Abstract
Introduction
Coronary artery ectasia (CAE), widenings in sections of the arteries, is a rare condition found in up to 3–5% of angiography cases. Sometimes recurrence of major adverse cardiac events (MACE) has been reported in the CAE subjects. The present systematic review aims to collect and summarize reports on whether the use of anticoagulants in addition to single antiplatelet/dual antiplatelet therapy (SAPT/DAPT) in CAE patients with significant occlusion/heavy thrombus is efficient and safe in decreasing the incidence/recurrence of MACE.
Material and methods
A systematically comprehensive search was performed covering PubMed, Scopus, ISI Web of Science, and Google Scholar databases.
Results
Twenty-five studies were found including 20 case reports, four case series, and one randomized clinical trial. Of 20 case reports 15 were male (75 %), and five were female (25 %). Of the four the case series, all showed positive outcomes after DAPT plus anticoagulant in more than 50 % of patients; two took only DAPT and 13 took anticoagulant ± DAPT, and five compared both. Cases received DAPT only experienced recurrences of MACE. The other cases were uneventful with less MACE and better outcomes after the use of anticoagulant ± DAPT. Results of these case-series included 457 CAE patients showed that more than 80 % of subjects were male, and in all studies tailored pharmacological interventions, including antiplatelet and anticoagulant (warfarin) therapies, resulted in less MACE and mortality.
Conclusion
It can be concluded that antiplatelet (SAPT/DAPT) must be applied in combination with anticoagulants to provide more efficient protection against MACE in CAE patients. However, further high-quality randomized clinical trials are needed to confirm the results.
Keywords: Coronary artery ectasia, Antiplatelet, Anticoagulant, Stenotic lesions
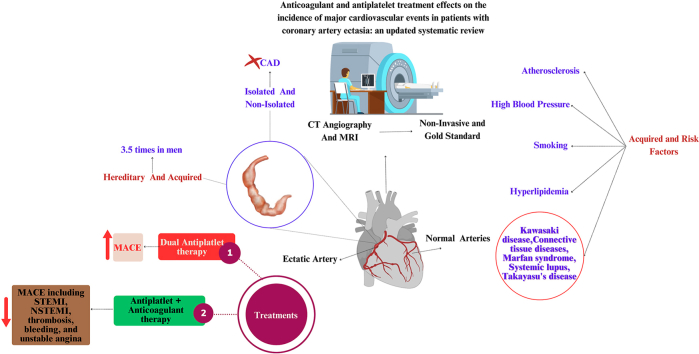
Graphical abstract
1. Introduction
Coronary artery ectasia (CAE) is an increase in the diameter of the coronary arteries, more than one and a half times its normal value. Its prevalence is up to 5 % of all coronary angiography and might induce acute myocardial infarction (AMI) sometimes.1, 2, 3 Isolated CAE was characterized as coronary ectasia without concurrent obstructive coronary artery disease (CAD) such as atherosclerosis and other cardiac problems. Isolated CAE is very rare with an angiographic frequency of 0.1–0.32 %.4
Causes of non-isolated CAE can be divided into hereditary and acquired. Acquired causes include atherosclerosis, Kawasaki disease, connective tissue diseases, Marfan syndrome, systemic lupus, Takayasu's disease, and several other causes, the most common is atherosclerosis.5,6
Atherosclerosis is associated with heightened enzymatic activity, including the upregulation of elastase and tryptase. Elevated levels of these enzymes, along with increased homocysteine, serve as predictive markers for the development of CAE in affected individuals. Notably, male gender constitutes a significant risk factor for CAE, as men are three times more likely to experience this condition compared to women.1,7, 8, 9 In a study by Wang et al included 4788 patients presenting with AMI the prevalence of CAE was 174, and 81 % of CAE subjects were male.10 Other risk factors are blood pressure,11 hyperlipidemia,12 smoking, and cocaine use.13 Diabetes plays the opposite role, so that the occurrence of CAE is less in people with diabetes.14,15
Despite the similarities in risk factors of coronary artery disease (CAD) and CAE, other histological characteristics unique to CAE patients with CAD include the severe loss of the musculoelastic media components and the relative preservation of the intima, which are regarded to be two key pathways in the pathogenesis of CAE.16, 17, 18 CAE most usually affects the right coronary artery (RCA).1
CAE is diagnosed through coronary artery angiography, MRI, and CT angiography, which in angiography is the gold standard; the blood supply disorder is evident. MRI has a diagnostic value equal to angiography for the diagnosis of CAE, which makes it a suitable method for diagnosing this disease due to its non-invasiveness.5 The aberrant coronary dilatation and flow disruptions, generally accompanied by increased thrombus burden in patients with MI, demand more effective and longer antithrombotic treatments. Dual antiplatelet (DAPT) is studied well for patients who received stent and thrombolytic.19,20 However, in the absence of sufficient large-scale data, the optimal antithrombotic therapy to prevent recurrent ischemic events in CAE patients is still unclear.21
Because there are few clinical reports, the best way to treat CAE has not yet been determined and the results in this regard are inconsistent. In the present study, we decided to systematically investigate the effect of antiplatelet and anticoagulants alone or in combination on MACE in patients with non-isolated CAE to compare the safety and outcomes.
