Abstract
The prevalence pattern of hypertension in developing countries is different from that in the developed countries. In India, a very large, populous and typical developing country, community surveys have documented that between three and six decades, prevalence of hypertension has increased by about 30 times among urban dwellers and by about 10 times among the rural inhabitants. Various factors might have contributed to this rising trend and among others, consequences of urbanization such as change in life style pattern, diet and stress, increased population and shrinking employment have been implicated. In this paper, we study the prevalence of hypertension in an urban community of India using the JNC VII criteria, with the aim of identifying the risk factors and suggesting intervention strategies. A total of 1609 respondents out of 1662 individuals participated in our cross-sectional survey of validated and structured questionnaire followed by blood pressure measurement. Results showed pre-hypertensive levels of blood pressures among 35.8% of the participants in systolic group (120-139mm of Hg) and 47.7% in diastolic group (80-89 mm of Hg). Systolic hypertension (140 mm of Hg) was present in 40.9% and diastolic hypertension (90 mm of Hg) in 29.3% of the participants. Age and sex-specific prevalence of hypertension showed progressive rise of systolic and diastolic hypertension in women when compared to men. Men showed progressive rise in systolic hypertension beyond fifth decade of life. Bivariate analysis showed significant relationship of hypertension with age, sedentary occupation, body mass index (BMI), diet, ischemic heart disease, and smoking. Multivariate analysis revealed age and BMI as risk factors, and non-vegetarian diet as protective factor with respect to hypertension. Prevalence of prehypertensives was high among younger subjects - particularly students and laborers who need special attention. Role of non-vegetarian diet as a protective factor might have been related to fish-eating behavior of the sample population, who also use mustard oil as cooking medium - both of which have significant level of essential polyunsaturated fatty acids. The observed prevalence of hypertension in this study and other studies suggest the need for a comprehensive national policy to control hypertension in India, and, in other similar developing countries.
Keywords: Hypertension, eastern India, urban study, JNC-VII criteria, prehypertensives, non-vegetarian diet, developing countries
1. BACKGROUND
An epidemiological shift in the prevalence of hypertension in developing countries as compared to developed countries has been observed 1,2. Studies from India and Bangladesh have shown upward trend in the prevalence of hypertension 3. India is a vast country with a heterogeneous and young population. Till recent past, control and prevention of communicable diseases was emphasized. Recently, attention has shifted to control and prevention of non-communicable diseases including stroke, hypertension and coronary artery disease at the national level in view of the rising trends. Community surveys from different regions and various ethnic populations are instrumental to formulate national consensus-driven policies to counteract the rising trend of non-communicable diseases. The prevalence of hypertension has increased by 30 times among the urban population over a period of 55 years and about 10 times among the rural population over a period of 36 years 4. Various hypotheses have been put forward to explain this rising trend and among these, consequences of urbanization such as change in life style pattern, diet and stress have been implicated. The current urbanization rate in India is 35% as compared to 15% in the 1950. With growing urbanization, socio-developmental changes have taken place over last 40-50 years. Dramatic changes in life style from traditional to modern have lead to physical inactivity due to technological advances. Rising affluence has modified the dietary pattern characterized by increased consumption of diets rich in fat, sugar and calories. Furthermore, increasing population growth at the current rate of about 2% in each year and technological advances have shrunken the employment opportunities particularly among young generation – leading to stress and hypertension in young persons, including students and laborers. The primary objective of this project was to study the prevalence of hypertension in an urban population in West Bengal- an eastern state of India - using the recently published “The Seventh Report Of Joint National committee on Prevention, Detection, Evaluation and Treatment of High blood Pressure (JNC-VII) criteria” 5. Additionally, the study aimed to identify the various risk factors for hypertension with the purpose to suggest possible interventions based on the risk factor analysis.
2. METHODOLOGY
Place of survey and the population
Malda, a district town in the state of West Bengal, had been the place of survey. Demographic characteristic of the sample population is given in table 1. The place has a tropical climate and is made of alluvial soil in the Gangetic plain. The population is stable and usually consumes mixed diet consisting of rice, fish as the chief protein component and mustard oil as the main cooking medium.
Table 1.
