Abstract
Purpose
Intraoperative identification and excision of specific lymphadenopathies is not always easy; it is, therefore, important to have complementary techniques that help us in the identification of these structures intraoperatively. The aim of this study is to present preliminary results of the use of ROLL technique (radioguided occult lesion localisation) as a method of excisional biopsy in the head and neck territory.
Material and methods
We present 10 cases of patients with difficult to localise lymphadenopathies in the head and neck territory that underwent the ROLL technique. The radiotracer was only injected in the nodes that we wanted to study; in this way, all of them were correctly identified and extracted without resecting those that had no signs of pathology avoiding removing healthy lymphatic tissue and reducing morbidity.
Results
The ROLL technique is a useful technique, since in all of the patients, the previously marked adenopathy was accurately identified and excised; we reduced the intraoperative time and avoided the complications derived from more aggressive cervical exploratory surgeries.
Keywords: ROLL, Radioguided surgery, Lymphadenopathy, Head and neck
Introduction
The term lymphadenopathy refers to the presence of a lymph node of abnormal size or consistency. Peripheral lymphadenopathy accounts for 0.6% of patients attending primary care. Most of the causes are usually benign such as infections, autoimmune diseases or iatrogenic causes, and 1% of cases are due to underlying malignant pathology. The probability of malignancy increases with age, being 4% after the age of 40 years and 0.4% below the age of 40 years [1].
The most common site of peripheral lymphadenopathy is the cervical area, and although they are usually self-limited, in persistent lymphadenopathies, it is important to carry out a structured differential diagnosis by means of a thorough anamnesis and physical examination, serological tests, imaging tests and biopsy, which will provide the definitive diagnosis [2]. Biopsy techniques can range from minimally invasive, such as fine-needle aspiration biopsy (FNA), through core needle biopsy (CNB) to excisional biopsy. Excisional biopsy is more sensitive for aetiological diagnosis as it allows an adequate sample size to be obtained to analyse and evaluate the architecture of the excised lymph node, which makes it the “gold standard” technique for the diagnosis of certain pathologies, such as lymphoma [3].
However, intraoperative localisation of lymphadenopathies in the head and neck territory is not always easy, as the cervical region has a lymphatic drainage that includes more than 100 lymph nodes [4]. This particularity can sometimes lead to the wrong lymph node being excised or even to the lymph node being mislocalised, resulting in blank biopsies. To avoid these unsuccessful biopsies, radioguided surgery techniques can be used [5].
The term GOSTT (Guided Intraoperative Scintigraphic Tumour Targeting) includes radioguided surgical procedures aimed at optimising minimally invasive tumour surgery, such as the detection of non-palpable lesions associated with sentinel node localisation (SNOLL) or the ROLL (radioguided occult lesion localisation) technique [6].
The ROLL technique is based on the injection of radioactive particles that remain stable at the injection site without migrating to other locations [7]. The application of this technique for the localisation of suspicious cervical adenopathies makes it possible to confirm, intraoperatively, that the adenopathy being removed is the one previously marked with the radiotracer [8], avoiding obtaining healthy lymphatic tissue, blank biopsies and reducing the morbidity and mortality caused by more aggressive surgeries derived from the "blind" search for adenopathies in complex anatomical locations [9].
The use of this procedure for the removal of specific adenopathies in the cervicofacial territory is not widely described in the literature. Therefore, the aim of this study is to define the specificity and sensitivity of the application of the ROLL technique in the excision of difficult to access or localise adenopathies in the head and neck territory.
Material and Methods
Approval was obtained from the ethics committee of University Hospital La Princesa. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
In the Department of Oral and Maxillofacial Surgery of a third-level hospital, 25 patients with isolated cervical lymphadenopathy with radiological characteristics of malignancy were evaluated over a period of 18 months, between January 2021 and September 2022. Ten of them were prospectively selected during that time for the application of the ROLL technique in lymphadenopathy removal surgery. These patients were selected because they had particularly complex cervical lymphadenopathies, either because of their depth, their proximity to structures such as large vessels or relevant nerve structures, or because they had non-pathological lymph nodes in their surroundings that could act as confusing factors during the procedure. Fine-needle aspirations were not executed prior to the described procedure.
Once the radioguided excisional biopsy is performed, the surgical specimen is typically preserved in formalin and sent to the department of anatomical pathology for further analysis. However, in cases where haematological pathology is suspected, the specimens are sent in a fresh state to ensure optimal evaluation.