2. Methods
The present systematic review and meta-analysis were performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement recommendations.22
2.1. Search strategy
A systematic search was conducted covering PubMed, Scopus, ISI Web of Science, and Google Scholar databases for any kind of observational studies from 2000 until April 2023 using following Medical Subject Heading [MeSH] and related keywords [“acute coronary syndrome,” OR “coronary artery ectasia,“] AND [“antiplatelet,” OR “anticoagulant,” OR “antithrombotic “OR “dual therapy,” OR “triple therapy,“]. Furthermore, a hand search was performed on the reference lists of the retrieved reviews and meta-analysis, for finding any additional references. The initial search was conducted independently by two researchers, and any discrepancies were worked out through discussion.
2.2. Selection criteria
Eligible studies included any type of studies with CAE patients as the main population and the use of anticoagulant/antiplatelet as either single therapy or dual/triple therapy as intervention.
2.3. Data extraction
Two independent authors extracted data using a standardized extraction form that includes the names of the authors, the year of publication, the number of cases, the age and gender of each patient, reported MACE for each study, the antiplatelet and anticoagulant medications, the outcome, and the follow-up period.
3. Results
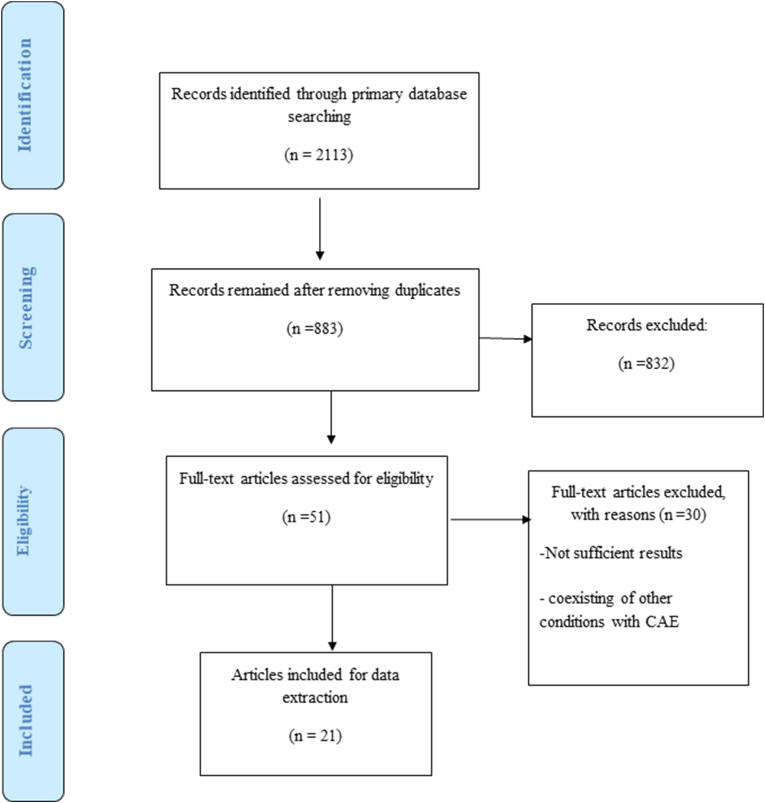
Fig. 1 shows the study selection flowchart of this study. We included all kinds of study designs with not considering the quality assessment scores due to the low number of studies and the fact that all studies except 1 were case reports/case series.
Fig. 1.
Flowchart of study selection
Finally, after removing duplicates, those with not related titles/abstracts, review papers, conferences, and those with not sufficient results 25 articles were included for data extraction and analyzing.23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46 Three of the articles reported 2 cases.26,32,37 Table 1 presented the summary of the characteristics and information related to each study/case. Four studies were case series,30,39,41,42 1 study was an on-going randomized clinical trial,24 and the rest were case reports. Of the 20 case reports 15 were male (75 %), and 5 were female (25 %). Most of the studies were from the USA and Japan.
Table 1.
Summary of the included studies.