Demographic, socioeconomic, and outcome variables
| Variable | Category | Frequency | Percent |
|---|---|---|---|
| Age in Years | < 20 | 69309 | 23.5 (23.2%)* |
| 20-29 | |||
| 30-39 | 344 | 21.4 ( 27.1%)* | |
| 40-49 | 351 | 21.8 ( 18.5%)* | |
| 50-59 | 261 | 16.2 ( 15.2%)* | |
| 60-69 | 166 | 10.3 (9.9%)* | |
| >= 70 | 109 | 6.8 ( 6.1%)* | |
| Gender | woman | 742 | 46.1 |
| man | 867 | 53.9 | |
| Occupation | student | 110 | 6.8 |
| manual worker | 368 | 22.9 | |
| housewife | 574 | 35.7 | |
| sedentary worker | 391 | 24.3 | |
| Missing | 166 | 10.3 | |
| Body Mass Index in Quantiles | 20th percentile | 18.4 | |
| 40th percentile | 20.7 | ||
| 60th percentile | 22.9 | ||
| 80th percentile | 25.6 | ||
| family history | Negative | 1167 | 72.5 |
| Positive | 442 | 27.5 | |
| Salt Intake | No | 1184 | 73.6 |
| Yes | 425 | 26.4 |
*- Proportionate national data
Population of English bazaar municipality under Malda Town is 1,61,448 (Men- 51.36% : women- 48.63%) according to census report (Census, 2001). It consists of twenty-five wards. About 1% of the population above the age of 18 years was studied in 2001. Initially, families were randomly selected from an administrative database on families residing in the locality. After selection of the families, all available members of the selected family who were at 18 years of age or above at the time of the study were then included for the door-to-door survey.
Definition of hypertension (Based on JNC-VII criteria)
Normal- Systolic and diastolic < 120/80
Prehypertensives: systolic 120-139 or diastolic 80-89 mm of Hg
Stage-1 hypertensives: systolic 140-159 or diastolic 90-99 mm of Hg
Stage-2 hypertensives: systolic 160 or diastolic 100 mm of Hg
The participants with history of hypertension and on antihypertensive drugs were also labeled as hypertensives.
Questionnaire
The following information was collected from each subject through a validated questionnaire administered by the volunteers: age, sex, occupation, income status, weight, height, pattern of salt intake, dietary pattern, history of diabetes, family history of hypertension, past history of any examination of blood pressure and hypertension, or any its complications, any symptom referable to target organ dysfunction, previous and present treatment profile, and addictions.
Methods
The volunteers had administered the structured questionnaires. After verifying the questionnaire, the doctors measured the blood pressure for each participant.
Blood pressure Measurement: Two graduate physicians of similar backgrounds with over 20 years of clinical experience (authors SD and KS) measured the blood pressure for each participant, using the auscultatory method with a standardized calibrated mercury column type sphygmomanometer and an appropriate sized cuff encircling at least 80% of the arm in the seated posture, with feet on the floor and arm supported at heart level. Following a standardized protocol, they made two separate measurements and recorded the average of the two measurements after proper rest and due explanation to the examined participant about the objective of the study. In some cases, where high blood pressure was recorded for the first time, the physicians checked the blood pressure more than twice and took the average of the two close readings. Systolic BP is the point at which the first of 2 or more sounds is heard (phase I) and diastolic BP is the point before the disappearance of sounds (phase 5).
All participants above 40 years underwent electrocardiograms (ECG), irrespective of level of blood pressure. Participants who were below 40 years of age, only those who had hypertension and complained of typical precordial pain suggestive of ischemic heart disease, had ECGs. Participants with typical central chest pain, suggestive ECG changes and on anti ischemic drugs are considered to be suffering from myocardial ischemia. Salt intake was assessed from the amount of salt used in cooking and extra salt used during meal.
Statistical Analysis
We used EPI-INFO-2002 software for data entry and analysis. We applied chi-square test to find out the results at 5% significance for the select risk factors and outcome variables. We put the significant variables from the bivariate analysis into a series of stepwise, unconditional multivariate logistic regression and calculated the Odds Ratios with 95% confidence intervals (CI) to assess the association between these variables and each of the following outcome measures: normal blood pressure, prehypertensive status, Stage I and Stage II hypertensives status.
3. RESULTS
Total 1662 participants were screened. Of them, 53 (3.2%) persons did not want to participate in the survey. Thus the results of 1609 persons could be analyzed. Detail demographic data was given in Table 1 and the proportionate national data had been given simultaneously. Our population showed slightly older than the national data. Total family screened was 526 (average adult persons per family was 3.15).
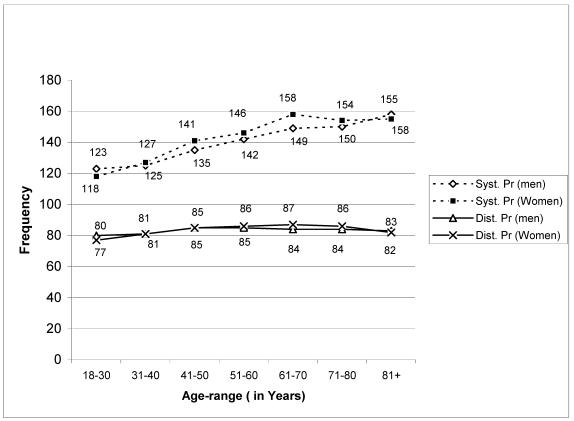
Fig 1 shows the distribution of mean systolic and diastolic pressure in different age groups of the sample population among both men and women.
