Abstract
Background:
The purpose of this study was to clarify the differences in the movement of the superficial microchambers and deep macrochambers of the heel fat pad during loading and unloading movements, and to clarify the influence of height and weight on this movement.
Methods:
The subjects were 21 healthy adults. The right foot was placed on an evaluation instrument stand made of polymethylpentene (PMP) resin plate, and the left foot was placed on a scale stand used to adjust the amount of load. When measuring, the heel fat pad is divided into the superficial microchamber layer and the deep macrochamber layer, and the thickness due to loading from 0% to 100% of the body weight and unloading from 100% to 0% is measured. Measurement was performed every 20% using an ultrasound imaging device. We also examined the rate of change in the thickness of the superficial and deep layers of the heel fat pad when applying 100% load (end load) from 0% load (unload).
Results:
No changes were observed in the superficial layer of the heel fat pad during unloading, but significant changes were observed in the deeper layers. Additionally, the thickness of the microchamber and macrochamber layers tended to increase under each loading condition as the height and weight increased. On the other hand, the rate of change in the thickness of the macrochamber layer tended to decrease.
Conclusion:
The microchamber layer and the macrochamber layer of the heel fat pad may have different functions. As height and weight increase, the thickness of the microchamber and macrochamber layers may increase, and the rate of change in the thickness of the macrochamber layer appears to decrease. Although the thickness increases as the load increases, we found that the related elasticity decreases.
Level of Evidence:
Level Ⅳ, cross-sectional survey study.
Keywords: heel fat pad, microchamber layer, macrochamber layer, ultrasound
Introduction
The heel is the part that first touches the ground (heel strike) during activities of daily living including walking, and the state of load and nonload is frequently repeated. The heel fat pad in the heel absorbs shocks during walking and running. Degeneration or destruction of the area because of continuous pressure load may reduce the shock absorption and dispersion functions and increase heel pain induction risk.1,7 Clarifying this will contribute to elucidation of heel pain pathology and the prevention methods.
Because function depends on tissue structure, many studies have focused on the morphology of the heel fat pad. However, there are limitations in evaluating dynamic soft tissue functions using static indicators.15,17,18 This is important in clarifying the heel fat pad function. Hsu et al have emphasized evaluating dynamic changes in clarifying the soft tissue function. Tissue behavior not only provides information about the tissue but also suggests the presence of disease. 5
Many studies have reported changes in the load on the heel fat pad using various methods.2,4,6,8,14,16,17 However, it was difficult to depict the internal structure in detail, and the heel fat pad was divided into 2 layers: the superficial layer (microchambers [MICs]) and the deep layer (macrochambers [MACs]). The former comprises elastic fibers, and the latter comprises collagen and elastic fibers. Because the adipose tissue morphology differs between the layers, the adipose tissue could exhibit different dynamic changes during loading.1,2,4,6,8,18 Research focused on the functional differences between the 2 layers is limited, and there are various limitations, such as a load limit (20 kg). 4 To solve these problems, we developed an evaluation instrument using a polymethylpentene (PMP) resin plate.12,14 By protecting the acoustic lens of the transducer with a 5-mm-thick PMP resin plate, this can measure changes in the shape of the heel fat pad when a full load is applied (Takiron Polymer Co, Ltd, Fukuoka, Japan). Because the resin plate used in this device has an acoustic impedance close to that of the human body, it is possible to measure the internal structure with high precision.
In our previous study, we reported that the thickness of the microchamber and macrochamber layers of the heel fat pad during nonloading increases with increasing weight and height. 13 This suggests that the structure of the heel fat pad may have changed as an adaptation to the increased load caused by increased height and weight. It is not yet clear how the function changes regarding to load.
Here, we used an evaluation instrument using a PMP resin plate to clarify the differences in the movements of the microchamber and macrochamber layers of the heel fat pad, and then investigated the effects of height and weight in healthy subjects on the microchamber and macrochamber layers of the heel fat pad during loading and unloading movements. The purpose was to clarify the effects on the behavior of microchamber and macrochamber layers.
