ABSTRACT
Cold climate and unique genetic and environmental factors may influence the prevalence of skin diseases in Greenland. However, there is a lack of epidemiological studies on skin diseases in the adult Greenlandic population. To address this unmet need a cross-sectional study, run by dermatologists from Denmark, the UK, and Switzerland estimated the prevalence and clinical manifestations of skin diseases among adults in East Greenland in May 2022. All adults ≥18 years in the town of Tasiilaq were invited, and 295 individuals aged 18–78 years participated (22.5% of the overall adult population in Tasiilaq). Two-hundred and three participants (69%) had visible signs of current skin disease, and among these, 242 cases of dermatoses were identified. The most common skin diseases were hand eczema (22.4%), lichen simplex (9.5%), discoid eczema (7.1%), psoriasis, atopic dermatitis and acne vulgaris (5.8% each). Scabies was the most frequent infectious skin disease (4.4%). No cases of skin cancer were identified. Atopic dermatitis and psoriasis presented with disease that was of limited extent and different from the classical presentations. Skin diseases showed a high prevalence among adults in East Greenland, and some of them were severe. This indicates a noteworthy public health problem that warrants better access to dermatologist support.
KEYWORDS: Arctic, atopic dermatitis, global health, Greenland, hand eczema, inuit, prevalence, psoriasis, skin disease
Introduction
Globally, skin diseases pose a public health concern by causing disability, physical discomfort, stigma, and loss of income [1,2]. According to the Global Burden of Disease Study, the global prevalence of skin diseases has increased by nearly 13% since 2010 [3,4]. Greenland is the world’s largest island located in the Arctic region. Its area spans almost 2.2 million square kilometres with 80% covered by an ice sheet. The inhabited regions are limited to the coastal areas, characterised by an arid climate with long, cold winters and low humidity.
Most of the Greenlandic population (89%) are of Inuit descent that has a unique genetic architecture from having lived in isolation for centuries [5]. Out of Greenland’s 56,600 inhabitants, most live in towns and settlements on the west coast, including 19,400 in the capital city of Nuuk, while only two towns and several settlements are located on the largely deserted east coast. The population of East Greenland was isolated from the rest of the world until the end of the 19th century. The traditional diet in Greenland is typically composed of sea mammals, fish, and wild game, but in recent decades there has been a shift towards a more Western diet [6,7].
The combination of a cold climate and unique genetic and environmental factors may influence the frequency of skin diseases. However, there is a general lack of knowledge about the prevalence of skin diseases in adults in the Arctic region and particularly in the Greenlandic population. In Nuuk, the prevalence of hidradenitis suppurativa (HS) among adults has been found to be 3.2%, while the prevalence of psoriasis was 0.9% in the general population [8,9]. Existing knowledge of other common skin diseases in Greenland is based on few studies of atopic dermatitis in children, and no studies have so far been conducted among adults in East Greenlandic populations [8–13].
We performed a cross-sectional survey to estimate the prevalence and characteristics of skin disease among the adult population living in Tasiilaq, and to provide knowledge on the management and prevention of skin diseases in the local population.
Materials and methods
Study design, population, and setting
The study was conducted in the town of Tasiilaq, East Greenland (latitude 66°) between May 4th to 11th, 2022. The annual mean temperature in Tasiilaq is −0.3°C and the total annual precipitation is 951.1 mm, mostly as snow [14]. Tasiilaq is the largest town on the east coast with a total population of 1,931 (adults n = 1,311, adult females n = 646 by 1 April 2022). According to the 2022 census, the adult population in Tasiilaq represented 3.1% of the adult Greenlandic population [15].
A population-based survey including a clinical skin examination was organised in Tasiilaq community hall, where all adults ≥18 years living in the town of Tasiilaq and neighbouring settlements were invited to participate, regardless of any prior or existing skin diseases. The study was advertised through social media, national broadcast radio, newspaper articles, and local posters. Informed and written consent was required from each participant before study inclusion. On the day of enrolment, each participant had their body mass index (BMI, kg/m2) measured and was interviewed using a questionnaire in either East Greenlandic, Danish, or English, assisted by local interpreters as needed. The interview included questions about sociodemographic data, risk factors for skin disease, previous skin disease, and current symptoms of skin disease, if any. Each participant was then offered a skin examination in a separate room, which was performed by a dermatologist or a dermatology-trained physician. All visible findings were recorded. The diagnosis of all skin disorders was based on a combination of clinical findings and reported symptoms. The diagnosis of atopic dermatitis was determined by using the Hanifin and Rajka criteria, [16] and atopic dermatitis severity was measured by Eczema Area and Severity Index (EASI), while psoriasis severity was measured by Psoriasis Area and Severity Index (PASI), and hand eczema was measured by Hand Eczema Severity Index (HECSI). Hand eczema and discoid eczema were reported separately from atopic eczema, and participants could be diagnosed with all three skin conditions during the skin examination. All data was entered into RedCap. The study was conducted in collaboration with the Global Psoriasis Atlas, the Global Atopic Dermatitis Atlas, and the Global Healthcare Study on Psoriasis.
