Abstract
Background
Whether there is a relationship between blood group and the likelihood of acquiring oral diseases. Therefore, the present study investigated the potential association between ABO blood groups and various dental conditions, including dental caries, gingivitis, malocclusion, and impacted teeth, in Saudi adults aged 18 years and older.
Methods
A cross-sectional study was conducted on 300 participants who met the inclusion criteria. Data collection included assessment of dental caries status using the decayed missing filled teeth (DMFT) and decayed missing filled surfaces (DMFS) indices, evaluation of gingivitis using the Gingival Index, classification of malocclusion according to Angle’s classification system, and recording the presence or absence of impacted teeth.
Results
The AB blood group had the significantly highest mean DMFS score (8.58±6.63), while the O blood group had the lowest mean DMFS score (6.37±4.43). Additionally, blood group O showed a slightly higher prevalence of gingivitis (51.92%) than the other blood groups. Blood group A demonstrated a higher prevalence of both Class II (34.2%) and Class III (19%) malocclusions, with statistically significant differences. Regarding impacted teeth, blood group AB (48.8%) had the highest occurrence.
Conclusion
There exists an association between oral disease and ABO blood group in Saudi adults. The results of this study indicate that individuals with specific blood types may be more prone to oral diseases, which can aid in the early diagnosis and prevention of these conditions.
Keywords: ABO blood groups, dental caries, gingivitis, malocclusion, impacted teeth
Introduction
Dental caries, commonly known as tooth decay, is primarily caused by acid produced by bacteria that dissolve the hard tissues of teeth, such as enamel, dentin, and cementum. However, the etiology of dental caries is multifactorial, involving the interplay between bacterial biofilms (dental plaque), environmental factors (eg, diet, saliva composition and flow rate, fluoride exposure), and the tooth structure itself. This interaction results in a dynamic balance between protective factors that promote tooth remineralization and destructive factors that facilitate tooth demineralization.1,2 Karl Landsteiner’s discovery of the ABO blood group system in the early 20th century significantly advanced medical science by categorizing individuals based on their blood types.3 Since then, studies have explored the potential connections between ABO blood groups and various diseases, including dental conditions. Initial studies examining the relationship between ABO blood groups and dental diseases date back to the 1930s.4,5
Kaslick et al‘s research on aggressive periodontitis highlighted differences in the prevalence among individuals with blood groups O and B, suggesting a possible link between blood groups and periodontal health.6 The four primary blood types, O, A, B, and AB, are determined by the specific antigens present on the surface of red blood cells. These antigens circulate in the bodily secretions of most individuals and are classified as secretors. Conversely, non-secretors lack these antigens in their secretions.7 This distinction is significant because non-secretors generally exhibit lower levels of immunoglobulin A (IgA) antibodies in their saliva, potentially compromising their ability to control bacterial populations within the oral cavity.8 Consequently, the secretion of blood group antigens into the saliva may inhibit bacterial adhesion to tooth surfaces, as many oral bacteria possess lectins that specifically bind to ABO antigens.9
Research on the correlation between blood groups and dental caries has yielded conflicting results. Some studies have suggested that secretors have a lower prevalence of dental caries than non-secretors, possibly because of the inhibitory effects of salivary antigens on bacterial attachment.10–13 However, other studies, such as those conducted by Chung et al in 1965 and Mazumdar et al in 2014, found no significant relationship between salivary secretor status or blood groups and the prevalence.14,15 These discrepancies may be attributed to variations in the geographical and demographic characteristics of the study populations. Gingivitis, characterized by inflammation of the gums, is primarily caused by plaque accumulation and subsequent bacterial infection.16 Some studies have hypothesized that blood group antigens may influence immune responses in gums, potentially affecting their severity or susceptibility to gingivitis.17
However, the exact mechanisms underlying this relationship remain unclear. The relationship between blood group and malocclusion, a condition in which teeth are misaligned, has also garnered research interest. Some studies have identified correlations between specific blood groups and a higher prevalence of certain types of malocclusions. For instance, deep bite malocclusion has been linked to blood type O, whereas class III malocclusion has been associated with blood type A.18 These findings suggest that genetic and biological factors related to the blood type may play a role in the development of malocclusion, although further research is required to confirm these associations. Tooth impaction, in which a tooth fails to emerge properly, is another area in which the blood group may exert influence. Few studies have suggested a possible weak association between certain blood groups and increased risk of tooth impaction. For example, individuals with type A blood may be more prone to impacted canines.19
