increased length of hospital stay and higher hospital costs. Stroke patients with dysphagia were 33.2% more likely to be transferred to the post-acute care facility and 1.7 times more likely to die in the hospital [5].
Acupuncture, a widely used swallowing therapy in China [6], has been recommended as an adjunctive treatment for dysphagia by Guidelines for adult stroke rehabilitation and recovery (Class: IIb, Level of Evidence: B) [7]. Although a number of clinical studies have shown that acupuncture could improve the swallowing function of stroke patients [8, 9], the cerebral mechanism of acupuncture treatment for PSD is still unclear.
Previous mechanism studies on acupuncture for PSD were primarily aimed at the single acupoint rather than acupuncture prescription, which was more commonly used in clinical practice [10]. Si Yuan et al. suggested acupuncture at Lianquan (CV23) could regulate the excitatory neurons in the paraventricular hypothalamus [11]. Meanwhile, Lulu Yao et al. demonstrated that electrical stimulation at the CV23 acupoint could improve the swallowing function in PSD model mice through the activation of motor cortex inputs to the nucleus tractus solitarii through the parabrachial nuclei [12]. However, the various types of acupuncture and the unknown clinical efficacy of single acupoint in existing studies resulted in inconsistent conclusions. In addition, the duration, times, and repetition intervals of treatment, vital parts of acupuncture dosage, could significantly impact the accumulated acupuncture efficacy. The mechanism of transient and accumulated acupuncture effect could be the key to exploring the mechanism of acupuncture effectiveness [13].
Resting state-functional Magnetic Resonance Imaging (rs-fMRI), a useful method for exploring the spatial localization of changes in neuronal activity [14], could help assess the prognosis and recovery of PSD [15]. fMRI studies have shown that dysphagia may be related to the neuronal activity in several distinct brain areas, including precentral gyrus, postcentral gyrus, insula, inferior frontal gyrus, cingulate cortex, pontine, medial medullary, and lateral medullary lesions [16, 17]. Meanwhile, white matter is critical in the neural control of swallowing [18]. Diffusion Tensor Imaging (DTI), a non-invasive imaging method, is developed based on diffusion-weighted imaging to study white matter fiber bundle injury [19]. White matter areas commonly implicated in swallowing control included the pyramidal tract, internal capsule, corona radiata, superior longitudinal fasciculus, external capsule, and corpus callosum [20]. Moreover, the adaptation of white matter can facilitate dysphagia recovery. Therefore, it is of fundamental and clinical significance to explore the neuroplasticity of acupuncture based on the above two neuroimaging techniques.
Imaging techniques, including fMRI and DTI, have been widely used in the studies of the acupuncture mechanism. The activation and functional connectivity network of specific brain areas have been suggested as closely related to the mechanism of acupuncture, and central integration plays a critical role in the acupuncture mechanism [21–23]. For instance, a DTI study showed that the mechanism of acupuncture treatment for poststroke dyskinesia might be closely related to the rehabilitation of the forceps minor [24]. However, most fMRI studies only respectively focused on the effect of the immediate or long-term intervention, which failed to investigate the relationship between immediate and long-term effects of acupuncture at the same acupoint or prescription. The mechanisms of potential associations and differences between immediate and long-term acupuncture effects, which should be an essential part of the mechanism of the dosage of acupuncture, remain unexplained.
Therefore, this randomized controlled trial with fMRI and DTI will evaluate the efficacy of acupuncture for PSD and explore the neural plasticity of immediate and long-term acupuncture treatment in improving swallowing function for PSD patients.
Methods/design study design
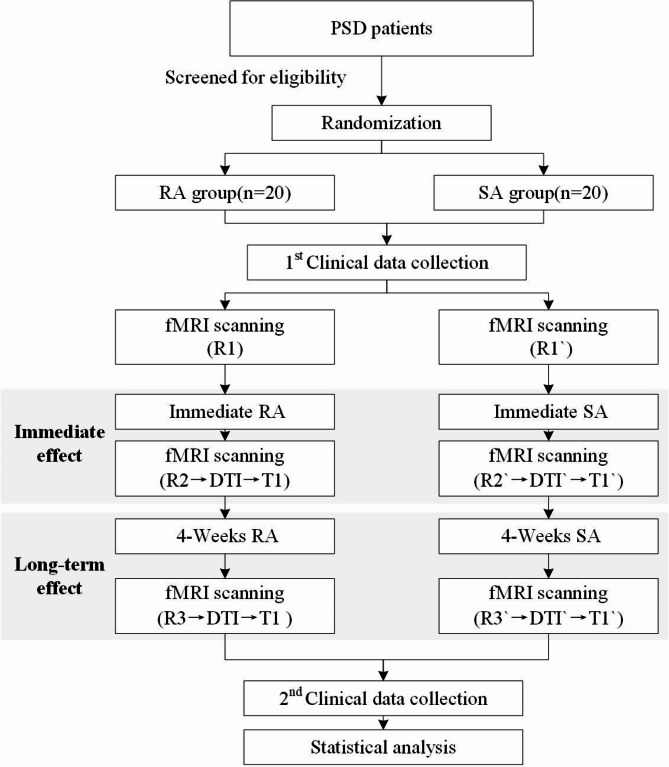
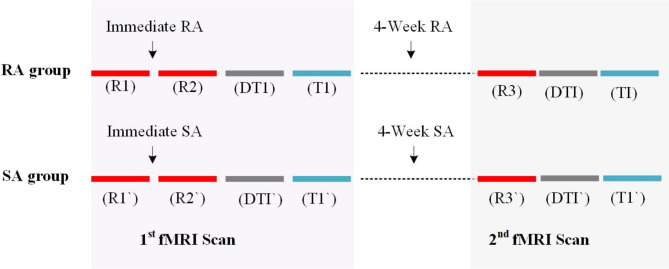
This is a randomized, single-blind, sham-controlled study with rs-fMRI and DTI. This protocol is under the Standard Protocol Items: Recommendations for Intervention Trials (SPIRIT) guidelines. Figures 1 and 2 provide the detailed information of the study design.
Fig. 1.
Flowchart of the trial. Legend: PSD, Post-Stroke Dysphagia; RA, Real Acupuncture; SA, Sham Acupuncture. fMRI, functional Magnetic Resonance Imaging
Fig. 2.
Scanning diagram. Legend: RA, Real Acupuncture; SA, Sham Acupuncture. fMRI, functional Magnetic Resonance Imaging
Recruitment
The study is carried out from October 2021 to September 2025 at the First Teaching Hospital of Tianjin University of Traditional Chinese Medicine (TUTCM). PSD patients will be recruited from the outpatient and inpatient departments.
Inclusion criteria
Patients who meet all of the following criteria will be included.