Material and Methods
Participants
The participants were 21 healthy people (12 men, 9 women) (Table 1). This study used simple random sampling. Participants who met the following were excluded: (1) engaged in strenuous physical activity or consumed alcohol in the past 48 hours; (2) history of foot or ankle surgery or major trauma; (3) ankle or heel pain, such as heel pain or ligament injury, or orthopaedic injuries to the feet; (4) rheumatic diseases such as osteoarthritis, gout, and rheumatoid arthritis; and (5) systemic diseases such as diabetes and/or connective tissue disorders.
Table 1.
Physical Characteristics of Participants. a
| Age, y | Height, cm | Body mass, kg | BMI | Macrochamber layer thickness, mm | Microchamber layer thickness, mm | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | 23.7 | (1.9) | 165.4 | (7.1) | 58.1 | (8.7) | 21.2 | (2.0) | 10.3 | (1.3) | 2.6 | (0.3) |
| Male | 24.6 | (1.8) | 170.6 | (3.9) | 63.4 | (7.2) | 21.8 | (2.2) | 11.0 | (1.0) | 2.9 | (0.3) |
| Female | 22.6 | (1.4) | 158.6 | (3.8) | 51.1 | (4.4) | 20.3 | (1.4) | 9.3 | (1.0) | 2.4 | (0.1) |
Abbreviation: BMI, body mass index.
Data are shown as mean (SD)
The purpose of the study, measurement methods, ethical considerations, etc, were explained to the participants in advance, and their consent obtained. The study protocol was approved by the Ethics Review Committee for Research Involving Human Subjects (approval number 2020-228).
Protocol
Load-measuring instruments
The load measuring device, as in the previous study, comprised two 4-legged iron frames (height, 400 mm; length and width of 350 mm).12,14 One is an evaluation table with a 20-mm-thick polycarbonate resin top plate mounted on a steel frame, and the other a table with a weight scale for measuring the load. The polycarbonate resin top plate has a cross hole, which is covered with a PMP resin plate through which images are taken from the sole of the foot.
We created an original aquarium using PMP, which facilitated evaluation under load. A 90-mm-high, 350-mm-long, and 155- mm-wide water tank made of 5-mm-thick PMP board was fixed in the cross hole cut out in the top plate, and water was stored in the tank to a height of 10 mm.12,14 Because the average foot axis angle during walking is approximately 7 degrees from the sagittal plane, the 2 evaluation tables were placed so that they were separated by 7 degrees from the sagittal plane.
Measuring the thickness of the heel fat pad using ultrasound
Measurements were taken by researchers with >8 years’ experience observing the heel fat pad and plantar aponeurosis. Measurements were performed using an ultrasonic diagnostic imaging device (ApplioαVerifia, Canon, JPN) with a 10-MHz high-frequency linear probe, with the screen upside down. As previously, we defined the area from the lower edge of the calcaneal eminence to the bottom of the fibrous septum as the macrochamber layer (MAC layer), and that from the bottom of the fibrous septum to the skin as the microchamber layer (MIC layer).4,12 -15 The MAC layer includes the plantar aponeurosis, MACs, and fibrous septum, and the MIC layer includes MICs and skin. The thickness of the plantar aponeurosis was measured 0.5 cm distal to the toe by connecting the calcaneal eminence and the second metatarsal bone with a line. 12 To measure the heel fat pad when no load was applied (0% load), a line perpendicular to the contact surface of the transducer was drawn from the most convex part of the calcaneal eminence. When measuring the heel fat pad under load (10% to 100% load), the whole layer is defined as the area from the most convex part of the calcaneal protuberance to the surface of the PMP resin plate, and the MAC layer is the same as when not under load. The MIC layer measured by the above method was measured from the bottom of the fibrous septum to the surface of the PMP resin plate.
Three images were taken at each load point, and the average value of the 3 images was used. Prior to measurement, we observed the heel fat pad using fresh frozen cadavers and measured ultrasonographic images of the same area to understand the structure before making measurements.
