Abstract
Background
Stroke frequently results in upper limb motor dysfunction, with traditional therapies often failing to yield sufficient improvements. Emerging technologies such as virtual reality (VR) and noninvasive brain stimulation (NIBS) present promising new rehabilitation possibilities.
Objectives
This study systematically reviews and meta-analyses the effectiveness of VR and NIBS in improving upper limb motor function in stroke patients.
Methods
Registered with PROSPERO (CRD42023494220) and adhering to the PRISMA guidelines, this study conducted a thorough search of databases including PubMed, MEDLINE, PEDro, REHABDATA, EMBASE, Web of Science, Cochrane, CNKI, Wanfang, and VIP from 2000 to December 1, 2023, to identify relevant studies. The inclusion criterion was stroke patients receiving combined VR and NIBS treatment, while exclusion criteria were studies with incomplete articles and data. The risk of bias was assessed using the Cochrane Collaboration tool. Statistical analysis was performed using Stata SE 15.0, employing either a fixed-effects model or a random-effects model based on the level of heterogeneity.
Results
A total of 11 studies involving 493 participants were included, showing a significant improvement in Fugl-Meyer Assessment Upper Extremity (FMA-UE) scores in the combined treatment group compared to the control group (SMD = 0.85, 95% CI [0.40, 1.31], p = 0.017). The Modified Ashworth Scale (MAS) scores significantly decreased (SMD = − 0.51, 95% CI [− 0.83, − 0.20], p = 0.032), the Modified Barthel Index (MBI) scores significantly increased (SMD = 0.97, 95% CI [0.76, 1.17], p = 0.004), and the Wolf Motor Function Test (WMFT) scores also significantly increased (SMD = 0.36, 95% CI [0.08, 0.64], p = 0.021). Subgroup analysis indicated that the duration of treatment influenced the outcomes in daily living activities.
Conclusions
The combination of VR and NIBS demonstrates significant improvements in upper limb motor function in stroke patients. The duration of treatment plays a critical role in influencing the outcomes, particularly in activities of daily living. This systematic review has limitations, including language bias, unclear randomization descriptions, potential study omissions, and insufficient follow-up periods. Future studies should focus on exploring long-term effects and optimizing treatment duration to maximize the benefits of combined VR and NIBS therapy.
Keywords: Stroke rehabilitation, Virtual reality, Noninvasive brain stimulation, Upper limb motor function, Systematic review, Meta-analysis
Introduction
Motor dysfunction is a common post-stroke complication with recovery of the affected upper limb typically being more limited than that of the lower limb due to its inherent flexibility [1]. Approximately 50–60% of stroke patients experience residual upper limb impairment after traditional physical therapy, which significantly impacts their daily life [2]. Since hand function is closely related to activities such as using a mobile phone, eating, and writing, its rehabilitation is crucial for overall well-being [3]. The motor relearning program after stroke is affected by various factors, including training intensity, task specificity, motivation, and feedback [4]. However, traditional rehabilitation approaches that focus primarily on repetition and intensity may not optimally restore neural plasticity and address the diverse needs of stroke patients [5].
Emerging technologies have shown promise in overcoming these limitations and enhancing physical function recovery. Among these, noninvasive brain stimulation (NIBS) has proven effective in enhancing neuroplasticity and facilitating stroke recovery [6]. Techniques like transcranial direct current stimulation (tDCS) and transcranial magnetic stimulation (TMS) use electrical and magnetic energy to modulate cortical excitability noninvasively, inducing sustained neuroplasticity changes [7]. The application of repetitive transcranial magnetic stimulation (rTMS) triggers neuronal growth in the brain, leading to the initiation of novel action potentials [8]. Studies have demonstrated the benefits of rTMS for upper limb rehabilitation in stroke patients across different stages of recovery [9], while tDCS has been shown to improve upper limb motor function in chronic stroke patients [10].
Similarly, virtual reality (VR) is increasingly effective in motor function recovery and neuroexcitation. VR training robustly engages key brain regions, including the prefrontal lobe and motor networks, driving significant improvements in motor function and spatial awareness [11].VR can be immersive or non-immersive, depending on the user’s isolation from the physical environment during interaction [12]. Recent studies indicate that VR is beneficial for post-stroke rehabilitation, with positive effects comparable to traditional treatments [13, 14]. Karamians et al. highlighted VR-based rehabilitation as potentially more effective than traditional training methods for upper limb recovery in stroke patients [15].
When combined, noninvasive brain stimulation [16] and virtual reality [17] can synergistically provide personalized training programs that encourage upper limb movement post-stroke. This integrated approach offers a more engaging and personalized rehabilitation experience, potentially overcoming the limitations of conventional therapeutic methods. Previous studies have confirmed the effectiveness of combined VR and NIBS therapy for upper limb rehabilitation in stroke patients [18–20]. Moreover, a meta-analysis showed that adding tDCS to VR-mediated movement observation and performance tasks enhances movement improvement after stroke [20].
Considering the limitations of previous meta-analysis, which included a limited number of studies and lacked quality assessment, this study aimed to analyze the current scientific evidence on combined VR and NIBS therapy for restoring upper limb motor function post-stroke. By expanding the range of databases and incorporating quality assessments, this research aims to provide a more comprehensive and reliable evaluation of the combined therapy’s efficacy.
Methods
Literature review design
This study is registered with PROSPERO (CRD42023494220) and was conducted in accordance with the 2020 version of the PRISMA statement.
Search strategy and data sources
A comprehensive systematic search was conducted from 2000 to December 1, 2023, in the following databases: PubMed, MEDLINE, PEDro, REHABDATA, EMBASE, Web of Science, CNKI, Wanfang, and VIP. The search strategy included terms related to virtual reality, stroke, and non-invasive brain stimulation. Specifically, we used combinations of medical subject headings (MeSH) terms and keywords such as “virtual reality,” “stroke,” “cerebrovascular accident,” “non-invasive brain stimulation,” “transcranial direct current stimulation,” and “transcranial magnetic stimulation.” The detailed search strategy and full list of search terms are provided in Table 1. Searches were not restricted by language, publication date, or publication status. The search will be updated before the final analysis to ensure inclusion of the most recent studies. We used the PICOS principle proposed by Cochrane: population (stroke); intervention (VR combined with NIBS); comparison (combined or conventional treatment); outcome [for the intervention and control groups, the study reported values for the change in upper limb functional score before and after treatment, including Fugl-Meyer Assessment Upper Extremity (FMA-UE), Modified Barthel Index (MBI), Modified Ashworth Scale (MAS), and the Wolf Motor Function Test (WFMT)]; and study design (RCT or non-RCT, irrespective of publication date, status, or language).
Table 1.
