Abstract
Purpose
Phakic lens implantation in the ciliary sulcus of the eye can be complicated by coincident ciliary body cysts (CBC). We developed an ultrasound imaging and mapping protocol for these cysts.
Methods
This is a retrospective case series of all patients who underwent ICL workup at a single institution from April 2015 to October 2019. A standardized ultrasound biomicroscopy (UBM) imaging protocol was developed to screen for CBCs in either the ciliary body or sulcus. The locations and dimensions of all CBCs were graphically represented.
Results
The prevalence of CBCs in 158 patients undergoing ICL workup was 34.8%. Among the 159 CBCs detected in 55 patients, 83 were in the sulcus (52%) and 76 were restricted to the ciliary body (48%). ICLs were implanted in 40 eyes with CBCs and 3 eyes with CBCs located within the sulcus horizontally required ICL repositioning due to ICL rotation or iris chafing.
Conclusion
CBCs were incidentally found in 34.8% of patients undergoing ICL workup. ICL implantation was complicated in 3 of the eyes with CBCs in the horizontal sulcus. Although CBCs are not an absolute contraindication for ICL surgery, we recommend preoperative UBM screening of the ciliary sulcus.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10792-024-03320-5.
Keywords: Ciliary sulcus ultrasonography, Ciliary body cyst, Implantable collamer phakic lens, Myopia
Introduction
The implantable collamer lens (ICL) (STAAR Surgical, Monrovia, CA, USA) is a foldable posterior chamber phakic intraocular lens used to correct refractive errors. ICL implantation can correct + 10 diopters (D) to − 18D of sphere and ≤ 6D of astigmatism. ICLs are manufactured to be centered horizontally within the eye and implanted in the ciliary sulcus. Each haptic has 2 footplates to stabilize the ICL against the sulcus wall and maintain its desired vault from the crystalline lens. However, in many instances the footplates have been found to rest elsewhere, such as atop the ciliary body [1, 2]. ICL length is chosen to achieve an optimal vault above the crystalline lens 250 and 750 μm. Lower vaults increase the risk of cataract formation [3, 4], and larger vaults can predispose to secondary glaucoma [5–7].
The presence of ciliary body cysts (CBCs) located at the iridociliary junction within the ciliary sulcus can complicate the positioning and vault of an ICL [8, 9]. CBCs are not uncommon in the general population. In previous studies, the prevalence of primary CBCs ranges from 4.9% to 54.3% [10–12]. Histological studies show these CBCs to be fluid-filled cavities with an epithelial-lined wall [12]. They are more common in women than men and usually located in the horizontal meridian [12]. Although CBCs are traditionally detected by mydriatic examination with a Goldmann 3-mirror contact lens, ultrasound biomicroscopy (UBM) provides significant advantages, such as cross-sectional imaging, surface contour, internal reflectivity and border detection [8, 10, 13]. It also permits accurate and reproducible localization.
During evaluation for ICL placement in our clinic, UBM is routinely used to measure the sulcus-to-sulcus horizontal diameter and other internal dimensions to enable the use of ICL sizing nomograms which utilize these values [14, 15]. In addition, we perform a 360-degree qualitative assessment of the ciliary sulcus looking for anatomical anomalies, such as CBCs, to prevent postoperative complications related to improper ICL vault. The purpose of this study was to measure the prevalence and location of CBCs in candidates for ICL surgery, as well as to evaluate the safety and outcomes of ICL placement in these patients.
Materials and methods
Patients who were evaluated from April 2017 to October 2019 for ICL implantation at Cleveland Clinic Abu Dhabi (CCAD) were included in this retrospective review. All patients underwent preoperative screening and examination, which included: uncorrected distance visual acuity (UDVA), best corrected distance visual acuity (BCVA), intraocular pressure (IOP) measurement, manifest spherical equivalent refraction (MRSE), slit lamp examination, gonioscopy, endothelial cell density (ECD) (CEM-530 Specular Microscopy, Nidek, Gamagori, Japan), corneal tomography (Galilei dual Scheimpflug system, Ziemer Ophthalmic System AG, Port, Switzerland), ocular biometry (IOL Master, Carl Zeiss Meditec AG, Jena, Germany), manual horizontal corneal diameter white-to-white measurement, cycloplegic refraction and dilated fundus examination.