Several studies have shown a possible association with blood groups and diseases such as diabetes mellitus, ischemic health disease, periodontitis, salivary gland tumors, oral cancer.20–24 On evaluating the literature, studies have shown inconclusive findings with blood groups and oral diseases. On the other hand very few studies have been conducted to understand the relationship between blood group and malocclusion.25–28 Hence this study was planned to close the knowledge gap regarding the relationship between blood types and oral diseases, and we anticipate that our results will be useful for further investigation. The present study was conducted to investigate the relationship between ABO blood groups and various dental conditions, such as dental caries, gingivitis, malocclusion, and impacted teeth, among Saudi adults attending the College of Dentistry at Prince Sattam Bin Abdulaziz University. To evaluate the correlation between the ABO blood group and prevalence of dental caries. To examine the association between ABO blood groups and gingivitis incidence. We analyzed the relationship between ABO blood group and the prevalence of malocclusion. To determine the correlation between ABO blood group and the occurrence of impacted teeth. To compare the associations of ABO blood groups with dental caries, gingivitis, malocclusion, and impacted teeth in Saudi adults aged ≥ 18 years. By focusing on this specific population, we hope to contribute to a more nuanced understanding of the interplay between blood-group antigens and dental health.
Materials and Methods
Study Design
A descriptive, cross-sectional study was conducted among Saudi adults aged 18 years and above from January 2024 to May 2024. The Standing Committee of Bioethics Research (SCBR) at Prince Sattam bin Abdulaziz University has approved the study protocol (SCBR-248/2024). This study was conducted in accordance with the principles of the Declaration of Helsinki.
Sample Size Estimation
The sample size was determined using the formula n = z²pq/d², considering p as 25% and allowable error 5%. The calculation yielded a sample size of 288, which was rounded off to 300.
Sampling Technique
Purposive sampling was used as sampling method. Data were collected when patients came for initial screening and participants were provided with comprehensive information about the study’s objectives and procedures. Informed consent was obtained from all participants, and certified records such as driving licenses and sehaty applications provided by the government based on the records that provided data of blood groups of the participating subjects were used to record the blood groups.
Eligibility Criteria
Participants included in the study were required to meet the following criteria: age > 18 years, possession of a minimum of 20 teeth, and eligibility of both males and females of Saudi origin for participation. The following criteria were used to exclude individuals from the study: refusal to provide consent, uncooperative behavior, pregnancy status, and lack of valid documents for blood group data or reports and expatriates.
Data Collection
Participants were coded to maintain anonymity until statistical analysis was completed. A specially prepared and pretested format, exclusively designed for recording all required and relevant general information and clinical findings, was used to record the data. Training and Calibration were performed by assigning a few participants to whom the investigators applied the self-designed format and recorded their findings. Some subjects were randomly called on different days, and the investigator repeated the examination.
Clinical Examination
Dental caries was assessed using the WHO modified criteria (1986) on the DMF-Index (Decayed, Missing, Filled Teeth) and the DMFS (Decayed, Missing, Filled Surfaces) index by Henry T. Klien, Carrole E. Palmar, and Knutson J.W. (1938). The presence or absence of gingivitis was determined using the Gingival Index (GI) by Loe and Silness (1963). This index was modified and checked for presence or absence of inflammation i.e Absence of inflammation/ normal gingiva was recorded as gingivitis absent. Mild, Moderate, and severe inflammation were defined as the presence of inflammation. Malocclusion was categorized according to Angle’s classification system. The molar relations of Angle’s Class I, Class II, and Class III were checked. If 3rd Molar was unerupted, OPG (Orthopantomography) was used to check for the presence or absence of impacted third molars and was recorded. Each tooth and gingiva was dried under an adequate light-mouth mirror, and an explorer and probe were used. The probe was pressed onto the gingiva to determine the firmness. To evaluate bleeding, the probe was used to run along the soft tissue wall near the entrance of the gingival sulcus.