PubMed search strategy
| Step | Retrievable |
|---|---|
| #1 | “virtual reality”[MeSH Terms] OR (“virtual”[All Fields] AND “reality”[All Fields]) OR “virtual reality”[All Fields] OR (“virtual reality”[MeSH Terms] OR (“virtual”[All Fields] AND “reality”[All Fields]) OR “virtual reality”[All Fields] OR (“reality”[All Fields] AND “virtual”[All Fields]) OR “reality virtual”[All Fields]) OR (“virtual reality”[MeSH Terms] OR (“virtual”[All Fields] AND “reality”[All Fields]) OR “virtual reality”[All Fields] OR (“virtual”[All Fields] AND “reality”[All Fields] AND “educational”[All Fields]) OR “virtual reality educational”[All Fields]) OR (“virtual reality”[MeSH Terms] OR (“virtual”[All Fields] AND “reality”[All Fields]) OR “virtual reality”[All Fields] OR (“educational”[All Fields] AND “virtual”[All Fields] AND “realities”[All Fields]) OR “educational virtual realities”[All Fields]) OR (“virtual reality”[MeSH Terms] OR (“virtual”[All Fields] AND “reality”[All Fields]) OR “virtual reality”[All Fields] OR (“educational”[All Fields] AND “virtual”[All Fields] AND “reality”[All Fields]) OR “educational virtual reality”[All Fields]) OR (“virtual reality”[MeSH Terms] OR (“virtual”[All Fields] AND “reality”[All Fields]) OR “virtual reality”[All Fields] OR (“reality”[All Fields] AND “educational”[All Fields] AND “virtual”[All Fields])) OR (“virtual reality”[MeSH Terms] OR (“virtual”[All Fields] AND “reality”[All Fields]) OR “virtual reality”[All Fields] OR (“virtual”[All Fields] AND “realities”[All Fields] AND “educational”[All Fields])) OR (“virtual reality”[MeSH Terms] OR (“virtual”[All Fields] AND “reality”[All Fields]) OR “virtual reality”[All Fields] OR (“virtual”[All Fields] AND “reality”[All Fields] AND “instructional”[All Fields]) OR “virtual reality instructional”[All Fields]) OR (“virtual reality”[MeSH Terms] OR (“virtual”[All Fields] AND “reality”[All Fields]) OR “virtual reality”[All Fields] OR (“instructional”[All Fields] AND “virtual”[All Fields] AND “realities”[All Fields])) OR (“virtual reality”[MeSH Terms] OR (“virtual”[All Fields] AND “reality”[All Fields]) OR “virtual reality”[All Fields] OR (“instructional”[All Fields] AND “virtual”[All Fields] AND “reality”[All Fields])) OR (“virtual reality”[MeSH Terms] OR (“virtual”[All Fields] AND “reality”[All Fields]) OR “virtual reality”[All Fields] OR (“realities”[All Fields] AND “instructional”[All Fields] AND “virtual”[All Fields])) OR (“virtual reality”[MeSH Terms] OR (“virtual”[All Fields] AND “reality”[All Fields]) OR “virtual reality”[All Fields] OR (“reality”[All Fields] AND “instructional”[All Fields] AND “virtual”[All Fields])) OR (“virtual reality”[MeSH Terms] OR (“virtual”[All Fields] AND “reality”[All Fields]) OR “virtual reality”[All Fields] OR (“virtual”[All Fields] AND “realities”[All Fields] AND “instructional”[All Fields])) |
| #2 | “stroke”[MeSH Terms] OR “stroke”[All Fields] OR “strokes”[All Fields] OR “stroke s”[All Fields] OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR “strokes”[All Fields] OR “stroke s”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“cerebrovascular”[All Fields] AND “accident”[All Fields]) OR “cerebrovascular accident”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“cerebrovascular”[All Fields] AND “accidents”[All Fields]) OR “cerebrovascular accidents”[All Fields]) OR ((“stroke”[MeSH Terms] OR “stroke”[All Fields] OR “cva”[All Fields]) AND (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“cerebrovascular”[All Fields] AND “accident”[All Fields]) OR “cerebrovascular accident”[All Fields])) OR (“CVAs”[All Fields] AND (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“cerebrovascular”[All Fields] AND “accident”[All Fields]) OR “cerebrovascular accident”[All Fields])) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“cerebrovascular”[All Fields] AND “apoplexy”[All Fields]) OR “cerebrovascular apoplexy”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“apoplexy”[All Fields] AND “cerebrovascular”[All Fields]) OR “apoplexy cerebrovascular”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“vascular”[All Fields] AND “accident”[All Fields] AND “brain”[All Fields]) OR “vascular accident brain”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“brain”[All Fields] AND “vascular”[All Fields] AND “accident”[All Fields]) OR “brain vascular accident”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“brain”[All Fields] AND “vascular”[All Fields] AND “accidents”[All Fields]) OR “brain vascular accidents”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“vascular”[All Fields] AND “accidents”[All Fields] AND “brain”[All Fields])) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“cerebrovascular”[All Fields] AND “stroke”[All Fields]) OR “cerebrovascular stroke”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“cerebrovascular”[All Fields] AND “strokes”[All Fields]) OR “cerebrovascular strokes”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“stroke”[All Fields] AND “cerebrovascular”[All Fields]) OR “stroke cerebrovascular”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“strokes”[All Fields] AND “cerebrovascular”[All Fields]) OR “strokes cerebrovascular”[All Fields]) OR (“apoplexies”[All Fields] OR “stroke”[MeSH Terms] OR “stroke”[All Fields] OR “apoplexy”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“cerebral”[All Fields] AND “stroke”[All Fields]) OR “cerebral stroke”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“cerebral”[All Fields] AND “strokes”[All Fields]) OR “cerebral strokes”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“stroke”[All Fields] AND “cerebral”[All Fields]) OR “stroke cerebral”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“strokes”[All Fields] AND “cerebral”[All Fields]) OR “strokes cerebral”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“stroke”[All Fields] AND “acute”[All Fields]) OR “stroke acute”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“acute”[All Fields] AND “stroke”[All Fields]) OR “acute stroke”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“acute”[All Fields] AND “strokes”[All Fields]) OR “acute strokes”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“strokes”[All Fields] AND “acute”[All Fields]) OR “strokes acute”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“cerebrovascular”[All Fields] AND “accident”[All Fields] AND “acute”[All Fields]) OR “cerebrovascular accident acute”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“acute”[All Fields] AND “cerebrovascular”[All Fields] AND “accident”[All Fields]) OR “acute cerebrovascular accident”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“acute”[All Fields] AND “cerebrovascular”[All Fields] AND “accidents”[All Fields]) OR “acute cerebrovascular accidents”[All Fields]) OR (“stroke”[MeSH Terms] OR “stroke”[All Fields] OR (“cerebrovascular”[All Fields] AND “accidents”[All Fields] AND “acute”[All Fields]) OR “cerebrovascular accidents acute”[All Fields]) |
| #3 | “NIBS”[All Fields] OR (“non-invasive”[All Fields] AND (“brain stimul”[Journal] OR (“brain”[All Fields] AND “stimulation”[All Fields]) OR “brain stimulation”[All Fields])) OR (“transcranial direct current stimulation”[MeSH Terms] OR (“transcranial”[All Fields] AND “direct”[All Fields] AND “current”[All Fields] AND “stimulation”[All Fields]) OR “transcranial direct current stimulation”[All Fields] OR “tdcs”[All Fields]) OR (“transcranial magnetic stimulation”[MeSH Terms] OR (“transcranial”[All Fields] AND “magnetic”[All Fields] AND “stimulation”[All Fields]) OR “transcranial magnetic stimulation”[All Fields] OR “rtms”[All Fields]) OR “iTBS”[All Fields] |
| #4 | #1 AND #2 AND #3 |
Inclusion criteria
Two authors (Nuo Zhang and Hujun Wang) independently screened the titles and abstracts of all the studies to determine eligibility. Any disagreements were resolved by consulting a third author (Hanming Wang). The inclusion criteria were as follows: (1) participants had a stroke; (2) received VR combined with NIBS treatment; (3) aimed to evaluate the effect of combined treatment on upper limb function; (4) included FMA-UE as an indicator; (5) RCT or non-RCT studies. The exclusion criteria were as follows: (1) duplicated studies; (2) studies not available in full text; (3) studies with incomplete data; (4) studies without quantitative data.