Qualitative UBM analysis was done with the 50 MHz Aviso S (Quantel Medical, Clermont-Ferrand, France) for 360-degrees around the ciliary sulcus looking for CBCs. The procedure is performed with a balanced salt solution filled ClearScan cover (ESI Inc. Minnesota, USA) over the tip of the ultrasound probe (Fig. 1). The ClearScan cover is comfortable for most patients due to its soft interface. This technique highly resolves soft tissue structures within a depth of 3 mm spanning 2 clock hours from the probe’s surface contact. Complete imaging of the ciliary body and sulcus is obtained with a series of transverse cuts, starting at the horizontal meridian, and progressing clockwise at 1 ½ clock hour intervals (i.e., 10:30–4:30, 12:00–6:00, 1:30–7:30) (Fig. 2).
Fig. 1.
Image of the 50 MHz Aviso S ultrasound biomicroscopy (UBM) probe with ClearScan cover. Top, Probe with ClearScan cover before assembly. Left, Disposable Clearscan Cover filled with balanced salt solution. Right, during contact of the anesthetized eye, care is taken to open the lids without applying pressure to the globe
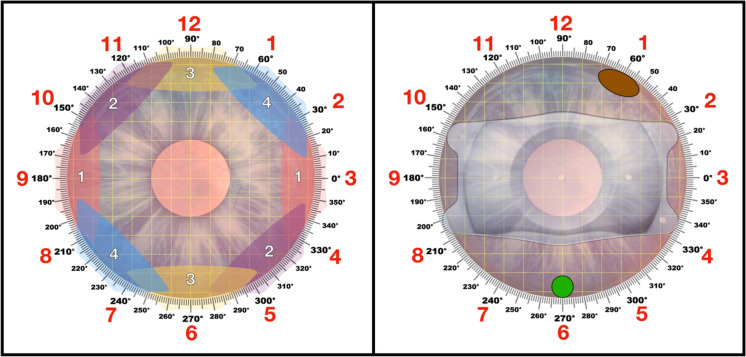
Fig. 2.
Screening protocol for ciliary body cysts (CBCs). Left, White numbered areas show the scanning sequence and approximate ultrasound imaging depth used to create a 360° map of all ciliary body cysts. A 1 mm square grid is overlaid (yellow lines) and clock hours are indicated (red numbers). Right, Screening map with implantable collamer lens (ICL) image overlaid depicting a 1 × 2 mm sulcus cyst at 1 o’clock (brown oval) and a 1 mm cyst confined to the ciliary body at 6 o’clock (green circle)
An echo-free, round or oval fluid-filled lesion detected in the ciliary body or sulcus was defined as a cyst. The number, size (horizontal and vertical diameters) and location by clock hour and anatomical location were measured and documented on a 2–dimensional map (Fig. 2). Cyst characteristics were further defined and recorded according to whether there was protrusion into the ciliary sulcus.
Quantitative measurement of the sulcus is then taken with the Compact Touch STS UBM (Quantel Medical, Cournon d’Auvergne, France) via a centered axial cut. The device measures the sulcus-to-sulcus (STS) diameter, aqueous depth (AQD), and distance between the STS plane and anterior crystalline lens surface (LC) (Fig. 3). All UBM examinations were completed by the same, experienced ultrasonography technician (KQ).
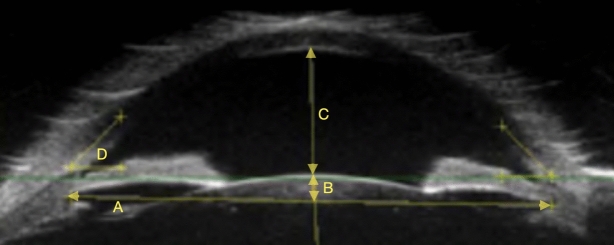
Fig. 3.