Fig 1.
Age & sex specific distribution of mean systolic and diastolic pressure among Sample population
Out of 1609 persons, Table 2 shows the distribution of different pressure range among various groups according to JNC-VII criteria. Only 14.1% of the participants had normal blood pressure. A large number of participants could be categorized in prehypertensive group. Overall prevalence of hypertension with a cut off mark of 140/90 mm of Hg is 24.9% (men and women). If cut off mark is 165/95 mm of Hg, the overall prevalence stands at 8.5% (men -7.6% and women-9.6%). Of the hypertensives, only 3 percent individuals were on antihypertensive medications at the time of survey, and half of them had blood pressure within normal range.
Table 2.
Frequency distribution of the different classes of hypertensives as per JNC-VII (Blood Pressure is in mm of Hg)
| Blood Pressure | N | Percentage | JNC-VII | Combined FrequencyIncluding systolic & diastolic pressure | Percentage |
|---|---|---|---|---|---|
| <120 & < 80 | 227 | 14.1 | Normal | 227 | 14.1 |
| 120-139 (Sys) | 576 | 35.8 | Prehypertensive | 944 | 58.7 |
| 80-89 (Diast) | 768 | 47.7 | Prehypertensive | ||
| 140-159 (Sys) | 372 | 23.1 | Stage I | 523 | 32.5 |
| 90-99 (Diast) | 264 | 16.4 | Stage I | ||
| >= 160 ( Sys) | 287 | 17.8 | Stage II | 350 | 21.8 |
| >= 100( Diast) | 208 | 12.9 | Stage II |
*Sys-Systolic pressure, Diast- Diastolic pressure
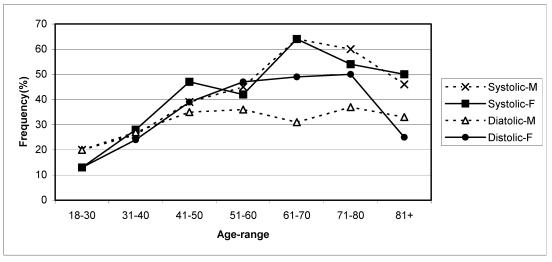
Fig 2 shows the influence of age and sex on distribution of both systolic and diastolic hypertension among the sample population. In participants below 40 years, both systolic and diastolic hypertension showed higher prevalence in men. After 40 years, systolic hypertension showed progressive age-dependent increase up to eighth decade in both sexes and only in women, the prevalence of diastolic hypertension remained higher up to eighth decade. Maximum prevalence of systolic hypertension was 64% among men in eighth decade and women in seventh decade. Maximum prevalence of diastolic hypertension had been recorded up to 50 % among women in seventh decade and 37% among men in eighth decade.
Fig 2.
Age and sex specific distribution of hypertension systolic >= 140 and diastolic blood pressure >= 90 mm Hg
Prevalence of stage I and stage II hypertension was higher among older individuals, sedentary workers, those with high body mass indices, smokers, individuals with history of ischemic heart disease and vegetarians (Table 3).
Table 3.
Bivariate relationships between risk factors and normal, prehypertension, Stage I, and Stage II Hypertension. P-values are based on ordinary chi-square tests of significance.