| Author/year | Country | Population | Study design | MACE diagnosis | CAE | antiplatelet therapy (A*) |
Anticoagulant therapy (B*) | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Gunasekaran et al 201929 | USA | 317 CAE patients | Case-series | sluggish flow/RACS | High-grade CAE | Dual (Aspirin/CPG) | + | MACE and mortality decreased after using A* + B* |
| Vieyra-Herrera et al 202338 | Spain | 69 CAE patients (age: 56 + 11 years old) | Case-series | STEMI/RACS/circumflex | Right CAE | Dual (Aspirin/CPG) | + | Decreased mortality rate and recurrent MACE after using A* + B* in 58 % (40/69) |
| Araiza-Garaygordobil et al 202223 | Mexico | 60 CAE patients |
Single-center randomized clinical trial | RACS/bleeding | Low & high-grade CAE | Dual vs Mono |
- vs + (Rivaroxaban) | NA/(on-going study) |
| Desai S, et al 202227 | USA | 60 years old CAE Male |
Case-report | NSTEMI | RCA/LAD/LCx | Dual (Aspirin/CPG) after 2 weeks only CPG | - vs + (Apixaban) | Replacement of aspirin with apixaban improved and decreased NSTEMI and chest pain (13 months follow-up) |
| Liu et al 202232 | China | 60 years old CAE Male |
Case-report | STEMI/thrombus in RCAS | Right CAE | Dual (Aspirin/CPG) | + (Low molecular weight heparin) |
Decreased mortality rate and recurrent MACE after using A* + B* (4 years follow-up) |
| Damay et al 201926 | Indonesia | 61 years old CAE Male |
Case-report | Unstable angina/RACS | Right CAE | Dual (Aspirin/CPG) | + (Warfarin) | Unstable angina improved better using A* +B* compared to A* (6 months follow-up) |
| Thor et al 201942 | Malaysia | 56-year-old male patient | Case-report | STEMI | RCA with abundant thrombus | Dual (Aspirin/CPG) | + (dabigatran) | Remained asymptomatic after 1 month A* + B* followed by a single antiplatelets and anticoagulation for the next 6 month |
| Tomioka et al 201635 | Japan | 78 years old CAE Female |
Case-report | 2 times recurrent myocardial infarction (MI) | Right CAE | Dual (Aspirin/CPG) | + (Heparin) | Recurrent MI improved successfully using A* + B* (12 months follow-up) |
| Choi et al 201843 | Canada | 58 years old CAE Male |
Case-report | STEMI | Atherosclerotic CAE | Mono (CPG) | + (IV eptifibatide + heparin) | All MACE improved successfully after A* + B* (2 months and 11 months follow-up) |
| Abugroun et al 201722 | USA | 65 years old CAE Male |
Case-report | STEMI/RCAS | Kawasaki CAE | Dual (Aspirin/CPG) | - vs + (Warfarin) | MACE was improved and managed better by the addition of B* to A* |
| Venuti & Mangano, 202237 | USA | 31 years old CAE Male |
Case-report | STEMI/RCAS | severely diffuse right CAE | Dual (Aspirin/CPG) | + (Rivaroxaban) | MACE was not reported after the use of A* + B* (2 months follow-up) |
| Bhuiyan et al 202224 | USA | 47 years old CAE Male |
Case-report | Recurrent STEMI/RCAS | Right CAE | Dual (Aspirin/CPG) | + Heparin (prolonged therapy) |
No further recurrence of MI after A* + B* |
| Latt et al 201739 | USA | 35 years old CAE Male |
Case-report | STEMI | two-vessel CAE | Dual (Aspirin/CPG) | – | MACE was not reported after the use of A* |
| Mrdović et al 200433 | Serbia and Montenegro | 47 years old CAE Male |
Case-report | STEMI/recurrent MI | Right CAE | Dual (Aspirin/CPG) | – | MACE was not resolved after the use of A* |
| Boles et al 201325 | Sweden | 61 years old CAE Female |
Case-report | STEMI/clot beneath the stent in the ectatic area | Right CAE | Dual (Aspirin/CPG)/Mono after 6 weeks (aspirin) | - vs + | No further recurrence of MI after A* + B* with A* as a priority |
| Boles et al 2013 (25) | Sweden | 55 years old CAE Male |
Case-report | STEMI | Dual (Aspirin/CPG) | - vs + (Warfarin) | No further recurrence of MI after A* + B* with A* as a priority | |
| Furugen, & Takagawa, 201228 |
Japan | 78 years old CAE Female |
Case-report | NSTEMI/ ACS due to thrombogenesis. |
LCx CAE |
Dual (Aspirin/CPG) | + (recombinant tissue-plasminogen activator + heparin) | No further recurrence of MACE after using A* + B* (3 months follow-up) |
| Tuncer et al 200836 | Netherlands | 70 years old CAE Male |
Case-report | NSTEMI | LCx CAE |
Mono (CPG) | + (Warfarin: moderate intensity) | No further recurrence of MACE after using A* + B* (3 months follow-up) |
| Tuncer et al 200836 | Netherlands | 39 years old CAE Male |
Case-report | STEMI | LCx CAE |
Mono (Aspirin) after 3 months changed to Dual (Aspirin/CPG) |
+ (Warfarin) after 3 months stopped | No further recurrence of MACE (6 weeks, 3 months, and 8 months follow-up) |
| Doi et al201741 | Japan | 1698 MI patients | Case-series | MI | + | + Warfarin was administered to 19 patients |
No recurrence of MACE in patients who took warfarin and achieved the %TTR (≥60 %) after 49-month | |
| Grigorov. 200940 |
South Africa | 2000 total/20 patients with CAE types I, II and III | Case-series | Stable angina (45 %), unstable angina or non-STEMI (25 %), and STEMI (30 %) | RCA in 95 % LAD in 65 % Cx in 50 % |
75 % with Warfarin | All patients on warfarin had a controlled prothrombin index (PI) between 30 and 50 % |
MACE: major adverse cardiovascular events.
RACS: Recurrent ACS.
A*: Antiplatelet therapy.
B*: Anticoagulant therapy.