Axial ultrasound biomicroscopy (UBM) measurements of a right eye. A = Sulcus-to-Sulcus, B = Distance between the STS plane and anterior crystalline lens surface, C = Aqueous depth, D = Interior chamber angle. UBM with probe position = 9:00, gain = 110 decibels, dynamic range = 60 decibels, total gain control = 15 decibels
The inclusion criteria for ICL placement were: 21–45 years of age, desire for spectacle and contact lens independence, stable refraction ≥ 1 year, AQD ≥ 2.8 mm, ECD ≥ 2200 cell/mm2, stable corneal tomography, gonioscopy grade ≥ III in all 4 quadrants, and no history of cataract, glaucoma, uveitis, or uncontrolled diabetes. Lens power calculations were performed considering the patient’s manifest and cycloplegic refraction using the manufacturer’s calculator (https://ocos.staarag.ch). A lens sizing calculation is performed with the manufacturer’s nomogram, which utilizes manual corneal white-to-white and AQD measurements. We also consider two external nomograms for ICL sizing recommendations. The Kojima ICL sizing nomogram is based on STS diameter, AQD and LC measurements [14]. The Dougherty ICL sizing nomogram is based on STS diameter and ICL power [15]. Final ICL size was at the discretion of the surgeon selecting the ICL closest to the average of the recommendations from all 3 sizing nomograms.
All ICL surgeries were performed by 4 experienced surgeons. The surgical procedure was performed through a 3.2 mm temporal corneal incision and 1 or 2 paracenteses as per surgeon preference. The anterior chamber was filled with a cohesive viscoelastic (Microvisc 1%; Bohus Biotech, Sousel, Portugal). A VICMO (spherical) or VTICMO (toric) ICL was inserted into the anterior chamber with an injector cartridge and implanted into the ciliary sulcus within the horizontal meridian. For toric ICLs, rotation to the recommended axis is performed using a digital intraoperative guidance system (Callisto, Carl Zeiss Meditec AG, Jena, Germany) from a preoperative reference image. Subsequently, viscoelastic is removed from the anterior chamber using a balanced salt solution. Acetylcholine 1% (Miochol®, Novartis, Camberley, UK) is instilled intracamerally to constrict the pupil, and compounded intracameral Cefuroxime 1 mg/0.1 mL is injected for infection prophylaxis prior to final hydration of corneal wounds. Postoperative follow-ups were performed at approximately 1 day, 1 week, 1-, 3-, 6- and 12-months following surgery. Postoperative evaluation included UDVA, CDVA, MRSE, IOP, slit lamp examination and ICL vault measurement via anterior segment ocular coherence tomography (Heidelberg Engineering, Heidelberg, Germany).
Statistical analysis
Statistical analyses were performed using Microsoft R Open (Microsoft Corporation [2020]. MicrosoftR: Microsoft R umbrella package. R package version 4.0.2.) and R Studio (RStudio Team [2021]. RStudio: Integrated Development Environment for R. RStudio, PBC, Boston, MA). Unadjusted descriptive statistics were reported for the sample overall, and by subgroups of patients with and without CBCs. Unadjusted group comparisons on continuous and dichotomous variables were made using t-tests and logistic regression respectively. To examine the relationship between an outcome and a set of predictors, we utilized multivariate fixed effects linear or logistic regression models to estimate the partial regression relationships. For eyes that underwent ICL placement, temporal trends among surgical patients were studied using linear mixed effects models. Further, likelihood ratio tests were used to check if CBC presence as a parameter improved the fit of the linear mixed effects models for post-operative outcomes (UDVA and IOP). In most instances, a two-tailed alpha of 0.05 is used to determine statistical significance, aside from AQD in which case one- and two-tailed tests were performed.
Results
Three hundred sixteen eyes of 158 consecutive patients (65 males, 93 females) who were undergoing workup for ICL implantation at Cleveland Clinic Abu Dhabi (CCAD) were included in this study. Mean patient age at the time of ICL evaluation was 31.1 (± 6.4) years (range 20–48 years). The mean preoperative MRSE was − 5.619 (± 3.74) diopters (D), (range − 23.375 to − 0.125) in myopic patients and + 4.025 (± 2.67) diopters (D), (range + 0.375 to + 7.125) in hyperopic patients. Among 158 patients (316 eyes), CBCs were detected in 55 patients (34.8%) (95% CI [27.8, 42.5]) and 81 eyes (25.6%) (95% CI [21.1, 30.7]). There were no solid tumors detected. Cysts were detected in 24 male (36.9%) and 31 female (33.3%) patients. They were unilateral in 30 patients and bilateral in 25 patients. Forty-two eyes (51.8%) had a single cyst, 16 eyes (19.7%) had 2 cysts, and 23 eyes (28.4%) had ≥ 3 cysts. The mean size of cysts was 0.45 mm ± 0.19 (range 0.14–1.19 mm) vertically and 0.56 mm ± 0.27 (range 0.05–1.66 mm) horizontally. Among 159 cysts detected, 83 (52.2%) were located within the sulcus and 76 (47.8%) were restricted to the ciliary body (Fig. 4).