| Variable | Category | Normal | Prehypertensive | Stage I | Stage II |
|---|---|---|---|---|---|
| Age in years | N (%) | N (%) | N (%) | N (%) | |
| p-value | 0.001** | 0.001** | 0.001** | 0.001** | |
| Less than 20 | 14 (20.3) | 49 (71) | 11 (15.9) | 4 (5.8) | |
| 20-29 | 65 (21) | 201 (65) | 66 (21.4) | 22 (7.1) | |
| 30-39 | 58 (16.9) | 231 (67.2) | 102 (29.7) | 34 (9.9) | |
| 40-49 | 44 (12.5) | 201 (57.3) | 119 (33.9) | 81 (23.1) | |
| 50-59 | 23 (8.8) | 127 (48.7) | 105 (40.2) | 94 (36) | |
| 60-69 | 16 (9.6) | 81 (48.8) | 80 (48.2) | 68 (41) | |
| 70 or above | 7 (6.4) | 54 (49.5) | 40 (36.7) | 47 (43.1) | |
| Gender | [0.13] | [0.92] | [0.07] | [0.33] | |
| p-value | 0.13 | 0.92 | 0.07 | 0.33 | |
| Women | 113 (15.2) | 434 (58.5) | 224 (30.2) | 153 (20.6) | |
| Men | 114 (13.1) | 510 (58.8) | 299 (34.5) | 197 (22.7) | |
| Occupation | p-value | 0.02* | 0.003** | 0.001** | 0.001** |
| Student | 15 (13.6) | 81 (73.6) | 23 (20.9) | 7 (6.4) | |
| Manual labor | 59 (16) | 228 (62) | 108 (29.3) | 72 (19.6) | |
| Housewife | 94 (16.4) | 330 (57.5) | 172 (30) | 118 (20.6) | |
| Sedentary | 38 (9.7) | 216 (55.2) | 160 (40.9) | 108 (27.6) | |
| BMI (Quintile) | p-value | 0.001** | 0.015** | 0.001** | 0.001** |
| Lowest | 68 (23) | 173 (58.4) | 69 (23.3) | 54 (18.2) | |
| Second | 55 (18.2) | 183 (60.6) | 77 (25.5) | 48 (15.9) | |
| Third | 32 (10.5) | 198 (65.1) | 115 (37.8) | 51 (16.8) | |
| Fourth | 33 (11.1) | 175 (59.1) | 104 (35.1) | 68 (23) | |
| Highest | 18 (5.9) | 156 (51.5) | 131 (43.2) | 105 (34.7) | |
| History of IHD | p-value | [0.99] | [0.003**] | [0.49] | [0.02*] |
| Negative | 222 (14.1) | 930 (59.3) | 508 (32.4) | 335 (21.4) | |
| Positive | 5 (12.5) | 14 (35) | 15 (37.5) | 15 (37.5) | |
| Smokers | p-value | [0.14] | [0.02*] | [0.35] | [0.001**] |
| Never Smokers | 224 (14.3) | 924 (59.2) | 504 (32.3) | 328 (21) | |
| Ever Smokers | 3 (6.3) | 20 (41.7) | 19 (39.6) | 22 (45.8) | |
| Diet | p-value | [0.17] | [0.04*] | [0.16] | [0.001**] |
| Vegetarian | 36 (11.5) | 167 (53.5) | 112 (35.9) | 90 (28.8) | |
| Nonvegetarian | 191 (14.7) | 777 (59.9) | 411 (31.7) | 260 (20) | |
| Salt intake | p-value | [0.75] | [0.91] | [0.59] | [0.01*] |
| Negative | 165 (13.9) | 696 (58.8) | 380 (32.1) | 274 (23.1) | |
| Positive | 62 (14.6) | 248 (58.4) | 143 (33.6) | 76 (17.9) |
After adjusting for the effects of all other variables, older age, higher body mass index and vegetarian diet turned out as independent risk factors for stage I or stage II hypertension (Table 4). Compared to those below 20 years of age, people who were 40 years or older had significantly increased risk of stage I and stage II hypertension. For stage II hypertension, association of age with risk of hypertension increased in a dose response manner. Thus, compared to those who were younger than 20 years, people between 40-49 years were nearly 4 times at risk of stage II hypertension, people between 50-59 years were more than 8 times at risk, and people above 60 years were over 14 times at risk of stage II hypertension.
Table 4.
Multivariate relationship between significant independent variables and normal, prehypertension, Stage I, and Stage II hypertension (95% confidence interval in the bracket).
| Variable | Category | Odds' Ratios (95% Confidence Interval) | |||
|---|---|---|---|---|---|
| Normal | Prehypertensive | Stage I | Stage II | ||
| Age in years | Less than 20 | Reference | Reference | Reference | Reference |
| 20-29 | 0.65 (0.30-1.40) | 0.97 (0.5-1.87) | 1.52 (0.67-3.42) | 1.04 (0.29-3.69) | |
| 30-39 | 0.46 (0.20-1.05) | 1.23 (0.61-2.49) | 2.33 (0.97-5.56) | 1.52 (0.39-5.93) | |
| 40-49 | 0.30 (0.13-0.71) | 0.89 (0.43-1.81) | 3.15 (1.32-7.51) | 3.92 (1.03-14.9) | |
| 50-59 | 0.21 (0.08-0.51) | 0.63 (0.3-1.30) | 3.47 (1.44-8.37) | 8.47 (2.23-32.1) | |
| 60-69 | 0.14 (0.05-0.39) | 0.63 (0.3-1.33) | 5.22 (2.12-12.8) | 13.7 (3.54-52.6) | |
| 70 or above | 0.09 (0.02-0.33) | 0.64 (0.29-1.40) | 3.07 (1.19-7.9) | 15.6 (3.94-61.8) | |
| Occupation | Student | Reference | Reference | Reference | Reference |
| Manual labor | 2.91 (1.35-6.24) | 0.66 (0.36-1.19) | 0.73 (0.37-1.44) | 0.86 (0.29-2.54) | |