(1) Meet the diagnostic criteria for ischemic stroke [25] and dysphagia [26];
(2) Course of ischemic stroke between 1 and 6 months;
(3) The Water Swallowing Test (WST) levels ranged from 3 to 5;
(4) Age between 40 and 80 years;
(5) Chinese native speaker;
(6) Right-handed according to the Edinburgh handedness inventory [27];
(7) Vital signs are stable and able to cooperate with the study;
(8) Participants or legal representatives sign the informed consent form voluntarily.
Exclusion criteria
Patients who meet any of the following criteria will be excluded.
(1) Dysphagia caused by other diseases (for example, head and neck cancer, oropharyngeal diseases, and so on);
(2) Dysphagia existed before the onset of this ischemic stroke;
(3) Expected to live for less than three months;
(4) With medullary injury;
(5) Suffering from cerebral hemorrhage, brain tumor, and other diseases resulting in abnormal brain MRI structure;
(6) Have contraindications to MRI scans, such as implanted metal, cochlear implants, or claustrophobia;
(7) Self-rating anxiety scale [28] scores ≥ 50 or self-rating depression scale [29] scores ≥ 50;
(8) Received acupuncture treatment within one week.
Withdrawal criteria
Subjects with any of the conditions listed below will be withdrawn.
Poor compliance, unwillingness to continue in the study, or voluntary withdrawal;
Severe adverse reactions, complications, or disease deterioration, making continuation unsuitable;
Did not adhere to the treatment protocol or had insufficient observation data, which influenced the assessment.
Sample size calculation
There is currently no precise method for estimating the sample size of acupuncture-related neuroimaging clinical trials. According to internationally recognized reviews, the sample size for each group should be at least 12 cases [30, 31]. Considering data loss and exclusion from later data analysis, this trial will require 20 subjects per group, for a total of 40 cases.
Randomization
Eligible subjects will be randomly divided into the Real Acupuncture (RA) group and Sham Acupuncture (SA) group in a 1:1 ratio using the minimization method. The factors related to fMRI and the prognosis of PSD, such as gender, age, and education, will be balanced.
Blinding
Participants will be blinded. In addition, they will be asked to guess their group, with options including RA group, SA group, and uncertain at the end of the study. All the participants will be separated into different cubicles to avoid communication during the intervention. Due to the particularity of acupuncture, acupuncturists will not be blinded. All outcome assessors and statistical analysts will be blinded to randomization assignment and intervention.
Interventions
Trained and certified acupuncturists with at least three years of experience will deliver interventions. Subjects in both groups will receive immediate acupuncture followed by 4-week of long-term acupuncture. Both the RA and SA treatments comprise 12 sessions (three sessions per week). In the MRI scanning room, immediate acupuncture will be performed with silver acupuncture needles (0.35 × 75 mm/ 0.30 × 40 mm, Hwato brand, Suzhou Medical Supplies Factory Co. LTD, Suzhou, China). The 4-week acupuncture will be performed in the outpatient room with disposable sterile acupuncture needles (0.30 × 75 mm /0.25 × 40 mm, Hwato brand, Suzhou Medical Supplies Factory Co. LTD, Suzhou, China.
RA group
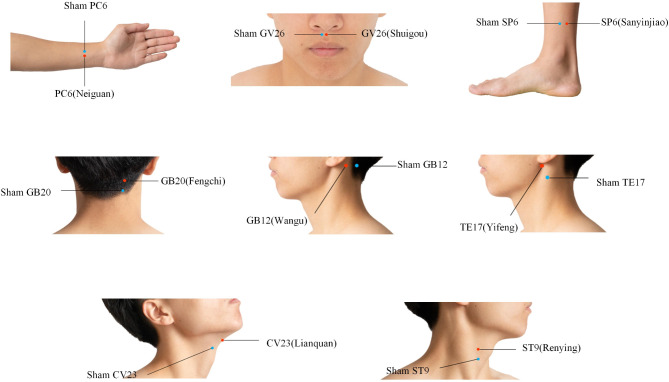
Patients in the RA group will receive acupuncture on the bilateral Neiguan (PC6), Shuigou (GV26), affected side Sanyinjiao (SP6), and bilateral Fengchi (GB20), Wangu (GB12), Yifeng (TE17), Lianquan (CV23), Renying (ST9), and Yanhoubi (Posterior pharyngeal wall). The locations of acupoints are shown in Table 1; Fig. 3.
Table 1.
Allocation of acupoints and Sham-acupoints
| Acupoints | Real Acupoints Location | Sham Acupoints Location |
|---|---|---|
| PC6 (Neiguan) | In the anterior area of the forearm, between the palmar longus tendon and the flexor carpi radialis tendon, and 2 cun (≈ 50 mm) above the transverse striae of the volar side of the wrist. | In the anterior area of the forearm, the radial side of the flexor carpi radialis tendon and 2 cun (≈ 50 mm) above the transverse striae of the volar side of the wrist. Avoid the PC(pericardium meridian of hand-jueyin), LU(lung meridian of hand-taiyin), and the median nerve. |
| GV26 (Shuigou) | On the face, the intersection of the upper 1/3 and the lower 2/3 of the philtrum. | On the face, under the right nostril, and 0.5 cun(≈ 15 mm) near the level of the intersection of the upper 1/3 and the lower 2/3 of the philtrum. Avoid ST(stomach meridian of foot-yangming) and CV(conception vessel). |
| SP6 (Sanyinjiao) | On the inner side of the Shank, the posterior medial edge of the tibia, and 3 cun(≈ 75 mm) above the tip of the medial malleolus. | On the inner side of the Shank, the midpoint of the medial tibia, and 3 cun(≈ 75 mm) above the tip of the medial malleolus. Avoid ST, SP(spleen meridian of foot-taiyin), the saphenous vein, and the saphenous nerve) |
| GB20 (Fengchi) | In the posterior region of the neck, under the occiput, in the depression between the upper part of the sternocleidomastoid muscle and the upper part of the trapezius muscle. | In the posterior region of the neck, on the outside edge of the trapezius muscle, level with the upper edge of the second cervical spine and the BL10(Tianzhu)point, and 1.5 cun(≈ 40 mm) beside the posterior midline. Avoid GB(gallbladder meridian of foot-shaoyang), BL(bladder meridian of foot-taiyang), and the greater occipital nerve. |
| GB12 (Wangu) | On the neck, at the posterior and inferior depression of the mastoid process behind the ear. | On the neck, at the level of the GB12(Wangu)point and 2.25 cun (≈ 57.5 mm) away from the back midline. Avoid the TE(triple energizer meridian of hand-shaoyang), GB, EX-HN14(Yiming)point, Anmian point, and the lesser occipital nerve. |
| TE17 (Yifeng) | On the neck, behind the earlobe, at the anterior and inferior depression of the mastoid process. | On the sternocleidomastoid muscle of the neck, level with the mandibular angle, and the midpoint of the line between TE16(Tianyou) and SI17(Tianrong). Avoid GB, SI(small intestine meridian of hand-taiyang ), and the great auricular nerve. |
| ST9 (Renying) | On the neck, level with the laryngeal prominence, at the anterior edge of the sternocleidomastoid muscle and the pulsation of the common carotid artery | On the neck, at the anterior edge of the sternocleidomastoid muscle and 1cun above the laryngeal prominence. Avoid ST and the transverse nerve of the neck. |
| CV23 (Lianquan) | In the anterior region of the neck, on the anterior median line, above the laryngeal prominence, and in the depression of the upper edge of the hyoid bone. | In the anterior region of the neck, above the laryngeal prominence, and in the depression on the right side of the lower edge of the hyoid bone, 1 cun (≈ 25 mm) is beside the anterior midline. Avoid CV and the transverse nerve of the neck. |
| Posterior pharyngeal wall (Yanhoubi) |
Fig. 3.