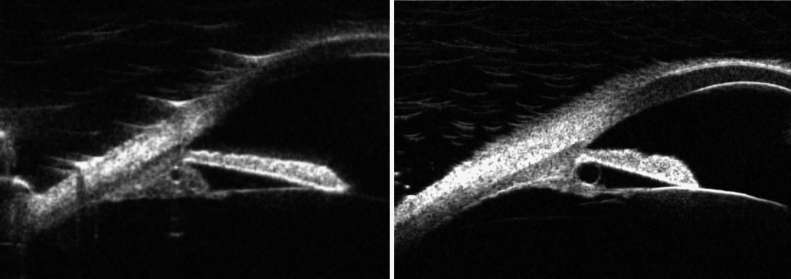
Fig. 4.
Axial cuts of the two types of ciliary body cysts (CBCs). Right, a small CBC that is restricted to the ciliary body. Left, a larger ciliary body cyst which exhibits substantial extension into the ciliary sulcus
Eighty-four (41.8%) CBCs were in the horizontal meridian (2–4 o’clock, 8–10 o’clock), 54 (26.9%) were in the vertical meridian (11–1 o’clock, 5–7 o’clock), and 63 (31.3%) were in an oblique meridian (remaining clock hours). There were no statistically significant differences between patients with and without CBCs for the preoperative parameters studied (Table 1).
Table 1.
Preoperative parameters in eyes with and without ciliary body cysts. UDVA = uncorrected distance visual acuity, CDVA = corrected distance visual acuity, MRSE = manifest refractive spherical equivalent, IOP = intraocular pressure, ECD = endothelial cell density, AQD aqueous depth, WTW = horizontal white to white measurement, STS = sulcus to sulcus, LC = distance between STS plane and anterior crystalline lens surface
| With cysts | No cysts | p (mean diff) | |||
|---|---|---|---|---|---|
| Mean/N | SD/% | Mean/N | SD/% | ||
| Age | 30.67 | 6.77 | 31.29 | 6.32 | 0.46 |
| Male | 36 | 44.4% | 94 | 40.0% | 0.48 |
| UDVA | 1.20 | 0.59 | 1.18 | 0.55 | 0.86 |
| CDVA | − 0.01 | 0.08 | 0.00 | 0.11 | 0.94 |
| MRSE | − 5.24 | 2.95 | − 5.64 | 4.00 | 0.41 |
| IOP | 12.8 | 3.5 | 13.0 | 3.0 | 0.69 |
| Gonioscopy grade | 3.76 | 0.51 | 3.87 | 0.37 | 0.09 |
| ECD | 2623 | 275 | 2679 | 308 | 0.17 |
| AQD | 3.23 | 0.27 | 3.29 | 0.25 | 0.08 |
| Corneal WTW | 11.66 | 0.39 | 11.73 | 0.47 | 0.28 |
| STS diameter | 11.70 | 0.55 | 11.79 | 0.58 | 0.26 |
| LC | 0.59 | 0.16 | 0.61 | 0.19 | 0.42 |
There was a trend towards decreased AQD in eyes with CBCs (3.23 ± 0.26 mm) compared to eyes without CBCs (3.29 ± 0.24 mm), but that difference did not reach statistical significance (p = 0.078) using a 2–tailed test. Because CBCs are known to be associated with anatomic angle narrowing [7, 16, 17], there is a theoretical reason for the eyes with CBCs to have shallow AQD. Therefore, we calculated the p-value to be 1- tailed in the expected direction, which showed that eyes with CBCs had lower AQD than eyes without CBCs (p = 0.04).
A substantial number of ICL candidates in our practice have keratoconus due to high prevalence in our region [18]. Keratoconus was present in 43.7% of our study subjects, and there was no statistically significant relationship between keratoconus and the presence of CBCs.