| Housewife | 2.78 (1.35-5.73) | 0.55 (0.32-0.98) | 0.76 (0.40-1.47) | 0.87 (0.30-2.51) | |
| Sedentary | 2.32 (1.04-5.15) | 0.61 (0.33-1.11) | 1.04 (0.52-2.04) | 0.70 (0.23-2.09) | |
| BMI | Lowest | Reference | Reference | Reference | Reference |
| Second | 0.67 (0.42-1.02) | 1.01 (0.71-1.43) | 1.19 (0.79-1.80) | 1.16 (0.71-1.89) | |
| Third | 0.37 (0.23-0.62) | 1.24 (0.87-1.77) | 1.96 (1.34-2.88) | 1.06 (0.66-1.71) | |
| Fourth | 0.42 (0.26-0.69) | 1.09 (0.76-1.56) | 1.61 (1.08-2.41) | 1.40 (0.87-2.27) | |
| Highest | 0.20 (0.11-0.37) | 0.81 (0.56-1.15) | 2.54 (1.73-3.76) | 2.92 (1.84-4.62) | |
| H/o of IHD | Negative | Reference | Reference | Reference | Reference |
| Positive | 1.13 (0.32-4.02) | 0.87 (0.41-1.87) | 0.73 (0.33-1.66) | 0.92 (0.39-2.18) | |
| Smokers | Never Smokers | Reference | Reference | Reference | Reference |
| Ever Smokers | 0.67 (0.15-2.94) | 0.72 (0.37-1.39) | 1.12 (0.57-2.21) | 1.47 (0.74-2.94) | |
| Diet | Vegetarian | Reference | Reference | Reference | Reference |
| Nonvegetarian | 1.46 (0.93-2.28) | 1.19 (0.90-1.59) | 0.79 (0.68-1.07) | 0.59 (0.42-0.84) | |
| Salt intake | Negative | Reference | Reference | Reference | Reference |
| Positive | 0.98 (0.68-1.42) | 0.94 (0.73-1.22) | 1.15 (0.87-1.50) | 0.78 (0.55-1.09) | |
After adjusting for the effects of all other factors, people with higher body mass indices were at significantly higher risk of stage I and stage II hypertension. Compared to people whose BMI were at the lower quantiles (i.e. people with BMI 18.4 or lower), people whose BMI was in the highest quantile (BMI equal to or more than 25.6) were about 2.5 times at risk of stage I hypertension and nearly 3 times at risk for stage II hypertension. Finally, after adjusting for the effects of all other factors, compared to vegetarians, non-vegetarians in this population (predominantly fish eaters) were about 40 percent lower risk of stage II hypertension (Table 4).
4. DISCUSSION
Hypertension is a major public health problem in India and in other developing countries 1-2. This is obvious from several Indian urban and rural studies 4, 6-16. The various studies estimated a prevalence rate of hypertension among urban population ranging from 1.24% in 1949 to 36.4 % in 2003 and for rural people from 1.99% in 1958 to 21.2% in 1994 1. However differential rates are due to different cut off marks in determining the level of hypertension and also differing age groups constituting the study population. Countries with an ageing population in developed countries will be expected to have a higher prevalence of hypertension than a developing country with a younger population such as India, but there are studies, which have documented a high prevalence rate of hypertension in developing countries 1,2.
Urban studies from India in last decade have shown increasing overall prevalence of hypertension from 6.64% in 1988 to 36.4% in 2003 considering cut off mark 140/90 mm of Hg 6-16. Our study showed an overall prevalence range of 24.9% among men, which is twenty times higher than a documented prevalence rate of 1.24 % among apparently healthy men in the police personnel carried out in 1949 in the same state 6. Unfortunately cut off mark of hypertension was not defined in the above study and the low rate in the previous study may be due to younger population, due to the study being restricted to an age – range between 18 to 50 years. Progressive urbanization, life style modification and sedentary habits are probably some of the important factors considered to be responsible for the higher prevalence of hypertension 17.
An analysis of mean systolic and diastolic pressures among Urban Indian population in the age range between 40-49 years showed an increase of mean systolic pressure 120.4 mm Hg and mean diastolic pressure 73.2mm Hg in 1942 to 128.7 and 84.2 in 1985, 128.8 and 83.2 in 1995 to 141 and 85 in the present study 4. Higher prevalence of hypertension is often indicated by a rise in mean systolic and diastolic pressure. Similar observation has been noted in Yugoslavia and in Japan when it was a developing nation and decrease in prevalence has also been noted in seven countries' study along with decrease in mean systolic and diastolic pressures 18.