RCA: Right coronary artery.
STEMI: ST-segment elevation myocardial infarction.
CPG: Clopidogrel.
LCx: left circumflex artery.
RCA: right coronary artery.
4. Discussion
While dual antiplatelet therapy (DAPT) is a standard treatment for patients with coronary artery ectasia (CAE), the utilization of anticoagulation in these individuals is not widely endorsed at present.28 Certain studies, focusing on notable flow disturbances within the ectatic segments, propose that anticoagulation should be prioritized as the primary therapy.47,48 The last systematic review to check the necessity of using anticoagulants in CAE patients included 13 studies until 2019.49 We included 25 studies in our systematic review, including 20 case reports 9 after 2019,27,28,33,38,43, 44, 45, 46,50,51 4 case-series studies (2 after 2019), and one ongoing randomized clinical trial.24
4.1. Case-reports
The population of male CAE patients of case-reports overall was 3 times more than females (75 % vs. 25 %), aligning with earlier research observations.1,8,9 All case-report studies included in the analysis, which employed a combination of antiplatelet and anticoagulant therapy, documented no recurrence of MACE, encompassing ST-elevation myocardial infarction (STEMI), non-ST-elevation myocardial infarction (NSTEMI), thrombosis, bleeding, and unstable angina. Two cases reported by Boles et al.26 and Desai et al.28 showed that replacement of dual antiplatelet therapy with mono antiplatelet therapy plus the use of anticoagulant therapy resulted in better management of MACE recurrence. Mrdović et al found that the use of only dual antiplatelet therapy was not successful in preventing MACE.34 Four other cases that also used mono antiplatelet therapy plus the use of anticoagulant therapy showed no further recurrence of MACE after different follow-up durations.32,37,52 Liu et al in their study showed that a combination of antiplatelet/anticoagulant therapy even after 4 years decreased the rate of mortality and MACE recurrence. All studies after 2019,25,28,33,38 showed that they used a combination of antiplatelet therapy and anticoagulant therapy successfully in preventing the recurrence of MACE. Compared with studies before 2019 (at least 2 of them reported no use of anticoagulants,34,40 it can be noted that physicians are increasingly preferring to use anticoagulants in conjunction with antiplatelets.
4.2. Case-series
In a case-Seri study of 20 CAE subjects by Grigorov (2009) in South Africa,41 most of the patients (95 %) were male. According to angiographic findings, none of the patients were recommended for surgery. Instead, 50 % underwent angioplasty, with or without a stent, while the remaining patients received solely medical therapy including ASA therapy of 160 mg/day (100 %), and majority of patients (75 %), regardless of the approach utilized, initiated treatment with warfarin and no mortality was reported.41 In another study by Gunasekaran et al, involving 317 patients with coronary artery ectasia (CAE), it was observed that either DAPT or oral anticoagulation usage correlated with a decreased occurrence of acute coronary syndrome (ACS) compared to those not on these therapies (17 % vs. 34 %, P = 0.03 and 29 % vs. 42 %, P = 0.02, respectively).30 In a case-seri study by Doi et al of the 51 CAE patients, 19 were prescribed warfarin upon discharge. Among these, 8 patients attained a percent time in the target therapeutic range (%TTR) of 60 % or higher. Notably, none of these patients experienced MACE during the observation period. Conversely, patients with a %TTR below 60 % or those not on warfarin exhibited a significantly higher incidence of MACE, with 14 out of 43 patients affected (33 %; P = 0.03). Results of these case-series included 457 CAE patients showed the importance of tailored pharmacological interventions, including antiplatelet and anticoagulant therapies, in managing CAE and mitigating associated cardiovascular risks.
4.3. Mechanisms and pathophysiological insights
CAE is a condition characterized by localized or diffuse dilation of coronary arteries. While atherosclerosis can contribute to CAE, it's not typically associated with plaque rupture, which is a common feature of acute coronary syndromes like MI. Instead, CAE is primarily characterized by the dilation of coronary arteries, which can lead to various complications such as stasis of blood and consequently distal embolization. The dilation of coronary arteries can lead turbulence and slow blood flow within the affected vessels. This stasis of blood can contribute to the formation of thrombi (blood clots) within the dilated segments. Consequently, thrombi formed within the dilated coronary arteries can dislodge and embolize, meaning they can travel downstream and occlude smaller blood vessels. This distal embolization can result in myocardial ischemia or infarction if the affected vessels supply blood to critical areas of the heart.53,54
There are some potential reasons that why adding an anticoagulant to dual antiplatelet therapy (DAPT) in the context of CAE could be effective. In CAE, there is abnormal dilatation of the coronary arteries, which can lead to disturbed blood flow and turbulent flow patterns. These conditions predispose individuals to thrombus formation within the ectatic segment. Anticoagulants such as heparin or direct oral anticoagulants (DOACs) can prevent the formation and propagation of thrombi by inhibiting the coagulation cascade, complementing the antiplatelet effect of DAPT. On the other hand, CAE is associated with endothelial dysfunction and anticoagulants may help improve endothelial function by reducing inflammation and oxidative stress, thus promoting vasodilation and reducing the risk of thrombus formation.