Of the 316 eyes that underwent workup for ICL placement, 147 eyes of 85 patients eventually proceeded with ICL placement. All patients who underwent ICL placement were myopic. In subgroup analysis of patients who underwent ICL placement, 107 eyes of 60 patients without CBCs had ICL implantation, and 40 eyes of 25 patients with CBCs had ICL implantation. Preoperative characteristics of these 2 groups revealed no statistically significant differences in age, gender, UDVA, CDVA, MRSE, or IOP. The average ICL vault measurement was 556.91 microns in patients without CBCs and 553.39 microns in patients with CBCs which was not statistically significant (p = 0.9517). Of the 40 eyes of 25 patients with CBCs that underwent ICL placement, 12 eyes of 8 patients had CBCs within the horizontal meridian located in the ciliary sulcus. The remainder of the eyes had CBCs located vertically, obliquely, or limited to the ciliary body where it was felt they would have no impact on ICL positioning or vault.
Of the eyes with CBCs within the horizontal sulcus that underwent ICL placement, surgery and postoperative follow up were uneventful, except for 3 eyes of 3 patients. All 3 eyes required secondary ICL repositioning. Two of the cases involved toric ICLs that postoperatively rotated away from the intended axis of implantation, resulting in decreased vision. One of these cases had a single 1 mm diameter horizontal sulcus CBC at 4 o’clock and the other had dual 0.5 mm diameter sulcus CBC’s at 9:00 and 9:30 o’clock. For the third case, after ICL placement in the horizontal meridian, the patient presented with photophobia, limbal injection and rare pigmented cells in the anterior chamber. The eye had 4 CBCs total, with one large 1 mm diameter CBC within the ciliary sulcus in the horizontal meridian at 4 o’clock. Postoperative UBM showed the temporal ICL footplate to be resting on the wall of the CBC at 4 o’clock instead of the wall of the sulcus. The nasal footplate was thus rotated forward and pushing against the posterior aspect of the iris nasally, causing posterior iris chafing of the nasal footplate. UBM imaging identified an axis at 83° where we felt the footplates would not interfere with any CBCs, so this non-toric ICL was rotated to that axis and the symptoms resolved.
We sought to understand the trajectory of two post-operative outcomes–UDVA and IOP–over time between the 2 groups of patients who underwent ICL placement with and without CBCs. Linear mixed effects regression models were adjusted for patient level random effects, with a randomly varying intercept by patient and a randomly varying intercept and slope for patient and eye laterality (see Appendix 1.1 for regression coefficient tables of supplementary). It was noted that UDVA on the logMAR scale had a statistically significant non-linear trajectory over time. On the other hand, IOP did not show a statistically significantly varying trajectory over time. The graphical representations of both trajectories are presented in Appendix 1.1 of supplementary for further examination. Exploration of hierarchically nested mixed-effects linear models was done using a likelihood ratio test (LRT) to check for an association between the presence of CBCs and post-operative outcomes in a given eye (see Appendix 1.1 of supplementary). The LRT for UDVA showed no significant association with CBC presence (χ2 = 2.59, p = 0.629), as did the LRT for IOP (χ2 = 3.13, p = 0.680).
Discussion
ICL placement is an excellent solution for vision correction. However, preoperative screening for sulcus pathology is important, and it is critical to understand if ICLs can be implanted in the presence of CBCs. Our protocol for screening the sulcus for CBCs prior to ICL placement is described. We consider the addition of the UBM to be extremely valuable, not only for preoperative ICL planning but also for managing postoperative complications. We prefer the ClearScan UBM technique as compared to the standard immersion shell technique. The ClearScan technique provides superior ciliary sulcus resolution (Fig. 5). Given that the ClearScan is a single-use, fluid-filled, soft latex interface, it increases sterility and comfort for the patient. Communication between the ultrasonographer and surgeon is advised to highlight the potential risk of interference between CBCs and proper ICL footplate seating.
Fig. 5.