Age related increase of hypertension is a common, but not a universal phenomenon. This is predominantly influenced by environmental factors as certain non migrant or tribal populations, who follow a primitive life style do not develop age related rise of prevalence of hypertension 19-21.
High prevalence of systolic hypertension at advanced age had been documented in few recently conducted surveys from India such as from Parsi community in Western India (73% in age group equivalent to 70 years) 13, among Kerallite (51.8%) from South India 12, Assamese (63.63% for people above 60 years of age) from North eastern India 22 and among elderly participants from WHO sponsored multicenter study in Southeast Asia (65%) 3 as compared to an age specific prevalence rate of 64% in seventh to eighth decade in the present study (Fig.2). Thus all the studies have recorded a high prevalence of hypertension. Systolic hypertension has been considered to be one of the most important cause of morbidity and mortality leading to cerebrovascular stroke, cardiovascular and renal diseases 23-24.
Influence of gender in hypertension prevalence has been observed among men who showed higher prevalence of both systolic and diastolic hypertension in young age, but higher prevalence of diastolic hypertension in women after 40 years may be related to increasing family stress and obesity which is common in middle aged woman 25.
The present study had shown a large proportion of sample population in the prehypertensive group. Table 2 has shown an inverse relation between prevalence of prehypertension and age and the particularly victims were students and laborers. These participants are of great interest since chance of progression to hypertension is high. Incidentally the previous study has shown increasing prevalence of coronary artery disease among young in India 26. The younger people in India are stressed out because of heavy competition in academic fields and also for securing employment. Studies have already established that the relationship between BP and risk of cardiovascular disease events is continuous, consistent and independent of other risk factors 5 and prehypertensives have greater chance to go into hypertension 27. Hence it is also possible that the young stressed individuals with prehypertensives level of blood pressures may be at risk factor to develop ischemic heart disease. However no study from India based on JNC- VII criteria is available for comparison. Future longitudinal study involving regular check up of blood pressure of students from secondary level as well as of laborers should be carried out to study the causal relationship between age-specific prehypertensive level of blood pressure and subsequent development of hypertension and coronary artery disease.
Though bivariate analysis showed significant correlation between hypertension with higher age, sedentary activity, smoking, body mass index which was an indicator of obesity and history of target organ dysfunction, multivariate analysis using the logistic regression only documented older age, non vegetarian diet and increasing BMI had significant influence on prevalence of hypertension. The relation of hypertension with advancing of age and BMI has already been documented in the past among Indian subjects 4.
The point of interest is protective effect of non-vegetarian diet. The study participants by custom are predominantly fish eater and they also consume mustard oil, which is a principal cooking medium. Mustard oil is edible oil and it has a right blend of n-3/n-6 polyunsaturated fatty acids, which help in reducing LDL, and it has very low amount of saturated fatty acids. Extraction of different fatty acids from mustard oil has shown the presence of erucic acid which is a monounsaturated fatty acid (cis-13-Docosenoic acid) and found in the range of 42-55% in Indian Mustard. Fish oil is the main source of omega-3 fatty acids (EPA- eicosapentaenoic acid and DHA -docosahexaenoic acid) and also omega-6 fatty acids- two main classes of essential fatty acids. Omega –3 fatty acid found in fish oil lowers blood triglyceride level and blood pressure possibly through generation of nitric oxide which has vasodilator property. EPA is more effective in reducing triglyceride level and DHA is more effective for reducing blood pressure. Thus in combination, they might have protective effect on the non-vegetarians as compared to the vegetarians 28-30. Beneficial effect of mustard oil has been observed among Indians in reducing ischemic heart disease in a recent study 31.
However, several potential limitations should be considered while interpreting the results of this study. First, the dietary data were obtained from a structured questionnaire and therefore response bias could not be ruled out. Data on cooking medium was not sought at the initial survey. However, subsequent surveys and common social norms indicate that the preferred cooking medium for about 98% of the population was mustard oil. Second, when considering systolic hypertension, diastolic pressure may vary widely from normal to abnormal range and vice-versa. And that we have not analyzed the correlation of socio-economic status with stage of hypertension to avoid bias, as participants did not want to reveal their actual income status.
In conclusion, we have shown that there is increasing trend of mean systolic and diastolic pressures and higher prevalence of hypertension in the urban community. We have also documented a large number of prehypertensive individuals according to the JNC-VII criteria, who are young and need special attention to avoid early progression to hypertension and possibly coronary artery disease that is common in India. Age and sex specific increase of prevalence of systolic and diastolic hypertension in both women and men indicate significant role of environmental factors. This suggests public health remedial measures to address growing hypertension in the community through health education about lifestyle changes, dietary modification, and avoidance of urban stress through, for example, practice of yoga. Our findings also suggest a protective role of non -vegetarian diet such as fish cooked in mustard oil on hypertensives. Individually, both fish and the mustard oil are rich in unsaturated fatty acids, and biologically, their beneficial effects are related not only to reduction of blood pressure, but also to lowering of lipids and to their antithrombotic effects 28. Useful role of fish cooked in mustard oil, as a protective factor needs to be probed further in future longitudinal studies.
