Abstract
Purpose of Review
The objective of this scoping review is to use a health equity lens to understand the extent and type of evidence that exists about the use of electronic nicotine delivery systems (ENDS) based on socioecological understandings of health influences (i.e., the US National Institute of Minority Health and Health Disparities’ (NIMHD) Research Framework). The research question guiding the review was as follows: What is the range and scope of research that exists to help characterize health disparities related to ENDS use?
Recent Findings
Ninety-eight articles published between 2019 and 2022 often examined racial/ethnic differences in ENDS use; however, other demographic characteristics, domains of influence across the life course, and levels of influence beyond individuals were rarely considered. As most studies were derived from large-scale, cross-sectional US national surveys, few longitudinal studies or intervention trials were published.
Summary
The use of the NIMHD framework to analyze recent literature helped identify research patterns and gaps that may be important to recognize for optimizing population health strategies to advance health equity. Future research on non-individual level factors influencing ENDS, interventions to effectively use ENDS for combustible cigarette cessation, and subpopulations susceptible to dual use may enhance existing science. Monitoring research using the NIMHD research framework can help researchers and policy makers to identify and when appropriate, prioritize support for overlooked but important research questions.
Keywords: Electronic nicotine delivery systems, E-cigarettes, Health equity, Health disparities, Social determinants of health
Introduction
Electronic nicotine delivery systems (ENDS) were introduced to the US market in 2007, and the use of ENDS has increased dramatically over the past decade such that over 9 million adults in the USA currently use ENDS each month [1]. Though early ENDS research described the use and experimentation among youth and young adults who predominately identified as non-Hispanic white (NHW), more recent evidence suggests that patterns of use are emerging among people who identify with minoritized groups defined by race, ethnicity, gender, sexual orientation, housing stability, and some health conditions [2–8]. This review used a health equity lens to better understand current science and research opportunities focused on ENDS use among adults, ages 30 years and older, as ENDS may reduce harm attributed to combustible tobacco use in this population.
Understanding the types and extent of ENDS-related disparities is imperative for preventing exploitative or disproportionate harm. For the purposes of this paper, health disparities are defined by differences that adversely affect disadvantaged populations. One way to study disparities in tobacco use is to examine whether rates of use differ among different groups. Differences in prevalence rates could be a signal that there are factors (e.g., targeted marketing) that may lead to disparities in health outcomes [9]. Identifying disparities can demonstrate specific needs for policy change or intervention and promote more equitable access to tobacco-related information, resources, and opportunities for harm reduction. Developing an understanding of how ENDS use or nicotine vaping may vary based on experiences across diverse populations with a specific focus on historically marginalized sub-populations will ensure more equitable distribution of scientific knowledge and research benefits to populations that have traditionally experienced disproportionate health burdens related to tobacco use. While long term health effects of ENDS use remain uncertain, ENDS have been proposed as a feasible method of quitting or reducing combustible cigarette smoking for some people. Since ENDS use may also lead to dual use of ENDS and combustible cigarettes for others, more research is needed to understand the potential health risks and harm reduction benefits of ENDS among adults [10–16]. Understanding the different circumstances and impacts of ENDS use in diverse populations is important to promote public health and inform prevention efforts to reduce tobacco-related health harm.
In 2019, the US National Institute on Minority Health and Health Disparities (NIMHD) released a research framework for understanding health disparities and advancing health equity (Fig. 1) [17]. The framework consolidates various socioecological understandings of health and illness into a model for examining health conditions in context and to inform interventions or disparities amelioration [17–19]. It acknowledges the complex and multifactorial pathways to disease/illness and outlines different domains of influence (biological, behavioral, physical/built environment, sociocultural environment, and healthcare system) over the life course as well as distinct levels of influence (individual, interpersonal, community, and societal). Our research team used this framework to organize a scoping review of ENDS research conducted among adults aged 30 years and older between 2019 and 2022. The objective of this review was to use the NIMHD research framework to understand the extent and types of evidence describing ENDS use. The research question guiding the review was as follows: What is the range and scope of research that exists to help characterize health disparities related to ENDS use? The review also sought to identify gaps for future research on ENDS use and its impact on diverse subgroups. Consistent with the framework, the terms used throughout the review (e.g., health disparity, social determinants of health, ENDS/e-cigarettes, and health equity) are defined in Table 1.
Fig. 1.
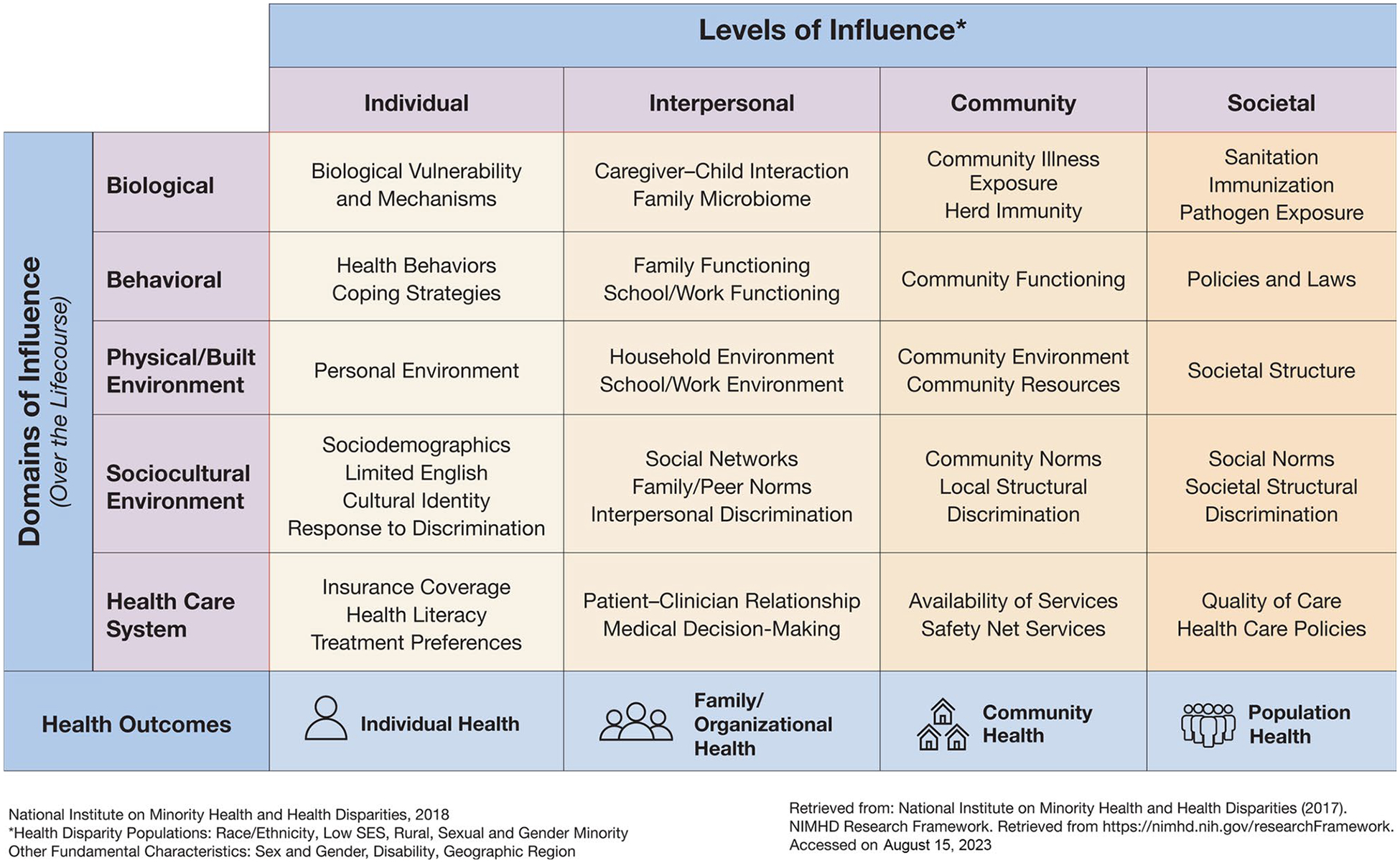
National Institute on Minority Health and Health Disparities Research Framework
Table 1.