Risk of bias and quality assessment
Two authors (Nuo Zhang and Hujun Wang) independently assessed the risk of bias in each included study using the Cochrane Collaboration tool. The quality was evaluated based on six aspects: random sequence generation (selection bias), allocation concealment (selection bias), blinding (performance bias and detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other potential sources of bias. The overall risk of bias across studies was assessed, and any discrepancies were discussed with a third author to reach a consensus. The methodological quality of the randomized controlled trials was evaluated using the Physiotherapy Evidence Database Research Organization (PEDro) scale, which contains 11 items (yes or no) with a total score of ten. One item related to external validity was not used in calculating the PEDro score. Studies with PEDro scores between 6 and 10 points were considered “high” quality, those with scores of 4–5 points were considered “moderate” quality, and those with scores of 0–3 points were considered “low” quality [21]. The two authors independently evaluated the risk of bias and methodological quality of each article by discussing the results with the third author to reach a consensus when the evaluations differed.
Data extraction and statistical analysis
Two authors independently extracted data from the included studies using a standardized data extraction form, and discrepancies were resolved through discussion to reach a consensus. Extracted data included: (1) basic information of the study (title, author, year of publication, country, study information); (2) PICO information (demographic characteristics, intervention implementation methods, outcome indicators); (3) methodology section (study design, intervention time, stimulation site, parameters) and other information (funding source, potential conflicts of interest, conclusions). Data were managed using Excel, and statistical analyses were performed using Stata SE 15.0 (Stata Corp LLC, College Station, TX). The fixed-effects model was used to calculate the overall effect size and 95% confidence interval (CI). The random-effects model was used for significant heterogeneity (p < 0.05, I2 ≥ 50%). A p value < 0.05 was used to indicate a significant difference between the experimental and control groups in the meta-analysis. To analyze the potential factors contributing to heterogeneity among studies, we used meta-regression analysis with robust variance estimation. By adding covariates to the regression model, we analyzed whether different covariates affected the effect of combined therapy. Subgroup analyses were performed based on the duration of combined therapy, dividing studies into < 4 weeks and > 4 weeks. Sensitivity analysis was carried out using the one-by-one exclusion method. Egger’s test was used to assess publication bias, with p < 0.05 indicating the presence of publication bias. Missing data were addressed by contacting study authors where necessary.
Results
Study characteristics
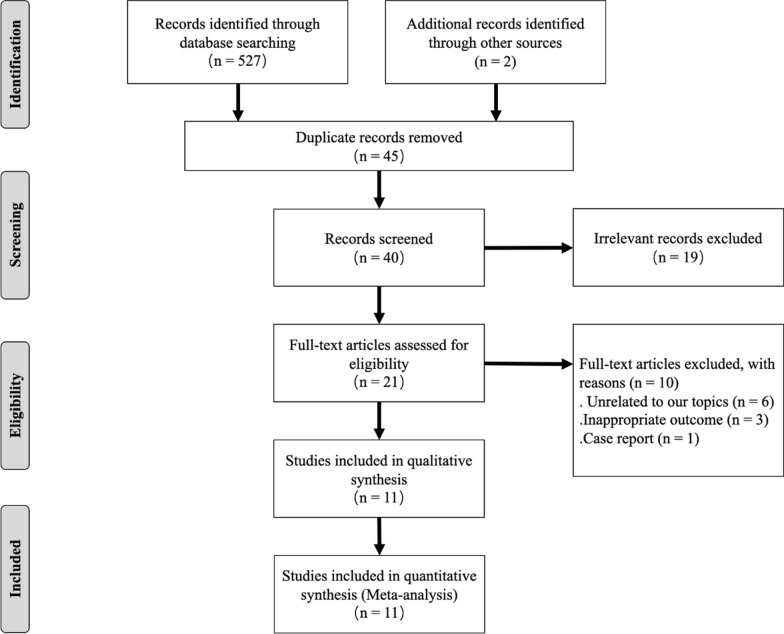
A total of 527 articles were retrieved from the database search, 21 of which were retained after removing duplicates and irrelevant records. During the detailed full-text screening, 10 studies were excluded for not meeting the inclusion criteria. Overall, the final quantitative analysis included 11 studies with a total of 493 participants. The detailed search and selection process are presented in the flow diagram (Fig. 1). The included studies were conducted between 2014 and 2022. In these studies, the mean age of the patients in the combined treatment group ranged from 43.6 to 73.4 years, and the average time from stroke onset ranged from 10 days to 4 years. The treatment frequency varied from 3 to 6 times per week, with one study not reporting the treatment duration. Positive treatment effects were reported in 8 studies, 2 studies showed unclear treatment effects, and 1 study showed no effects. The studies employed different combinations of NIBS and VR: 2 used rTMS combined with VR, 8 used tDCS combined with VR, and 1 used iTBS combined with VR. The characteristics of all included studies are summarized in Table 2.
Fig. 1.
Flow diagram of the literature screening process
Table 2.
Details of all the studies
| Study | Nation | Type of study | Sample size (intervention/control) | Age | Duration of stroke | NIBS type/Location/Parameter | Groups | Intervention | Outcome measures |
|---|---|---|---|---|---|---|---|---|---|
| Zheng et al., 2015 | China | Double-blind RCT | 55/53 | 65.4 ± 13.5 years | 19.3 ± 7.3 Day | low-frequency rTMS, unaffected M1, 1HZ, 1800 pulses, 90% rMT |
Intervention group: real rTMS + VR control group: sham rTMS + VR |
All participants received 1 h of PT, 30 min of OT, and 30 min of VR training; exercise intensity in both groups is 30 min/session, 6 times/week for 4 weeks |
primary outcome: 1. FMA-UE 2. WMFT secondary outcome: 3. MBI 4. SF-36 |
| Lee and Chun, 2014 | Korea | RCT | 20/19 | 63.1 ± 10.3 years | 17.8 ± 7.3 Day | tDCS, cathode: unaffected M1, 2 mA |
Intervention group: tDCS + VR control group1: tDCS + OT control group2: VR |
All groups received same intensity of practices (30 min/d, 5 times/week for 3 weeks) |
1. MAS 2. MMT 3. MFT 4. FMA-UE 5. MBI |
