Abstract
The effect of combinations of the mutagenic base analog 5-fluorouracil (FU) and the antiviral inhibitors guanidine hydrochloride (G) and heparin (H) on the infectivity of foot-and-mouth disease virus (FMDV) in cell culture has been investigated. Related FMDV clones differing up to 106-fold in relative fitness in BHK-21 cells have been compared. Systematic extinction of intermediate fitness virus was attained with a combination of FU and G but not with the mutagen or the inhibitor alone. Systematic extinction of high-fitness FMDV required the combination of FU, G, and H. FMDV showing high relative fitness in BHK-21 cells but decreased replicative ability in CHO cells behaved as a low-fitness virus with regard to extinction mutagenesis in CHO cells. This confirms that relative fitness, rather than a specific genomic sequence, determines the FMDV response to enhanced mutagenesis. Mutant spectrum analysis of several genomic regions from a preextinction population showed a statistically significant increase in the number of mutations compared with virus passaged in parallel in the absence of FU and inhibitors. Also, in a preextinction population the types of mutations that can be attributed to the mutagenic action of FU were significantly more frequent than other mutation types. The results suggest that combinations of mutagenic agents and antiviral inhibitors can effectively drive high-fitness virus into extinction.
An increase in the mutation rate during replication of RNA viruses can result in a decrease of viral infectivity and occasional virus extinction (11, 34, 39, 40, 60). Studies with the important animal pathogen foot-and-mouth disease virus (FMDV)—a member of the Picornaviridae family (53, 63)—have shown that a small replicative population size and low viral fitness favored virus extinction (60). This was documented with single and multiple passages of FMDVs differing up to 106-fold in relative fitness in the absence or presence of the mutagenic base analogs 5-fluorourocil (FU) or 5-azacytidine, individually or in combination (59, 60). Mutagenic treatments resulted in occasional, not systematic, viral extinction, while parallel passages in the absence of mutagens never led to loss of infectivity, no matter how low the initial viral population size and fitness were (59, 60). These results suggested the possibility that a combination of an antiviral inhibitor, to reduce the replicative load of virus, and a mutagenic agent could be more effective in producing viral extinction than a mutagenic agent used in isolation. To test this possibility we have studied the effect of the mutagenic base analog FU and the antiviral inhibitors guanidine hydrochloride (G) and heparin (H) on the infectivity of FMDV clones and populations depicting a wide range of relative fitness values. FU has been shown to be mutagenic for a number of RNA viruses (6, 20, 31, 34, 51, 71), including FMDV (59, 60). G at millimolar concentrations blocks the replication of picornaviruses (5, 7, 15, 49, 52, 55), arboviruses (27), and several plant viruses (13, 67). In poliovirus, the target of G is the ATPase activity of nonstructural protein 2C (49), a protein involved in viral replication and encapsidation. In FMDV, amino acid substitutions at 2C have also been associated with resistance to G (56). Heparins are sulfated polysaccharides (9) which bind FMDV when the virus has been passaged in cell culture and has adapted to using heparan sulfate (HS) as a receptor (2, 35, 54). Adaptation to use of HS as a receptor has been associated with substitutions which lead to positively charged amino acids at exposed positions of the capsid (2, 54).
Here we report that high-frequency extinctions of FMDV of low and intermediate fitness values can be achieved with a combination of FU and G but not with either drug alone. Extinction of high-fitness FMDV populations required a triple combination of G and H together with FU. Mutation frequencies in the mutant spectrum of three genomic regions of a preextinction population obtained by the combined action of an inhibitor and a mutagen were compared to values in genomes passaged in standard conditions and also to values previously determined for FMDV populations subjected to one or multiple passages in the presence of FU (60). We found that mutation frequencies increased up to fourfold. There was also a statistically significant increase in the number of mutations in preextinction populations with respect to control populations, and the frequency of mutation types that can be attributed to the mutagenic action of FU was significantly higher than the frequency of other types of mutations.
MATERIALS AND METHODS
Cells and viruses.
The origins of baby hamster kidney 21 cells (BHK-21) and Chinese hamster ovary cells (CHO) have been previously described (3, 18, 25, 62). Both cell types were grown in Dulbecco's modified Eagle's medium (DMEM) (Gibco) supplemented with nonessential amino acids (Gibco), 50 mg of gentamicin (Sigma)/ml, and 5% fetal calf serum (Gibco).
FMDV C-S8c1 is a plaque-purified derivative of the European serotype C natural isolate C1 Santa Pau-Spain 70 (62). MARLS is a monoclonal antibody escape mutant obtained from FMDV C-S8c1 passaged 213 times in BHK-21 cells (C-S8c1p213) (3). MARLS includes the substitution L-144→S at antigenic site A, located within the G-H loop of the capsid protein VP1 (43, 44). In BHK-21 cells, the replicative fitness of MARLS is about 130-fold higher than that of C-S8c1 (59). In CHO cells the replicative fitness of MARLS is lower than in BHK-21 cells, as indicated by a delayed kinetics of viral production and a 10-fold reduction in the viral titer at the point of complete cytopathic effect. No ranking of the relative fitnesses of FMDV mutants has been established with CHO cells. Clones H −1 to −5 are a series of low-fitness subclones from the clone H5 (derived from C-S8c1p113 [23]) after 95 plaque-to-plaque transfers in BHK-21 cells (C. Escarmís et al., unpublished results). Relative fitness of the H
−1 to −5 are a series of low-fitness subclones from the clone H5 (derived from C-S8c1p113 [23]) after 95 plaque-to-plaque transfers in BHK-21 cells (C. Escarmís et al., unpublished results). Relative fitness of the H subclones was estimated on the basis of the number of infectious progeny produced per plaque (23): their relative fitness is about 104-fold lower than that of C-S8c1 virus. A good correspondence between relative fitness values obtained in growth competition experiments and those estimated on the basis of infectious progeny production has been previously documented with several FMDV clones and populations (23); Escarmís et al., unpublished results).
subclones was estimated on the basis of the number of infectious progeny produced per plaque (23): their relative fitness is about 104-fold lower than that of C-S8c1 virus. A good correspondence between relative fitness values obtained in growth competition experiments and those estimated on the basis of infectious progeny production has been previously documented with several FMDV clones and populations (23); Escarmís et al., unpublished results).
Procedures for infection of BHK-21 cell monolayers with FMDV in liquid medium and for plaque assays in semisolid agar medium have been previously described (3, 18, 62). The standard viral production assay with BHK-21 cells consisted of the infection of 9 × 105 cells with FMDV at a multiplicity of infection of approximately 0.05 PFU per cell. Further passages were carried out with 0.1 ml of the supernatant of the previous infection. For assays with CHO cells, 9 × 105 cells were infected with FMDV MARLS at a multiplicity of infection of 1 PFU per cell in the first passage, and the following passages were carried out with 0.1 ml of the supernatant of the previous passage. Except for preextinction populations, the multiplicity of infection of successive passages ranged from 0.001 to 1 PFU per cell, and the value for each individual infection can be calculated from the titers shown in the corresponding figures. To control for the absence of viral contamination, parallel passages of supernatants of mock-infected cells were carried out throughout the experiments, with no evidence of infectivity or cytopathology in the cultures. Viruses were titrated at every passage, on BHK-21 cell monolayers, in triplicate.
Mutagenic and antiviral treatments.