Definitions of key terms used in the National Institute of Minority Health and Health Disparities (NIMHD) Research Framework
| Term | Definition |
|---|---|
| Health disparity | A particular type of health difference that is closely linked with economic, social, or environmental disadvantage. Health disparities adversely affect groups of people who have systematically experienced greater social or economic obstacles to health based on their racial or ethnic group, religion, socioeconomic status, gender, age, or mental health; cognitive, sensory, or physical disability; sexual orientation or gender identity; geographic location; or other characteristics historically linked to discrimination or exclusion |
| Social determinants of health | Conditions in the environments in which people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks |
| ENDS/e-cigarettes | Vapes, vaporizers, vape pens, hookah pens, electronic cigarettes (e-cigarettes or e-cigs), e-cigars, and e-pipes are some of the many tobacco product terms used to describe electronic nicotine delivery systems (ENDS) |
| Health equity | The absence of disparities or avoidable differences among socioeconomic and demographic groups or geographical areas in health status and health outcomes such as disease, disability, or mortality |
Sources: U.S. Centers for Disease Control and Prevention, CDC’s Office of Health Equity, U.S. Food and Drug Administration, World Health Organization
Methods
Search Strategy
To identify relevant studies, a medical librarian (MF) conducted an initial search on MEDLINE to identify index terms. Medical subject heading (MeSH) analysis was then performed on key articles provided by the research team for each database, with search terms iteratively translated and refined. The final set of terms were then used to formally search MEDLINE, Embase, PsycInfo, and Web of Science.
To maximize sensitivity, the formal search used controlled vocabulary terms and synonymous free-text words to capture the concepts of the NIMHD framework and ENDS (See all search terms in the Supplementary Materials). The search strategy was reviewed by an independent librarian, using the Peer Review of Electronic Search Strategies (PRESS) standard to make sure the search strategy in this scoping review is comprehensive and unbiased. Search terms included diverse population subgroups at-risk for harm by tobacco and nicotine products such as people who identify with groups defined by race and ethnicity, gender identity, sexual orientation, rurality, diagnosed health conditions, or socioeconomic status.
Inclusion and Exclusion Criteria
We included peer-reviewed articles published in English among US adult populations from 2007 (the year e-cigarettes entered the US market) to 2022. However, upon uncovering past scoping reviews and to focus on use behaviors synchronic with more recent changes in the ENDS marketplace, we revised the years covered in this scoping review to include literature published between January 2019 and April 2022. We included studies focused on adults 30 years and older. When age groups were not explicitly defined, we only included studies where 50% or more of participants were 30 years or older. We also included studies with a mean age higher than 30 years if our target age group was intermixed with younger adults or youth. Studies conducted outside of the USA, qualitative studies, case reports, commentaries/editorials, articles about models or methods, meta-analyses, and systematic reviews were excluded. We excluded articles outside of the USA because the NIMHD framework was originally developed for the US context and may require adaptation for use in other countries or sociopolitical contexts.
Study Selection
The search results were pooled in EndNote and de-duplicated [http://www.endnote.com]. Then, this set was uploaded to Covidence [http://www.covidence.org] for screening. Two independent reviewers screened the titles and abstracts to exclude any papers that met our exclusion criteria. Potentially relevant sources were retrieved in full, and two reviewers read the text to determine their eligibility for this review. Reasons for exclusion were recorded. At each stage, disagreements between reviewers were resolved through discussion or review by a third reviewer [20].
Results
Overall, 98 articles met criteria (see the annotated reference list for review articles). Analyses of the 98 articles are presented, organized by the populations studied and the elements of the NIMHD research framework that were examined. While terms describing demographic and socioeconomic groups evolve, we have used language found within the source articles. Groups classified by race and/or ethnicity garnered the most attention for analysis and reporting (39.8%), followed by people from lower socioeconomic positions (23.5%), people with physical illnesses/health conditions (17.3%), people with lower educational attainment (12.2%), people with substance use disorder (10.2%), people with mental health conditions (9.2%), sexual and gender minority populations (6.1%), and women of reproductive age (3.1%) (Table 2). Other populations studied included people in urban areas (5.1%), people in rural areas (3.1%), and active or veteran members of the military (3.1%). Other groups examined in studies included people who reported adverse childhood experiences, immigrants, and people sleeping less than recommended.
Table 2.
Characterization of articles included in the scoping review of ENDS use guided by the NIMHD research framework
| Characteristic or factor | N = 98 | Percent |
|---|---|---|
| Study type | ||
| Observational | 93 | 94.9% |
| Randomized control trial | 5 | 5.1% |
| Populations examined in studies | ||
| People from racially and ethnically diverse groups | 39 | 39.8% |
| People from lower socioeconomic positions | 23 | 23.5% |
| People with physical illnesses | 17 | 17.3% |
| People with lower educational attainment | 12 | 12.2% |
| People with substance use disorder(s) | 10 | 10.2% |
| People with mental health conditions | 9 | 9.2% |
| Sexual/gender minoritized populations | 6 | 6.1% |
| Urban populations | 5 | 5.1% |
| Focus on women of reproductive age | 3 | 3.1% |
| Rural populations | 3 | 3.1% |
| US military or veterans | 3 | 3.1% |
| Geographic distribution of studies in the US | ||
| National | 68 | 69.4% |
| Local or state | 30 | 30.6% |
| HHS Region 1 (CT, ME, MA, NH, RI, VT) | 2 | 2.0% |
| HHS Region 2 (NJ, NY, Puerto Rico, the Virgin Islands) | 1 | 0.1% |
| HHS Region 3 (DE, DC, MD, PA, VA, WV) | 0 | 0.0% |
| HHS Region 4 (AL, FL, GA, KY, MS, NC, SC, TN) | 2 | 2.0% |
| HHS Region 5 (IL, IN, MI, MN, OH, WI) | 5 | 5.1% |
| HHS Region 6 (AR, LA, NM, OK, TX) | 5 | 5.1% |
| HHS Region 7 (IO, KS, MO, NE) | 0 | 0.0% |
| HHS Region 8 (CO, MT, ND, SD, UT, WY) | 0 | 0.0% |
| HHS Region 9 (AZ, CA, HA, NV, American Samoa, Northern Mariana Islands, Micronesia, Guam, Marshall Islands, Palau) | 4 | 4.1% |
| HHS Region 10 (AK, ID, OR, WA) | 2 | 2.0% |
| More than one HHS region | 9 | 9.2% |
| NIMHD framework domain of influence examined | ||
| Biological | 9 | 9.2% |
| Behavioral | 84 | 85.7% |
| Physical/built environment | 12 | 12.2% |
| Sociocultural environment | 72 | 73.5% |
| Health systems | 18 | 18.4% |
| Health equity level of influence examined | ||
| Individual | 95 | 96.9% |
| Interpersonal | 12 | 12.2% |
| Community | 20 | 20.4% |
| Societal | 20 | 20.4% |
The U.S. Department of Health and Human Services (HHS) has defined regions to facilitate and maintain partnerships with state, local, and tribal leaders
People from Racially and Ethnically Diverse Groups
The included studies primarily used race and ethnicity variables for stratified analysis or statistical controls. Studies that examined racial and ethnic differences in ENDS use or risk perceptions frequently compared non-Hispanic white (NHW) populations to non-Hispanic black (NHB) and/or Hispanic/Latinx (Hispanic) populations [21, 21, 22, 22, 23, 23–29]. Moreover, although 40–50% of all combustible cigarette smokers reported using ENDS for smoking cessation, one study found that NHB people who smoke were less likely than NHW and Hispanic people to use ENDS for smoking cessation [21, 30–34, 34, 34, 35, 35, 36, 36, 36,35].