Location of Acupoints and Sham-acupoints
The inserted depth of acupoints are various: PC6 at a depth of 0.5-1.0 cun (≈ 15–25 mm), GV26 at a depth of 0.3–0.5 cun (≈ 9–15 mm), SP6 at a depth of 1.0-1.5 cun (≈ 25–40 mm), GB20 and CV23 at a depth of 2.5-3 cun (≈ 65–75 mm), GB12 and TE17 at a depth of 2-2.5 cun (≈ 50–65 mm), and ST9 at a depth of 0.5-1.0cun (≈ 15–25 mm). After needles enter the skin, using lifting-thrusting, twirling-rotating, and sparrow pecking-like manipulation to obtain the sensation of “deqi”. Then, use five needles to prick Yanhoubi 3–5 times until there is a small amount of bleeding, and remove the needle as soon as bleeding onset. For immediate acupuncture, no needles were retained. For 4-week acupuncture, all needles will be retained in the acupoints (except Yanhoubi) for 30 min.
SA group
Since the depth of some acupoints in our study cannot be reached by Streitberger’s sham needle, we chose the blinding design of the non-acupoint shallow needling method [32–34]. This method has been used in many published high-quality randomized controlled trials [35–37]. The SA group will receive a superficial skin penetration at sham acupoints without manipulation for “deqi”. Sham acupoints are located beside the meridians and anatomical locations associated with dysphagia to avoid the therapeutic effect. Five blunt needles together will be used to prick Yanhoubi 3–5 times without bleeding and needle retention. Table 1 and Fig. 3 provide the locations of acupoints in SA group.
Basic treatment
During the 4-week acupuncture, all participants will receive basic treatment, including regular drugs for stroke treatment and swallowing rehabilitation training. The application of drugs is according to the Chinese Guidelines for the Diagnosis and Treatment of Acute Ischemic Stroke 2018 [38] and the Chinese Guidelines for Secondary Prevention of ischemic stroke and transient ischemic attack 2014 [39]. Swallowing rehabilitation training, which will be applied three sessions per week for four consecutive weeks, includes diet modification, texture modification of food and fluid, and adjustment of swallowing postures [40, 41].
Functional MRI and DTI data acquisition
DTI and fMRI scannings use a 3.0T MRI scanner (Siemens 3T Skyra MR, Muenchen, Germany) equipped with a standard 16-channel head coil. A 3-dimensional T1-weighted sequence will be used to gain the high-resolution structural image. The parameters of T1 are as follows: Repetition Time (TR) /Echo Time (TE) = 2000 ms/1.97 ms, flip angle = 8°, number of excitation = 0.5, Field of View (FOV) = 256 mm ×256 mm, data matrix = 256 × 256, slice thickness = 1 mm, gap = 0 mm, slices = 192. The Blood Oxygenation Level-Dependent (BOLD) rs-fMRI will be obtained with the Gradient-Recalled Echo-Planar Imaging (GRE-EPI) sequence. The parameters of fMRI are as follows: TR/TE = 2000 ms /30 ms, flip angle = 90°, FOV = 220 mm ×220 mm, data matrix = 64 × 64, slice thickness = 3 mm, gap = 3 mm, slices = 37. For DTI, a whole brain diffusion-weighted single-shot spin-echo EPI sequence was applied. The parameters of DTI are as follows: TR/TE = 2000ms /1.97ms, FOV = 256 mm×256 mm, data matrix = 128 × 128, NEX = 2, slice thickness = 1.0 mm, with diffusion gradients (b-value = 1000s/mm2) applied in 20 non-collinear directions and one image without diffusion weighting (i.e., b-value = 0).
24 h hours before scanning, subjects will be asked to keep a regular lifestyle and avoid drinking alcohol, coffee, and tea. Before the MRI, subjects will calmly stay in a restroom for 15–20 min. During canning, foam earplugs and sponge pads will be used to isolate noise and reduce head movement, respectively. Subjects will be asked to close their eyes, stay awake, keep their bodies still, and think less. If subjects experience unbearable discomfort during the scan, the scan will be suspended immediately.
Outcome measure
Primary outcomes
The primary outcomes are the fMRI and DTI indicators, including:
fMRI
(1) Regional Homogeneity (ReHo).
ReHo is based on Kendall’s coefficient concordance to measure the similarity of the time series of a given voxel to those of its nearest neighbors in a voxel-wise way [42]. It has been applied to characterize the local spontaneous neural activity alternations in neuropsychiatric disorders as well as in the studies of the central effects of acupuncture [43–45].
(2) Amplitude of Low-Frequency Fluctuation (ALFF).
ALFF measures the average amplitude of fluctuations in the low-frequency range, which is considered a valid method for studying the signal characteristics of single voxels or local brain regions reflecting the spontaneous neural activity of the cerebral cortex [46, 47]. It has been widely used to study the spontaneous activity of the human brain in various situations [48, 49].
(3) Fractional Amplitude of Low-Frequency Fluctuation (fALFF).
fALFF is an improved ALFF analysis method. fALFF approach can successfully suppress the physiological noise in the cisterns and ventricles found by ALFF. It is sensitive and specific in detecting spontaneous brain activities [50].
(4) Percent Amplitude of Fluctuation (PerAF).
PerAF measures the percentage of BOLD fluctuations relative to the mean BOLD signal intensity for each time point and averages across the whole time series. Compared to ALFF, PerAF is a scale-independent method. And it also avoids confounding mixtures from voxel-specific fluctuation amplitude in fALFF [51].
(5) Functional Connectivity (FC).
FC is defined as the temporal correlation of a neurophysiological index measured in different brain areas [52]. It depicts the relationship between the neuronal activity patterns of anatomically separated brain regions, reflecting the level of functional communication between regions [53]. We will use FC to explore the crucial part that functional communication plays in acupuncture therapy.
DTI
Fractional Anisotropy (FA).
FA, one of the quantitative values of anisotropic diffusion provided by DTI, can detect subtle changes in the diffusion characteristics of white matter [54, 55]. Youngkook Kim et al. suggested that the initial FA value of the frontal operculum could be related to the dysphagia outcome [56] and supported the role of the affected FA from the frontal operculum in predicting poststroke dysphagia. The lowest FA values are indicative of non-white matter tissue in healthy brains [57].
-
(2)
Mean Diffusivity (MD).
