Abstract
Introduction
Conventional nasolabial flap has been widely used for reconstruction for head and neck defects. Recent decades witnessed modification of this flap like islanded version based on subcutaneous pedicle or facial artery and vein. The later modification obviated a need for pedicle division, secondary procedures and facilitates reach of the flap to distant sites. Especially, the islanded nasolabial flap pedicled on facial artery and vein can have a long pedicle to conveniently reach the tongue, floor of mouth when the flap is routed through retromandibular area.
Methods
A retrospective analysis was done on 14 patients analyzing the functional outcome like deglutition, speech, and aesthetic outcome of flap donor area, recruiting patients in which islanded nasolabial flap was done based on facial vessels for early stages of cancer tongue and lip.
Results
In our series of 14 operated cases, all flaps survived. All the flaps were islanded over the skeletonized facial artery and vein. Tip necrosis occurred in one case. The donor site was closed primarily in all cases. The average speech scoring was grade five, Vancouver scar score of the flap donor area was 2.5 and intelligible speech was difficult in only three cases in follow up.
Conclusion
We found this flap useful for reconstruction of small to moderate size defects of oral malignancy following excision with acceptable aesthetic and functional outcome in most of the patients.
Keywords: Oral cancer reconstruction, Islanded nasolabial flap, Nasolabial flap, Functional outcomes
Introduction
Surgical excision is the mainstay of treatment for head and neck cancer. Tumor extirpation leads to significant functional morbidity, cosmetic disfigurement, along with anatomical distortion of the resected structures. Reconstruction provides a solution or betterment in restoring form, function, and aesthetics. Reconstruction of head and neck region is challenging. Microvascular tissue transfer has revolutionized the head and neck reconstruction. Many a times oral cavity soft tissue defects are of limited size to justify a large dimension free tissue transfer for reconstruction and on the other hand also preclude primary closure. In such scenario considering a local flap may be prudent alternative to the free flap. The conventional nasolabial flap serves to reconstruct small to moderate size defects with limited accessibility to distant areas, the need for pedicle division and de-epithelialization of a portion of the flap depending on the location of defect.
The islanded modification of this flap based on facial artery and vein helps the reach of the flap to different defect location of the tongue, cheek, lip easier including the definitive blood supply, thus a useful reconstructive tool for these areas. In this article we share our experience and analyze the outcome of reconstruction with islanded pedicled nasolabial flap recruited in a series of cases of tongue and lip defects.
Methods
This retrospective analysis was done on the patients reconstructed with islanded nasolabial flap for head and neck reconstruction from January 2021 to January 2023. Out of 14 patients, 11 were male and 3 females with age between 22 and 63 years. In this series, 12 patients had tongue defects and two patients with lip defects. The reconstruction procedure was done by the Plastic surgery team, following the excision of the tumor by ENT team. The patient demographic details, TNM tumor staging, histopathology of the lesion, procedure performed, and flap size were noted (Table 1). Post operatively, patients were followed up at 1 month,3 month and 6 months interval. Vancouver scar scoring of the flap donor site and functional outcome analysis by assessing the speech and dysphagia was done. (Table 2, 3, 4) [1].
Table 1.