Statistical analysis
Statistical analysis was performed in SAS Studio (https://www.sas.com). The prevalence was defined as the proportion of study participants with an identified skin disease relative to the total number of study participants. Confidence intervals were calculated with the Wilson score interval.
Public health measures
Participants who were diagnosed with a skin disease, including those previously diagnosed and treated, were informed about locally available treatment options and future prevention strategies for the condition. With permission from participants, the local health system was informed about their skin disorders and possible preventative measures. Treatments were prescribed by the local health system. Cases suspected of occupational hand eczema were reported to the Greenlandic Center for Work Injuries and the Danish Labour Market Insurance. Outpatient consultations were arranged at Tasiilaq Hospital if a participant required medical follow-up for their skin condition, and hospital admission was arranged if a participant had skin disease severe enough to require urgent treatment.
Ethics
The study was conducted according to the principles of the Helsinki II Declaration and was approved by the National Scientific Ethics Committee for Greenland (KVUG-2021-23) and the Agency of Health and Prevention in Greenland. The Global Healthcare Study on Psoriasis has been approved by the Business Administration System of the Swiss Ethics Committee (BASEC: 2020–00002).
Results
A total of 295 participants aged 18–78 years were included in the study. Of these, 283 (95.9%) were of Inuit descent, and 163 (55.2%) were female (Table 1). All participants lived in Tasiilaq, except for five who lived in the neighbouring settlements. The number of participants corresponded to 22.5% of the total adult population of Tasiilaq (295/1,311).
Table 1.
Sociodemographic characteristics of the survey participants.
| Characteristics | Total (N = 295)* |
Inuit (N = 283) |
Mixed Inuit/Danish or other† (N = 12) |
|---|---|---|---|
| Sex, Female | 163 (55.3) | 157 (55.5) | 6 (50.0) |
| Ethnicity | |||
| Inuit | 283 (95.9) | 283 (100) | – |
| Mixed Inuit/Danish | 9 (3.1) | – | 9 (75.0) |
| Other† | 3 (1.0) | – | 3 (25.0) |
| Age, years, median (IQR) | 38 (29-54) | 38 (29-54) | 49 (30-56) |
| BMI, kg/m [2], median (IQR) | 26.6 (23.9-30.9) | 26.6 (23.9-30.9) | 26.4 (23.5-30.3) |
| Accommodation | |||
| House/attached house | 167 (56.8) | 158 (56.0) | 9 (75.0) |
| Apartment | 118 (40.1) | 115 (40.8) | 3 (25.0) |
| Nursing home/dormitory | 9 (3.1) | 9 (3.2) | – |
| Household crowding | |||
| ≤2 | 64 (21.9) | 58 (20.7) | 6 (50.0) |
| 3-5 | 160 (54.8) | 155 (55.4) | 5 (41.7) |
| ≥6 | 68 (23.3) | 67 (23.9) | 1 (8.3) |
| Educational level‡ | |||
| Low | 151 (51.2) | 149 (52.7) | 2 (16.7) |
| Medium | 29 (9.8) | 27 (9.5) | 2 (16.7) |
| High | 115 (39.0) | 107 (37.8) | 8 (66.7) |
| Employment status | |||
| Unemployed | 43 (14.6) | 43 (15.2) | – |
| Unskilled work§ | 87 (29.5) | 85 (30.0) | 2 (16.7) |
| Semi-skilled work | 61 (20.7) | 60 (21.2) | 1 (8.3) |
| Skilled work | 67 (22.7) | 58 (20.5) | 9 (75.0) |
| Full-time student or retired | 37 (12.5) | 37 (13.1) | – |
| Traditional Diet¶ | |||
| ≤1 time weekly | 73 (27.1) | 68 (26.2) | 5 (55.6) |
| 2-5 times weekly | 149 (55.4) | 145 (55.8) | 4 (44.4) |
| ≥6 times weekly | 47 (17.6) | 47 (18.1) | – |
| Smoking status | |||
| Current | 202 (68.5) | 196 (69,3) | 6 (50.0) |
| Former | 44 (14.9) | 42 (14.8) | 2 (16.7) |
| Never | 49 (16.6) | 45 (16.9) | 4 (33.3) |
| Alcohol consumption | |||
| No | 131 (44.6) | 127 (45.0) | 4 (33.3) |
| Yes | 163 (55.4) | 155 (55.0) | 8 (66.7) |
| ≤14 units weekly | 137 (84.0) | 130 (83.9) | 6 (75.0) |
| ≥14 units weekly | 26 (16.0) | 25 (16.1) | 2 (25.0) |
| History of physician diagnosed skin disease | |||
| No | 154 (52.4) | 149 (52.7) | 5 (41.7) |
| Yes | 140 (47.6) | 133 (47.0) | 7 (58.3) |
| Skin examination | |||
| No | 35 (11.9) | 32 (11.3) | 3 (25.0) |
| Yes | 260 (88.1) | 251 (88.7) | 9 (75.0) |
| Skin disease identified in the study | |||
| No | 92 (31.2) | 88 (31.1) | 4 (33.3) |
| Yes | 203 (68.8) | 195 (68.9) | 8 (66.6) |
Data are n (%) unless otherwise stated. *There are missing data N for the following variables: Accommodation 1, household crowding 3, alcohol consumption 1, traditional diet 26, history of physician diagnosed skin disease 1. †Mixed Inuit/Danish was defined as individuals with parents of both Danish and Greenlandic descent. Other was defined as nationalities other than Greenlandic. These included Danish, Norwegian, Icelandic and Faroese. ‡Educational level: low defined as no or primary education; medium defined as secondary education; high defined as post-secondary education. §Unskilled work includes hunters and fishers. ¶Traditional diet: Marine mammals, fish, and game. BMI=Body mass index.