MD is a measure of the diffusion degree and is independent of direction. It is positively associated with free water molecules in the tissue [19]. In addition, MD quantifies cellular and membrane density, whereas an increase in MD indicates disease processes such as edema or necrosis [58].
Secondary outcomes
The secondary outcomes contain the efficacy-related scales, the Modified version of the Massachusetts General Hospital Acupuncture Sensation Scale (M-MASS), and the fMRI sensation record table. Efficacy-related scales will be evaluated before and after 4-weeks of treatment. The M-MASS and fMRI sensation record table will be completed at the end of each fMRI scanning.
(1) The efficacy-related indicators
Functional Oral Intake Scale (FOIS), WST, Swallowing Quality of Life Questionnaire (SWAL-QOL), and National Institute of Health Stroke Scale (NIHSS) will be evaluated.
FOIS is a commonly used scale in PSD studies [59–61]. Studies have shown it is suitable for assessing and documenting changes in functional eating ability in stroke patients over time [62]. WST is a standardized test used worldwide to screen dysphagia and detect aspiration [63]. It will be used with FOIS for a more comprehensive assessment of swallowing ability. SWAL-QOL is to evaluate the swallowing-related quality of life after stroke. It exhibited excellent internal consistency, reliability, and short-term reproducibility in clinical practice [64]. We use it to observe the effectiveness of acupuncture in improving patient quality of life. NIHSS, an easy, quick, and valid scale with high intra-observer and inter-observer reliability, is widely used in China and abroad [65, 66]. We will use it to evaluate the extent of neurological deficit and disease development.
(2) M-MASS
It is a scale designed to measure the sensations evoked by acupuncture stimulation [67]. Research has proven that it is a reliable and effective tool for reporting acupuncture-related sensations [68], and it has developed several versions [68, 69]. Since “Tong Guan Li Qiao” acupuncture therapy requires some special “deqi” feelings of acupuncture, we will use the modified MASS, which adds the sensation of the stick in the throat, muscle twitch, distal radiating, and tearful eyes to evaluate the patient’s perception; the sensation of bleeding, needle end swinging, heaviness, tightness, rough, and blocked to evaluate the acupuncturist’s perception (Supplementary material).
(3) Sensation record
Considering that the fMRI scanning process is easily affected by subjective thinking and psychological activities, this study will record the sensations, including somatesthesia, psychological state, and thinking activities of subjects during the scanning to explore the influence of various factors on the test results (Supplementary material ).
Data management
Clinical data will be managed with the clinical research data management system of the TUTCM. The third-party inspection company Beijing Zhonglian Leadian Pharmaceutical Technology Co., Ltd. will supervise the study and monitor data regularly.
Data analysis
Imaging data analysis
The fMRI data will be preprocessed using SPM12 (https://www.fil.ion.ucl.ac.uk/spm/) and REST plus V.1.25 (http://restfmri.net/forum/restplus) with Matlab 2018 (R2018; MathWorks, Inc., Natick, MA). Data preprocessing includes the first ten time points removed, slice time correction, realignment, spatial normalization in Montreal Neurological Institute (MNI) space and resampled at 3 mm × 3 mm × 3 mm voxel size, spatial smooth with a 6 mm full width at half maximum Gaussian kernel, detrend, nuisance covariates regression, and filtering. After standard preprocessing, ReHo, ALFF, fALFF, and PerAF analysis will be calculated to explore brain activity. Two sample Students’ t-test and paired Students’ t-test will be conducted respectively to examine the difference in acupuncture-related central responses between groups and within groups. The results will be corrected by Gaussian Random Field Theory (voxel-level P < 0.05, cluster-level P < 0.05).
TBSS processing of DTI images was performed using the FMRIB Software Library (FSL; ver. 5.0.9; https://www.fmrib.ox.ac.uk/fsl). Firstly, data format conversion, head moving eddy current correction, gradient direction correction, scalp peeling, and brain area extraction will be processed, following the creation of the FA and MD parameters. And then, conduct the image registration and build the mean FA/MD image and mean FA/MD skeleton. Finally, permutation tests by randomized order and multiple comparison correction by threshold-free cluster enhancement (TFCE) order will be conducted [70].
Clinical data analysis
The analysis will be based on the modified Intention-To-Treat analysis (mITT). SPSS software (V.25.0. Armonk, NY. IBM Corp.) will be used for statistical analysis. Normally-distributed continuous variables will be expressed by mean ± standard deviation ( ). Non-normally distributed continuous variables will be expressed by median and quartile [M (P25, P75)]. Two sample Students’ t test will be used for normally distributed continuous variables, the Mann-Whitney U-test will be used for non-normally distributed variables, and paired Students’ t test will be used to compare changes within groups. Categorical variables will be described as frequencies or percentages. The chi-square test or Fisher’s exact probability method will be used to compare the unordered categorical variables, and the Kruskal-Wallis H rank sum test will be used for ordered categorical variables.
). Non-normally distributed continuous variables will be expressed by median and quartile [M (P25, P75)]. Two sample Students’ t test will be used for normally distributed continuous variables, the Mann-Whitney U-test will be used for non-normally distributed variables, and paired Students’ t test will be used to compare changes within groups. Categorical variables will be described as frequencies or percentages. The chi-square test or Fisher’s exact probability method will be used to compare the unordered categorical variables, and the Kruskal-Wallis H rank sum test will be used for ordered categorical variables.
Furthermore, we will conduct a correlation analysis between FOIS/WST/M-MASS scales and DTI/rs-fMRI indicators. Depending on whether the data meet the normality test and linear relationship, we will choose the Pearson correlation coefficient or Spearman correlation coefficient for analysis. All data will be analyzed using SPSS software (V.25.0. Armonk, NY. IBM Corp.). P value < 0.05 will be considered significant. Finally, we will use Stata/MP software (V17.0 USA) to calculate Bang’s blinding index to evaluate the implementation of the blinding.
Patient safety
Any Adverse Events (AEs) or Serious Adverse Events (SAEs) that occurred during the intervention, whether or not related to the intervention, will be recorded in detail. Researchers will judge the relevance of AEs/SAEs and treatment based on information such as the cause, time, and process. Common acupuncture-related AEs include fainting, stuck needles, broken needles, bent needles, bleeding, edema, and other minor AEs will be treated by the attending acupuncturist immediately. For SAEs, such as stroke recurrence or organ damage, researchers will immediately stop the treatment and send the patient to the emergency department. The research team will bear treatment costs. SAEs will be reported to the ethics committee within 24 h.
Dissemination
The study will comply with the declaration of Helsinki principles (World Medical Association version, 2013). All participants will voluntarily sign an informed consent form before participating in this trial. The study has been registered at the Chinese Clinical Trial Registry (ChiCTR2300067480). Study results will be disseminated by publication in a peer-reviewed medical journal and made available via open access.