Even in the absence of significant stenosis, CAE can lead to microembolization of thrombotic material, which can cause MI. Anticoagulants can help prevent the formation of microemboli and reduce the risk of ischemic events. It is worth to mention that the choice to add anticoagulation to DAPT may also depend on individual patient factors such as age, comorbidities, bleeding risk, and other concurrent medications. Some patients with CAE may have additional risk factors for thrombosis, such as atrial fibrillation or hypercoagulable states, which could warrant the use of anticoagulants in addition to antiplatelet therapy.46
From another point of the view, cerine proteases, are a class of enzymes that play a crucial role in the coagulation cascade, which is the series of biochemical reactions that leads to the formation of blood clots. These enzymes act as catalytic components, facilitating the conversion of inactive proenzymes into active forms that ultimately generate fibrin, the main component of blood clots. In the contest of CAE there is evidence suggesting that levels of serine proteases may be elevated. This elevation can contribute to a procoagulant state, meaning it promotes blood clot formation. This heightened procoagulant state in CAE patients increases the risk of thrombus formation within the ectatic coronary arteries, potentially leading to adverse cardiovascular events such as myocardial infarction or ischemia. Additionally, research has revealed elevated levels of cathepsins in CAE patients. Cathepsins are a group of protease enzymes involved in various cellular processes, including the degradation of proteins. Elevated levels of cathepsins can contribute to inflammation, plaque instability, and endothelial dysfunction, all of which are implicated in the pathogenesis of CAE. Given the elevated levels of both serine proteases and cathepsins in CAE patients, there is a concern that these individuals may have an increased propensity for thrombosis. Therefore, utilizing anticoagulation therapy alongside antiplatelet therapy in CAE patients aims to counteract these procoagulant factors and reduce the risk of thrombus formation. Anticoagulants inhibit the coagulation cascade by targeting various components involved in blood clot formation, such as thrombin or factor Xa. By doing so, they help to prevent the formation and propagation of blood clots. When used in conjunction with antiplatelet therapy, which inhibits platelet activation and aggregation, anticoagulants provide a more comprehensive approach to reducing the risk of thrombotic events in CAE patients.26,55, 56, 57
The exploration and investigation of the management of CAE with significant occlusion represent a crucial and evolving area of research in cardiovascular medicine. This specific focus on CAE with significant occlusion underscores the imperative need for advanced strategies and interventions tailored to address the unique challenges posed by this complex condition. The future of research holds promise for groundbreaking advancements in both diagnostic and therapeutic modalities. Researchers are anticipated to delve deeper into the underlying mechanisms, risk factors, and optimal treatment approaches for this specific subset of CAE cases. Cutting-edge imaging technologies, innovative interventional procedures, and personalized treatment regimens are likely to emerge as key areas of exploration, aiming to enhance clinical outcomes and quality of life for affected individuals. Furthermore, collaborative efforts among multidisciplinary teams comprising cardiologists, radiologists, and researchers will be pivotal in unraveling the intricacies of CAE with significant occlusion. As the field progresses, a comprehensive understanding of the pathophysiology and targeted interventions will pave the way for more effective management strategies, ultimately contributing to improved patient prognosis and a reduction in the burden of cardiovascular disease. Continuous monitoring of emerging research findings in this domain is essential for staying abreast of the evolving landscape and ensuring the translation of knowledge into enhanced clinical practices.
5. Conclusion
In conclusion, the incorporation of anticoagulants alongside antiplatelet therapy represents a promising avenue for the management of non-isolated coronary artery ectasia with significant occlusion. Future research endeavors should focus on elucidating the optimal combination, dosages, and duration of these therapies to strike a balance between efficacy and safety. As the field progresses, the integration of anticoagulants into the treatment paradigm holds the potential to significantly improve patient outcomes, reducing the burden of cardiovascular events and mortality in this challenging subset of CAE patients.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Swaye P.S., Fisher L.D., Litwin P., et al. Aneurysmal coronary artery disease. Circulation. 1983;67(1):134–138. doi: 10.1161/01.cir.67.1.134. [DOI] [PubMed] [Google Scholar]