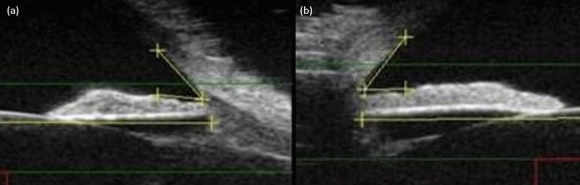
Axial ultrasound biomicroscopy (UBM) imaging of in the horizontal plane of the same eye with a UBM probe centered on the pupil and bisecting the eye utilizing the clear scan cover (left) and the immersion scleral shell technique (right). Utilizing identical UBM settings, imaging with the Clear Scan shows a more detailed view of the ciliary body structures than the Scleral Shell technique due to deeper penetration within the tissue
We found the prevalence of incidental CBCs to be 34.8% (95% CI [27.8, 42.5]). This data adds to a handful of other studies assessing the prevalence of CBCs in different regions of the world. In a retrospective review of UBM cases in Brazil, CBCs were detected in 56 (4.9%) of 1157 patients [11]. In a prospective analysis of patients in Japan, CBCs were detected in 63 (54.3%) of 116 patients [10]. Lastly, a retrospective review of UBM cases at Wills Eye Institute found that CBCs were detected in 39 (14.8%) of 263 patients [12]. Taken together, CBCs are more prevalent than realized because they are usually asymptomatic and require advanced examination and/or imaging techniques to locate.
Overall preoperative characteristics and postoperative outcomes, including UDVA and IOP, were similar in eyes that underwent ICL placement with and without CBCs. In this retrospective review, it was at the surgeon and patient’s discretion as to whether to proceed with ICL placement in the presence of CBCs. Many of these cases did not go forward after careful informed consent discussion between the patient and surgeon about the inherent risks of implanting an ICL in an eye with CBCs. Most of the eyes with CBCs that underwent ICL implantation had CBCs either limited to the ciliary body or within a vertical or oblique region that would not interfere with ICL positioning or vault, because ICL placement in these eyes is generally considered safe. However, of the 40 eyes of 25 patients with CBCs that underwent ICL placement, 12 eyes of 8 patients had CBCs within the horizontal meridian located in the ciliary sulcus. Extra consideration and more extensive postoperative monitoring must be taken in these eyes, as there are known case reports of intraocular cysts affecting ICL positioning and leading to glaucoma.9 In our retrospective review, 3 eyes of 3 patients with an ICL in the horizontal sulcus required reoperation with secondary ICL repositioning due to incorrect toric alignment in 2 eyes and iris chafing causing pigment release in the other. Exercise caution when rotating an ICL away from the horizontal meridian because the sulcus-to-sulcus diameter is typically greater vertically, compared to horizontally [19–22], resulting in reduced ICL vault in the vertical meridian.
Two prior studies have assessed the safety and efficacy of ICL placement in eyes with CBCs. Zhao et al. assessed ICL placement in 37 eyes of 19 patients with CBCs [23]. Surgery resulted in no complications and good refractive results. They monitored CBC size postoperatively over 18 months and found no change in the CBC number, dimensions or characteristics after ICL placement. Li et al. assessed the outcomes of ICL surgery in 54 eyes with CBCs, and they concluded that ICL placement was safe in eyes with a single CBC smaller than 1 mm or single quadrant CBCs [24]. However, they recommended avoiding ICL placement in eyes with multiple and/or multi-quadrant CBCs.
In patients found to have incidental CBCs during preoperative UBM screening, we recommend first informing the patient and reassuring them that no tumor or neoplastic process is present. If CBCs are present within the ciliary sulcus in the horizontal meridian, we warn the patient that postoperative ICL vault may be affected. If ICL vault is abnormal postoperatively, then additional surgical intervention might be required, whether it be ICL exchange, rotation or explantation. We believe that undiagnosed CBCs within the sulcus might be an underlying cause of excessive ICL vault or other reported complications [21]. Routinely screening the sulcus preoperatively for sulcus pathology via UBM makes the surgeon better prepared to anticipate and manage cases related to improper ICL vault.
This study has several weaknesses. First, this was not a population-based screening, so the prevalence of CBCs in this study cannot be attributed to the regional population as there is inherent sampling bias towards patients with high refractive error. The patients in this review were coming for ICL workup and were also skewed towards younger myopic patients. Therefore, we believe this data to be relevant to ICL surgeons. Second, this study was retrospective in nature, so the decision as to whether to proceed with ICL placement was at the surgeon’s discretion upon consultation with the patient.