People from Low Socioeconomic Positions or with Low Educational Attainment
Recent studies have documented an increase in ENDS use among populations with lower socioeconomic status such as people experiencing food insecurity [37•], those who had their last routine medical checkup more than 5 years prior to the survey [30•] and those who have completed lower levels of education [38•]. While many studies found that low income people were less likely than those with more income to use ENDS for smoking cessation, one study observed that people of low socioeconomic status were more likely to choose harm reduction behaviors (i.e., switching from combustible cigarettes to ENDS) over harm elimination behaviors (i.e., quitting tobacco use) when compared to people with more household income [39•]. Another study found that among dual users of ENDS and cigarettes, people with lower income were more likely to become exclusive users of combustible cigarettes [22••]. Lower levels of income, education, and employment were associated with lower levels of ENDS use for sustained combustible cigarette cessation [25, 40–42,30].
Sexual/Gender Minority (SGM) Populations
Higher rates of ENDS use among people who identified as lesbian, gay, bisexual, transgender, or queer were observed. Pregnant women who identified as lesbian were more likely to report dual use or ENDS use during their third trimester of pregnancy when compared to heterosexual women who were also pregnant [8, 26, 27, 33, 43–45,45].
People with Physical Illnesses and Health Conditions
People affected by cancers, cardiovascular diseases, oral/dental conditions, human immunodeficiency virus (HIV), independent living disabilities, and asthma were included in ENDS studies that described people with physical illnesses or health conditions [46, 47, 47–56]. Survivors of tobacco-related cancers had a higher prevalence of current ENDS and combustible cigarette use compared to survivors of non-tobacco-related cancers [51•]. People diagnosed with respiratory disease, heart failure, stroke, tobacco-related cancers, oral HPV-16 infection, chronic lung disease, and cancer survivors had a higher likelihood of using ENDS compared to people without such diagnoses [14, 51, 52, 54, 57–59,60].
Some studies of vaping found that people using both devices with nicotine only and those with non-tobacco substances such as nicotine-free solutions or marijuana had increased odds of illness. For example, the odds of lung disease among people who reported never using tobacco were higher among daily ENDS users than among people who never used ENDS [61•]. The odds of having asthma, but not chronic obstructive pulmonary disease, were higher among women of childbearing age who currently used ENDS and did not have a history of combustible cigarette use, compared to non-tobacco users [48•]. Finally, significant associations were found between dual use (i.e., ENDS and combustible tobacco use) and asthma, some cancers, gastrointestinal upset, history of stroke, heart failure, lung disease, respiratory conditions, and sleep problems [14, 26, 57, 58, 61–66].
Geography
Most studies relied on US national data, followed by data collected at the state or local level (Table 2). Nine studies crossed state lines and included more than one US Department of Health and Human Services region [12, 25, 32, 67–74,75].
Dual Use, Smoking Cessation, and Other Substance Use Health Disparity Populations
Dual use of ENDS and combustible cigarette smoking are the most frequently examined behavior in included studies of ENDS use among adults. The studies in this review found that people with physical and mental health comorbidities were more likely to engage in dual use (i.e., use ENDS and combustible cigarettes) [14, 22, 28, 36, 36, 43, 43, 46, 47, 76–84]. In the context of potential menthol bans at the state and national levels, one study found that people who smoke menthol cigarettes may most benefit from the use of ENDS for cessation purposes [85•].
The use of other substances was frequently studied in relation to ENDS use [25, 25, 72, 86, 86, 87, 87–90,91].
Patients with mental health conditions or symptoms such as anxiety, depression, serious psychological distress, and other mental health conditions were more likely to try ENDS, be current ENDS users, and be at risk for future ENDS use. [76, 92–96,90].
NIMHD Framework: Domains of Influence
Most studies considered behavioral (85.7%) or sociocultural environmental (73.5%) domains of influence on ENDS use. Biological (9.2%), built/physical environment (12.2%), and health system (18.4%) influences were less likely to be examined as factors influencing ENDS use or perceptions in existing research. The NIMHD framework defines behavioral influences as areas of influence over the life course that include health behaviors, coping strategies, functioning in roles (family) and locations (school/work/community), and policies and laws intending to guide behaviors and actions [17]. Most studies were cross-sectional and examined the use of ENDS as a predictor or outcome using comparison groups of non-users or users of combustible cigarettes [17, 22, 25, 30, 31, 35, 37, 42, 46, 56, 69, 71, 74, 89, 90, 96–102,103].
NIMHD Framework: Levels of Influence
The studies overwhelmingly focused on individual-level factors (96.9%) influencing ENDS use. Fewer studies examined the influence of interpersonal (12.2%), community (20.4%), or societal (20.4%) level factors on e-cigarette use. Interpersonal levels of influence examined in selected studies included household, peer, familial, and relationship factors such as trusted sources of information [45, 75, 87, 104–107]. Community levels of influence explored were community norms and neighborhood factors [24, 26, 45, 73, 74, 74, 88, 90, 104, 104, 108, 108, 109,110].
Discussion
This scoping review examined ENDS use across various subgroups and circumstances to understand patterns and gaps in recent research. Published research tends to describe ENDS use based on US national surveys. Research examining relationships between subpopulations and contextual influences was rarely the primary focus of research; such analyses exist in the form of covariates or stratified analysis, suggesting that different research types may advance or extend current insights. For example, research examining the influence of physical environments on dual use or ENDS use for cessation for certain subgroups or understanding how individuals from subgroups access and engage with health information might help develop novel behavioral interventions. We observed that people categorized by racial and ethnic groups were the most examined in the literature, but there is a need for additional research to understand individual and societal-level factors that lead to ENDS use not only among various health disparity populations but also among people who smoke mentholated tobacco products or people with diagnosed health conditions. More studies are needed to understand differences in tobacco product use among and between diverse populations. We know there is great variation among practices, societal norms, and behaviors when it comes to each unique population group. Factors shaping ENDS use are complex. Beyond racial and ethnic categories, research should also consider populations characterized by rural geography, sexual/gender minority status, immigration experience, or socioeconomic status. This review corroborated findings that people who identify with a SGM group as well as people diagnosed with some illnesses or health conditions also experience disparities in ENDS use [111–114]. Since racial/ethnic differences in ENDS outcomes sometimes demonstrated interactions with more distal health influences such as education or income, studies examining intersectional identity groups (e.g., racial/ethnic subgroups by gender) may be important for monitoring and preventing tobacco-related disparities [9, 21, 22, 24]. Examining prevalence rates among subpopulations is an initial step in identifying health disparities related to tobacco use. The review also identified minimal human research covering the influences of biology, environments, and health systems on ENDS use behaviors among adults.