Discussion
This protocol presents an objective design of a randomized, single-blind trial that will evaluate the efficacy and explore the neural plasticity of acupuncture treatment for PSD. This trial will be the first neuroimaging study to explore the immediate and long-term effect of practical acupuncture prescription, rather than single acupoint, for PSD. The combination of DTI and rs-fMRI results could examine the improvement of white matter microstructure and gray matter function after acupuncture treatment. Combined with the results of acupuncture efficacy for PSD, this trial will initially probe into the time-dosage-effect mechanism of acupuncture.
Acupuncture, one of the most common alternative and complementary therapies worldwide, has been recommended for treating musculoskeletal tissue, connective tissue, and neurological disorders [71]. Acupuncture treatment dosage, including duration, repetition intervals, and the number of treatments, could differ significantly and impact the treatment effect [13]. The effect of long-term acupuncture treatment could be a cumulative result containing each transient acupuncture effect, which should be an essential part of the mechanism of the acupuncture dosage. Therefore, this study will explore the neural plasticity of transient and accumulated acupuncture effect on PSD and evaluate the efficacy of acupuncture for PSD in order to probe into the time-dosage-effect mechanism of acupuncture treatment.
In this study, the conclusion will be based on outcomes from rs-fMRI, DTI, and the scales for assessment of swallowing function. The relationship among the improvement of white matter microstructure, gray matter function, and swallowing function will be explored, which may provide more evidence for the mechanisms of acupuncture effectiveness on PSD. Rs-fMRI, a novel paradigm that examines spontaneous brain function without a task, could detect spatially distributed networks of temporal synchronization and characterize resting-state networks [72]. Moreover, an increasing number of studies [73, 74] suggested the correlations between resting-state network alterations and disease progression and severity. In addition, white matter is critical in the neural control of swallowing. DTI, a sensitive marker of neuropathology, could measure and describe characteristics of white matter, such as FA and MD. It could help identify specific white matter tracts of interest for swallowing control [75, 76]. The correlation analysis of FOIS/WST/M-MASS and DTI/rs-fMRI indicators could reveal the relationship between swallowing function, acupuncture sensation, and the improvement of white matter microstructure and gray matter function after acupuncture treatment.
Moreover, previous fMRI studies [11, 77, 78] usually select single or local acupoints for acupuncture to observe the mechanism of its effectiveness on PSD. However, single or local acupoints are rarely used alone in clinical practice, and their efficacy in improving swallowing function lacks clinical validation. Therefore, we chose “Tong Guan Li Qiao” acupuncture therapy with strict and detailed operation standards as the acupuncture prescription for RA group. Our team’s previous research has shown that “Tong Guan Li Qiao” acupuncture therapy could improve PSD patients’ swallowing ability and quality of life [79].
In addition, a challenge for the clinical applications of rs-fMRI is the potentially confounding effect of aging or concomitant vascular diseases on the neurovascular coupling and, consequently, the fMRI response [72]. Therefore, the quality control approaches are the precondition for the result reliability: (1) Restriction on age, right-handedness, and area of infarction in the inclusion and exclusion; (2) Strict acupuncture operation by trained, certified acupuncturists with at least three years of experience; (3) Highly repeatable intervention based on detailed and strict acupuncture prescription, “Tong Guan Li Qiao” acupuncture therapy; (4) After the scanning process, patients were required to record sensation during scanning, including somatesthesia, psychological state, and thinking activities to explore the influence of various factors on the test results.
In summary, this randomized, single-blind trial with fMRI and DTI will evaluate the efficacy and explore the neural plasticity of acupuncture treatment for PSD. It will provide evidence for acupuncture efficacy on PSD and initially probe into the time-dosage-effect mechanism of acupuncture. In addition, quality control approaches will be adopted to increase the reliability of the results.
Trial status
This protocol is Version 2.0 (23rd April 2023). The first participant was included on 26th May 2023. The recruitment will be completed in approximately September 2025.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We sincerely thank the collaborating investigators, subjects, and their families for their support of the project.
Abbreviations
- PSD
Post-Stroke Dysphagia
- rs-fMRI
resting state-functional Magnetic Resonance Imaging
- DTI
Diffusion Tensor Imaging
- SPIRIT
Standard Protocol Items: Recommendations for Intervention Trials
- TUTCM
Tianjin University of Traditional Chinese Medicine
- WST
Water Swallowing Test
- RA
Real Acupuncture
- SA
Sham Acupuncture
- TR
Repetition Time
- TE
Echo Time
- FOV
Field of View
- BOLD
Blood Oxygenation Level-Dependent
- GRE-EPI
Gradient-Recalled Echo-Planar Imaging
- ReHo
Regional Homogeneity
- ALFF
Amplitude of Low-Frequency Fluctuation
- fALFF
fractional Amplitude of Low-Frequency Fluctuation
- PerAF
Percent Amplitude of Fluctuation
- FC
Functional Connectivity
- FA
Fractional Anisotropy
- MD
Mean Diffusivity
- M-MASS
Modified version of the Massachusetts General Hospital Acupuncture Sensation Scale
- FOIS
Functional Oral Intake Scale
- SWAL-QOL
Swallowing Quality of Life Questionnaire
- NIHSS
National Institute of Health Stroke Scale
- MNI
Montreal Neurological Institute
- mITT
modified Intention-To-Treat
- AEs
Adverse Events
- SAEs
Serious Adverse Events
Author contributions
WL, WYG, and QZ conceived, designed, and wrote this protocol. XNF is the guarantor of this review and approved the final manuscript. YBL, HBJ, KCL, and SJL provide the tables and figures. YZD, SW provided a clinical perspective, especially on manual acupuncture. LL, YS, JL, and SY provided the writing and modification of part of the article. XZJ, LR, and JHL assist with fMRI and DTI scanning, and data analysis.
Funding
This study is supported by Tianjin Science and Technology Plan Projects (No. 21JCZDJC00890), National Natural Science Foundation of China (No.82374578), and National Key R & D Program of China (No. 2018YFC1705004). This study has been peer-reviewed by independent reviewers by the funding body(Tianjin Municipal Science and Technology Bureau).
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Ethical approval was granted on 9th November 2022 and revised on 5th May 2023 by the Ethics Committee of First Teaching Hospital of Tianjin University of Traditional Chinese Medicine (Ethics Reference No: TYLL2022[K]No.032). All the participants will be given and signed a written consent form before being recruited into our study. In case of essential protocol modifications, a new version of the protocol with appropriate amendments will be submitted to the ethics committee for approval. Further studies may begin when the new protocol or changes to the existing protocol have been approved by the ethics committee. In addition, if administrative changes to the protocol are minor corrections and/or clarifications that have no effect on conducting the study, then these administrative changes will be agreed upon by the ethics committee, and will be documented in a memorandum. Substantive protocol amendments will also be transparently described in trial reports.
Consent for publication
Participants signed informed consent regarding publishing their photographs.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Wei Liu, Wenyi Ge and Qi Zhao contributed equally to this work.