Statistical Analysis
The results were interpreted at a 95% confidence interval, with statistical significance set at a p-value of less than 0.05. Continuous data were presented as means and standard deviations, whereas discrete data were presented as counts and percentages. One-way Analysis of Variance (ANOVA) was used to assess the impact of blood groups on DMFT and DMFS scores, and comparative analyses between groups were conducted using chi-square analysis and Spearman correlation for qualitative data. The findings were summarized and presented using tables and figures to facilitate comprehension and interpretation.
Results
Sociodemographic Details of the Study Participants
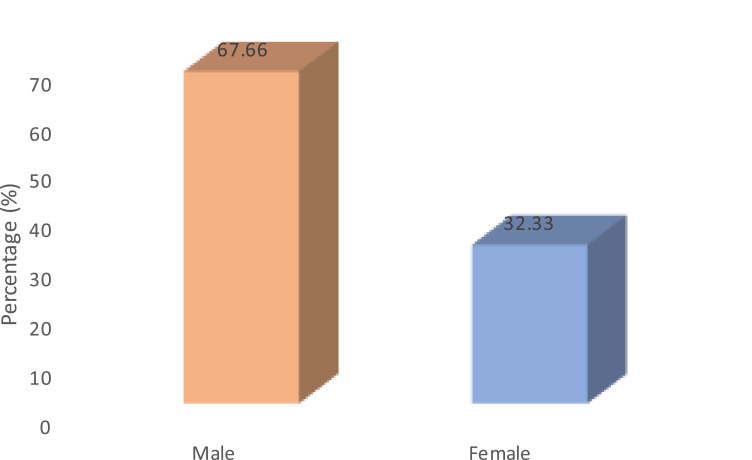
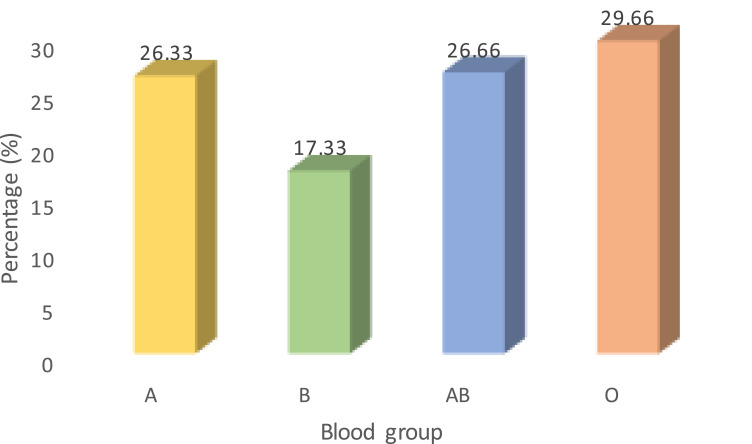
In this study a total of 300 participants were involved. Of the participants, males comprised of 187 (67.66%) remaining 113 (32.33%) were females (Figure 1). There was no significant difference in the mean age between male (25.02 ± 1.94) and female (25.07 ± 2.03), (p>0.05). Blood group O (29.66%) had the highest frequency and A (17.33%) blood group had the lowest frequency among all the participants (Figure 2).
Figure 1.
Distribution of study participants according to gender.
Figure 2.
Distribution of study participants based on type of blood group.
Clinical Characteristics
The mean DMFT score was slightly high in individuals with AB blood group (4.48 ± 2.67) and low in O blood group (4.03 ± 2.43). But the difference was not found to statistically significant (p>0.05) (Table 1). Individuals with AB blood group had highest mean DMFS score (8.58 ± 6.63) compared to other blood groups. Participants with O blood group had a lowest mean DMFS score (6.37 ± 4.43). Mean DMFS scores and blood group showed statistically significant difference (p<0.05) (Table 2).
Table 1.
Comparison of Mean DMFT According to Different Blood Groups of Study Participants
| Blood Group type | DMFT | ANOVA | p value and significance | |
|---|---|---|---|---|
| Mean | SD | |||
| A | 4.37 | 2.56 | 0.547 | 0.650 |
| B | 4.13 | 2.48 | ||
| AB | 4.48 | 2.67 | ||
| O | 4.03 | 2.43 | ||
Abbreviations: DMFT, decayed missing filled teeth index; SD, Standard deviation; ANOVA, Analysis of variance; ABO, ABO blood grouping system.