Other research gaps identified by this review include the circumstances and effectiveness of ENDS for quitting combustible cigarettes or harm reduction, longitudinal studies of ENDS and health outcomes, and understanding ENDS prevention and cessation among adults 30 years and older. While many people may turn to ENDS as a cessation aid or to reduce smoking cigarettes, the literature suggests that there is much to learn about whether or under what conditions ENDS use can be effective as a smoking cessation aid, especially for some of the subgroups identified in this review. The current Cochrane review on ENDS for combustible tobacco cessation found high certainty evidence that those randomized to nicotine e-cigarettes were more likely to abstain from combustible tobacco use after 6 months of follow-up than those randomized to nicotine replacement therapy (approximately 4 more quitters per 100 people); however, much of the ENDS for combustible tobacco cessation literature is characterized by low to moderate certainty, high or uncertain risk of bias, and imprecise estimates [16]. Research beyond ENDS efficacy for cessation could examine whether and how ENDS as a combustible tobacco cessation tool affects population subgroups differently. Future research could also focus on developing, testing, and disseminating interventions to support more equitable opportunities to promote health and well-being. Such interventions may include using ENDS for combustible smoking cessation in subpopulations that may benefit most or preventing ENDS use among subpopulations that would otherwise not use tobacco products to minimize harm.
This review examined articles about adults ages 30 years and older which tended to describe and assess use behaviors and health effects. However, studies focused on youth and younger adults may have examined a broader range of articles such as those focused on ENDS marketing and policy implementation. Though fewer in number than articles examining individual-level factors, the articles focused on community and societal-level influences in this review serve as persuasive, evidentiary companions to studies of marketing [115, 116] and policies [117, 118] that demonstrate the layered milieux of influences that foster or deter ENDS initiation, use, or cessation. Among studies seeking to explore differential use, there was significant variation in the comparison groups selected for comparison to ENDS uses. Some studies compared ENDS users to users of tobacco products; other studies relied on never users. Another limitation of this study is the lack of uniform age groupings in research studies. The excluded studies focused on young adults defined them differently (e.g., 18–25 years, 18–29 years, and 18–34 years). We excluded studies where most of the population was under 30 years, which may limit the representativeness of the findings for studies that include all people ages 30 years and older. Moreover, since the NIMHD framework was originally developed to examine minority health and health disparities within the US context, we only included US studies in this review. The framework may be adapted to apply to international or global research; however, such adaptation was not feasible due to the constraints of this review.
Conclusions
Advancing health equity in the arenas of nicotine and tobacco use requires understanding the current state of affairs, documenting disparities in use rates, and recognizing the research knowledge and gaps that inform policy and public health decision-making. Using the NIMHD research framework to assess domains and levels of influence around a phenomenon of interest is one way to monitor the growth and development of scientific knowledge production that may benefit health for all people. Structured monitoring with such a framework could support generative and corrective actions to promote more equitable conditions for health and health research. Though tremendous progress has been made documenting tobacco-related disparities, deliberate attention is required to understand novel and emerging tobacco and other nicotine products. This review used the NIMHD framework to identify abundant opportunities for future research as well as conceptual domains that might help researchers better document and design studies that examine the complex interactions between domains and levels of influence that shape ENDS-related phenomena.
Supplementary Material
Acknowledgements
The authors thank and acknowledge Syrena Carver, Whitney Allen, Angela DeLucia, Nicholas Franco, Juhan Lee, and Thomas Liss for assistance reviewing abstracts and articles and extracting article data for this review.
Funding
Research reported in this publication was supported by grant numbers U54DA036151 and R01 DA049878 from the National Institute on Drug Abuse (NIDA) and FDA Center for Tobacco Products (CTP). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
Footnotes
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s40429-023-00521-3.
Conflict of Interest The authors declare no competing interests.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Cornelius ME, Loretan CG, Wang TW, Jamal A, Homa DM. Tobacco product use among adults - United States, 2020. MMWR Morb Mortal Wkly Rep. 2022;71:397–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Atuegwu NC, Oncken C, Laubenbacher RC, Perez MF, Mortensen EM. Factors associated with e-cigarette use in US young adult never smokers of conventional cigarettes: a machine learning approach. Int J Environ Res Public Health. 2020;17(19):7271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. E-cigarette use among youth and young adults: a report of the surgeon general [Internet]. 2016;Chapter 5. [PubMed]
- 4.Bentivegna K, Atuegwu NC, Oncken C, DiFranza JR, Mortensen EM. Electronic cigarettes associated with incident and polysubstance use among youth. J Adolesc Health. 2021;68(1):123–9. 10.1016/j.jadohealth.2020.05.026. [DOI] [PubMed] [Google Scholar]
- 5.Unger JB, Soto DW, Leventhal A. E-cigarette use and subsequent cigarette and marijuana use among Hispanic young adults. Drug Alcohol Depend. 2016;163:261–4. 10.1016/j.drugalcdep.2016.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnson SE, O’Brien EK, Coleman B, Tessman GK, Hoffman L, Delahanty J. Sexual and gender minority U.S. youth tobacco use: Population Assessment of Tobacco and Health (PATH) study wave 3, 2015–2016. Am J Prev Med. 2019;57(2):256–61. 10.1016/j.amepre.2019.03.021. [DOI] [PubMed] [Google Scholar]
- 7.Simon P, Buta E, Gueorguieva R, Kong G, Morean ME, Camenga DR, et al. Transitions across tobacco use profiles among adolescents: results from the Population Assessment of Tobacco and Health (PATH) study waves 1 and 2. Addiction. 2020;115(4):740–7. 10.1111/add.14828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee J, Tan AS. Intersectionality of sexual orientation with race and ethnicity and associations with e-cigarette use status among US youth. Am J Prev Med. 2022;63(5):669–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Institute of Minority Health and Health Disparities. Minority health and health disparities: definitions and parameters. https://www.nimhd.nih.gov/about/strategic-plan/nih-strategic-plan-definitions-and-parameters.html (2016). Accessed 7/22/23.
- 10.Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N, et al. A randomized trial of e-cigarettes versus nicotine-replacement therapy. N Engl J Med. 2019;380(7):629–37. [DOI] [PubMed] [Google Scholar]
- 11.Zhu S-H, Zhuang Y-L, Wong S, Cummins SE, Tedeschi GJ. E-cigarette use and associated changes in population smoking cessation: evidence from US current population surveys. bmj. 2017;358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.•.Fetterman JL, Keith RJ, Palmisano JN, McGlasson KL, Weisbrod RM, Majid S, et al. Alterations in vascular function associated with the use of combustible and electronic cigarettes. J Am Heart Assoc. 2020;9(9):e014570. 10.1161/JAHA.119.014570. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 13.•.Jones DM, Ashley DL, Weaver SR, Eriksen MP. Flavored ENDS use among adults who have used cigarettes and ENDS, 2016–2017. Tob Regul Sci. 2019;5(6):518–31. 10.18001/trs.5.6.4. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 14.•.Gathright EC, Wu W-C, Scott-Sheldon LAJ. Electronic cigarette use among heart failure patients: findings from the Population Assessment of Tobacco and Health study (Wave 1: 2013–2014). Heart lung: J Crit Care. 2020;49(3):229–32. 10.1016/j.hrtlng.2019.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 15.Balfour DJK, Benowitz NL, Colby SM, Hatsukami DK, Lando HA, Leischow SJ, Lerman C, Mermelstein RJ, Niaura R, Perkins KA, Pomerleau OF, Rigotti NA, Swan GE, Warner KE, West R. Balancing consideration of the risks and benefits of e-cigarettes. Am J Public Health. 2021;111(9):1661–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hartmann-Boyce J, Lindson N, Butler AR, McRobbie H, Bullen C, Begh R et al. Electronic cigarettes for smoking cessation. Cochrane Database of Systematic Reviews. 2022(11). 10.1002/14651858.CD010216.pub7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alvidrez J, Castille D, Laude-Sharp M, Rosario A, Tabor D. The national institute on minority health and health disparities research framework. Am J Public Health. 2019;109(S1):S16–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Institute of Minority Health and Health Disparities. NIMHD Research Framework. 2017. [Google Scholar]
- 19.Bronfenbrenner U The ecology of human development: experiments by nature and design. Harvard University Press; 1979. [Google Scholar]
- 20.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 21.•.Assari S, Mistry R, Bazargan M. Race, Educational attainment, and e-cigarette use. J Med Res Innov. 2020;4(1). 10.32892/jmri.185. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 22.••.Brouwer AF, Jeon J, Hirschtick JL, Jimenez-Mendoza E, Mistry R, Bondarenko IV, et al. Transitions between cigarette, ENDS and dual use in adults in the PATH study (waves 1–4): multistate transition modelling accounting for complex survey design. Tob Control. 2020. 10.1136/tobaccocontrol-2020-055967. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article that reports results from modeling multiple transitions between states of combustible cigarette, ENDS use, and dual use over four waves of the commonly used PATH survey and surfaces the complexities of cross product transitions over time as well as differences between groups by race and ethnicity.