| Viana et al., 2014 | Brazil | Double-blind RCT | 10/10 | 56.0 ± 10.2 years | 31.9 ± 18.2 Month | tDCS, anode: affected M1, 2 mA |
Intervention group: real tDCS + VR control group: sham tDCS + VR |
Both groups received 60 min VR (4 games, 15 min each), 3 times/week, 5 weeks in total |
primary outcome: 1. FMA-UE 2. WMFT secondary outcome: 3. MAS 4. Grip strength 5. SSQOL |
| Llorens et al., 2017 | Spain | n-RCT | 7 | 55.9 ± 8.1 years | 365.1 ± 383.9 Day | tDCS, anode: unaffected M1, 2 mA | Intervention group: tDCS + VR | Participants received 75 sessions (25 times PT + 25 times tDCS and VE + 25 times PT) in 3 phases. 3–5 times/week for all study phases |
1. FMA-UE 2. WMFT |
| Chen et al., 2021 | Taiwan, China | Double-blind RCT | 12/11 | 54.36 ± 10.56 years | 5.01 ± 4.39 Month | iTBS, affected hand M1, 50HZ, 1200 pulses, 80%rMT |
Intervention group: real iTBS + VR control group: sham iTBS + VR |
All participants received 60 min VR, 20 min iTBS, 5 times/week, a total of 3 weeks |
primary outcome: 1. FMA-UE 2. MAS secondary outcome: 3. ARAT 4. NHPT 5. BBT 6. MAL 7. SIS |
| Yao et al., 2020 | China | RCT | 20/20 | 63.0 ± 7.5 years | 60.5 ± 35.5 Day | tDCS, cathode: unaffected M1, 2 mA |
Intervention group: real tDCS + VR control group: sham tDCS + VR |
All patients received tDCS and VR (20 min/d and 5 sessions/week for 2 weeks), and conventional OT and PT |
1. FMA-UE 2. ARAT 3. MBI |
| Llorens et al., 2021 | Spain | RCT | 14/15 | 54.9 ± 9.4 years | 9.0 ± 2.3 Month | tDCS, anode: unaffected M1(C3 or C4), 2 mA |
Intervention group: tDCS + VR control group: conventional PT |
Intervention group received 30 min intervention and 30 min PT sessions; control group received 60 min PT, 3–5 times a week, 25 sessions in total |
1. FMA-UE 2. WMFT 3. NSA |
| Zhu et al., 2022 | China | n-RCT | 35/35 | 66.97 ± 2.09 years | 4.69 ± 0.64 Month | rTMS, 5HZ |
Intervention group: conventional PT + VR + rTMS control group: conventional PT + VR |
All participants received VR training 20 min/d, 5 times/week for 8 weeks; intervention group received rTMS 20 min/d, 6 times/week, 8 weeks in total |
1. FMA-UE 2. MBI 3. MMSE 4. MoCA |
| Zhao et al., 2021 | China | n-RCT | 39/39 | 60.40 ± 7.25 years | 38.30 ± 8.94 Day | tDCS, M1, 1.4 mA |
Intervention group: conventional PT + tDCS + VR control group: conventional PT |
All participants received conventional PT; intervention group received tDCS 25 min and VR training 30 min, 5 times/wk, 4 weeks in total |
1. FMA-UE 2. MAS 3. MBI 4. SEP |
| Liu et al., 2020 | China | RCT | 15/15 | 62.86 ± 9.05 years | 9.33 ± 2.15 Month | tDCS, anode: unaffected M1(C3 or C4), 2 mA |
Intervention group: tDCS + VR control group1: tDCS control group2: VR |
Same intensity of practice in all groups (20 min/d, 5 times/wk for 4 wk) |
1. FMA-UE 2. WMFT 3. MBI |
| Cui et al., 2017 | China | n-RCT | 21/21 | 53.38 ± 9.74 years | 55.71 ± 32.49 Day | rTMS, unaffected M1, 1HZ, 800 pulse, 80% rMT |
Intervention group: rTMS + VR control group: VR |
All participants received conventional PT, VR training 20 min/d 5 times/wk, a total of 4 weeks, intervention group received rTMS with same intensity additionally |
1. FMA-UE 2. MBI 3. STEF 4. Brunnstrom |
PEDro = Physiotherapy Evidence Database Research Organization; RCT = randomized controlled trial; FMA-UE = Fugl-Meyer Assessment Upper Extremity; WMFT-FAS = Wolf Motor Function Test Functional Assessment Scale; MBI = Modified Barthel Index; SF-36 = 36-item Short Form Health Survey; MAS = Modified Ashworth Scale; MMT = manual muscle test; MFT = Manual Function Test; SSQoL = Stroke Specific Quality of Life; ARAT = Action Research Arm Test, NHPT = Nine Hole Peg Test, BBT = Box and Block Test, MAL = Motor Activity Log, SIS = Stroke Impact Scale, SEP = Somatosensor Evoked Potential, NSA = Nottingham Sensory Assessment, MMSE = Mini-Mental State Examination, MoCA = Montreal Cognitive Assessment, STEF = Simple Test for Evaluating Hand Function, tDCS = transcranial direct current stimulation; rTMS = repetitive transcranial magnetic stimulation; UE = upper extremity; VR = virtual reality; PT = physical therapy; OT = occupational therapy
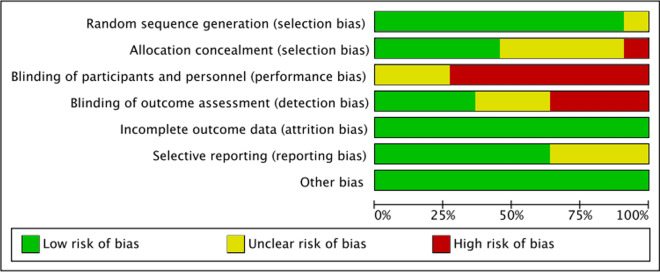
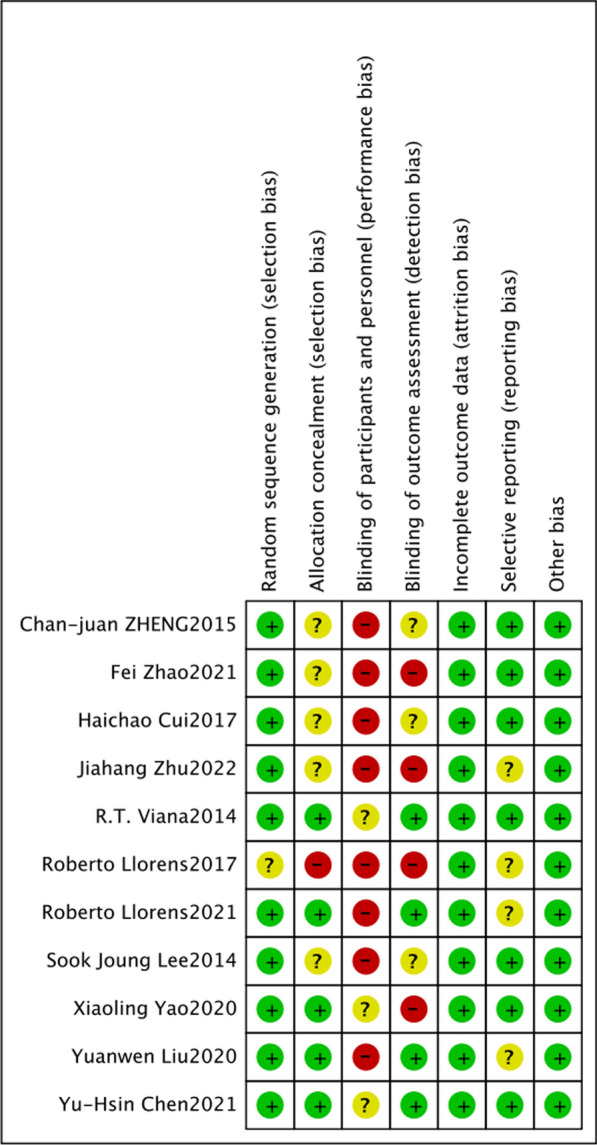
Risk of bias and study quality
Figure 2 presents the overall risk of bias assessment. One study did not report the method of generating the random sequence, one study did not implement allocation concealment, and five studies did not report on allocation concealment. Eight studies did not involve blinding of participants or personnel, and three studies did not report on blinding. Four studies did not use blinding for outcome assessment, and three studies did not report on this aspect. Four studies did not report on selective reporting. No studies had attrition bias or other biases. It is inferred that the main risk of bias in the selected articles was due to the difficulty of blinding subjects and therapists.
Fig. 2.
Risk of bias graph
According to the PEDro scores of all 11 articles in Table 3, seven were high-quality studies, three were moderate-quality studies, and one was a low-quality study. All studies achieved random allocation of subjects, obtained similar baselines among groups, reported intergroup statistical results, and provided point measures and measures of variability. However, most articles did not score on items 5, 6, or 9, indicating challenges in subject and therapist blinding (Fig. 3).