Table 2.
Comparison of Mean DMFS According to Different Blood Groups of Study Participants
| Blood Group type | DMFS | F | p value | |
|---|---|---|---|---|
| Mean | SD | |||
| A | 8.24b | 5.87 | 2.760 | 0.042 |
| B | 7.07c | 5.15 | ||
| AB | 8.58d | 6.63 | ||
| O | 6.37bcd | 4.43 | ||
Note: bcdp<0.05 Tukey’s HSD post hoc test.
The percentage of gingivitis score was significantly high in individuals with B blood group (51.92%) compared to O (31.46%), A (29.11%) and AB (28.75%) blood groups (p<0.05). The prevalence of impacted tooth is found to be more in individuals with AB blood group and least is observed in B blood group individuals (p<0.05). Majority of the participants in all the blood groups had Angle’s Class I malocclusion. Class II (34.2%) and class III (19.0%) malocclusion was observed to be more with A blood group. Blood group and malocclusion showed statistically significant association with p<0.05 (Table 3). Spearman correlation coefficient test showed a negative and weak correlation between blood groups and dental diseases. The relationship was not found to be statistically significant (Table 4).
Table 3.
Comparison of Percentage of Gingivitis, Presence of Impacted Tooth and Type of Malocclusion According to the Blood Group
| Blood Group | Gingivitis | Impacted Molar | Malocclusion | ||||
|---|---|---|---|---|---|---|---|
| Present N(%) | Absent N(%) | Present N(%) | Absent N(%) | Class I N(%) | Class II N(%) | Class III N(%) | |
| A | 23 (22.8) | 56 (28.1) | 26 (25) | 53 (27) | 37 (20.4) | 27 (37.5)* | 15 (32)* |
| B | 27 (26.7) | 25 (12.6) | 14 (13.5) | 38 (19.4) | 34 (18.8) | 09 (12.5) | 09 (19) |
| AB | 23 (22.8) | 57 (28.6) | 39 (37.5)* | 41 (21) | 58 (32)* | 11 (15.3) | 11 (23.4) |
| O | 28 (27.7)* | 61 (30.7) | 25 (24) | 64 (32.6) | 52 (28.8) | 25 (34.7) | 12 (25.6) |
| X2 value | 9.554 | 10.190 | 14.228 | ||||
| p value | 0.023 | 0.017 | 0.027 | ||||
Notes: X2value = chi square value, p value is by Pearson chi-square for categorical variables.
Table 4.
Correlation of Blood Group and Dental Diseases
| DMFT | DMFS | Gingivitis | Impaction | Malocclusion | ||
|---|---|---|---|---|---|---|
| Blood groups | r | −0.036 | −0.072 | 0.026 | −0.006 | −0.096 |
| p value | 0.532 | 0.215 | 0.657 | 0.922 | 0.098 | |
| N | 300 | 300 | 300 | 300 | 300 | |
Notes: Correlation Strength: r≥0.70 = Strong; r=0.69 −0.30 = Moderate; r=0.29–0.01 = Weak.
