Dear Editor,
With this letter, we want to report our experience using CO2 laser to treat a facial skin condition caused by Muir–Torre syndrome (MTS). MTS is an autosomal dominant variant of hereditary non‐polyposis colorectal cancer, whose mechanism lies in mutations in DNA mismatch repair genes, causing microsatellite instability. It is known that the most critical aspect of the disease is visceral malignancy insurgence, with colorectal carcinoma being the most prevalent, but one of its most visible hallmarks include sebaceous skin neoplasms, which can impair self‐esteem and quality of life.
Skin manifestations of MTS include sebaceous adenomas, epitheliomas, carcinomas, cystic sebaceous tumours, basal cell carcinomas with sebaceous differentiation and keratoacanthomas. Typically, these are yellowish, slow‐growing papules and nodules, primarily on the face, and are hard to control and treat.
The case regards a 56‐year‐old North Italian woman, diagnosed MTS at 17, presented with a significant family history of early‐age colorectal cancer and numerous facial sebaceous lesions from puberty. Genetic testing confirmed a heterozygote mutation in the MSH2 gene.
Over the last decade, she has undergone various dermatological treatments for cosmetic improvement of her lesions. An initial 3‐month course of oral isotretinoin (1 mg/kg/day) yielded minimal benefit [1]. Subsequent surgical therapies, including curettage, electro‐dissection, needling and deroofing, only slightly reduced lesion number and size. Despite pre‐treatment with topical lidocaine, the patient discontinued these painful procedures.
During her last examination, 73 yellowish papules (1–3 mm in diameter) were counted on her face (Figure 1A). Given the limited success with previous treatments, we opted for fractional carbon dioxide (CO2) laser therapy based on the literature and our laser know‐how in different diseases [2, 3, 4, 5].
FIGURE 1.
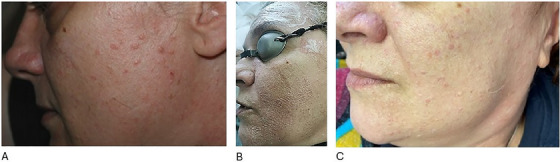
(A) Close‐up of facial skin before fractioned CO2 laser treatment. (B) Facial skin during fractioned CO2 laser treatment. (C) Patient after three CO2 laser sessions: the skin appears smoother, and the sebaceous lesions are less prominent.
We treated the affected facial area using a CO2 laser with fractional mode (400 µm distance, single stack, 11 W, single pass with 5%–10% overlap). Each session was preceded by a 30‐min application of 40 mg/g lidocaine cream. The treatment cycle consisted of three sessions every 2 months for three cycles in total. The patient tolerated the treatments well.
Post‐treatment, the lesion count decreased from 73 to 51, a 31% reduction (Figure 1B). The average lesion diameter reduced from 2.2 to 1.8 mm, indicating a 19% size reduction (p < 0.001). Notably, the patient reported an acceptable pain level, with an NRS score of 4/10 during treatment and 3/10 or lower at other times, demonstrating the tolerability and safety of the CO2 laser therapy.
At the 1‐month follow‐up visit, the patient expressed her satisfaction with the treatment and willingness to halt subsequent therapy (Figure 1C). This positive feedback further reinforces the efficacy of the CO2 laser therapy in managing her condition.
Fractional CO2 laser therapy is an advancement of continuous pulsed CO2 treatment. Similar to studies that used the effects of micro‐thermal zones to induce collagen remodelling [3, 5], it aims to reach similar endpoints to those of fully ablative treatments but with fewer side effects, especially on the face. It promotes skin remodelling, reduces scar risk and improves tolerability.
We think it may be another viable alternative for managing multiple facial sebaceous hyperplasia, including those in syndromic cases like MTS, especially for patients with poor results from conventional therapies and low tolerance for traditional methods.
Ethics Statement
The authors have nothing to report.
Consent
The patients in this manuscript have given written informed consent to publish their case details.
Conflicts of Interest
The authors declare no conflicts of interest.
Acknowledgements
The authors have nothing to report.
Leuzzi Miriam and Zengarini Corrado are co‐first authors.
Funding: This research was supported by the University of Bologna.
Data Availability Statement
Data available on request from the authors.
References
- 1. Tagliolatto S., de Oliveira Santos Neto O., de Avelar Alchorne M. M., and Enokihara M. Y., “Sebaceous Hyperplasia: Systemic Treatment With Isotretinoin,” Anais Brasileiros De Dermatologia 90 (2015): 211–215, 10.1590/abd1806-4841.20153192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Piccolo D., Zingoni T., Fusco I., Madeddu F., and Conforti C., “A Faster CO2 Fractional Scanner System Mode for Skin Rejuvenation. A Clinical Study,” Skin Research and Technology 30 (2024): e13843, 10.1111/srt.13843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bonan P., Fusco I., Bruscino N., et al., “Laser‐Assisted Blepharoplasty: An Innovative Safe and Effective Technique,” Skin Research and Technology 29 (2023): e13351, 10.1111/srt.13351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yoo S., Kim J., Jeong E. T., Hwang S. J., Kang N.‐G., and Lee J., “Penetration Rates Into the Stratum Corneum Layer: A Novel Quantitative Indicator for Assessing Skin Barrier Function,” Skin Research and Technology 30 (2024): e13655, 10.1111/srt.13655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zengarini C., Guglielmo A., Mussi M., et al., “Primary Cutaneous CD4 + Small/Medium T‐Cell Lymphoproliferative Disorder Nodule Successfully Treated With Laser CO2 Ablation: A Case Report and Literature Review,” Dermatology Reports (2024), 10.4081/dr.2024.9884. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request from the authors.