A descriptive analysis was performed of the results obtained in our department after the application of the ROLL technique in these kinds of suspicious lymph nodes.
Surgical Technique
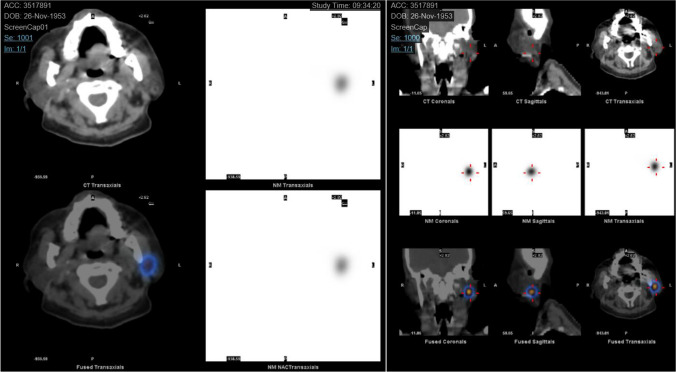
Firstly, the technical viability of injecting the radiotracer into the lymph node to be studied is confirmed under ultrasound (US) guidance. If this is technically possible, if the depth of the lesion and the visualisation with ultrasound allow it, the surgical intervention is scheduled in collaboration with the Nuclear Medicine Department of our hospital. On the scheduled day, the patient comes to the hospital on a 12-h fast, and the ultrasound-guided injection of the radiotracer is performed (Fig. 1). Immediately afterwards, a confirmatory SPECT-CT is then performed to confirm that the exact adenopathy has been marked by comparing these images with those of the previous diagnostic CT scan (Fig. 2). If the entire procedure has been carried out correctly, approximately 2 h later, the biopsy is performed in the operating room under general anaesthesia or sedation, depending on the patient's characteristics and the location of the lymph nodes.
Fig. 1.
Ultrasound-guided radiotracer injection
Fig. 2.
SPECT-CT showing the radiotracer injected in the specific adenopathy
Once in the operating room and with the patient already under anaesthesia, it is necessary to perform the external count with the gamma probe (GP) to determine the approximate location of the adenopathy. A GP is a portable instrument consisting of a detector, a preamplifier, a collimator, a screen and a sound signal generator. When the probe is brought close to the radioactive particles, the gamma photons detected by the crystal are both converted to an audible signal and to a digital numerical display that will show the counts. According to the inverse square principle, the count rate decreases proportionally with the square of the distance between the detector and the radioactive target. Thus, the principle of counting at three different locations is the basis of the technique. These three counting points are as follows: inside the patient or "in vivo", after removing the adenopathy outside the patient or "ex vivo", and in the remaining tissue of the surgical field (Table 1). With these principles in mind, the surgery is guided by the probe counting, from the most appropriate place for the approximate incision to the exact location of the lymph node. The marked lymph node is identified by comparing its radioactive activity with the underlying activity, which is defined as the average of the count rate of the surrounding tissue field [10]. Generally, the ratio of beads of the lymph node to be marked to the background varies from 10:1 to 20:1. Once located, the counts are measured at the three points in order to confirm the excision of all the marked tissue (Fig. 3).
Table 1.
Counting points, possible results and interpretation
| In vivo | Ex vivo | Surgical bed | Interpretation |
|---|---|---|---|
| + | + | − | The correct adenopathy completely removed |
| + | − | + | The incorrect adenopathy removed |
| + | + | + | The correct adenopathy not completely removed |
| + | − | − | Additional tissue technical errors |
Fig. 3.

Intraoperative correct excision confirmation with the gamma probe
Results (Table 2)
Table 2.