Discussion
The ABO blood group system, discovered by Karl Landsteiner in 1902, is one of the most fundamental classifications of human biology.29,30 Landsteiner’s groundbreaking work established that individuals possess different antigens on the surface of their blood cells, leading to the classification of blood cells into four main types: A, B, AB, and O.7 This system has played a crucial role in blood transfusions, ensuring compatibility between donors and recipients and reducing the risk of adverse reactions.31 Beyond its application in transfusion medicine, researchers have increasingly explored the potential associations between ABO blood groups and various health conditions including cardiovascular diseases, cancer susceptibility, and gastrointestinal disorders.32,33
Although the association between ABO blood groups and systemic diseases has been extensively studied, relatively little attention has been paid to their potential roles in maxillofacial pathologies. The maxillofacial region encompasses the structures of the face, jaw, and oral cavity, making it a critical area for both functional and aesthetic considerations. Maxillofacial pathologies encompass a wide range of conditions, including malocclusion, gingivitis, dental impaction, and caries, which can significantly affect an individual’s quality of life.34,35 Understanding the relationship between ABO blood groups and these pathologies could provide valuable insights into their etiology and pathogenesis, potentially leading to improved diagnostic and therapeutic approaches.36,37
Malocclusion refers to any deviation from ideal alignment of the upper and lower teeth when the jaws is closed.35 It can result from a combination of genetic, environmental, and behavioral factors, including genetic predisposition, childhood habits, and jaw abnormalities.36 In this study, we observed significant differences in the prevalence of malocclusion among individuals with different ABO blood groups. Specifically, Class II and Class III malocclusions were more prevalent in participants with blood group A, followed by Class II in the O blood group and Class III malocclusion in the B blood group. Malocclusion was slightly predominant in patients in group A. These findings are consistent with those of previous studies, suggesting an association between certain blood groups and specific types of malocclusions.25–28,38,39 However, contrasting results have been reported in literature, highlighting the complexity of this relationship and the need for further investigation.40
Gingivitis is characterized by inflammation of the gums and is often caused by poor oral hygiene, leading to accumulation of plaques and bacterial toxins along the gumline.41 Although gingivitis is reversible with proper dental care, untreated cases can progress to periodontitis, a more severe form of gum disease that can result in tooth loss and other complications.42 In our study, we found a significant association between certain ABO blood groups and the prevalence of gingivitis. Specifically, individuals in blood group B had the highest prevalence of gingivitis, followed by those in blood group O. These findings are consistent with those of previous studies, indicating a potential link between specific blood groups and susceptibility to gingival inflammation.43,44 However, conflicting results have also been reported, suggesting that additional factors such as geographic and racial differences may influence this relationship.21,45
Dental impaction occurs when one or more teeth fail to erupt properly in their normal positions within the dental arch.46 Third molars, also known as wisdom teeth, are the most commonly impacted teeth, followed by mandibular second premolars and mandibular second molars.47 In the present study, we considered only the third molars as third molar impaction. Although the etiology of dental impaction is multifactorial, including genetic predisposition, overcrowding, and abnormal tooth development, the potential role of ABO blood groups in this condition remains unclear.48 In our study, we found significant differences in the prevalence of dental impaction among individuals with different ABO blood groups. These findings are in contrast to those of previous research indicating a lack of association between blood groups and dental impaction.49,50 However, further studies with larger sample sizes are needed to confirm these results and explore the potential underlying mechanisms.
Dental caries, commonly known as tooth decay, is a multifactorial disease that results from the interaction between bacteria, host factors, and dietary carbohydrates.51 It is characterized by the demineralization of tooth enamel, leading to the formation of cavities and potential complications such as tooth loss and infection.52 In our study, we observed variations in the dental caries indices among individuals with different ABO blood groups. Specifically, participants with blood group AB exhibited higher Decayed, Missing, and Filled Teeth (DMFT) scores than those with other blood groups. Additionally, participants with blood groups AB and A showed higher DMFS (Decayed, Missing, and Filled Surfaces) scores than those with other blood groups. These findings are consistent with previous research suggesting a potential association between certain blood groups and an increased susceptibility to dental caries.2,53,54 However, further studies are needed to elucidate the underlying mechanisms and confirm these observations.
However, the study has limitations. The sample size in this study is small and limited to one geographic area. The participants were recruited using purposive sampling technique. Therefore, findings should be interpreted with caution. In the present study socio-demographic details, oral hygiene practices, dental visit, dietary pattern were not taken into consideration. These factors can directly or indirectly influence the occurrence of oral disease. To know the causal relationship between blood group and oral diseases one must conduct longitudinal studies.
Conclusion
The findings of this study indicate that oral diseases are associated with ABO blood groups. Individuals with AB group have higher prevalence of DMFS and more prone for impaction of molars. Whereas individuals with A blood group have higher chance of developing class II and class III malocclusion. Therefore, individuals with high risk for developing oral diseases should be screened frequently and are recommended to take preventive measures that will reduce oral diseases and improve oral health related quality of life. Further genetic studies are needed to determine the susceptibility to oral diseases with certain blood type. Additionally large community-based studies are suggested by considering behavior, life style, diet and socio-demographic factors to elicit the causal relationship between ABO blood group and oral diseases.
Funding Statement
The authors extend their appreciation to Prince Sattam bin Abdulaziz University for funding this research through project number (PSAU/2024/01/88903).