Evaluation of loading and unloading of the heel fat pad (MIC layer and MAC layer) and plantar aponeurosis
The measurement foot was unified to the right foot. The lower edge of the calcaneal prominence from the sole of the foot in the longitudinal direction was detected via the PMP resin plate and it was placed in the water tank so that the second metatarsal and the calcaneal protuberance were aligned with the straight line drawn on the PMP load measuring device. The right foot was then put in.
According to previous research, the load was evaluated from the state where the heel fat pad was not in contact with the PMP resin plate (unload) to the state where 100% of the heel’s own body weight was applied (end load), and the state where 100% of the heel fat pad was applied (end load) until the heel fat pad separates from the PMP resin plate (fully relaxed) was defined as the unloaded evaluation. 4
The amount of load on the right leg was adjusted based on the value on the left leg scale. The amount of load was measured every 20% of the actual weight, and the load from 0% to 100% was evaluated as a load (total of 5 points), and the load from 100% to 0% was evaluated as an unloaded weight (total of 5 points). A second examiner observed the load and instructed the participant to maintain that load for 5 seconds on reaching the measurement point. Three ultrasonographic images were taken at each measurement point, and the average value of the 3 images was used in this study.
Considering the possibility that the participants’ posture would collapse during the measurement, a wall was prepared to rest their hands. Additionally, to avoid leaning forward and causing the heel to float, a mark was placed at eye level when the participant was in a standing position, and the participant was asked not to take his or her eyes away from the mark during the measurement. Furthermore, we checked from the rear to make sure that the calcaneus did not invert or deviate when the load was applied, and to ensure that the axis of the load did not shift, the foot was placed in a straight line drawn on the polycarbonate resin top plate. Measurement was started with the toe in contact with the ground.
Based on the above, the items to be considered in this study were to evaluate the MIC layer, MAC layer, and plantar aponeurosis thickness under each loading and unloading condition. Following previous research, we calculated the amount of change in the thickness of the MIC layer and MAC layer (Amount of change [equation 1]) and the rate of change (Rate of change [equation 2]) from the values at unload and end load, the thickness change ratio (Deformation proportion × 100 [equation 3]) of the MIC layer and MAC layer for the entire heel fat pad was calculated. The calculation formula is shown in Table 2. 4
Table 2.
Calculation Formula for Evaluating the Function of the Heel Fat Pad.
| Amount of change (MIC layer) | = | 0% loading (MIC layer) | – | 100% loading (MIC layer) | |
| Or | |||||
| Amount of change (MAC layer) | = | 0% loading (MAC layer) | – | 100% loading (MAC layer) | (1) |
| Rate of change (MIC layer) | = | Amount of change (MIC layer) | × | 100 | |
| 0% loading (MIC layer) | |||||
| Or | |||||
| Rate of change (MAC layer) | = | Amount of change (MAC layer) | × | 100 | (2) |
| 0% loading (MAC layer) | |||||
| Deformation proportion × 100 (MIC layer) | = | Amount of change (MIC layer) | × | 100 | |
| Amount of change (MIC layer)+Amount of change (MAC layer) | |||||
| Or | |||||
| Deformation proportion × 100 (MAC layer) | = | Amount of change (MAC layer) | × | 100 | (3) |
| Amount of change (MIC layer)+Amount of change (MAC layer) | |||||
Abbreviations: MAC, macrochamber; MIC, microchamber.
Statistical Analysis
Statistical analysis was performed using SPSS software (SPSS Statistics 28, IBM, USA). Sample size estimation was performed for each item.
Prior to comparing the 3 points in the MAC layer and MIC layer, the Shapiro-Wilk test was performed, and because normality was assumed, a 2-way analysis of variance was performed. If the test result of the difference in measured values was significant, the Bonferroni method was performed as a post hoc test.
Prior to comparing the loading and unloading processes in the MAC layer and MIC layer in 10% increments, the Shapiro-Wilk test was performed, and because normality was assumed, a paired t test was performed. If the test result of the difference in measured values was significant, the Bonferroni method was performed as a post hoc test.
Before comparing the amount of thickness change and thickness change rate of the MAC layer and MIC layer during the loading and unloading processes, and the thickness change rate of the shallow layer and deep layer with respect to the entire heel fat pad, the Shapiro-Wilk test was performed. Because normality was assumed, a paired t test was used.