The participants had a median age of 38 years (interquartile range [IQR] 29–54) and a median BMI of 26.6 (IQR 23.9–30.9). Most participants (55.4%, n = 149) consumed a traditional diet of marine mammals, fish, and game 2–5 times weekly, had no education or only primary education (51.2%, n = 151), were current smokers (68.5%, n = 202), and consumed alcohol (55.4%, n = 163). Excessive alcohol consumption (≥14 units weekly) was reported by 16.0% (n = 26) of the participants who consumed alcohol. However, many participants reported occasional excessive alcohol consumption. Nearly half of the participants (47.6%, n = 140) had previously been diagnosed with a skin disease by a physician, and 123 (41.7%) had undergone treatment.
A skin examination was performed on 260 participants, including individuals with and without symptoms of skin disease. The remaining participants who were not examined reported no symptoms of skin disease.
We identified 242 cases of dermatoses in 203 participants (females n = 107, Table 2). The prevalence of skin diseases among the participants was 68.8% (203/295; 95% confidence interval [CI]: 63.3–73.8). Most disorders were eczematous; hand eczema showed the highest prevalence at 22.4% (95% CI: 18.0–27.5; n = 66, Figure 1b), followed by lichen simplex (9.5%, 95% CI: 3.9–9.4; n = 28), and discoid eczema (7.1%, 95% CI: 4.7–10.6; n = 21). Other frequent dermatoses included atopic dermatitis, psoriasis, and acne vulgaris (5.8% for each, 95% CI: 3.6–9.0; n = 17, Figure 1a), scabies (4.4%, 95% CI: 2.6–7.4; n = 13, Figure 1d), rosacea (2.0%, 95% CI: 0.9–4.4; n = 6), and verruca vulgaris (1.4%, 95% CI: 0.5–3.4; n = 4). Urticaria and nonsegmental vitiligo accounted for one case each (0.3%, 95% CI: 0.1–1.9), while we found no cases of HS or skin cancers.
Table 2.
Cases of dermatoses among the 203 study participants with skin conditions.
| Dermatoses | Total n* (female n) | Prevalence %† (95% CI) |
|---|---|---|
| Inflammatory dermatoses | ||
| Psoriasis vulgaris | 16 (8) | 5.4 (3.4–8.6) |
| Sebopsoriasis | 1 (0) | 0.3 (0.1–1.9) |
| Palmoplantar pustulosis | 5 (4) | 1.7 (0.7–3.9) |
| Seborrhoeic dermatitis | 7 (1) | 2.4 (1.2–4.8) |
| Urticaria | 1 (0) | 0.3 (0.1–1.9) |
| Total | 30 (13) | 10.2 (7.2–14.1) |
| Eczematous disorders | ||
| Hand eczema | 66 (44) | 22.4 (18.0–27.5) |
| Atopic dermatitis | 17 (14) | 5.8 (3.6–9.0) |
| Lichen simplex | 28 (8) | 9.5 (3.9–9.4) |
| Hyperkeratotic plantar eczema | 1 (0) | 0.3 (0.1–1.9) |
| Hyperkeratotic palmoplantar eczema | 2 (0) | 0.7 (0.2–2.4) |
| Discoid eczema | 21 (9) | 7.1 (4.7–10.6) |
| Phototoxic eczema | 1 (0) | 0.3 (0.1–1.9) |
| Unspecified eczema | 7 (2) | 2.4 (1.2–4.8) |