- 2.Dahhan A. Coronary artery ectasia in atherosclerotic coronary artery disease, inflammatory disorders, and sickle cell disease. Cardiovasc Ther. 2015;33(2):79–88. doi: 10.1111/1755-5922.12106. [DOI] [PubMed] [Google Scholar]
- 3.Markis J.E., Joffe C.D., Cohn P.F., Feen D.J., Herman M.V., Gorlin R. Clinical significance of coronary arterial ectasia. Am J Cardiol. 1976;37(2):217–222. doi: 10.1016/0002-9149(76)90315-5. [DOI] [PubMed] [Google Scholar]
- 4.Malviya A., Jha P.K., Mishra A. Isolated coronary artery ectasia: clinical, angiographic, and follow up characteristics. Indian Heart J. 2017;69(5):619–623. doi: 10.1016/j.ihj.2016.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roberts W.C. Natural history, clinical consequences, and morphologic features of coronary arterial aneurysms in adults. Am J Cardiol. 2011;108(6):814–821. doi: 10.1016/j.amjcard.2011.05.009. [DOI] [PubMed] [Google Scholar]
- 6.Newburger J.W., Takahashi M., Burns J.C. Kawasaki disease. J Am Coll Cardiol. 2016;67(14):1738–1749. doi: 10.1016/j.jacc.2015.12.073. [DOI] [PubMed] [Google Scholar]
- 7.Antoniadis A.P., Chatzizisis Y.S., Giannoglou G.D. Pathogenetic mechanisms of coronary ectasia. Int J Cardiol. 2008;130(3):335–343. doi: 10.1016/j.ijcard.2008.05.071. [DOI] [PubMed] [Google Scholar]
- 8.Demopoulos V.P., Olympios C.D., Fakiolas C.N., et al. The natural history of aneurysmal coronary artery disease. Heart. 1997;78(2):136–141. doi: 10.1136/hrt.78.2.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Giannoglou G.D., Antoniadis A.P., Chatzizisis Y.S., Damvopoulou E., Parcharidis G.E., Louridas G.E. Prevalence of ectasia in human coronary arteries in patients in northern Greece referred for coronary angiography. Am J Cardiol. 2006;98(3):314–318. doi: 10.1016/j.amjcard.2006.02.034. [DOI] [PubMed] [Google Scholar]
- 10.Wang X., Montero-Cabezas J.M., Mandurino-Mirizzi A., et al. Prevalence and long-term outcomes of patients with coronary artery ectasia presenting with acute myocardial infarction. Am J Cardiol. 2021;156:9–15. doi: 10.1016/j.amjcard.2021.06.037. [DOI] [PubMed] [Google Scholar]
- 11.Bahremand M., Zereshki E., Matin B.K., Rezaei M., Omrani H. Hypertension and coronary artery ectasia: a systematic review and meta-analysis study. Clinical hypertension. 2021;27(1):1–10. doi: 10.1186/s40885-021-00170-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Qin Y., Tang C., Ma C., Yan G. Risk factors for coronary artery ectasia and the relationship between hyperlipidemia and coronary artery ectasia. Coron Artery Dis. 2019;30(3):211–215. doi: 10.1097/MCA.0000000000000709. [DOI] [PubMed] [Google Scholar]
- 13.Satran A., Bart B.A., Henry C.R., et al. Increased prevalence of coronary artery aneurysms among cocaine users. Circulation. 2005;111(19):2424–2429. doi: 10.1161/01.CIR.0000165121.50527.DE. [DOI] [PubMed] [Google Scholar]
- 14.Androulakis A.E., Andrikopoulos G.K., Kartalis A.N., et al. Relation of coronary artery ectasia to diabetes mellitus. Am J Cardiol. 2004;93(9):1165–1167. doi: 10.1016/j.amjcard.2004.01.049. [DOI] [PubMed] [Google Scholar]
- 15.Pinar Bermúdez E., López Palop R., Lozano Martínez-Luengas I., et al. [Coronary ectasia: prevalence, and clinical and angiographic characteristics] Rev Esp Cardiol. 2003;56(5):473–479. doi: 10.1016/s0300-8932(03)76902-4. [DOI] [PubMed] [Google Scholar]
- 16.Lamblin N., Bauters C., Hermant X., Lablanche J.M., Helbecque N., Amouyel P. Polymorphisms in the promoter regions of MMP-2, MMP-3, MMP-9 and MMP-12 genes as determinants of aneurysmal coronary artery disease. J Am Coll Cardiol. 2002;40(1):43–48. doi: 10.1016/s0735-1097(02)01909-5. [DOI] [PubMed] [Google Scholar]
- 17.Finkelstein A., Michowitz Y., Abashidze A., Miller H., Keren G., George J. Temporal association between circulating proteolytic, inflammatory and neurohormonal markers in patients with coronary ectasia. Atherosclerosis. 2005;179(2):353–359. doi: 10.1016/j.atherosclerosis.2004.10.020. [DOI] [PubMed] [Google Scholar]
- 18.Turhan H., Erbay A.R., Yasar A.S., et al. Plasma soluble adhesion molecules; intercellular adhesion molecule-1, vascular cell adhesion molecule-1 and E-selectin levels in patients with isolated coronary artery ectasia. Coron Artery Dis. 2005;16(1):45–50. doi: 10.1097/00019501-200502000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Magnani G., Valgimigli M. Dual antiplatelet therapy after drug-eluting stent implantation. Intervent Cardiol. 2016;11(1):51–53. doi: 10.15420/icr.2015:17:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Luo L., Wang S., Tang K., et al. Efficacy and safety of dual antiplatelet therapy after percutaneous coronary drug-eluting stenting: a network meta-analysis. Medicine (Baltim) 2022;101(42) doi: 10.1097/MD.0000000000031158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Esposito L., Di Maio M., Silverio A., et al. Treatment and outcome of patients with coronary artery ectasia: current evidence and novel opportunities for an old dilemma. Frontiers in Cardiovascular Medicine. 