To prepare culture medium containing FU (Sigma), the appropriate amount of analog was dissolved in DMEM to yield a 2.5-mg/ml solution, which was diluted in DMEM as needed for the experiments. To prepare medium containing G (Sigma), the appropriate amount was dissolved in DMEM to yield a 4 mM solution (0.38 mg/ml). To prepare medium containing a mixture of both FU and G, the appropriate amount of G was added to DMEM containing FU (200 μg/ml) to yield FUG, a solution containing FU (200 μg/ml) and G (4 mM). H (Heparin sodium salt; Sigma) was dissolved in water and diluted in DMEM or FUG (to yield FUGH, a solution containing FU [200 μg/ml], G [4 mM], and H [1 mg/ml]) as needed for the experiments. All solutions were sterilized by filtration. Media were supplemented with 2% fetal calf serum and stored at 4°C for a maximum of 14 days. The effect of FU, inhibitors, or their combination on cell viability was monitored by trypan blue exclusion as described previously (60). Before counting, cells were washed with DMEM, detached by trypsin treatment, and resuspended in DMEM supplemented with 2% fetal calf serum. Viable BHK-21 cells comprised at least 20% of the total (Fig. 1), under the doses and times of exposure used for the experiments. CHO cells were more resistant than BHK-21 cells to the treatments, and after exposure to FUG, approximately 80% of the cells were viable (N. Pariente et al., unpublished data).
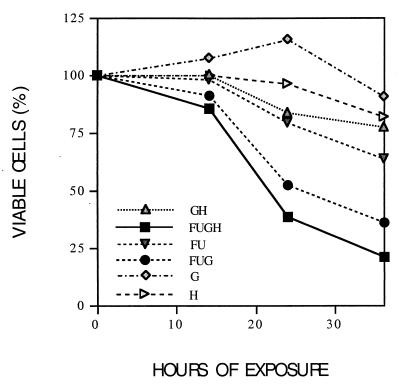
FIG. 1.
BHK-21 cell viability in the presence of FU, G, and H, alone or in combination. The origin of BHK-21 cells and FMDV C-S8c1, as well as procedures for cell growth, antiviral treatment, quantification of cell viability, and infections with FMDV, are detailed in Materials and Methods. Percent cell viabilities (trypan blue exclusion) were calculated relative to those in parallel, untreated cell cultures, counting 300 to 700 cells per sample. Hours of exposure refers to the time elapsed between the addition of the mutagen or antiviral agent to cells and the determination of cell viability. Standard deviations (not included in the plots) never exceeded 20%.
In order to establish whether the 20% of BHK-21 cells that were left after 37 h of exposure to FUGH were able to sustain FMDV replication, cell monolayers that had been preincubated for 13 h with FU and for 24 h with FUGH were washed with DMEM and incubated for 2 h with DMEM supplemented with 2% fetal calf serum. Then, the cells were infected either with MARLS, at a multiplicity of infection of about 10 PFU per cell, or with the low-fitness H clone, at about 0.005 PFU per cell. Parallel infections of confluent BHK-21 cell monolayers were carried out as a control. The titer of MARLS attained in treated cells was 1 × 107 PFU/ml, versus 4 × 108 PFU/ml in untreated cells. In the case of the low-fitness H
clone, at about 0.005 PFU per cell. Parallel infections of confluent BHK-21 cell monolayers were carried out as a control. The titer of MARLS attained in treated cells was 1 × 107 PFU/ml, versus 4 × 108 PFU/ml in untreated cells. In the case of the low-fitness H clone, titers were 7 × 104 PFU/ml and 1 × 107 PFU/ml, respectively. This implies that cytotoxicity cannot account for viral extinction, since even a very low-fitness virus can carry out its life cycle in treated cells in infections started with very low numbers of infectious units.
clone, titers were 7 × 104 PFU/ml and 1 × 107 PFU/ml, respectively. This implies that cytotoxicity cannot account for viral extinction, since even a very low-fitness virus can carry out its life cycle in treated cells in infections started with very low numbers of infectious units.
Viral infections in the presence of FU, inhibitors, or their combination.
Different standard single infections were carried out in parallel. (i) In control infections (absence of mutagen and inhibitors), confluent cell monolayers were infected with FMDV (adsorption for 45 min at 37°C), washed for 1 min with 0.1 M phosphate buffer (pH 6.0) (to inactivate unadsorbed virions), and washed again extensively with DMEM. The infection was allowed to proceed in DMEM supplemented with 2% fetal calf serum. (ii) For infections in the presence of FU, confluent cell monolayers were pretreated for 13 h with 200 μg of FU/ml and then washed with DMEM; the procedure was done as for the control infections, and the infection was allowed to proceed in the presence of the same concentration of FU. (iii) For infections in the presence of G, no pretreatment of the cell monolayer was performed; after addition of FMDV and washing of the cell monolayers, the infection was allowed to proceed in the presence of 4 mM G. (iv) For infections in FUG, confluent cell monolayers were pretreated for 13 h with 200 μg of FU/ml and then washed with DMEM. After virus adsorption and washing of cell monolayers, the infection proceeded in the presence of FUG. (v) For infections in H, no pretreatment of the cell monolayer was performed; FMDVs were preincubated with 1 mg of H/ml for 30 min at room temperature. After inoculation and washing of the cell monolayers, the infection was allowed to proceed in the presence of 1 mg of H/ml. (vi) For infections in the presence of FUGH, confluent cell monolayers were pretreated for 13 h with 200 μg of FU/ml and then washed with DMEM. Viruses were preincubated with 1 mg of H/ml for 30 min at room temperature. After virus adsorption and washing of the cell monolayers, the infection proceeded in the presence of FUGH. All infections were allowed to continue for approximately 24 h.
For serial passage of virus, 0.1 ml of cell culture supernatant from the previous infection was used to infect a cell monolayer pretreated with a mutagen as described above for the standard single infections. Virus was titrated after each passage. When no cytopathology was observed, at least three serial blind passages using undiluted cell culture supernatant, in the absence of mutagen and antiviral agents, were carried out prior to viral detection tests. Viral extinction is defined on the basis of two criteria, as previously described (60): absence of infectivity in the cell culture supernatant after the last blind passage and no amplification of viral genomic regions by reverse transcription and PCR amplification. Populations passaged in the presence of a mutagen or antiviral agents are indicated with the abbreviation of the culture medium used, followed by the passage number (e.g., C-S8c1FUGp1 is C-S8c1 passaged once in the presence of a mixture of FU and G).
cDNA synthesis, PCR amplification, and nucleotide sequencing.
Viral RNA was extracted as previously described (60) using 150 μl of culture medium; for preextinction populations (virus in the passage prior to extinction), the volume used was 1 ml due to the low viral load present in these samples. cDNA synthesis and PCR amplification (reverse transcription-PCR [RT-PCR]) were performed as previously described (23). In all cases cDNA synthesis was carried out using avian myeloblastosis virus reverse transcriptase (Promega). Amplification was performed with Taq polymerase (Perkin-Elmer) for determination of the consensus sequences and for the extinction test. Amplifications intended for molecular cloning and nucleotide sequencing of individual clones were carried out with the Expand High Fidelity PCR System (Roche) (4). To ensure an excess of template molecules for amplification, only the samples for which RT-PCR amplification of 1/10 of the initial RNA template was also positive were used for molecular cloning of the cDNA. Three FMDV genomic regions were subjected to RT-PCR amplification: residues 3193 to 3869 (spanning the VP1-coding region), residues 4280 to 5349 (spanning the 2C-coding region), and residues 6609 to 8035 (spanning the entire 3D [polymerase]-coding region). Numbering of FMDV genomic nucleotides is that used in reference 65. The oligonucleotide primers used to amplify the VP1- and 3D-coding regions have been previously described (60). The following primers were used for 2C amplification: 5′-TCGGAGCTCCGATTCTGTTGGCCGGGTTG-3′, termed 2BR3SacI (sense, 5′ position 4253), and 5′-AAAGAATTCAATTGCTGCCTCGTGTTG-3′, termed 3AD4EcoRI (antisense, 5′ position 5376); they include restriction enzyme sites for SacI and EcoRI, respectively (underlined). Amplified cDNAs coding for VP1, 2C, and 3D were digested with the appropriate restriction enzymes, ligated to plasmid pGEM-4Z (Promega) previously digested with the same restriction enzymes, and cloned into Escherichia coli DH5α as described previously (60). DNA from bacterial colonies was obtained by direct PCR amplification from colony lysates using the commercial primers SP6 and T7 (Promega), which are complementary to positions flanking the polylinker site of pGEM-4Z. Nucleotide sequences were determined using the Big Dye Terminator Cycle Sequencing kit (ABI Prism; Perkin-Elmer) and the automated sequencer ABI373. Each mutation was confirmed by two independent sequencing assays using primers of different orientation. Sequences were analyzed with the DNA Star 4.0, Genedoc, and GCG package programs.