Table 3.
PEDro scale of articles
| Author, year | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 | Item 11 | Total score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Zheng et al. 2015 | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7/10H |
| Lee and Chun 2014 | Y | N | Y | N | N | Y | Y | N | Y | Y | 6/10H |
| Viana et al. 2014 | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | 9/10H |
| Llorens et al. 2017 | N | N | N | N | N | N | N | Y | N | Y | 2/10 L |
| Yu Hsin Chen et al. 2021 | Y | Y | Y | Y | N | Y | Y | N | Y | Y | 8/10H |
| Xiaoling Yao et al. 2020 | Y | Y | Y | Y | N | N | Y | N | Y | Y | 7/10H |
| Roberto Llorens et al. 2021 | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7/10H |
| Hangjia Zhu et al. 2022 | Y | N | Y | N | N | N | N | N | Y | Y | 4/10 M |
| Fei Zhao et al. 2021 | Y | Y | Y | N | N | N | N | N | Y | Y | 5/10 M |
| Yuanwen Liu et al. 2020 | Y | Y | Y | N | N | Y | N | N | Y | Y | 6/10H |
| Haichao Cui et al. 2017 | Y | Y | Y | N | N | N | N | N | Y | Y | 5/10 M |
H = high quality; M = moderate quality; L = low quality
Fig. 3.
Risk of bias summary
Outcome measures
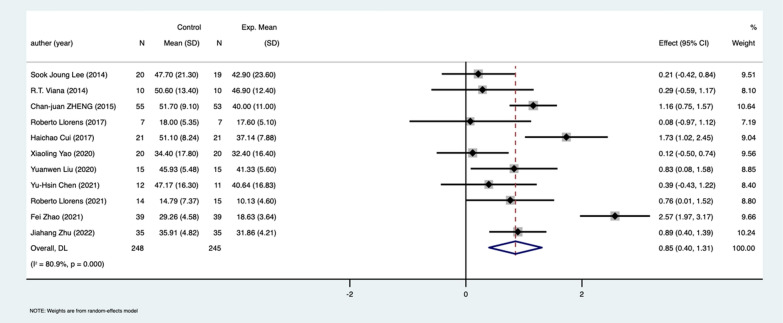
Fugl-Meyer assessment upper extremity
In this study, the FMA scores exclusively pertained to the upper extremities, which have a maximum score of 66, aligning with the research focus on upper limb motor function. All 11 included studies reported FMA-UE results. The meta-analysis showed that despite the intervention group’s FMA-UE scores being lower than those of the control group, the combined treatment group exhibited a significantly larger effect size (SMD = 0.85, 95% CI [0.4–1.31], p = 0.017; Fig. 4). However, significant heterogeneity was found (I2 = 80.9%). Meta-regression analysis for publication year, study type, age, trial duration, disease course, and treatment duration indicated that disease duration was a significant factor affecting heterogeneity (p = 0.047; Table 4). Egger’s test for publication bias had an intercept of 1.78 and a p value of 0.348, suggesting that there was no publication bias. The bottom row of Fig. 4 describes the overall effect size of the treatment estimated using a random-effects model.
Fig. 4.
Meta-analysis of the effect of VR combined with NIBS training on FMA-UE
Table 4.
Results of meta-regression analysis
| Model variables | Coefficients | Standard errors | 95% CI lower | 95% CI upper | P values |
|---|---|---|---|---|---|
| year | − 0.021 | 0.063 | − 0.195 | 0.154 | 0.759 |
| Is RCT | − 0.710 | 0.411 | − 1.852 | 0.431 | 0.159 |
| Study Length | 0.189 | 0.220 | − 0.421 | 0.800 | 0.437 |
| Duration | − 0.002 | 0.001 | − 0.004 | 0.000 | 0.047 |
| Treatment Length | − 0.037 | 0.002 | − 0.090 | 0.017 | 0.130 |
| Age | 0.018 | 0.037 | − 0.085 | 0.121 | 0.652 |
| _cons | 42.674 | 127.321 | − 310.826 | 396.175 | 0.754 |
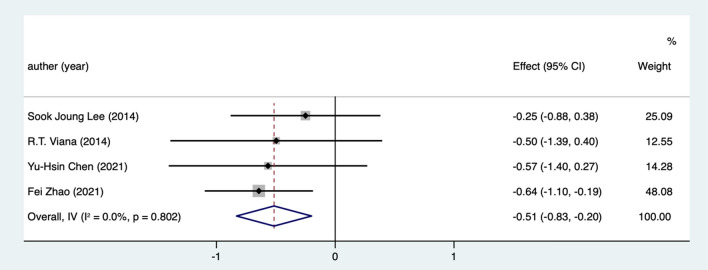
Modified Ashworth scale
Four studies reported the effect of combined treatment on muscle spasticity in stroke patients. The meta-analysis showed that the combined treatment group had significantly lower MAS scores compared to the control group (SMD = − 0.51, 95% CI [− 0.83, − 0.20], p = 0.032; Fig. 5). The heterogeneity test showed I2 = 0%, indicating no heterogeneity among the studies.
Fig. 5.
Meta-analysis of the effect of VR combined with NIBS training on MAS
Modified Barthel index
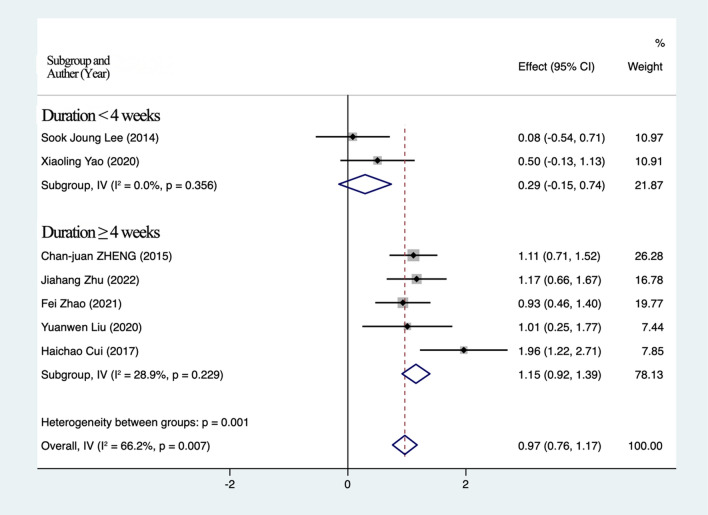
Seven studies reported MBI results. The meta-analysis showed that the combined treatment significantly improved the daily living abilities of stroke patients compared to traditional treatment (SMD = 0.97, 95% CI [0.76–1.17], P = 0.004; Fig. 6). The heterogeneity test indicated significant heterogeneity (I2 = 66.2%). Subgroup analysis based on treatment duration (< 4 weeks or > 4 weeks) reduced heterogeneity within subgroups but showed no significant differences, suggesting that treatment duration is a potential factor affecting daily living abilities.
Fig. 6.