2022;8 doi: 10.3389/fcvm.2021.805727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 23.Abugroun A., Vilchez D., Hallak O., Shahrrava A. A history of Kawasaki disease from childhood and coronary artery ectasia with recurrent st elevation myocardial infarction: a therapeutic challenge. Cardiol Res. 2017;8(6):344–348. doi: 10.14740/cr641w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Araiza-Garaygordobil D., Gopar-Nieto R., Sierra-Lara Martínez D., et al. Dual antiplatelet therapy versus antiplatelet monotherapy plus oral anticoagulation in patients with acute coronary syndrome and coronary artery ectasia: design and rationale of OVER-TIME randomized clinical trial. High Blood Pres Cardiovasc Prev. 2022;29(5):463–468. doi: 10.1007/s40292-022-00535-4. [DOI] [PubMed] [Google Scholar]
- 25.Bhuiyan M., Badar F., Ashraf A., Chryssos E.D., Iftikhar A. Recurrent ST-elevation myocardial infarction (STEMI) in coronary artery aneurysm secondary to atherosclerosis. Cureus. 2022;14(9) doi: 10.7759/cureus.28757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boles U., Rakhit R., Shiu M.F., Patel K., Henein M. Coronary artery ectasia as a culprit for acute myocardial infarction: review of pathophysiology and management. Anadolu Kardiyol Derg. 2013;13(7):695–701. doi: 10.5152/akd.2013.227. [DOI] [PubMed] [Google Scholar]
- 27.Damay V., Pranata R., Wiharja W. Recurrent acute coronary syndrome in a patient with right coronary artery ectasia: a case report. J Med Case Rep. 2019;13(1):78. doi: 10.1186/s13256-019-1979-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Desai S.D.J., Klag J. Coronary artery ectasia and oral anticoagulation: a case report. Int J Clin Cardiol. 2022;9(245) [Google Scholar]
- 29.Furugen M., Takagawa Y. Staged interventional management of a massive thrombus related to coronary artery ectasia in acute coronary syndrome. Cardiovasc Interv Ther. 2012;27(1):57–61. doi: 10.1007/s12928-011-0083-y. [DOI] [PubMed] [Google Scholar]
- 30.Gunasekaran P., Stanojevic D., Drees T., et al. Prognostic significance, angiographic characteristics and impact of antithrombotic and anticoagulant therapy on outcomes in high versus low grade coronary artery ectasia: a long-term follow-up study. Cathet Cardiovasc Interv. 2019;93(7):1219–1227. doi: 10.1002/ccd.27929. [DOI] [PubMed] [Google Scholar]
- 31.Koyama Y., Miura M., Kobayashi T., et al. A registry study of Kawasaki disease patients with coronary artery aneurysms (KIDCAR): a report on a multicenter prospective registry study three years after commencement. Eur J Pediatr. 2023;182(2):633–640. doi: 10.1007/s00431-022-04719-x. [DOI] [PubMed] [Google Scholar]
- 32.Lima B., Varma S.K., Lowe J.E. Nonsurgical management of left main coronary artery aneurysms: report of 2 cases and review of the literature. Tex Heart Inst J. 2006;33(3):376–379. [PMC free article] [PubMed] [Google Scholar]
- 33.Liu R.F., Gao X.Y., Liang S.W., Zhao H.Q. Antithrombotic treatment strategy for patients with coronary artery ectasia and acute myocardial infarction: a case report. World J Clin Cases. 2022;10(12):3936–3943. doi: 10.12998/wjcc.v10.i12.3936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mrdović I., Jozić T., Asanin M., Perunicić J., Ostojić M. Myocardial reinfarction in a patient with coronary ectasia. Cardiology. 2004;102(1):32–34. doi: 10.1159/000077000. [DOI] [PubMed] [Google Scholar]
- 35.Okada T., Endo A., Ito S., et al. Acute coronary syndrome in a puerperal patient with coronary artery ectasia due to a coronary artery fistula. Intern Med. 2016;55(18):2635–2638. doi: 10.2169/internalmedicine.55.6597. [DOI] [PubMed] [Google Scholar]
- 36.Tomioka T., Takeuchi S., Ito Y., Shioiri H., Koyama J., Inoue K. Recurrent acute myocardial infarction in a patient with severe coronary artery ectasia: implication of antithrombotic therapy. Am J Case Rep. 2016;17:939–943. doi: 10.12659/AJCR.900474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tuncer C., Sokmen G., Sokmen A., Suner A. Diffuse coronary ectasia and intracoronary thrombus involving left circumflex coronary artery and presenting as acute coronary syndrome: report of two cases. Int J Cardiol. 2008;128(1):e25–e27. doi: 10.1016/j.ijcard.2007.04.158. [DOI] [PubMed] [Google Scholar]