The heterogeneity of the mutant spectrum of viral quasispecies was quantitated by use of the mutation frequency and normalized Shannon entropy (Sn) (68). Mutation frequency is the number of different mutations found relative to the number of nucleotides sequenced; it is calculated by dividing the number of different mutations found in a set of genomes (compared to the consensus nucleotide sequence of the same set) by the total number of nucleotides sequenced (16, 21). Sn is a measure of the proportion of identical sequences in a mutant distribution. The possible values of the Sn range from zero (when all genomes are identical) to one (when all genomes differ from one another) (60, 68).
RESULTS
Systematic extinction of C-S8c1 by a combination of FU and G.
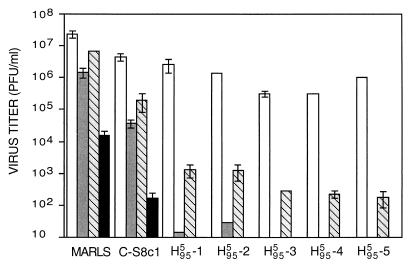
G at a concentration of 4 mM in the culture medium causes a 10- to 102-fold reduction in the production of FMDV C-S8c1 with no significant effect on BHK-21 cell viability. The combination of 200 μg of FU/ml and 4 mM G (FUG) resulted in a decrease of cell viability to about 40% of that of the untreated cells (Fig. 1). To test whether FUG was more effective than either FU or G alone in inhibiting viral production, FMDV MARLS, C-S8c1, and five low-fitness subclones derived from H were used to infect BHK-21 cells in the absence or presence of FU, G, or FUG. The FMDVs used differed up to 106-fold in relative fitness value (see Materials and Methods). The results (Fig. 2) show that FUG led to reductions in viral production that were 102- to 103-fold larger than those observed in the presence of FU or G alone. Yields of the subclones H
were used to infect BHK-21 cells in the absence or presence of FU, G, or FUG. The FMDVs used differed up to 106-fold in relative fitness value (see Materials and Methods). The results (Fig. 2) show that FUG led to reductions in viral production that were 102- to 103-fold larger than those observed in the presence of FU or G alone. Yields of the subclones H −3, H
−3, H −4 and H
−4 and H −5 in the presence of FU were undetectable, but virus reemerged after one passage. However, extinction of the subclones H
−5 in the presence of FU were undetectable, but virus reemerged after one passage. However, extinction of the subclones H −1 to H
−1 to H −5 was observed in all cases in one passage in the presence of FUG.
−5 was observed in all cases in one passage in the presence of FUG.
FIG. 2.
Effect of viral fitness on the decrease of infectivity in a single round of infection in the absence or presence of FU, G, or the mixture of both (FUG). FMDV MARLS, C-S8c1, and H clones are described in Materials and Methods. Empty columns indicate viral production in the absence of mutagen or antiviral agent; gray columns indicate viral production in the presence of 200 μg of FU/ml; striped gray columns indicate viral production in the presence of 4 mM G; and black columns show viral production in the presence of FUG. In this experiment 9 × 105 BHK-21 cells were infected with 5 × 104 PFU of virus. Extinction of the five H
clones are described in Materials and Methods. Empty columns indicate viral production in the absence of mutagen or antiviral agent; gray columns indicate viral production in the presence of 200 μg of FU/ml; striped gray columns indicate viral production in the presence of 4 mM G; and black columns show viral production in the presence of FUG. In this experiment 9 × 105 BHK-21 cells were infected with 5 × 104 PFU of virus. Extinction of the five H FUGp1 clones was confirmed by three additional blind passages, in the absence of mutagen and inhibitor with no evidence of infectivity, and no RT-PCR-amplifiable material in the supernatant of the third passage. Yields of H
FUGp1 clones was confirmed by three additional blind passages, in the absence of mutagen and inhibitor with no evidence of infectivity, and no RT-PCR-amplifiable material in the supernatant of the third passage. Yields of H −3, H
−3, H −4, and H
−4, and H −5 clones in the presence of FU were undetectable (<10 PFU/ml), but virus reemerged after one blind passage in the absence of the mutagen. However, these clones were extinguished upon a second passage in the presence of FU. Titrations were done in triplicate, and standard deviations are indicated. Procedures for chemical mutagenesis, antiviral treatment, and determination of viral infectivity are described in Materials and Methods.
−5 clones in the presence of FU were undetectable (<10 PFU/ml), but virus reemerged after one blind passage in the absence of the mutagen. However, these clones were extinguished upon a second passage in the presence of FU. Titrations were done in triplicate, and standard deviations are indicated. Procedures for chemical mutagenesis, antiviral treatment, and determination of viral infectivity are described in Materials and Methods.
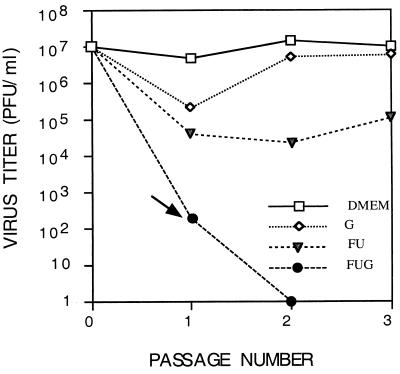
Previous results showed that serial passage of FMDV C-S8c1 in the presence of FU resulted in occasional, not systematic, extinction of the virus (60). To evaluate the frequency of extinctions of C-S8c1 in the presence of FUG, serial passages were carried out as detailed in Materials and Methods. Extinction of C-S8c1 was observed at passage 2 in the presence of FUG but not in the presence of FU or G alone (Fig. 3). To test the robustness of C-S8c1 extinction under these conditions, 46 replicates of an infection of 3 × 105 BHK-21 cells with 104 PFU of C-S8c1 in the presence of FUG were analyzed. Extinction was observed in all cases at the second passage. Thus, the combination of the mutagenic base analog FU and the antiviral inhibitor G was much more effective than FU alone in producing viral extinction. Systematic extinction was observed with the standard reference FMDV C-S8c1 clone after two passages and with low-fitness H clones after only one passage in the presence of the mutagen-inhibitor combination.
clones after only one passage in the presence of the mutagen-inhibitor combination.
FIG. 3.
Serial passages of C-S8c1 in the absence or presence of FU, G, or FUG. In this experiment, 9 × 105 BHK-21 cells were infected with 5 × 104 PFU of FMDV C-S8c1, and subsequent infections were carried out with 0.1 ml of supernatant of the previous passage (the multiplicity of infection at each passage can be calculated from the titers shown in ordinate). The origin of FMDV C-S8c1, conditions for mutagenic and antiviral treatment, and those for determination of FMDV infectivity are described in Materials and Methods. The preextinction population is indicated by an arrow. Viral extinction was confirmed by three additional blind passages in the absence of mutagen and inhibitor with no evidence of infectivity, and no RT-PCR-amplifiable material was found in the supernatant of the third passage. All titrations were done in triplicate. Standard deviations (not included in the plots) never exceeded 15%.