| Eczema craquelé | 3 (0) | 1.0 (0.3–2.9) |
| Total | 146 (77) | 49.5 (43.8–55.2) |
| Infections and infestations | ||
| Scabies | 13 (8) | 4.4 (2.6–7.4) |
| Verruca vulgaris | 4 (2) | 1.4 (0.5–3.4) |
| Impetigo | 1 (1) | 0.3 (0.1–1.9) |
| Infected eczema | 1 (0) | 0.3 (0.1–1.9) |
| Insect bites | 1 (0) | 0.3 (0.1–1.9) |
| Pityriasis versicolor | 1 (1) | 0.3 (0.1–1.9) |
| Tinea corporis | 1 (0) | 0.3 (0.1–1.9) |
| Tinea pedis | 2 (2) | 0.7 (0.2–2.4) |
| Total | 24 (14) | 8.1 (5.5–11.8) |
| Pigmentary disorders | ||
| Blue naevus | 1 (0) | 0.3 (0.1–1.9) |
| Melasma | 3 (3) | 1.0 (0.3–2.9) |
| Nonsegmental vitiligo | 1 (0) | 0.3 (0.1–1.9) |
| Postinflammatory hypopigmentation | 1 (1) | 0.3 (0.1–1.9) |
| Postinflammatory hyperpigmentation | 1 (1) | 0.3 (0.1–1.9) |
| Total | 7 (5) | 2.4 (1.2–4.8) |
| Other | ||
| Acne vulgaris | 17 (9) | 5.8 (3.6–9.0) |
| Rosacea | 6 (4) | 2.0 (0.9–4.4) |
| Ichthyosis vulgaris | 1 (1) | 0.3 (0.1–1.9) |
| Lichenoid primary cutaneous amyloidosis | 3 (1) | 1.0 (0.3–2.9) |
| Seborrhoeic keratosis | 1 (1) | 0.3 (0.1–1.9) |
| Granuloma annulare | 1 (1) | 0.3 (0.1–1.9) |
| Prurigo nodularis | 1 (1) | 0.3 (0.1–1.9) |
| Panniculitis | 1 (1) | 0.3 (0.1–1.9) |
| Xerosis | 3 (2) | 1.0 (0.3–2.9) |
| Clavus | 1 (1) | 0.3 (0.1–1.9) |
| Total | 35 (22) | 11.9 (8.7–16.1) |
Each skin condition was diagnosed by a physician trained in dermatology. CI, confidence interval. †Compared to the total number of study participants.
Figure 1.
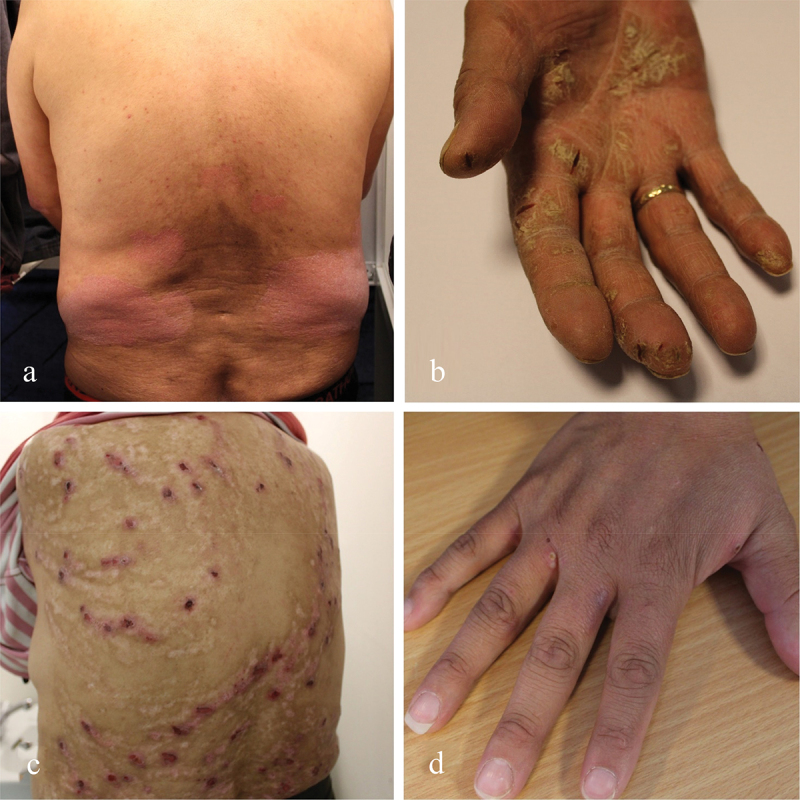
A selection of skin diseases identified during the study. a) Psoriasis vulgaris, b) Hand eczema, c) Prurigo nodularis, d) Scabies.
Most skin diseases had typical clinical manifestations. For hand eczema, the lesions were moderate according to the HECSI (mean 21.0, range 2–112) while for atopic dermatitis, the lesions were mild or almost clear according to the EASI (mean 2.5, range 0.3–5.2). Because of their mild lesions, atopic dermatitis was sometimes challenging to distinguish from discoid eczema. The median age of disease onset of atopic dermatitis was three years (IQR: 0–10, Table 3). For psoriasis, the lesions were atypical and characterised by thin, almost eczematous lesions, similar to discoid eczema on limbs and seborrhoeic dermatitis and dandruff on the face and scalp respectively (mean PASI 4.8, range 0.4–15.8, Figure 1a). Participants with psoriasis had the highest BMI at 30.4 (IQR: 24.8–33.4) compared to participants with other frequent skin diseases (Table 3). Most of the participants with psoriasis were current smokers (58.8%, n = 10), and 11 (64.7%) consumed alcohol, which was more than the participants with hand eczema (51.5%) and atopic dermatitis (43.8%).
Table 3.