References
- 1.Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36(12):2756–63. [DOI] [PubMed] [Google Scholar]
- 2.Cohen DL, Roffe C, Beavan J, Blackett B, Fairfield CA, Hamdy S, Havard D, McFarlane M, McLauglin C, Randall M, et al. Post-stroke dysphagia: a review and design considerations for future trials. Int J Stroke: Official J Int Stroke Soc. 2016;11(4):399–411. [DOI] [PubMed] [Google Scholar]
- 3.Wilkinson JM, Codipilly DC, Wilfahrt RP. Dysphagia: evaluation and collaborative management. Am Family Phys. 2021;103(2):97–106. [PubMed] [Google Scholar]
- 4.Smithard DG, Smeeton NC, Wolfe CD. Long-term outcome after stroke: does dysphagia matter? Age Ageing. 2007;36(1):90–4. [DOI] [PubMed] [Google Scholar]
- 5.Muehlemann N, Jouaneton B, de Léotoing L, Chalé JJ, Fernandes J, Kägi G, Sarikaya H, Arnold M. Hospital costs impact of post ischemic stroke dysphagia: database analyses of hospital discharges in France and Switzerland. PLoS ONE. 2019;14(1):e0210313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xie Y, Wang L, He J, Wu T. Acupuncture for dysphagia in acute stroke. Cochrane Database Syst Rev 2008(3):Cd006076. [DOI] [PMC free article] [PubMed]
- 7.Winstein CJ, Stein J, Arena R, Bates B, Cherney LR, Cramer SC, Deruyter F, Eng JJ, Fisher B, Harvey RL, et al. Guidelines for adult Stroke Rehabilitation and Recovery: a Guideline for Healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2016;47(6):e98–169. [DOI] [PubMed] [Google Scholar]
- 8.Zhong L, Wang J, Li F, Bao X, Liu H, Wang P. The Effectiveness of Acupuncture for Dysphagia after Stroke: A Systematic Review and Meta-Analysis. Evidence-based complementary and alternative medicine: eCAM 2021, 2021:8837625.
- 9.Lu Y, Chen Y, Huang D, Li J. Efficacy of acupuncture for dysphagia after stroke: a systematic review and meta-analysis. Annals Palliat Med. 2021;10(3):3410–22. [DOI] [PubMed] [Google Scholar]
- 10.Zhu B, Wang Y, Zhang G, Ouyang H, Zhang J, Zheng Y, Zhang S, Wu C, Qu S, Chen J, et al. Acupuncture at KI3 in healthy volunteers induces specific cortical functional activity: an fMRI study. BMC Complement Altern Med. 2015;15:361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yuan S, Deng B, Ye Q, Wu Z, Wu J, Wang L, Xu Q, Yao L, Xu N. Excitatory neurons in paraventricular hypothalamus contributed to the mechanism underlying acupuncture regulating the swallowing function. Sci Rep. 2022;12(1):5797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yao L, Ye Q, Liu Y, Yao S, Yuan S, Xu Q, Deng B, Tang X, Shi J, Luo J, et al. Electroacupuncture improves swallowing function in a post-stroke dysphagia mouse model by activating the motor cortex inputs to the nucleus tractus solitarii through the parabrachial nuclei. Nat Commun. 2023;14(1):810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fei YT, Cao HJ, Xia RY, Chai QY, Liang CH, Feng YT, Du YR, Yu MK, Guyatt G, Thabane L, et al. Methodological challenges in design and conduct of randomised controlled trials in acupuncture. BMJ. 2022;376:e064345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Logothetis NK. What we can do and what we cannot do with fMRI. Nature. 2008;453(7197):869–78. [DOI] [PubMed] [Google Scholar]
- 15.Li S, Luo C, Yu B, Yan B, Gong Q, He C, He L, Huang X, Yao D, Lui S, et al. Functional magnetic resonance imaging study on dysphagia after unilateral hemispheric stroke: a preliminary study. J Neurol Neurosurg Psychiatry. 2009;80(12):1320–9. [DOI] [PubMed] [Google Scholar]
- 16.Flowers HL, Skoretz SA, Streiner DL, Silver FL, Martino R. MRI-based neuroanatomical predictors of dysphagia after acute ischemic stroke: a systematic review and meta-analysis. Cerebrovasc Dis. 2011;32(1):1–10. [DOI] [PubMed] [Google Scholar]
- 17.Miller AJ. The neurobiology of swallowing and dysphagia. Dev Disabil Res Rev. 2008;14(2):77–86. [DOI] [PubMed] [Google Scholar]
- 18.Jang SH, Lee J, Kim MS. Dysphagia prognosis prediction via corticobulbar tract assessment in lateral medullary infarction: a diffusion tensor tractography study. Dysphagia. 2021;36(4):680–8. [DOI] [PubMed] [Google Scholar]
- 19.Hao X, Liu Z, He S, Wang Y, Zhao Y, Wang R. Application of DTI and fMRI in moyamoya disease. Front Neurol. 2022;13:948830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alvar A, Hahn Arkenberg R, McGowan B, Cheng H, Malandraki GA. The role of White Matter in the neural control of swallowing: a systematic review. Front Hum Neurosci. 2021;15:628424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ma SM, Wang L, Su XT, Yang NN, Huang J, Lin LL, Shao JK, Yang JW, Liu CZ. Acupuncture improves White Matter Perfusion and Integrity in Rat Model of Vascular Dementia: an MRI-Based imaging study. Front Aging Neurosci. 2020;12:582904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cai RL, Shen GM, Wang H, Guan YY. Brain functional connectivity network studies of acupuncture: a systematic review on resting-state fMRI. J Integr Med. 2018;16(1):26–33. [DOI] [PubMed] [Google Scholar]
- 23.Li B, Deng S, Sang B, Zhu W, Zhuo B, Zhang M, Qin C, Lyu Y, Du Y, Meng Z. Revealing the Neuroimaging Mechanism of Acupuncture for Poststroke Aphasia: A Systematic Review. Neural plasticity 2022, 2022:5635596. [DOI] [PMC free article] [PubMed]
- 24.Zhao N, Zhang J, Qiu M, Wang C, Xiang Y, Wang H, Xie J, Liu S, Wu J. Scalp acupuncture plus low-frequency rTMS promotes repair of brain white matter tracts in stroke patients: a DTI study. J Integr Neurosci. 2018;17(1):61–9. [DOI] [PubMed] [Google Scholar]
- 25.BIN P, Bo W. Chinese guidelines for diagnosis and treatment of acute ischemic stroke 2018. Chin J Neurol. 2018;51(09):666–82. [Google Scholar]
- 26.Network S. Management of Patients with Stroke: Identification and Management of Dysphagia. A National Clinical Guideline. Stroke; Swallowing Disorders.