Meta-analysis of the effect of VR combined with NIBS training on MBI
Wolf motor function test
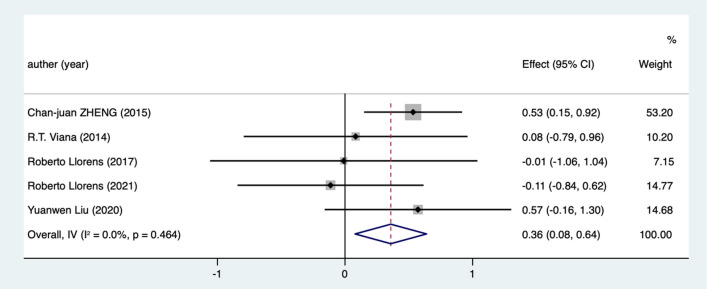
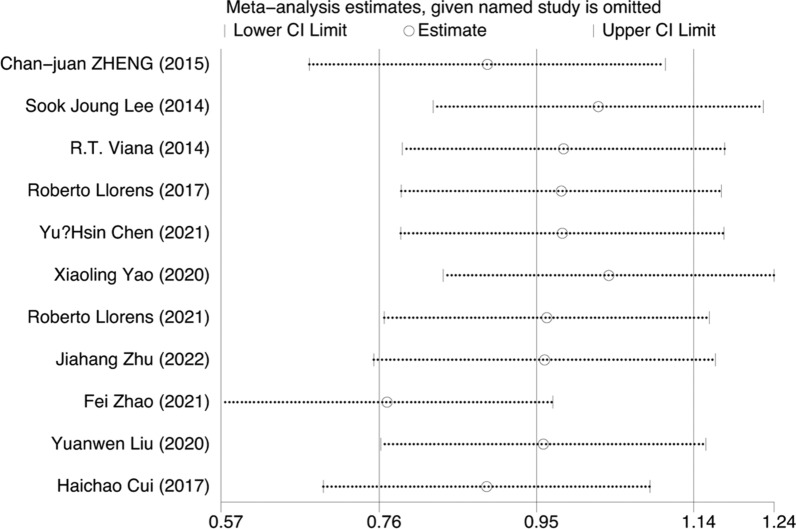
Five studies reported WMFT results. The heterogeneity test indicated I2 = 0%, indicating no heterogeneity among the studies. The meta-analysis showed that the combined treatment group had significantly higher WMFT scores compared to the control group (SMD = 0.36, 95% CI [0.08–0.64], p = 0.021; Figs. 7, 8).
Fig. 7.
Meta-analysis of the effect of combined VR and NIBS training on WMFT
Fig. 8.
Results of sensitivity analysis
Sensitivity results
Based on the leave-one-out sensitivity analysis, the results showed that excluding any of the 11 studies did not exceed the 95% confidence interval and was consistent with the main results, indicating that the findings were robust.
Discussion
In this study, a meta-analysis was performed to analyze the effectiveness of NIBS combined with VR training to improve upper limb motor function in stroke patients.
Outcome measures
The Fugl-Meyer Assessment Upper Extremity is the most frequently utilized metric across all the studies included in this meta-analysis, providing a standard measure of upper limb motor function. Additionally, other functional assessments such as the Wolf Motor Function Test, the Modified Ashworth Scale, and the Modified Barthel Index were widely employed in these studies to evaluate various aspects of motor impairment and functional independence. Furthermore, it’s important to note that some outcome measures not included in the meta-analysis can also assess upper limb function comprehensively. For example, Chen [19] implemented the Action Research Arm Test, Nine Hole Peg Test, Box and Block Test, and Motor Activity Log to conduct an extensive assessment of upper extremity motor function and fine motor skills. On the other hand, Zhao [22] focused on the neurophysiological level by utilizing changes in sensory-motor evoked potential latency and peak amplitude to assess the function of sensory and motor nerval conduction systems. This array of assessment tools underscores the multidimensional nature of upper limb rehabilitation and the need for both broad and specific metrics to fully understand recovery dynamics.
Fugl-Meyer assessment upper extremity
This meta-analysis highlights significant improvements in FMA-UE scores with combined NIBS and VR treatment compared to traditional or single training methods (SMD = 0.85, 95% CI [0.40, 1.31], p = 0.017). This result aligns with previous findings by Subramanian et al. [20], emphasizing the potential of combined interventions in enhancing motor recovery. The substantial improvement in FMA-UE scores suggests that integrating NIBS with VR can effectively target and enhance motor learning and neuroplasticity, crucial for upper limb rehabilitation. Notably, the baseline FMA-UE scores for the intervention group were lower than those of the control group, elucidating the initially lower post-intervention scores observed in Fig. 4. This discrepancy likely reflects the inclusion of patients with more severe motor impairments in the intervention group. Nevertheless, the significant improvement in FMA-UE scores in the intervention group highlights the efficacy of the combined VR and NIBS intervention, even in patients with more pronounced deficits at baseline. However, the high heterogeneity (I2 = 80.9%) observed across studies necessitates further analysis to identify contributing factors.
One notable source of heterogeneity is the duration of stroke before intervention. Meta-regression analysis indicated that longer durations since stroke onset were associated with reduced efficacy (p = 0.047). This finding is consistent with Viana et al. [23] and Llorens et al. [24], who reported that stroke patients with a history of more than one year showed limited training effects. These results suggest that early intervention post-stroke may be critical for maximizing therapeutic outcomes. This underscores the importance of timely rehabilitation and possibly revising clinical guidelines to prioritize early-stage interventions.
Modified Ashworth scale
The analysis of MAS scores revealed a significant reduction in muscle spasticity in the combined treatment group compared to the control group (SMD = − 0.51, 95% CI [− 0.83, − 0.20], p = 0.032). The lack of heterogeneity (I2 = 0%) suggests a consistent effect across studies, reinforcing the reliability of these results. These outcomes align with the mechanisms of NIBS, which involve altering cortical excitability, reduce spasticity, and promoting motor recovery through neuromodulation.
Modified Barthel index
The meta-analysis showed significant improvements in MBI scores, indicating enhanced daily living abilities in stroke patients receiving combined therapy (SMD = 0.97, 95% CI [0.76, 1.17], p = 0.004). However, substantial heterogeneity was observed (I2 = 66.2%). Subgroup analysis based on treatment duration (< 4 weeks vs. > 4 weeks) revealed that treatment duration is a significant factor influencing ADL outcomes. While the overall improvement in MBI underscores the functional benefits of combined therapy, the variability in results suggests that longer treatment durations may be necessary to achieve consistent improvements in ADLs. This finding highlights the need for personalized treatment plans that consider the duration and intensity of interventions to optimize patient outcomes.
Wolf motor function test
The WMFT results indicated significant improvements in motor function with combined therapy (SMD = 0.36, 95% CI [0.08, 0.64], p = 0.021). The absence of heterogeneity (I2 = 0%) in WMFT scores across studies suggests a uniform benefit of combined therapy in enhancing upper limb motor function. This consistency aligns with the established role of VR in providing engaging and task-specific training environments, which are essential for motor learning and recovery. The positive effects on WMFT scores reinforce the potential of VR combined with NIBS to facilitate functional motor recovery.
Intensity and duration of virtual reality interventions
The studies reviewed varied in VR intervention durations, ranging from 2 to 8 weeks, with a primary duration of 4 weeks and an intervention frequency of 5 times per week. Session durations ranged from 13 to 60 min [19, 23], with 20 [24, 25] and 30 min [26, 27] being the most common. This variability could contribute to the observed heterogeneity in treatment effects. Standardizing VR protocols, including session duration and frequency, could help clarify the optimal parameters for effective intervention. Future research should aim to determine the most effective dose–response relationship to maximize therapeutic benefits.
NIBS location and protocol
This meta-analysis included studies employing different NIBS protocols: tDCS in 7 studies, rTMS in 3 studies, and iTBS in 1 study. The variability in NIBS protocols, such as the use of cathodal versus anodal stimulation and targeting of the affected versus unaffected primary motor cortex (M1), adds complexity to interpreting the results. For instance, cathodal and anodal stimulation of the unaffected M1 [24, 25, 27–29] showed significant intervention effects, whereas anodal stimulation of the affected M1 [23] did not. These findings suggest that the site and type of stimulation are crucial factors influencing the efficacy of NIBS. The results indicate that targeting the unaffected hemisphere may enhance the compensatory mechanisms, facilitating recovery in the affected hemisphere [30].