Acknowledgments
We gratefully acknowledge the active help rendered by Apurba Chakraborty, Sumit Sarkar, Sujit Sarkar, Tridib Sanyal, Alok Bhaduri, Malda English Bazar Municipality and the team of the councilors, Mr. Udayan Saraswati for computer assistance and the people of Malda town for their co-operation. Our heartfelt thanks to Sonoscan- Malda for logistic support, and to Dr. M K Roy and Dr. A Misra for reviewing the manuscript and useful suggestion.
Biographies
Shyamal Kumar Das is the professor of neuromedicine at Bangur Institute of Neurology at the Institute of Postgraduate Medical Education and Research, Kolkata, India. He is also the chief of movement disorders clinic at the Bangur Institute of Neurology at Kolkata, India. Prof Das obtained his MD and superspecialty training in Neurology from the Postgraduate Institute of Medical Education and Research, Chandigarh, India between 1982-1985. He did a fellowship in movement disorders at the University of Calgary, Canada, between 1996-1997. He has numerous publications in leading international journals on Internal Medicine and Neuromedicine. His primary research interests include neuroepidemiology and movement disorders.
Kalyan Sanyal is currently working as a senior consultant physician in the Maldah District, West Bengal, India. Dr. Sanyal completed his medical graduation in 1975, and his specialty training in Internal Medicine in 1985. He has well over 16 years of experience as a consultant physician. His primary research interest is in neuroepidemiology.
Arindam Basu is the Assistant Director of the UC Berkeley (University of California at Berkeley, California) based Fogarty International Training Program in Occupational and Environmental Health in India. He is both an otolaryngologist and an epidemiologist. Dr. Basu graduated in the year 1990 from Medical College, Calcutta, India and had further graduate training in otolaryngology and public health between 1993-1999. He had clinical and postgraduate training in medicine and public health from Calcutta University, ESU, Pennsylvania, St. Louis University, Missouri, USA, and Washington University School of Medicine, St. Louis. He returned to India in 2000, and continued to work as a consultant otolaryngologist and epidemiologist. In 2002, he joined the UC Berkeley based Fogarty International Training Program in Environmental and Occupational health at the Institute of Postgraduate Medical Education and Research as assistant director. His research interests include clinical outcomes research in otolaryngology, clinical epidemiology, and environmental and occupational health.
References
- 1.Nissien A, Bothig S, Grenroth H, Lopez AD. Hypertension in developing countries. World Health Stat Q. 1988;41:141–154. [PubMed] [Google Scholar]
- 2.Reddy KS. Hypertension control in developing countries: generic issues. J Hum Hypertension. 1996;10:S33–38. [PubMed] [Google Scholar]
- 3.Hypertension study group. Prevalence, awareness, treatment and control of hypertension among the elderly in Bangladesh and India: a multicentre study. Bull World Health Organ. 2001;79:490–500. [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta R. Meta analysis of prevalence of hypertension in India. Indian Heart Journal. 1997;49:43–48. [PubMed] [Google Scholar]
- 5.Chobanion AV, Bakris GL, Black HR. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure- The JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 6.Dutta BB. Studies on blood pressure, height, weight, chest and abdominal measurements of 2500 members of the Calcutta Police with short notes on their medical impediments. Indian Med Gazette. 1949;84:238–243. [PMC free article] [PubMed] [Google Scholar]
- 7.Washir HS, Ramchandran P, Nath LM. Prevalence of hypertension in a closed urban community. Indian Heart Journal. 1984;36:250–253. [PubMed] [Google Scholar]
- 8.Hussain SA, Nayak KC, Gupta A. A study of prevalence of hypertension with reference to economic, educational, environmental and hereditary factors in general population of North-West Rajasthan. Indian Heart Journal. 1988;40:148–151. [PubMed] [Google Scholar]
- 9.Gupta R, Gupta S, Gupta VP, Prakash H. The prevalence and determinants of hypertension in the Urban population OF Jaipur in Western India. J Hypertension. 1995;13:1193–1200. doi: 10.1097/00004872-199510000-00014. [DOI] [PubMed] [Google Scholar]