In conclusion, incidental CBCs were found in roughly one third of patients undergoing ICL workup at CCAD. We recommend methodical UBM preoperative imaging of the ciliary sulcus prior to ICL implantation. Given an increased incidence of reoperation in 25% of eyes where there are sulcus CBCs in the axis of horizontal ICL implantation (from 2 to 4 o’clock and/or 8–10 o’clock), we recommend caution against surgery in these cases. In cases where there are oblique sulcus cysts and astigmatism correction is needed, we recommend requesting toric ICL manufacturing as opposed to reserving a toric ICL, which might require as much as 21 degrees of cyclorotation for astigmatism axis alignment. When considering ICL placement in eyes with CBCs, the possibility of needing to reposition or explant an ICL should be included in the preoperative discussion with the patient.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by B.K.A., I.R.C. and N.P. The first draft of the manuscript was written by B.K.A. and S.E.N. and all authors commented on previous versions of the manuscript. Statistical analysis was performed by T.L.S.J. and O.K.. Conceptualization: S.E.N., B.K.A., I.R.C. and K.Q.; Methodology, S.E.N. and B.K.K.; Formal analysis and investigation: T.L.S.J. and O.K.; Writing—original draft preparation: S.E.N. and B.K.A.; Writing—review and editing: S.E.N., B.K.A., I.R.C. and N.P.; Funding acquisition: n/a Resources, n/a; Supervision, B.K.A.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data availability
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Cleveland Clinic Abu Dhabi (study number RE 19-031, date of approval: 2nd January 2020) for studies involving humans.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zaldivar R, Adamek P, Quintero G, Cerviño A (2022) Descriptive analysis of footplate position after myopic implantable collamer lens implantation using a very high-frequency ultrasound robotic scanner. Clin Ophthalmol 16:3993–4001. 10.2147/opth.s393223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang X, Chen X, Wang X, Yuan F, Zhou X (2018) Analysis of intraocular positions of posterior implantable collamer lens by full-scale ultrasound biomicroscopy. BMC Ophthalmol 18(1):114. 10.1186/s12886-018-0783-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.AlSabaani NA, Behrens A, Jastanieah S, Al Malki S, Al Jindan M, Al MS (2016) Causes of phakic implantable collamer lens explantation/exchange at king Khaled eye specialist hospital. Middle East Afr J Ophthalmol 23(4):293–295. 10.4103/0974-9233.194076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maeng HS, Chung TY, Lee DH, Chung ES (2011) Risk factor evaluation for cataract development in patients with low vaulting after phakic intraocular lens implantation. J Cataract Refract Surg 37(5):881–885. 10.1016/j.jcrs.2010.11.037 [DOI] [PubMed] [Google Scholar]
- 5.Thomas R, Mulligan N, Aylward GW, Billson FA (1989) Angle closure glaucoma due to iris and ciliary body cysts. Aust N Z J Ophthalmol 17(3):317–319. 10.1111/j.1442-9071.1989.tb00541.x [DOI] [PubMed] [Google Scholar]
- 6.Ritch R, Chang BM, Liebmann JM (2003) Angle closure in younger patients. Ophthalmology 110(10):1880–1889. 10.1016/s0161-6420(03)00563-3 [DOI] [PubMed] [Google Scholar]
- 7.Seki M, Fukuchi T, Yoshino T et al (2014) Secondary glaucoma associated with bilateral complete ring cysts of the ciliary body. J Glaucoma 23(7):477–481. 10.1097/IJG.0b013e31827a088c [DOI] [PubMed] [Google Scholar]
- 8.Marigo FA, Esaki K, Finger PT et al (1999) Differential diagnosis of anterior segment cysts by ultrasound biomicroscopy. Ophthalmology 106(11):2131–2135. 10.1016/s0161-6420(99)90495-5 [DOI] [PubMed] [Google Scholar]