NIBS stimulation intensity and duration
In the 7 studies using tDCS, most used a stimulation intensity of 2 mA [22]. The duration of each tDCS and rTMS session ranged from 13 to 60 min, with the most common duration being between 20 and 30 min. Additionally, the stimulation frequency was generally 5 times per week. For rTMS, the parameters included 1 Hz stimulation with 800 or 1800 pulses at 80% or 90% of the resting motor threshold (rMT) [26, 31], while iTBS was set at 50 Hz with 1200 pulses at 80% of the rMT [19]. The differences in stimulation intensity and duration likely contribute to the variability in outcomes. Standardizing these parameters in future studies could help determine the optimal settings for maximizing therapeutic effects.
Study quality and heterogeneity
The effectiveness of NIBS may be influenced by the duration of stroke, with early-stage intervention showing more promise. Viana’s study [23], with a high PEDro score, did not show significant improvements with tDCS in patients one year post-stroke, whereas Yao et al.’s study [25] (PEDro score 7) with a larger sample size of subacute or chronic stroke patients demonstrated significant benefits. The quality of the included studies varied, with PEDro scores ranging from 2 to 9, indicating a mix of high, moderate, and low-quality studies. The primary sources of bias included lack of blinding and unclear randomization methods, particularly in Chinese studies. Ensuring rigorous methodological standards in future studies will be crucial for obtaining more reliable and generalizable results.
Limitations
This systematic review has several limitations. Language bias may exist as only English and Chinese articles were included. Additionally, randomization, allocation concealment, and blinding descriptions were unclear in several studies, leading to potential biases. Although the search strategy was comprehensive, some eligible studies may have been missed. The variability in sample sizes and insufficient follow-up periods limit the ability to observe long-term effects. Future research should use a broader range of outcome measures and extend follow-up periods to better understand the intervention’s impact on functionality and quality of life.
Future research considerations
To address the limitations identified in this study, future research should focus on several key areas. Firstly, standardizing protocols for VR and NIBS interventions is crucial to reduce heterogeneity and improve comparability across studies. Establishing consistent parameters such as duration, intensity, and frequency will enable more reliable and reproducible results. Secondly, a broader range of outcome measures should be included to capture the multifaceted impact of these interventions. In addition to motor function, assessments of cognitive function, fine motor skills, sensory processing, and quality of life are essential for a comprehensive understanding of the treatment effects. Thirdly, extending follow-up periods is necessary to evaluate the sustainability and long-term benefits of the interventions, determining whether initial improvements are maintained over time. Additionally, expanding the inclusion criteria to encompass studies published in multiple languages will minimize language bias and enhance the generalizability of findings. Lastly, future studies should emphasize methodological rigor by providing clear and detailed descriptions of randomization procedures, allocation concealment, and blinding techniques. By addressing these considerations, future research can strengthen the evidence base for VR and NIBS in stroke rehabilitation, leading to more effective and personalized treatment protocols for improving upper limb motor function in stroke patients.
Conclusion
The integration of NIBS and VR has shown promising results in enhancing the recovery of fundamental upper limb motor function in stroke patients within a year post-onset. However, this combined approach did not significantly improve muscle tone, daily living activities, or advanced functional abilities.
Although most experimental interventions lasted for 4 weeks, analysis suggests that longer durations result in better effects. The frequency of intervention is typically 5 times a week, with VR training sessions lasting 20–25 min and NIBS stimulation sessions lasting 20–30 min. For the intensity and stimulation area of NIBS, when using tDCS, cathodal or anodal stimulation is applied to the unaffected primary motor cortex (M1) with a stimulation intensity of 2 mA. When using rTMS, the unaffected M1 can be targeted with an intensity of 1 Hz, 800–1800 pulses, or 80–90% of the resting motor threshold (rMT) to enhance the stimulation effect.
In addition to the commonly used evaluation indicators for upper limb motor function in hemiplegic patients, future research should incorporate additional assessment tools, such as cognitive and fine motor skill evaluations, based on changes in stimulation areas and the degree of training. Researchers should also consider using advanced indicators, such as motor and sensory evoked potentials, functional magnetic resonance imaging (fMRI), and biomechanical analysis of movement patterns, to gain a more comprehensive understanding of the intervention’s impact.
To fully understand the long-term benefits and persistence of intervention effects, it is recommended that future studies include long-term follow-up periods. This approach will help in assessing the sustainability of the improvements and provide more robust evidence for the effectiveness of combining NIBS and VR in stroke rehabilitation. By addressing these aspects, future research can build on the current findings to optimize treatment protocols and ultimately improve the quality of life for stroke patients.
Author contributions
In accordance with our authorship policy for BMC, which offers guidance and sets criteria for authorship, the specific contributions of each author to this manuscript are detailed as follows: Nuo Zhang (N.Z.) and Hujun Wang (H.W.), contributed equally to this work. They were both heavily involved in the conception and design of the study, data collection, and analysis. Hanming Wang (H.W.) contributed significantly to the methodology development and played a key role in interpreting the data. Shuyan Qie (S.Q.), as the corresponding author, was responsible for drafting the manuscript and revising it critically for important intellectual content. Additionally, S.Q. provided supervision and guidance throughout the research process. All the authors are affiliated with the Department of Rehabilitation, Beijing Rehabilitation Hospital, Capital Medical University, Beijing, 100144, China. Each author has read and approved the final version of the manuscript. They have agreed to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This statement supersedes any previous authorship information in the manuscript and is the one that will be published.
Funding
This study was supported by the Ministry of Science and Technology of the People’s Republic of China under the project ‘Study on the effects and mechanisms of multi-type physical stimulation methods on body function and the construction of an AI-assisted systematic, standardized, and hierarchical physical stimulation load intensity detection system’ (2022YFC3600501).
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Nuo Zhang and Hujun Wang contributed equally.