- 23.•.Boyle RG, Sharma E, Lauten K, D’Silva J, St Claire AW. Examining use and dual use of tobacco products and marijuana among Minnesota adults. Subst Use Misuse. 2021;56(11):1586–92. 10.1080/10826084.2021.1936049. [DOI] [PubMed] [Google Scholar]; Review article
- 24.•.Harlow AF, Stokes A, Brooks DR. Socioeconomic and racial/ethnic differences in e-cigarette uptake among cigarette smokers: longitudinal analysis of the Population Assessment of Tobacco and Health (PATH) study. Nicotine Tob Res. 2019;21(10):1385–93. 10.1093/ntr/nty141. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article that identifies patterns of differential use for using ENDS for combustible cigarette cessation by race, ethnicity, and proxy variables for income.
- 25.•.John WS, Grover K, Greenblatt LH, Schwartz RP, Wu L-T. E-Cigarette use among adult primary care patients: results from a multisite study. J Gen Intern Med. 2020;35(1):268–75. 10.1007/s11606-019-05488-4. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 26.•.Leavens ELS, Ford BR, Ojo-Fati O, Winkelman TNA, Vickery KD, Japuntich SJ, et al. Electronic cigarette use patterns and chronic health conditions among people experiencing homelessness in MN: a statewide survey. BMC Public Health. 2020;20(1):1889. 10.1186/s12889-020-09919-4. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 27.•.O’Cleirigh C, King D, Stanton AM, Goldin A, Kirakosian N, Crane HM, et al. Patterns of e-cigarette use among primary care patients at an urban community center. J Community Health. 2022;47(1):1–8. 10.1007/s10900-021-01015-x. [DOI] [PubMed] [Google Scholar]; (Review article)
- 28.•.Spears CA, Jones DM, Weaver SR, Huang J, Yang B, Pechacek TF, et al. Sociodemographic correlates of electronic nicotine delivery systems (ENDS) use in the United States, 2016–2017. Am J Public Health. 2019;109(9):1224–32. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 29.Webb Hooper M, Kolar SK. Racial/Ethnic Differences in electronic cigarette use and reasons for use among current and former smokers: findings from a community-based sample. Int J Environ Res Public Health. 2016;13(10). 10.3390/ijerph13101009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.•.Chido-Amajuoyi OG, Mantey D, Cunningham S, Yu R, Kelder S, Hawk E, et al. Characteristics of us adults attempting tobacco use cessation using e-cigarettes. Addict Behav. 2020;100:106123. 10.1016/j.addbeh.2019.106123. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article that examines more contextual factors than many articles, this article found different use of ENDs for tobacco cessation based on demographic and social characteristics including race, ethnicity, age, gender, health seeking behaviors, and provider advice.
- 31.•.Cardona S, Calixte R, Rivera A, Islam JY, Vidot DC, Camacho-Rivera M. Perceptions and patterns of cigarette and e-cigarette use among Hispanics: a heterogeneity analysis of the 2017–2019 Health Information National Trends Survey. Int J Environ Res Public Health. 2021;18(12). 10.3390/ijerph18126378. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article that highlights why researchers must examine subgroup differences within larger ethnicity categories such as Hispanic in order to identify differential risks as well as different strategies and opportunities for intervention or harm reduction.
- 32.•.Uddin SMI, Osei AD, Obisesan OH, El-Shahawy O, Dzaye O, Cainzos-Achirica M, et al. Prevalence, trends, and distribution of nicotine and marijuana use in e-cigarettes among US adults: the behavioral risk factor surveillance system 2016–2018. Prev Med. 2020;139:106175. 10.1016/j.ypmed.2020.106175. [DOI] [PMC free article] [PubMed] [Google Scholar]; (Review article)
- 33.•.Mattingly DT, Patel A, Hirschtick JL, Fleischer NL. Sociodemographic differences in patterns of nicotine and cannabis vaping among US adults. Preventive medicine reports. 2022;26:101715. 10.1016/j.pmedr.2022.101715. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 34.•.Mayer M, Reyes-Guzman C, Grana R, Choi K, Freedman ND. Demographic characteristics, cigarette smoking, and e-cigarette use among US adults. JAMA Netw Open. 2020;3(10):e2020694. 10.1001/jamanetworkopen.2020.20694. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 35.•.Rao M, Bar L, Yu Y, Srinivasan M, Mukherjea A, Li J, et al. Disaggregating Asian American cigarette and alternative tobacco product use: results from the National Health Interview Survey (NHIS) 2006–2018. J Racial Ethn Health Disparities. 2021. 10.1007/s40615-021-01024-5. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article that highlights why researchers must examine subgroup differences within larger racial categories such as Asian American to identify differential risks as well as different strategies and opportunities for intervention or harm reduction.
- 36.•.Rhoades DA, Comiford AL, Dvorak JD, Ding K, Driskill LM, Hopkins AM, et al. Dual versus never use of e-cigarettes among American Indians who smoke. Am J Prev Med. 2019;57(3):e59–68. 10.1016/j.amepre.2019.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 37.•.Gu D, Max WB, Yao T, Wang Y, Keeler C, Sung H-Y. Association between e-cigarette use and food insecurity among low-income adults. Tob Control. 2022. 10.1136/tobaccocontrol-2021-057110. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 38.•.Kingsbury JH, D’Silva J, O’Gara E, Parks MJ, Boyle RG. How much progress have we made? Trends in disparities in tobacco use. Prev Chronic Dis. 2020;17:E107. 10.5888/pcd17.200090. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 39.•.Kurti AN, Bunn JY, Tang K, Nighbor T, Gaalema DE, Coleman-Cowger V, et al. Impact of electronic nicotine delivery systems and other respondent characteristics on tobacco use transitions among a U.S. national sample of women of reproductive age. Drug Alcohol Dependence. 2020;207:107801. 10.1016/j.drugalcdep.2019.107801. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 40.•.Leventhal AM, Dai H, Higgins ST. Smoking cessation prevalence and inequalities in the United States: 2014–2019. J Natl Cancer Inst. 2022;114(3):381–90. 10.1093/jnci/djab208. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article. This analysis of a large national survey found socioeconomic differences in smoking cessation attempts, sustained quit attempts and use of cessation treatments that were inconsistent with interest in quitting and motivation to quit, suggesting challenges with access.
- 41.•.Syamlal G, Clark KA, Blackley DJ, King BA. Prevalence of electronic cigarette use among adult workers—United States, 2017–2018. Morb Mortal Wkly Rep. 2021;70(9):297. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article that considers the role of occupation and workplace as factors for e-cigarette use.