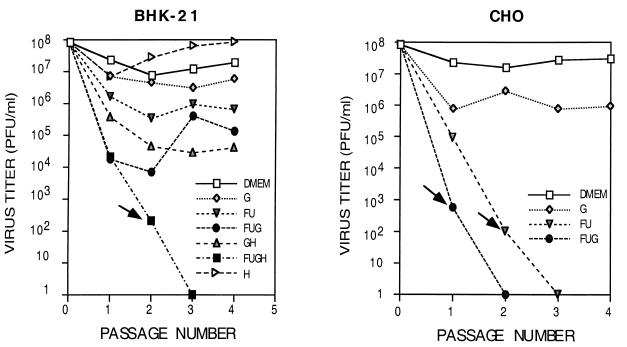
Efficient extinction of MARLS in CHO cells.
MARLS displays a 130-fold-greater fitness than C-S8c1 in BHK-21 cells (59, 60), as a result of 213 serial passages in BHK-21 cells (3). However, its fitness in CHO cells is at a much lower level, as judged from a 10-fold-lower progeny production, than in BHK-21 cells. Therefore, if difficulties for extinction of MARLS in infections in the presence of FUG were due to its high fitness (Fig. 2), MARLS should manifest an increased susceptibility to FU and FUG in infections of CHO cells. The results (Fig. 4) show that extinction of MARLS occurred after three passages in CHO cells with FU and after two passages with FUG, suggesting that resistance to extinction of MARLS in BHK-21 cells was due to its high fitness in the environment provided by BHK-21 cells and not to an intrinsic property of the MARLS genome to be refractory to extinction.
FIG. 4.
Infectivity values upon passage of FMDV MARLS in the absence or presence of FU, G, or FUG in BHK-21 and CHO cells. Conditions for mutagenic and antiviral treatments and for determination of FMDV infectivity are detailed in Materials and Methods. Left panel: FMDV MARLS was tested by infecting 9 × 105 BHK-21 cells with 5 × 104 PFU of virus, and the next passages were carried out by infecting cells with 0.1 ml of supernatant from the previous passage. Right panel: 9 × 105 CHO cells were infected with 9 × 105 PFU of FMDV MARLS, and passages were carried out as for the infections of BHK-21 cells. The multiplicity of infection at each passage can be calculated from the titers shown in ordinate. Preextinction populations are indicated by arrows. Viral extinction was ascertained by three additional blind passages in the absence of mutagen and inhibitors, with no evidence of infectivity and RT-PCR-amplifiable material in the supernatant of the third passage. All titrations were done in triplicate. Standard deviations (not included in the plots) never exceeded 15%.
High-fitness virus can be extinguished with the combination of a mutagen and two inhibitors.
The effect of FUG on FMDV C-S8c1 suggested that extinction of high-fitness MARLS in BHK-21 cells could be favored by decreases in the viral load achieved with the combination of two antiviral inhibitors targeted to different steps in the virus life cycle. To test this possibility, the the effect of combination of FU, G, and H (FUGH) on production of MARLS in BHK-21 cells was tested. The FUGH treatment resulted in a decrease of cell viability to about 20% of the untreated cells (Fig. 1). Control experiments (described in Materials and Methods) ruled out cytotoxicity as being responsible for the absence of viral production. The results (Fig. 4) show that a combination of two inhibitors and a mutagen can lead to extinction of MARLS in BHK-21 cells in three passages. In order to elucidate how systematic the extinctions were, 47 repetitions of the passages in the presence of FUGH were performed. In 40 cases extinction of MARLS was obtained in the third passage and in 7 cases in the fourth passage. Therefore, a combination of a mutagen and multiple inhibitors is effective in promoting systematic extinction of high-fitness FMDV.
Evidence for FU-induced mutations in a preextinction population and moderate increases in mutation frequency.
Consensus nucleotide sequences and sequences from molecular clones were obtained from the mixture of the supernatants of the 46 replicates of the C-S8c1FUGp1 preextinction population and C-S8c1DMEMp1 (Fig. 3). Three genomic regions were analyzed, the ones encoding the capsid protein VP1 and the nonstructural proteins 2C and 3D. Increases in mutation frequencies ranged between 1.5- and 4-fold; the maximum difference was found in 3D (Table 1) as in a previous report (60). The number of mutations observed in the C-S8c1FUGp1 population was significantly higher than that obtained with C-S8c1DMEMp1, as measured with the χ2 test (P < 0.005 and P > 0.001; χ2, 1 degree of freedom). The most abundant mutations found in the preextinction populations were the transitions A→G and U→C (Table 2), which have been associated with the mutagenic action of FU (37, 59, 72). The number of A→G and U→C transitions was found to be significantly higher than other mutation types with the χ2 test (P < 0.025 and P > 0.01; χ2, 1 degree of freedom). Increases were found in Shannon entropy, which is a measure of the different types of nucleotide sequences found in the mutant spectrum of the genomic region under study. Thus, in the three genomic regions analyzed, the mutant spectrum of the population near extinction was more complex than that in the corresponding control population (Table 1).
TABLE 1.
Genetic heterogeneity in the mutant spectrum of FMDV C-S8c1 populations subjected to one passage in DMEM or in FUGa
| C-S8c1 population | Encoded proteinb | No. of clonesc | No. of nucleotidesd | Mutation frequencye | Snf |
|---|---|---|---|---|---|
| DMEMp1 | VP1 | 25 | 16,075 | 5.0 × 10−4 (100) | 0.38 |
| 2C | 20 | 19,080 | 5.2 × 10−4 (80) | 0.56 | |
| 3D | 20 | 28,080 | 1.1 × 10−4 (67) | 0.20 | |
| FUGp1 | VP1 | 20 | 12,860 | 9.3 × 10−4 (50) | 0.54 |
| 2C | 20 | 19,080 | 7.9 × 10−4 (67) | 0.75 | |
| 3D | 19 | 26,676 | 4.5 × 10−4 (42) | 0.53 |
The populations analyzed and the antiviral treatments are described in Materials and Methods and in the legend for Fig. 3. C-S8c1FUGp1 is the preextinction population indicated with an arrow in Fig. 3. C-S8c1DMEMp1 is the population passaged in parallel in DMEM.
VP1 is encoded at positions 3193 to 3869, 2C at 4280 to 5349, and 3D at 6609 to 8035 of the FMDV genome; numbering is as in reference (65).
Number of cDNA clones in E. coli analyzed (the procedure is detailed in Materials and Methods).
Total number of nucleotides sequenced for each genomic region.
Number of different mutations found divided by the number of nucleotides sequenced (for each population and genomic region), expressed as substitutions per nucleotide. Mutations were counted comparing the sequence of each individual clone with the consensus sequence of the corresponding population. The percentage of nonsynonymous mutations is indicated in parenthesis.
TABLE 2.
Types of mutations in the mutant spectrum of FMDV C-S8c1 preextinction and control populationsa
| Mutation typeb | No. of mutations in C-S8c1 population
|
|
|---|---|---|
| DMEMp1 | FUGp1 | |
| A→C | 1 | 1 |
| A→G | 1 | 13 |
| A→U | 0 | 1 |
| C→A | 6 | 1 |
| C→G | 0 | 1 |
| C→U | 3 | 4 |
| G→A | 1 | 1 |
| G→C | 0 | 0 |
| G→U | 1 | 3 |
| U→A | 0 | 0 |
| U→C | 3 | 14 |
| U→G | 0 | 0 |
| Total | 16 | 39 |
Populations, nucleotides analyzed, number of clones, and treatment conditions are described in Materials and Methods, in footnotes a and c of Table 1, and in the legend for Fig. 3.