Pearson correlation coefficient was used to determine the relationship between the thickness of the MAC layer and the MIC layer, height, and weight, and the relationship between the rate of change in the shallow and deep heel fat pad thickness, height, and weight. Multiple regression analysis was performed using the stepwise method. The shallow and deep heel fat pad thicknesses and thickness change rates were used as dependent variables, and height and weight were used as independent variables. The correlation results were categorized as follows: 0.00 to 0.20 / –0.00 to 0.20 (poor correlation); 0.21 to 0.40 / –0.21 to 0.40 (fair correlation); 0.41 to 0.60 / –0.41 to 0.60 (moderate correlation); 0.61 to 0.80 / –0.61 to 0.80 (good correlation); 0.81 to 1.00 / –0.81 to 1.00 (very good correlation). The significance level was set at less than 5%.
Results
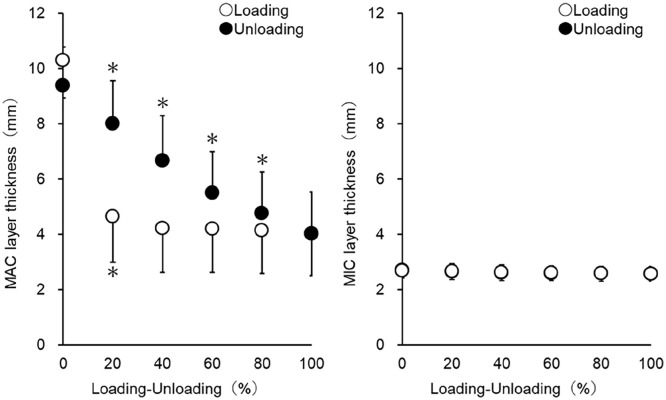
A 3-point comparison of the MAC layer and MIC layer revealed significant differences between initial contact and maximal load and between maximal load and unloading in the deep layer. However, no significant difference was observed between the 3 points in the MIC layer. Significant differences were observed in all points between the MIC and MAC layers (Figure 1).
Figure 1.
MIC and MAC layers thickness of the HFP during unload, end load, and fully relaxed state. (HFP, heel fat pad; MAC, macrochamber; MIC, microchamber.) *Significantly different from end load and unload, fully relaxed (P < .05). †Significant difference from MIC and MAC layers (P < .05).
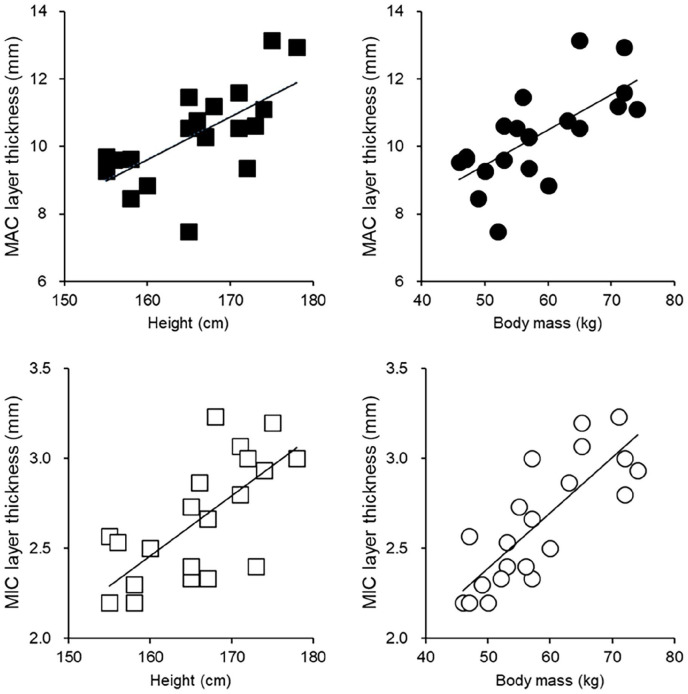
When comparing the loading and unloading processes in the MIC and MAC layers of the heel fat pad at 10% increments, significant changes were seen in the MAC layer up to 30% during the loading process, and significant changes were seen at all stages of the unloading process. However, no significant changes were observed in the loading and unloading processes in the MIC layer (Figure 2).