- 42.•.Mshigeni SK, Rittenhouse A, Gwanzura T, Arroyo R, Vaughn C. Understanding demographics characteristics of e-cigarette users in California and the need for tailored interventions. Am J Health Educ. 2021;52(4):185–93. 10.1080/19325037.2021.1930610. [DOI] [Google Scholar]; Review article
- 43.•.Beck DC, Veliz PT, McCabe SE, Boyd CJ, Evans-Polce R. Cigarette, e-cigarette, and dual use during the third trimester of pregnancy in a national sample of heterosexual and sexual minority women. Am J Addict. 2021;30(6):593–600. 10.1111/ajad.13217. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 44.•.Al Rifai M, Mirbolouk M, Jia X, Nasir K, Pickett JK, Nambi V, et al. E-cigarette use and risk behaviors among lesbian, gay, bisexual, and transgender adults: the behavioral risk factor surveillance system (BRFSS) survey. Kansas J Med. 2020;13:318. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 45.•.Keller-Hamilton B, Stevens EM, Wedel AV, LaPolt DT, Miranda A, Wagener TL, et al. Associations of race and ethnicity with tobacco messaging exposures and tobacco use among bisexual and pansexual women. Prev Med Rep. 2022;25:101657. 10.1016/j.pmedr.2021.101657. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 46.•.Gimm G, Parekh T, Rossheim ME. Prevalence and risk factors of e-cigarette use among working-age adults with and without disabilities in 2017–2018. Disabil Health J. 2021;14(2):101048. 10.1016/j.dhjo.2020.101048. [DOI] [PubMed] [Google Scholar]; (Review article that raises the importance of examining use patterns among people with disabilities as well as considering different types of disabilities.)
- 47.•.Salloum RG, Huo J, Lee J-H, Lee J, Dallery J, George T, et al. Tobacco and e-cigarette use among cancer survivors in the United States. PLoS ONE. 2019;14(12):e0226110. 10.1371/journal.pone.0226110. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 48.•.Parekh T, Owens C, Fay K, Phillips J, Kitsantas P. Use of e-cigarettes and development of respiratory conditions in women of childbearing age. South Med J. 2020;113(10):488–94. 10.14423/SMJ.0000000000001158. [DOI] [PubMed] [Google Scholar]; Review article
- 49.•.Huilgol P, Bhatt SP, Biligowda N, Wright NC, Wells JM. Association of e-cigarette use with oral health: a population-based cross-sectional questionnaire study. J Public Health. 2019;41(2):354–61. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 50.•.Reynolds LM, Zamora C, Lee UJ, Stokes AC, Benjamin EJ, Bhatnagar A, et al. Tobacco use prevalence and transitions from 2013 to 2018 among adults with a history of cardiovascular disease. J Am Heart Assoc. 2021;10(12):e021118. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 51.•.Bjurlin MA, Basak R, Zambrano I, Schatz D, El Shahawy O, Sherman S et al. Patterns and associations of smoking and electronic cigarette use among survivors of tobacco related and non-tobacco related cancers: a nationally representative cross-sectional analysis. Cancer Epidemiol. 2021:101913. 10.1016/j.canep.2021.101913. [DOI] [PubMed] [Google Scholar]; Review article
- 52.•.Dewar EO, Dee EC, Arega MA, Ahn C, Sanford NN. Trends in frequency of e-cigarette use among cancer patients and survivors in the United States, 2014–2018. Addict Behav. 2021;119:106913. 10.1016/j.addbeh.2021.106913. [DOI] [PubMed] [Google Scholar]; Review article
- 53.•.Fucito LM, Bold KW, Baldassarri SR, LaVigne JP, Ford B, Sather P, et al. Use and perceptions of electronic nicotine delivery systems among patients attending lung cancer screening who smoke. Prev Med Rep. 2021;23:101444. 10.1016/j.pmedr.2021.101444. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 54.•.Herndon P, Jassal JS, Cramer JD. Association between e-cigarette use and oral HPV-16 infection. Oral Oncol. 2022;125:105676. 10.1016/j.oraloncology.2021.105676. [DOI] [PubMed] [Google Scholar]; Review article
- 55.•.Herriges MJ, Pinkhasov R, Shapiro O, Jacob JM, Basnet A, Bratslavsky G et al. E-cigarette use and the risk of bladder and lung cancer. J Clin Oncol. 2022;40(6 SUPPL). 10.1200/JCO.2022.40.6_suppl.443. [DOI] [Google Scholar]; Review article
- 56.•.Philip HE, Hein DM, Sanford NN. Racial disparities in e-cigarette use among conventionally smoking cancer survivors in the United States, 2014–2018. Subst Use Misuse. 2022;57(4):660–3. 10.1080/10826084.2021.2019786. [DOI] [PubMed] [Google Scholar]; Review article
- 57.•.Bricknell RAT, Ducaud C, Figueroa A, Schwarzman LS, Rodriguez P, Castro G, et al. An association between electronic nicotine delivery systems use and a history of stroke using the 2016 behavioral risk factor surveillance system. Medicine. 2021;100(36):e27180. 10.1097/MD.0000000000027180. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 58.•.Xie W, Kathuria H, Galiatsatos P, Blaha MJ, Hamburg NM, Robertson RM, et al. Association of electronic cigarette use with incident respiratory conditions among US adults from 2013 to 2018. JAMA Netw Open. 2020;3(11):e2020816. 10.1001/jamanetworkopen.2020.20816. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 59.•.Golla A, Chen A, Tseng VL, Chan Lee SY, Pan D, Yu F et al. Association between e-cigarette use and visual impairment. InvestigOphthalmol Vis Sci. 2021;62(8). [Google Scholar]; Review article
- 60.•.Vemulapalli A, Mandapati SR, Kotha A, Aryal S. Association between vaping and untreated caries: a cross-sectional study of National Health and Nutrition Examination Survey 2017–2018 data. J Am Dental Assoc (1939). 2021;152(9):720–9. 10.1016/j.adaj.2021.04.014. [DOI] [PubMed] [Google Scholar]; Review article
- 61.•.Barrameda R, Nguyen T, Wong V, Castro G, Rodriguez de la Vega P, Lozano J, et al. Use of e-cigarettes and self-reported lung disease among US adults. Publ Health Rep (Washington, DC: 1974). 2020;135(6):785–95. 10.1177/0033354920951140. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 62.•.Debnath D, Singh P, Vanjarapu JMR, Wert Y, Shrimanker I, Goel S, et al. Gastrointestinal upset: could e-cigarettes be the cause? Am J Gastroenterol. 2019;114(Supplement):S1621. 10.14309/01.ajg.0000601512.93240.1d. [DOI] [Google Scholar]; Review article
- 63.•.So CJ, Meers JM, Alfano CA, Garey L, Zvolensky MJ. Main and interactive effects of nicotine product type on sleep health among dual combustible and e-cigarette users. Am J Addict. 2021;30(2):147–55. 10.1111/ajad.13130. [DOI] [PubMed] [Google Scholar]; Review article
- 64.•.Wiener RC, Waters C, Bhandari R, Trickett Shockey AK, Alshaarawy O. The association of sleep duration and the use of electronic cigarettes, NHANES, 2015–2016. Sleep disorders. 2020;2020:8010923. 10.1155/2020/8010923. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 65.•.Tran L, Tran P, Tran L. A cross-sectional analysis of electronic cigarette use in US adults by asthma status. Clin Respir J. 2020;14(10):991–7. [DOI] [PubMed] [Google Scholar]; Review article
- 66.•.Critcher CR, Siegel M. Re-examining the association between e-cigarette use and myocardial infarction: a cautionary tale. Am J Prev Med. 2021;61(4):474–82. 10.1016/j.amepre.2021.05.003. [DOI] [PubMed] [Google Scholar]; Review article