Mutations are those found in the analysis of the mutant spectra of the VP1-, 2C-, and 3D-coding regions of the indicated C-S8c1 populations.
DISCUSSION
The possibility of a new antiviral strategy based on increasing the mutation rate above a threshold value (16, 34, 36, 40, 41) stems from the quasispecies dynamics of RNA virus populations (21, 57, 64). Error rates during RNA genome replication dictate that viral genomes consist of a complex mutant spectrum often dominated by a most fit genome, termed the master sequence (21, 22). Error-prone replication predicts an error threshold relationship of the form
 |
1 |
in which vmax is the maximum length (information contents) that can be stably maintained in a viral genome, ς0 is the selective advantage (superiority) of the master sequence over the mutant spectrum, and q̄ is the average copying fidelity (in a scale from 0 to 1) during genome replication; therefore (1 − q̄) is the average error rate (21, 22, 57, 64). According to the error threshold relationship, an increase in the error rate above a threshold value should result in the loss of information carried by the viral genome and therefore in a loss of infectivity. Experimental support for this theoretical prediction has been obtained by subjecting vesicular stomatitis virus, poliovirus (10, 11, 34, 39), and human immunodeficiency virus type 1 (40) to increased levels of mutagenesis. In the case of FMDV we showed previously that low fitness and reduced viral loads favored viral extinction upon replication in the presence of FU or 5-azacytidine or their combination (59, 60). Relative fitness among viral populations is conceptually parallel to relative fitness among components of the mutant spectrum within a viral population. The parameter ς0 in equation 1 represents the superiority of the master sequence over its mutant spectrum, and its value is larger the higher the relative fitness of the mutant distribution (21, 22, 57). Therefore, virus extinction should be favored in populations with low relative fitness, as observed experimentally (59, 60).
Further evidence that low fitness rather than a specific genomic structure was responsible for virus extinction has been obtained with infection of CHO cells with MARLS. This virus showed low fitness in CHO, as evidenced both by a 10-fold-lower progeny production than in BHK-21 cells and a 10-fold increase in progeny production after eight serial passages in CHO cells (N. Pariente et al., unpublished results). MARLS was prone to extinction with a combination of mutagen and one inhibitor and with the mutagen alone in CHO cells but not in BHK-21 cells (compare the graphics in Fig. 4). The viral load also has a definite influence in the adaptation (fitness increase) of viral quasispecies. When the viral population size is small, genetic drift and a decrease in fitness prevail (8, 23, 73, 74), while when the replicative size of the same virus clones and populations is large, competitive selection of increasingly adapted mutant swarms leads to exponential increases in viral fitness (24, 46, 47, 69).
These previous theoretical and experimental observations suggested that a combination of a mutagenic agent and antiviral inhibitors should increase the frequency of viral extinctions. This has indeed been documented in the present report by using FMDV clones and populations differing by about 106-fold in relative fitness values. For the reference virus C-S8c1, whose relative fitness value is taken as 1 (23, 24), a combination of FU and G resulted in 47 extinction events out of 47 trials. For MARLS, which has a 130-fold-greater fitness than C-S8c1 in BHK-21 cells, two inhibitors were needed in combination with FU, to obtain viral extinction. This extinction was also obtained for each of 48 trials, in fewer than five passages. We term this occurrence systematic extinction, since chances of virus surviving for a larger number of passages under these adverse evolutionary conditions must be negligible. Not unexpectedly, clones whose fitness was 103- to 104-fold-lower than that of C-S8c1 did not survive even a single round of infection under the same conditions.
The mutant spectrum of an FMDV C-S8c1 preextinction population, subjected to passages in the presence of FUG, has been compared with the mutant spectrum of a C-S8c1 population passaged in DMEM. With the RT-PCR amplification system used, the mutation frequency values found in the mutant spectra analyzed cannot be affected by mutations introduced during the amplification procedures (1, 4, 59, 60). There was a significant bias toward the type of mutations induced by FU expected from the ambiguous reading of fluorouridine in template molecules (37, 59, 72). In the VP1-, 2C-and 3D-coding regions, 50, 67, and 42%, respectively, of the mutations were nonsynonymous (Table 1). The locations of amino acid replacements in VP1, 2C, and 3D are given in Table 3. Two amino acid replacements were found in the carboxy-terminal region of VP1 (antigenic site C [43]) (Q191→H and H197→R). In 2C, replacement R109→H affected the A domain, a Walker nucleoside triphosphate binding motif (49). In 3D, except for the T365→A change in β strand 4, which is a very conserved position among picornavirus polymerases (75), all other replacements were located on loops linking α helices and β strands, assuming that structural elements of poliovirus 3D (30) coincide with those of FMDV 3D upon alignment of the two amino acid sequences (42).
TABLE 3.
Amino acid replacements found in VP1, 2C, and 3D of the mutant spectrum of preextinction population C-S8c1FUGp1
| Protein | Amino acid replacementa | Structural or functional elementb |
|---|---|---|
| VP1 | P111→Q | l |
| F159→S | βH | |
| I169→V | βI | |
| Q191→H | l | |
| H197→R | l | |
| 2C | D56→G | N-terminus, amphipathic domain |
| I85→V | Unknown | |
| R109→H | Between the 2C loop and the A domain | |
| S112→P | A domain | |
| T135→A | Unknown | |
| D146→G | Unknown | |
| T213→A | Unknown | |
| R226→G | Unknown | |
| I248→T | Unknown | |
| K317→T | C-terminus, RNA binding domain | |
| 3D | V143→A | l |
| Q232→H | l | |
| I290→T | l | |
| T365→A | β4 | |
| I452→V | l |
The single-letter amino acid code is used; amino acids are numbered independently for each protein, as in (references 23, 24, 43, 44, 59, and 65).
Structural elements (β, β strand; 1, loop) of VP1 are assigned according to the three-dimensional structure of FMDV C-S8c1 (38); structural elements of 3D are based on the three-dimensional structure of poliovirus 3D (30), assuming that the equivalent positions of FMDV in an alignment of the two sequences (42) belong to the same structure. The assignment of functional domains of 2C are based on those described for poliovirus in references 28, and 49 and references therein; sequence identity was based in an alignment between 2C of poliovirus (66) and FMDV C-S8c1 (65) (N. Pariente, unpublished results).
One of the possible drawbacks of the combination therapy presented herein would be the appearance of guanidine-resistant FMDV mutants due to the action of FU. There have been several guanidine-resistant mutants of poliovirus described, and some of FMDV serotype O, and most of them involve transition mutations presumably favored by FU (50, 56). Nevertheless, none of the clones analyzed from a preextinction FMDV population showed mutations described as responsible for a guanidine-resistant phenotype, despite the fact that FMDV replication in the presence of G alone can result in selection of resistant mutants (55, N. Pariente et al., unpublished results). In case resistant mutants arose during treatments with mutagen and inhibitors, there would be a competition between the selection of the inhibitor-resistant mutant and the mutational force towards extinction. When such a force dominates, chances of selecting resistant mutants diminish, and this may explain why no G-resistant mutants were detected in the mutant spectra analyzed. The option of using two inhibitors that act on different steps of the viral life cycle reduces the possibility of the mutagen generating escape mutants. The FMDV-FUG or -FUGH combination system provides a simple cell culture model system for studying the dynamics of mutational pressure in relation to G-resistant or H-resistant mutant generation and efficiency of extinction. These studies are currently in progress.