Figure 2.
Processes of the change in MIC and MAC layers through loading and unloading. (MAC, macrochamber; MIC, microchamber.) *Statistically significant difference from 20% before.
Regarding the amount of change in thickness of the MIC and MAC layers of the heel fat pad, the thickness change rate, and the ratio of thickness change of the MIC and MAC layers to the entire heel fat pad, there was a significant difference between the MIC and MAC layers during the loading and unloading processes (Table 3).
Table 3.
Microchamber and Macrochamber Layer Tissue Properties.
| Microchamber Layer, Mean (SD) |
Macrochamber Layer, Mean (SD) |
P | |||
|---|---|---|---|---|---|
| Loading cycle | |||||
| Amount of change, mm | 0.1 | (0.1) | 6.2 | (0.9) | .001 |
| Rate of change, % | 4.3 | (2.0) | 60.6 | (11.1) | .001 |
| Deformation proportion × 100 (%) | 1.8 | (0.8) | 98.2 | (0.8) | .001 |
| Unloading cycle | |||||
| Amount of change, mm | 0.1 | (0.1) | 5.2 | (0.8) | .001 |
| Rate of change, % | 4.1 | (2.0) | 56.6 | (11.5) | .001 |
| Deformation proportion × 100 (%) | 2.1 | (1.1) | 97.9 | (1.1) | .001 |
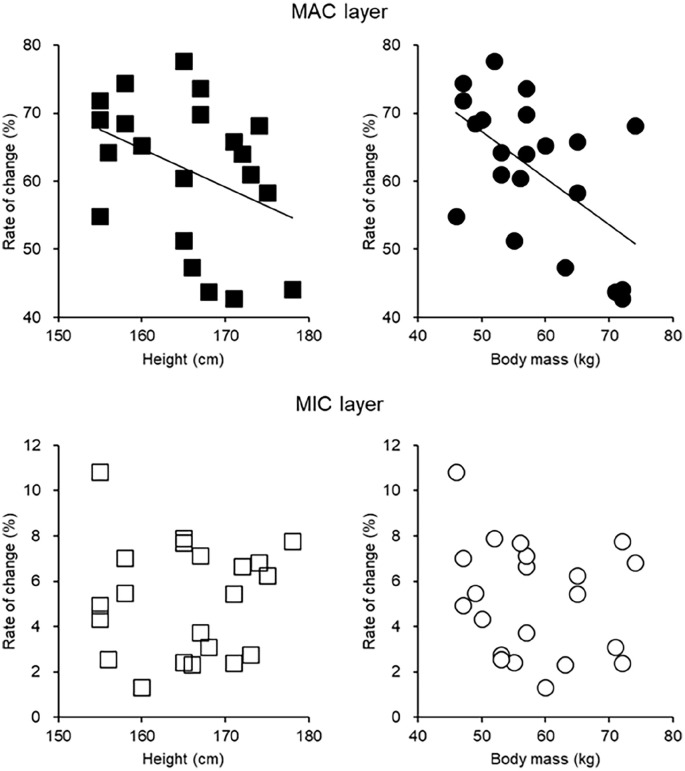
Regarding the relationship between the thickness of the MIC and MAC heel fat pads, height, and weight, there was a good positive correlation in the MIC layer for height (r = 0.711, P < .05) and weight (r = 0.805, P < .05). In the MAC layer, a good positive correlation was observed with height (r = 0.672, P < .05) and weight (r = 0.682, P < .05). Multiple regression analysis revealed a significant variable with body weight, which was a large factor (MIC layer: R2 = 0.648, P < .001, weight: β = 0.805; MAC layer: R2 = 0.465, P < .001, weight: β = 0.682) (Figure 3).
Figure 3.
Relationship between the MIC and MAC layers’ thickness during unloaded state and height and weight. (MAC, macrochamber; MIC, microchamber.)