- 67.Hawkins SS, Wylie BJ, Hacker MR. Use of ENDS and cigarettes during pregnancy. Am J Prev Med. 2020;58(1):122–8. 10.1016/j.amepre.2019.08.031. [DOI] [PubMed] [Google Scholar]
- 68.•.Lin J, Zhu K, Hoang PK, Solivan-Ortiz AM, Larsen SL, Irwin SP, et al. Electronic cigarette use and related factors among active duty service members in the U.S. military. Mil Med. 2020;185(3–4):418–27. 10.1093/milmed/usz267. [DOI] [PubMed] [Google Scholar]; Review article
- 69.•.Nabi-Burza E, Drehmer JE, Walters BH, Willemsen MC, Zeegers MPA, Winickoff JP. Smoking cessation treatment for parents who dual use e-cigarettes and traditional cigarettes. J Smok Cessat. 2021;2021:6639731. 10.1155/2021/6639731. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 70.•.Rubenstein D, Sokolovsky AW, Aston ER, Nollen NL, Schmid CH, Rice M, et al. Predictors of smoking reduction among African American and Latinx smokers in a randomized controlled trial of JUUL e-cigarettes. Addict Behav. 2021;122:107037. 10.1016/j.addbeh.2021.107037. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 71.•.Stellefson M, Wang MQ, Balanay JAG, Wu R. Health risk disparities among employed adults with COPD living in Central Appalachian U.S. States. Am J Health Educ. 2020;51(5):265–77. 10.1080/19325037.2020.1802373. [DOI] [Google Scholar]; Review article
- 72.•.Wang-Schweig M, Jason LA, Stevens E, Chaparro J. Tobacco use among recovery home residents: vapers less confident to quit. Am J Health Behav. 2019;43(6):1064–74. 10.5993/AJHB.43.6.5. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 73.•.Lewis-Thames MW, Langston ME, Fuzzell L, Khan S, Moore JX, Han Y. Rural-urban differences e-cigarette ever use, the perception of harm, and e-cigarette information seeking behaviors among U.S. adults in a nationally representative study. Prev Med. 2020;130:105898. 10.1016/j.ypmed.2019.105898. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 74.•.Mumford EA, Stillman FA, Tanenbaum E, Doogan NJ, Roberts ME, Wewers ME, et al. Regional rural-urban differences in e-cigarette use and reasons for use in the United States. J Rural Health: Off J Am Rural Health Assoc Natl Rural Health Care Assoc. 2019;35(3):395–404. 10.1111/jrh.12333. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 75.•.Kosterman R, Epstein M, Bailey JA, Hawkins JD. Is e-cigarette use associated with better health and functioning among smokers approaching midlife? Drug Alcohol Depend. 2022;234:109395. 10.1016/j.drugalcdep.2022.109395. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 76.•.Nguyen N, Kapiteni K, Straus ER, Guydish J. Factors associated with dual and polytobacco use among people in residential substance use disorder treatment. Am J Addict. 2021;30(5):496–504. 10.1111/ajad.13206. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 77.•.Usidame B, Hirschtick J, Zavala-Arciniega L, Mattingly DT, Patel A, Meza R, et al. Exclusive and dual menthol/non-menthol cigarette use with ENDS among adults, 2013–2019. Prev Med Rep. 2021;24:101566. 10.1016/j.pmedr.2021.101566. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 78.•.Al Rifai M, Mirbolouk M, Jia X, Nasir K, Pickett JK, Nambi V, et al. E-cigarette use and risk behaviors among lesbian, gay, bisexual, and transgender adults: the Behavioral Risk Factor Surveillance System (BRFSS) survey. Kans J Med. 2020;13:318–21. 10.17161/kjm.vol13.13861. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 79.•.Boozary LK, Frank-Pearce SG, Alexander AC, Waring JJ, Ehlke SJ, Businelle MS, et al. Correlates of e-cigarette use among adults initiating smoking cessation treatment. Drug Alcohol Depend. 2021;224:108724. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 80.•.Selya AS, Shiffman S, Greenberg M, Augustson EM. Dual use of cigarettes and JUUL: trajectory and cigarette consumption. Am J Health Behav. 2021;45(3):464–85. [DOI] [PubMed] [Google Scholar]; Review article
- 81.•.Glasser AM, Vojjala M, Cantrell J, Levy DT, Giovenco DP, Abrams D, et al. Patterns of e-cigarette use and subsequent cigarette smoking cessation over 2 years (2013/2014–2015/2016) in the population assessment of tobacco and health study. Nicotine Tob Res. 2021;23(4):669–77. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 82.•.Zavala-Arciniega L, Hirschtick JL, Meza R, Fleischer NL. E-cigarette characteristics and cigarette smoking cessation behaviors among US adult dual users of cigarettes and e-cigarettes. Prev Med Rep. 2022;26:101748. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 83.•.Farsalinos KE, Niaura R. E-cigarettes and smoking cessation in the United States according to frequency of e-cigarette use and quitting duration: analysis of the 2016 and 2017 National Health Interview Surveys. Nicotine Tob Res. 2020;22(5):655–62. [DOI] [PubMed] [Google Scholar]; Review article
- 84.Azagba S, Qeadan F, Shan L, Latham K, Wolfson M. E-cigarette use and transition in adult smoking frequency: a longitudinal study. Am J Prev Med. 2020;59(3):367. [DOI] [PubMed] [Google Scholar]
- 85.•.Cook S, Hirschtick JL, Patel A, Brouwer A, Jeon J, Levy DT, et al. A longitudinal study of menthol cigarette use and smoking cessation among adult smokers in the US: assessing the roles of racial disparities and e-cigarette use. Prev Med. 2022;154:106882. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 86.•.Parker MA, Villanti AC. Patterns and frequency of current e-cigarette use in United States adults. Subst Use Misuse. 2019;54(12):2075–81. 10.1080/10826084.2019.1626433. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 87.•.El Shahawy O, Sherman SE, Palamar JJ. High prevalence of tobacco product and e-cigarette use among electronic dance music party attendees. Subst Use Misuse. 2020;55(10):1561–6. 10.1080/10826084.2020.1717536. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 88.•.Parekh T, Desai R. A comparative analysis of e-cigarette users and state-specific prevalence change in the United States between 2017 and 2018. Cureus. 2020;12(12):e12079. 10.7759/cureus.12079. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 89.•.Roberts W, Verplaetse T, Peltier MKR, Moore KE, Gueorguieva R, McKee SA. Prospective association of e-cigarette and cigarette use with alcohol use in two waves of the Population Assessment of Tobacco and Health. Addiction (Abingdon, England) 2020;115(8):1571–9. 10.1111/add.14980. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 90.•.Dixit D, Herbst E, Das S. E-cigarette use and perceptions among veterans receiving outpatient treatment in veterans affairs substance use and mental health clinics. Mil Med. 2020. 10.1093/milmed/usaa292. [DOI] [PubMed] [Google Scholar]; Review article that provides a good example of considering different comparison groups: ENDS patterns among veterans seeking specific types of care in one state were compared to those of veterans seeking similar care in another state as well as to ENDS patterns within the general population of adults.