References
- 1.Kwakkel G, Kollen BJ, van der Grond J, Prevo AJH. Probability of regaining dexterity in the flaccid upper limb: impact of severity of paresis and time since onset in acute stroke. Stroke. 2003;34(9):2181–6. [DOI] [PubMed] [Google Scholar]
- 2.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Executive summary: heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation. 2014;129(3):399–410. [DOI] [PubMed] [Google Scholar]
- 3.Zheng Y, Peng Y, Xu G, Li L, Wang J. Using corticomuscular coherence to reflect function recovery of paretic upper limb after stroke: a case study. Vol. 8, Frontiers in neurology. Switzerland; 2017. p. 728. [DOI] [PMC free article] [PubMed]
- 4.Kleim JA, Jones TA. Principles of experience-dependent neural plasticity: implications for rehabilitation after brain damage. J Speech Lang Hear Res. 2008;51(1):S225–39. [DOI] [PubMed] [Google Scholar]
- 5.Mekbib DB, Han J, Zhang L, Fang S, Jiang H, Zhu J, et al. Virtual reality therapy for upper limb rehabilitation in patients with stroke: a meta-analysis of randomized clinical trials. Brain Inj. 2020;34(4):456–65. [DOI] [PubMed] [Google Scholar]
- 6.Sánchez-Cuesta FJ, Arroyo-Ferrer A, González-Zamorano Y, Vourvopoulos A, Badia SBI, Figuereido P, et al. Clinical effects of immersive multimodal BCI-VR training after bilateral neuromodulation with rTMS on upper limb motor recovery after stroke. A study protocol for a randomized controlled trial. Medicina (Kaunas). 2021;57(8):736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hara T, Shanmugalingam A, McIntyre A, Burhan AM. The effect of non-invasive brain stimulation (NIBS) on attention and memory function in stroke rehabilitation patients: a systematic review and meta-analysis. Diagnostics (Basel, Switzerland). 2021;11(2):227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fitzgerald PB, Fountain S, Daskalakis ZJ. A comprehensive review of the effects of rTMS on motor cortical excitability and inhibition. Clin Neurophysiol Off J Int Fed Clin Neurophysiol. 2006;117(12):2584–96. [DOI] [PubMed] [Google Scholar]
- 9.Hsu W-Y, Cheng C-H, Liao K-K, Lee I-H, Lin Y-Y. Effects of repetitive transcranial magnetic stimulation on motor functions in patients with stroke: a meta-analysis. Stroke. 2012;43(7):1849–57. [DOI] [PubMed] [Google Scholar]
- 10.Butler AJ, Shuster M, O’Hara E, Hurley K, Middlebrooks D, Guilkey K. A meta-analysis of the efficacy of anodal transcranial direct current stimulation for upper limb motor recovery in stroke survivors. J Hand Ther Off J Am Soc Hand Ther. 2013;26(2):162–70. [DOI] [PubMed] [Google Scholar]
- 11.Mao Y, Chen P, Li L, Huang D. Virtual reality training improves balance function. Neural Regen Res. 2014;9(17):1628–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bevilacqua R, Maranesi E, Riccardi GR, Di Donna V, Pelliccioni P, Luzi R, et al. Non-immersive virtual reality for rehabilitation of the older people: a systematic review into efficacy and effectiveness. J Clin Med. 2019;8(11):1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holden MK. Virtual environments for motor rehabilitation: review. Cyberpsychol Behav impact Internet, Multimed virtual Real Behav Soc. 2005;8(3):187–9. [DOI] [PubMed] [Google Scholar]
- 14.Laver KE, Lange B, George S, Deutsch JE, Saposnik G, Crotty M. Virtual reality for stroke rehabilitation. Cochrane database Syst Rev. 2017 Nov;11(11):CD008349. [DOI] [PMC free article] [PubMed]
- 15.Karamians R, Proffitt R, Kline D, Gauthier LV. Effectiveness of virtual reality- and gaming-based interventions for upper extremity rehabilitation poststroke: a meta-analysis. Arch Phys Med Rehabil. 2020;101(5):885–96. [DOI] [PubMed] [Google Scholar]
- 16.Ahmed I, Mustafaoglu R, Benkhalifa N, Yakhoub YH. Does noninvasive brain stimulation combined with other therapies improve upper extremity motor impairment, functional performance, and participation in activities of daily living after stroke? A systematic review and meta-analysis of randomized controlle. Top Stroke Rehabil. 2023;30(3):213–34. [DOI] [PubMed] [Google Scholar]
- 17.Subramanian SK, Lourenço CB, Chilingaryan G, Sveistrup H, Levin MF. Arm motor recovery using a virtual reality intervention in chronic stroke: randomized control trial. Neurorehabil Neural Repair. 2013;27(1):13–23. [DOI] [PubMed] [Google Scholar]
- 18.Massetti T, Crocetta TB, da Silva TD, Trevizan IL, Arab C, Caromano FA, et al. Application and outcomes of therapy combining transcranial direct current stimulation and virtual reality: a systematic review. Disabil Rehabil Assist Technol. 2017;12(6):551–9. [DOI] [PubMed] [Google Scholar]
- 19.Chen YH, Chen CL, Huang YZ, Chen HC, Chen CY, Wu CY, et al. Augmented efficacy of intermittent theta burst stimulation on the virtual reality-based cycling training for upper limb function in patients with stroke: a double-blinded, randomized controlled trial. J Neuroeng Rehabil. 2021;18(1):1–14. 10.1186/s12984-021-00885-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Subramanian SK, Prasanna SS. Virtual reality and noninvasive brain stimulation in stroke: how effective is their combination for upper limb motor improvement? A meta-analysis. PM R. 2018;10(11):1261–70. 10.1016/j.pmrj.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 21.Cashin AG, McAuley JH. Clinimetrics: physiotherapy evidence database (PEDro) scale. J Physiother. 2020;66(1):59. [DOI] [PubMed] [Google Scholar]
- 22.Fei Z, Jiewen T, Xiao B, Hejun L. Effect of transcranial direct- current stimulation plus virtual reality on the recovery of upper limb function in patients with cerebral infarction. 2021;4–8.
- 23.Viana RT, Laurentino GEC, Souza RJP, Fonseca JB, Silva Filho EM, Dias SN, et al. Effects of the addition of transcranial direct current stimulation to virtual reality therapy after stroke: A pilot randomized controlled trial. NeuroRehabilitation. 2014;34(3):437–46. [DOI] [PubMed] [Google Scholar]
- 24.Llorens R, Borrego A, Latorre J, Alcaniz M, Colomer C, Noe E. A combined transcranial direct current stimulation and virtual reality-based intervention on upper limb function in chronic stroke survivors with severe hemiparesis. Int Conf Virtual Rehabil ICVR. 2017;2017. [DOI] [PMC free article] [PubMed]
- 25.Yao X, Cui L, Wang J, Feng W, Bao Y, Xie Q, et al. Effects of transcranial direct current stimulation with virtual reality on upper limb function in patients with ischemic stroke: a randomized controlled trial. J Neuroeng Rehabil. 2020;17(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zheng CJ, Liao WJ, Xia WG. Effect of combined low-frequency repetitive transcranial magnetic stimulation and virtual reality training on upper limb function in subacute stroke: a double-blind randomized controlled trail. J Huazhong Univ Sci Technol Med Sci. 2015;35(2):248–54. [DOI] [PubMed] [Google Scholar]
- 27.Lee SJ, Chun MH. Combination transcranial direct current stimulation and virtual reality therapy for upper extremity training in patients with subacute stroke. Arch Phys Med Rehabil. 2014;95(3):431–8. 10.1016/j.apmr.2013.10.027. [DOI] [PubMed] [Google Scholar]
- 28.Llorens R, Fuentes MA, Borrego A, Latorre J, Alcañiz M, Colomer C, et al. Effectiveness of a combined transcranial direct current stimulation and virtual reality-based intervention on upper limb function in chronic individuals post-stroke with persistent severe hemiparesis: a randomized controlled trial. J Neuroeng Rehabil. 2021;18(1):1–13. 10.1186/s12984-021-00896-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu Y, Huang L, Zhang S, Ai Y, Li LHX. Effects of transcranial direct current stimulation combined with virtual reality training on upper limb function of stroke patient: a pilot randomized controlled single-blind trial. West China Med J. 2020;35(5):544–9. [Google Scholar]
- 30.Wang Q, Zhang D, Zhao YY, Hai H, Ma YW. Effects of high-frequency repetitive transcranial magnetic stimulation over the contralesional motor cortex on motor recovery in severe hemiplegic stroke: a randomized clinical trial. Brain Stimul. 2020;13(4):979–86. 10.1016/j.brs.2020.03.020. [DOI] [PubMed] [Google Scholar]
- 31.Cui H, Zhai H, Zhang M, Chen W. Effect of acupuncture combined with low-frequency repetitive transcranial magnetic stimulation on the upper limb dysfunction after stroke. 2017;37(6):1195–9.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.