- 9.Gharaibeh AM, Liehneova I, Mojzis P, Ziak P, Alió JL (2020) Iris and ciliary body cysts and phakic intraocular lenses. Eur J Ophthalmol 30(5):974–977. 10.1177/1120672119876532 [DOI] [PubMed] [Google Scholar]
- 10.Kunimatsu S, Araie M, Ohara K, Hamada C (1999) Ultrasound biomicroscopy of ciliary body cysts. Am J Ophthalmol 127(1):48–55. 10.1016/s0002-9394(98)00308-0 [DOI] [PubMed] [Google Scholar]
- 11.Cronemberger S, Ferreira DM, Diniz Filho A, Mérula RV, Calixto N (2006) [Iridociliary cysts on ultrasound biomicroscopic examinations] Prevalência de cistos iridociliares em exames de biomicroscopia ultra-sônica. Arq Bras Oftalmol 69(4):471–5. 10.1590/s0004-27492006000400003 [DOI] [PubMed] [Google Scholar]
- 12.Shields JA, Kline MW, Augsburger JJ (1984) Primary iris cysts: a review of the literature and report of 62 cases. Br J Ophthalmol 68(3):152–166. 10.1136/bjo.68.3.152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Augsburger JJ, Affel LL, Benarosh DA (1996) Ultrasound biomicroscopy of cystic lesions of the iris and ciliary body. Trans Am Ophthalmol Soc 94: 259–71; discussion 271–4. 10.1016/s0002-9394(14)70165-5 [DOI] [PMC free article] [PubMed]
- 14.Kojima T, Yokoyama S, Ito M et al (2012) Optimization of an implantable collamer lens sizing method using high-frequency ultrasound biomicroscopy. Am J Ophthalmol 153(4):632-637.e1. 10.1016/j.ajo.2011.06.031 [DOI] [PubMed] [Google Scholar]
- 15.Dougherty PJ, Rivera RP, Schneider D, Lane SS, Brown D, Vukich J (2011) Improving accuracy of phakic intraocular lens sizing using high-frequency ultrasound biomicroscopy. J Cataract Refract Surg 37(1):13–18. 10.1016/j.jcrs.2010.07.014 [DOI] [PubMed] [Google Scholar]
- 16.McWhae JA, Rinke M, Crichton AC, Van Wyngaarden C (2007) Multiple bilateral iridociliary cysts: ultrasound biomicroscopy and clinical characteristics. Can J Ophthalmol 42(2):268–271 [PubMed] [Google Scholar]
- 17.Kaushik S, Ichhpujani P, Kaur S, Singh PS (2014) Optic Disk Pit and Iridociliary cyst precipitating angle closure glaucoma. J Curr Glaucoma Pract 8(1):33–35. 10.5005/jp-journals-10008-1158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Armstrong BK, Smith SD, Romac Coc I, Agarwal P, Mustapha N, Navon S (2021) Screening for keratoconus in a high-risk adolescent population. Ophthalmic Epidemiol 28(3):191–197. 10.1080/09286586.2020.1804593 [DOI] [PubMed] [Google Scholar]
- 19.Biermann J, Bredow L, Boehringer D, Reinhard T (2011) Evaluation of ciliary sulcus diameter using ultrasound biomicroscopy in emmetropic eyes and myopic eyes. J Cataract Refract Surg 37(9):1686–1693. 10.1016/j.jcrs.2011.03.048 [DOI] [PubMed] [Google Scholar]
- 20.Gao J, Liao RF (2013) Correlation between white-to-white diameter and ciliary sulcus diameter of high myopia eyes. Zhonghua Yan Ke Za Zhi 49(7):627–632 [PubMed] [Google Scholar]
- 21.Matarazzo F, Day AC, Fernandez-Vega Cueto L, Maurino V (2018) Vertical implantable collamer lens (ICL) rotation for the management of high vault due to lens oversizing. Int Ophthalmol 38(6):2689–2692. 10.1007/s10792-017-0757-2 [DOI] [PubMed] [Google Scholar]
- 22.Zaldivar R, Adamek P, Cerviño A (2022) Intraoperative adjustment of implantable collamer lens vault by lens rotation aided by intraoperative OCT. J Cataract Refract Surg 48(9):999–1003. 10.1097/j.jcrs.0000000000000915 [DOI] [PubMed] [Google Scholar]
- 23.Zhao J, Luo D, Sun Y et al (2019) Implanting a posterior chamber phakic intraocular lens in highly myopic eyes with peripheral primary iris and ciliary body cysts. Eur J Ophthalmol 29(2):171–177. 10.1177/1120672118766445 [DOI] [PubMed] [Google Scholar]
- 24.Li Z, Xu Z, Wang Y, Liu Q, Chen B (2018) Implantable collamer lens surgery in patients with primary iris and/or ciliary body cysts. BMC Ophthalmol 18(1):287. 10.1186/s12886-018-0935-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.