- 91.•.Campbell BK, Le T, Gubner NR, Guydish J. Health risk perceptions and reasons for use of tobacco products among clients in addictions treatment. Addict Behav. 2019;91:149–55. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 92.•.Obisesan OH, Mirbolouk M, Osei AD, Orimoloye OA, Uddin SMI, Dzaye O, et al. Association between e-cigarette use and depression in the behavioral risk factor surveillance system, 2016–2017. JAMA Netw Open. 2019;2(12):e1916800. 10.1001/jamanetworkopen.2019.16800. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 93.•.Kaplan B, Thrul J, Cohen JE. Association of cigarette and electronic nicotine delivery systems use with internalizing and externalizing problems among US adults: findings from wave 3 (2015–2016) of the PATH study. PLoS ONE. 2021;16(6):e0253061. 10.1371/journal.pone.0253061. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 94.•.Spears CA, Jones DM, Weaver SR, Yang B, Pechacek TF, Eriksen MP. Electronic nicotine delivery system (ENDS) use in relation to mental health conditions, past-month serious psychological distress and cigarette smoking status, 2017. Addiction (Abingdon, England). 2019;114(2):315–25. 10.1111/add.14464. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 95.•.Budenz A, Klein A, Prutzman Y. The relationship between trauma exposure and adult tobacco use: analysis of the National Epidemiologic Survey on Alcohol and Related Conditions (III). Nicotine Tob Res. 2021;23(10):1716–26. 10.1093/ntr/ntab057. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 96.•.Blondino CT, Clifford JS, Lu J, Prom-Wormley EC. The association between internalizing and externalizing severity with current use of cigarettes, e-cigarettes, and alcohol in adults: wave 1 of the Population Assessment of Tobacco and Health (PATH) study. Addict Behav. 2021;119:106890. 10.1016/j.addbeh.2021.106890. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 97.•.Al Rifai M, Merchant AT, Nambi V, Jia X, Gulati M, Valero-Elizondo J, et al. Temporal trends in e-cigarette use among U.S. adults: behavioral risk factor surveillance system, 2016 to 2018. Am J Med. 2020;133(9):e508–11. 10.1016/j.amjmed.2019.12.020. [DOI] [PubMed] [Google Scholar]; Review article that looks at temporal patterns of e-cigarette use among adults stratified by sexual orientation and gender identify characteristics as well as other demographic characteristics such as ethnicity.
- 98.•.Mattingly DT, Zavala-Arciniega L, Hirschtick JL, Meza R, Levy DT, Fleischer NL. trends in exclusive, dual and polytobacco use among U.S. adults, 2014–2019: results from two nationally representative surveys. Int J Environ Res Public Health. 2021;18(24). 10.3390/ijerph182413092. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article. One of several examples in this review that compares results from two or more national population level surveys. Such studies help distinguish evidence convincingly replicated across studies from findings that require additional exploration.
- 99.•.Correa-Fernandez V, Tavakoli N, Motsenbocker M, Kim H. Hispanics/Latinos’ cigarette and e-cigarette use: behavioral and self-rated health. Am J Health Behav. 2021;45(1):95–110. 10.5993/AJHB.45.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 100.•.Rhoades DA, Comiford AL, Dvorak JD, Ding K, Hopkins M, Spicer P, et al. Perceptions of smoking and vaping on weight control among adult American Indians who smoke. J Community Health. 2019;44(6):1120–6. 10.1007/s10900-019-00694-x. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 101.•.Rollins LG, Sokol NA, McCallum M, England L, Matteson K, Werner E, et al. Electronic cigarette use during preconception and/or pregnancy: prevalence, characteristics, and concurrent mental health conditions. J Women’s Health (2002). 2020;29(6):780–8. 10.1089/jwh.2019.8089. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 102.•.Syamlal G, Clark KA, Blackley DJ, King BA. Prevalence of electronic cigarette use among adult workers - United States, 2017–2018. MMWR Morb Mortal Wkly Rep. 2021;70(9):297–303. 10.15585/mmwr.mm7009a1. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 103.•.Wang Y, Laestadius L, Stimpson JP, Wilson FA. Association between e-cigarette use and acculturation among adult immigrants in the United States. Subst Abuse: Res Treatment. 2019;13:1178221819855086. 10.1177/1178221819855086. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 104.•.Alcala HE, Shimoga SV. It is about trust: trust in sources of tobacco health information, perceptions of harm, and use of e-cigarettes. Nicotine & tobacco research: official journal of the Society for Research on Nicotine and Tobacco. 2020;22(5):822–6. 10.1093/ntr/ntz004. [DOI] [PubMed] [Google Scholar]; Review article
- 105.•.Kosterman R, Epstein M, Bailey JA, Furlong M, Hawkins JD. The role of electronic cigarette use for quitting or reducing combustible cigarette use in the 30s: longitudinal changes and moderated relationships. Drug Alcohol Depend. 2021;227:108940. 10.1016/j.drugalcdep.2021.108940. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 106.•.Kosterman R, Epstein M, Bailey JA, Oesterle S, Furlong M, Hawkins JD. Adult social environments and the use of combustible and electronic cigarettes: opportunities for reducing smoking in the 30s. Nicotine Tob Res. 2021;23(3):518–26. 10.1093/ntr/ntaa019. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 107.•.Martinasek MP, Wheldon CW, Parsons CA, Bell LA, Lipski BK. Understanding adverse childhood experiences as predictors of cigarette and e-cigarette use. Am J Prev Med. 2021;60(6):737–46. 10.1016/j.amepre.2021.01.004. [DOI] [PubMed] [Google Scholar]; Review article
- 108.Dai H, Benowitz NL, Achutan C, Farazi PA, Degarege A, Khan AS. Exposure to toxicants associated with use and transitions between cigarettes, e-cigarettes, and no tobacco. JAMA Netw Open. 2022;5(2):e2147891. 10.1001/jamanetworkopen.2021.47891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.•.Fahey MC, Talcott GW, McMurry TL, Klesges RC, Tubman D, Krukowski RA, et al. When, how, & where tobacco initiation and relapse occur during U.S. Air Force technical training. Mil Med. 2020;185(5–6):e609–15. 10.1093/milmed/usaa016. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 110.•.Azagba S, Shan L. Examining the role of acculturation in e-cigarette use among u.s. immigrant adults. Int J Environ Res Public Health. 2021;18(7). 10.3390/ijerph18073658. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review article
- 111.Rodriguez-Bolanos R, Arillo-Santillan E, Guzman-Rodriguez C, Barrientos-Gutierrez I, Gallegos-Carrillo K, Titus A, et al. Similarities and differences in substance use patterns among lesbian, gay, bisexual, and heterosexual Mexican adult smokers. LGBT Health. 2021;8(8):545–53. 10.1089/lgbt.2020.0457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Mirbolouk M, Charkhchi P, Kianoush S, Uddin SMI, Orimoloye OA, Jaber R, et al. Prevalence and distribution of e-cigarette use among U.S. adults: behavioral risk factor surveillance system, 2016. Ann Intern Med. 2018;169(7):429–38. 10.7326/M17-3440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Cummins SE, Zhu S-H, Tedeschi GJ, Gamst AC, Myers MG. Use of e-cigarettes by individuals with mental health conditions. Tob Control. 2014;23(Suppl 3):iii48–53. 10.1136/tobaccocontrol-2013-051511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Spears CA, Jones DM, Weaver SR, Pechacek TF, Eriksen MP. Use of electronic nicotine delivery systems among adults with mental health conditions, 2015. Int J Environ Res Public Health. 2016;14(1). 10.3390/ijerph14010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wagoner KG, Reboussin DM, King JL, Orlan E, Cornacchione Ross J, Sutfin EL. Who is exposed to e-cigarette advertising and where? Differences between adolescents, young adults and older adults. Int J Environ Res Public Health. 2019;16(14):2533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Lee J, Suttiratana SC, Sen I, Kong G. E-cigarette marketing on social media: a scoping review. Curr Addict Rep. 2023:1–9.37359146 [Google Scholar]
- 117.Tan AS, Lee C-J, Bigman CA. Public support for selected e-cigarette regulations and associations with overall information exposure and contradictory information exposure about e-cigarettes: findings from a national survey of US adults. Prev Med. 2015;81:268–74. [DOI] [PubMed] [Google Scholar]
- 118.Choi K, Omole T, Wills T, Merianos AL. E-cigarette-inclusive smoke-free policies, excise taxes, tobacco 21 and changes in youth e-cigarette use: 2017–2019. Tob Control. 2022;31(6):758–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