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki. The Standing Committee of Bioethics Research at Prince Sattam bin Abdulaziz University approved the study protocol (SCBR-248/2024).
Data Sharing Statement
Data is contained within this article.
Informed Consent Statement
Informed consent was obtained from all the participants involved in the study. The participants were briefed about the nature of the study and potential risks, benefits, and rights, and written consent was obtained prior to their participation. The confidentiality and anonymity of human subjects were rigorously maintained throughout the study. Information was anonymized to protect the privacy of the participants.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas, took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Fejerskov O, Kidd EAM. Dental Caries: The Disease and Its Clinical Management. 2nd ed. Oxford: Blackwell Munksgaard; 2008. [Google Scholar]
- 2.Selwitz RH, Ismail AI, Pitts NB. Dental caries. Lancet. 2007;369(9555):51–59. doi: 10.1016/S0140-6736(07)60031-2 [DOI] [PubMed] [Google Scholar]
- 3.Landsteiner K. Zur Kenntnis der antifermentativen, lytischen und agglutinierenden Wirkungen des Blutserums und der Lymphe. Zentralblatt für Bakteriologie. 1900;27:357–362. German. [Google Scholar]
- 4.Clarke JK, Hirschfeld I. Investigation of the correlation between blood groups and susceptibility to dental caries. J Am Dent Assoc. 1938;25:1932–1942. [Google Scholar]
- 5.Fischer D, Robinson HBG. A further study of the relation of blood group to caries incidence. J Dent Res. 1948;27(5):541–548. doi: 10.1177/00220345480270041501 [DOI] [PubMed] [Google Scholar]
- 6.Kaslick RS, Chasens AI, Tuckman MA, Kaufman B. Association between ABO blood groups, HLA-A antigens and periodontal diseases in young adults: a follow-up study. J Periodontol. 1971;42(6):420–427. doi: 10.1902/jop.1971.42.7.420 [DOI] [PubMed] [Google Scholar]
- 7.Daniels G. Human Blood Groups. 3rd ed. Oxford: Wiley-Blackwell; 2013. [Google Scholar]
- 8.Aird I, Bentall HH, Roberts JA. A relationship between cancer of stomach and the ABO blood groups. Br Med J. 1953;1(4814):799–801. doi: 10.1136/bmj.1.4814.799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cooling L. Blood groups in infection and host susceptibility. Clin Microbiol Rev. 2015;28(3):801–870. doi: 10.1128/CMR.00109-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhattacharya A, Pandey A, Pal S, Sarkar S, Sayal K. ABO blood grouping and its relation with dental caries in school going children of Kanpur city. J Indian Dent Assoc. 2013;7(2):59–62. [Google Scholar]
- 11.Svensater G, Welin J, Wilkins JC, Beighton D, Hamilton IR. Protein expression by planktonic and biofilm cells of Streptococcus mutans. FEMS Microbiol Lett. 2001;205(1):139–146. [DOI] [PubMed] [Google Scholar]
- 12.Chauhan SP, Mani AM, Shaik MV, Husain A. Association of dental caries with ABO blood grouping among patients visiting a dental college. J Clin Diagn Res. 2017;11(1):ZC27–ZC30. [Google Scholar]
- 13.Saravia ME, Nelson-Filho P, Silva RA, De Rossi A, Faria G. ABO blood group typing and dental caries in Brazilian patients. J Dent Child. 2008;75(2):124–128. [Google Scholar]
- 14.Chung CS, Speed WE, Zappa JL, Palat M, Muller HE. Correlation between caries susceptibility and blood group secretor status. J Dent Res. 1965;44(2):471–474. doi: 10.1177/00220345650440030501 [DOI] [PubMed] [Google Scholar]
- 15.Mazumdar P, Das UK, Das D, Goswami S. Relationship between dental caries and blood group: an observational study. J Dent Med Sci. 2014;13(1):31–33. [Google Scholar]