Results
| No. of patients | N = 10 | ||
|---|---|---|---|
| Sex | Six women | ||
| Four men | |||
| Age | Average 64 years | ||
| Previous pathology | Squamous cell carcinoma | 3 | |
| Lymphoma | 4 | ||
| Suspected malignancy | 2 | ||
| Melanoma | 1 | ||
| Localisation | Deep laterocervical | 6 | 1 level Ib |
| 2 level IIb | |||
| 3 level IIIb | |||
| Supraclavicular | 2 | 2 level IVb | |
| Intraglandular (parotid gland) | 2 | ||
| Histology | Schwannoma | 1 | |
| Reactive lymphadenitis | 8 | ||
| Ganglionar metastasis | 1 | ||
Of the 10 patients selected, 6 were female (60%) and 4 were male (40%) with a mean age of 64 years [48–73]. The previous pathology presented in 4 (40%) of them was squamous cell carcinoma of the head and neck, 3 (30%) were diagnosed with lymphoma, 2 (20%) had suspected malignant lymphadenopathy of unknown origin and 1 (10%) was diagnosed with melanoma. The location of the adenopathies was in the cervical lymph node territory in 80% of the cases (one in level Ib, two in level IIb, three in level III and two in level IV), while in 20% of the cases, the location was intraglandular, 100% of these being intraparotid.
In cases where locoregional metastasis was suspected, specifically in squamous cell carcinoma and melanoma, the lymphadenopathies were found on the same side as the primary tumour. In cases where haematological neoplasms were suspected, bilateral cervical lymphadenopathies were observed, and the lymph node with the highest radiological suspicion was identified and marked with the radiotracer. In two of the three cases, the supraclavicular lymphadenopathies exhibited the highest radiological suspicion; in the third case, the radiologically most suspicious lymph node was located at the cervical level III. Lastly, intraparotid lymphadenopathies were considered suspicious for tumours of unknown origin.
In the 100% of the patients, we obtained a reliable pathological diagnosis as the entire lymphadenopathy was removed, and blank biopsies were avoided since enough sample was extracted.
The definitive histological diagnosis showed the following results: Only one of the cases was metastatic lymph nodes while eight were diagnosed of reactive lymphadenitis, and in the remaining patient, a neurological tumour was found (Table 2). For the patient with positive findings of metastatic squamous cell carcinoma, a functional ipsilateral cervical lymph node dissection was performed. Patients diagnosed with reactive lymphadenitis were monitored until complete clinical resolution, which was achieved in all cases. Schwannoma case was referred to our hospital's neurosurgery department for appropriate surgical intervention and subsequent radiotherapy.
The ROLL technique had a sensitivity and specificity in this sample of 100% for the diagnosis and removal of these specific lymph nodes, avoiding greater morbidity from more aggressive surgeries derived from the unguided search for lymph nodes and the removal of more lymph node tissue than necessary for diagnosis. At the same time, there were no complications derived from the technique except for surgical wound infection in one of the 10 patients.
Discussion
The ROLL technique is based on the injection of radioactive particles that remain stable at the injection site without migrating to other locations, which differs from the sentinel lymph node technique where a radiotracer capable of migrating from the tumour to the lymph node drainage territory is required. In both procedures, the particle used will be Technetium-99 (99-Tc); however, in the sentinel lymph node technique, it is in nanocolloid form (80 mn), while in the ROLL technique, it will be associated with macroaggregates of albumin (MAA) (10–90 m), which will give the particle size and stability necessary to remain at the injection site [11].
This procedure was originally described for the detection of occult deep lesions in breast cancer [12] and has now gained importance in the treatment of head and neck cancer, especially in thyroid tumours [13]. On the one hand, in non-palpable breast lesions, it has been demonstrated to reduce surgical time, and, in addition, it helps to identify the incision site as it is guided by the gamma probe [14]. On the other hand, in thyroid cancer and especially in recurrences, it has been shown to improve tumour localisation, to increase the surgical success rate and to reduce morbidity [15].
Over time, the use of this technique has become increasingly relevant and has been extended to other applications, such as the localisation of deep non-breast lesions [16], the detection of non-palpable adenopathies in lymphomas [17] and the localisation of hypermetabolic adenopathies suspicious of malignancy in different territories detected on PET/CT [18]. However, there are few studies in the literature focusing on the use of the ROLL technique for the localisation and excision of suspicious lymphadenopathies in the head and neck territory specifically. It is in this anatomical area where its application may become more relevant, especially in the location of lymphadenopathies that are difficult to access due to their complex anatomy, such as the most posterior area of cervical level V, the supraclavicular fossa or below the body or mandibular angle [19]. It can also be useful in intraglandular territories such as at the parotid region, where there are a large number of lymph nodes that can act as a confounding factor [20], or in cases, where the anatomy is disrupted by the presence of fibrous tissue resulting from surgery or previous radiotherapy treatment [21].