The need of combination therapy with two or more inhibitors to limit the chances of generating and selecting inhibitor-resistant mutants in viral quasispecies has been emphasized (17, 19, 29, 33). Early experiments suggested a more effective control of influenza virus by a combined vaccine-antiviral strategy (32, 45, 70). In a conceptually parallel study, ribavirin (1-β-d-ribofuranosyl-1H-1,2,4-triazole-3-carboxamide) treatment prevented the appearance of neutralization-resistant mutants of lymphocytic choriomeningitis virus in mice (58). Recent reports (10, 11) have documented that ribavirin can be mutagenic for poliovirus and that in this system reduction of infectious virus production correlated with mutagenic activity of the nucleotide analog. These results were interpreted as suggesting that the antipoliovirus activity of ribavirin could be due to the transition of viral replication into error catastrophe (10, 11), although viral extinction was not observed. Ribavirin is used in the therapy of a number of viral infections (12, 14, 48, 61). Certainly the contribution of inhibition versus mutagenesis in the antiviral action of ribavirin deserves further investigation. Also, the possible contribution of inhibition of virus-specific RNA synthesis in the extinction by FU—suggested by the reduction in viral production in a single round of infection in the presence of FU (59, 60)—requires further investigation. Our observations on the benefits of a combination of a mutagenic agent and one or several antiviral inhibitors are consistent with current views on adaptability of viral quasispecies (8, 16, 21–24, 26, 46, 47, 69). The lesser the opportunity of a virus to replicate, the lower the chances of survival in the face of an antiviral response, be it natural (an immune response) or induced externally (through immune stimulation, immunotherapy, or drug administrations).
ACKNOWLEDGMENTS
We are indebted to C. Escarmís, C. M. Ruiz-Jarabo, and E. Baranowski for helpful discussions, J. C. de la Torre for the critical reading of the manuscript, and M. Dávila for technical assistance.
Research in Madrid was supported by grants PM97-0060-C02-01, EU FAIR 5 PL-97-3665, and Fundación Ramón Areces. N.P. was supported by a predoctoral fellowship from MEC (Spain), and S.S. was supported by a predoctoral fellowship from CAM. Work in Manchester was supported by a Sir Henry Wellcome award for innovative research (053995) to P.R.L. and E.D. and an International Research Collaboration grant from the Wellcome Trust (049862) to P.R.L. and E.D.
REFERENCES
- 1.Arias A, Lazaro E, Escarmis C, Domingo E. Molecular intermediates of fitness gain of an RNA virus: characterization of a mutant spectrum by biological and molecular cloning. J Gen Virol. 2001;82:1049–1060. doi: 10.1099/0022-1317-82-5-1049. [DOI] [PubMed] [Google Scholar]
- 2.Baranowski E, Ruíz-Jarabo C M, Sevilla N, Andreu D, Beck E, Domingo E. Cell recognition by foot-and-mouth disease virus that lacks the RGD integrin-binding motif: flexibility in aphthovirus receptor usage. J Virol. 2000;74:1641–1647. doi: 10.1128/jvi.74.4.1641-1647.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baranowski E, Sevilla N, Verdaguer N, Ruíz-Jarabo C M, Beck E, Domingo E. Multiple virulence determinants of foot-and-mouth disease virus in cell culture. J Virol. 1998;72:6362–6372. doi: 10.1128/jvi.72.8.6362-6372.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barnes W M. PCR amplification of up to 35-kb DNA with high fidelity and high yield from lambda bacteriophage templates. Proc Natl Acad Sci USA. 1994;91:2216–2220. doi: 10.1073/pnas.91.6.2216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Black D N, Brown F. Effect of actinomycin D and guanidine on the formation of a ribonucleic acid polymerase induced by foot-and-mouth-disease virus and on the replication of virus and viral ribonucleic acid. Biochem J. 1969;112:317–323. doi: 10.1042/bj1120317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caplen H, Peters C J, Bishop D H. Mutagen-directed attenuation of Rift Valley fever virus as a method for vaccine development. J Gen Virol. 1985;66:2271–2277. doi: 10.1099/0022-1317-66-10-2271. [DOI] [PubMed] [Google Scholar]
- 7.Carrasco L. Picornavirus inhibitors. Pharmacol Ther. 1994;64:215–290. doi: 10.1016/0163-7258(94)90040-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chao L. Fitness of RNA virus decreased by Muller's ratchet. Nature. 1990;348:454–455. doi: 10.1038/348454a0. [DOI] [PubMed] [Google Scholar]
- 9.Conrad H E. Heparin-binding proteins. San Diego, Calif: Academic Press; 1998. [Google Scholar]
- 10.Crotty S, Cameron C E, Andino R. RNA virus error catastrophe: direct molecular test by using ribavirin. Proc Natl Acad Sci USA. 2001;98:6895–6900. doi: 10.1073/pnas.111085598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crotty S, Maag D, Arnold J J, Zhong W, Lau J Y N, Hong Z, Andino R, Cameron C E. The broad-spectrum antiviral ribonucleotide, ribavirin, is an RNA virus mutagen. Nat Med. 2000;6:1375–1379. doi: 10.1038/82191. [DOI] [PubMed] [Google Scholar]
- 12.Davis G L, Esteban-Mur R, Rustgi V, Hoefs J, Gordon S C, Trepo C, Shiffman M L, Zeuzem S, Craxi A, Ling M H, Albrecht J. Interferon alfa-2b alone or in combination with ribavirin for the treatment of relapse of chronic hepatitis C. International Hepatitis Interventional Therapy Group. N Engl J Med. 1998;339:1493–1499. doi: 10.1056/NEJM199811193392102. [DOI] [PubMed] [Google Scholar]
- 13.Dawson W O. Guanidine inhibits tobacco mosaic virus RNA synthesis at two stages. Intervirology. 1975;6:83–89. doi: 10.1159/000149459. [DOI] [PubMed] [Google Scholar]
- 14.De Clercq E. Antiviral agents: characteristic activity spectrum depending on the molecular target with which they interact. Adv Virus Res. 1993;42:1–55. doi: 10.1016/s0065-3527(08)60082-2. [DOI] [PubMed] [Google Scholar]
- 15.de la Torre J C, Wimmer E, Holland J J. Very high frequency of reversion to guanidine resistance in clonal pools of guanidine-dependent type 1 poliovirus. J Virol. 1990;64:664–671. doi: 10.1128/jvi.64.2.664-671.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Domingo E. Viruses at the edge of adaptation. Virology. 2000;270:251–253. doi: 10.1006/viro.2000.0320. [DOI] [PubMed] [Google Scholar]
- 17.Domingo E, Biebricher C, Eigen M, Holland J J. Quasispecies and RNA virus evolution: principles and consequences. Austin, Tex: Landes Bioscience; 2001. [Google Scholar]
- 18.Domingo E, Dávila M, Ortín J. Nucleotide sequence heterogeneity of the RNA from a natural population of foot-and-mouth-disease virus. Gene. 1980;11:333–346. doi: 10.1016/0378-1119(80)90073-6. [DOI] [PubMed] [Google Scholar]
- 19.Domingo E, Holland J J. Complications of RNA heterogeneity for the engineering of virus vaccines and antiviral agents. Genet Eng (NY) 1992;14:13–31. doi: 10.1007/978-1-4615-3424-2_2. [DOI] [PubMed] [Google Scholar]