Details of the operated cases
| S. NO. | Age(years)Gender | Diagnosis | Stage of tumor | Procedure done | Histopathology | Speech score | Dysphagia score | Scar score | Flap size |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 63/Male | Carcinoma lower lip | T2N0M0 | WLE + SLND 1–3 + IPNLF | Well differentiated squamous cell carcinoma | 6 | 1 | 4 | 5 × 3.7.0 cm |
| 2 | 44/Female | Carcinoma left lateral border of tongue | T2N1M0 | WLE + SLND1-4 + IPNLF | Moderately differentiated squamous cell carcinoma | 6 | 4 | 7 | 6.0 × 4.0 cm |
| 3 | 22/Male |
Verrucous Lesion left Lateral BorderOf tongue |
WLE + IPNLF | Verrucous hyperplasia with ulcero inflammatory pathology | 6 | 1 | 3 | 5.5 × 3.2 cm | |
| 4 | 41/Male | Carcinoma left lateral border of tongue | T2N2M0 | WLE + MRND Type 3 + IPNLF + Tracheostomy | Moderately differentiated squamous cell carcinoma | 3 | 4 | 3 | 5.6 × 4.0 cm |
| 5 | 37/Male | Carcinoma right lateral border of tongue | T2N0M0 | WLE + IPNLF | Moderately differentiated squamous cell carcinoma | 3 | 3 | 2 | 6.5 × 4.0 cm |
| 6 | 47/Female | Carcinoma right lateral border of tongue | T2N0M0 | WLE + SLND1-4 + Right IPNLF | Moderately differentiated squamous cell carcinoma | 4 | 1 | 3 | 6.2 × 3.8 cm |
| 7 | 50/Male | Carcinoma left lateral border of tongue | T2N0M0 | WLE + SLND 1–3 + Left IPNLF | Moderately differentiated squamous cell carcinoma | 6 | 1 | 2 | 6 × 3.7 cm |
| 8 | 40/Male | Carcinoma left lateral border of tongue | T2N0M0 | WLE + Left SLND1-4 + Right SLND1-3 + IPNLF | Well differentiated squamous cell carcinoma | 4 | 6 | 1 | 7.0 × 4.0 cm |
| 9 | 33/Male | Carcinoma right lateral border of tongue | T2N0M0 | WLE + SLND 1–3 + IPNLF + Tracheostomy | Moderately differentiated squamous cell carcinoma | 6 | 4 | 2 | 5.0 × 3.2 cm |
| 10 | 32/Male | Carcinoma left lateral border of tongue | T3N2CM0 | WLE + Right SND 1–4 + Contralateral IPNLF + Tracheostomy | Moderately differentiated scc | 3 | 3 | 2 | 5.2 × 3.0 cm |
| 11 | 45/Male | Carcinoma right lateral border of tongue | T2N1M0 | WLE + Right SOND + IPLNF | Moderately differentiated squamous cell carcinoma | 4 | 3 | 2 | 6.8 × 3.5 cm |
| 12 | 34/Male | Carcinoma.right lateral border of tongue | T2N0M0 | WLE + SOND + IPNLF | Well differentiated squamous cell carcinoma | 6 | 3 | 2 | 6.0 × 3.2 cm |
| 13 | 35/Male | Carcinoma right lateral border of tongue | T2N0M0 | WLE + SOND + IPNLF | Well differentiated squamous cell carcinoma | 6 | 3 | 1 | 5.0 cm X 2 8 cm |
| 14 | 62/Female | Carcinoma.lower lip | T2N0M0 | WLE + SOND + IPNLF | Well differentiated squamous cell carcinoma | 7 | 1 | 1 | 5.0 × 3.0 cm |
WLE: Wide local excision
SOND: Supraomohyoid neck dissection
SLND: Selective lymph node dissection
MRND: Modified radical neck dissection
IPNLF: Islanded pedicled Nasolabial flap
Table 2.
Assessment of dysphagia
| Grade-1 | No complain in swallowing |
|---|---|
| Grade-2 | Minimal complaints, able to swallow without difficulty with bolus. |
| Grade-3 | Minimal complaints, able to swallow without difficulty without bolus. |
| Grade-4 | Moderate complaints and difficulty swallowing with bolus |
| Grade-5 | Moderate complaint and difficulty swallowing without bolus |
| Grade-6 | Severe complaints with difficulty in swallowing with or without bolus |
| Grade-7 | Severe complaints, unable to swallow |
Table 3.
Assessment of speech
| Grade-1 | Speech is unintelligible |
|---|---|
| Grade-2 | Speech is usually unintelligible |
| Grade-3 | Speech intelligibility is difficult |
| Grade-4 | Speech is intelligible with careful listening |
| Grade-5 | Speech is intelligible although noticeably in error |
| Grade-6 | Sound errors are occasionally noticed in continuous speech |
| Grade-7 | No sound errors were noticed in continuous speech |
Table 4.
Vancouver scar scoring
| Scar Characteristic | Score |
|---|---|
| Vascularity | |
| Normal | 0 |
| Pink | 1 |
| Red | 2 |
| Purple | 3 |
| Pigmentation | |
| Normal | 0 |
| Hypopigmentation | 1 |
| Hyperpigmentation | 2 |
| Pliability | |
| Normal | 0 |
| Supple | 1 |
| Yielding | 2 |
| Firm | 3 |
| Ropes | 4 |
| Contracture | 5 |
| Height (mm) | |
| Flat | 0 |
| <2 | 1 |
| 2–5 | 2 |
| >5 | 3 |
| Total Score | 13 |
Results
At 6 months follow up average speech scoring was grade five and in approximately (20%)three patients’ intelligible speech was difficult. The average score for dysphagia was three in carcinoma tongue patients at 6 months. Except for one patient, dysphagia was not a major complaint. The average Vancouver scar score of the flap donor area was 2.5. In 12 out of 14 (85%) patients it was below or equal to 3 and thus aesthetically acceptable. Complications like deviation of angle of mouth seen in one case, asymmetric animation of the ipsilateral lip and upward deviation on attempt to smile was observed in two cases. With lip split to approach the tumor, marginal necrosis of the ipsilateral lip was seen in two cases, maybe due to sacrifice of the labial branches, while harvesting the flap. However, this healed by secondary intention. In our series all flaps survived, though tip necrosis was observed in one case. The maximum and minimum dimension of the harvested flap was 7 × 4cm2 5 × 2.8 cm2 respectively. The donor site was closed primarily in all cases. All the flaps were islanded over the skeletonized facial artery and vein. The average duration of flap harvest was 1 h and 15 min with a range of 50 min to 90 min.