- 10.Anand MR. Epidemiology of hypertension. In: Anand MP, editor. Hypertension: an international monograph 2001. New Delhi: IJCP; 2001. pp. 10–25. [Google Scholar]
- 11.Kalavathy MC, Thankppan KR, Sarma PS, Vasan RS. Prevalence, awareness, treatment and control of hypertension in an eldely community-based sample in Kerala India. National Medical Journal of India. 2000;13:9–15. [PubMed] [Google Scholar]
- 12.Shanthirani CS, Pradeepa R, Deepa R, Premalatha G, Saroja R, Mohan V. Prevalence and risk factors of hypertension in a selected South Indian Population- the Chennai Urban Population study. Journal of Associated Physician of India. 2003;51:20–27. [PubMed] [Google Scholar]
- 13.Bharucha NE, Kuruvilla T. Hypertension in the Parsi community of Bombay: a study on prevalence, awareness and compliance to treatment. BMC Public Health. 2003;3:1. doi: 10.1186/1471-2458-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gupta R, Sharma AK. Prevalence of hypertension and subtypes in an Indian rural population: clinical and electrocardiographic correlates. J Hum Hypertens. 1994;11:823–829. [PubMed] [Google Scholar]
- 15.Chopra RN, Chopra GS. A study of normal blood pressure in Indians. Indian Medical Gazette. 1942;77:21–22. [PMC free article] [PubMed] [Google Scholar]
- 16.Sharma BK, Arora OP, Bhargha V, Sanghvi S, Purohit S. Prevalence of hypertension among the industrial workers and professional classes in Ludhiana, Punjab. Indian Heart Journal. 1985;37:380–385. [PubMed] [Google Scholar]
- 17.Mohan R. Urbanization in India: patterns and emerging policy issues. In: Gughler J, editor. The Urban transformation of the developing world. New York: Oxford University Press; 1996. pp. 93–131. [Google Scholar]
- 18.Toshima H, Koga Y, Blackburn H, Keya A. Lessons for science from the seven countries study. Tokyo: Springer-Verlag; 1994. [Google Scholar]
- 19.Whelton PK. Epidemiology of hypertension. Lancet. 1994;344:101–106. doi: 10.1016/s0140-6736(94)91285-8. [DOI] [PubMed] [Google Scholar]
- 20.Roberts J, Maurer K. Blood pressure levels of persons 6-74 years, United States, 1971-74. Vital and health statistics series 11, no-203. DHEW Publ No (HRA) 78-1648. Washington DC: US Government printing office; 1977. [PubMed] [Google Scholar]
- 21.Dash SC, Swain PK, Sunderam KR, Malhotra KK. Hypertension epidemiology in an Indian Tribal population. Journal of Associated Physician Of India. 1986;34:567–570. [PubMed] [Google Scholar]
- 22.Hazarika NC, Biswas D, Mahanta J. Hypertension in the elderly population of Assam. Journal of Associated Physician Of India. 2003;51:567–573. [PubMed] [Google Scholar]
- 23.National high blood pressure education program working group. National high blood pressure education program working group report in the elderly. Hypertension. 1994;23:275–85. [PubMed] [Google Scholar]
- 24.SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. JAMA. 1991;265:3255–3264. [PubMed] [Google Scholar]
- 25.Isles CS. Prevalence, epidemiology and pathology of hypertension. In: Warrell DA, editor. Oxford Textbook of Medicine, 4th ed. Oxford: Oxford University Press; 2000. pp. 1153–1160. [Google Scholar]
- 26.Gupta R, Gupta V. Meta analysis of coronary heart disease prevalence in India. Indian Heart Journal. 1996;48:241–245. [PubMed] [Google Scholar]
- 27.Vasan RS, Larson MC. et al. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham heart study. JAMA. 2002;287:1003–1010. [Google Scholar]
- 28.Lungershausen YK, Abbey M, Nestel PJ. et al. Reduction of blood pressure and plasma triglycerides by omega-3 fatty acids in treated hypertensives. J Hypertens. 1994;12:1041–1045. [PubMed] [Google Scholar]
- 29.Radack K, Deck C, Huster G. The effects of low doses of n-3 fatty acid supplementation on blood pressure in hypertensive subjects: a randomized controlled trial. Arch Intern Med. 1991;151:1173–1180. [PubMed] [Google Scholar]
- 30.Appel LJ, Miller ER III, Seidler AJ. et al. Does supplementation of diet with 'fish oil' reduce blood pressure? A meta-analysis of controlled clinical trials. Arch Intern Med. 1993;153:1429–1438. [PubMed] [Google Scholar]
- 31.Rastogi T, Srinath Reddy K, Vaz M. et al. Diets rich in vegetables and use of mustard oil could contribute to the lower risk of IHD among Indians. American Journal of Clinical Nutrition. 2004;79:582–592. doi: 10.1093/ajcn/79.4.582. [DOI] [PubMed] [Google Scholar]