Characteristics of the participants with the most frequent skin disorders.
| Characteristics | Hand eczema (N = 66) | Lichen simplex (N = 28) | Discoid eczema (N = 21) | Atopic dermatitis (N = 17) | Psoriasis (N = 17) | Acne vulgaris (N = 17) |
|---|---|---|---|---|---|---|
| Sex, Female | 43 (65.2) | 8 (28.6) | 9 (42.9) | 14 (82.4) | 8 (47.1) | 9 (52.9) |
| Ethnicity | ||||||
| Inuit | 64 (97.0) | 27 (96.4) | 20 (95.2) | 17 (100) | 16 (94.1) | 17 (100) |
| Mixed Inuit/Danish | 1 (1.5) | 1 (3.6) | 1 (4.8) | - | 1 (5.9) | - |
| Other† | 1 (1.5) | – | – | – | – | – |
| Age, years, median (IQR) | 40 (30-54) | 39 (30-56) | 45 (30-55) | 35 (25-53) | 52 (33-55) | 22 (21-28) |
| BMI, kg/m [2], median (IQR) | 26.5 (24.4-30.2) | 26.4 (23.8-31.1) | 25.8 (24.1-29.7) | 27.1 (24.6-27.9) | 30.4 (24.8-33.4) | 23.5 (22.1-29.8) |
| Accommodation | ||||||
| House/attached house | 43 (66.2) | 16 (57.1) | 12 (57.1) | 11 (64.7) | 14 (82.4) | 7 (41.2) |
| Apartment | 22 (33.8) | 12 (42.9) | 9 (42.9) | 6 (35.3) | 3 (17.6) | 9 (52.9) |
| Nursing home/dormitory | – | – | – | – | – | 1 (5.9) |
| Household crowding | ||||||
| ≤2 | 17 (26.2) | 4 (14.3) | 4 (19.0) | 4 (23.5) | 4 (23.5) | 1 (5.9) |
| 3-5 | 33 (50.0) | 18 (64.3) | 13 (61.9) | 10 (58.8) | 12 (70.6) | 9 (52.9) |
| ≥6 | 15 (22.7) | 6 (21.4) | 4 (19.0) | 3 (17.6) | 1 (5.9) | 7 (41.2) |
| Educational level‡ | ||||||
| Low | 33 (50.0) | 15 (53.6) | 9 (42.9) | 9 (52.9) | 7 (41.2) | 9 (52.9) |
| Medium | 4 (6.1) | 2 (7.1) | 8 (38.1) | 5 (29.4) | 3 (17.6) | 4 (23.5) |
| High | 29 (43.9) | 11 (39.3) | 10 (47.6) | 3 (17.6) | 7 (41.2) | 4 (23.5) |
| Employment status | ||||||
| Unemployed | 10 (15.2) | 2 (7.1) | 5 (23.8) | 1 (5.9) | 1 (5.9) | 3 (17.6) |
| Unskilled work§ | 18 (27.3) | 13 (46.4) | 3 (14.3) | 3 (17.6) | 6 (35.3) | 9 (52.9) |
| Semi-skilled work | 17 (25.8) | 4 (14.3) | 4 (19.0) | 5 (29.4) | 3 (17.6) | 2 (11.8) |
| Skilled work | 17 (25.8) | 5 (17.9) | 6 (28.6) | 6 (35.3) | 6 (35.3) | 1 (5.9) |
| Full-time student or retired | 4 (6.1) | 4 (14.3) | 3 (14.3) | 2 (11.8) | 1 (5.9) | 2 (11.8) |
| Traditional Diet¶ | ||||||
| ≤1 time weekly | 21 (31.8) | 10 (35.7) | 12 (57.1) | 5 (29.4) | 13 (76.5) | 8 (47.1) |
| 2-5 times weekly | 34 (51.5) | 13 (46.4) | 5 (23.8) | 11 (64.7) | 2 (11.8) | 7 (41.2) |
| ≥6 times weekly | 11 (16.7) | 5 (17.9) | 4 (19.0) | 1 (5.9) | 2 (11.8) | 2 (11.8) |
| Smoking status | ||||||
| Current | 44 (66.7) | 23 (82.1) | 13 (61.9) | 12 (70.6) | 10 (58.8) | 16 (94.1) |
| Former | 10 (15.2) | 5 (17.9) | 5 (23.8) | 4 (23.5) | 4 (23.5) | 1 (5.9) |
| Never | 12 (18.2) | – | 3 (14.3) | 1 (5.9) | 3 (17.6) | – |
| Alcohol consumption | ||||||
| No | 31 (47.7) | 16 (57.1) | 7 (33.3) | 9 (56.3) | 6 (35.3) | 9 (52.9) |
| Yes | 34 (52.3) | 12 (42.9) | 14 (66.6) | 7 (43.8) | 11 (64.7) | 8 (47.1) |
| ≤14 units weekly | 26 (76.5) | 9 (75.0) | 12 (85.7) | 4 (57.1) | 8 (72.7) | 5 (62.5) |
| ≥14 units weekly | 8 (23.5) | 3 (25.0) | 2 (14.3) | 3 (42.9) | 3 (27.3) | 3 (37.5) |
| Age at disease onset, years, median (IQR) | 25 (19-40) | – | – | 3 (0-10) | 27 (21-35) | – |
| Missing, n | 29 | 28 | 21 | – | 6 | 17 |
Data are n (%) unless otherwise stated. There are missing data N for the following variables: Accommodation (hand eczema n = 1), household crowding (hand eczema n = 1), alcohol consumption (hand eczema n = 1; atopic dermatitis n = 1). †Mixed Inuit/Danish was defined as individuals with parents of both Danish and Greenlandic descent. Other was defined as nationalities other than Greenlandic. These included Danish, Norwegian, Icelandic and Faroese. ‡Educational level: low defined as no or primary education; medium defined as secondary education; high defined as post-secondary education. §Unskilled work includes hunters and fishers. ¶Traditional diet: Marine mammals, fish, and game. BMI=Body mass index.