Surgical Technique
Before flap harvest a pattern/template of tongue or lip defect was made and marked at the nasolabial area. The facial artery and vein were isolated through an incision made over the pre-masseteric area at the lower border of mandible deep to the muscle plane. Then flap harvest was done from superior to inferior direction in a sub muscular plane including the facial artery and vein, the superior limit being at least 1.5 cm below the medial canthus. While raising the flap paddle, parotid duct, buccal branches of facial nerve were protected. Care was taken to prevent injury to the marginal mandibular nerve while dissecting facial artery and vein at lower border of mandible. The marginal mandibular nerve is usually found superficial to facial vessels. Through a space created between the nerve and mandible, the flap is delivered to the submandibular area in the neck. The donor site was closed primarily in layers, deep dermal closure done with 4 − 0 vicryl and skin approximated with 5 − 0 prolene sutures. In 12 cases for tongue defect reconstruction, the flap pedicle consisting of the facial artery and vein was dissected up to the origin in neck, getting a pedicle length of approximately 6–7 cm and the flap was tunneled through retromandibular route to reach the defect. While passing the flap through retromandibular area, care is taken to avoid twists in the pedicle. The pedicle length can be increased by meticulous dissection of the facial artery from submandibular gland by clipping its branches and dissection of facial vein up to internal jugular vein. Sacrificing the facial artery on one side has no effect on the face vascularity. In other two cases of lip defect reconstruction, the flap was islanded, facial artery and vein were skeletonized, and passed through a subcutaneous tunnel to reach the defect. For lip and adjacent cheek, alveolus defects, the flap is routed through subcutaneous route; not through retro mandibular route.
Discussion
The indication of reconstruction in head neck defects cannot be overemphasized and even a small size soft tissue defect in the oral cavity needs to be reconstructed to avoid functional morbidities like trismus, difficulty in speech deglutition, microstomia [2, 3]. Especially when mobile structures like tongue, lip, floor of the mouth are concerned, before reconstruction, the defects should be judged properly. Reconstruction should restore volume and mobility of tongue for optimal functional outcome [2, 3]. Tight closure and skin grafting following cancer excision though easy to perform have deleterious effects and disadvantages like reduced mobility and pronunciation due to scarring and tethering [4]. Microvascular tissue transfers certainly made a significant difference in outcome and efficiently addressed the reconstructive goals [3, 5, 6]. These are time taking procedures and needs expertise in microsurgery and increases the cost of treatment due to prolong hospital stay. For a resource constrained, high volume set up alternative options like local flaps serving the reconstruction goals are preferable for small to moderate defects. Conventional nasolabial flaps used for facial and oral cavity reconstruction have limited reach to oral cavity with a subcutaneous pedicle which needs to be divided [7]. Also, to avoid pedicle compression and bite of the pedicle while passing above the mandible, teeth extraction may be needed [8]. The de-epithelialization of part of conventional nasolabial flap paddle makes the effective skin paddle dimension smaller for reconstruction. The advantages of the modification of nasolabial flap are worth mentioning. The facial artery and vein incorporated with this flap can be dissected up to the origin in the neck gaining a pedicle length of 6–7 cm. This allows the flap to pass through the retromandibular area to reach intra oral sites like floor, ipsilateral tongue, cheek, and even contra lateral tongue defects without a stretch of the pedicle. In case of sacrifice of ipsilateral facial artery during ipsilateral neck dissection, contralateral nasolabial flap may be harvested and can be used for contralateral tongue defect (Fig. 1) [9]. Islanded flap has sufficient pedicle length for comfortable positioning and inset of the flap to the mobile structure like tongue avoiding tethering (Fig. 2). The restriction of tongue mobility is less affected with this modality of reconstruction and speech, deglutition outcomes are better than the conventional nasolabial flap. By islanding the flap over skeletonized facial artery and vein mimics a small free flap with robust vascularity, easy passage through retro mandibular area and orienting and inserting the flap as per the defect locations without a need for micro vascular anastomosis and de-epithelialization. Microvascular skill and set up is not required to carry out this flap reconstruction so also flap monitoring at regular intervals. The trainees and beginners can easily execute this flap with less intra operative time. Since the flap donor and recipient areas are on same operative field, no separate team is needed for closure of donor site. A flap width of size 4 cm. can be closed primarily with acceptable a scar line over the nasolabial fold.