- 27.Oldfield RC. The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia 1971, 9. [DOI] [PubMed]
- 28.Zung W. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–9. [DOI] [PubMed] [Google Scholar]
- 29.ZUNG WWK. A self-rating Depression Scale. Arch Gen Psychiatry. 1965;12(1):63–70. [DOI] [PubMed] [Google Scholar]
- 30.Mayer EA, Aziz Q, Coen S, Kern M, Labus JS, Lane R, Kuo B, Naliboff B, Tracey I. Brain imaging approaches to the study of functional GI disorders: a Rome working team report. Neurogastroenterol Motil. 2009;21(6):579–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Szucs D, Ioannidis JP. Sample size evolution in neuroimaging research: an evaluation of highly-cited studies (1990–2012) and of latest practices (2017–2018) in high-impact journals. NeuroImage. 2020;221:117164. [DOI] [PubMed] [Google Scholar]
- 32.Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet (London England). 1998;352(9125):364–5. [DOI] [PubMed] [Google Scholar]
- 33.Park J, White A, Stevinson C, Ernst E, James M. Validating a new non-penetrating sham acupuncture device: two randomised controlled trials. Acupunct Medicine: J Br Med Acupunct Soc. 2002;20(4):168–74. [DOI] [PubMed] [Google Scholar]
- 34.Takakura N, Yajima H. A double-blind placebo needle for acupuncture research. BMC Complement Altern Med. 2007;7:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hershman DL, Unger JM, Greenlee H, Capodice JL, Lew DL, Darke AK, Kengla AT, Melnik MK, Jorgensen CW, Kreisle WH, et al. Effect of acupuncture vs Sham acupuncture or Waitlist Control on Joint Pain related to aromatase inhibitors among women with early-stage breast Cancer: a Randomized Clinical Trial. JAMA. 2018;320(2):167–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yang JW, Wang LQ, Zou X, Yan SY, Wang Y, Zhao JJ, Tu JF, Wang J, Shi GX, Hu H, et al. Effect of acupuncture for Postprandial Distress Syndrome: a Randomized Clinical Trial. Ann Intern Med. 2020;172(12):777–85. [DOI] [PubMed] [Google Scholar]
- 37.Sun Y, Liu Y, Liu B, Zhou K, Yue Z, Zhang W, Fu W, Yang J, Li N, He L, et al. Efficacy of acupuncture for Chronic Prostatitis/Chronic Pelvic Pain Syndrome: a Randomized Trial. Ann Intern Med. 2021;174(10):1357–66. [DOI] [PubMed] [Google Scholar]
- 38.Chinese Society of Neurology CSS. Chinese guidelines for diagnosis and treatment of acute ischemic stroke 2018. Chin J Neurol. 2018;51(9):17. [Google Scholar]
- 39.Chinese Society of Neurology CSS. Chinese guidelines for secondary Prevention of ischemic stroke and transient ischemic attack 2014. Chin J Neurol 2015.
- 40.Expert consensus on evaluation and Treatment of swallowing disorders in China. (2017 edition). Chin J Phys Med Rehabil 2018, 40(01):1–10.
- 41.Yongjun W, Shaoshi W, Xingquan Z, Chunxue W, Yi Y, Haiqing S, Jing Z, Min L, Ruijun J. Chinese stroke dysphagia and Nutrition Management Manual. Chin J Stroke. 2019;14(11):1153–69. [Google Scholar]
- 42.Zang Y, Jiang T, Lu Y, He Y, Tian L. Regional homogeneity approach to fMRI data analysis. NeuroImage. 2004;22(1):394–400. [DOI] [PubMed] [Google Scholar]
- 43.Adhikari BM, Hong LE, Zhao Z, Wang DJJ, Thompson PM, Jahanshad N, Zhu AH, Holiga S, Turner JA, van Erp TGM, et al. Cerebral blood flow and cardiovascular risk effects on resting brain regional homogeneity. NeuroImage. 2022;262:119555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cao J, Tu Y, Wilson G, Orr SP, Kong J. Characterizing the analgesic effects of real and imagined acupuncture using functional and structure MRI. NeuroImage. 2020;221:117176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wei Y, Duan J, Womer F, Zhu Y, Yin Z, Cui L, Li C, Liu Z, Wei S, Jiang X, et al. Applying dimensional psychopathology: transdiagnostic associations among regional homogeneity, leptin and depressive symptoms. Translational Psychiatry. 2020;10(1):248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zang YF, He Y, Zhu CZ, Cao QJ, Sui MQ, Liang M, Tian LX, Jiang TZ, Wang YF. Altered baseline brain activity in children with ADHD revealed by resting-state functional MRI. Brain Dev. 2007;29(2):83–91. [DOI] [PubMed] [Google Scholar]
- 47.Yang H, Long XY, Yang Y, Yan H, Zhu CZ, Zhou XP, Zang YF, Gong QY. Amplitude of low frequency fluctuation within visual areas revealed by resting-state functional MRI. NeuroImage. 2007;36(1):144–52. [DOI] [PubMed] [Google Scholar]
- 48.Kong C, Xu D, Wang Y, Wang B, Wen J, Wang X, Zhan L, Sun Z, Jia X, Li M, et al. Amplitude of low-frequency fluctuations in multiple-frequency bands in patients with intracranial tuberculosis: a prospective cross-sectional study. Quant Imaging Med Surg. 2022;12(8):4120–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang J, Liu D, Qian S, Qu X, Zhang P, Ding N, Zang Y. The neural correlates of amplitude of low-frequency fluctuation: a multimodal resting-state MEG and fMRI-EEG study. Cerebral cortex (New York, NY: 1991) 2022. [DOI] [PubMed]
- 50.Zou QH, Zhu CZ, Yang Y, Zuo XN, Long XY, Cao QJ, Wang YF, Zang YF. An improved approach to detection of amplitude of low-frequency fluctuation (ALFF) for resting-state fMRI: fractional ALFF. J Neurosci Methods. 2008;172(1):137–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jia XZ, Sun JW, Ji GJ, Liao W, Lv YT, Wang J, Wang Z, Zhang H, Liu DQ, Zang YF. Percent amplitude of fluctuation: a simple measure for resting-state fMRI signal at single voxel level. PLoS ONE. 2020;15(1):e0227021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Friston KJ, Frith CD, Liddle PF, Frackowiak RS. Functional connectivity: the principal-component analysis of large (PET) data sets. J Cereb Blood flow Metabolism: Official J Int Soc Cereb Blood Flow Metabolism. 1993;13(1):5–14. [DOI] [PubMed] [Google Scholar]
- 53.Biswal BB, Van Kylen J, Hyde JS. Simultaneous assessment of flow and BOLD signals in resting-state functional connectivity maps. NMR Biomed. 1997;10(4–5):165–70. [DOI] [PubMed] [Google Scholar]
- 54.Assaf Y, Pasternak O. Diffusion tensor imaging (DTI)-based white matter mapping in brain research: a review. J Mol Neuroscience: MN. 2008;34(1):51–61. [DOI] [PubMed] [Google Scholar]