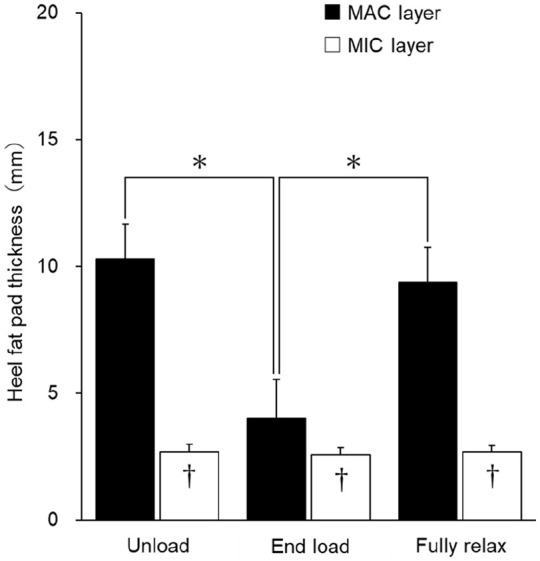
Regarding the relationship between the rate of change in thickness of the MIC and MAC layers of the heel fat pad and height and weight, in the MIC layer, for height (r = 0.024, P > .05) and weight (r = 0.198, P > .05), no significant correlation was found. In the MAC layer, a fair negative correlation was found for height (r = −0.383, P < .05) and a moderate negative correlation for weight (r = −0.571, P < .05; MAC layer: R2 = 0.327, P < .05; weight: β = −0.572) (Figure 4).
Figure 4.
Relationship between the change rate of MIC and MAC layer thickness during full loading and height and weight. (MAC, macrochamber; MIC, microchamber.)
Discussion
We used an evaluation instrument using a PMP resin plate to estimate the difference in movement between the MIC and MAC layers of the heel fat pad. During unloading, we found the change in the MAC layer relative to the entire thickness of the heel fat pad was approximately 98%, whereas the change in the MIC layer was around 2%, with the deep layer accounting for most of the change. There is evidence from anatomical findings that the superficial and deep layers of the heel fat pad have different tissue morphology, with the deep layer responsible for shock absorption and the superficial layer responsible for controlling excessive deep deformation.1,4,6,8,18 Previous studies that examined changes in the MIC and MAC layers when a simulated load or a 20-kg load was applied to human organisms reported that morphologic changes in the MAC layer was significant.3,4 This study was the first to include all body weight and evaluate changes in the MIC and MAC layers. As shown previously, the depth changed significantly even at full load, and the change increased with load. However, no change was observed in the MIC layer even when the load increased.
Regarding the relationship between the thickness of the MIC and MAC layers of the heel fat pad, height, and weight, when height and weight are high, the thickness of the MIC and MAC layers increases morphologically, but the rate of change in the thickness of the MIC layer remains the same. This study revealed that the rate of thickness change in MAC layers is low. Although it is difficult to say from this study whether this change is an adaptation to overload or a change due to a decline in functional characteristics, it is generally assumed that the thick heel fat pad has superior functional characteristics. The results of this study suggest that this cannot be said to be the case.
The heel fat pad is said to undergo degenerative changes because of aging and lesions because of diseases such as diabetes.3,11,13 In fact, it has been reported that the heel fat pad becomes thinner with age, with degeneration and destruction of elastic fibers as well as loss and outflow of healthy adipose tissue. 9 Heel pain is particularly common in people between the ages of 40 and 60, and thinning of the MAC layer of the heel fat pad is seen after this age. 10 Since, expectedly, changes in the shape of the MAC layer will lead to a decrease in shock absorption capacity and an increase in compressive stress, leading to heel pain, rather than comprehensively considering the 2 layers as the heel fat pad, it was important to consider the 2 layers separately. 12 Additionally, in patients with heel pain, the thinning of the heel fat pad and fibrosis of the septum described above occur; hence, it is expected that the maximum deformation (=maximum load point) will be reached at an early stage of loading. Because repeated heel contact in a thinned state may increase the risk of heel pain induction, it is extremely important to consider changes in load. We also confirmed that the internal structure of the heel fat pad during loading can be evaluated clearly and in detail by using a PMP resin plate.