- 20.Eastman P S, Blair C D. Temperature-sensitive mutants of Japanese encephalitis virus. J Virol. 1985;55:611–616. doi: 10.1128/jvi.55.3.611-616.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eigen M, Biebricher C K. Sequence space and quasispecies distribution. In: Domingo E, Ahlquist P, Holland J J, editors. RNA genetics. Vol. 3. Boca Raton, Fla: CRC Press; 1988. pp. 211–245. [Google Scholar]
- 22.Eigen M, Schuster P. The hypercycle. A principle of natural self-organization. Berlin, Germany: Springer; 1979. [DOI] [PubMed] [Google Scholar]
- 23.Escarmís C, Dávila M, Charpentier N, Bracho A, Moya A, Domingo E. Genetic lesions associated with Muller's ratchet in an RNA virus. J Mol Biol. 1996;264:255–267. doi: 10.1006/jmbi.1996.0639. [DOI] [PubMed] [Google Scholar]
- 24.Escarmís C, Dávila M, Domingo E. Multiple molecular pathways for fitness recovery of an RNA virus debilitated by operation of Muller's ratchet. J Mol Biol. 1999;285:495–505. doi: 10.1006/jmbi.1998.2366. [DOI] [PubMed] [Google Scholar]
- 25.Esko J D, Stewart T E, Taylor W H. Animal cell mutants defective in glycosaminoglycan biosynthesis. Proc Natl Acad Sci USA. 1985;82:3197–3201. doi: 10.1073/pnas.82.10.3197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Flint S J, Enquist L W, Krug R M, Racaniello V R, Skalka A M. Virology. Molecular biology, pathogenesis, and control. Washington D.C.: ASM Press; 2000. [Google Scholar]
- 27.Friedman R M. Basis for variable response of arboviruses to guanidine treatment. J Virol. 1970;6:628–636. doi: 10.1128/jvi.6.5.628-636.1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goodfellow L, Chaudhry Y, Richardson A, Meredith J, Almond J W, Barclay W, Evans D J. Identification of a cis-acting replication element within the poliovirus coding region. J Virol. 2000;74:4590–4600. doi: 10.1128/jvi.74.10.4590-4600.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hammer S M, Squires K E, Hughes M D, Grimes J M, Demeter L M, Currier J S, Eron J J, Jr, Feinberg J E, Balfour H H, Jr, Deyton L R, Chodakewitz J A, Fischl M A. A controlled trial of two nucleoside analogues plus indinavir in persons with human immunodeficiency virus infection and CD4 cell counts of 200 per cubic millimeter or less. AIDS Clinical Trials Group 320 Study Team. N Engl J Med. 1997;337:725–733. doi: 10.1056/NEJM199709113371101. [DOI] [PubMed] [Google Scholar]
- 30.Hansen J, Long A M, Schultz S. Structure of the RNA-dependent RNA polymerase of poliovirus. Structure. 1997;15:1109–1122. doi: 10.1016/s0969-2126(97)00261-x. [DOI] [PubMed] [Google Scholar]
- 31.Haspel M V, Lampert P W, Oldstone M B. Temperature-sensitive mutants of mouse hepatitis virus produce a high incidence of demyelination. Proc Natl Acad Sci USA. 1978;75:4033–4036. doi: 10.1073/pnas.75.8.4033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hayden F G. Combinations of antiviral agents for treatment of influenza virus infections. J Antimicrob Chemother. 1986;18:177–183. doi: 10.1093/jac/18.supplement_b.177. [DOI] [PubMed] [Google Scholar]
- 33.Ho D D. Toward HIV eradication or remission: the tasks ahead. Science. 1998;280:1866–1867. doi: 10.1126/science.280.5371.1866. [DOI] [PubMed] [Google Scholar]
- 34.Holland J J, Domingo E, de la Torre J C, Steinhauer D A. Mutation frequencies at defined single codon sites in vesicular stomatitis virus and poliovirus can be increased only slightly by chemical mutagenesis. J Virol. 1990;64:3960–3962. doi: 10.1128/jvi.64.8.3960-3962.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jackson T, Ellard F M, Ghazaleh R A, Brookes S M, Blakemore W E, Corteyn A H, Stuart D L, Newman J W, King A M. Efficient infection of cells in culture by type O foot-and-mouth disease virus requires binding to cell surface heparan sulfate. J Virol. 1996;70:5282–5287. doi: 10.1128/jvi.70.8.5282-5287.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ji J, Hoffmann J S, Loeh L. Mutagenicity and pausing of HIV reverse transcriptase during HIV plus-strand DNA synthesis. Nucleic Acids Res. 1994;22:47–52. doi: 10.1093/nar/22.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kunz B A, Kohalmi S E. Modulation of mutagenesis by deoxyribonucleotide levels. Annu Rev Genet. 1991;25:339–359. doi: 10.1146/annurev.ge.25.120191.002011. [DOI] [PubMed] [Google Scholar]
- 38.Lea S, Hernández J, Blakemore W, Brocchi E, Curry S, Domingo E, Fry E, Abu-Ghazaleh R, King A, Newman J, Stuart D, Mateu M G. The structure and antigenicity of a type C foot-and-mouth disease virus. Structure. 1994;2:123–139. doi: 10.1016/s0969-2126(00)00014-9. [DOI] [PubMed] [Google Scholar]
- 39.Lee C H, Gilbertson D L, Novella I S, Huerta R, Domingo E, Holland J J. Negative effects of chemical mutagenesis on the adaptive behavior of vesicular stomatitis virus. J Virol. 1997;71:3636–3640. doi: 10.1128/jvi.71.5.3636-3640.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Loeb L A, Essigmann J M, Kazazi F, Zhang J, Rose K D, Mullins J I. Lethal mutagenesis of HIV with mutagenic nucleoside analogs. Proc Natl Acad Sci USA. 1999;96:1492–1497. doi: 10.1073/pnas.96.4.1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Loeb L A, Mullins J I. Lethal mutagenesis of HIV by mutagenic ribonucleoside analogs. AIDS Res Hum Retrovir. 2000;13:1–3. doi: 10.1089/088922200309539. [DOI] [PubMed] [Google Scholar]
- 42.Martínez-Salas E, Ortín J, Domingo E. Sequence of the viral replicase gene from foot-and-mouth disease virus C1-Santa Pau (C-S8) Gene. 1985;35:55–61. doi: 10.1016/0378-1119(85)90157-x. [DOI] [PubMed] [Google Scholar]
- 43.Mateu M G. Antibody recognition of picornaviruses and escape from neutralization: a structural view. Virus Res. 1995;38:1–24. doi: 10.1016/0168-1702(95)00048-u. [DOI] [PubMed] [Google Scholar]
- 44.Mateu M G, Martinez M A, Capucci L, Andreu D, Giralt E, Sobrino F, Brocchi E, Domingo E. A single amino acid substitution affects multiple overlapping epitopes in the major antigenic site of foot-and-mouth disease virus of serotype C. J Gen Virol. 1990;71:629–637. doi: 10.1099/0022-1317-71-3-629. [DOI] [PubMed] [Google Scholar]
- 45.Murphy B R, Webster R G. Orthomyxoviruses. In: Fields B M, editor. Fields virology. Philadelphia, Pa: Lippincott-Ravel Publishers; 1996. pp. 1397–1445. [Google Scholar]
- 46.Novella I S, Duarte E A, Elena S F, Moya A, Domingo E, Holland J J. Exponential increases of RNA virus fitness during large population transmissions. Proc Natl Acad Sci USA. 1995;92:5841–5844. doi: 10.1073/pnas.92.13.5841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Novella I S, Hershey C L, Escarmis C, Domingo E, Holland J J. Lack of evolutionary stasis during alternating replication of an arbovirus in insect and mammalian cells. J Mol Biol. 1999;287:459–465. doi: 10.1006/jmbi.1999.2635. [DOI] [PubMed] [Google Scholar]