A treatment plan was provided for most participants with a skin disease (75.4%, 153/203). The prescribed treatments mainly included topical corticosteroids and topical calcineurin inhibitors. Outpatient consultations were arranged for 14 participants, who had more severe skin diseases, including severe prurigo nodularis (Figure 1c), while 4 participants were admitted to the hospital for treatment. All four admitted participants were diagnosed with persistent scabies.
Discussion
This was the first cross-sectional study to estimate the prevalence of skin diseases among adults in Greenland. This study included 295 adults, which corresponded to nearly a quarter of the adult population in Tasiilaq. Inflammatory dermatoses, particularly eczematous disorders, were the most frequent skin diseases.
Hand eczema showed the highest prevalence of all skin disorders at 22.4%, which was also higher compared to the self-reported prevalence in Danish adults from the general population at 5.8%. [17] However, selection bias may have increased the prevalence in the East Greenlandic population. According to the survey, 27.3% (n = 18) of the participants with hand eczema were unskilled physical labourers, which included fishing, hunting, cleaning, and cooking. Additionally, many participants engaged in fishing and hunting during their spare time. The combination of repetitive work-related mechanical exposures and a cold and dry climate may potentially account for the high prevalence of hand eczema, thus presenting a health hazard for individuals working with physical labour in Arctic regions.
The prevalence of atopic dermatitis in Tasiilaq was 5.8%, as expected much lower than the prevalence reported among Greenlandic children in 2023 (35.2%) and the incidence reported in 2001 (177 cases per 1,000 child years at risk). [12,18] The lower prevalence of atopic dermatitis in Greenlandic adults can be explained by a natural resolution in adolescence, but may also reflect an increasing prevalence among children caused by environmental changes such as improved housing and hygiene, dietary changes, and increased use of antibiotics. [12] In addition, this study was conducted in a rural setting, where the prevalence of atopic dermatitis may be lower than that observed in urban settings in previous studies. [12,13] The lower prevalence in rural areas may be explained by differences in living standards, diet, and education.
The Hanifin and Rajka criteria to diagnose atopic dermatitis rely on typical clinical presentations, but we observed atypical, mild lesions, which often resembled discoid eczema. Additionally, the cold and dry Arctic climate increases the risk of eczema in weather exposed areas such as the hands, neck and ankles, which could also have affected the clinical presentation of atopic dermatitis.
The prevalence of psoriasis at 5.8% was higher than the hospital-based prevalence reported in the capital Nuuk at 0.9% [9] and considerably higher than most countries worldwide. [19] However, the study conducted in Nuuk used the entire population of Nuuk as a reference, and the prevalence estimate should be regarded as a conservative minimum. The clinical presentation of psoriasis was atypical with mild and thin lesions, which showed similarities to discoid eczema and seborrhoeic dermatitis (Figure 1a). The clinical presentation of psoriasis in relation to ethnicity has been sparsely studied, although it may vary across different ethnic groups. [20] Most participants with psoriasis exhibited known lifestyle-related risk factors for psoriasis, including current smoking, alcohol consumption, and being overweight (Table 3). [21] The smoking and drinking patterns among participants with psoriasis were comparable to those observed in participants with other prevalent diseases. Participants who consumed alcohol commonly reported monthly binge drinking followed by abstinence, which mirrored the alcohol consumption patterns observed in the rest of Greenland. [22] Interestingly, we identified no cases of HS. A previous study reported a prevalence of 3.2% in Nuuk, which predominantly affected individuals of Inuit descent. [8] HS lesions are often located in the anogenital and inguinal areas and can be associated with stigma, which could have discouraged some from participating. HS is caused by a combination of genetic and environmental factors, and its prevalence in Arctic populations requires additional research.
Consistent with other studies conducted among Inuit populations, we did not identify any cases of skin cancer [23]. These results align with data from the Association of the Nordic Cancer Registry (NORDCAN), which has documented very few cases of malignant melanoma and squamous cell carcinoma annually in Greenland in recent years. [24] Inuit populations may have a lower risk of skin cancer because of darker skin types.[25]
Scabies was the most frequent infectious disease with a prevalence of 4.4%, and all four participants who were admitted to hospital had scabies infections. Many study participants lived in overcrowded households with up to nine family members (mostly children), where they had persistent infections that had been unsuccessfully treated. The continuous spread of scabies within some households may result from overcrowding and a cold Arctic climate, which causes extended periods of indoor stay, thereby providing optimal conditions for recurrent scabies infections. [26] Since children were excluded from this study, it is highly possible that the prevalence of scabies in the general population of Tasiilaq exceeded 4.4%, thus posing a greater health concern than reported in this study.