Our previous study11,12,14 demonstrated significant morphologic changes in the MAC layer of the heel fat pad under simulated loads. The current study builds on that foundation by including full body weight loading scenarios, providing a more comprehensive understanding of MIC and MAC layer responses to varying loads. By extending our investigation to encompass real-life loading conditions, we underscore the practical implications of our findings in biomechanical research.
By further applying this, it can be derived from various motion measurements. Understanding the biomechanical behavior of daily life activities such as walking and running is extremely important for understanding various future movements. Although this study was conducted on healthy participants, we used the values obtained here as a standard to measure the changes in weight and unloading of the heel fat pad that has actually degenerated because of degenerative changes or lesions. It is thought that this study may lead to elucidation of the relationship between heel fat pads and the mechanism behind heel pain. Understanding the differential responses of the MIC and MAC layers to loading can aid in early diagnosis and targeted interventions. Physicians may be able to apply this knowledge to develop treatment plans that mitigate the effects of load-induced heel pain and optimize shock absorption.
Limitations
Because the load unloading operation was a continuous operation, it was not possible to control the adjustment of the load amount. Furthermore, because foot pressure was not measured, there is no doubt that the entire load was applied to the measured foot; however, it was difficult to determine whether it was applied to the heel. The sample size was small, and in order to calculate more reliable values, it is necessary to increase the sample size. Because the loading speed was fixed uniformly and was slower than the original loading speed during walking, it cannot be denied that the change was different from the load change during walking. Because water was used instead of ultrasound gel, the effect of buoyancy was not taken into account.
Conclusion
This study indicates that the functions of the microchamber and macrochamber layers of the heel fat pad may be different. As height and weight increase, the thickness of the 2 layers may have increased, and the rate of change in the thickness of the macrochamber layer is thought to have decreased, and although the thickness increases as the load increases, it was shown that the elasticity may decrease.
Supplemental Material
Supplemental material, sj-pdf-1-fao-10.1177_24730114241278927 for Effect of Height and Weight on Heel Fat Pad Movements Between Microchamber and Macrochamber Layers in Loading and Unloading by Toshihiro Maemichi, Masatomo Matsumoto, Toshiharu Tsutsui, Shota Ichikawa, Takumi Okunuki, Hirofumi Tanaka and Tsukasa Kumai in Foot & Ankle Orthopaedics
Footnotes
Ethical Approval: This study was approved by the ethics committee (approval number: 2020-228) and conducted according to the principles of the Declaration of Helsinki. Written informed consent was obtained from all participants and their guardians.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Disclosure forms for all authors are available online.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Public Interest Incorporated Foundation, Yamaha Motor Foundation for Sports.
ORCID iDs: Toshihiro Maemichi, PhD, JSPO-AT,  https://orcid.org/0000-0001-8683-2059
https://orcid.org/0000-0001-8683-2059
Tsukasa Kumai, PhD, MD,  https://orcid.org/0000-0003-3738-9171
https://orcid.org/0000-0003-3738-9171
References
- 1. Buschmann WR, Jahss MH, Kummer F, Desai P, Gee RO, Ricci JL. Histology and histomorphometric analysis of the normal and atrophic heel fat pad. Foot Ankle Int. 1995;16(5):254-258. [DOI] [PubMed] [Google Scholar]