In addition to assisting the surgeon in the localisation of certain structures, it avoids the complications of more aggressive surgical dissections derived from the traditional search for lymphadenopathies. In the case of parotid lymph nodes, it avoids noble structures such as the facial nerve. Thus, none of the patients in our sample with intraglandular lymphadenopathy developed either paresis or paraesthesia of any branch of the seventh nerve. In the same way, it avoids spinal nerve injury in territories of the posterior cervical triangle [22]. It is a safe and minimally invasive technique: In our sample, the patients did not present any complications derived from the technique, from the difficulty involved in the location of the lesions of interest, nor was there any damage to noble anatomical structures. Only one of the 10 patients had a complication, and it was derived from infection of the surgical wound, which was resolved after a week of antibiotic treatment.
The ROLL technique is a comfortable procedure for both the patient and the surgeon. On the one hand, in contrast with the wire lesion marking technique, in which the injection of the radiotracer has to be performed at least 24 h before surgery, this technique allows the injection and biopsy to be performed on the same day. On the other hand, it allows the surgeon to make the incision in a completely different location than the injection site of the radiotracer, as the entry location of the harpoon is not always optimal for the incision and can lead to unsatisfactory aesthetic results [23]. In addition, the ROLL technique has been shown to be more accurate in marking the lesion, guiding the surgery more precisely and allowing for safer free margins of the resected tissue [24].
Potential disadvantages of the technique are undoubtedly the need to involve other medical departments, such as the nuclear medicine department, and the difficulty in the organisation and the scheduling of the surgical procedure. On the other hand, it slightly increases the cost of the procedure. Those disadvantages that will actually lead to an unfavourable technical outcome are related to the extravasation of the radiotracer, the contamination of the skin or the injection site or, in the case of radioguided breast surgery, ductal infusion of the radiotracer [25]. In our case, we had no complications arising from the procedure itself.
The ROLL technique has proven to be an effective technique for intraoperative localisation of complex lymphadenopathies in the maxillofacial territory with a sensitivity and specificity of 100%, although studies with larger sample sizes are needed to support these results. This, together with the reduction of postoperative morbidity derived from more aggressive surgeries in which a greater amount of lymphatic tissue is removed than necessary, as well as the reduction of intraoperative time by enabling the localisation of the lymph nodes, makes the ROLL technique a procedure to be taken into account in the localisation and excision of selected lymphadenopathies that are difficult to access or locate in the head and neck area.
Acknowledgements
All authors certify that they have no affiliations with or involvement in any organisation or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Author Contributions
MFM, VCM and IHP helped in conceptualisation. MFM, VCM, ILV, IHP and VEH helped in methodology. MFM, VCM, IHP, VEH, ILV and MFM-G worked in formal analysis and investigation. MFM contributed to writing—original draft preparation. VCM, IHP, ILV and VEH contributed to writing—review and editing. MFM-G worked in resources. MFM-G and VEH worked in supervision. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Declarations
Conflict of Interest
All authors certify that they have no affiliations with or involvement in any organisation or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical Approval