- 55.Kimura M, Yabuuchi H, Matsumoto R, Kobayashi K, Yamashita Y, Nagatomo K, Mikayama R, Kamitani T, Sagiyama K, Yamasaki Y. The reproducibility of measurements using a standardization phantom for the evaluation of fractional anisotropy (FA) derived from diffusion tensor imaging (DTI). Magma (New York NY). 2020;33(2):293–8. [DOI] [PubMed] [Google Scholar]
- 56.Kim Y, Han YJ, Park HY, Park GY, Jung M, Lee S, Im S. Neural correlates in the development of and recovery from dysphagia after supratentorial stroke: a prospective tractography study. NeuroImage Clin. 2022;35:103103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jeurissen B, Leemans A, Tournier JD, Jones DK, Sijbers J. Investigating the prevalence of complex fiber configurations in white matter tissue with diffusion magnetic resonance imaging. Hum Brain Mapp. 2013;34(11):2747–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ranzenberger LR, Snyder T. Diffusion Tensor Imaging. In: StatPearls. edn. Treasure Island (FL): StatPearls Publishing Copyright © 2023, StatPearls Publishing LLC.; 2023. [PubMed]
- 59.Chen HJ, Chen JL, Chen CY, Lee M, Chang WH, Huang TT. Effect of an Oral Health Programme on oral health, oral intake, and Nutrition in patients with stroke and Dysphagia in Taiwan: a Randomised Controlled Trial. Int J Environ Res Public Health 2019, 16(12). [DOI] [PMC free article] [PubMed]
- 60.Souza JT, Ribeiro PW, de Paiva SAR, Tanni SE, Minicucci MF, Zornoff LAM, Polegato BF, Bazan SGZ, Modolo GP, Bazan R, et al. Dysphagia and tube feeding after stroke are associated with poorer functional and mortality outcomes. Clin Nutr. 2020;39(9):2786–92. [DOI] [PubMed] [Google Scholar]
- 61.Farpour S, Asadi-Shekaari M, Borhani Haghighi A, Farpour HR. Improving swallowing function and ability in Post Stroke Dysphagia: a Randomized Clinical Trial. Dysphagia 2022:1–10. [DOI] [PMC free article] [PubMed]
- 62.Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86(8):1516–20. [DOI] [PubMed] [Google Scholar]
- 63.Osawa A, Maeshima S, Tanahashi N. Water-swallowing test: screening for aspiration in stroke patients. Cerebrovasc Dis. 2013;35(3):276–81. [DOI] [PubMed] [Google Scholar]
- 64.McHorney CA, Robbins J, Lomax K, Rosenbek JC, Chignell K, Kramer AE, Bricker DE. The SWAL-QOL and SWAL-CARE outcomes tool for oropharyngeal dysphagia in adults: III. Documentation of reliability and validity. Dysphagia. 2002;17(2):97–114. [DOI] [PubMed] [Google Scholar]
- 65.Brott T, Adams HP Jr., Olinger CP, Marler JR, Barsan WG, Biller J, Spilker J, Holleran R, Eberle R, Hertzberg V, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989;20(7):864–70. [DOI] [PubMed] [Google Scholar]
- 66.Harrison JK, McArthur KS, Quinn TJ. Assessment scales in stroke: clinimetric and clinical considerations. Clin Interv Aging. 2013;8:201–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kong J, Gollub R, Huang T, Polich G, Napadow V, Hui K, Vangel M, Rosen B, Kaptchuk TJ. Acupuncture de qi, from qualitative history to quantitative measurement. J Altern Complement Med (New York NY). 2007;13(10):1059–70. [DOI] [PubMed] [Google Scholar]
- 68.Yu DT, Jones AY, Pang MY. Development and validation of the Chinese version of the Massachusetts General Hospital acupuncture sensation scale: an exploratory and methodological study. Acupunct Medicine: J Br Med Acupunct Soc. 2012;30(3):214–21. [DOI] [PubMed] [Google Scholar]
- 69.Nishiwaki M, Takayama M, Yajima H, Nasu M, Kong J, Takakura N. The Japanese Version of the Massachusetts General Hospital acupuncture sensation scale: a validation study. Evidence-based Complement Altern Medicine: eCAM. 2017;2017:7093967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Liu L, Huang Q, Yang S, Wen Y, He W, Liu H, Meng L, Jiang H, Xia J, Liao W, et al. Micro-structural white matter abnormalities and cognitive impairment in asymptomatic carotid plaque patients: a DTI study using TBSS analysis. Clin Neurol Neurosurg. 2020;197:106096. [DOI] [PubMed] [Google Scholar]
- 71.Tang X, Shi X, Zhao H, Lu L, Chen Z, Feng Y, Liu L, Duan R, Zhang P, Xu Y, et al. Characteristics and quality of clinical practice guidelines addressing acupuncture interventions: a systematic survey of 133 guidelines and 433 acupuncture recommendations. BMJ open. 2022;12(2):e058834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Barkhof F, Haller S, Rombouts SA. Resting-state functional MR imaging: a new window to the brain. Radiology. 2014;272(1):29–49. [DOI] [PubMed] [Google Scholar]
- 73.Bluhm RL, Miller J, Lanius RA, Osuch EA, Boksman K, Neufeld RW, Théberge J, Schaefer B, Williamson P. Spontaneous low-frequency fluctuations in the BOLD signal in schizophrenic patients: anomalies in the default network. Schizophr Bull. 2007;33(4):1004–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Greicius MD, Flores BH, Menon V, Glover GH, Solvason HB, Kenna H, Reiss AL, Schatzberg AF. Resting-state functional connectivity in major depression: abnormally increased contributions from subgenual cingulate cortex and thalamus. Biol Psychiatry. 2007;62(5):429–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wilmskoetter J, Bonilha L, Martin-Harris B, Elm JJ, Horn J, Bonilha HS. Mapping acute lesion locations to physiological swallow impairments after stroke. NeuroImage Clin. 2019;22:101685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Im S, Han YJ, Kim SH, Yoon MJ, Oh J, Kim Y. Role of bilateral corticobulbar tracts in dysphagia after middle cerebral artery stroke. Eur J Neurol. 2020;27(11):2158–67. [DOI] [PubMed] [Google Scholar]
- 77.Zihan Z, Xiaonong F, Shu W, Jian L. The application of functional magnetic resonance imaging in the study of the mechanism of acupuncture for post-stroke dysphagia. Shanghai J Acupunct Moxibustion. 2022;41(03):313–7. [Google Scholar]
- 78.Churong L, Xinfei Z, Haofeng M, Xiaoting Z, Lina C, Xiaoyan C, Ruixian Z. MRI effects of Treatment for Dysphagia after Pseudobulbar Palsy by needling the Root of Tongue. Guiding J Traditional Chin Med Pharmacol. 2019;25(06):112–5. [Google Scholar]
- 79.Zhang CH, Bian JL, Meng ZH, Meng LN, Ren XS, Wang ZL, Guo XY, Shi XM. Tongguan Liqiao acupuncture therapy improves dysphagia after brainstem stroke. Neural Regeneration Res. 2016;11(2):285–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.