Fig. 1.
1a Squamous cell carcinoma anterior part of the left side tongue. 1b Right side Islanded nasolabial flap elevated over facial vessels. 1c Flap insetted to the contralateral tongue defect. 1d Flap well settled over the contralateral tongue. 1e Follow up nasolabial scar
Fig. 2.
2a Squamous cell carcinoma of lateral border of tongue. 2b Islanded nasolabial flap elevated over facial vessels and delivered in the neck dissection area. 2c Intra -operative photo showing flap insetted to the tongue defect. 2d Follow up photo with scar at the nasolabial fold. 2e Follow up photo showing flap well settled on the tongue
For full thickness lip defects as in Fig. 3 after cancer resection, islanded nasolabial flap is a superior alternative to local flap options like, Abbe, Estlander or Karapandzic flap, as borrowing tissue from lip lead to variable degree of microstomia and two stages are necessary in some of the local flaps. A transposition nasolabial flap is well described for lower lip defects, but for defects preserving the lip commissure, the islanded modification better suits to the defect without distorting the commissure architecture. Islanded nasolabial flap provides sufficient tissue for subtotal to total lip defects with lip competency and speech outcome.
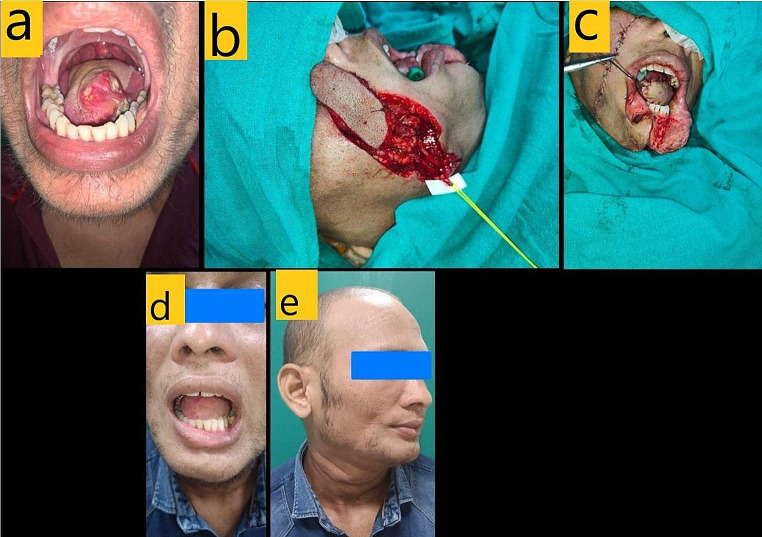
Fig. 3.
3a Squamous cell carcinoma lower lip. 3a Lip defect after excision of the lesion. 3c Flap subcutaneously tunneled and insetted after elevation. 3d Follow-up photo with flap well settle. 3e Follow-up photo with flap well settled with mouth open
Among the local flap, submental flap is be used for tongue defect but the lymph node clearance at 1a zone will be compromised to preserve the submental branch. Facial artery musculo mucosal flap and palatal flap have limited tissue content and reach for defect location over tongue, floor of mouth and lip. Regional flap like PMMC flap is bulky thus not suitable when functional outcomes like speech, deglutition are kept in mind.
Islanded pedicled flap has certain limitations. The main drawback is its limited size and bulk. This modification of inferiorly based islanded nasolabial flap can only be carried out when the facial vessels are not adhered to involved IB lymph nodes and preserved during neck dissection. Before harvesting the modified nasolabial flaps, the continuity and patency of facial vessels must be checked with handheld doppler or non-ligation of the same should be confirmed during neck dissection. Also, this inferiorly based version has a limited reach to the upper part of oral cavity. The flap cannot be executed in advanced cheek cancers where the nasolabial skin is excised along with the tumor.