Approval was obtained from the ethics committee of University Hospital La Princesa. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Richner S, Laifer G (2010) Peripheral lymphadenopathy in immunocompetent adults. Swiss Med Wkly 140(7–8):98–104 (PMID: 20069473) [DOI] [PubMed] [Google Scholar]
- 2.Lee Y, Terry R, Lukes RJ (1980) Lymph node biopsy for diagnosis: a statistical study. J Surg Oncol 14(1):53–60. 10.1002/jso.2930140108. (PMID: 7382513) [DOI] [PubMed] [Google Scholar]
- 3.Khalbuss WE, Teot LA, Monaco SE (2010) Diagnostic accuracy and limitations of fine-needle aspiration cytology of bone and soft tissue lesions: a review of 1114 cases with cytological-histological correlation. Cancer Cytopathol 118(1):24–32. 10.1002/cncy.20058. (PMID: 20091838) [DOI] [PubMed] [Google Scholar]
- 4.Kulzer MH, Branstetter BF (2017) Chapter 1. Neck anatomy, imaging-based level nodal classification and impact of primary tumor site on patterns of nodal metastasis. Semin Ultrasound CT MR 38: 454–465 [DOI] [PubMed]
- 5.Vidal-Sicart S, Fuertes Cabero S, Danús Lainez M, Valdés Olmos R, Paredes Barranco P, Rayo Madrid JI, Rioja Martín ME, Díaz Expósito R, Goñi Gironés E (2019) Update on radioguided surgery: from international consensus on sentinel node in head and neck cancer to the advances on gynaecological tumors and localization of non-palpable lesions. Rev Esp Med Nucl Imagen Mol 38(3):173–182. 10.1016/j.remn.2018.10.007. (Epub 2018 Dec 20. PMID: 30579916) [DOI] [PubMed] [Google Scholar]
- 6.Bowles H, Sánchez N, Tapias A, Paredes P, Campos F, Bluemel C, Valdés Olmos RA, Vidal-Sicart S (2017) Radioguided surgery and the GOSTT concept: From pre-operative image and intraoperative navigation to image-assisted excision. Rev Esp Med Nucl Imagen Mol 36(3):175–184. 10.1016/j.remn.2016.09.004. (Epub 2016 Oct 25. PMID: 27793632) [DOI] [PubMed] [Google Scholar]
- 7.Süslü NS, Katar O, Tuncel M (2022) Role of indocyanine green combined with radiotracer-Technetium 99 m in neck surgery for primary and recurrent head and neck cancer: preliminary results of a tertiary cancer center. Eur Arch Otorhinolaryngol 279(3):1549–1560. 10.1007/s00405-021-06931-1. (Epub 2021 Jun 19 PMID: 34146148) [DOI] [PubMed] [Google Scholar]
- 8.Manca G, Mazzarri S, Rubello D, Tardelli E, Delgado-Bolton RC, Giammarile F, Roncella M, Volterrani D, Colletti PM (2017) Radioguided occult lesion localization: technical procedures and clinical applications. Clin Nucl Med 42(12):e498–e503. 10.1097/RLU.0000000000001858. (PMID: 29035996) [DOI] [PubMed] [Google Scholar]
- 9.Borsò E, Grosso M, Boni G, Manca G, Bianchi P, Puccini M, Arganini M, Cabria M, Piccardo A, Arlandini A, Orlandini C, Mariani G (2013) Radioguided occult lesion localization of cervical recurrences from differentiated thyroid cancer: technical feasibility and clinical results. Q J Nucl Med Mol Imaging 57(4):401–411 (PMID: 24322795) [PubMed] [Google Scholar]
- 10.Ingeniería 19 (1): 87–96, ISSN: 1409-2441; 2009. San José, Costa Rica
- 11.de la Riva Pérez PA, Carrera Salazar D, Paredes Barranco P, Goñi GE (2022) Survey of the radioguided surgery working group (GTCRG-RGSWG) of the Spanish Society of Nuclear Medicine and Molecular Imaging (SEMNIM): radioguided localization of non-palpable breast lesions with or without indication for selective sentinel node biopsy: ROLL, SNOLL and 125I seeds. Rev Esp Med Nucl Imagen Mol 41(4):223–230. 10.1016/j.remnie.2022.05.014 [DOI] [PubMed] [Google Scholar]
- 12.Niinikoski L, Hukkinen K, Leidenius MHK, Vaara P, Voynov A, Heikkilä P, Mattson J, Meretoja TJ (2019) Resection margins and local recurrences of impalpable breast cancer: Comparison between radioguided occult lesion localization (ROLL) and radioactive seed localization (RSL). Breast 47:93–101. 10.1016/j.breast.2019.07.004. (Epub 2019 Jul 23 PMID: 31362135) [DOI] [PubMed] [Google Scholar]
- 13.Dalcı K, Topal U, Ünal AG, Eray İC, Yalav O, Güney İB, Sakman G (2019) Is radioguided occult lesion localization (ROLL) an effective and reliable method in thyroid cancer and parathyroid redo surgery? Ann Ital Chir 8:S0003469X19031464 [PubMed] [Google Scholar]