- 48.Pawlotsky J M. Hepatitis C virus resistance to antiviral therapy. Hepatology. 2000;32:889–896. doi: 10.1053/jhep.2000.19150. [DOI] [PubMed] [Google Scholar]
- 49.Pfister T, Wimmer E. Characterization of the nucleoside triphosphatase activity of poliovirus protein 2C reveals a mechanism by which guanidine inhibits poliovirus replication. J Biol Chem. 1999;274:6992–7001. doi: 10.1074/jbc.274.11.6992. [DOI] [PubMed] [Google Scholar]
- 50.Pincus S E, Wimmer E. Production of guanidine-resistant and -dependent poliovirus mutants from cloned cDNA: mutations in polypeptide 2C are directly responsible for altered guanidine sensitivity. J Virol. 1986;60:793–796. doi: 10.1128/jvi.60.2.793-796.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pringle C R. Genetic characteristics of conditional lethal mutants of vesicular stomatitis virus induced by 5-fluorouracil, 5-azacytidine, and ethyl methane sulfonate. J Virol. 1970;5:559–567. doi: 10.1128/jvi.5.5.559-567.1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Righstel W A, Dice J R, McAlpine R J, Timm E A, McLean I W J, Dixon G J, Schabel F M J. Antiviral effect of guanidine. Science. 1961;134:558–559. doi: 10.1126/science.134.3478.558. [DOI] [PubMed] [Google Scholar]
- 53.Riviere Y, Oldstone M B A. Genetic reassortants of lymphocytic choriomeningitis virus: unexpected disease and mechanism of pathogenesis. J Virol. 1986;59:363–368. doi: 10.1128/jvi.59.2.363-368.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sa-Carvalho D, Rieder E, Baxt B, Rodarte R, Tanuri A, Mason P W. Tissue culture adaptation of foot-and-mouth disease virus selects viruses that bind to heparin and are attenuated in cattle. J Virol. 1997;71:5115–5123. doi: 10.1128/jvi.71.7.5115-5123.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Saunders K, King A M. Guanidine-resistant mutants of aphthovirus induce the synthesis of an altered nonstructural polypeptide, P34. J Virol. 1982;42:389–394. doi: 10.1128/jvi.42.2.389-394.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Saunders K, King A M, McCahon D, Newman J W, Slade W R, Forss S. Recombination and oligonucleotide analysis of guanidine-resistant foot-and-mouth disease virus mutants. J Virol. 1985;56:921–929. doi: 10.1128/jvi.56.3.921-929.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Schuster P, Stadler P F. Nature and evolution of early replicons. In: Domingo E, Webster R G, Holland J J, editors. Origin and evolution of viruses. San Diego, Calif: Academic Press; 1999. pp. 1–24. [Google Scholar]
- 58.Seiler P, Senn B M, Klenerman P, Kalinke U, Hengartner H, Zinkernagel R M. Additive effect of neutralizing antibody and antiviral drug treatment in preventing virus escape and persistence. J Virol. 2000;74:5896–5901. doi: 10.1128/jvi.74.13.5896-5901.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sierra S. Caracterización de la respuesta del virus de la fiebre aftosa a mutagénesis química. Tesis Doctoral. Ph.D. Thesis. Madrid, Spain: Universidad Autónoma de Madrid; 2001. [Google Scholar]
- 60.Sierra S, Dávila M, Lowenstein P R, Domingo E. Response of foot-and-mouth disease virus to increased mutagenesis. Influence of viral load and fitness in loss of infectivity. J Virol. 2000;74:8316–8323. doi: 10.1128/jvi.74.18.8316-8323.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Smith R A, Kirkpatrick W. Ribavirin: a broad spectrum antiviral agent. New York, N.Y: Academic Press, Inc.; 1980. [Google Scholar]
- 62.Sobrino F, Dávila M, Ortín J, Domingo E. Multiple genetic variants arise in the course of replication of foot-and-mouth disease virus in cell culture. Virology. 1983;128:310–318. doi: 10.1016/0042-6822(83)90258-1. [DOI] [PubMed] [Google Scholar]
- 63.Sobrino F, Sáiz M, Jiménez-Clavero M A, Núñez J L, Rosas M F, Baranowski E, Ley V. Foot-and-mouth disease virus: a long known virus, but a current threat. Vet Res. 2001;32:1–30. doi: 10.1051/vetres:2001106. [DOI] [PubMed] [Google Scholar]
- 64.Swetina J, Schuster P. Self-replication with errors. A model for polynucleotide replication. Biophys Chem. 1982;16:329–345. doi: 10.1016/0301-4622(82)87037-3. [DOI] [PubMed] [Google Scholar]
- 65.Toja M, Escarmis C, Domingo E. Genomic nucleotide sequence of a foot-and-mouth disease virus clone and its persistent derivatives. Implications for the evolution of viral quasispecies during a persistent infection. Virus Res. 1999;64:161–171. doi: 10.1016/s0168-1702(99)00089-1. [DOI] [PubMed] [Google Scholar]
- 66.Toyoda H, Kohara M, Kataoka Y, Suganuma T, Omata T, Imura N, Nomoto A. Complete nucleotide sequences of all three poliovirus serotype genomes. Implication for genetic relationship, gene function and antigenic determinants. J Mol Biol. 1984;174:561–585. doi: 10.1016/0022-2836(84)90084-6. [DOI] [PubMed] [Google Scholar]
- 67.Varma J P. Inhibition of tobacco necrosis virus by guanidine carbonate. Virology. 1968;36:305–308. doi: 10.1016/0042-6822(68)90149-9. [DOI] [PubMed] [Google Scholar]
- 68.Volkenstein M V. Physical approaches to biological evolution. Berlin, Germany: Springer-Verlag; 1994. [Google Scholar]
- 69.Weaver S C, Brault A C, Kang W, Holland J J. Genetic and fitness changes accompanying adaptation of an arbovirus to vertebrate and invertebrate cells. J Virol. 1999;73:4316–4326. doi: 10.1128/jvi.73.5.4316-4326.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Webster R G, Kawaoka Y, Bean W J. Vaccination as a strategy to reduce the emergence of amantadine- and rimantadine-resistant strains of A/Chick/Pennsylvania/83 (H5N2) influenza virus. J Antimicrob Chemother. 1986;18:157–164. doi: 10.1093/jac/18.supplement_b.157. [DOI] [PubMed] [Google Scholar]
- 71.Wittmann H G, Wittmann-Liebold B. Protein chemical studies of two RNA viruses and their mutants. Cold Spring Harbor Symp Quant Biol. 1966;31:163–172. doi: 10.1101/sqb.1966.031.01.024. [DOI] [PubMed] [Google Scholar]
- 72.Yu H, Eritja R, Bloom L B, Goodman M F. Ionization of bromouracil and fluorouracil stimulates base mispairing frequencies with guanine. J Biol Chem. 1993;268:15935–15943. [PubMed] [Google Scholar]
- 73.Yuste E, Lopez-Galindez C, Domingo E. Unusual distribution of mutations associated with serial bottleneck passages of human immunodeficiency virus type 1. J Virol. 2000;74:9546–9552. doi: 10.1128/jvi.74.20.9546-9552.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yuste E, Sánchez-Palomino S, Casado C, Domingo E, López-Galíndez C. Drastic fitness loss in human immunodeficiency virus type 1 upon serial bottleneck events. J Virol. 1999;73:2745–2751. doi: 10.1128/jvi.73.4.2745-2751.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zimmern D. Evolution of RNA viruses. In: Domingo E, Holland J J, Ahlquist P, editors. RNA Genetics. Vol. 2. Boca Raton, Fla: CRC Press Inc.; 1988. pp. 211–240. [Google Scholar]