Some participants presented with severe skin disease, including a case of prurigo nodularis (Figure 1c). Healthcare provision in Greenland is logistically challenged by long distances and harsh weather. Currently, no dermatologists work permanently in Greenland, and one general practitioner is in charge of clinical guidelines for dermatology in Greenland. [27] The access to some new and costly treatments such as biologic therapies is limited. Specialist care is therefore facilitated through tele dermatology, which enables patients to connect with dermatologists based at Bispebjerg Hospital in Copenhagen, Denmark.
Strengths and limitations
This study has some limitations. The study was conducted with voluntary participation, leading to potential selection bias as individuals with undiagnosed skin diseases were more likely to participate, while those who were already diagnosed or had no skin disease were less inclined to take part. Additionally, the low number of participants from the settlements could be explained by the need to travel by boat to Tasiilaq. However, all adults living in and around Tasiilaq were encouraged to participate regardless of skin disease, and participation was made more accessible as it was conducted in the community hall. Skin examination was limited to participants who agreed to be examined, potentially leading to falsely lower rates for some common dermatoses. Still, we are confident that we identified most skin diseases, since most participants who were offered a skin examination accepted. The prevalence from our study reflects the prevalence in adults only since children were not eligible. It was common for participants to bring their children, who frequently presented with skin diseases, but they were excluded because of age restrictions of our research ethics approval. Thus, we suspect some diseases might show a higher prevalence in the general population, including scabies.
This study also had its strengths. To secure consistent evaluation of the diagnoses, each participant was interviewed and examined by at least one physician with a minimum of one year of experience in dermatology, and most were specialists. Additionally, there was a high participation rate as nearly a quarter of the entire adult population in Tasiilaq were included over the course of one week.
Conclusion
The prevalence of skin diseases among adults in the town of Tasiilaq, East Greenland in May 2022, was 68.8% (203/295). The most frequent skin diseases were hand eczema (22.4%), lichen simplex (9.5%), discoid eczema (7.1%), psoriasis, atopic dermatitis and acne vulgaris (5.8% each), and scabies (4.4%). Based on these findings, skin diseases represent a significant public health problem in Greenland because of their high prevalence and a lack of dermatologists in the country.
Acknowledgments
We thank the medical doctors Hans Christian Florian Sørensen and Lydia Maria Helms at Tasiilaq Hospital for their valuable cooperation in planning and organising this study. We also thank Rebekah Swan of the Global Psoriasis Atlas and medical student Kunuk Hansen for their support in facilitating the study. Finally, we thank the interpreters and all the participants for their participation. Written informed consent to share and publish photographs was granted by the participants.
Funding Statement
Aage Bang Foundation. The funder had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The Global Psoriasis Atlas, which is funded in part by the LEO Foundation, AbbVie, Almirall, Amgen, Janssen, Lilly, Novartis and UCB. The Global Atopic Dermatitis Atlas, which is funded by the LEO Foundation.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- [1].Richard MA, Saint Aroman M, Baissac C, et al. Burden of visible [face and hands] skin diseases: results from a large international survey. Ann Dermatol Venereol. 2023;150(2):95–9. doi: 10.1016/j.annder.2022.11.008 [DOI] [PubMed] [Google Scholar]
- [2].Lim HW, Collins SAB, Resneck JS, et al. The burden of skin disease in the United States. J Am Acad Dermatol. 2017;76(5):958–972.e2. doi: 10.1016/j.jaad.2016.12.043 [DOI] [PubMed] [Google Scholar]
- [3].Abbafati C, Abbas KM, Abbasi M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].The Lancet: Skin and subcutaneous diseases—Level 2 cause . Published 2020. [cited 2023 Oct 30]. Available from: https://www.thelancet.com/pb-assets/Lancet/gbd/summaries/diseases/skin-subcutaneous-diseases.pdf
- [5].Moltke I, Fumagalli M, Korneliussen TS, et al. Uncovering the genetic history of the present-day greenlandic population. Am J Hum Genet. 2015;96(1):54–69. doi: 10.1016/j.ajhg.2014.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Bjerregaard P, Jørgensen ME, Backer V, et al. Prevalence of obesity among inuit in Greenland and temporal trend by social position. Am J Hum Biol. 2013;25(3):335–340. doi: 10.1002/ajhb.22372 [DOI] [PubMed] [Google Scholar]