- 14.Kiruparan N, Kiruparan P, Debnath D (2022) Use of wire-guided and radio-guided occult lesion localization for non-palpable breast lesions: a systematic literature review and meta-analysis of current evidence. Asian J Surg 45(1):79–88. 10.1016/j.asjsur.2021.06.055. (Epub 2021 Sep 1 PMID: 34479779) [DOI] [PubMed] [Google Scholar]
- 15.Tuncel M, Süslü N (2019) Radioguided occult lesion localization in patients with recurrent thyroid cancer. Eur Arch Otorhinolaryngol 276(6):1757–1766. 10.1007/s00405-019-05377-w. (Epub 2019 Mar 18 PMID: 30887167) [DOI] [PubMed] [Google Scholar]
- 16.Infante JR, Rayo JI, Serrano J, Domínguez ML, García L, Durán C, Moreno M (2015) Aplicación clínica de la técnica ROLL en patología no mamaria. Uso complementario tras estudio PET-TAC [Clinical application of ROLL technique in non-breast diseases. Complementary use after PET-CT study]. Rev Esp Med Nucl Imagen Mol 34(3):162–166. 10.1016/j.remn.2014.08.006. (Epub 2014 Oct 8. PMID: 25304844) [DOI] [PubMed] [Google Scholar]
- 17.Cadena-Piñeros E, Parra-Charris JS (2019) Radioguided surgery of non-palpable neck lymph node in lymphoma patients. Indian J Otolaryngol Head Neck Surg. 71(4):430–434. 10.1007/s12070-019-01591-4. (Epub 2019 Jan 19. PMID: 31750099; PMCID: PMC6838245) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Infante JR, Rayo JI, Serrano J, Jiménez JL, Moreno M, Martínez A, Jiménez P, Cobo A (2021) Application of the ROLL technique as a method of excisional biopsy in oncological pathology. Cir Esp (Engl Ed). 99(1):49–54. English, Spanish. 10.1016/j.ciresp.2020.04.005. Epub 2020 May 6. PMID: 32386936 [DOI] [PubMed]
- 19.Lallemant B, Mallet Y, Ala-Eddine C, Lartigau E, Lefèbvre JL (2003) La classification radio-chirurgicale des niveaux ganglionnaires cervicaux [Radiological and surgical classification of head and neck lymph node anatomy]. Ann Otolaryngol Chir Cervicofac 120(4):216–224 (French. PMID: 13130297) [PubMed] [Google Scholar]
- 20.Zhang MH, Ginat DT (2020) Normative measurements of parotid lymph nodes on CT imaging. Surg Radiol Anat 42(9):1109–1112. 10.1007/s00276-020-02494-8. (Epub 2020 May 14 PMID: 32410047) [DOI] [PubMed] [Google Scholar]
- 21.Sroussi HY, Epstein JB, Bensadoun RJ, Saunders DP, Lalla RV, Migliorati CA, Heaivilin N, Zumsteg ZS (2017) Common oral complications of head and neck cancer radiation therapy: mucositis, infections, saliva change, fibrosis, sensory dysfunctions, dental caries, periodontal disease, and osteoradionecrosis. Cancer Med 6(12):2918–2931. 10.1002/cam4.1221. (Epub 2017 Oct 25. PMID: 29071801; PMCID: PMC5727249) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chiesa-Estomba CM, Soriano-Reixach M, Thomas-Arrizabalaga I, Sistiaga-Suarez JA, González-García JA, Larruscain E, Altuna X (2021) Complications after functional neck dissection in head and neck cancer patients: an observational, retrospective, single-centre study. ORL J Otorhinolaryngol Relat Spec 83(5):372–380. 10.1159/000514459. (Epub 2021 May 19 PMID: 34010845) [DOI] [PubMed] [Google Scholar]
- 23.Nadeem R, Chagla LS, Harris O, Desmond S, Thind R, Titterrell C, Audisio RA (2005) Occult breast lesions: a comparison between radioguided occult lesion localisation (ROLL) vs. wire-guided lumpectomy (WGL). Breast 14(4):283–289. 10.1016/j.breast.2005.04.002. (PMID: 15985370) [DOI] [PubMed] [Google Scholar]
- 24.Moreira IC, Ventura SR, Ramos I, Fougo JL, Rodrigues PP (2020) Preoperative localisation techniques in breast conservative surgery: a systematic review and meta-analysis. Surg Oncol 35:351–373. 10.1016/j.suronc.2020.09.004. (Epub 2020 Sep 16. PMID: 33002840) [DOI] [PubMed] [Google Scholar]
- 25.Tayeh S, Wazir U, Mokbel K (2021) The evolving role of radiofrequency guided localisation in breast surgery: a systematic review. Cancers (Basel) 13(19):4996. 10.3390/cancers13194996. (PMID: 34638480; PMCID: PMC8508195) [DOI] [PMC free article] [PubMed] [Google Scholar]