- 16.Preshaw PM, Seymour RA, Heasman PA. Current concepts in periodontal pathogenesis. Dent Update. 2004;31(10):570–578. doi: 10.12968/denu.2004.31.10.570 [DOI] [PubMed] [Google Scholar]
- 17.Shetty S, Munshi AK. Association of blood group and Rh factor with periodontitis and oral hygiene status in children. Indian Soc Pedod Prev Dent. 2000;18(3):140–145. [Google Scholar]
- 18.Bailit HL, Doykos JD, Swanson LT. Dental caries, size of the dentition, and age at menarche in females. Hum Biol. 1968;40(2):245–261. [Google Scholar]
- 19.Hunter ML, Priest SJ. Malocclusion: an overview of classification, etiology and clinical implications. Pediatr Dent. 2004;26(6):502–506. [Google Scholar]
- 20.Sharjeel S, Wasi M, Jafri A, et al. The correlation between blood group type and diabetes mellitus type II: a case-control observational study from Pakistan. Cureus. 2021;13(11):e19898. doi: 10.7759/cureus.19898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Demir T, Tezel A, Orbak R, Eltas A, Kara C, Kavrut F. The effect of ABO blood types on periodontal status. Eur J Dent. 2007;1(03):139–143. doi: 10.1055/s-0039-1698329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pinkston JA, Cole P. ABO blood groups and salivary gland tumours (Alabama, United States). Cancer Causes Control. 1996;7(6):572–574. doi: 10.1007/BF00051698 [DOI] [PubMed] [Google Scholar]
- 23.Raaghavan VM, Bailoor DN, Jhansirani P. Incidence of ABO blood groups in oral cancer in south Kanara district. J Indian Dent Assoc. 1986;58:305–308. [Google Scholar]
- 24.Whincup PH, Cook DG, Phillips AN, Shaper AG. ABO blood group and ischaemic heart disease in British men. BMJ. 1990;300(6741):1679–1682. doi: 10.1136/bmj.300.6741.1679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sharma R, Preethi PN, Nagarathna C, Navin HK. Association of ABO blood groups with malocclusion in population of Jaipur, India: a prospective study. Int J Sci Stud. 2015;2(11):45–51. [Google Scholar]
- 26.Al-Khatieeb MM, Al-Joubori SK, Taha SS. Association of ABO blood group and rhesus factor with dental malocclusion in a population of Baghdad, Iraq. Int J Med Res Health Sci. 2018;7(1):165–169. [Google Scholar]
- 27.Prasad Gupta S. Association of ABO blood groups with occlusal pattern among orthodontic patients of Kathmandu District. EC Dental Sci. 2018;17(12):2119–2129. [Google Scholar]
- 28.Shokor FF, Ab Rahaman WS, Alam MK. Craniofacial morphology with genetic influence of ABO blood group in Malaysian orthodontic patients. Int J Pharm Bio Sci. 2015;6(4):412–418.51. [Google Scholar]
- 29.Landsteiner K. Zur Kenntnis der antifermentativen, lytischen und agglutinierenden Wirkungen des Blutserums und der Lymphe. Wiener klinische Wochenschrift. 1902;25(6):1132–1134. German. [Google Scholar]
- 30.Yamamoto F, Clausen H, White T, Marken J, Hakomori S. Molecular genetic basis of the histo-blood group ABO system. Nature. 1990;345(6272):229–233. doi: 10.1038/345229a0 [DOI] [PubMed] [Google Scholar]
- 31.Roback JD, Combs MR, Grossman BJ, Hillyer CD. Technical manual. Am Assoc Blood Banks. 2008. [Google Scholar]
- 32.Franchini M, Liumbruno GM, Lippi G. The prognostic value of ABO blood group in patients with von Willebrand disease. Thromb Haemost. 2016;115(5):929–931. [Google Scholar]
- 33.O’Donnell J, Laffan MA. The relationship between ABO histo-blood group, factor VIII and von Willebrand factor. Transfus Med. 2001;11(4):343–351. doi: 10.1046/j.1365-3148.2001.00315.x [DOI] [PubMed] [Google Scholar]
- 34.Fonseca RJ. Oral and Maxillofacial Surgery: Elsevier Health Sciences; 2017. [Google Scholar]
- 35.Proffit WR, Fields HW, Sarver DM. Contemporary Orthodontics: Elsevier Health Sciences; 2018. [Google Scholar]