- 2. De Clercq D, Aerts P, Kunnen M. The mechanical characteristics of the human heel pad during foot strike in running: an in vivo cineradiographic study. J Biomech. 1994;27(10):1213-1222. [DOI] [PubMed] [Google Scholar]
- 3. Hsu C-C, Tsai W-C, Hsiao T-Y, et al. Diabetic effects on microchambers and macrochambers tissue properties in human heel pads. Clin Biomech (Bristol, Avon). 2009;24(8):682-686. [DOI] [PubMed] [Google Scholar]
- 4. Hsu C-C, Tsai W-C, Wang C-L, Pao S-H, Shau Y-W, Chuan Y-S. Microchambers and macrochambers in heel pads: are they functionally different? J Appl Physiol (1985). 2007;102(6):2227-2231. [DOI] [PubMed] [Google Scholar]
- 5. Hsu T-C, Lee Y-S, Shau Y-W. Biomechanics of the heel pad for type 2 diabetic patients. Clin Biomech (Bristol, Avon). 2002;17(4):291-296. [DOI] [PubMed] [Google Scholar]
- 6. Jørgensen U, Bojsen-Møller F. Shock absorbency of factors in the shoe/heel interaction—with special focus on role of the heel pad. Foot Ankle. 1989;9(6):294-299. [DOI] [PubMed] [Google Scholar]
- 7. Ker RF, Bennett MB, Alexander RM, Kester RC. Foot strike and the properties of the human heel pad. Proc Inst Mech Eng H. 1989;203(4):191-196. [DOI] [PubMed] [Google Scholar]
- 8. Kimani JK. The structural and functional organization of the connective tissue in the human foot with reference to the histomorphology of the elastic fibre system. Acta Morphol Neerl Scand. 1984;22(4):313-323. [PubMed] [Google Scholar]
- 9. Kuhns JG. Changes in elastic adipose tissue. J Bone Joint Surg Am. 1949;31A(3):541-547. [PubMed] [Google Scholar]
- 10. Lapidus PW, Guidotti FP. Painful heel: report of 323 patients with 364 painful heels. Clin Orthop Relat Res. 1965;39:178-186. [PubMed] [Google Scholar]
- 11. Maemichi T, Matsumoto M, Okunuki T, Kumai T. Changes in functional characteristics of heel fat pad with age. Clin Biomech (Bristol, Avon). 2024;118:106294. [DOI] [PubMed] [Google Scholar]
- 12. Maemichi T, Matsumoto M, Tsutsui T, et al. Functional morphologic changes of the heel fat pad and plantar fascia in patients with heel pain during weightbearing and nonweightbearing. Foot Ankle Orthop. 2024;9(2):1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Maemichi T, Tsutsui T, Matsumoto M, Iizuka S, Torii S, Kumai T. The relationship of heel fat pad thickness with age and physiques in Japanese. Clin Biomech (Bristol, Avon). 2020;80:105110. [DOI] [PubMed] [Google Scholar]
- 14. Matsumoto M, Maemichi T, Wada M, et al. Ultrasonic evaluation of the heel fat pad under weight-bearing conditions using a polymethylpentene resin plate: part 1. Ultrasound Med Biol. 2022;48(2):358-372. [DOI] [PubMed] [Google Scholar]
- 15. Matsumoto M, Maemichi T, Wada M, et al. Ultrasonic evaluation of the heel fat pad under loading conditions using a polymethylpentene resin plate: part 2. Reliability and agreement study. Ultrasound Med Biol. 2023;49(2):460-472. [DOI] [PubMed] [Google Scholar]
- 16. Perhamre S, Lundin F, Klässbo M, Norlin R. A heel cup improves the function of the heel pad in Sever’s injury: effects on heel pad thickness, peak pressure and pain. Scand J Med Sci Sports. 2012;22(4):516-522. [DOI] [PubMed] [Google Scholar]
- 17. Prichasuk S. The heel pad in plantar heel pain. J Bone Joint Surg Br. 1994;76(1):140-142. [PubMed] [Google Scholar]
- 18. Wearing SC, Smeathers JE, Yates B, Urry SR, Dubois P. Bulk compressive properties of the heel fat pad during walking: a pilot investigation in plantar heel pain. Clin Biomech (Bristol, Avon). 2009;24(4):397-402. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-fao-10.1177_24730114241278927 for Effect of Height and Weight on Heel Fat Pad Movements Between Microchamber and Macrochamber Layers in Loading and Unloading by Toshihiro Maemichi, Masatomo Matsumoto, Toshiharu Tsutsui, Shota Ichikawa, Takumi Okunuki, Hirofumi Tanaka and Tsukasa Kumai in Foot & Ankle Orthopaedics