- 38.Venuti N., Mangano A. Severe coronary artery ectasia in a 31-year-old presenting with an inferior ST-elevation myocardial infarction: a case report. Cureus. 2022;14(4) doi: 10.7759/cureus.24340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vieyra-Herrera G., García-Navarrete M.G., Dámazo-Escobedo C.A., González-Pacheco H., Rodríguez-Chavez L.L., Silva-Ruz C. Outlook of coronary ectasia at the national institute of cardiology ignacio chávez: a cross-sectional study. Arch Cardiol Mex. 2023;93(2):197–202. doi: 10.24875/ACM.21000380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Latt H., Aung S., Kyaw K., Seher R. Coronary artery ectasia presenting with acute inferior wall myocardial infarction in a young adult. J Community Hosp Intern Med Perspect. 2017;7(4):262–264. doi: 10.1080/20009666.2017.1369376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Grigorov V. Invasive and anticoagulant treatment for coronary ectasia: a single operator's experience in a tertiary hospital in South Africa. Cardiovasc J Afr. 2009;20(4):229–232. [PMC free article] [PubMed] [Google Scholar]
- 42.Doi T., Kataoka Y., Noguchi T., et al. Coronary artery ectasia predicts future cardiac events in patients with acute myocardial infarction. Arterioscler Thromb Vasc Biol. 2017;37(12):2350–2355. doi: 10.1161/ATVBAHA.117.309683. [DOI] [PubMed] [Google Scholar]
- 43.Saraswat A., Rahman A., Batra R. Intracoronary administration of thrombolysis for severe coronary artery ectasia presenting as an acute inferior ST-segment elevation myocardial infarction. J Invasive Cardiol. 2017;29(10):E153. [PubMed] [Google Scholar]
- 44.Singal S., Parulkar Sanchita S., Parulkar Anshul B., Tuohy C., Saad M. Acute st-elevation myocardial infarction: a case of coronary artery ectasia and intracoronary thrombolysis. J Am Coll Cardiol. 2022;79(9_Supplement):2993. [Google Scholar]
- 45.Jafaripour I., Ansari Ramandi M.M., Gholami A., Pourkia R., Amin K. Successful intracoronary thrombolysis in a patient with anterior myocardial infarction and large thrombus burden associated with coronary artery ectasia. Clinical Case Reports. 2021;9(1):93–97. doi: 10.1002/ccr3.3449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee J., Ramkumar S., Khav N., Dundon B.K. Coronary artery ectasia presenting with ST-elevation myocardial infarction in a young indigenous man: a case report. European Heart Journal - Case Reports. 2020;4(5):1–5. doi: 10.1093/ehjcr/ytaa253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sorrell V.L., Davis M.J., Bove A.A. Origins of coronary artery ectasia. Lancet. 1996;347(8995):136–137. doi: 10.1016/s0140-6736(96)90335-9. [DOI] [PubMed] [Google Scholar]
- 48.Swanton R.H., Thomas M.L., Coltart D.J., Jenkins B.S., Webb-Peploe M.M., Williams B.T. Coronary artery ectasia--a variant of occlusive coronary arteriosclerosis. Br Heart J. 1978;40(4):393–400. doi: 10.1136/hrt.40.4.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pranata R., Yonas E., Chintya V., Alkatiri A.A. Is anticoagulant necessary in patients with coronary artery ectasia presenting with acute coronary syndrome? A systematic review of case reports. Int J Angiol. 2019;28(4):231–236. doi: 10.1055/s-0039-1692706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Thor T.G., Chuang V.T.G., Lam K.H. Dabigatran as the anticoagulant of choice for treating acute myocardial infarction in a patient with ectatic coronary artery and thrombus. ASEAN Heart Journal. 2019;26(4):1–3. [Google Scholar]
- 51.Al-Zakhari R., Aljammali S., Galligan S., Rotatori F. Coronary artery ectasia: a case report discussing the causes, diagnosis, and treatment. Cureus. 2021;13(4) doi: 10.7759/cureus.14431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Choi H.J.S., Luong C., Fung A., Tsang T.S.M. ST-elevation myocardial infarction in coronary ectasia: a case report. Diseases. 2018;6(4) doi: 10.3390/diseases6040104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Genena K., Ali M., Christmas D., Siu H. Coronary artery ectasia presenting as a non-ST elevation myocardial infarction in a young adult: case presentation and literature review. Case Rep Cardiol. 2018;2018 doi: 10.1155/2018/9817812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Esposito L., Di Maio M., Silverio A., et al. Treatment and outcome of patients with coronary artery ectasia: current evidence and novel opportunities for an old dilemma. Front Cardiovasc Med. 2021;8 doi: 10.3389/fcvm.2021.805727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Devabhaktuni S., Mercedes A., Diep J., Ahsan C. Coronary artery ectasia-A review of current literature. Curr Cardiol Rev. 2016;12(4):318–323. doi: 10.2174/1573403X12666160504100159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liu J., Sukhova G.K., Yang J.T., et al. Cathepsin L expression and regulation in human abdominal aortic aneurysm, atherosclerosis, and vascular cells. Atherosclerosis. 2006;184(2):302–311. doi: 10.1016/j.atherosclerosis.2005.05.012. [DOI] [PubMed] [Google Scholar]
- 57.Erden I., Erden E.C., Ozhan H., Karabulut A., Ordu S., Yazici M. Outcome of primary percutaneous intervention in patients with infarct-related coronary artery ectasia. Angiology. 2010;61(6):574–579. doi: 10.1177/0003319709361197. [DOI] [PubMed] [Google Scholar]