- 36.Verma P, Kumar A, Dixit S, Mohan K, Gupta N, Mandal G. Assessment of relationship of ABO blood groups in oral cancer patients - a retrospective study. Ann Maxillofac Surg. 2021;11(1):80–85. doi: 10.4103/ams.ams_265_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mahalakshmi IP, Sinha P, Nagaraj T, Okade D, Nonitha S, Veerabasaivaiah BT. Relationship between ABO blood group and Rh factor with oral potentially malignant disorder. J Oral Maxillofac Pathol. 2022;26(1):57–59. doi: 10.4103/jomfp.jomfp_75_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mossey PA. The heritability of malocclusion: part 1 - Genetics, principles and terminology. Br J Orthod. 1999;26(2):103–113. doi: 10.1093/ortho/26.2.103 [DOI] [PubMed] [Google Scholar]
- 39.Hassan AH, Amin HE. Association of orthodontic treatment needs and oral health-related quality of life in young adults. Am J Orthod Dentofacial Orthop. 2010;137(1):42–47. doi: 10.1016/j.ajodo.2008.02.024 [DOI] [PubMed] [Google Scholar]
- 40.Rai B, Kaur J. Association between ABO blood groups and malocclusion. J Orthod Sci. 2011;1(4):114–118. [Google Scholar]
- 41.Kolodziej R, Plichta M, Pawlowska E, Czajka-Jakubowska A. Evaluation of the relationship between ABO blood types and dental caries in a Polish population. Pol J Environ Stud. 2015;24(5):2071–2075. [Google Scholar]
- 42.Newman MG, Takei H, Klokkevold PR, Carranza FA. Carranza’s Clinical Periodontology: Elsevier Health Sciences; 2018. [Google Scholar]
- 43.Kinane D, Stathopoulou PG, Papapanou PN. Periodontal diseases. Nat Rev Dis Primers. 2017;3(1):17038. doi: 10.1038/nrdp.2017.38 [DOI] [PubMed] [Google Scholar]
- 44.Khartade BV, Aher V, Patil A, Dharmadhikari C. Association between ABO blood group and periodontal disease: a preliminary study. J Indian Soc Periodontol. 2011;15(1):56–59. [Google Scholar]
- 45.Al-Ahmad HT, Hamamy HA. The ABO blood group and periodontal status. J Periodontol. 2006;77(3):400–404. [Google Scholar]
- 46.Idowu BI, Mafeni JO, Otoh EC. Periodontal health status and blood group: an investigative study. Indian J Dent Res. 2011;22(5):701–705. [Google Scholar]
- 47.Peterson LJ. Contemporary Oral and Maxillofacial Surgery. Elsevier Health Sciences. 2014. [Google Scholar]
- 48.Chu FC, Li TK, Lui VK, Newsome PR, Chow RL, Cheung LK. Prevalence of impacted teeth and associated pathologies - a radiographic study of the Hong Kong Chinese population. Hong Kong Med J. 2003;9(3):158–163. [PubMed] [Google Scholar]
- 49.Ahmed I, Gul-e-Erum HM. Prevalence of impacted molars and associated pathologies – a radiographic study. Pak Oral Dent J. 2009;29(2):187–190. [Google Scholar]
- 50.Chavan RS, Sharma S. Prevalence of impacted teeth and its correlation with blood groups. Int J Dent Clin. 2018;10(2):47–51. [Google Scholar]
- 51.Maheshwari S, Maheshwari PK, Verma R, Sharma D. Correlation between impacted third molar and ABO blood groups: a cross-sectional study. J Clin Diagn Res. 2016;10(2):ZC52–ZC54. [Google Scholar]
- 52.Featherstone JD. The science and practice of caries prevention. J Am Dent Assoc. 2000;131(7):887–899. doi: 10.14219/jada.archive.2000.0307 [DOI] [PubMed] [Google Scholar]
- 53.Hegde MN, Hegde ND, Bhat GS. Evaluation of association between dental caries and blood groups in South Kanara population. J Indian Soc Pedod Prev Dent. 2008;26(4):153–155. doi: 10.4103/0970-4388.44030 [DOI] [PubMed] [Google Scholar]
- 54.Ben salameh Z, Kassab S, Al-Natsheh M, Taha H. Association of ABO blood groups with caries incidence in Palestinian young adults. Int J Dent Hyg. 2013;11(2):112–116. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is contained within this article.