Our study has similar outcome in terms of flap survivability, orocutaneous fistula as that of Saha et al. and Chakraborty et al. [10, 11]. Liquid diet was started on day 4 and soft diet on day 7 post operatively. The average stay of the non tracheo-stomized patients was 7 days which is much less in comparison to free flaps (15 days) in our set up.
Conclusion
The inferiorly based islanded nasolabial flap on facial vessels is a useful versatile flap for small to moderate size oral cavity defects. The head and neck reconstruction team should be aware of this modification and versed with flap harvest technique. Robust blood supply, easy execution with less intra -operative time make this flap a suitable option in a resource constrained and busy set up. Considering minimal donor site morbidity with good functional outcome; this can be opted as first choice for small to moderate size defects of lip, intra oral area within its reach in early stages of malignancy.
Author contributions
Dr Jiten Kumar Mishra, Dr Shamendra Anand Sahu, Dr Ripu Daman Arora: Concept, Design, writing, supervision. Dr Abi Sindhuja, Dr Karthik Nagaraja Rao: Writing, Literature search, Analysis, Interpretation.
Funding
No funding was received to assist with the preparation of this manuscript.
Declarations
Competing interests
Authors have no financial interests that are directly or indirectly related to the work submitted for publication.
Human and animal rights
The research involved human Participants, and well-informed consent was taken from everyone. The exemption from the ethical committee review was obtained in view of the retrospective study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Teichgraeber J, Bowman J, Goepfert H (1985) New test series for the functional evaluation of oral cavity cancer. Head Neck Surg 8(1):9–20 [DOI] [PubMed] [Google Scholar]
- 2.Ji YB, Cho YH, Song CM, Kim YH, Kim JT, Ahn HC et al (2017) Long-term functional outcomes after resection of tongue cancer: determining the optimal reconstruction method. Eur Arch Oto-Rhino-Laryngol off J Eur Fed Oto-Rhino-Laryngol soc EUFOS Affil Ger soc Oto-Rhino-Laryngol -. Head Neck Surg 274(10):3751–3756 [DOI] [PubMed] [Google Scholar]
- 3.Lam L, Samman N (2013) Speech and swallowing following tongue cancer surgery and free flap reconstruction–a systematic review. Oral Oncol 49(6):507–524 [DOI] [PubMed] [Google Scholar]
- 4.López-Jornet P, Camacho-Alonso F (2013) Comparison of pain and swelling after removal of oral leukoplakia with CO2 laser and cold knife: a randomized clinical trial. Med Oral Patol Oral Cir Bucal 18(1):e38–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nakatsuka T, Harii K, Asato H, Takushima A, Ebihara S, Kimata Y et al (2003) Analytic review of 2372 free flap transfers for head and neck reconstruction following cancer resection. J Reconstr Microsurg 19(6):363–368 discussion 369 [DOI] [PubMed] [Google Scholar]
- 6.Eckardt A, Meyer A, Laas U, Hausamen JE (2007) Reconstruction of defects in the head and neck with free flaps: 20 years experience. Br J Oral Maxillofac Surg 45(1):11–15 [DOI] [PubMed] [Google Scholar]
- 7.Varghese BT, Sebastian P, Cherian T, Mohan PM, Ahmed I, Koshy CM, Thomas S (2001) Nasolabial flaps in oral reconstruction: an analysis of 224 cases. Br J Plast Surg 54(6):499–503 [DOI] [PubMed] [Google Scholar]
- 8.Kallappa S, Shah N (2019) Outcome of Nasolabial Flap in the Reconstruction of Head and Neck defects. Indian J Surg Oncol 10(4):577–581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nueangkhota P, Liang Y, jie, Zheng G sen, Su Y, xiong, Yang W (2016) fa, Liao G qing. Reconstruction of Tongue Defects with the Contralateral Nasolabial Island Flap. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg. 74(4):851–9 [DOI] [PubMed]
- 10.Shah GH, Misra G, Meena A (2021) Pedicled Islanded Nasolabial Flap tunneled under Mandible for Tongue Reconstruction. J Maxillofac Oral Surg 20(1):100–104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chakrabarti S, Gupta DK, Gupta M, Daga D, Mishra A, Sharma SS et al (2020) Versatility and reliability of Islanded Pedicled Nasolabial Flap in Head and Neck Cancer Reconstruction. Laryngoscope 130(8):1967–1972 [DOI] [PubMed] [Google Scholar]