- [7].Kuhnlein HV, Receveur O, Soueida R, et al. Arctic indigenous peoples experience the nutrition transition with changing dietary patterns and obesity. J Nutr. 2004;134(6):1447–1453. doi: 10.1093/jn/134.6.1447 [DOI] [PubMed] [Google Scholar]
- [8].Botvid SHC, Hove LS, Bouazzi D, et al. Hidradenitis suppurativa prevalence in Nuuk, Greenland: physician validation of a hidradenitis suppurativa questionnaire in a Greenlandic setting. Acta Derm Venereol. 2023;103:3–5. doi: 10.2340/actadv.v103.4410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Botvid SHC, Storgaard Hove L, Backe MB, et al. Low prevalence of patients diagnosed with psoriasis in Nuuk: a call for increased awareness of chronic skin disease in Greenland. Int J Circumpolar Health. 2022;81(1). doi: 10.1080/22423982.2022.2068111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Harvald B. Genetic epidemiology of Greenland. Clin Genet. 1989;36(5):364–367. doi: 10.1111/j.1399-0004.1989.tb03214.x [DOI] [PubMed] [Google Scholar]
- [11].Kromann N, Green A. Epidemiological studies in the Upernavik District, Greenland: incidence of some chronic diseases 1950–1974. Acta Med Scand. 1980;208(1–6):401–406. doi: 10.1111/j.0954-6820.1980.tb01221.x [DOI] [PubMed] [Google Scholar]
- [12].Andersson AM, Kaiser H, Skov L, et al. Prevalence and risk factors for atopic dermatitis in Greenlandic children. Clin Exp Dermatol. 2023;48(4):352–360. doi: 10.1093/ced/llac132 [DOI] [PubMed] [Google Scholar]
- [13].Andersson AM, Halling AS, Loft N, et al. Atopic dermatitis among children and adolescents in the Arctic region - a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2021;35(8):1642–1654. doi: 10.1111/jdv.17276 [DOI] [PubMed] [Google Scholar]
- [14].Danish Meteorological Institute. Climate norms for Greenland . 2020. [cited 2023 Sep 22]. Available from: https://www.dmi.dk/vejrarkiv/normaler-gronland/
- [15].Statistics Greenland . [cited 2023 Sep 21]. Available from: https://stat.gl
- [16].Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol. 1980;60(92):44–47. doi: 10.2340/00015555924447 [DOI] [Google Scholar]
- [17].Quaade AS, Alinaghi F, Dietz JBN, et al. Chronic hand eczema: a prevalent disease in the general population associated with reduced quality of life and poor overall health measures. Contact Dermatitis. 2023;89(6):453–463. doi: 10.1111/cod.14407 [DOI] [PubMed] [Google Scholar]
- [18].Tamsmark TH, Koch A, Melbye M, et al. Incidence and predictors of atopic dermatitis in an open birth cohort in Sisimiut, Greenland. Acta Paediatr Int J Paediatr. 2001;90(9):982–988. doi: 10.1111/j.1651-2227.2001.tb01352.x [DOI] [PubMed] [Google Scholar]
- [19].Parisi R, Iskandar IYK, Kontopantelis E, et al. National, regional, and worldwide epidemiology of psoriasis: systematic analysis and modelling study. BMJ. 2020;369. doi: 10.1136/bmj.m1590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Abrouk M, Lee K, Brodsky M, et al. Ethnicity affects the presenting severity of psoriasis. J Am Acad Dermatol. 2017;77(1):180–182. doi: 10.1016/j.jaad.2017.02.042 [DOI] [PubMed] [Google Scholar]
- [21].Griffiths CEM, Armstrong AW, Gudjonsson JE, et al. Psoriasis. The Lancet. 2021;397(10281):1301–1315. doi: 10.1016/S0140-6736(20)32549-6 [DOI] [PubMed] [Google Scholar]
- [22].Bjerregaard P, Larsen CVL, Sørensen IK, et al. Alcohol in Greenland 1950-2018: consumption, drinking patterns, and consequences. Int J Circumpolar Health. 2020;79(1). doi: 10.1080/22423982.2020.1814550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Miller AB, Gaudette LA. Cancers of skin, bone, connective tissues, brain, eye, thyroid and other specified and unspecified sites in inuit. Acta Oncol (Madr). 1996;35(5):607–616. doi: 10.3109/02841869609096994 [DOI] [PubMed] [Google Scholar]
- [24].NORDCAN . Factsheets: skin cancer in Greenland. [cited 2024 Apr 30]. Available from: https://nordcan.iarc.fr/en/factsheets
- [25].Noonan FP, de Fabo EC. UV-B radiation: a health risk in the Arctic? Polar Res. 1999;18(2):361–365. doi: 10.3402/polar.v18i2.6596 [DOI] [Google Scholar]
- [26].Bruce M, Zulz T, Koch A. Surveillance of infectious diseases in the Arctic. Public Health. 2016;137(907):5–12. doi: 10.1016/j.puhe.2016.06.014 [DOI] [PubMed] [Google Scholar]
- [27].Mikkelsen CS, Poulsen CB, Bjerring P, et al. Skin diseases in the world’s indigenous peoples - with special focus on Greenland’s Inuit’s population. Our Dermatol Online. 2024;15(2):179–187. doi: 10.7241/ourd.20242 [DOI] [Google Scholar]


